Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study
Abstract
1. Introduction
2. Results
3. Discussion
4. Materials and Methods
4.1. Study Design and Participants
4.2. Description of the Initial Cohort
4.3. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Novel Coronavirus (2019-nCoV). Situation Report. Available online: https://www.who.int/fr/news/item/27-04-2020-who-timeline---covid-19). (accessed on 15 December 2020).
- Young, B.; Tong, T.T.; Sin, L.Y. The place for remdesivir in COVID-19 treatment. Lancet Infect. Dis. 2021, 21, 20–21. [Google Scholar] [CrossRef]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E. Remdesivir for the treatment of covid-19—Preliminary report. N. Engl. J. Med. 2020, 383, 992–993. [Google Scholar] [CrossRef]
- Quek, E.; Tahir, H. COVID-19 vaccines: What happened to evidence-based medicine? Br. J. Hosp. Med. 2021, 82, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Mercer, J.; Schelhaas, M.; Helenius, A. Virus entry by endocytosis. Annu. Rev. Biochem. 2010, 79, 803–833. [Google Scholar] [CrossRef] [PubMed]
- Stadler, K.; Ha, H.R.; Ciminale, V.; Spirli, C.; Saletti, G.; Schiavon, M.; Bruttomesso, D.; Bigler, L.; Follath, F.; Pettenazzo, A.; et al. Amiodarone alters late endosomes and inhibits SARS coronavirus infection at a post-endosomal level. Am. J. Respir Cell Mol. Biol. 2008, 39, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Pastenkos, G.; Miller, J.L.; Pritchard, S.M.; Nicola, A.V. Role of Sphingomyelin in Alphaherpesvirus Entry. J. Virol. 2019, 93, e01547-18. [Google Scholar] [CrossRef] [PubMed]
