Importance of Rose Bengal Loaded with Nanoparticles for Anti-Cancer Photodynamic Therapy
Abstract
:1. Introduction
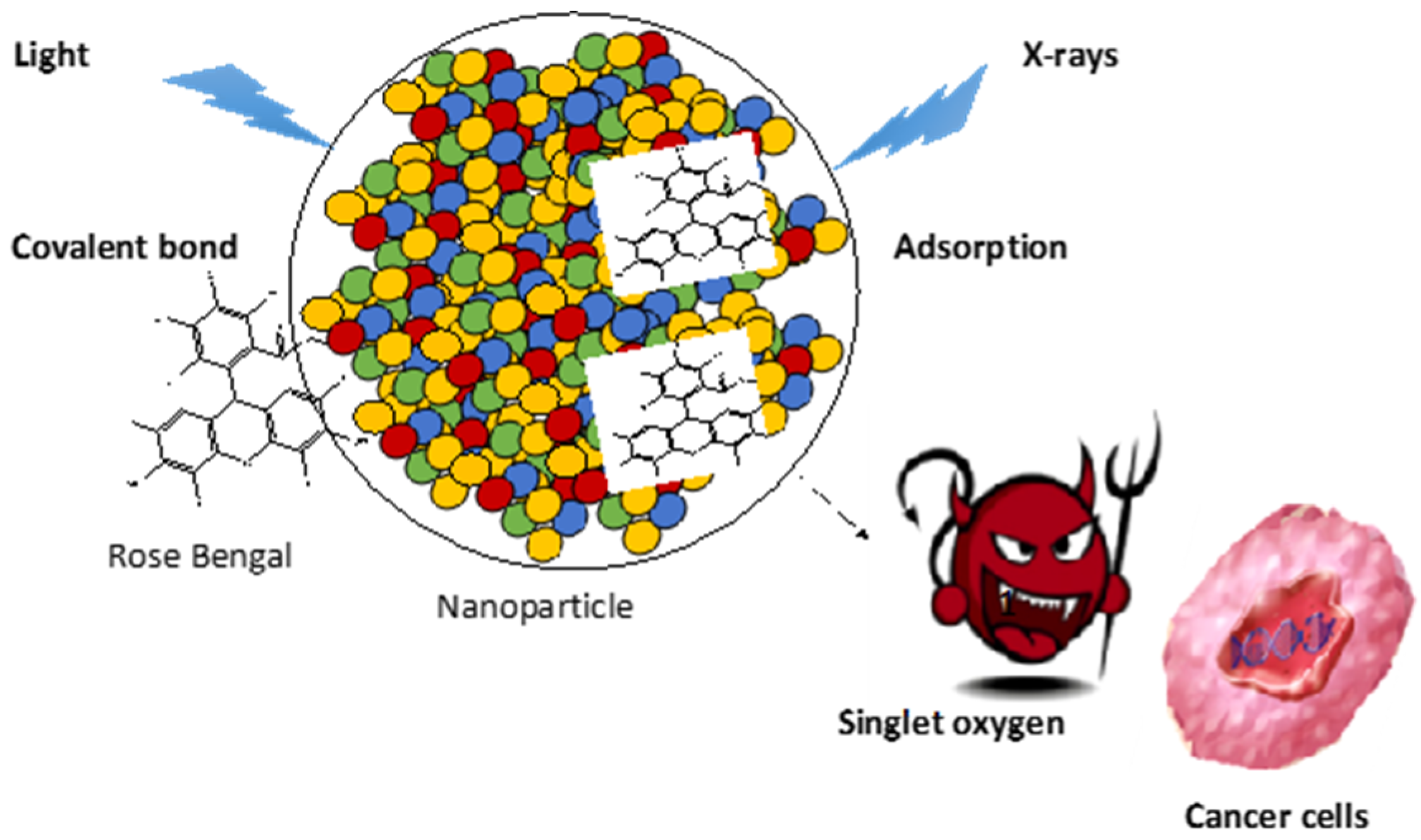
2. Photodynamic Therapy
2.1. Upconversion Nanoparticles (UCNPs)
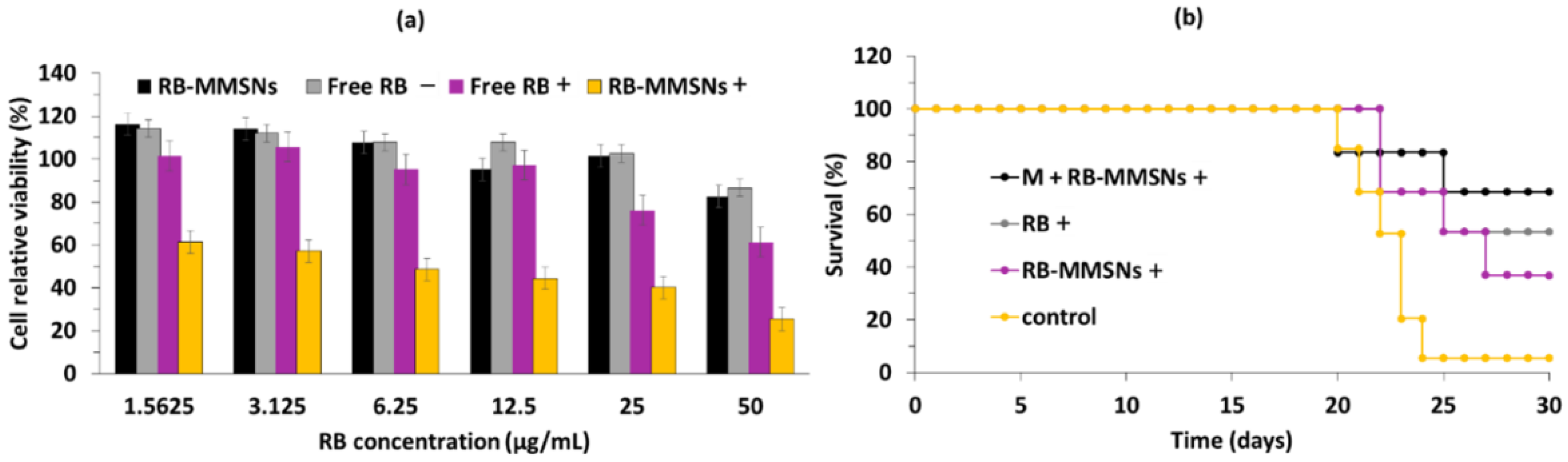
2.2. Silica Nanoparticles
2.3. Organic NPs (Polymers, Micelles, Peptides)
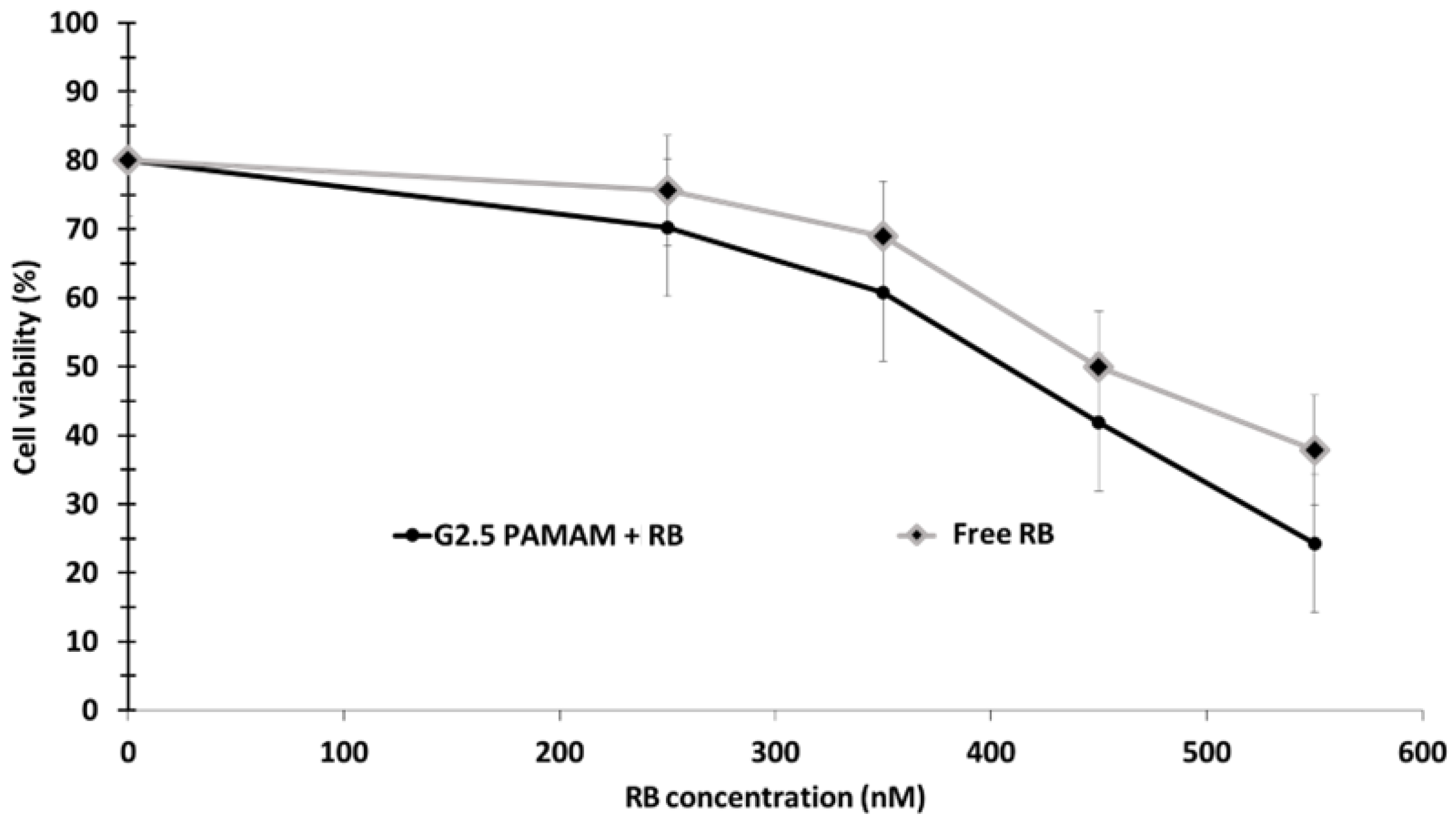
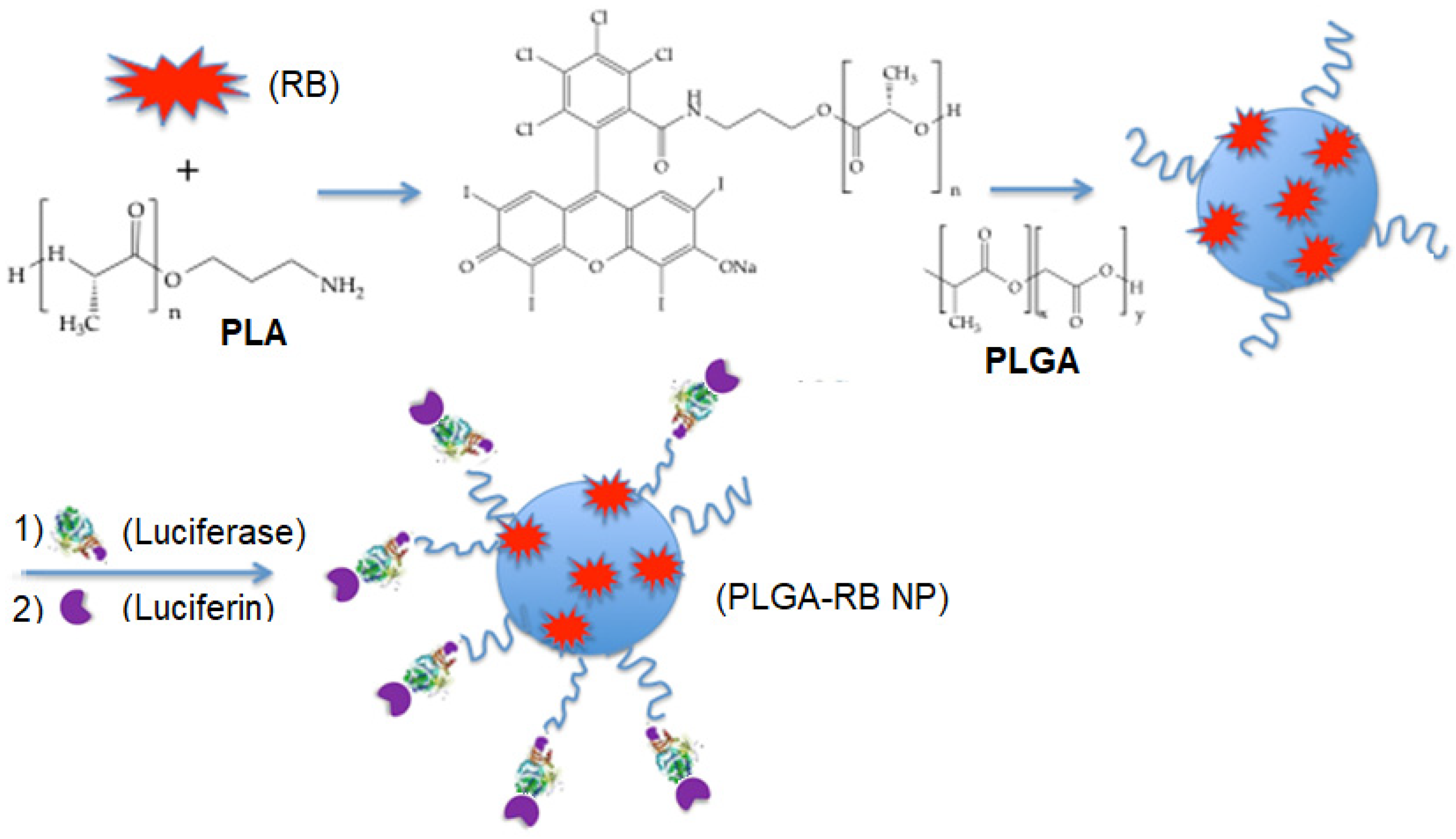
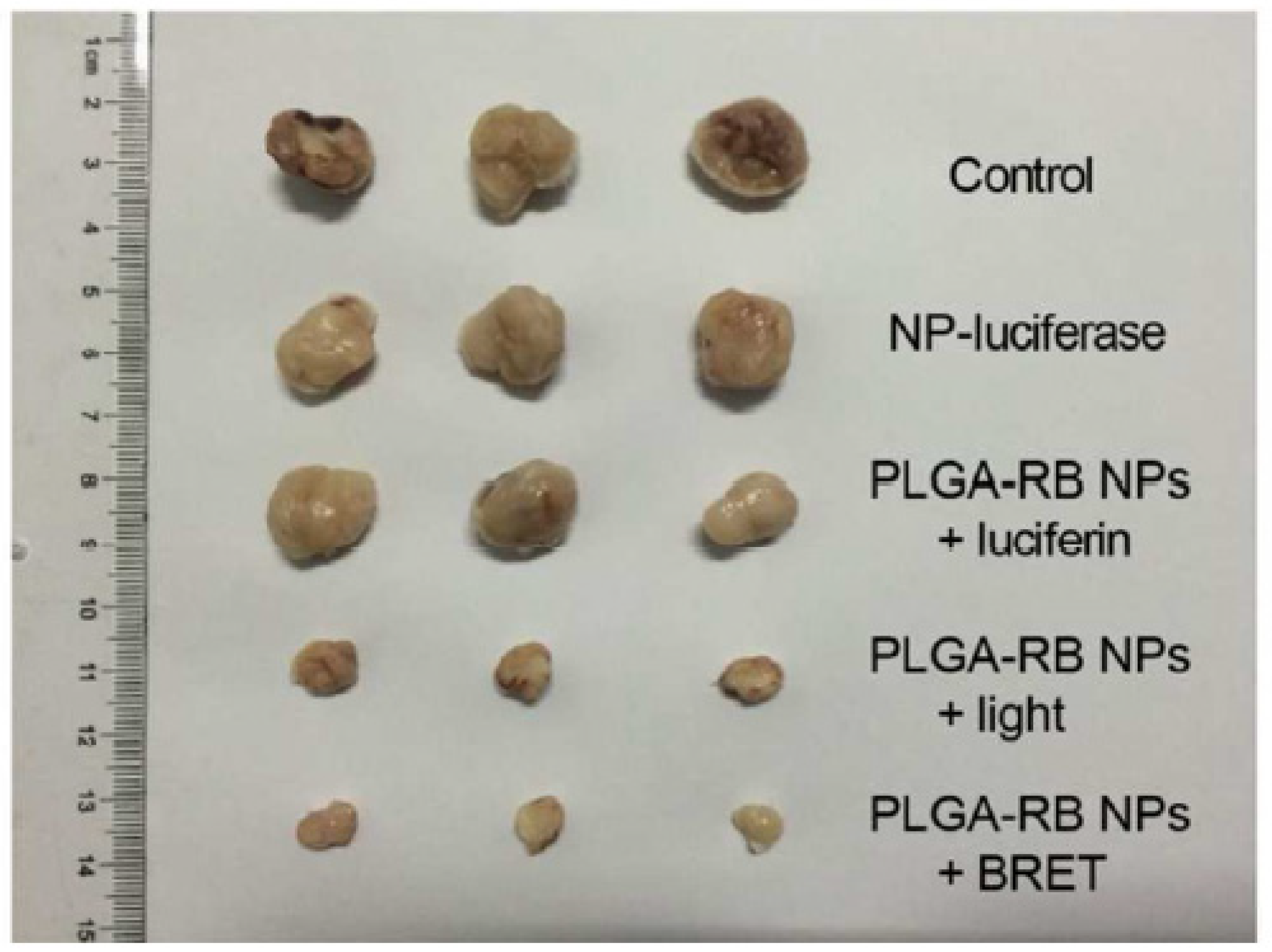
2.3.1. Polymer NPs
2.3.2. Peptide NPs
2.3.3. Micelle NPs
2.4. Gold Nanoparticles
2.5. Polymer Dot Nanoparticles
2.6. Other Nanoparticles
2.6.1. Nanocapsules
2.6.2. Nanocomplexes
2.6.3. Magnetic Nanoparticles
2.6.4. pH-Sensitive Nanoparticles
2.6.5. Nanohybrid Nanoparticles
2.6.6. Nanogels
3. X-ray Photodynamic Therapy (X-PDT)
3.1. Silica Nanoparticles
3.2. Polymer Nanoparticles
3.3. Nanocomposites
3.4. Other Nanoparticles
3.4.1. Mesoporous LaF3:Tb Scintillating Nanoparticles
3.4.2. Nanophosphors
3.4.3. Lanthanide@MOF Nanoprobes
4. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AB3 | Anti-cancer drug |
| ABDA | 9,10-Anthracenediyl-bis(methylene) dimalonic acid |
| ABMDMA | 9,10-Anthracenediyl-bis(methylene)dimalonic acid |
| ABS | Acetate buffer solution |
| ADPA | 10-dipropionic acid, disodium salt |
| AEP | 2-aminoethyl dihydrogen phosphate |
| AFM | Atomic force microscope |
| ATF | Amino terminal fragment of urokinase plasminogen activator |
| AuNPs | Gold nanoparticles |
| Azo | Azobenzene |
| BFNS | Bifunctional nanospheres |
| BP | Bis-pyrene |
| bPEI | Branched polyethylenimine |
| BRET | Bioluminescence resonance energy transfer |
| BSA | Bovine serum albumin |
| BTSA | Bis(trimethylsilyl)acetamide |
| BT | Barium–titanate |
| CaB | Cathepsin B |
| CD | Cyclodextrin |
| cDDP | Cis-diaminedichloroplatine(II) |
| Ce6 | Chlorin e6 |
| CLSM | Confocal laser scanning microscopy |
| CQDs | Carbon quantum dots |
| CR | Core–satellite superstructure |
| C18RB | Hydrocarbonized RB |
| Cs-Na | Nitroimidazole-modified chitosan |
| CTAB | Cetyltrimethylammoniumbromide |
| CTS | Chitosan |
| Cy3 | Cyanine 3 |
| DCFH-DA | Dichlorodihydrofluorescein-diacetate |
| DLS | Dynamic light scattering |
| DMA | 9,10-Dimethylanthracene |
| DNA | Deoxyribonucleic acid |
| DOX | Doxorubicin |
| DPBF | 1,3-diphenylisobenzofuran |
| EADC | 1-Ethyl-3-(3-dimethylaminopropyl)carbodiimide |
| EDC | N-Ethyl-N′-(3-(dimethylamino)propyl)carbodiimide |
| EPR | Enhanced permeability effect |
| FA | Folic acid |
| FITS | Fluorescein isothiocyanate |
| FRET | Förster resonance energy transfer |
| 5FU | 5-Fluorouracil |
| GG | Guar gum |
| GRDs | Gadolinium-rose bengal coordination polymer nanodots |
| GSH | Glutathione |
| HA | Hyaluronic acid |
| HAx | Hexamethylenediamine |
| HCPT | 10-Hydroxycamptothecin |
| HMSNs | Hollow mesoporous silica nanoparticles |
| HSPC | Hydrogenated soy L-a-phosphatidylcholine |
| IR | Infrared |
| IR825 | NIR-absorbing dye |
| LIFU | Low-intensity focused ultrasound |
| Ln | Lanthanide |
| LNP | Luminescent lanthanide nanoparticles |
| MB | Methylene blue |
| MF | Multifunctional |
| MMSN | Magnetic mesoporous silica nanoparticle |
| MNCs | Magnetic nanoclusters |
| Mo | Oxymolybdate |
| MOF | Metal–organic frameworks |
| MRI | Magnetic resonance imaging |
| MS | Mesoporous silica |
| MSNs | Mesoporous silica nanoparticles |
| MTD | Maximum tolerated dose |
| MTT | 3-[4,5-Dimethylthiazol-2-yl]-2,5 diphenyl tetrazolium bromide |
| MUCNPs | Multi-shelled upconversion nanoparticles |
| NCs | Nanocarriers |
| Nd | Not determined |
| NHS | N-Hydroxysuccinimide |
| NIR | Near infrared |
| NPs | Nanoparticles |
| OA | Oleic acid |
| 1O2 | Singlet oxygen |
| PAA | Polyacrylic acid |
| PAH | Poly(allylamine) |
| PAMAM | Poly(amidoamine) |
| PARN | Amphiphilic peptide nanocapsules |
| PBS | Phosphate buffer solution |
| PCL | PEG-block-poly(ε-caprolactone) |
| Pdots | Polymer dots |
| PDT | Photodynamic therapy |
| PE | Phosphoethanolamine |
| PEG | Polyethyleneglycol |
| PEG-b-PAsp | Polyethylene glycol-b-poly(aspartic acid) |
| PEI | Polyethylene imine |
| PE-NH2 | 1,2-Dioleoyl-sn-glycero-phosphoethanolamine-N(hexanoylamine) |
| PFH | Perfluorohexane |
| PGA | Poly(glycolic acid) |
| PHLA | Partially hydrolyzed α-lactalbumin |
| p.i | Post injection |
| PLA | Poly(lactic acid) |
| PLGA | Poly(lactic-co-glycolic acid) |
| PPADT | Poly-(1,4-phenyleneacetone dimethylenethioketal) |
| PS | Photosensitizer |
| PTT | Photothermal therapy |
| PTX | Paclitaxel |
| PVA | Poly(vinyl alcohol) |
| PVK | Poly(N-vinyl carbazole) |
| QDs | Quantum dots |
| QSY7 | ROS quenching |
| RB | Rose Bengal |
| RBD | Rose bengal ω-carboxyheptyl ester |
| RET | Resonance energy transfer |
| ROS | Reactive oxygen species |
| ScNPs | Scintillating nanoparticles |
| SHG | Second harmonic generation |
| SOSG | Singlet oxygen sensor green |
| SSTRs | Somatostatin receptors |
| TEM | Transmission emission microscopy |
| TEOS | Tetraethyl orthosilicate |
| TMP–OH | 2,2,6,6-Tetramethyl-4-piperidinol |
| TOPO | Trioctylphosphine oxide |
| TPA | Two-photon activation |
| TUNEL | Terminal deoxynucleotidyl transferase dUTP nick end labeling |
| UCL | Upconversion luminescence |
| UCNPs | Upconversion nanoparticles |
| UPA | Urokinase plasminogen activator |
| US | Ultrasound |
| UV | Ultraviolet |
| WEN | White emitting NaYF4 |
| XLNPs | X-ray-luminescent nanoparticles |
| X-PDT | Photodynamic therapy induced by X-ray |
| ZIF-90 | Zeolitic imidazolate framework-90 |
| ZnPc-COOH | Zinc β-carboxyphthalocyanine |
References
- Malik, R.; Manocha, A.; Suresh, D. Photodynamic therapy—A strategic review. Indian J. Dent. Res. 2010, 21, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Selvasekar, C.R.; Birbeck, N.; McMillan, T.J.; Wainwright, M.; Walker, S.J. Photodynamic therapy and the alimentary tract. Aliment. Pharmacol. Ther. 2001, 15, 899–915. [Google Scholar] [CrossRef] [PubMed]
- Stranadko, E.P.; Ponomarev, G.V.; Mechkov, V.; Ryabov, M.; Ivanov, A.V.; Reshetnickov, A.V.; Koraboyev, U.M. First experience of photodithazine clinical application for photodynamic therapy of malignant tumors. In Proceedings of the Optical Methods for Tumor Treatment and Detection: Mechanisms and Techniques in Photodynamic Therapy IX, San Jose, CA, USA, 29 March 2000; pp. 138–144. [Google Scholar]
- Macdonald, I.J.; Dougherty, T.J. Basic principles of photodynamic therapy. J. Porphyr. Phthalocyanines 2001, 5, 105–129. [Google Scholar] [CrossRef]
