Segmental Upregulation of ASIC1 Channels in the Formalin Acute Pain Mouse Model
Abstract
1. Introduction
2. Results
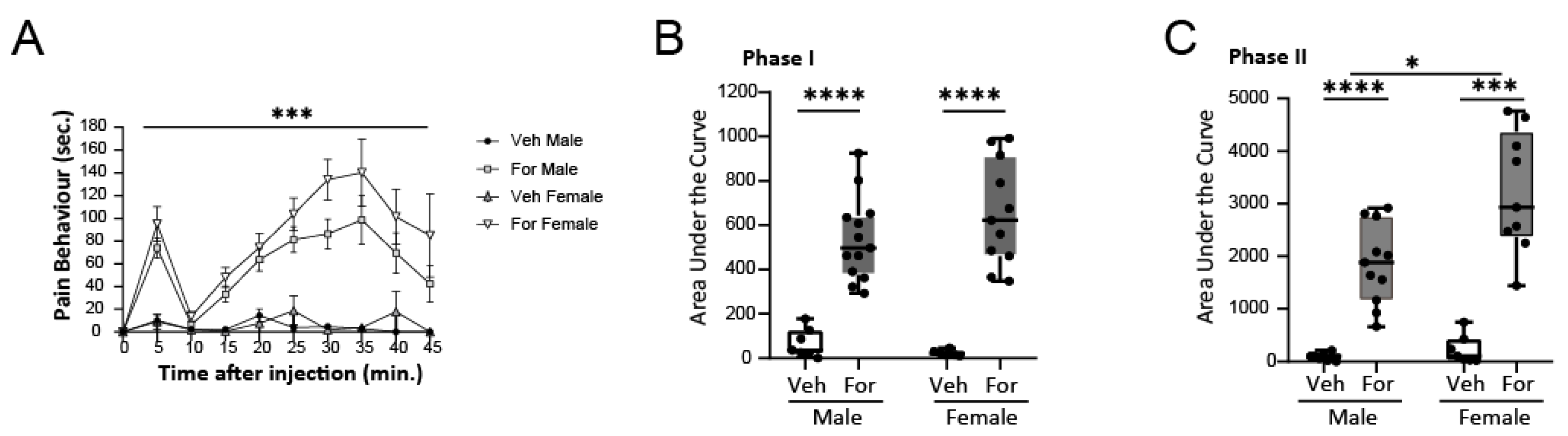
2.1. Formalin Test to Assess the Pain Pathway in Mice
2.2. Elevated ASIC1 Protein in Central and Peripheral Areas in Pain
2.3. Signaling Down-Stream ASIC1a
2.4. Regulation of ASIC1 Protein: Potential Upstream Mechanisms Involved
3. Discussion
4. Materials and Methods
4.1. Animal Model and Formalin Test
4.2. Tissue Collection
4.3. Protein Analysis
4.4. Quantitative PCR
4.5. Data Analysis and Figure Preparation
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Boscardin, E.; Alijevic, O.; Hummler, E.; Frateschi, S.; Kellenberger, S. The function and regulation of acid-sensing ion channels (ASICs) and the epithelial Na + channel (ENaC): IUPHAR Review 19. Br. J. Pharmacol. 2016, 173, 2671–2701. [Google Scholar] [CrossRef] [PubMed]
- Uchitel, O.D.; González Inchauspe, C.; Weissmann, C. Synaptic signals mediated by protons and acid-sensing ion channels. Synapse 2019, 73, e22120. [Google Scholar] [CrossRef] [PubMed]
- Rook, M.L.; Musgaard, M.; MacLean, D.M. Coupling structure with function in acid-sensing ion channels: Challenges in pursuit of proton sensors. J. Physiol. 2021, 599, 417–430. [Google Scholar] [CrossRef] [PubMed]
- Lingueglia, E. Acid-sensing Ion Channels in Sensory Perception. J. Biol. Chem. 2007, 282, 17325–17329. [Google Scholar] [CrossRef] [PubMed]
- Duan, B.; Wu, L.-J.; Yu, Y.-Q.; Ding, Y.; Jing, L.; Xu, L.; Chen, J.; Xu, T.-L. Upregulation of acid-sensing ion channel ASIC1a in spinal dorsal horn neurons contributes to inflammatory pain hypersensitivity. J. Neurosci. Off. J. Soc. Neurosci. 2007, 27, 11139–11148. [Google Scholar] [CrossRef]
- Papalampropoulou-Tsiridou, M.; Labrecque, S.; Godin, A.G.; De Koninck, Y.; Wang, F. Differential Expression of Acid—Sensing Ion Channels in Mouse Primary Afferents in Naïve and Injured Conditions. Front. Cell. Neurosci. 2020, 14, 103. [Google Scholar] [CrossRef]
- Qiang, M.; Dong, X.; Zha, Z.; Zuo, X.K.; Song, X.L.; Zhao, L.; Yuan, C.; Huang, C.; Tao, P.; Hu, Q.; et al. Selection of an ASIC1a-blocking combinatorial antibody that protects cells from ischemic death. Proc. Natl. Acad. Sci. USA 2018, 115, E7469–E7477. [Google Scholar] [CrossRef]
- Kalpachidou, T.; Kummer, K.K.; Kress, M. Non-coding RNAs in neuropathic pain. Neuronal Signal. 2020, 4, NS20190099. [Google Scholar] [CrossRef]
- Wu, S.; Bono, J.; Tao, Y.X. Long noncoding RNA (lncRNA): A target in neuropathic pain. Expert Opin. Ther. Targets 2019, 23, 15–20. [Google Scholar] [CrossRef]
- Bali, K.K.; Kuner, R. Noncoding RNAs: Key molecules in understanding and treating pain. Trends Mol. Med. 2014, 20, 437–448. [Google Scholar] [CrossRef]
- Xu, M.; Wu, R.; Zhang, L.; Zhu, H.Y.; Xu, G.Y.; Qian, W.; Zhang, P.A. Decreased mir-485-5p contributes to inflammatory pain through post-transcriptional upregulation of asic1 in rat dorsal root ganglion. J. Pain Res. 2020, 13, 3013–3022. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Rojas, V.A.; García, G.; Noriega-Navarro, R.; Guzmán-Priego, C.G.; Torres-López, J.E.; Granados-Soto, V.; Murbartián, J. Peripheral and spinal TRPA1 channels contribute to formalin-induced long-lasting mechanical hypersensitivity. J. Pain Res. 2018, 11, 51–60. [Google Scholar] [CrossRef] [PubMed]