- Johansen, L.M.; DeWald, L.E.; Shoemaker, C.J.; Hoffstrom, B.G.; Lear-Rooney, C.M.; Stossel, A.; Nelson, E.; Delos, S.E.; Simmons, J.A.; Grenier, J.M.; et al. A screen of approved drugs and molecular probes identifies therapeutics with anti-Ebola virus activity. Sci. Transl. Med. 2015, 7, 290ra89. [Google Scholar] [CrossRef]
- Du, X.; Zuo, X.; Meng, F.; Wu, F.; Zhao, X.; Li, C.; Cheng, G.; Qin, F.X.F. Combinatorial screening of a panel of FDA-approved drugs identifies several candidates with anti-Ebola activities. Biochem. Biophys. Res. Commun. 2020, 522, 862–868. [Google Scholar] [CrossRef]
- Xia, B.T.; Beckmann, N.; Winer, L.K.; Pugh, A.M.; Pritts, T.A.; Nomellini, V.; Gulbins, E.; Caldwell, C.C. Amitriptyline Reduces Inflammation and Mortality in a Murine Model of Sepsis. Cell Physiol. Biochem. 2019, 52, 565–579. [Google Scholar] [CrossRef]
- Xia, B.T.; Beckmann, N.; Winer, L.K.; Kim, Y.; Goetzman, H.S.; Veile, R.E.; Gulbins, E.; Goodman, M.D.; Nomellini, V.; Caldwell, C.C. Amitriptyline Treatment Mitigates Sepsis-Induced Tumor Necrosis Factor Expression and Coagulopathy. Shock 2019, 51, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Peng, X.; Ai, Y.; Li, L.; Zhao, S.; Liu, Z.; Peng, Q.; Deng, S.; Huang, Y.; Mo, Y.; et al. Amitriptyline Reduces Sepsis-Induced Brain Damage Through TrkA Signaling Pathway. J. Mol. Neurosci. 2020, 70, 2049–2057. [Google Scholar] [CrossRef]