- Lan, M.; Zhao, S.; Liu, W.; Lee, C.S.; Zhang, W.; Wang, P. Photosensitizers for photodynamic therapy. Adv. Healthc. Mater. 2019, 8, 1900132. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.-D.; Ye, J.; Zhang, X.-Q.; Zhang, N.; Xiao, M.-T. Recent advances in supramolecular activatable phthalocyanine-based photosensitizers for anti-cancer therapy. Coordin. Chem. Rev. 2021, 447, 214155. [Google Scholar] [CrossRef]
- Li, D.; Pan, J.; Xu, S.; Fu, S.; Chu, C.; Liu, G. Activatable Second Near-Infrared Fluorescent Probes: A New Accurate Diagnosis Strategy for Diseases. Biosensors 2021, 11, 436. [Google Scholar] [CrossRef]
- Chatterjee, D.K.; Fong, L.S.; Zhang, Y. Nanoparticles in photodynamic therapy: An emerging paradigm. Adv. Drug Deliv. Rev. 2008, 60, 1627–1637. [Google Scholar] [CrossRef]
- Gunaydin, G.; Gedik, M.E.; Ayan, S. Photodynamic Therapy—Current Limitations and Novel Approaches. Front. Chem. 2021, 9, 400. [Google Scholar] [CrossRef]
- Chaudhuri, S.; Sardar, S.; Bagchi, D.; Dutta, S.; Debnath, S.; Saha, P.; Lemmens, P.; Pal, S.K. Photoinduced Dynamics and Toxicity of a Cancer Drug in Proximity of Inorganic Nanoparticles under Visible Light. ChemPhysChem 2015, 17, 270–277. [Google Scholar] [CrossRef]
- Mol, J.A.; Docter, R.; Hennemann, G.; Visser, T.J. Modification of rat liver iodothyronine 5′-deiodinase activity with diethylpyrocarbonate and Rose Bengal; Evidence for an active site histidine residue. Biochem. Biophys. Res. Commun. 1984, 120, 28–36. [Google Scholar] [CrossRef]
- Machado, L.M.; Castro, R.S.; Fontes, B.M. Staining Patterns in Dry Eye Syndrome: Rose Bengal versus Lissamine Green. Cornea 2009, 28, 732–734. [Google Scholar] [CrossRef] [PubMed]
- Qin, J.; Kunda, N.; Qiao, G.; Calata, J.F.; Pardiwala, K.; Prabhakar, B.S.; Maker, A.V. Colon cancer cell treatment with rose bengal generates a protective immune response via immunogenic cell death. Cell Death Dis. 2017, 8, e2584. [Google Scholar] [CrossRef] [PubMed]
- Zheng, B.; Zhong, D.; Xie, T.; Zhou, J.; Li, W.; Ilyas, A.; Lu, Y.; Zhou, M.; Deng, R. Near-infrared photosensitization via direct triplet energy transfer from lanthanide nanoparticles. Chem 2021, 7, 1615–1625. [Google Scholar] [CrossRef]
- Wang, J.; Deng, R. Energy Transfer in Dye-Coupled Lanthanide-Doped Nanoparticles: From Design to Application. Chem. Asian J. 2018, 13, 614–625. [Google Scholar] [CrossRef]
- Oar, M.A.; Serin, J.M.; Dichtel, W.R.; Fréchet, J.M.J.; Ohulchanskyy, T.Y.; Prasad, P.N. Photosensitization of Singlet Oxygen via Two-Photon-Excited Fluorescence Resonance Energy Transfer in a Water-Soluble Dendrimer. Chem. Mater. 2005, 17, 2267–2275. [Google Scholar] [CrossRef]
- Wilhelm, S. Perspectives for Upconverting Nanoparticles. ACS Nano 2017, 11, 10644–10653. [Google Scholar] [CrossRef]
- Huang, L.; Zhao, Y.; Zhang, H.; Huang, K.; Yang, J.; Han, G. Expanding Anti-Stokes Shifting in Triplet-Triplet Annihilation Upconversion for In Vivo Anticancer Prodrug Activation. Angew. Chem. 2017, 129, 14592–14596. [Google Scholar] [CrossRef]
- Han, S.; Deng, R.; Xie, X.; Liu, X. Enhancing Luminescence in Lanthanide-Doped Upconversion Nanoparticles. Angew. Chem. Int. Ed. 2014, 53, 11702–11715. [Google Scholar] [CrossRef]
- Liu, K.; Liu, X.; Zeng, Q.; Zhang, Y.; Tu, L.; Liu, T.; Kong, X.; Wang, Y.; Cao, F.; Lambrechts, S.; et al. Covalently Assembled NIR Nanoplatform for Simultaneous Fluorescence Imaging and Photodynamic Therapy of Cancer Cells. ACS Nano 2012, 6, 4054–4062. [Google Scholar] [CrossRef]
- Chen, Q.; Wang, C.; Cheng, L.; He, W.; Cheng, Z.; Liu, Z. Protein modified upconversion nanoparticles for imaging-guided combined photothermal and photodynamic therapy. Biomaterials 2014, 35, 2915–2923. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, L.; Dong, C.; Su, L.; Wang, H.; Chang, J. Smart pH-responsive upconversion nanoparticles for enhanced tumor cellular internalization and near-infrared light-triggered photodynamic therapy. Chem. Commun. 2015, 51, 406–408. [Google Scholar] [CrossRef] [PubMed]
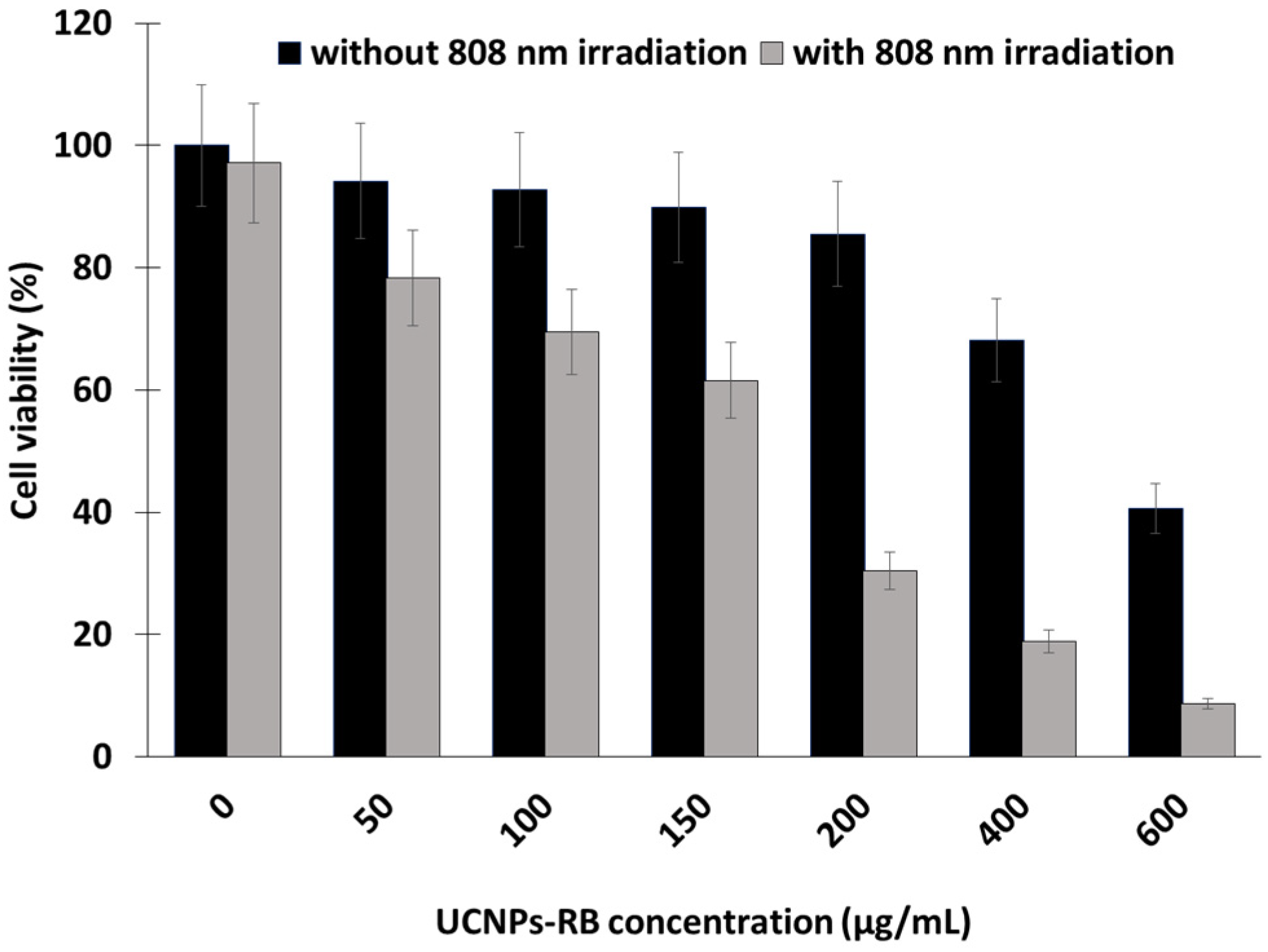
- Wang, D.; Xue, B.; Kong, X.; Tu, L.; Liu, X.; Zhang, Y.; Chang, Y.; Luo, Y.; Zhao, H.; Zhang, H. 808 nm driven Nd3+-sensitized upconversion nanostructures for photodynamic therapy and simultaneous fluorescence imaging. Nanoscale 2014, 7, 190–197. [Google Scholar] [CrossRef]
- Lu, S.; Tu, D.; Hu, P.; Xu, J.; Li, R.; Wang, M.; Chen, Z.; Huang, M.; Chen, X. Multifunctional Nano-Bioprobes Based on Rattle-Structured Upconverting Luminescent Nanoparticles. Angew. Chem. Int. Ed. 2015, 54, 7915–7919. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Tang, J.; Pan, D.-X.; Sun, L.-D.; Chen, C.; Liu, Y.; Wang, Y.-F.; Shi, S.; Yan, C.-H. A Versatile Imaging and Therapeutic Platform Based on Dual-Band Luminescent Lanthanide Nanoparticles toward Tumor Metastasis Inhibition. ACS Nano 2016, 10, 2766–2773. [Google Scholar] [CrossRef]
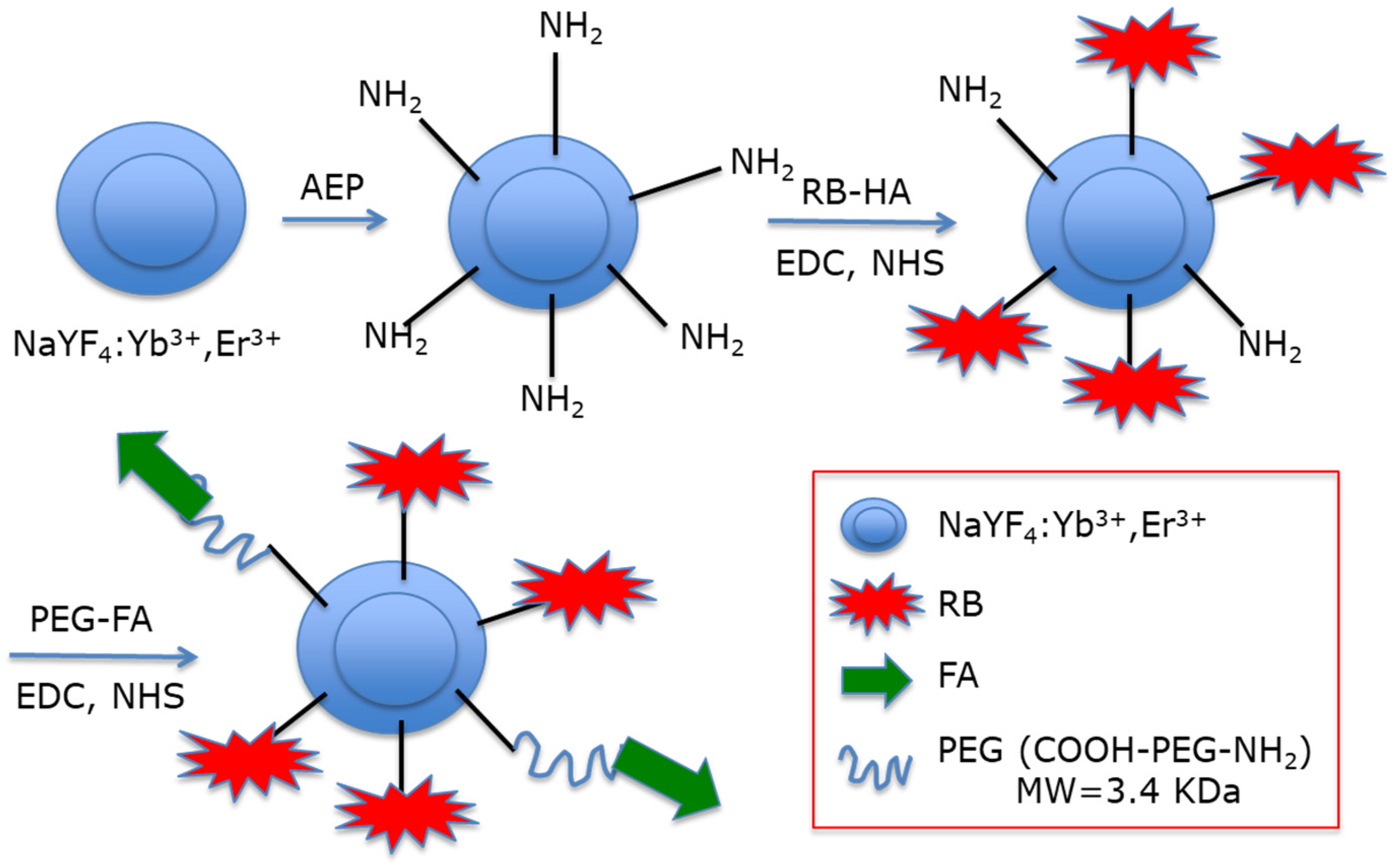
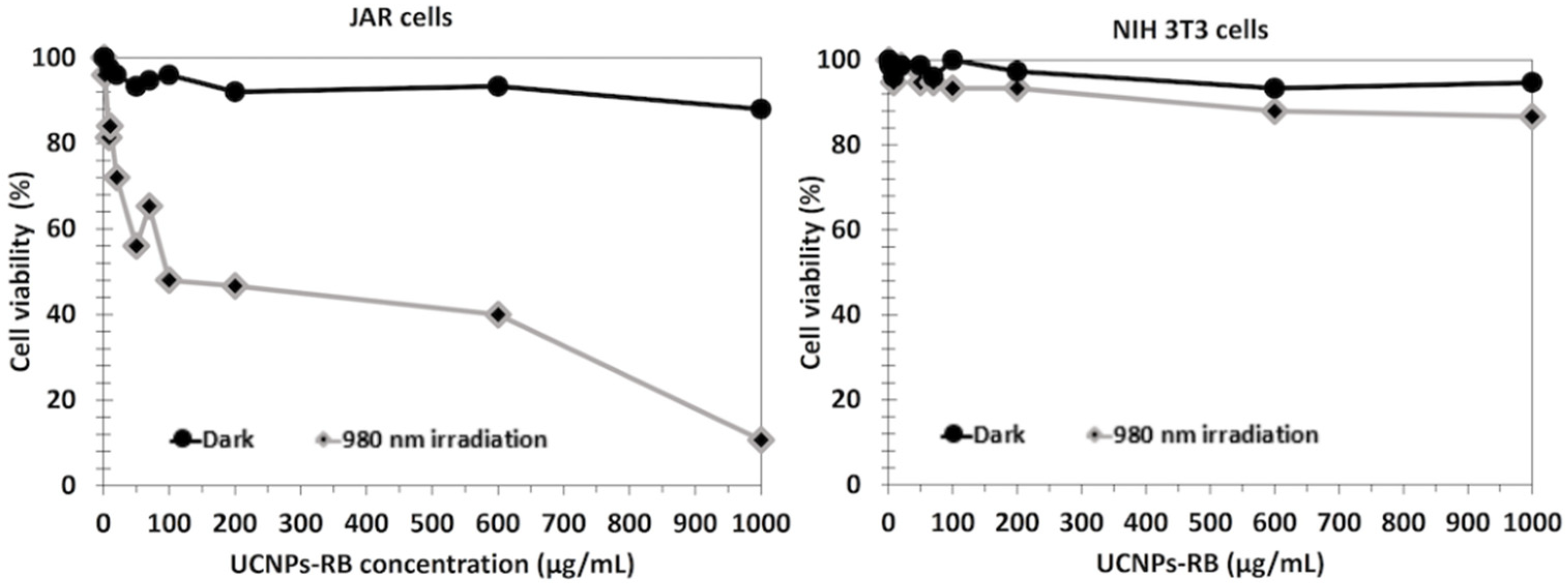
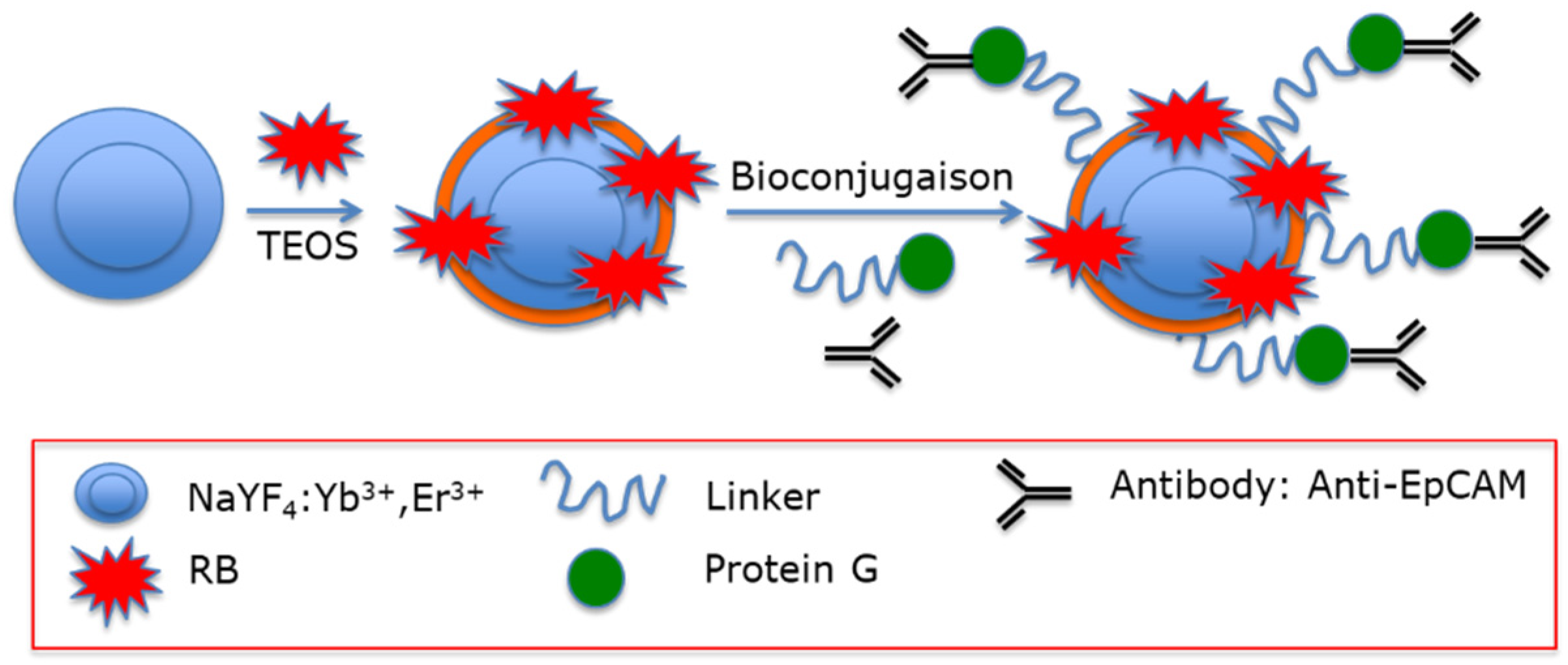
- Liang, L.; Care, A.; Zhang, R.; Lu, Y.; Packer, N.H.; Sunna, A.; Qian, Y.; Zvyagin, A.V. Facile Assembly of Functional Upconversion Nanoparticles for Targeted Cancer Imaging and Photodynamic Therapy. ACS Appl. Mater. Interfaces 2016, 8, 11945–11953. [Google Scholar] [CrossRef]
- Ai, F.; Sun, T.; Xu, Z.; Wang, Z.; Kong, W.; To, M.W.; Wang, F.; Zhu, G. An upconversion nanoplatform for simultaneous photodynamic therapy and Pt chemotherapy to combat cisplatin resistance. Dalton Trans. 2016, 45, 13052–13060. [Google Scholar] [CrossRef] [PubMed]
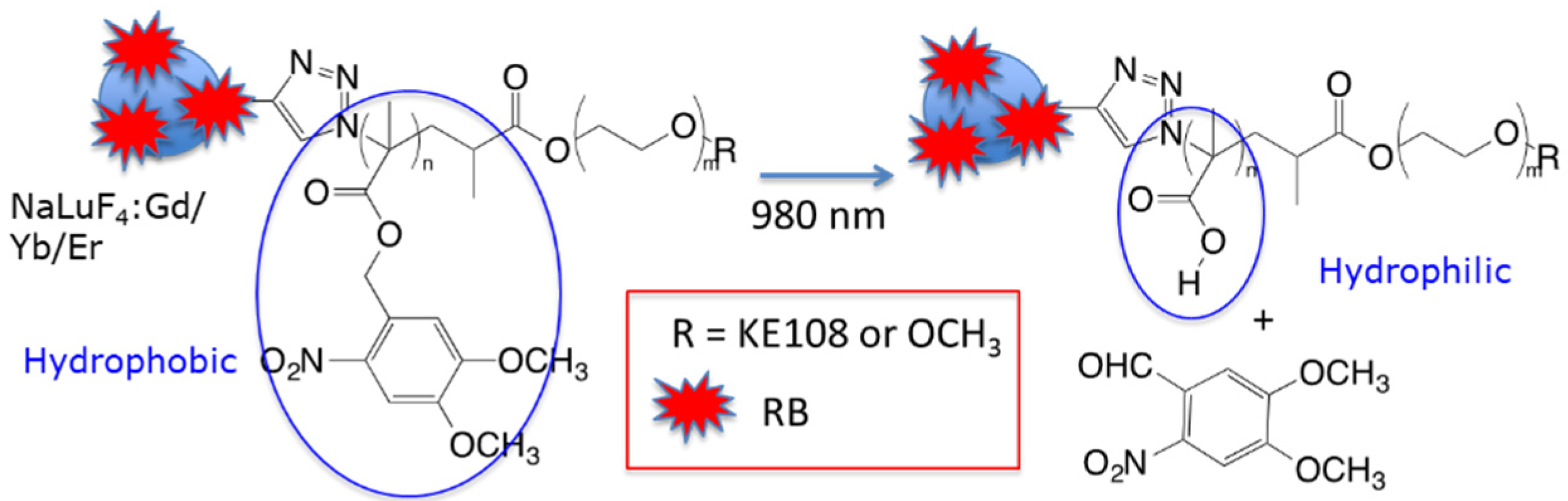
- Chen, G.; Jaskula-Sztul, R.; Esquibel, C.R.; Lou, I.; Zheng, Q.; Dammalapati, A.; Harrison, A.; Eliceiri, K.; Tang, W.; Chen, H.; et al. Neuroendocrine Tumor-Targeted Upconversion Nanoparticle-Based Micelles for Simultaneous NIR-Controlled Combination Chemotherapy and Photodynamic Therapy, and Fluorescence Imaging. Adv. Funct. Mater. 2017, 27, 1604671. [Google Scholar] [CrossRef]
- Chang, Y.; Li, X.; Zhang, L.; Xia, L.; Liu, X.; Li, C.; Zhang, Y.; Tu, L.; Xue, B.; Zhao, H.; et al. Precise Photodynamic Therapy of Cancer via Subcellular Dynamic Tracing of Dual-loaded Upconversion Nanophotosensitizers. Sci. Rep. 2017, 7, 45633. [Google Scholar] [CrossRef]
- Hou, B.; Yang, W.; Dong, C.; Zheng, B.; Zhang, Y.; Wu, J.; Wang, H.; Chang, J. Controlled co-release of doxorubicin and reactive oxygen species for synergistic therapy by NIR remote-triggered nanoimpellers. Mater. Sci. Eng. C 2017, 74, 94–102. [Google Scholar] [CrossRef]