- García, G.; Martínez-Rojas, V.A.; Murbartián, J. TREK-1 potassium channels participate in acute and long-lasting nociceptive hypersensitivity induced by formalin in rats. Behav. Brain Res. 2021, 413, 113446. [Google Scholar] [CrossRef]
- Kanai, Y.; Hara, T.; Imai, A.; Kanai, Y. Participation of the spinal TRPV1 receptors in formalin-evoked pain transduction: A study using a selective TRPV1 antagonist, iodo-resiniferatoxin. J. Pharm. Pharmacol. 2010, 58, 489–493. [Google Scholar] [CrossRef]
- Ferreira, J.; Santos, A.R.S.; Calixto, J.B. Antinociception produced by systemic, spinal and supraspinal administration of amiloride in mice. Life Sci. 1999, 65, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Jeong, S.; Lee, S.H.; Kim, Y.O.; Yoon, M.H. Antinociceptive effects of amiloride and benzamil in neuropathic pain model rats. J. Korean Med. Sci. 2013, 28, 1238–1243. [Google Scholar] [CrossRef][Green Version]
- Mazzuca, M.; Heurteaux, C.; Alloui, A.; Diochot, S.; Baron, A.; Voilley, N.; Blondeau, N.; Escoubas, P.; Gélot, A.; Cupo, A.; et al. A tarantula peptide against pain via ASIC1a channels and opioid mechanisms. Nat. Neurosci. 2007, 10, 943–945. [Google Scholar] [CrossRef]
- Salinas, L.C.C.; Rozenfeld, P.; Gatto, R.G.; Reisin, R.C.; Uchitel, O.D.; Weissmann, C.; Castellanos, L.C.S.; Rozenfeld, P.; Gatto, R.G.; Reisin, R.C.; et al. Upregulation of ASIC1a channels in an in vitro model of Fabry disease. Neurochem. Int. 2020, 140, 104824. [Google Scholar] [CrossRef]
- Salinas Castellanos, L.C.; Uchitel, O.D.; Weissmann, C. Signaling Pathways in Proton and Non-proton ASIC1a Activation. Front. Cell. Neurosci. 2021, 15, 735414. [Google Scholar] [CrossRef]
- Ji, R.R.; Baba, H.; Brenner, G.J.; Woolf, C.J. Nociceptive-specific activation of ERK in spinal neurons contributes to pain hypersensitivity. Nat. Neurosci. 1999, 2, 1114–1119. [Google Scholar] [CrossRef]
- Qu, Y.J.; Jia, L.; Zhang, X.; Wei, H.; Yue, S.W. MAPK Pathways Are Involved in Neuropathic Pain in Rats with Chronic Compression of the Dorsal Root Ganglion. Evid.-Based Complement. Altern. Med. 2016, 2016, 6153215. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.; Quirion, R. The ERK/MAPK pathway, as a target for the treatment of neuropathic pain. Expert Opin. Ther. Targets 2005, 9, 699–713. [Google Scholar] [CrossRef]
- Dai, R.P.; Li, C.Q.; Zhang, J.W.; Li, F.; Shi, X.D.; Zhang, J.Y.; Zhou, X.F. Biphasic activation of extracellular signal-regulated kinase in anterior cingulate cortex distinctly regulates the development of pain-related anxiety and mechanical hypersensitivity in rats after incision. Anesthesiology 2011, 115, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.; Zhuo, M. Activation of Erk in the anterior cingulate cortex during the induction and expression of chronic pain. Mol. Pain 2008, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Cao, H.; Gao, Y.J.; Ren, W.H.; Li, T.T.; Duan, K.Z.; Cui, Y.H.; Cao, X.H.; Zhao, Z.Q.; Ji, R.R.; Zhang, Y.Q. Activation of extracellular signal-regulated kinase in the anterior cingulate cortex contributes to the induction and expression of affective pain. J. Neurosci. 2009, 29, 3307–3321. [Google Scholar] [CrossRef]
