Neuropeptide S Receptor as an Innovative Therapeutic Target for Parkinson Disease
Abstract
1. Introduction
2. Pathophysiology and Pharmacotherapy of Parkinson Disease: The Relevance of Innovative Treatments
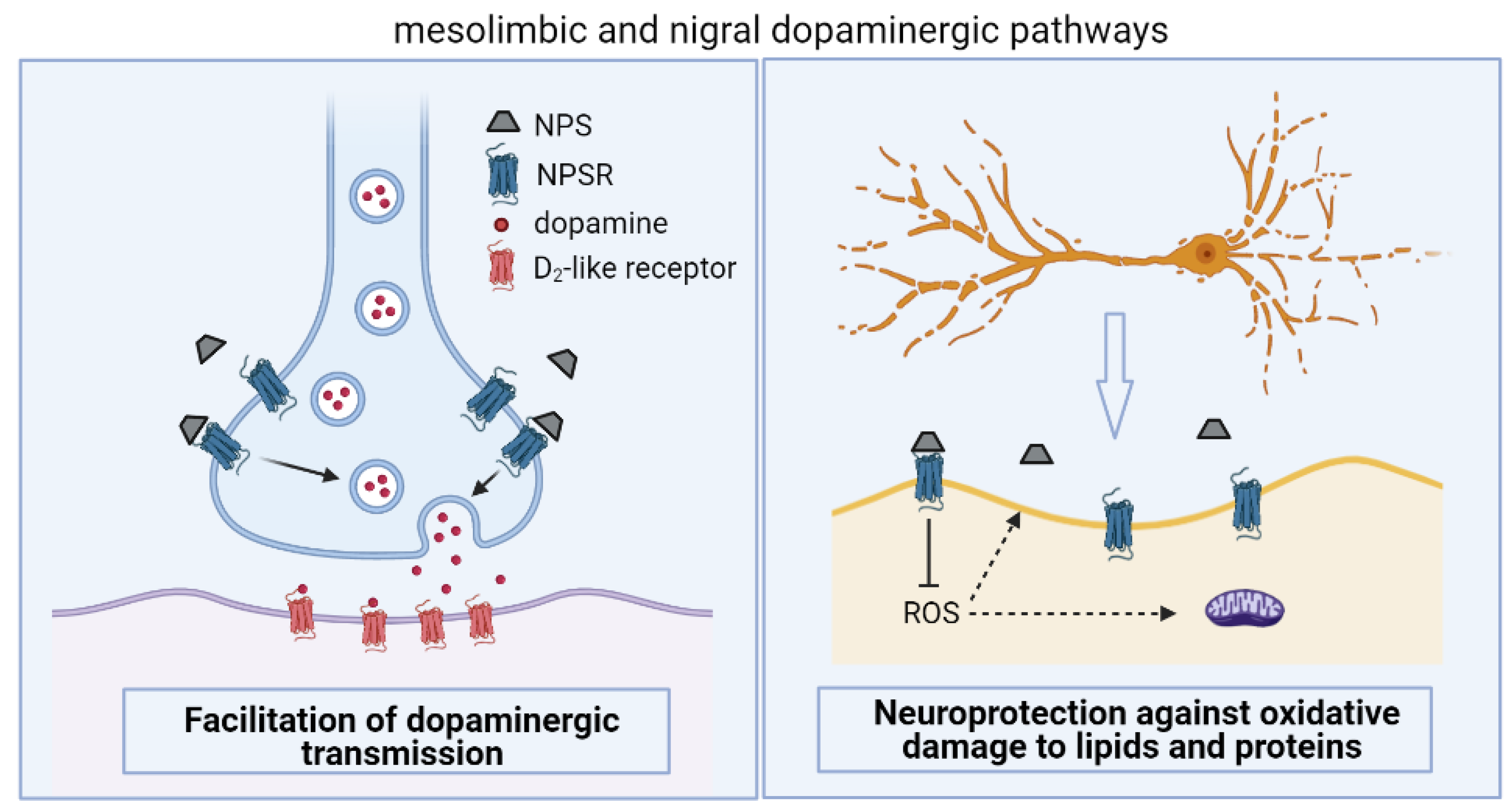
3. Behavioral Effects of Neuropeptide S: Implications for Parkinson Disease
4. Putative Mechanisms by Which Neuropeptide S Alleviates Parkinson Disease Signs and Symptoms
5. General Conclusions and Future Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sato, S.; Shintani, Y.; Miyajima, N.; Yoshimura, K. Novel G-Protein Coupled Receptor Protein and DNA Thereof. WIPO Patent WO2002034904, 26 June 2003. Available online: https://patents.google.com/patent/WO2003051923A2/en (accessed on 7 June 2021).