- Kumar, B.; Rathnam, V.S.S.; Kundu, S.; Saxena, N.; Banerjee, I.; Giri, S. White-light-emitting NaYF4 Nanoplatform for NIR Upconversion-mediated Photodynamic Therapy and Bioimaging. ChemNanoMat 2018, 4, 583–595. [Google Scholar] [CrossRef]
- Sabri, T.; Pawelek, P.D.; Capobianco, J.A. Dual Activity of Rose Bengal Functionalized to Albumin-Coated Lanthanide-Doped Upconverting Nanoparticles: Targeting and Photodynamic Therapy. ACS Appl. Mater. Interfaces 2018, 10, 26947–26953. [Google Scholar] [CrossRef] [PubMed]
- Buchner, M.; García Calavia, P.; Muhr, V.; Kröninger, A.; Baeumner, A.J.; Hirsch, T.; Russell, D.A.; Marín, M.J. Photosensitiser functionalised luminescent upconverting nanoparticles for efficient photodynamic therapy of breast cancer cells. Photochem. Photobiol. Sci. 2019, 18, 98–109. [Google Scholar] [CrossRef] [PubMed]
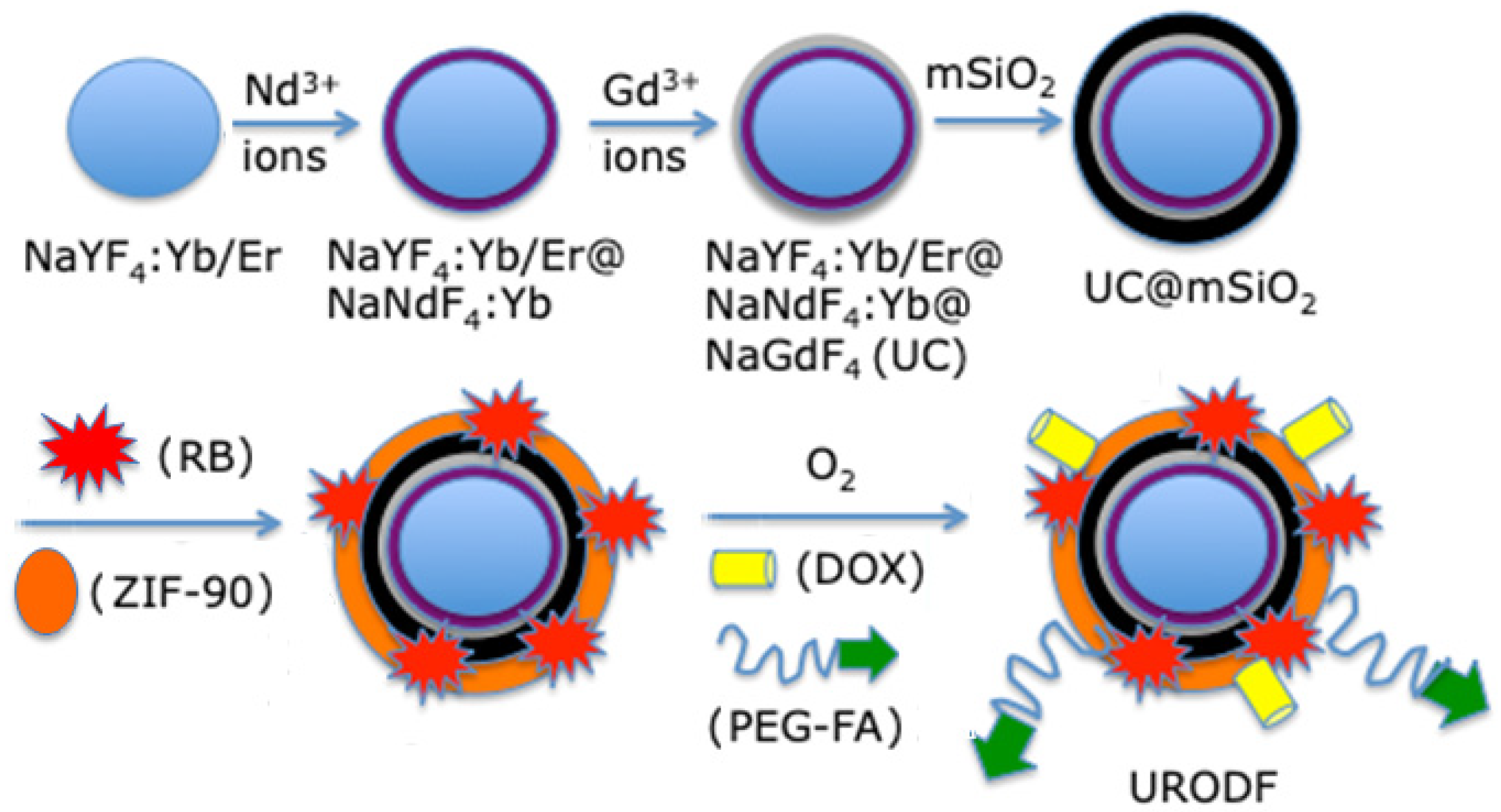
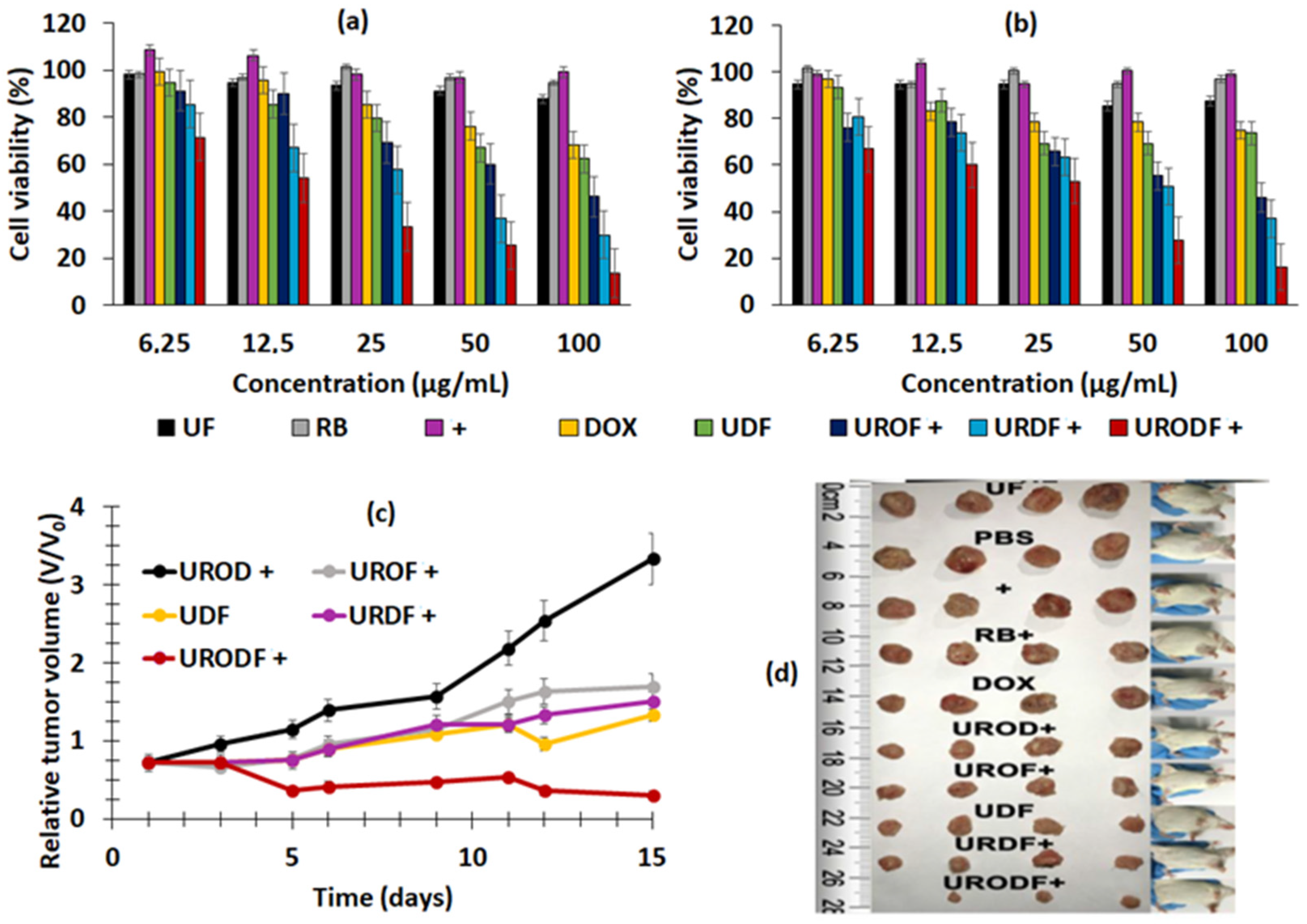
- Xie, Z.; Cai, X.; Sun, C.; Liang, S.; Shao, S.; Huang, S.; Cheng, Z.; Pang, M.; Xing, B.; Al Kheraif, A.Z.; et al. O2-Loaded pH-Responsive Multifunctional Nanodrug Carrier for Overcoming Hypoxia and Highly Efficient Chemo-Photodynamic Cancer Therapy. Chem. Mater. 2019, 31, 483–490. [Google Scholar] [CrossRef]
- Kumar, B.; Murali, A.; Bharath, A.B.; Giri, S. Guar gum modified upconversion nanocomposites for colorectal cancer treatment through enzyme-responsive drug release and NIR-triggered photodynamic therapy. Nanotechnology 2019, 30, 315102. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Ji, Z.; He, S. SHG-enhanced NIR-excited in vitro photodynamic therapy using composite nanoparticles of barium titanate and rose Bengal. RSC Adv. 2019, 9, 8056–8064. [Google Scholar] [CrossRef]
- Song, D.; Chi, S.; Li, X.; Wang, C.; Li, Z.; Liu, Z. Upconversion System with Quantum Dots as Sensitizer: Improved Photoluminescence and PDT Efficiency. ACS Appl. Mater. Interfaces 2019, 11, 41100–41108. [Google Scholar] [CrossRef]
- Wawrzyńczyk, D.; Cichy, B.; Zaręba, J.K.; Bazylińska, U. On the interaction between up-converting NaYF4:Er3+,Yb3+ nanoparticles and Rose Bengal molecules constrained within the double core of multifunctional nanocarriers. J. Mater. Chem. C 2019, 7, 15021–15034. [Google Scholar] [CrossRef]
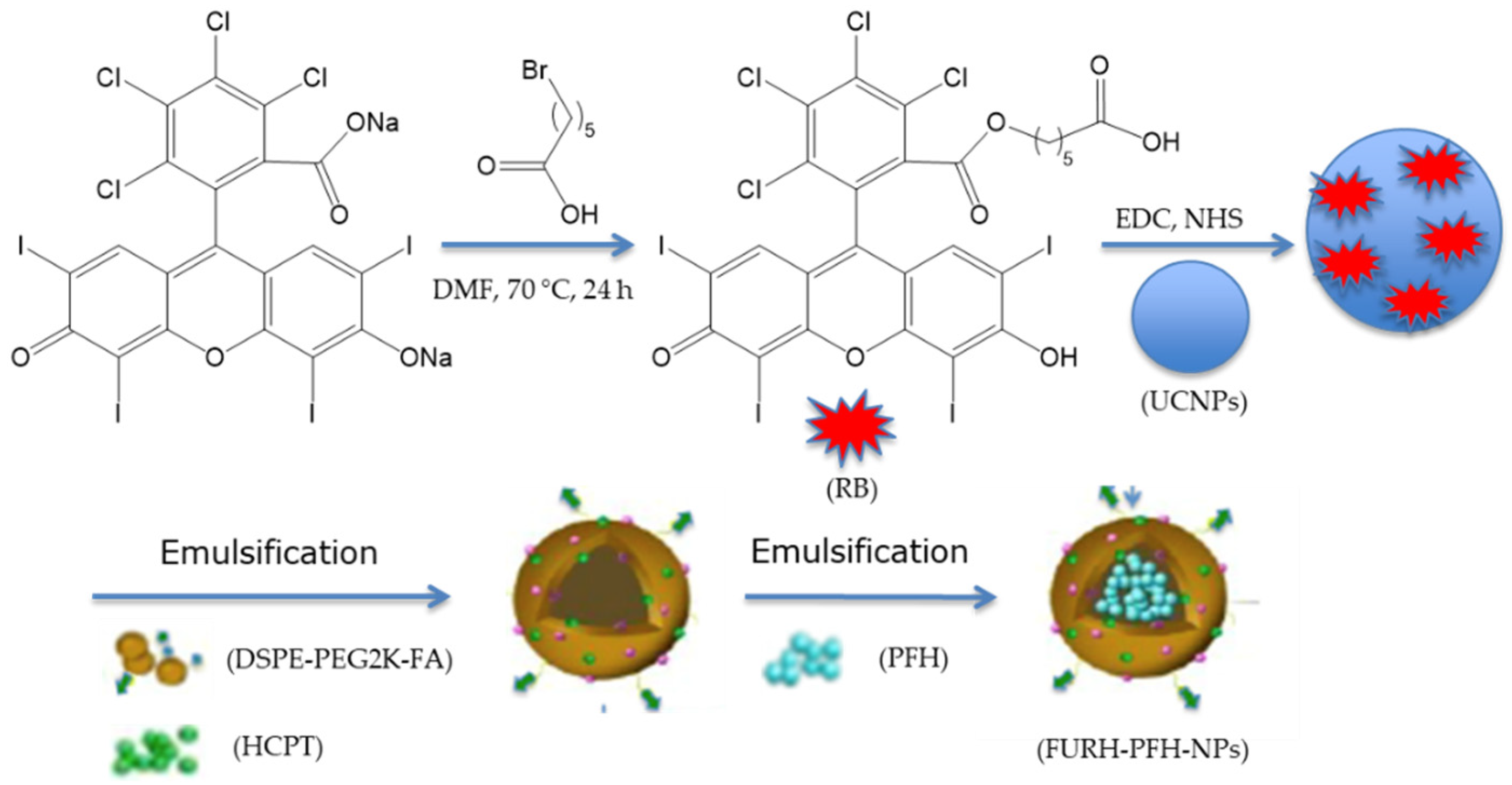
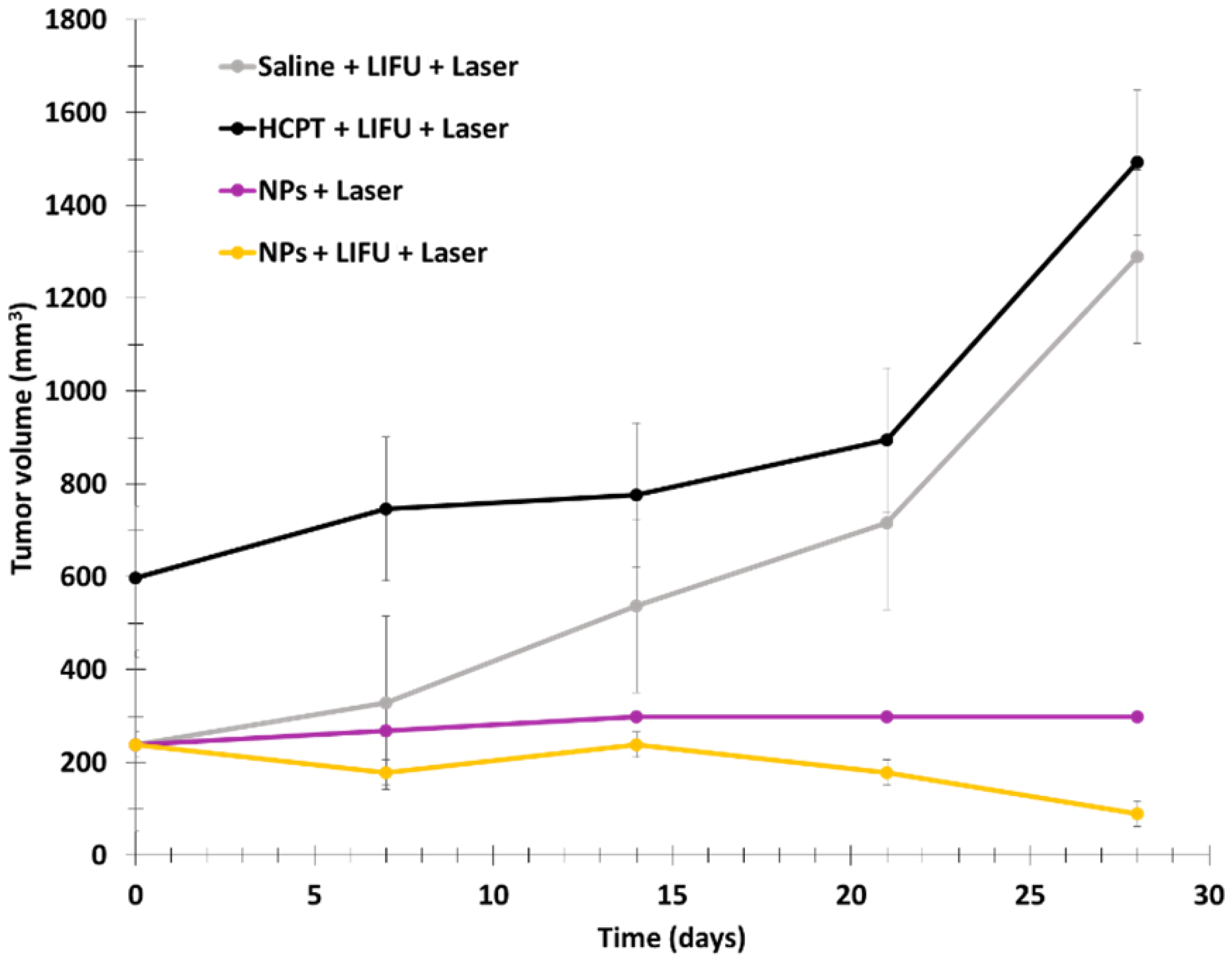
- Wang, H.-Y.; Hou, L.; Li, H.-L.; Wang, X.; Cao, Y.; Zhang, B.-Y.; Wang, J.-T.; Wei, S.-J.; Dang, H.-W.; Ran, H.-T. A nanosystem loaded with perfluorohexane and rose bengal coupled upconversion nanoparticles for multimodal imaging and synergetic chemo-photodynamic therapy of cancer. Biomater. Sci. 2020, 8, 2488–2506. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, X.; Zhang, Y.; He, Y.; Liu, Y.; Ju, H. Activatable photodynamic therapy with therapeutic effect prediction based on a self-correction upconversion nanoprobe. ACS Appl. Mater. Interfaces 2020, 12, 19313–19323. [Google Scholar] [CrossRef]
- Han, R.; Tang, K.; Hou, Y.; Yu, J.; Wang, C.; Wang, Y. Fabrication of core/shell/shell structure nanoparticle with anticancer drug and dual-photosensitizer co-loading for synergistic chemotherapy and photodynamic therapy. Microporous Mesoporous Mater. 2020, 297, 110049. [Google Scholar] [CrossRef]
- Jin, F.-Y.; Qi, J.; Zhu, M.; Liu, D.; You, Y.; Shu, G.; Du, Y.; Wang, J.; Yu, H.; Sun, M.; et al. NIR-Triggered Sequentially Responsive Nanocarriers Amplified Cascade Synergistic Effect of Chemo-Photodynamic Therapy with Inspired Antitumor Immunity. ACS Appl. Mater. Interfaces 2020, 12, 32372–32387. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Qiao, X.; He, G.; Sun, X.; Feng, D.; Hu, L.; Xu, H.; Xu, H.-B.; Ma, S.; Tian, J. Core-satellite metal-organic framework@upconversion nanoparticle superstructures via electrostatic self-assembly for efficient photodynamic theranostics. Nano Res. 2020, 13, 3377–3386. [Google Scholar] [CrossRef]
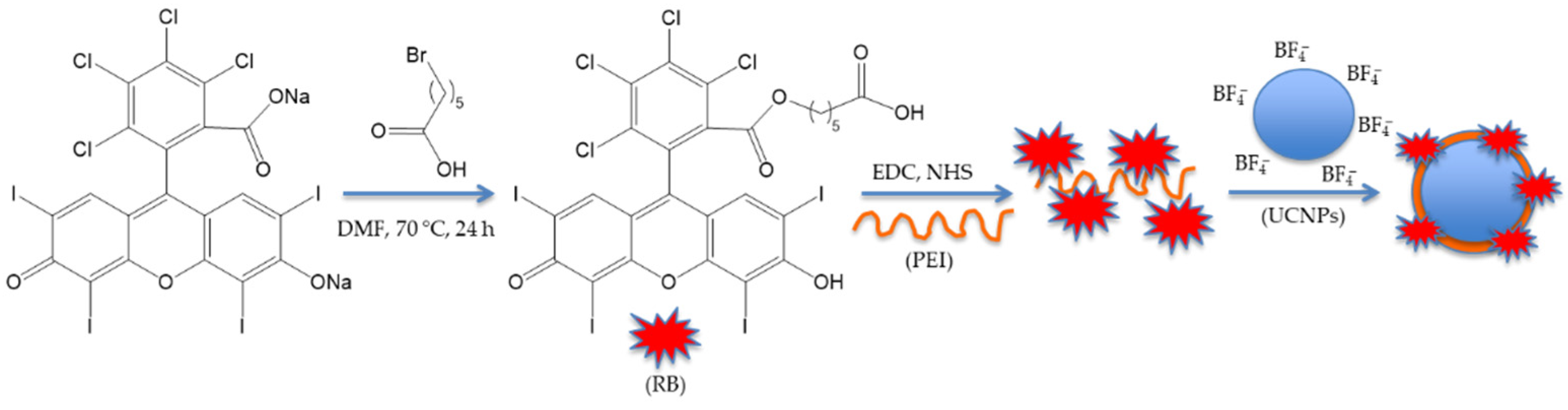
- Borodziuk, A.; Kowalik, P.; Duda, M.; Wojciechowski, T.; Minikayev, R.; Kalinowska, D.; Klepka, M.; Sobczak, K.; Kłopotowski, Ł.; Sikora, B. Unmodified Rose Bengal photosensitizer conjugated with NaYF4:Yb,Er upconverting nanoparticles for efficient photodynamic therapy. Nanotechnology 2020, 31, 465101. [Google Scholar] [CrossRef] [PubMed]
- Tezuka, K.; Umezawa, M.; Liu, T.-I.; Nomura, K.; Okubo, K.; Chiu, H.-C.; Kamimura, M.; Soga, K. Upconversion Luminescent Nanostructure with Ultrasmall Ceramic Nanoparticles Coupled with Rose Bengal for NIR-Induced Photodynamic Therapy. ACS Appl. Bio Mater. 2021, 4, 4462–4469. [Google Scholar] [CrossRef]
- Quignard, S. Silica Nanoparticles Behaviour in Biological Medium: From Cells to Biomaterials Comportement des Nanoparticules de Silice en Milieu Biologique: Des Cellules aux Biomatériaux; Université Pierre et Marie Curie: Paris, France, 2012. [Google Scholar]
- Natarajan, S.K.; Selvaraj, S. Mesoporous silica nanoparticles: Importance of surface modifications and its role in drug delivery. RSC Adv. 2014, 4, 14328–14334. [Google Scholar] [CrossRef]
- Soares-Santos, P.C.; Nogueira, H.I.; Félix, V.; Drew, M.G.; Sá Ferreira, R.A.; Carlos, L.D.; Trindade, T. Novel lanthanide luminescent materials based on complexes of 3-hydroxypicolinic acid and silica nanoparticles. Chem. Mater. 2003, 15, 100–108. [Google Scholar] [CrossRef]
- Uppal, A.; Jain, B.; Gupta, P.K.; Das, K. Photodynamic Action of Rose Bengal Silica Nanoparticle Complex on Breast and Oral Cancer Cell Lines. Photochem. Photobiol. 2011, 87, 1146–1151. [Google Scholar] [CrossRef] [PubMed]
- Gianotti, E.; MartinsEstevão, B.; Cucinotta, F.; Hioka, N.; Rizzi, M.; Renò, F.; Marchese, L. An Efficient Rose Bengal Based Nanoplatform for Photodynamic Therapy. Chem. A Eur. J. 2014, 20, 10921–10925. [Google Scholar] [CrossRef] [PubMed]
- Martins Estevão, B.; Cucinotta, F.; Hioka, N.; Cossi, M.; Argeri, M.; Paul, G. Rose Bengal incorporated in mesostructured silica nanoparticles: Structural characterization, theoretical modeling and singlet oxygen delivery. Phys. Chem. Chem. Phys. 2015, 17, 26804–26812. [Google Scholar] [CrossRef]
- Yildirim, A.; Turkaydin, M.; Garipcan, B.; Bayindir, M. Cytotoxicity of multifunctional surfactant containing capped mesoporous silica nanoparticles. RSC Adv. 2016, 6, 32060–32069. [Google Scholar] [CrossRef]
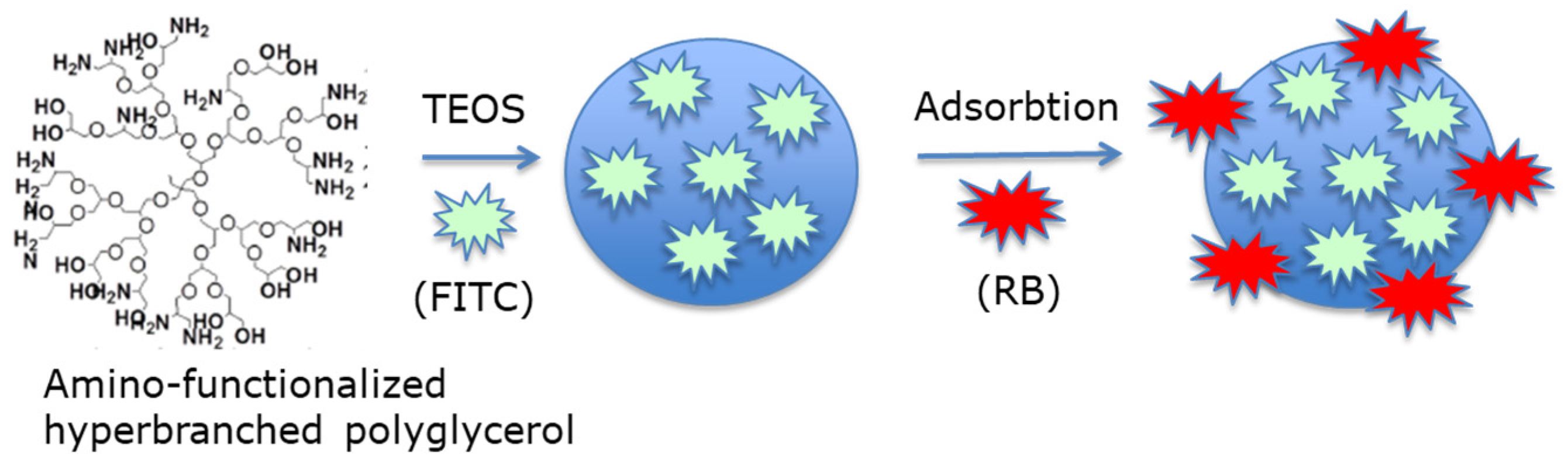
- Liu, H.; Yang, Y.; Wang, A.; Han, M.; Cui, W.; Li, J. Hyperbranched Polyglycerol-Doped Mesoporous Silica Nanoparticles for One- and Two-Photon Activated Photodynamic Therapy. Adv. Funct. Mater. 2016, 26, 2561–2570. [Google Scholar] [CrossRef]