- Okine, B.N.; Mc Laughlin, G.; Gaspar, J.C.; Harhen, B.; Roche, M.; Finn, D.P. Antinociceptive Effects of the GPR55 Antagonist CID16020046 Injected into the Rat Anterior Cingulate Cortex. Neuroscience 2020, 443, 19–29. [Google Scholar] [CrossRef]
- Skerratt, S.E.; West, C.W. Ion channel therapeutics for pain. Channels 2015, 9, 344. [Google Scholar] [CrossRef]
- Bouali-Benazzouz, R.; Landry, M.; Benazzouz, A.; Fossat, P. Neuropathic pain modeling: Focus on synaptic and ion channel mechanisms. Prog. Neurobiol. 2021, 201, 102030. [Google Scholar] [CrossRef]
- Voilley, N. Acid-sensing ion channels (ASICs): New targets for the analgesic effects of non-steroid anti-inflammatory drugs (NSAIDs). Curr. Drug Targets Inflamm. Allergy 2004, 3, 71–79. [Google Scholar] [CrossRef]
- Chen, B.; Liu, J.; Ho, T.; Ding, X.; Mo, Y. ERK-mediated NF-κB activation through ASIC1 in response to acidosis. Oncogenesis 2016, 5, e279. [Google Scholar] [CrossRef] [PubMed]
- Carattino, M.D.; Montalbetti, N. Acid-sensing ion channels in sensory signaling. Am. J. Physiol. Renal Physiol. 2020, 318, F531–F543. [Google Scholar] [CrossRef] [PubMed]
- Staniland, A.A.; McMahon, S.B. Mice lacking acid-sensing ion channels (ASIC) 1 or 2, but not ASIC3, show increased pain behaviour in the formalin test. Eur. J. Pain 2009, 13, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Tian, L.J.; DU, Y.R.; Xiao, Y.; Lv, Z.M.; Yu, Y.Q.; Cui, X.Y.; Chen, J. Mediating roles of the vanilloid receptor TRPV1 in activation of rat primary afferent nociceptive neurons by formaldehyde. Sheng Li Xue Bao 2009, 61, 404–416. [Google Scholar]
- Malmberg, A.B.; Yaksh, T.L. Antinociceptive actions of spinal nonsteroidal anti-inflammatory agents on the formalin test in the rat. J. Pharmacol. Exp. Ther. 1992, 263, 136–146. [Google Scholar]
- Voilley, N.; De Weille, J.; Mamet, J.; Lazdunski, M. Nonsteroid anti-inflammatory drugs inhibit both the activity and the inflammation-induced expression of acid-sensing ion channels in nociceptors. J. Neurosci. 2001, 21, 8026–8033. [Google Scholar] [CrossRef]
- Rigaud, M.; Gemes, G.; Barabas, M.-E.; Chernoff, D.I.; Abram, S.E.; Stucky, C.L.; Hogan, Q.H. Species and strain differences in rodent sciatic nerve anatomy: Implications for studies of neuropathic pain. Pain 2008, 136, 188–201. [Google Scholar] [CrossRef] [PubMed]
- Lindborg, J.A.; Niemi, J.P.; Howarth, M.A.; Liu, K.W.; Moore, C.Z.; Mahajan, D.; Zigmond, R.E. Molecular and cellular identification of the immune response in peripheral ganglia following nerve injury. J. Neuroinflamm. 2018, 15, 192. [Google Scholar] [CrossRef] [PubMed]
- Ando, H.; Hirose, M.; Kurosawa, G.; Impey, S.; Mikoshiba, K. Time-lapse imaging of microRNA activity reveals the kinetics of microRNA activation in single living cells. Sci. Rep. 2017, 7, 12642. [Google Scholar] [CrossRef]
- Perry, M.M.; Moschos, S.A.; Williams, A.E.; Shepherd, N.J.; Larner-Svensson, H.M.; Lindsay, M.A. Rapid changes in microRNA-146a expression negatively regulate the interleukin-1β induced inflammatory response in human lung alveolar epithelial cells. J. Immunol. 2008, 180, 5689. [Google Scholar] [CrossRef]