- Xu, Y.L.; Reinscheid, R.K.; Huitron-Resendiz, S.; Clark, S.D.; Wang, Z.; Lin, S.H.; Brucher, F.A.; Zeng, J.; Ly, N.K.; Henriksen, S.J.; et al. Neuropeptide S: A neuropeptide promoting arousal and anxiolytic-like effects. Neuron 2004, 43, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Reinscheid, R.K.; Xu, Y.L. Neuropeptide S and its receptor: A newly deorphanized G protein-coupled receptor system. Neuroscientist 2005, 11, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Okamura, N.; Habay, S.A.; Zeng, J.; Chamberlin, A.R.; Reinscheid, R.K. Synthesis and pharmacological in vitro and in vivo profile of 3-oxo-1,1-diphenyl-tetrahydro-oxazolo[3,4-a]pyrazine-7-carboxylic acid 4-fluoro-benzylamide (SHA 68), a selective antagonist of the neuropeptide S receptor. J. Pharmacol. Exp. Ther. 2008, 325, 893–901. [Google Scholar] [CrossRef]
- Ruzza, C.; Rizzi, A.; Trapella, C.; Pela’, M.; Camarda, V.; Ruggieri, V.; Filaferro, M.; Cifani, C.; Reinscheid, R.K.; Vitale, G.; et al. Further studies on the pharmacological profile of the neuropeptide S receptor antagonist SHA 68. Peptides 2010, 31, 915–925. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.L.; Gall, C.M.; Jackson, V.R.; Civelli, O.; Reinscheid, R.K. Distribution of neuropeptide S receptor mRNA and neurochemical characteristics of neuropeptide S-expressing neurons in the rat brain. J. Comp. Neurol. 2007, 500, 84–102. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.D.; Duangdao, D.M.; Schulz, S.; Zhang, L.; Liu, X.; Xu, Y.L.; Reinscheid, R.K. Anatomical characterization of the neuropeptide S system in the mouse brain by in situ hybridization and immunohistochemistry. J. Comp. Neurol. 2011, 519, 1867–1893. [Google Scholar] [CrossRef] [PubMed]
- Leonard, S.K.; Ring, R.H. Immunohistochemical localization of the neuropeptide S receptor in the rat central nervous system. Neuroscience 2011, 172, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Guerrini, R.; Salvadori, S.; Rizzi, A.; Regoli, D.; Calo’, G. Neurobiology, pharmacology, and medicinal chemistry of neuropeptide S and its receptor. Med. Res. Rev. 2010, 30, 751–777. [Google Scholar] [CrossRef]
- Ruzza, C.; Calò, G.; Di Maro, S.; Pacifico, S.; Trapella, C.; Salvadori, S.; Preti, D.; Guerrini, R. Neuropeptide S receptor ligands: A patent review (2005–2016). Expert Opin. Ther. Pat. 2017, 27, 347–362. [Google Scholar] [CrossRef]
- Bülbül, M.; Sinen, O.; Özkan, A.; Aslan, M.A.; Ağar, A. Central neuropeptide-S treatment improves neurofunctions of 6-OHDA-induced Parkinsonian rats. Exp. Neurol. 2019, 317, 78–86. [Google Scholar] [CrossRef] [PubMed]
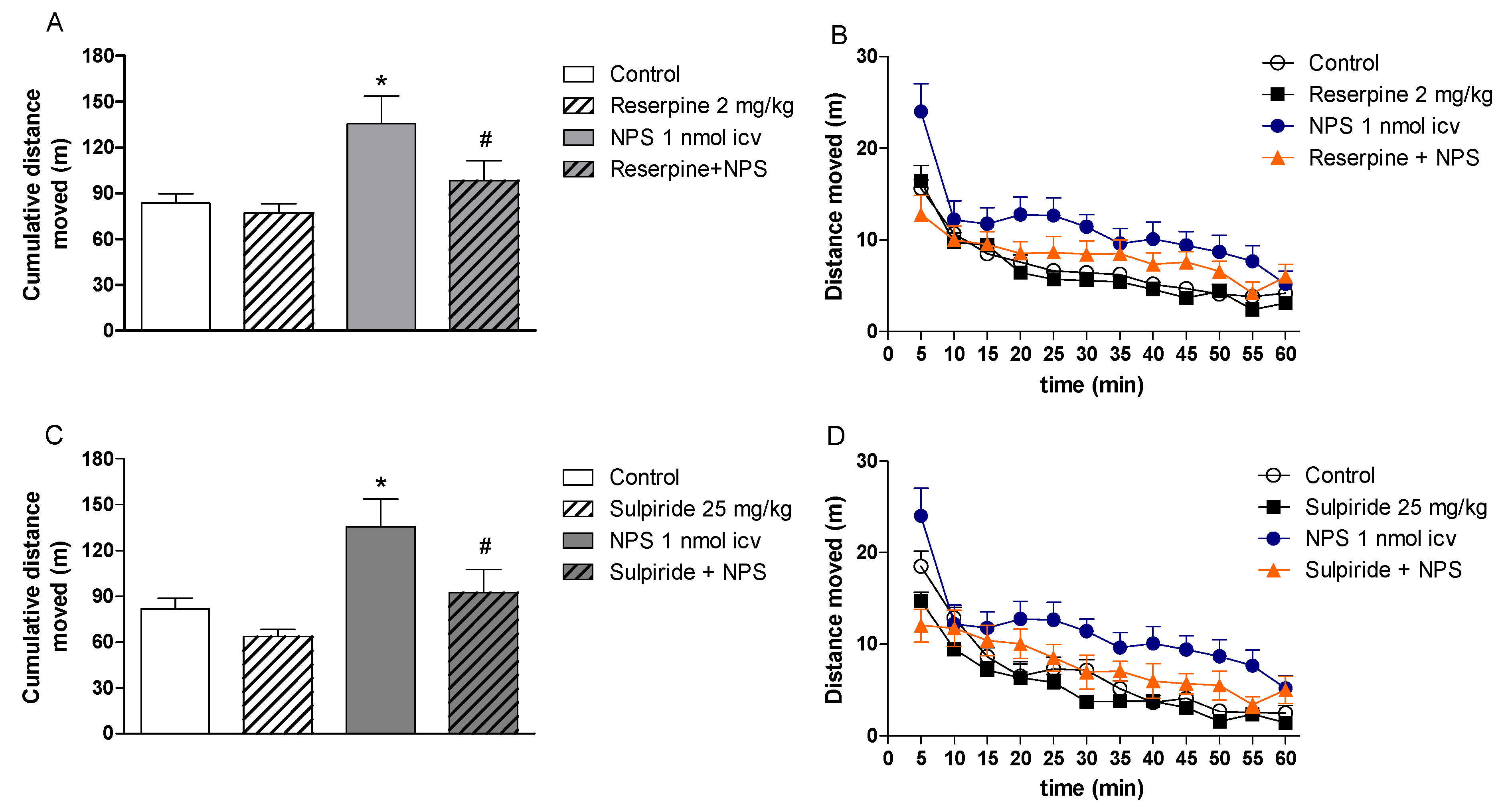
- Didonet, J.J.; Cavalcante, J.C.; Souza, L.S.; Costa, M.S.; André, E.; Soares-Rachetti, V.P.; Guerrini, R.; Calo’, G.; Gavioli, E.C. Neuropeptide S counteracts 6-OHDA-induced motor deficits in mice. Behav. Brain Res. 2014, 266, 29–36. [Google Scholar] [CrossRef]
- Sinen, O.; Bülbül, M.; Derin, N.; Ozkan, A.; Akcay, G.; Aslan, M.A.; Agar, A. The effect of chronic neuropeptide-S treatment on non-motor parameters in experimental model of Parkinson’s disease. Int. J. Neurosci. 2020, 22, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sinen, O.; Özkan, A.; Ağar, A.; Bülbül, M. Neuropeptide-S prevents 6-OHDA-induced gastric dysmotility in rats. Brain Res. 2021, 1762, 147442. [Google Scholar] [CrossRef] [PubMed]
- Li, M.S.; Peng, Y.L.; Jiang, J.H.; Xue, H.X.; Wang, P.; Zhang, P.J.; Han, R.W.; Chang, M.; Wang, R. Neuropeptide S Increases locomotion activity through corticotropin-releasing factor receptor 1 in substantia nigra of mice. Peptides 2015, 71, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Ruzza, C.; Rizzi, A.; Camarda, V.; Pulga, A.; Marzola, G.; Filaferro, M.; Novi, C.; Ruggieri, V.; Marzola, E.; Vitale, G.; et al. (tBu-D-Gly5)NPS, a pure and potent antagonist of the neuropeptide S receptor: In vitro and in vivo studies. Peptides 2012, 34, 404–411. [Google Scholar] [CrossRef]