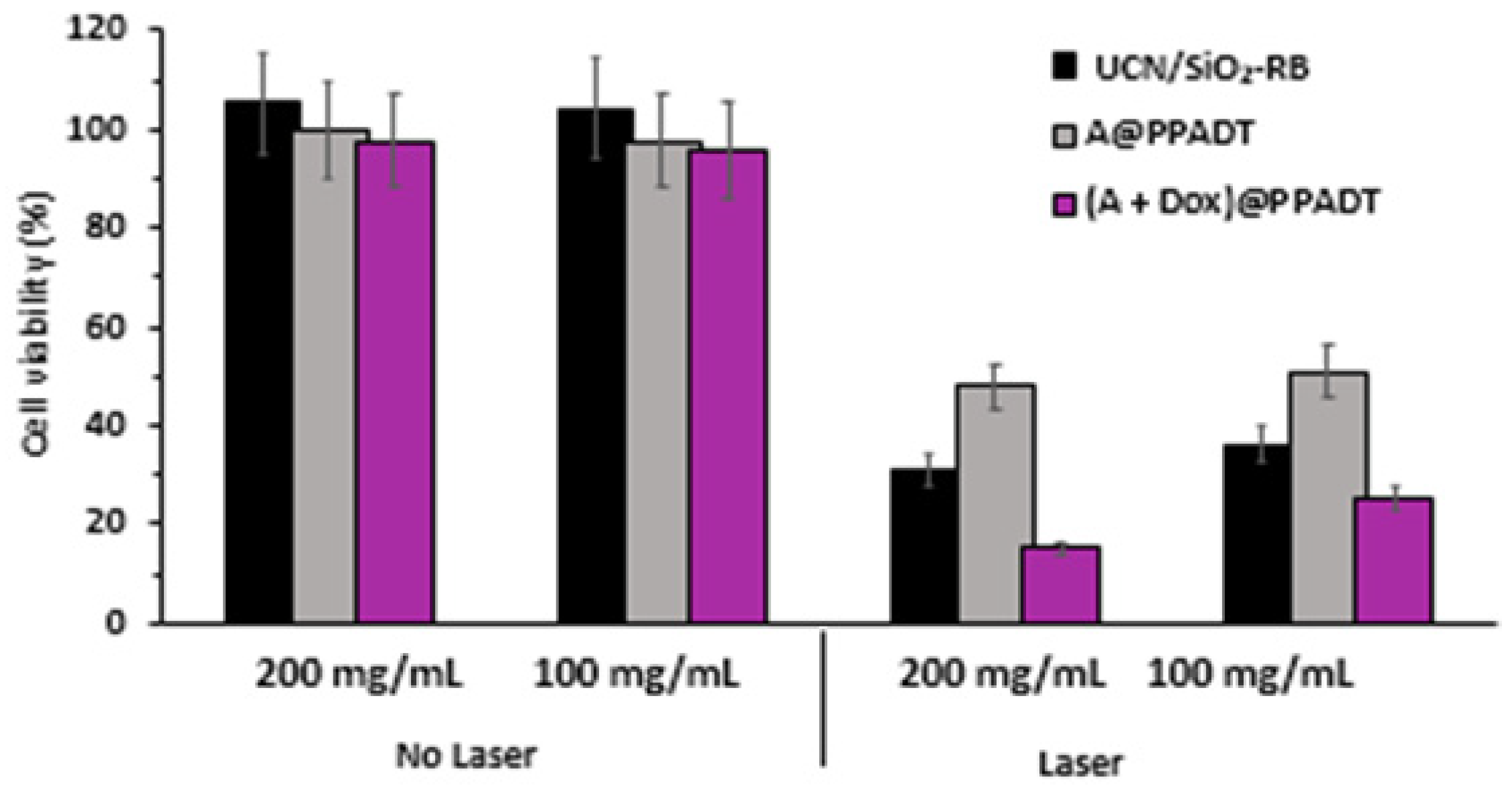
- Zhou, F.; Zheng, B.; Zhang, Y.; Wu, Y.; Wang, H.; Chang, J. Construction of near-infrared light-triggered reactive oxygen species-sensitive (UCN/SiO2-RB + DOX)@PPADT nanoparticles for simultaneous chemotherapy and photodynamic therapy. Nanotechnology 2016, 27, 235601. [Google Scholar] [CrossRef]
- Oliveira, R.C.D.S.; Corrêa, R.J.; Teixeira, R.S.P.; Queiroz, D.D.; Souza, R.D.S.; Garden, S.J.; de Lucas, N.C.; Pereira, M.D.; Forero, J.S.B.; Romani, E.C.; et al. Silica nanoparticles doped with anthraquinone for lung cancer phototherapy. J. Photochem. Photobiol. B Biol. 2016, 165, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Zhan, J.; Ma, Z.; Wang, D.; Li, X.; Li, X.; Le, L.; Kang, A.; Hu, P.; She, L.; Yang, F. Magnetic and pH dual-responsive mesoporous silica nanocomposites for effective and low-toxic photodynamic therapy. Int. J. Nanomed. 2017, 12, 2733–2748. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Liu, X.; Xiao, Y.; Chen, F.; Xiao, F. A multifunctional nanoplatform based on mesoporous silica nanoparticles for imaging-guided chemo/photodynamic synergetic therapy. RSC Adv. 2017, 7, 31133–31141. [Google Scholar] [CrossRef]
- Yan, T.; Cheng, J.; Liu, Z.; Cheng, F.; Wei, X.; He, J. pH-Sensitive mesoporous silica nanoparticles for chemo-photodynamic combination therapy. Colloids Surf. B Biointerfaces 2018, 161, 442–448. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Koyani, R.D.; Muñoz, C.; Sengar, P.; Contreras, O.E.; Juárez, P.; Hirata, G.A. Blue light triggered generation of reactive oxygen species from silica coated Gd3Al5O12:Ce3+ nanoparticles loaded with rose Bengal. Data Brief 2018, 20, 1023–1028. [Google Scholar] [CrossRef]
- Jain, A.; Koyani, R.D.; Muñoz, C.; Sengar, P.; Contreras, O.E.; Juárez, P.; Hirata, G.A. Magnetic-luminescent cerium-doped gadolinium aluminum garnet nanoparticles for simultaneous imaging and photodynamic therapy of cancer cells. J. Colloid Interface Sci. 2018, 526, 220–229. [Google Scholar] [CrossRef]
- Hu, G.; Yang, L.; Li, Y.; Wang, L. Continuous and scalable fabrication of stable and biocompatible MOF@SiO2 nanoparticles for drug loading. J. Mater. Chem. B 2018, 6, 7936–7942. [Google Scholar] [CrossRef]
- Chen, K.; Chang, C.; Liu, Z.; Zhou, Y.; Xu, Q.; Li, C.; Huang, C.; Xu, H.; Xu, P.; Lu, B. Hyaluronic acid targeted and pH-responsive nanocarriers based on hollow mesoporous silica nanoparticles for chemo-photodynamic combination therapy. Colloids Surf. B Biointerfaces 2020, 194, 111166. [Google Scholar] [CrossRef]
- Miletto, I.; Gionco, C.; Paganini, M.C.; Martinotti, S.; Ranzato, E.; Giamello, E.; Marchese, L.; Gianotti, E. Vis-NIR luminescent lanthanide-doped core-shell nanoparticles for imaging and photodynamic therapy. J. Photochem. Photobiol. A Chem. 2020, 403, 112840. [Google Scholar] [CrossRef]
- Prieto-Montero, R.; Prieto-Castañeda, A.; Katsumiti, A.; Cajaraville, M.; Agarrabeitia, A.; Ortiz, M.; Martínez-Martínez, V. Functionalization of Photosensitized Silica Nanoparticles for Advanced Photodynamic Therapy of Cancer. Int. J. Mol. Sci. 2021, 22, 6618. [Google Scholar] [CrossRef]
- Berthet, M. Nanoparticules Biodégradables et Multifonctionnelles pour la Régénération Tissulaire de Plaies Cutanées Profondes. Ph.D. Thesis, University of Claude Bernard Lyon 1, Villeurbanne, France, 2017. [Google Scholar]
- Castro, F.; Pinto, M.L.; Pereira, C.L.; Serre, K.; Barbosa, M.A.; Vermaelen, K.; Gärtner, F.; Gonçalves, R.M.; De Wever, O.; Oliveira, M.J. Chitosan/γ-PGA nanoparticles-based immunotherapy as adjuvant to radiotherapy in breast cancer. Biomaterials 2020, 257, 120218. [Google Scholar] [CrossRef] [PubMed]
- Bala, I.; Hariharan, S.; Kumar, M.N.V.R. PLGA Nanoparticles in Drug Delivery: The State of the Art. Crit. Rev. Ther. Drug Carr. Syst. 2004, 21, 387–422. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Preuß, A.; Hackbarth, S.; Wacker, M.; Langer, K.; Röder, B. Novel photosensitizer-protein nanoparticles for photodynamic therapy: Photophysical characterization and in vitro investigations. J. Photochem. Photobiol. B Biol. 2009, 96, 66–74. [Google Scholar] [CrossRef]
- Karthikeyan, K.; Babu, A.; Kim, S.-J.; Murugesan, R.; Jeyasubramanian, K. Enhanced photodynamic efficacy and efficient delivery of Rose Bengal using nanostructured poly(amidoamine) dendrimers: Potential application in photodynamic therapy of cancer. Cancer Nanotechnol. 2011, 2, 95–103. [Google Scholar] [CrossRef]
- Baumann, P.; Balasubramanian, V.; Onaca-Fischer, O.; Sienkiewicz, A.; Palivan, C.G. Light-responsive polymer nanoreactors: A source of reactive oxygen species on demand. Nanoscale 2012, 5, 217–224. [Google Scholar] [CrossRef]
- Bhattacharyya, S.; Barman, M.K.; Baidya, A.; Patra, A. Singlet Oxygen Generation from Polymer Nanoparticles–Photosensitizer Conjugates Using FRET Cascade. J. Phys. Chem. C 2014, 118, 9733–9740. [Google Scholar] [CrossRef]
- Han, S.; Hwang, B.W.; Jeon, E.Y.; Jung, D.; Lee, G.H.; Keum, D.H.; Kim, K.S.; Yun, S.H.; Cha, H.J.; Hahn, S.K. Upconversion Nanoparticles/Hyaluronate–Rose Bengal Conjugate Complex for Noninvasive Photochemical Tissue Bonding. ACS Nano 2017, 11, 9979–9988. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Hou, W.; Liu, S.; Sun, K.; Li, M.; Wu, C. Biodegradable Polymer Nanoparticles for Photodynamic Therapy by Bioluminescence Resonance Energy Transfer. Biomacromolecules 2017, 19, 201–208. [Google Scholar] [CrossRef]
- Chang, Y.-C.; Del Valle, A.C.; Yeh, H.-P.; He, Y.; Huang, Y.-F. Development of Photo-Activated ROS-Responsive Nanoplatform as a Dual-Functional Drug Carrier in Combinational Chemo-Photodynamic Therapy. Front. Chem. 2019, 6, 647. [Google Scholar] [CrossRef]
- Bazylińska, U.; Wawrzyńczyk, D.; Szewczyk, A.; Kulbacka, J. Engineering and biological assessment of double core nanoplatform for co-delivery of hybrid fluorophores to human melanoma. J. Inorg. Biochem. 2020, 208, 111088. [Google Scholar] [CrossRef]
- Sun, B.; Wang, L.; Li, Q.; He, P.; Liu, H.; Wang, H.; Yang, Y.; Li, J. Bis(pyrene)-Doped Cationic Dipeptide Nanoparticles for Two-Photon-Activated Photodynamic Therapy. Biomacromolecules 2017, 18, 3506–3513. [Google Scholar] [CrossRef]
- Liu, Z.; Li, J.; Jiang, Y.; Wang, D. Multifunctional nanocapsules on a seesaw balancing sonodynamic and photodynamic therapies against superficial malignant tumors by effective immune-enhancement. Biomaterials 2019, 218, 119251. [Google Scholar] [CrossRef] [PubMed]