- Kornhuber, J.; Philipp, T.P.; Gulbins, E.; Muehlbacher, M. Functional Inhibitors of Acid Sphingomyelinase (FIASMAs). Handb. Exp. Pharmacol. 2013, 215, 169–186. [Google Scholar] [CrossRef]
- Borbone, N.; Piccialli, G.; Roviello, G.N.; Oliviero, G. Nucleoside Analogs and Nucleoside Precursors as Drugs in the Fight against SARS-CoV-2 and Other Coronaviruses. Molecules 2021, 26, 986. [Google Scholar] [CrossRef]
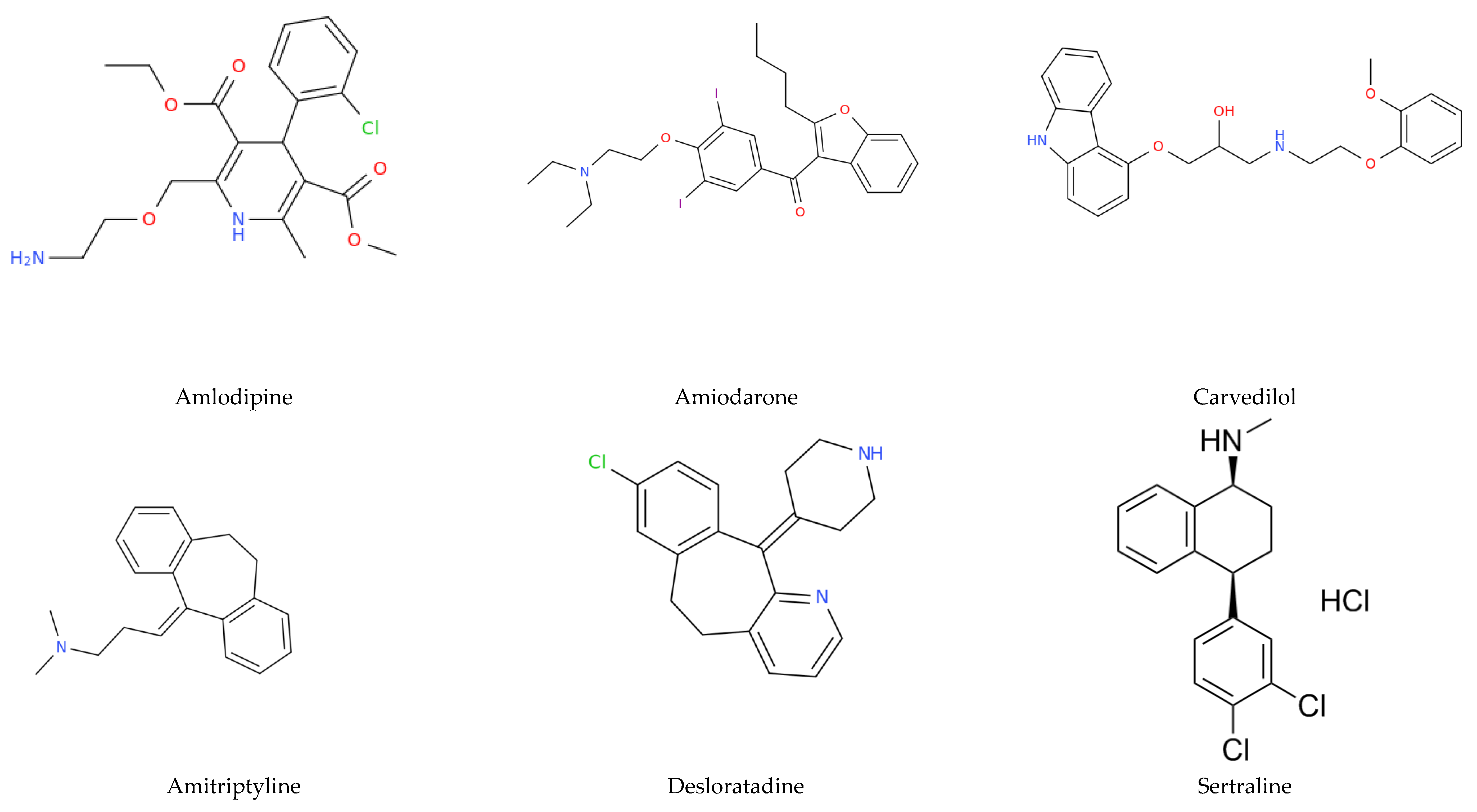
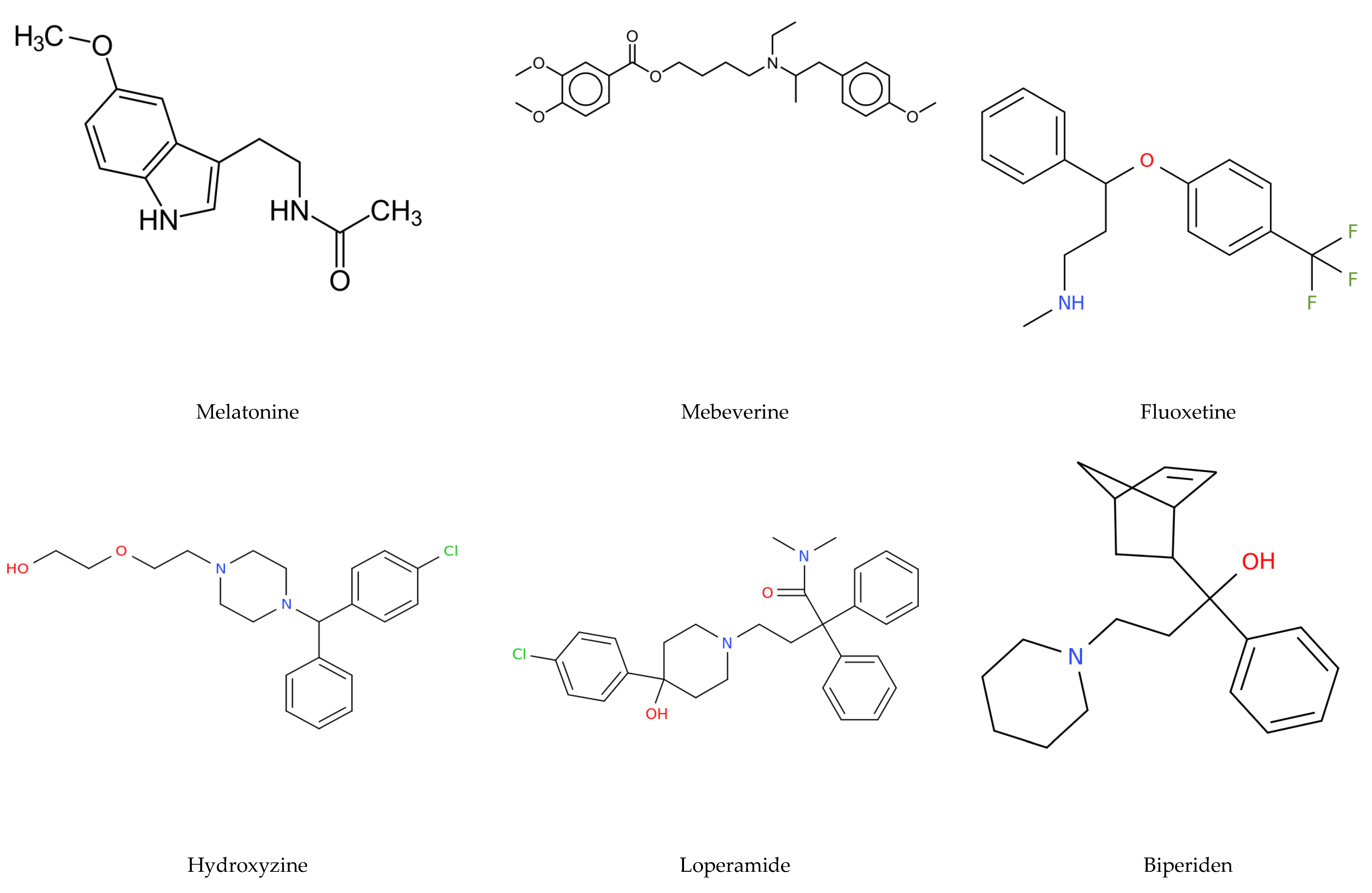
- Le Corre, P.; Loas, G. Repurposing functional inhibitors of acid sphingomyelinase (FIASMAs): An opportunity against SARS-CoV-2 infection. J. Clin. Pharm. Ther. 2021, 00, 1–7. [Google Scholar]
- Carpinteiro, A.; Edwards, M.J.; Hoffmann, M.; Kochs, G.; Gripp, B.; Weigang, S.; Adams, C.; Carpinteiro, E.; Gulbins, A.; Keitsch, S.; et al. Pharmacological Inhibition of Acid Sphingomyelinase Prevents Uptake of SARS-CoV-2 by Epithelial Cells. Cell Rep. Med. 2020, 1, 100142. [Google Scholar] [CrossRef]
- Carpinteiro, A.; Edwards, M.J.; Hoffmann, M.; Kochs, G.; Gripp, B.; Weigang, S.; Adams, C.; Carpinteiro, E.; Gulbins, A.; Keitsch, S.; et al. Inhibition of Acid Sphingomyelinase Blocks Infection with SARS-CoV-2. Available online: http://dx.doi.org/10.2139/ssrn.3646562 (accessed on 15 December 2020).