- Camarda, V.; Ruzza, C.; Rizzi, A.; Trapella, C.; Guerrini, R.; Reinscheid, R.K.; Calo’, G. In vitro and in vivo pharmacological characterization of the novel neuropeptide S receptor ligands QA1 and PI1. Peptides 2013, 48, 27–35. [Google Scholar] [CrossRef]
- Castro, A.A.; Moretti, M.; Casagrande, T.S.; Martinello, C.; Petronilho, F.; Steckert, A.V.; Guerrini, R.; Calo’, G.; Dal Pizzol, F.; Quevedo, J.; et al. Neuropeptide S produces hyperlocomotion and prevents oxidative stress damage in the mouse brain: A comparative study with amphetamine and diazepam. Pharmacol. Biochem. Behav. 2009, 91, 636–642. [Google Scholar] [CrossRef] [PubMed]
- Roth, A.L.; Marzola, E.; Rizzi, A.; Arduin, M.; Trapella, C.; Corti, C.; Vergura, R.; Martinelli, P.; Salvadori, S.; Regoli, D.; et al. Structure-activity studies on neuropeptide S: Identification of the amino acid residues crucial for receptor activation. J. Biol. Chem. 2006, 281, 20809–20816. [Google Scholar] [CrossRef]
- Pacheco, R.; Pescador, B.B.; Mendonça, B.P.; Ramos, S.F.; Guerrini, R.; Calo’, G.; de Andrade, V.M.; Gavioli, E.C.; Boeck, C.R. Role of the ecto-nucleotidases in the cooperative effect of adenosine and neuropeptide-S on locomotor activity in mice. Pharmacol. Biochem. Behav. 2011, 99, 726–730. [Google Scholar] [CrossRef][Green Version]
- Castro, A.A.; Casagrande, T.S.; Moretti, M.; Constantino, L.; Petronilho, F.; Guerra, G.C.; Calo’, G.; Guerrini, R.; Dal-Pizzol, F.; Quevedo, J.; et al. Lithium attenuates behavioral and biochemical effects of neuropeptide S in mice. Peptides 2009, 30, 1914–1920. [Google Scholar] [CrossRef]
- Boeck, C.R.; Martinello, C.; de Castro, A.A.; Moretti, M.; Dos Santos Casagrande, T.; Guerrini, R.; Calo’, G.; Gavioli, E.C. Blockade of adenosine A2A receptor counteracts neuropeptide-S-induced hyperlocomotion in mice. Naunyn Schmiedebergs Arch. Pharmacol. 2010, 381, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Paneda, C.; Huitron-Resendiz, S.; Frago, L.M.; Chowen, J.A.; Picetti, R.; de Lecea, L.; Roberts, A.J. Neuropeptide S reinstates cocaine-seeking behavior and increases locomotor activity through corticotropin-releasing factor receptor 1 in mice. J. Neurosci. 2009, 29, 4155–4161. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lukas, M.; Neumann, I.D. Nasal application of neuropeptide S reduces anxiety and prolongs memory in rats: Social versus non-social effects. Neuropharmacology 2012, 62, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Zoicas, I.; Menon, R.; Neumann, I.D. Neuropeptide S reduces fear and avoidance of con-specifics induced by social fear conditioning and social defeat, respectively. Neuropharmacology 2016, 108, 284–291. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, A.; Vergura, R.; Marzola, G.; Ruzza, C.; Guerrini, R.; Salvadori, S.; Regoli, D.; Calo’, G. Neuropeptide S is a stimulatory anxiolytic agent: A behavioural study in mice. Br. J. Pharmacol. 2008, 154, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Mochizuki, T.; Kim, J.; Sasaki, K. Microinjection of neuropeptide S into the rat ventral tegmental area induces hyperactivity and increases extracellular levels of dopamine metabolites in the nucleus accumbens shell. Peptides 2010, 31, 926–931. [Google Scholar] [CrossRef] [PubMed]