- Korpusik, A.B.; Tan, Y.; Garrison, J.B.; Tan, W.; Sumerlin, B.S. Aptamer-Conjugated Micelles for Targeted Photodynamic Therapy Via Photoinitiated Polymerization-Induced Self-Assembly. Macromolecules 2021, 54, 7354–7363. [Google Scholar] [CrossRef]
- Calavia, P.G.; Bruce, G.; Pérez-García, L.; Russell, D.A. Photosensitiser-gold nanoparticle conjugates for photodynamic therapy of cancer. Photochem. Photobiol. Sci. 2018, 17, 1534–1552. [Google Scholar] [CrossRef] [PubMed]
- Dykman, L.A.; Khlebtsov, N.G. Gold nanoparticles in biology and medicine: Recent advances and prospects. Acta Nat. 2011, 3, 34–55. [Google Scholar] [CrossRef]
- Kalus, M.-R.; Rehbock, C.; Bärsch, N.; Barcikowski, S. Colloids created by light: Laser-generated nanoparticles for applications in biology and medicine. Mater. Today Proc. 2017, 4, S93–S100. [Google Scholar] [CrossRef]
- Sahoo, G.P.; Bar, H.; Bhui, D.K.; Sarkar, P.; Samanta, S.; Pyne, S.; Ash, S.; Misra, A. Synthesis and photo physical properties of star shaped gold nanoparticles. Colloids Surf. A Physicochem. Eng. Asp. 2011, 375, 30–34. [Google Scholar] [CrossRef]
- Wang, B.; Wang, J.-H.; Liu, Q.; Huang, H.; Chen, M.; Li, K.; Li, C.; Yu, X.-F.; Chu, P.K. Rose-bengal-conjugated gold nanorods for in vivo photodynamic and photothermal oral cancer therapies. Biomaterials 2013, 35, 1954–1966. [Google Scholar] [CrossRef]
- Prasanna, S.W.; Poorani, G.; Kumar, M.S.; Aruna, P.; Ganesan, S. Photodynamic efficacy of Rosebengal-gold nanoparticle complex on Vero and HeLa cell lines. Mater. Express 2014, 4, 359–366. [Google Scholar] [CrossRef]
- Kautzka, Z.; Clement, S.; Goldys, E.M.; Deng, W. Light-triggered liposomal cargo delivery platform incorporating photosensitizers and gold nanoparticles for enhanced singlet oxygen generation and increased cytotoxicity. Int. J. Nanomed. 2017, 12, 969–977. [Google Scholar] [CrossRef] [PubMed]
- Fu, Y.; Liu, H.; Ren, Z.; Li, X.; Huang, J.; Best, S.; Han, G. Luminescent CaTiO3:Yb,Er nanofibers co-conjugated with Rose Bengal and gold nanorods for potential synergistic photodynamic/photothermal therapy. J. Mater. Chem. B 2017, 5, 5128–5136. [Google Scholar] [CrossRef] [PubMed]
- Rosenthal, S.J.; Chang, J.C.; Kovtun, O.; McBride, J.; Tomlinson, I.D. Biocompatible Quantum Dots for Biological Applications. Chem. Biol. 2011, 18, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Wu, I.-C.; Liu, Z.; Tang, Y.; Chen, H.; Yu, J.; Wu, C.; Chiu, D.T. Semiconducting polymer dots with bright narrow-band emission at 800 nm for biological applications. Chem. Sci. 2017, 8, 3390–3398. [Google Scholar] [CrossRef]
- Haimov, E.; Weitman, H.; Ickowicz, D.; Malik, Z.; Ehrenberg, B. Pdots nanoparticles load photosensitizers and enhance efficiently their photodynamic effect by FRET. RSC Adv. 2015, 5, 18482–18491. [Google Scholar] [CrossRef]
- Hua, X.-W.; Bao, Y.-W.; Chen, Z.; Wu, F.-G. Carbon quantum dots with intrinsic mitochondrial targeting ability for mitochondria-based theranostics. Nanoscale 2017, 9, 10948–10960. [Google Scholar] [CrossRef] [PubMed]
- Subramani, K.; Mehta, M. Nanodiagnostics in microbiology and dentistry. In Emerging Nanotechnologies in Dentistry; Elsevier: Amsterdam, The Netherlands, 2018; pp. 391–419. [Google Scholar] [CrossRef]
- Zhang, H.; Peng, S.; Xu, S.; Chen, Z. Bifunctional nanocapsules for magnetic resonance imaging and photodynamic therapy. RSC Adv. 2016, 6, 104731–104734. [Google Scholar] [CrossRef]
- Cao, H.; Wang, L.; Yang, Y.; Li, J.; Qi, Y.; Li, Y.; Li, Y.; Wang, H.; Li, J. An Assembled Nanocomplex for Improving both Therapeutic Efficiency and Treatment Depth in Photodynamic Therapy. Angew. Chem. 2018, 130, 7885–7889. [Google Scholar] [CrossRef]
- Cao, H.; Qi, Y.; Yang, Y.; Wang, L.; Sun, J.; Li, Y.; Xia, J.; Wang, H.; Li, A.P.D.J. Assembled Nanocomplex for Improving Photodynamic Therapy through Intraparticle Fluorescence Resonance Energy Transfer. Chem. Asian J. 2018, 13, 3540–3546. [Google Scholar] [CrossRef]
- Gravel, O. The Emergence of Liquid Mixing from Spinning Magnetic Nanoparticules in Rotating Magnetic Fields: Visualisation and Characterisation towards a Better Understanding of the Underlying phenomena. Master’s Thesis, University of Laval, Quebec City, QC, Canada, 2014. [Google Scholar]
- Colombo, M.; Carregal-Romero, S.; Casula, M.F.; Gutiérrez, L.; Morales, M.P.; Böhm, I.B.; Heverhagen, J.T.; Prosperi, D.; Parak, W.J. Biological applications of magnetic nanoparticles. Chem. Soc. Rev. 2012, 41, 4306–4334. [Google Scholar] [CrossRef] [PubMed]
- Yeh, H.-P.; Del Valle, A.C.; Syu, M.-C.; Qian, Y.; Chang, Y.-C.; Huang, Y.-F. A New Photosensitized Oxidation-Responsive Nanoplatform for Controlled Drug Release and Photodynamic Cancer Therapy. ACS Appl. Mater. Interfaces 2018, 10, 21160–21172. [Google Scholar] [CrossRef] [PubMed]
- Peng, C.-L.; Yang, L.-Y.; Luo, T.-Y.; Lai, P.-S.; Yang, S.-J.; Lin, W.-J.; Shieh, M.-J. Development of pH sensitive 2-(diisopropylamino)ethyl methacrylate based nanoparticles for photodynamic therapy. Nanotechnology 2010, 21, 155103. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Wang, J.; Cui, R.; Xu, D.; Zhu, L.; Li, Z.; Chen, H.; Gao, Y.; Jia, L. Hypoxia/pH dual-responsive nitroimidazole-modified chitosan/rose bengal derivative nanoparticles for enhanced photodynamic anticancer therapy. Dyes Pigments 2020, 179, 108395. [Google Scholar] [CrossRef]
- Francés-Soriano, L.; Zakharko, M.A.; González-Béjar, M.; Panchenko, P.A.; Herranz-Pérez, V.; Pritmov, D.A.; Grin, M.A.; Mironov, A.F.; García-Verdugo, J.M.; Fedorova, O.A.; et al. Nanohybrid for Photodynamic Therapy and Fluorescence Imaging Tracking without Therapy. Chem. Mater. 2018, 30, 3677–3682. [Google Scholar] [CrossRef]
- Su, P.; Zhu, Z.; Fan, Q.; Cao, J.; Wang, Y.; Yang, X.; Cheng, B.; Liu, W.; Tang, Y. Surface ligand coordination induced self-assembly of a nanohybrid for efficient photodynamic therapy and imaging. Inorg. Chem. Front. 2018, 5, 2620–2629. [Google Scholar] [CrossRef]
- Yin, Y.; Hu, B.; Yuan, X.; Cai, L.; Gao, H.; Yang, Q. Nanogel: A Versatile Nano-Delivery System for Biomedical Applications. Pharmaceutics 2020, 12, 290. [Google Scholar] [CrossRef]
- Torres-Martínez, A.; Bedrina, B.; Falomir, E.; Marín, M.J.; Angulo-Pachón, C.A.; Galindo, F.; Miravet, J.F. Non-Polymeric Nanogels as Versatile Nanocarriers: Intracellular Transport of the Photosensitizers Rose Bengal and Hypericin for Photodynamic Therapy. ACS Appl. Bio Mater. 2021, 4, 3658–3669. [Google Scholar] [CrossRef]
- Elmenoufy, A.H.; Tang, Y.; Hu, J.; Xu, H.; Yang, X. A novel deep photodynamic therapy modality combined with CT imaging established via X-ray stimulated silica-modified lanthanide scintillating nanoparticles. Chem. Commun. 2015, 51, 12247–12250. [Google Scholar] [CrossRef] [Green Version]