- Schloer, S.; Brunotte, L.; Goretzko, J.; Mecate-Zambrano, A.; Korthals, N.; Gerke, V.; Ludwig, S.; Rescher, U. Targeting the endolysosomal host-SARS-CoV-2 interface by clinically licensed functional inhibitors of acid sphingomyelinase (FIASMA) including the antidepressant fluoxetine. Emerg. Microbes Infect. 2020, 9, 2245–2255. [Google Scholar] [CrossRef]
- Solaimanzadeh, I. Nifedipine and Amlodipine Are Associated With Improved Mortality and Decreased Risk for Intubation and Mechanical Ventilation in Elderly Patients Hospitalized for COVID-19. Cureus 2020, 12, e8069. [Google Scholar] [CrossRef]
- Zhang, L.K.; Sun, Y.; Zeng, H.; Wang, Q.; Jiang, X.; Shang, W.-J.; Wu, Y.; Li, S.; Zhang, Y.-L.; Hao, Z.-N.; et al. Calcium channel blocker amlodipine besylate therapy is associated with reduced case fatality rate of COVID-19 patients with hypertension. Cell Discov. 2020, 6, 96. [Google Scholar] [CrossRef]
- Hoertel, N.; Sánchez-Rico, M.; Vernet, R.; Beeker, N.; Jannot, A.-S.; Neuraz, A.; Salamanca, E.; Paris, N.; Daniel, C.; Gramfort, A.; et al. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: Results from an observational study. Mol. Psychiatry 2021. [Google Scholar] [CrossRef]
- Lenze, E.J.; Mattar, C.; Zorumski, C.F.; Stevens, A.; Schweiger, J.; Nicol, G.E.; Miller, J.P.; Yang, L.; Yingling, M.; Avidan, M.S.; et al. Fluvoxamine vs Placebo and Clinical Deterioration in Outpatients with Symptomatic COVID-19: A Randomized Clinical Trial. JAMA 2020, 324, 2292–2300. [Google Scholar] [CrossRef] [PubMed]
- Hoertel, N.; Sánchez-Rico, M.; Vernet, R.; Jannot, A.S.; Neuraz, A.; Blanco, C.; Lemogne, C.; Airagnes, G.; Paris, N.; Daniel, C.; et al. Observational Study of Chlorpromazine in Hospitalized Patients with COVID-19. Clin. Drug Investig. 2021, 1–13. [Google Scholar]
- Xiao, X.; Wang, C.; Chang, D.; Wang, Y.; Dong, X.; Jiao, T.; Zhao, Z.; Ren, L.; Dela Cruz, C.S.; Sharma, L.; et al. Identification of Potent and Safe Antiviral Therapeutic Candidates Against SARS-CoV-2. Front. Immunol. 2020, 11, 586572. [Google Scholar] [CrossRef] [PubMed]
- Jayaseelan, V.P.; Paramasivam, A. Repurposing calcium channel blockers as antiviral drugs. J. Cell Commun. Signal. 2020, 14, 467–468. [Google Scholar] [CrossRef] [PubMed]
- Hernández, R.; Carvajal, A.R.; Armas-de Hernández, M.J.; Guerrero-Pajuelo, J.; Armas-Padilla, M.C.; Barragán, O.; Machado-de Alvarado, I. The effects of the calcium antagonist amlodipine on blood pressure and platelet aggregation in hypertensive patients. Postgrad. Med. J. 1991, 67, S38–S40. [Google Scholar] [PubMed]
- Statistica Software; Version 7.1; Statsoft: Tulsa, OK, USA, 2005.