- Duangdao, D.M.; Clark, S.D.; Okamura, N.; Reinscheid, R.K. Behavioral phenotyping of neuropeptide S receptor knockout mice. Behav. Brain Res. 2009, 205, 1–9. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Zhu, H.; Mingler, M.K.; McBride, M.L.; Murphy, A.J.; Valenzuela, D.M.; Yancopoulos, G.D.; Williams, M.T.; Vorhees, C.V.; Rothenberg, M.E. Abnormal response to stress and impaired NPS-induced hyperlocomotion, anxiolytic effect and corticosterone increase in mice lacking NPSR1. Psychoneuroendocrinology 2010, 35, 1119–1132. [Google Scholar] [CrossRef]
- Fendt, M.; Buchi, M.; Burki, H.; Imobersteg, S.; Ricoux, B.; Suply, T.; Sailer, A.W. Neuropeptide S receptor deficiency modulates spontaneous locomotor activity and the acoustic startle response. Behav. Brain Res. 2011, 217, 1–9. [Google Scholar] [CrossRef]
- Ruzza, C.; Pulga, A.; Rizzi, A.; Marzola, G.; Guerrini, R.; Calo’, G. Behavioural phenotypic characterization of CD-1 mice lacking the neuropeptide S receptor. Neuropharmacology 2012, 62, 1999–2009. [Google Scholar] [CrossRef]
- Liu, X.; Si, W.; Garau, C.; Jüngling, K.; Pape, H.C.; Schulz, S.; Reinscheid, R.K. Neuropeptide S precursor knockout mice display memory and arousal deficits. Eur. J. Neurosci. 2017, 46, 1689–1700. [Google Scholar] [CrossRef]
- Smith, K.L.; Patterson, M.; Dhillo, W.S.; Patel, S.R.; Semjonous, N.M.; Gardiner, J.V.; Ghatei, M.A.; Bloom, S.R. Neuropeptide S stimulates the hypothalamo-pituitary-adrenal axis and inhibits food intake. Endocrinology 2006, 147, 3510–3518. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; de Lecea, L.; Ikemoto, S. Intraventricular administration of neuropeptide S has reward-like effects. Eur. J. Pharmacol. 2011, 658, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Ensho, T.; Nakahara, K.; Suzuki, Y.; Murakami, N. Neuropeptide S increases motor activity and thermogenesis in the rat through sympathetic activation. Neuropeptides 2017, 65, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Grund, T.; Neumann, I.D. Neuropeptide S Induces Acute Anxiolysis by Phospholipase C-Dependent Signaling within the Medial Amygdala. Neuropsychopharmacology 2018, 43, 1156–1163. [Google Scholar] [CrossRef]
- Cline, M.A.; Godlove, D.C.; Nandar, W.; Bowden, C.N.; Prall, B.C. Anorexigenic effects of central neuropeptide S involve the hypothalamus in chicks (Gallus gallus). Comp. Biochem. Physiol. Part A Mol. Integr. Physiol. 2007, 148, 657–663. [Google Scholar] [CrossRef]
- Armstrong, M.J.; Okun, M.S. Diagnosis and Treatment of Parkinson Disease. JAMA 2020, 323, 548–560. [Google Scholar] [CrossRef]
- Postuma, R.B.; Poewe, W.; Litvan, I.; Lewis, S.; Lang, A.E.; Halliday, G.; Goetz, C.G.; Chan, P.; Slow, E.; Seppi, K.; et al. Validation of the MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2018, 33, 1601–1608. [Google Scholar] [CrossRef]
- Berg, D.; Postuma, R.B.; Adler, C.H.; Bloem, B.R.; Chan, P.; Dubois, B.; Gasser, T.; Goetz, C.G.; Halliday, G.; Joseph, L.; et al. MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 2015, 30, 1600–1611. [Google Scholar] [CrossRef]
- Schapira, A.H.V.; Chaudhuri, K.R.; Jenner, P. Non-motor features of Parkinson disease. Nat. Rev. Neurosci. 2017, 18, 435–450. [Google Scholar] [CrossRef]
- Dorsey, E.R.; Elbaz, A.; Nichols, E.; Abd-Allah, F.; Abdelalim, A.; Adsuar, J.C.; Ansha, M.G.; Brayne, C.; Choi, J.-Y.J. GBD 2016 Parkinson’s Disease Collaborators. Global, regional, and national burden of Parkinson’s disease, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018, 17, 939–953. [Google Scholar] [CrossRef]
- Haaxma, C.A.; Bloem, B.R.; Borm, G.T.; Oyen, W.J.; Leenders, K.L.; Eshuis, S.; Booij, J.; Dluzen, D.E.; Horstink, M.W. Gender differences in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2007, 78, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.E.; Obeso, J.A. Challenges in Parkinson’s disease: Restoration of the nigrostriatal dopamine system is not enough. Lancet Neurol. 2004, 3, 309–316. [Google Scholar] [CrossRef]