- Hsu, C.-C.; Lin, S.-L.; Chang, C.A. Lanthanide-Doped Core–Shell–Shell Nanocomposite for Dual Photodynamic Therapy and Luminescence Imaging by a Single X-ray Excitation Source. ACS Appl. Mater. Interfaces 2018, 10, 7859–7870. [Google Scholar] [CrossRef]
- Sun, W.; Shi, T.; Luo, L.; Chen, X.; Lv, P.; Lv, Y.; Zhuang, Y.; Zhu, J.; Liu, G.; Chen, X.; et al. Monodisperse and Uniform Mesoporous Silicate Nanosensitizers Achieve Low-Dose X-ray-Induced Deep-Penetrating Photodynamic Therapy. Adv. Mater. 2019, 31, 1808024. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.; Wang, X.; Jiang, Z.; Yu, X.; Liu, X.; Mao, R.; Chen, X.; Li, W. Codoping Enhanced Radioluminescence of Nanoscintillators for X-ray-Activated Synergistic Cancer Therapy and Prognosis Using Metabolomics. ACS Nano 2019, 13, 10419–10433. [Google Scholar] [CrossRef] [PubMed]
- Bekah, D.; Cooper, D.; Kudinov, K.; Hill, C.; Seuntjens, J.; Bradforth, S.; Nadeau, J. Synthesis and characterization of biologically stable, doped LaF3 nanoparticles co-conjugated to PEG and photosensitizers. J. Photochem. Photobiol. A Chem. 2016, 329, 26–34. [Google Scholar] [CrossRef]
- Maiti, D.; Zhong, J.; Zhang, Z.; Zhou, H.; Xion, S.; Dong, Z.; Kumar, S.; Liu, Z.; Yang, K. Polyoxomolybdate (POM) nanoclusters with radiosensitizing and scintillating properties for low dose X-ray inducible radiation-radiodynamic therapy. Nanoscale Horizons 2019, 5, 109–118. [Google Scholar] [CrossRef]
- Sun, W.; Luo, L.; Feng, Y.; Qiu, Y.; Shi, C.; Meng, S.; Chen, X.; Chen, H. Gadolinium–Rose Bengal Coordination Polymer Nanodots for MR-/Fluorescence-Image-Guided Radiation and Photodynamic Therapy. Adv. Mater. 2020, 32, 2000377. [Google Scholar] [CrossRef]
- Zhang, W.; Zhang, X.; Shen, Y.; Shi, F.; Song, C.; Liu, T.; Gao, P.; Lan, B.; Liu, M.; Wang, S.; et al. Ultra-high FRET efficiency NaGdF4:Tb3+-Rose Bengal biocompatible nanocomposite for X-ray excited photodynamic therapy application. Biomaterials 2018, 184, 31–40. [Google Scholar] [CrossRef]
- Zhang, X.; Lan, B.; Wang, S.; Gao, P.; Liu, T.; Rong, J.; Xiao, F.; Wei, L.; Lu, H.; Pang, C.; et al. Low-Dose X-ray Excited Photodynamic Therapy Based on NaLuF4:Tb3+–Rose Bengal Nanocomposite. Bioconjug. Chem. 2019, 30, 2191–2200. [Google Scholar] [CrossRef] [PubMed]
- Polozhentsev, O.E.; Pankin, I.A.; Khodakova, D.V.; Medvedev, P.V.; Goncharova, A.S.; Maksimov, A.Y.; Kit, O.I.; Soldatov, A.V. Synthesis, Characterization and Biodistribution of GdF3:Tb3+@RB Nanocomposites. Materials 2022, 15, 569. [Google Scholar] [CrossRef]
- Tang, Y.; Hu, J.; Elmenoufy, A.H.; Yang, X. Highly Efficient FRET System Capable of Deep Photodynamic Therapy Established on X-ray Excited Mesoporous LaF3:Tb Scintillating Nanoparticles. ACS Appl. Mater. Interfaces 2015, 7, 12261–12269. [Google Scholar] [CrossRef]
- Darafsheh, A.; Najmr, S.; Paik, T.; Tenuto, M.; Murray, C.; Finlay, J.; Friedberg, J.S. Characterization of rare-earth-doped nanophosphors for photodynamic therapy excited by clinical ionizing radiation beams. In Proceedings of the Optical Methods for Tumor Treatment and Detection: Mechanisms and Techniques in Photodynamic Therapy XXIV, San Francisco, CA, USA, 2 March 2015. [Google Scholar]
- Ponomarenko, S.A.; Surin, N.M.; Borshchev, O.V.; Luponosov, Y.N.; Akimov, D.Y.; Alexandrov, I.S.; Burenkov, A.A.; Kovalenko, A.G.; Stekhanov, V.N.; Kleymyuk, E.A.; et al. Nanostructured organosilicon luminophores and their application in highly efficient plastic scintillators. Sci. Rep. 2014, 4, 6549. [Google Scholar] [CrossRef]
- Ren, Y.; Rosch, J.G.; Landry, M.R.; Winter, H.; Khan, S.; Pratx, G.; Sun, C. Tb-Doped core–shell–shell nanophosphors for enhanced X-ray induced luminescence and sensitization of radiodynamic therapy. Biomater. Sci. 2020, 9, 496–505. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Li, Y.; Du, L.; Deng, Z.; Jiang, M.; Zeng, S. Soft X-ray Stimulated Lanthanide@MOF Nanoprobe for Amplifying Deep Tissue Synergistic Photodynamic and Antitumor Immunotherapy. Adv. Health Mater. 2021, 10, 2101174. [Google Scholar] [CrossRef] [PubMed]

















| PDT UCNPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling NP-RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [20] | UCNPs@RB@FA-(NaYF4:Yb3+, Er3+) | 20 without RB | 980 nm, 1.5 W/cm2, 10 min | DPBF | Covalent | JAR NIH 3T3 | Cytotoxicity (+) | nd | nd |
| [25] | UCNPs-RB | 25 without RB | In vitro: 0.8 W/cm2, 8 min In vivo: 808 nm, 520 mW/cm2 | DPBF | Covalent | 4T1 | Cytotoxicity (+) | 4T1 breast cancer bearing mice | PDT (+) |
| [21] | UCNP@BSA-RB&IR825 | 60 | 980 nm, 0.4 W/cm2 in vitro: 10 min in vivo: 30 min | SOSG | Encapsulation | 4T1 | Cytotoxicity (+) | 4T1 tumor-bearing mice | PDT (+) |
| [43] | Er@Nd-RB Upconversion | 216 | 808 nm laser (in vitro: 1 W/cm2, in vivo: 1.25 W/cm2), 5 min | DCFH-DA | Encapsulation | 4T1 | Cytotoxicity (+) | 4T1 tumor-bearing mice- Healthy BALB/c | PDT (+) |
| [37] | UCNP@BSA-RB&IR825 | 16 | In vitro: 808 nm, 0.75 W/cm2, 5 min In vivo: 808 nm, 0.95 W/cm2, 15 min | ABDA | Encapsulation | HeLa HCT116 | Cytotoxicity (+) | 4T1 tumor-bearing mice | PDT (+) |
| [29] | UCNPs-RB&ZnPc | 24–32 | 980 nm, 0.25 W/cm2, 15 min | DPBF | Encapsulation | A549 | Cytotoxicity (+) | Hepa1-6 tumor-bearing mice | PDT (+) |
| [30] | Nd3+/Yb3 UCNPs with Ag2Se QD | 120 | 980 nm, 2.0 W/cm2, 10 min | ABDA | Covalent | HeLa | Cytotoxicity (+) | nd | nd |
| [28] | NaYF4: 20%Yb3+, 2% Er3+@ NaYF4 | 29 | 980 nm, 0.5 W/cm2, 10 min | DPBF | Covalent | NET | Cytotoxicity (+) | TT-tumor-bearing mice | PDT (+) |
| [27] | UCN@mSiO2-(Azo + RB) | 35.9 | 808 nm, 6 W/cm2, 5 min | DPBF | Covalent | A2780 A2780cisR | Cytotoxicity (+) | nd | nd |
| [26] | PNBMA-PEG@ RB@AB3@KE108 | 29 | 980 nm, 1.5 W/cm2, 30 min | DPBF | Adsorption | HT-29 | Cytotoxicity (+) | Mouse anti-human CD326 (EpCAM) (clone HEA-125) | PDT (+) |
| [22] | RB-UPPLVs | 40 | 980 nm, 2.5 W/cm2, 20 min | ABDA | Encapsulation | HeLa | Cytotoxicity (+) | nd | nd |
| [23] | NaYF4:Yb/Ho@NaYF4:Nd@NaYF4 | 0.4 to 4.2 | 808 nm, 0.67 W/cm2, 10 min | DPBF | Covalent | HeLa | Cytotoxicity (+) | nd | nd |
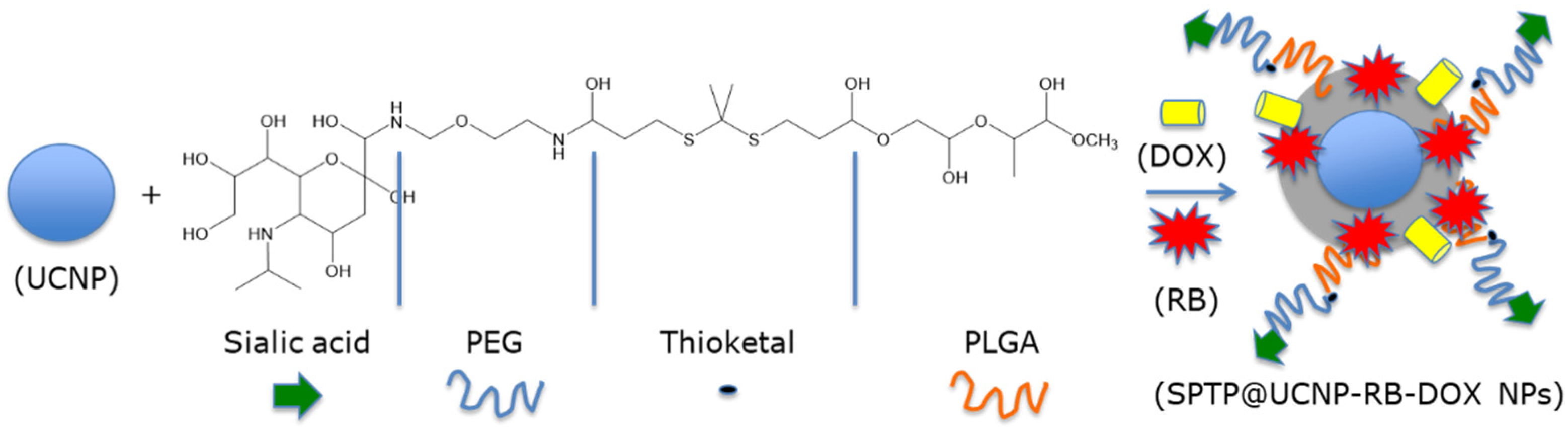
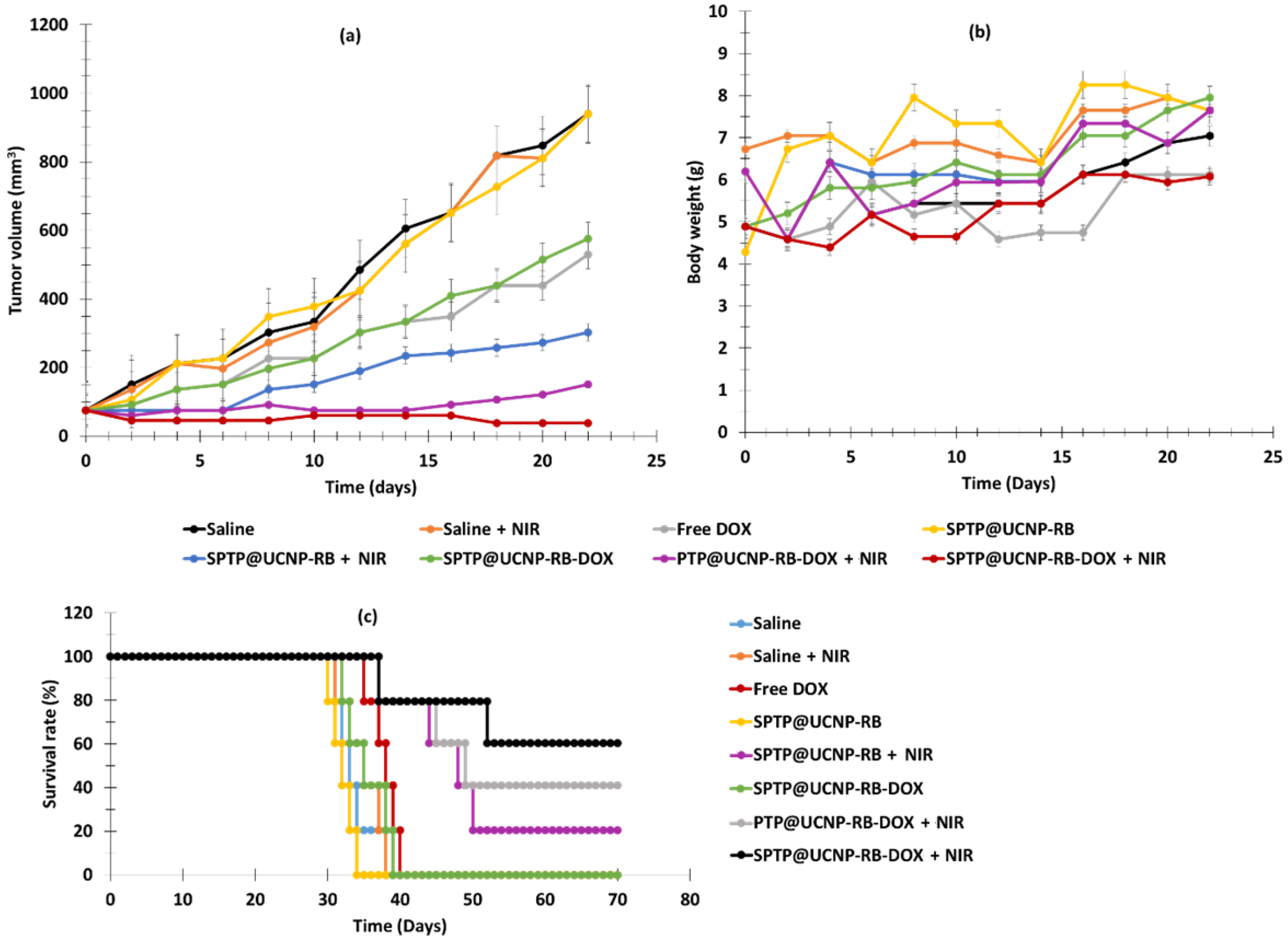
| [42] | SPTP@UCNP-RB-DOX | 54.3 | 980 nm, 0.5 W/cm2, 5–10 min | DPBF | Adsorption | 4T1 | Cytotoxicity (+) | TNBC | PDT (+) |
| [35] | CSGUR-MSGG/5FU@RB@FA | 72.3 | 980 nm, 30 min | DPBF | Covalent | HT-29 | Cytotoxicity (+) | nd | nd |