| Demographic/Clinical Characteristics. | n (%) |
|---|---|
| Age | 63.24 +/− 17.4 * |
| Sex | |
| Female | 145 (41.4) |
| Male | 205 (58.6) |
| Comorbidities | |
| Hypertension | 184 (52.6) |
| Diabetes | 95 (27.1) |
| Chronic lung diseases | 66 (18.9) |
| Chronic liver diseases | 39 (10.3) |
| Chronic cardiac diseases | 110 (31.4) |
| Chronic rheumatic disease | 54 (15.4) |
| Chronic kidney disease | 79 (22.6) |
| Malignant neoplasm | 51 (14.6) |
| Chronic neurologic disorders | 74 (21.1) |
| Dementia | 28 (8) |
| Chronic hematologic disease | 42 (12) |
| Asthma | 28 (8) |
| Obesity | 96 (27.8) |
| Smoking | 39 (11.1) |
| Mortality | 72 (20.6) |
| FIASMAs | 93 (26.6) |
| Amlodipine | 60 (17.1) |
| n = 350, FIASMAs as Forced Predictor | n = 317, AMLODIPINE as Forced Predictor | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Univariate Analysis | Multivariable Analysis | Univariate Analysis | Multivariable Analysis | ||||||||
| OR | 95% CI | p-Value | aOR | 95% CI | p-Value | OR | 95% CI | p-Value | aOR | 95% CI | p-Value | |
| Age | 1.06 | 1.04–1.08 | <10−4 | 1.05 | 1.02–1.07 | 0.00015 | 1.06 | 1.03–1.08 | <10−4 | 1.04 | 1.02–1.07 | 0.0009 |
| Female sex (vs. male) | 0.75 | 0.43–1.32 | 0.32 | 0.83 | 0.46–1.49 | 0.53 | ||||||
| Comorbidities | ||||||||||||
| Hypertension | 2.88 | 1.63–5.08 | 0.0003 | 1.95 | 0.99–3.82 | 0.052 | 2.93 | 1.59–5.43 | 0.0006 | 2.78 | 1.33–5.79 | 0.0062 |
| Diabetes | 1.58 | 0.9–2.76 | 0.11 | 1.62 | 0.89–2.97 | 0.11 | ||||||
| Chronic lung diseases | 1.6 | 0.86–2.97 | 0.14 | 1.51 | 0.76–3 | 0.23 | ||||||
| Chronic liver diseases | 0.92 | 0.39–2.21 | 0.86 | 0.99 | 0.38–2.53 | 0.98 | ||||||
| Chronic cardiac diseases | 2.97 | 1.74–5.07 | <10−4 | 1.31 | 0.7–2.46 | 0.39 | 2.2 | 1.22–3.96 | 0.0085 | 0.86 | 0.42–1.74 | 0.66 |
| Chronic rheumatic disease | 1.27 | 0.64–2.54 | 0.49 | 1.53 | 0.74–3.17 | 0.25 | ||||||
| Chronic kidney disease | 2.61 | 1.48–4.59 | 0.0009 | 1.48 | 0.78–2.8 | 0.23 | 2.34 | 1.26–4.35 | 0.007 | 1.28 | 0.61–2.68 | 0.51 |
| Malignant neoplasm | 3.06 | 1.62–5.8 | 0.0006 | 2.09 | 1.03–4.22 | 0.039 | 3.81 | 1.91–7.57 | 0.0001 | 2.71 | 1.23–5.97 | 0.013 |
| Chronic neurologic disorders | 2.49 | 1.4–4.43 | 0.0019 | 1.26 | 0.65–2.45 | 0.49 | 2.24 | 1.2–4.24 | 0.012 | 1.05 | 0.5–2.22 | 0.89 |
| Dementia | 3.27 | 1.47–7.3 | 0.0036 | 1.14 | 0.46–2.82 | 0.77 | 3.31 | 1.34–8.19 | 0.009 | 0.98 | 0.34–2.84 | 0.98 |
| Chronic hematologic disease | 1.65 | 0.8–3.43 | 0.17 | 2.22 | 1.04–4.72 | 0.038 | 1.15 | 0.47–2.83 | 0.76 | |||
| Asthma | 0.28 | 0.06–1.2 | 0.09 | 0.37 | 0.08–1.62 | 0.18 | ||||||
| Obesity | 0.67 | 0.36–1.26 | 0.21 | 0.91 | 0.48–1.75 | 0.78 | ||||||
| Smoking | 0.67 | 0.27–1.68 | 0.4 | 0.69 | 0.25–1.86 | 0.46 | ||||||
| FIASMAs or AMLODIPINE | 0.99 | 0.55–1.76 | 0.97 | 0.53 | 0.27–1.04 | 0.064 | 0.51 | 0.22–1.19 | 0.12 | 0.24 | 0.09–0.62 | 0.0031 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Darquennes, G.; Le Corre, P.; Le Moine, O.; Loas, G. Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study. Pharmaceuticals 2021, 14, 226. https://doi.org/10.3390/ph14030226
Darquennes G, Le Corre P, Le Moine O, Loas G. Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study. Pharmaceuticals. 2021; 14(3):226. https://doi.org/10.3390/ph14030226
Chicago/Turabian StyleDarquennes, Gil, Pascal Le Corre, Olivier Le Moine, and Gwenolé Loas. 2021. "Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study" Pharmaceuticals 14, no. 3: 226. https://doi.org/10.3390/ph14030226
APA StyleDarquennes, G., Le Corre, P., Le Moine, O., & Loas, G. (2021). Association between Functional Inhibitors of Acid Sphingomyelinase (FIASMAs) and Reduced Risk of Death in COVID-19 Patients: A Retrospective Cohort Study. Pharmaceuticals, 14(3), 226. https://doi.org/10.3390/ph14030226