- Kynast, K.L.; Russe, O.Q.; Möser, C.V.; Geisslinger, G.; Niederberger, E. Modulation of central nervous system-specific microRNA-124a alters the inflammatory response in the formalin test in mice. Pain 2013, 154, 368–376. [Google Scholar] [CrossRef]
- de la Rosa, I.A.; Perez-Sanchez, C.; Ruiz-Limon, P.; Patiño-Trives, A.; Torres-Granados, C.; Jimenez-Gomez, Y.; del Carmen Abalos-Aguilera, M.; Cecchi, I.; Ortega, R.; Caracuel, M.A.; et al. Impaired microRNA processing in neutrophils from rheumatoid arthritis patients confers their pathogenic profile. Modulation by biological therapies. Haematologica 2020, 105, 2250. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, C.; Sharma, A.R.; Sharma, G.; Lee, S.S. The Interplay among miRNAs, Major Cytokines, and Cancer-Related Inflammation. Mol. Ther. Nucleic Acids 2020, 20, 606. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.X.; Shen, Y.; Liu, Y.; Wang, H.F.; Liang, C.Y.; Luo, M. Inflammation-dependent downregulation of miR-532-3p mediates apoptotic signaling in human sarcopenia through targeting BAK1. Int. J. Biol. Sci. 2020, 16, 1481–1494. [Google Scholar] [CrossRef] [PubMed]
- Melemedjian, O.K.; Asiedu, M.N.; Tillu, D.V.; Peebles, K.A.; Yan, J.; Ertz, N.; Dussor, G.O.; Price, T.J. IL-6- and NGF-induced rapid control of protein synthesis and nociceptive plasticity via convergent signaling to the eIF4F complex. J. Neurosci. 2010, 30, 15113–15123. [Google Scholar] [CrossRef]
- Um, S.W.; Kim, M.J.; Leem, J.W.; Bai, S.J.; Lee, B.H. Pain-Relieving Effects of mTOR Inhibitor in the Anterior Cingulate Cortex of Neuropathic Rats. Mol. Neurobiol. 2019, 56, 2482–2494. [Google Scholar] [CrossRef]
- Gaumond, I.; Arsenault, P.; Marchand, S. The role of sex hormones on formalin-induced nociceptive responses. Brain Res. 2002, 958, 139–145. [Google Scholar] [CrossRef]
- Kim, S.J.; Calejesan, A.A.; Li, P.; Wei, F.; Zhuo, M. Sex differences in late behavioral response to subcutaneous formalin injection in mice. Brain Res. 1999, 829, 185–189. [Google Scholar] [CrossRef]
- Perissin, L.; Facchin, P.; Porro, C.A. Tonic pain response in mice: Effects of sex, season and time of day. Life Sci. 2003, 72, 897–907. [Google Scholar] [CrossRef]
- Chanda, M.L.; Mogil, J.S. Sex differences in the effects of amiloride on formalin test nociception in mice. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2006, 291, 335–342. [Google Scholar] [CrossRef]
- Cui, C.; Yang, W.; Shi, J.; Zhou, Y.; Yang, J.; Cui, Q.; Zhou, Y. Identification and Analysis of Human Sex-biased MicroRNAs. Genomics. Proteom. Bioinform. 2018, 16, 200. [Google Scholar] [CrossRef]
- Guo, L.; Zhang, Q.; Ma, X.; Wang, J.; Liang, T. miRNA and mRNA expression analysis reveals potential sex-biased miRNA expression. Sci. Rep. 2017, 7, 39812. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Eghbali, M. Influence of sex differences on microRNA gene regulation in disease. Biol. Sex Differ. 2014, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Jaggi, A.S.; Singh, N. Role of different brain areas in peripheral nerve injury-induced neuropathic pain. Brain Res. 2011, 1381, 187–201. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Koga, K.; Descalzi, G.; Qiu, S.; Wang, J.; Zhang, L.S.; Zhang, Z.J.; He, X.B.; Qin, X.; Xu, F.Q.; et al. Postsynaptic potentiation of corticospinal projecting neurons in the anterior cingulate cortex after nerve injury. Mol. Pain 2014, 10. [Google Scholar] [CrossRef]