- De Virgilio, A.; Greco, A.; Fabbrini, G.; Inghilleri, M.; Rizzo, M.I.; Gallo, A.; Conte, M.; Rosato, C.; Ciniglio-Appiani, M.; de Vincentiis, M. Parkinson’s disease: Autoimmunity and neuroinflammation. Autoimmun. Rev. 2016, 15, 1005–1011. [Google Scholar] [CrossRef]
- Olanow, C.W.; Stern, M.B.; Sethi, K. The scientific and clinical basis for the treatment of Parkinson disease. Neurology 2009, 72, S1–S136. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Oroz, M.C.; Jahanshahi, M.; Krack, P.; Litvan, I.; Macias, R.; Bezard, E.; Obeso, J.A. Initial clinical manifestations of Parkinson’s disease: Features and pathophysiological mechanisms. Lancet Neurol. 2009, 8, 1128–1139. [Google Scholar] [CrossRef]
- Kistner, A.; Lhommee, E.; Krack, P. Mechanisms of body weight fluctuations in Parkinson’s disease. Front. Neurol. 2014, 5, 1–16. [Google Scholar] [CrossRef]
- Obeso, J.A.; Rodriguez-Oroz, M.C.; Stamelou, M.; Bhatia, K.P.; Burn, D.J. The expanding universe of disorders of the basal ganglia. Lancet 2014, 384, 523–531. [Google Scholar] [CrossRef]
- McDonald, C.; Gordon, G.; Hand, A.; Walker, R.W.; Fisher, J.M. 200 years of Parkinson’s disease: What have we learnt from James Parkinson? Age Ageing 2018, 47, 209–214. [Google Scholar] [CrossRef]
- Millan, M.J. From the cell to the clinic: A comparative review of the partial D2/D3receptor agonist and a2-adrenoceptor antagonist, piribedil, in the treatment of Parkinson’s disease. Pharmacol. Ther. 2010, 128, 229–273. [Google Scholar] [CrossRef]
- Fahn, S. The medical treatment of Parkinson disease from James Parkinson to George Cotzias. Mov. Disord. 2015, 30, 4–18. [Google Scholar] [CrossRef]
- Connolly, B.S.; Lang, A.E. Pharmacological treatment of Parkinson disease: A review. JAMA J. Am. Med. Assoc. 2014, 311, 1670–1683. [Google Scholar] [CrossRef] [PubMed]
- Antonini, A.; Tolosa, E.; Mizuno, Y.; Yamamoto, M.; Poewe, W.H. A reassessment of risks and benefits of dopamine agonists in Parkinson’s disease. Lancet Neurol. 2009, 8, 929–937. [Google Scholar] [CrossRef]
- Turcano, P.; Mielke, M.M.; Bower, J.H.; Parisi, J.E.; Cutsforth-Gregory, J.K.; Ahlskog, J.E.; Savica, R. Levodopa-induced dyskinesia in Parkinson disease: A population-based cohort study. Neurology 2018, 91, e2238–e2243. [Google Scholar] [CrossRef] [PubMed]
- Gray, R.; Ives, N.; Rick, C.; Patel, S.; Gray, A.; Jenkinson, C.; McIntosh, E.; Wheatley, K.; Williams, A.; Clarke, C.E. Long-term effectiveness of dopamine agonists and monoamine oxidase B inhibitors compared with levodopa as initial treatment for Parkinson’s disease (PD MED): A large, open-label, pragmatic randomised trial. Lancet 2014, 384, 1196–1205. [Google Scholar] [CrossRef]
- Garcia-Ruiz, P.J.; Martinez-Castrillo, J.C.; Alonso-Canovas, A.; Barcenas, A.H.; Vela, L.; Sanchez, A.P.; Mata, M.; Olmedilla, G.N.; Mahillo, F.I. Impulse control disorder in patients with Parkinson’s disease under dopamine agonist therapy: A multicentre study. J. Neurol. Neurosurg. Psychiatry 2014, 85, 840–844. [Google Scholar] [CrossRef]
- Pondal, M.; Marras, C.; Miyasaki, J.; Moro, E.; Armstrong, M.J.; Strafella, A.P.; Shah, B.B.; Fox, S.; Prashanth, L.K.; Phielipp, N.; et al. Clinical features of dopamine agonist withdrawal syndrome in a movement disorders clinic. J. Neurol. Neurosurg. Psychiatry 2013, 84, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Espay, A.J.; Lang, A.E. Common myths in the use of levodopa in Parkinson disease: When clinical trials misinform clinical practice. JAMA Neurol. 2017, 74, 633–634. [Google Scholar] [CrossRef]