| [40] | STPT@UCNP-RB-DOX | 56.1 ± 1.0 | 808 nm, 1.5 W/cm2, 40 min | DPBF | Covalent | HeLa MCF-7 NIH 3T3 | Cytotoxicity (+) | BALB/c nude mice with HeLa tumor | PDT (+) |
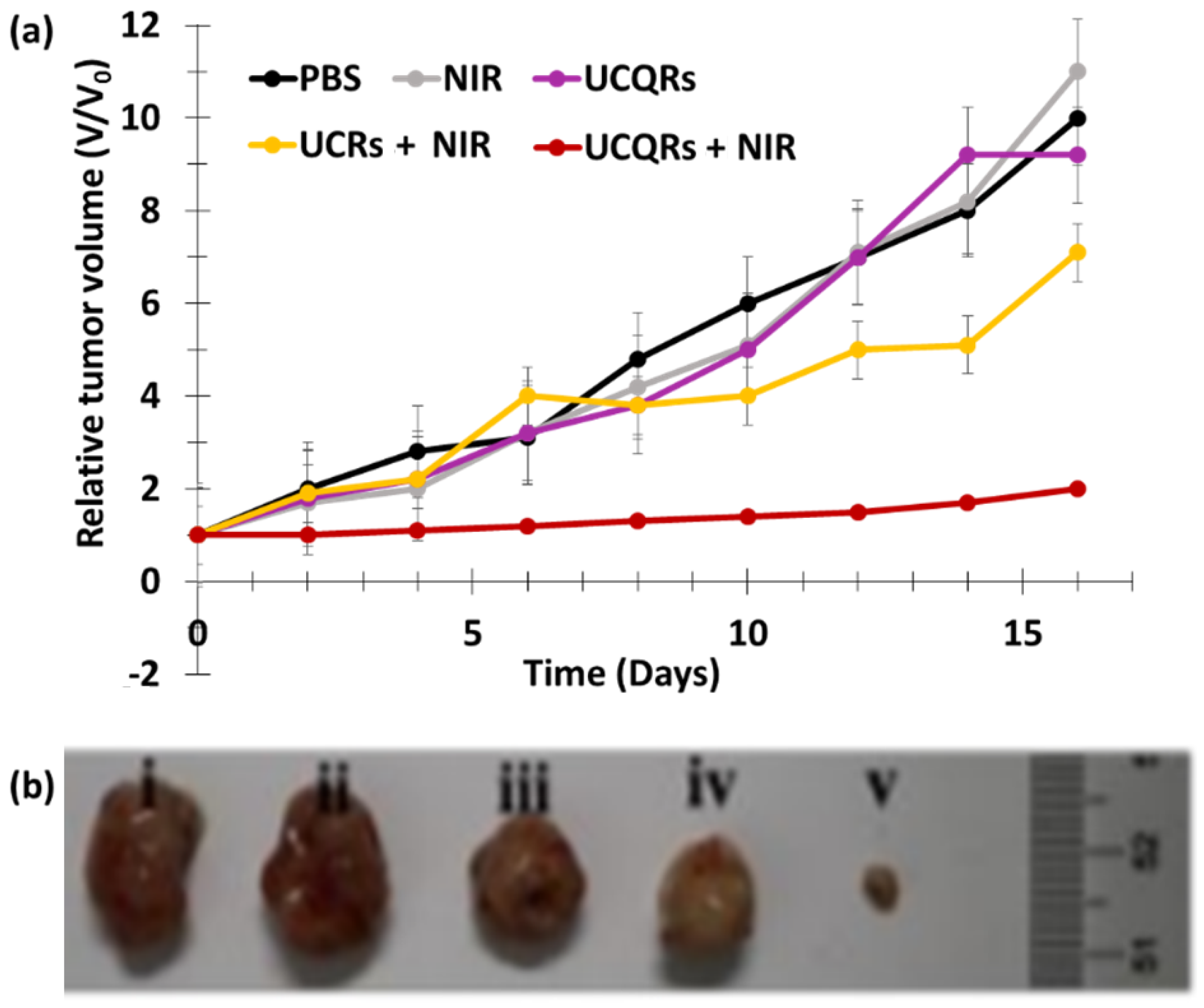
| [39] | FA/UCNPs-RB/HCPT/PFH@Lipid | 223.6 ± 68.8 | 980 nm, 0.2 W/cm2, 2 min | DPBF | Covalent | SKOV-3 | Cytotoxicity (+) | SKOV3 tumor-bearing mice | PDT (+) |
| [41] | NaYF4:Gd@NaYF4:Er,Yb@NaYF4:Nd,Yb NPs @ RB, Cy3 and pep-QSY7 | 130 | 808 nm, 0.5 W/cm2, 10 min | ABDA | Covalent | HeLa | Cytotoxicity (+) | HeLa tumor-bearing mice | PDT (+) |
| [37] | FA/UCNPs-RB/HCPT/PFH@Lipid | 62.57 without RB | 808 nm, 1.6 W/cm2, 10 min | ABDA | Encapsulation | HeLa | Cytotoxicity (+) | Lewis lung carcinoma (LLC) tumor-bearing mice | PDT (+) |
| [36] | BT@PAH/RB/PAH, BT–RB | 70 | 532 nm, 30 mW/cm2, 3 min | DPBF | Loading | HeLa | Cytotoxicity (+) | nd | nd |
| [34] | Nd3+/Yb3 UCNPs) with Ag2Se QDs, RB | 150 | 808 nm, 0.5 W/cm2, 10 min | DPBF | Encapsulation | HeLa | Cytotoxicity (+) | tumor-bearing BALB/c mice | PDT (+) |
| [33] | Barium titanate NPs | 23.7 without RB | 980 nm, 200 mW/cm2, 6 min | ABDA | Covalent | SK-BR-3 | Cytotoxicity (+) | nd | nd |
| [32] | NaGdF4:Yb3+/Er3+@BSA@RB | 78 | 980 nm, 13 W/cm2, 10 min | DPBF | Covalent | A549 | Cytotoxicity (+) | nd | nd |
| [31] | NaYF4:Yb,Er,Gd@NaYF4@ SiO2-RB | 91 | 980 nm, 2.5 W/cm2, 20 min | DPBF | Adsorption | HeLa | Cytotoxicity (+) | nd | nd |
| [44] | NaGdF4:Yb3+/Er3+ @ RB | 41.1 | 980 nm, 2 W/cm2, 10 min | DPBF | Covalent | 4T1 | Cytotoxicity (+) | nd | nd |
| [45] | PEG-block-Polymer/C18RB/NaYF4:Yb3+/Er3+ | 8.7 | 980 nm, 2W/cm2, 30 min | DPBF | Encapsulate | Colon-26 | Cytotoxicity (+) | nd | nd |
| [32] | NaYF4:2%Er,20%Yb)@SiO2-RB | 78 | 980 nm, 13 W/cm2, 10 min | DPBF | Covalent | A549 | Cytotoxicity (+) | nd | nd |
| [24] | UCNP@OS@RB | 27 | 980 nm, 0.5 W/cm2, 10 min | DPBF | Adsorption | HT1299 | Affinity and Cytotoxicity (+) | nd | nd |
| PDT Silica NPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling between NPs and RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [63] | Ln:ZrO2@SiO2@RB | 20–25 thick | 633 nm, 4 mW He-Ne laser, 10 min | DPBF | Covalent | HeLa | Cytotoxicity (+) | nd | nd |
| [50] | Mesoporous silica NPs@RB | 160–180 | green light, 5 min | nd | Covalent | SK-MEL-28 | Cytotoxicity (+) | nd | nd |
| [59] | Silica coated (Gd3Al5O12:Ce3+)-RB | 74.13 ± 9.04 | 470 nm, 20 mW/cm2, 15–30–45 min | DPBF | Loaded | MDA-MB-231 | Cytotoxicity (+) | nd | nd |
| [58] | MSN@DOX@RB | 200 | 532 nm, 0.5 W/cm2, 5 min | nd | Covalent | MCF-7 | Cytotoxicity (+) | nd | nd |
| [57] | MSN@C-dots/RB | 104 | 540 nm, 300 mW/cm2, 5 min | DPBF | Encapsulation | H1299 | Cytotoxicity (+) | nd | nd |
| [54] | UCN/SiO2-RB DOX)@PPADT | 38.2 ± 3.6 | 980 nm, 1.0 W/cm2, 20 min | ABDA | Covalent | HeLa | Cytotoxicity (+) | nd | nd |
| [55] | SiNP-AAP-RB | 5–15 | 410 nm, 1.6 J/cm2, 15 min | Direct | Covalent | A549 | Cytotoxicity (+) | nd | nd |
| [52] | Silica capped rMSN-ts | Lenght 33 ± 27 and width 103 ± 15 | 5 mV green laser, 30 s | Direct | Covalent | MCF7 L269 | Cytotoxicity (+) | nd | nd |
| [53] | FITC-PGSN-RB | 100 | 480 nm, 100 W xenon lamp, 10 min | ABDA | Adsorption | HeLa | Cytoxicity (+) | nd | nd |
| [51] | RB-MSNs NPs | 150–180 | nd | Direct | Encapsulation | nd | nd | nd | nd |
| [62] | RB-DOX@HMSNs | 170 | 532 nm, 10 mW/cm2, 5 min | DPBF | Encapsulation | 4T1 | Cytotoxicity (+) | nd | nd |
| [61] | RB@ZIF-8@SiO2@RB NPs (drug loaded MOFs@SiO2 NPs) | 93.8 | 532 nm, 200 mW/cm2, 2 min or 100 mW/cm2, 7 min | DPBF | Encapsulation | 4T1 | Cytotoxicity (+) | BALB/c mice bearing AT1 tumors | PDT (+) |
| [56] | RB–MMSNs | 190 | 535 nm, 25 mW/cm2, 3 min | Uric acid | Encapsultation | B16 HeLa L929 | Cytotoxicity (+) | C57BL/6J mice | PDT (+) |
| [64] | RB-PEG5000-MSNs | 50 | 518 nm, 10 J/cm2, 5 min | Direct | Covalent | HeLa | Cytotoxicity (+) | nd | nd |
| [49] | RB-SiNP | electrostatic = 35 ± 5 covalent = 50 ± 5 | 480 nm, 1 h (fluence not cited) | SOSG | Covalent/Electrotatic | MCF-7 4451 | Cytoxicity (+) | nd | nd |
| PDT Organic NPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling between NPs and RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [72] | UCNP/PAH/HA-RB | 30.34 | 980 nm, 1.5 mW/cm2, 30 min | nd | Covalent | NIH3T3 | Cytotoxicity (+) | nd | nd |
| [78] | POEGMA-b-P(HPMA-co-RBMA) | 52 | 590–595 nm, 0.2 mW/cm2, 15 min | ADPA | Covalent | HCT116 K562 | Cytotoxicity (+) | nd | nd |
| [70] | RB-BTSA | 109 ± 5 | 490 nm, 30–135 J/cm2, 5–30 min | TMP–OH | Encapsulation | HeLa | Cytotoxicity (+) | nd | nd |
| [73] | PLGA-NP-RB | 28 | 520 nm, 200 mW/cm2, 30 min | nd | Encapsulation | MCF-7 HeLa | Cytotoxicity (+) | H22 tumor-bearing mice | PDT (+) |
| [71] | PVK@C153@RB | 340 | No biological test | 2-chlorophenol | Encapsulation | nd | nd | nd | nd |
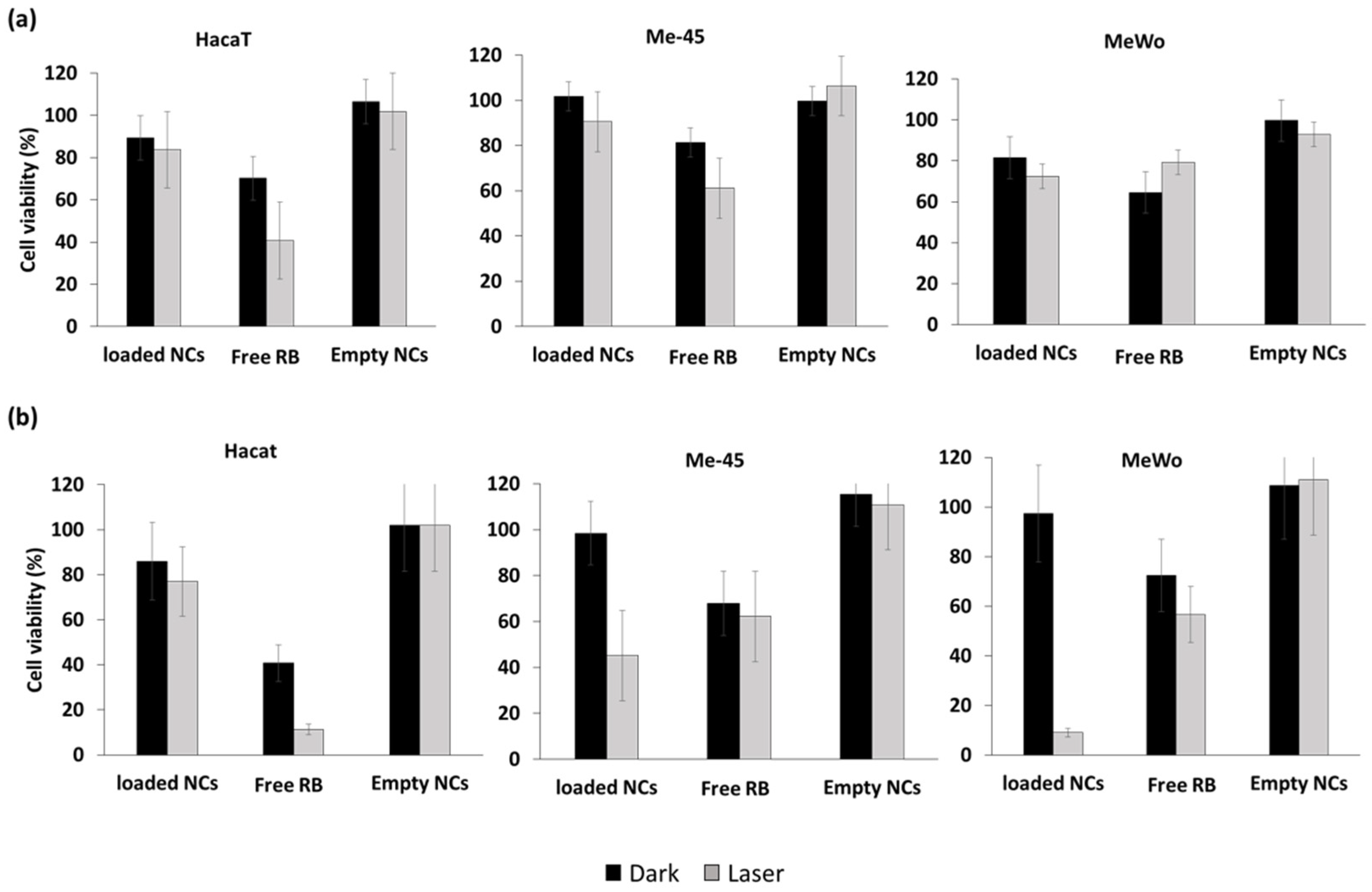
| [75] | NaYF4:Er3+,Yb3+ NPs@SPAN-20 micelles@RB@ TOPO@Cremophor@PLGA copolymer | 150 | 980 nm, 10 J/cm2, 6.2 W/cm2, 5 min | nd | Encapsulation | Me-45 MeWo HaCaT | Cytotoxicity (+) | Melanoma cells innoculated on monoclonal mouse | PDT (+) |
| [74] | HBNCs@RB | 220 | 632 nm, 15 mW/cm2, 60 min | DCFH-DA, | Encapsulation | Tramp-C1 | Cytotoxicity (+) | nd | nd |
| [69] | PAPAM dendrimers G 2.5-RB | 20 | 150 W xenon lamp 540 nm, 10 min | Iodure reaction | Covalent | DLA | Cytotoxicity (+) | nd | nd |
| [77] | polypeptide C18GR7RGDS | 17.28 | 808 nm, 1.5 W/cm2, 3 min | DPBF | Encapsulation | B16 HeLa | Cytotoxicity (+) | nd | nd |
| [76] | BP-CDPNP-RB | 280 | Two photons (810 nm, 245 mW/cm2, 20 min | ABDA | Encapsulation | MCF-7 | Cytotoxicity (+) | nd | nd |
| [77] | PARN@RB | 17.28 | 808 nm, 1.5 W/cm2, 3 min | DPBF DCF-DA | Encapsulation | B16 | Cytotoxicity (+) | HeLa tumor-bearing mice | PDT (+) |
| PDT Gold NPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling between NPs and RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [84] | AuNPs-RB | AuNPs-RB complexes: Electrostatic (53) Covalent (49) | 500 nm, 5 J/cm2 | nd | Covalent | Vero HeLa | Affinity (+) | nd | nd |
| [85] | Gold NPs@RB@DOX | 124.6 | 532 nm, 14.3 mW/cm2, 6 min | SOSG | Encapsulation | HCT116 MCF-7 CCD 841 CoN | Cytotoxicity (+) | nd | nd |
| [86] | CTO-RB-AuNR | 0.273 | 980 nm, 1.5 W/cm2, 6 min | DPBF | Covalent | Hep G2 | Cytotoxicity (+) | nd | nd |
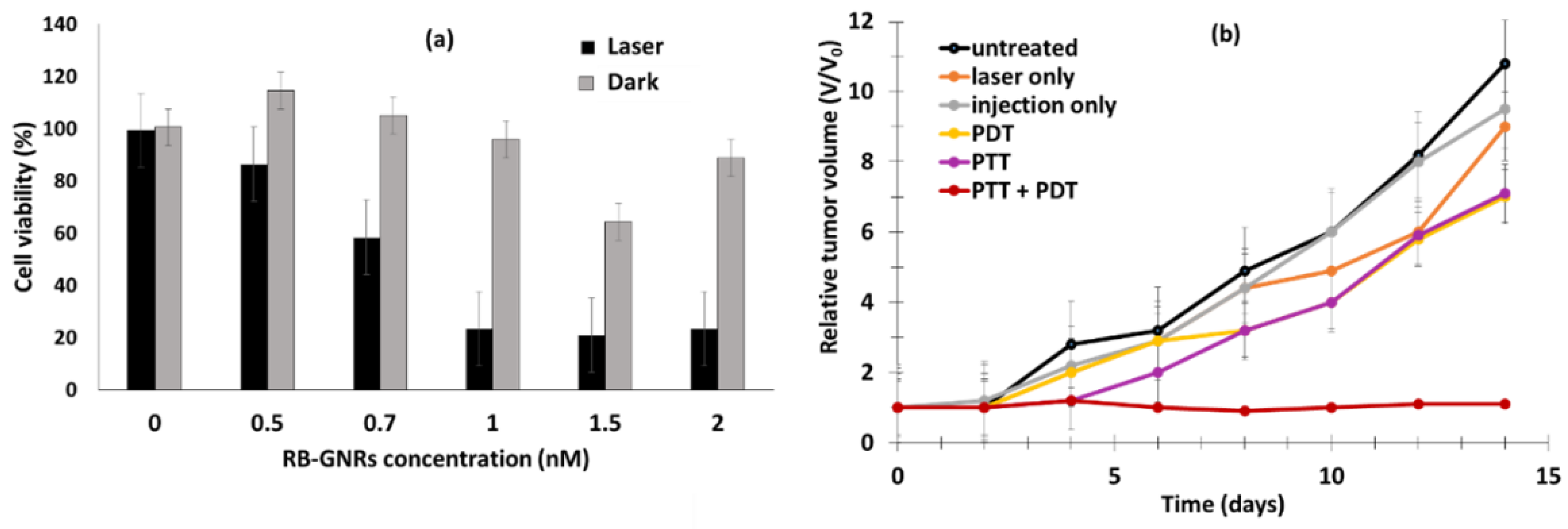
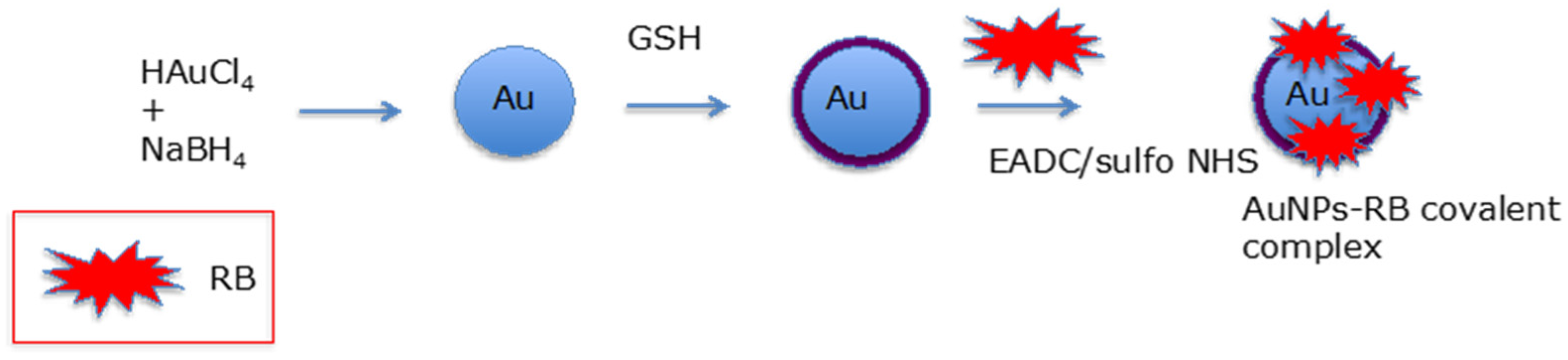
| [83] | AuNRs@RB | 13 ± 2 | PDT: 532 nm, 1.76 W/cm2, 10 min PTT: 810 nm NIR light, 8.16 W/cm2, 5 min | ABDA | Covalent | Cal-27 | Cytotoxicity (+) | Male Syrian Golden hamsters with oral carcinomas | PDT (+) |