- Zhao, R.; Zhou, H.; Huang, L.; Xie, Z.; Wang, J.; Gan, W.-B.; Yang, G. Neuropathic Pain Causes Pyramidal Neuronal Hyperactivity in the Anterior Cingulate Cortex. Front. Cell. Neurosci. 2018, 12, 107. [Google Scholar] [CrossRef]
- Lee, I.O.; Jeong, Y.S. Effects of different concentrations of formalin on paw edema and pain behaviors in rats. J. Korean Med. Sci. 2002, 17, 81–85. [Google Scholar] [CrossRef]
- Munro, G. Pharmacological assessment of the rat formalin test utilizing the clinically used analgesic drugs gabapentin, lamotrigine, morphine, duloxetine, tramadol and ibuprofen: Influence of low and high formalin concentrations. Eur. J. Pharmacol. 2009, 605, 95–102. [Google Scholar] [CrossRef]
- Hu, S.W.; Zhang, Q.; Xia, S.H.; Zhao, W.N.; Li, Q.Z.; Yang, J.X.; An, S.; Ding, H.L.; Zhang, H.; Cao, J.L. Contralateral Projection of Anterior Cingulate Cortex Contributes to Mirror-Image Pain. J. Neurosci. 2021, 41, 9988–10003. [Google Scholar] [CrossRef]
- Lopes, D.M.; Cater, H.L.; Thakur, M.; Wells, S.; McMahon, S.B. A refinement to the formalin test in mice [version 2; peer review: 2 approved]. F1000Research 2019, 8, 891. [Google Scholar] [CrossRef]
- Hylden, J.L.K.; Wilcox, G.L. Intrathecal morphine in mice: A new technique. Eur. J. Pharmacol. 1980, 67, 313–316. [Google Scholar] [CrossRef]
- Paulazo, M.A.; Sodero, A.O. SIRT-1 Activity Sustains Cholesterol Synthesis in the Brain. Neuroscience 2021, 476, 116–124. [Google Scholar] [CrossRef] [PubMed]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gobetto, M.N.; Castellanos, L.C.S.; Contreras, N.E.; Sodero, A.O.; Cambiagno, D.A.; Malnati, G.O.M.; Montes, M.M.; Uchitel, O.D.; Weissmann, C. Segmental Upregulation of ASIC1 Channels in the Formalin Acute Pain Mouse Model. Pharmaceuticals 2022, 15, 1539. https://doi.org/10.3390/ph15121539
Gobetto MN, Castellanos LCS, Contreras NE, Sodero AO, Cambiagno DA, Malnati GOM, Montes MM, Uchitel OD, Weissmann C. Segmental Upregulation of ASIC1 Channels in the Formalin Acute Pain Mouse Model. Pharmaceuticals. 2022; 15(12):1539. https://doi.org/10.3390/ph15121539
Chicago/Turabian StyleGobetto, María Natalia, Libia Catalina Salinas Castellanos, Natalia Estefanía Contreras, Alejandro Omar Sodero, Damián Alejandro Cambiagno, Georgina Oriana Mingolo Malnati, Mayra Micaela Montes, Osvaldo Daniel Uchitel, and Carina Weissmann. 2022. "Segmental Upregulation of ASIC1 Channels in the Formalin Acute Pain Mouse Model" Pharmaceuticals 15, no. 12: 1539. https://doi.org/10.3390/ph15121539
APA StyleGobetto, M. N., Castellanos, L. C. S., Contreras, N. E., Sodero, A. O., Cambiagno, D. A., Malnati, G. O. M., Montes, M. M., Uchitel, O. D., & Weissmann, C. (2022). Segmental Upregulation of ASIC1 Channels in the Formalin Acute Pain Mouse Model. Pharmaceuticals, 15(12), 1539. https://doi.org/10.3390/ph15121539