- Kushikata, T.; Yoshida, H.; Kudo, M.; Salvadori, S.; Calo’, G.; Hirota, K. The effects of neuropeptide S on general anesthesia in rats. Anesth. Analg. 2011, 112, 845–849. [Google Scholar] [CrossRef]
- Han, R.W.; Yin, X.Q.; Chang, M.; Peng, Y.L.; Li, W.; Wang, R. Neuropeptide S facilitates spatial memory and mitigates spatial memory impairment induced by N-methyl-D-aspartate receptor antagonist in mice. Neurosci. Lett. 2009, 455, 74–77. [Google Scholar] [CrossRef]
- Zhao, Z.; Huang, L.; Wu, H.; Li, Y.; Zhang, L.; Yin, Y.; Xiang, Z.; Zhao, Z. Neuropeptide S mitigates spatial memory impairment induced by rapid eye movement sleep deprivation in rats. Neuroreport 2010, 21, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Han, R.W.; Zhang, R.S.; Xu, H.J.; Chang, M.; Peng, Y.L.; Wang, R. Neuropeptide S enhances memory and mitigates memory impairment induced by MK801, scopolamine or Aβ1-42 in mice novel object and object location recognition tasks. Neuropharmacology 2013, 70, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Shao, Y.F.; Wang, C.; Xie, J.F.; Kong, X.P.; Xin, L.; Dong, C.Y.; Li, J.; Ren, W.T.; Hou, Y.P. Neuropeptide S ameliorates olfactory spatial memory impairment induced by scopolamine and MK801 through activation of cognate receptorexpressing neurons in the subiculum complex. Brain Struct. Funct. 2016, 221, 3327–3336. [Google Scholar] [CrossRef] [PubMed]
- Pape, H.C.; Jüngling, K.; Seidenbecher, T.; Lesting, J.; Reinscheid, R.K. Neuropeptide S: A transmitter system in the brain regulating fear and anxiety. Neuropharmacology 2010, 58, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Shirayama, Y.; Ishima, T.; Oda, Y.; Okamura, N.; Iyo, M.; Hashimoto, K. Opposite roles for neuropeptide S in the nucleus accumbens and bed nucleus of the stria terminalis in learned helplessness rats. Behav. Brain Res. 2015, 291, 67–71. [Google Scholar] [CrossRef]
- Leonard, S.K.; Dwyer, J.M.; Sukoff-Rizzo, S.J.; Platt, B.; Logue, S.F.; Neal, S.J.; Malberg, J.E.; Beyer, C.E.; Schechter, L.E.; Rosenzweig-Lipson, S.; et al. Pharmacology of neuropeptide S in mice: Therapeutic relevance to anxiety disorders. Psychopharmacology 2008, 197, 601–611. [Google Scholar] [CrossRef]
- Guerrini, R.; Camarda, V.; Trapella, C.; Calò, G.; Rizzi, A.; Ruzza, C.; Fiorini, S.; Marzola, E.; Reinscheid, R.K.; Regoli, D.; et al. Synthesis and biological activity of human neuropeptide S analogues modified in position 5: Identification of potent and pure neuropeptide S receptor antagonists. J. Med. Chem. 2009, 52, 524–529. [Google Scholar] [CrossRef]
- Hassler, C.; Zhang, Y.; Gilmour, B.; Graf, T.; Fennell, T.; Snyder, R.; Deschamps, J.R.; Reinscheid, R.K.; Garau, C.; Runyon, S.P. Identification of neuropeptide S antagonists: Structure-activity relationship studies, X-ray crystallography, and in vivo evaluation. ACS Chem. Neurosci. 2014, 5, 731–744. [Google Scholar] [CrossRef]
- Visser, J.E.; Bloem, B.R. Role of the basal ganglia in balance control. Neural Plast. 2005, 12, 161–272. [Google Scholar] [CrossRef]
- Ionescu, I.A.; Dine, J.; Yen, Y.C.; Buell, D.R.; Herrmann, L.; Holsboer, F.; Eder, M.; Landgraf, R.; Schmidt, U. Intranasally administered neuropeptide S (NPS) exerts anxiolytic effects following internalization into NPS receptor-expressing neurons. Neuropsychopharmacology 2012, 37, 1323–1337. [Google Scholar] [CrossRef][Green Version]
- Lochhead, J.J.; Thorne, R.G. Intranasal delivery of biologics to the central nervous system. Adv. Drug Deliv. Rev. 2012, 64, 614–628. [Google Scholar] [CrossRef]
- Si, W.; Aluisio, L.; Okamura, N.; Clark, S.D.; Fraser, I.; Sutton, S.W.; Bonaventure, P.; Reinscheid, R.K. Neuropeptide S stimulates dopaminergic neurotransmission in the medial prefrontal cortex. J. Neurochem. 2010, 115, 475–482. [Google Scholar] [CrossRef]