| PDT Polymer Dots NPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling between NPs and RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [89] | Pdots-RB with: PEG350-PE, PEG2000-PE, PEG5000-PE | PEG350-PE: 43 ± 9 PEG2000-PE: 77 ± 0.3 PEG5000-PE: 60 ± 0.15 | 473 nm, 0.15 mJ/cm2, between 1 h and 4 h | DMA | Encapsulated in the coating of Pdots | MCF-7 | Cytotoxicity (+) | nd | nd |
| [90] | CQDS-RB | CQDs-RB: 33.1 ± 8.7 CQDs: 2.1 ± 0.3 | 532 nm, 20 mW/cm2, 30 min | SOSG | Covalent | MCF-7 | Cytotoxicity (+) | nd | nd |
| PDT Nanogels, Nanohybrid NPs, pH-Sensitive NPs, Magnetic NPs, Nanocomplexes, Nanocapsules | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling NPs-RB | Biological Tests/In Vitro | Biological Test/In Vivo | |||
| Cells Used | Results | Mice Used | Results | |||||||
| [92] | Ca2+/Gd3+-RB nanocapsules/RGD | 300 | 550 nm, 100 mW/cm2, 15 min | DPBF | Encapsulation | HepG2 | Cytotoxicity (+) | nd | nd | |
| [94] | BP-RB Bis(pyrene)-RB | 70 | 100 W xenon lamp (810 nm, 20 min) | ABDA | Encapsulation | MCF-7 | Cytotoxicity (+) | NIH mice (female) | PDT (+) | |
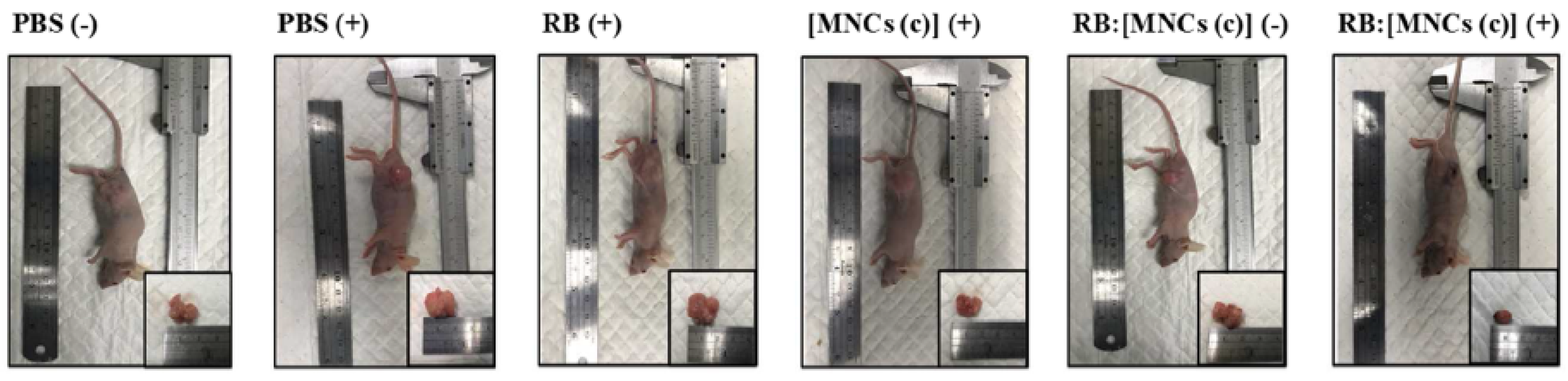
| [97] | (MNCs)-RB | 108.6 | 632 nm, 15 mW/cm2 or 532 nm, 100 mW/cm2 for 5 min | DCFH-DA | Electrostatic | MCF-7 Tramp-C1 SKOV-3 | Cytotoxicity (+) | BALB/c nude mice bearing MCF-7/MDR | PDT (+) | |
| [99] | Cs-Na/RB, Cs-Na-RBD | Cs-Na/RB: 50 Cs-Na/RBD: 60 | 518 nm, 4.0 W/cm2, 10 min | DCFH-DA | Encapsulation | PC9 | Cytotoxicity (+) | nd | nd | |
| [101] | UCNPs@MF-RB/PEG | 75 | 980 nm, 0.5 mW/cm2, 15 min | DPBF | Covalent | HeLa | Cytotoxicity (+) | nd | nd | |
| [103] | RB loaded in nanogel | 218 | 11 W LEDs (400–700 nm), 2 min | ABDA | Encapsulation | HT-29 | Cytotoxicity (+) | nd | nd | |
| X-PDT Silica NPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Tpe of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling NPs-RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [104] | LaF3:Tb@SiO2-RB (ScNP-RB) | 45 | No biological test | DPBF | Covalent | nd | nd | nd | nd |
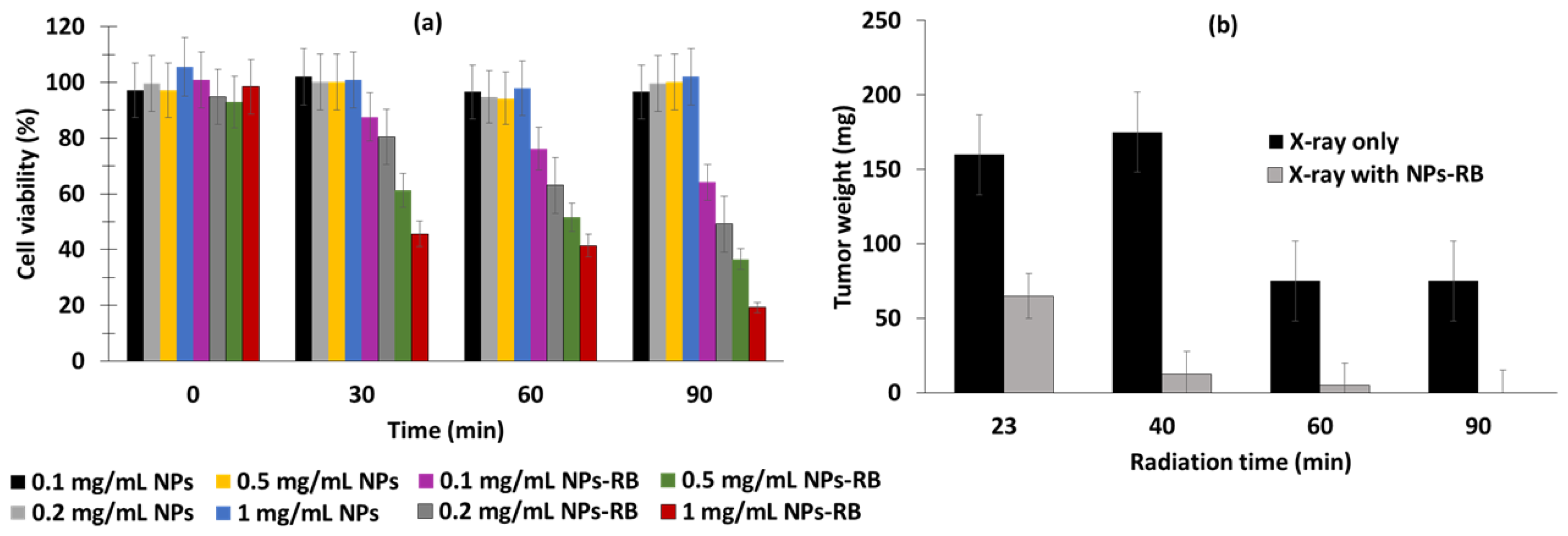
| [107] | CeF3:Tb3+, Gd3+ coated with MSN, loading with RB | 89.2 | 160 kV (1 Gy/min) | Iodure reaction | Covalent | 4T1 Renca Mgc893 | Toxicity (+) | BALB/c, 4T1 | PDT (+) |
| [105] | CSS (NaLuF4:Gd,Eu@NaLuF4:Gd@NaLuF4:Gd,Tb)- CSS@MSiO2@PAH-RB | 27.5 | 160 kV, 25 mA, 1, 3, 5 Gy | nd | Adsorption | MCF-7/MDA-MB-231 | Cytotoxicity (+) | nd | nd |
| [60] | Gd2.98Ce0.02Al5O12 NPs (GAG) coated with mSiO2 and loaded with RB, GAG@mSiO2@RB | 147 | Blue light (470 nm) 20 mW/cm2 (55 kV) | nd | Adsorption | MDA-MB-231 | Cytotoxicity (+) | nd | nd |
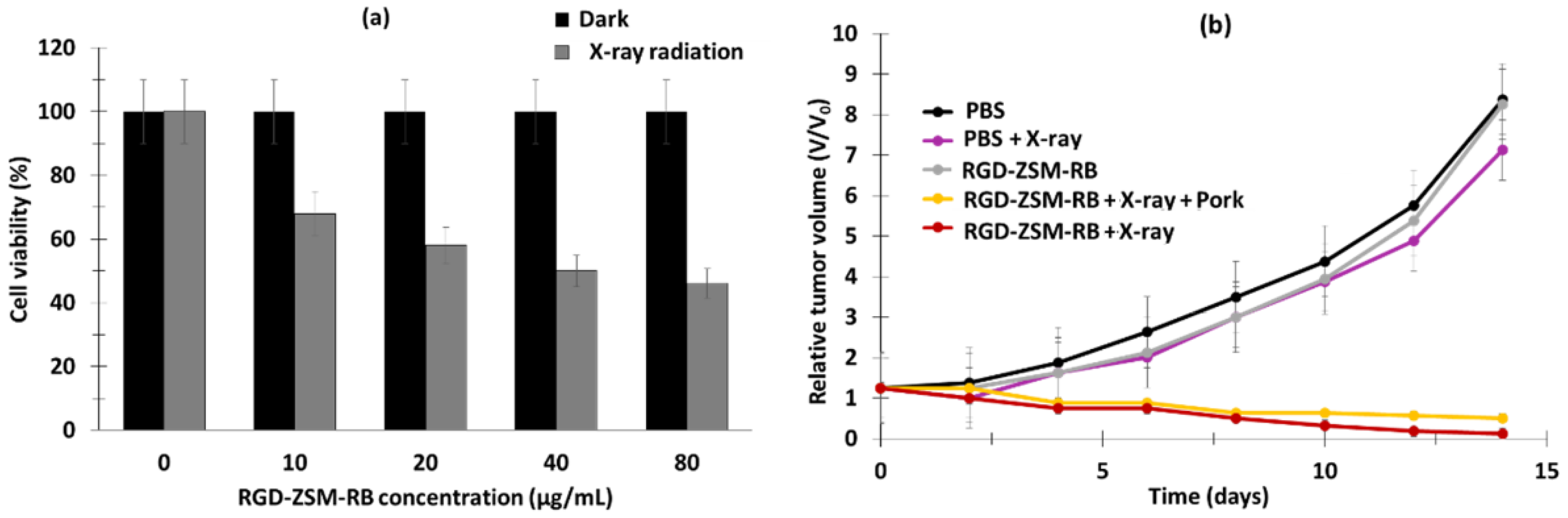
| [106] | RB-ZSM-RGD | 80.8 ± 3.5 | 50 kV, 1.0 Gy, 10 min | SOSG | Covalent | U87MG | Cytotoxicity (+) | Nude mice U98 MG | PDT (+) |
| X-PDT Polymer NPs | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | NPs Size (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling NPs-RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells | Results | Mice Used | Results | ||||||
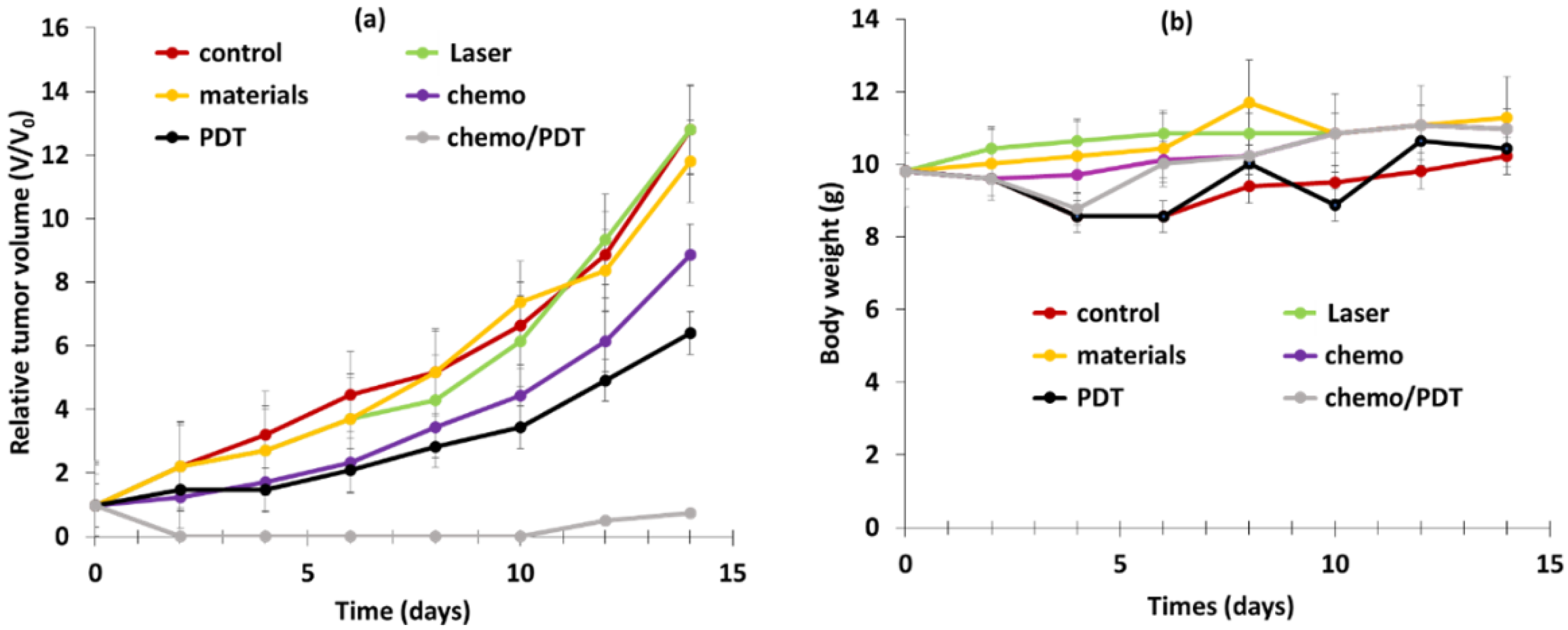
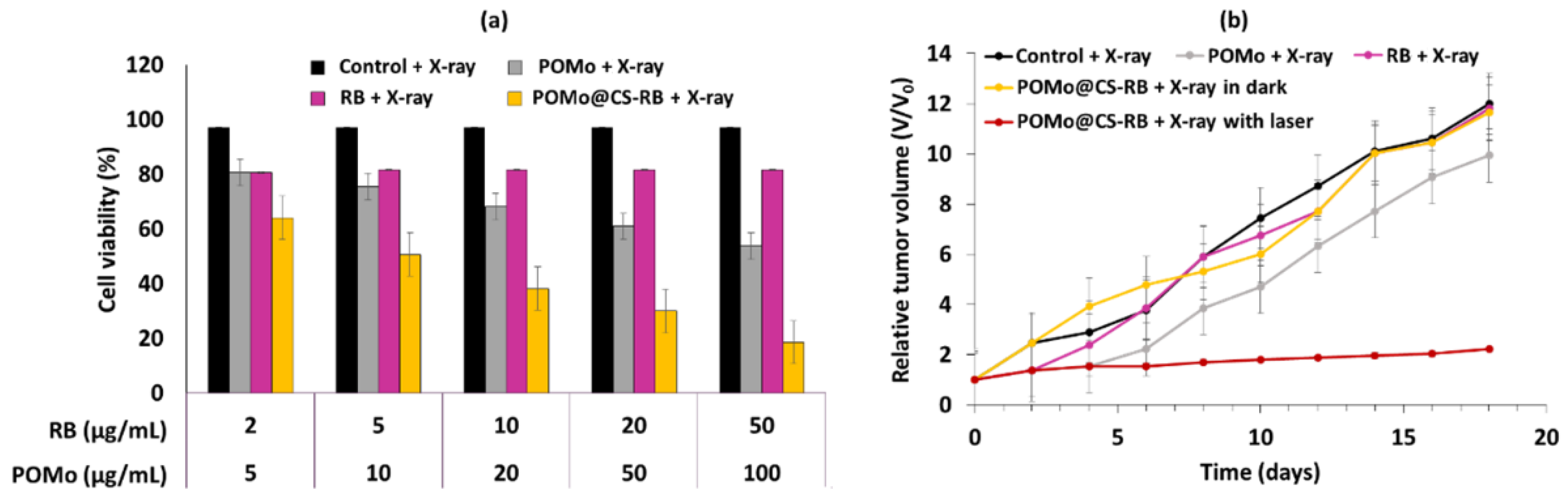
| [110] | Gadolinium (Gd)–RB coordination polymer nanodots (GRDs) | 3.3 ± 0.8 | In vitro: 532 nm, 30 mW/cm2, 5 min; 1 Gy In vivo: 532 nm, 140 mW/cm2, 15 min; 1 Gy | SOSG | Coordination | 4T1 | Cytotoxicity (+) | BALB/c mice, 4T1-tumor-bearing mice | PDT (+) |
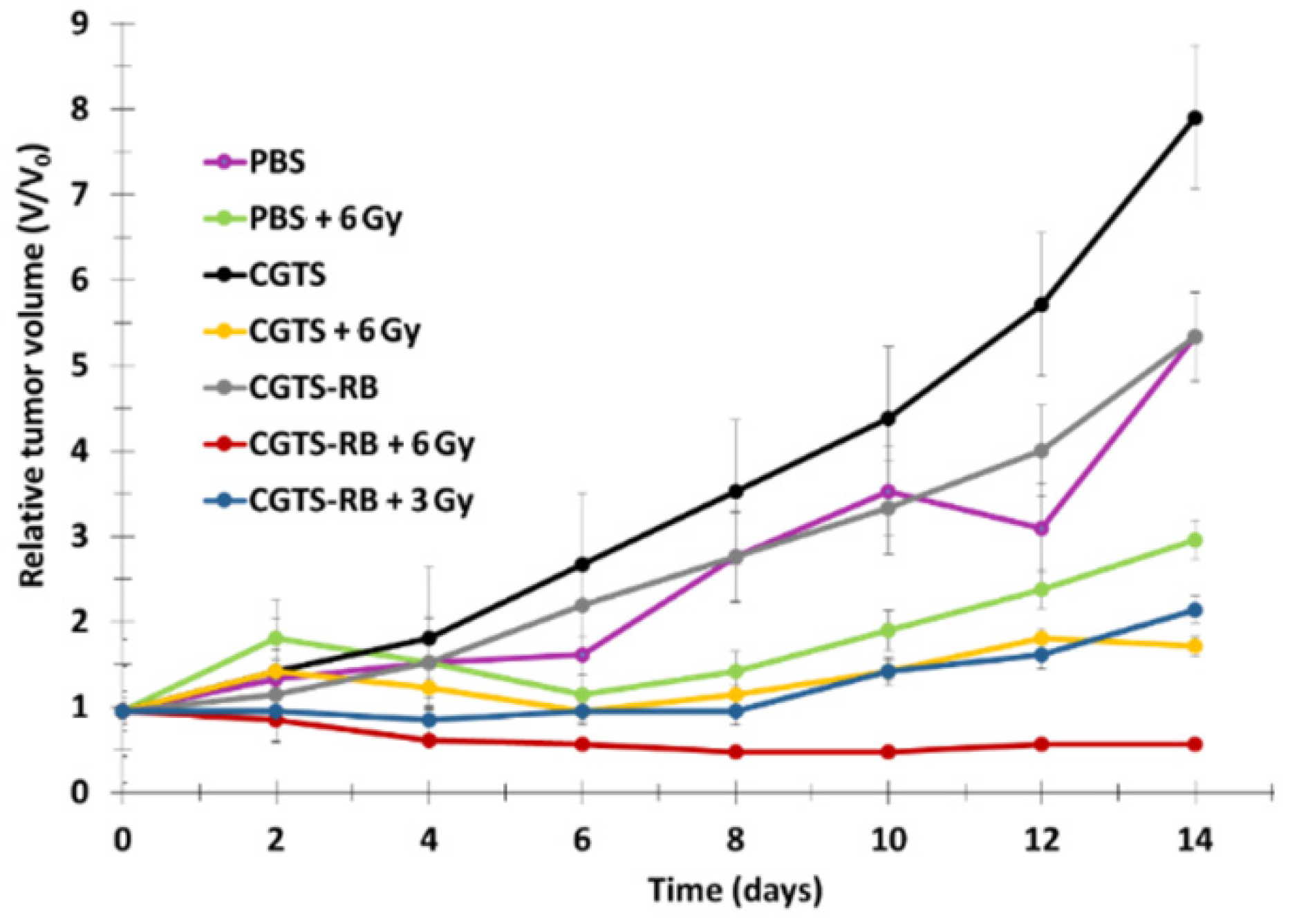
| [109] | POMo@CS–RB | 80 | 2 Gy/min (160 kV) | SOSG | Adsorption | 4T1 | Cytotoxicity (+) | BALB/c mice, 4T1-tumor-bearing mice | PDT (+) |
| [108] | Ln NPs-PEG-RB | 4 | 2 Gy (150 kV) | nd | Covalent | nd | nd | B16 murine mela noma cells | PDT (+) |
| X-PDT Nanocomposites | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| References | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling NPs-RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [112] | β-NaGdF4:Tb3+-RB | 25.6 | 80 kV, 0.5 mA (0,05–2 Gy), 20 min | DPBF | Covalent | HepG2 | Cytotoxicity (+) | Nude Mice with subcutaneous HepG2 xenografts | PDT (+) |
| [111] | β-NaGdF4:Tb3+-RB | 10 | 80 kV, 0.5 mA and 45 cm distance (1.17 Gy/h) | DPBF | Covalent | HepG2 | Cytotoxicity (+) | Female BALB/c nude mice | PDT (+) |
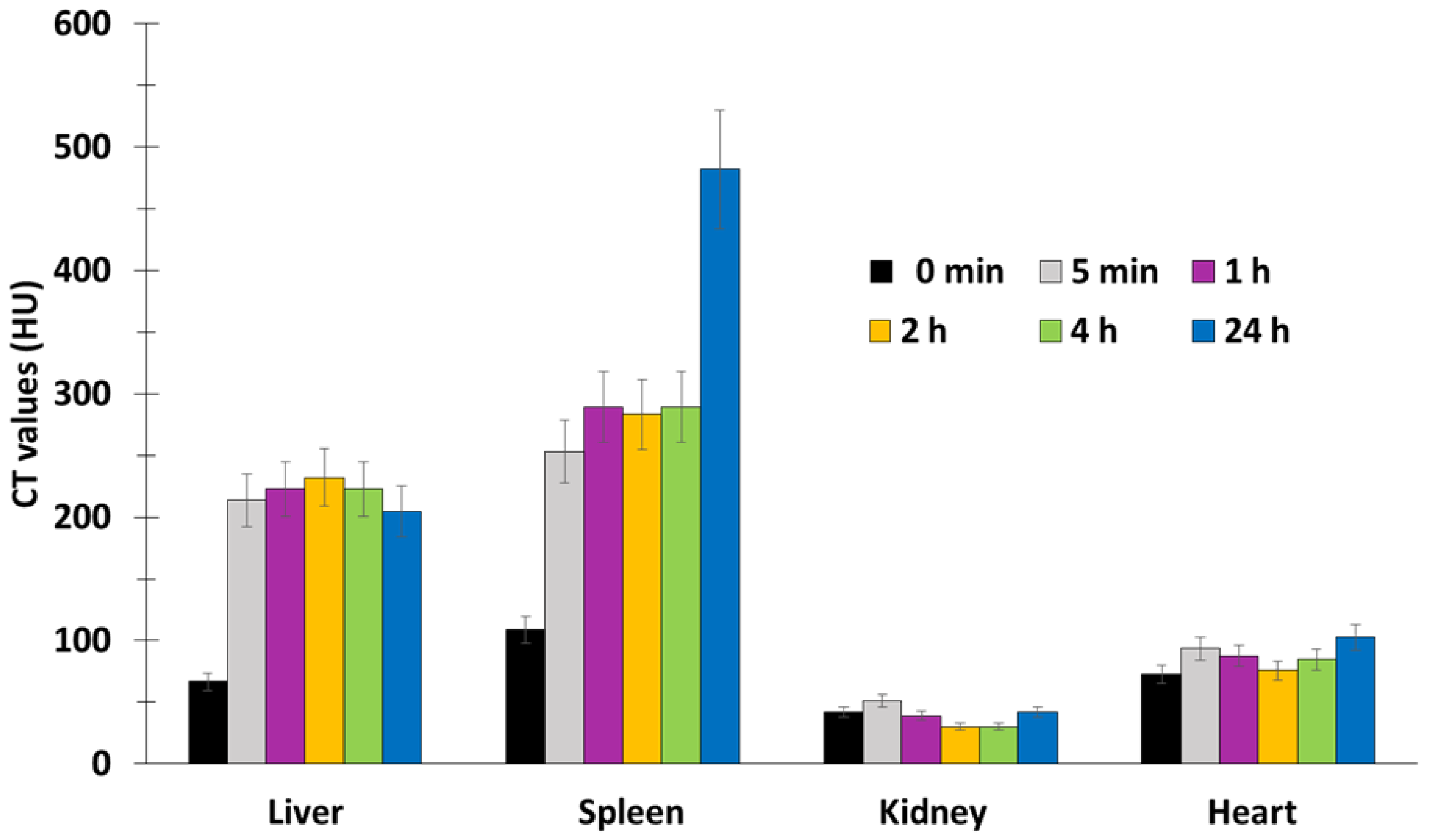
| [113] | PEG-capped GdF3:Tb3+@RB nanocomposites | Length: 250 Width: 60 | 136 mGy/4 min | nd | Adsorption | nd | nd | BALB/c (ca. 3 months age, weight 34–35 g) male mice | PDT (+) |
| X-PDT Lanthanide@MOF, Nanoprobes, Nanophosphors, ScNPs@RB | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Reference | Type of NPs | Size of NPs (nm) | Irradiation Conditions | Type of 1O2 Detection | Type of Coupling NP-RB | Biological Tests/In Vitro | Biological Test/In Vivo | ||
| Cells Used | Results | Mice Used | Results | ||||||
| [118] | SNPs@Zr-MOF@RB- SNPs | 30 | 45 kV (0, 3, 6, 9, 12, 15 min). | DPBF | Covalent | 4T1 | Cytotoxicity (+) | 4T1 tumor-bearing BALB/c mice) | PDT (+) |
| [114] | ScNPs: LaF3:Tb-RB | 38.9 | 75 kV, 2.0 mA | DPBF | Encapsulation | nd | nd | nd | nd |
| [117] | NaGdF4@NaGdF4:Tb@NaYF4 (CSS)@RB@cRGD | 18.8 | 4 Gy/min | DPBF | Covalent | U87MG HepG2 NIH-3T3 | Cytotocity (+) | nd | nd |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dhaini, B.; Wagner, L.; Moinard, M.; Daouk, J.; Arnoux, P.; Schohn, H.; Schneller, P.; Acherar, S.; Hamieh, T.; Frochot, C. Importance of Rose Bengal Loaded with Nanoparticles for Anti-Cancer Photodynamic Therapy. Pharmaceuticals 2022, 15, 1093. https://doi.org/10.3390/ph15091093
Dhaini B, Wagner L, Moinard M, Daouk J, Arnoux P, Schohn H, Schneller P, Acherar S, Hamieh T, Frochot C. Importance of Rose Bengal Loaded with Nanoparticles for Anti-Cancer Photodynamic Therapy. Pharmaceuticals. 2022; 15(9):1093. https://doi.org/10.3390/ph15091093
Chicago/Turabian StyleDhaini, Batoul, Laurène Wagner, Morgane Moinard, Joël Daouk, Philippe Arnoux, Hervé Schohn, Perrine Schneller, Samir Acherar, Tayssir Hamieh, and Céline Frochot. 2022. "Importance of Rose Bengal Loaded with Nanoparticles for Anti-Cancer Photodynamic Therapy" Pharmaceuticals 15, no. 9: 1093. https://doi.org/10.3390/ph15091093
APA StyleDhaini, B., Wagner, L., Moinard, M., Daouk, J., Arnoux, P., Schohn, H., Schneller, P., Acherar, S., Hamieh, T., & Frochot, C. (2022). Importance of Rose Bengal Loaded with Nanoparticles for Anti-Cancer Photodynamic Therapy. Pharmaceuticals, 15(9), 1093. https://doi.org/10.3390/ph15091093