- Ramos, S.F.; Mendonca, B.P.; Leffa, D.D.; Pacheco, R.; Damiani, A.P.; Hainzenreder, G.; Petronilho, F.; Dal-Pizzol, F.; Guerrini, R.; Calo’, G.; et al. Effects of neuropeptide S on seizures and oxidative damage induced by pentylenetetrazole in mice. Pharmacol. Biochem. Behav. 2012, 103, 197–203. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Samuel, F.; Flavin, W.P.; Iqbal, S.; Pacelli, C.; Sri Renganathan, S.D.; Trudeau, L.E.; Campbell, E.M.; Fraser, P.E.; Tandon, A. Effects of Serine 129 Phosphorylation on α-Synuclein Aggregation, Membrane Association, and Internalization. J. Biol. Chem. 2016, 291, 4374–4385. [Google Scholar] [CrossRef]
- Sato, H.; Arawaka, S.; Hara, S.; Fukushima, S.; Koga, K.; Koyama, S.; Kato, T. Authentically phosphorylated α-synuclein at Ser129 accelerates neurodegeneration in a rat model of familial Parkinson’s disease. J. Neurosci. 2011, 31, 16884–16894. [Google Scholar] [CrossRef] [PubMed]
- Puspita, L.; Chung, S.Y.; Shim, J.W. Oxidative stress and cellular pathologies in Parkinson’s disease. Mol. Brain 2017, 10, 53. [Google Scholar] [CrossRef] [PubMed]
- Morelli, M.; Carta, A.R.; Jenner, P. Adenosine A2A receptors and Parkinson’s disease. Handb. Exp. Pharmacol. 2009, 193, 589–615. [Google Scholar] [CrossRef]
- Ren, X.; Chen, J.F. Caffeine and Parkinson’s Disease: Multiple Benefits and Emerging Mechanisms. Front. Neurosci. 2020, 14, 602697. [Google Scholar] [CrossRef]
- Beck, B.; Fernette, B.; Stricker-Krongrad, A. Peptide S is a novel potent inhibitor of voluntary and fast-induced food intake in rats. Biochem. Biophys. Res. Commun. 2005, 332, 859–865. [Google Scholar] [CrossRef]
- Cline, M.A.; Prall, B.C.; Smith, M.L.; Calchary, W.A.; Siegel, P.B. Differential appetite-related responses to central neuropeptide S in lines of chickens divergently selected for low or high body weight. J. Neuroendocr. 2008, 20, 904–908. [Google Scholar] [CrossRef]
- Holanda, V.A.D.; Asth, L.; Santos, A.R.; Guerrini, R.; Soares-Rachetti, V.d.P.; Calo’, G.; André, E.; Gavioli, E.C. Central adenosine A1 and A2A receptors mediate the antinociceptive effects of neuropeptide S in the mouse formalin test. Life Sci. 2015, 120, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Lage, R.; Diéguez, C.; López, M. Caffeine treatment regulates neuropeptide S system expression in the rat brain. Neurosci. Lett. 2006, 410, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Domschke, K.; Klauke, B.; Winter, B.; Gajewska, A.; Herrmann, M.J.; Warrings, B.; Mühlberger, A.; Wosnitza, K.; Dlugos, A.; Naunin, S.; et al. Modification of caffeine effects on the affect-modulated startle by neuropeptide S receptor gene variation. Psychopharmacology 2012, 222, 533–541. [Google Scholar] [CrossRef] [PubMed]
| Animal Specie (Condition) | Active Doses and Route of Administration | Experimental Assay | Behavioral Effects | References |
|---|---|---|---|---|
| mouse (naïve) | 0.1–1 nmol (icv) | open field test | ↑ total distance moved; ↑ number of rearings | [2,4,5,15,16,17] |
| ↑ total distance moved | [7,18,19,20,21,22] | |||
| 0.45 nM, 2 µL (icv) | ↑ ambulatory activity | [23] | ||
| 7, 14, and 28 nmol (intranasal) | no effects on distance moved | [24] | ||
| 1, 10 and 50 nmol (icv) | home cage locomotion | no effects on spentaneous locomotion | [25] | |
| 0.1–1 nmol (icv) | activity cage | ↑ number of pulses in naïve and habituated mouse | [26] | |
| 0.05–0.5 nmol (intra-VTA) | ↑ total distance moved; ↑ number of rearings | [27] | ||
| mouse (diazepam-treated) | 0.1–1 nmol (icv) | activity cage | ↑ number of pulses | [26] |
| NPSR (−/−) mouse | 0.1 nmol (icv) | open field test | no effects on locomotion | [28] |
| - | no differences compared to wild type mice | [28,29,30,31] | ||
| - | ↓ distance moved in the dark phase | [30] | ||
| NPS (−/−) and NPS (+/−) precursor mouse | - | open field test | ↓ cumulative distance moved | [32] |
| rat (naïve) | 0.1–10 nmol (icv) | open field test | ↑ horizontal activity; ↑ rearing activity | [33,34,35] |
| 0.2 nmol (into MeA) | ↑ total distance moved | [36] | ||
| chicken | 0.625 μg (icv) | open field test | ↑ total distance moved | [37] |
| Animal Model of PD | Specie (Strain, Weight, Sex) | NPS Treatment (Dose, Route, etc) | Effects of NPS | References |
|---|---|---|---|---|
| 6-OHDA, icv, 50 µg/2 µL | mouse (Swiss, 28–35 g, female) | 0.1 and 1 nmol (icv), 15 min before behavioral test | Acute NPS reversed 6-OHDA-induced motor incoordination | [12] |
| 6-OHDA, into right MFB, 12 µg/3 µL | rat (Wistar, 250–300 g, male) | 1 nmol (icv), 7 consecutive days after 6-OHDA 10 nmol (icv), acutely, on 7th day after 6-OHDA | Acute NPS reversed 6-OHDA-induced motor incoordination, locomotor deficits and catalepsy; Repeated NPS reversed 6-OHDA-induced hypolocomotion and motor incoordination; Acute and repeated NPS restored 6-OHDA-induced dopamine concentrations deficits in nigral microdialysates; Repeated NPS partially attenuated 6-OHDA-induced degeneration on nigral TH immunoreactive cells; Repeated NPS attenuated 6-OHDA-induced nigral 4-HNE immunoreactivity | [11] |
| 6-OHDA, into right MFB, 12 µg/3 µL | rat (Wistar, 250–300 g, male) | 1 nmol (icv), 7 consecutive days after 6-OHDA | Repeated NPS restored 6-OHDA-induced reference and working memory deficits in the radial maze task; Repeated NPS restored 6-OHDA-induced anhedonic behavior in the sucrose preference test; Repeated NPS reduced 6-OHDA-induced dopamine deficits in the hippocampus, but not in the striatum; Repeated NPS partially attenuated 6-OHDA-induced degeneration on nigral TH immunoreactive cells | [13] |
| 6-OHDA, into right MFB, 12 µg/3 µL | rat (Wistar, 250–300 g, male) | 1 nmol (icv), 7 consecutive days after 6-OHDA | Repeated NPS reversed 6-OHDA-induced locomotor deficits in an unfamiliar environment; Repeated NPS partially attenuated 6-OHDA-induced degeneration on nigral TH immunoreactive cells; Repeated NPS reversed 6-OHDA-induced changes in gastric empty; Repeated NPS prevented 6-OHDA-induced expression of phosphorylated α-synuclein in substantia nigra, dorsal motor nucleus of the vagus and hypoglossal nucleus; Repeated NPS attenuated 6-OHDA-induced degeneration of the cholinergic neurons of the dorsal motor nucleus of the vagus | [14] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holanda, V.A.D.; Didonet, J.J.; Costa, M.B.B.; do Nascimento Rangel, A.H.; da Silva, E.D., Jr.; Gavioli, E.C. Neuropeptide S Receptor as an Innovative Therapeutic Target for Parkinson Disease. Pharmaceuticals 2021, 14, 775. https://doi.org/10.3390/ph14080775
Holanda VAD, Didonet JJ, Costa MBB, do Nascimento Rangel AH, da Silva ED Jr., Gavioli EC. Neuropeptide S Receptor as an Innovative Therapeutic Target for Parkinson Disease. Pharmaceuticals. 2021; 14(8):775. https://doi.org/10.3390/ph14080775
Chicago/Turabian StyleHolanda, Victor A. D., Julia J. Didonet, Manara B. B. Costa, Adriano H. do Nascimento Rangel, Edilson D. da Silva, Jr., and Elaine C. Gavioli. 2021. "Neuropeptide S Receptor as an Innovative Therapeutic Target for Parkinson Disease" Pharmaceuticals 14, no. 8: 775. https://doi.org/10.3390/ph14080775
APA StyleHolanda, V. A. D., Didonet, J. J., Costa, M. B. B., do Nascimento Rangel, A. H., da Silva, E. D., Jr., & Gavioli, E. C. (2021). Neuropeptide S Receptor as an Innovative Therapeutic Target for Parkinson Disease. Pharmaceuticals, 14(8), 775. https://doi.org/10.3390/ph14080775







