Oral Administration of East Asian Herbal Medicine for Peripheral Neuropathy: A Systematic Review and Meta-Analysis with Association Rule Analysis to Identify Core Herb Combinations
Abstract
:1. Introduction
1.1. Description of the Condition
1.2. Description of the Intervention
1.3. How the Intervention Might Work
1.4. Why It Is Important to Conduct This Review
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.2.1. Types of Studies
2.2.2. Types of Patients
2.2.3. Types of Interventions
2.2.4. Types of Outcome Measurements
2.3. Data Extraction
2.4. Risk of Bias in Individual Studies
2.5. Statistical Analysis
2.5.1. Meta-Analysis
2.5.2. Association Rule Analysis
2.6. Quality of Evidence According to Outcome Measurements
3. Results
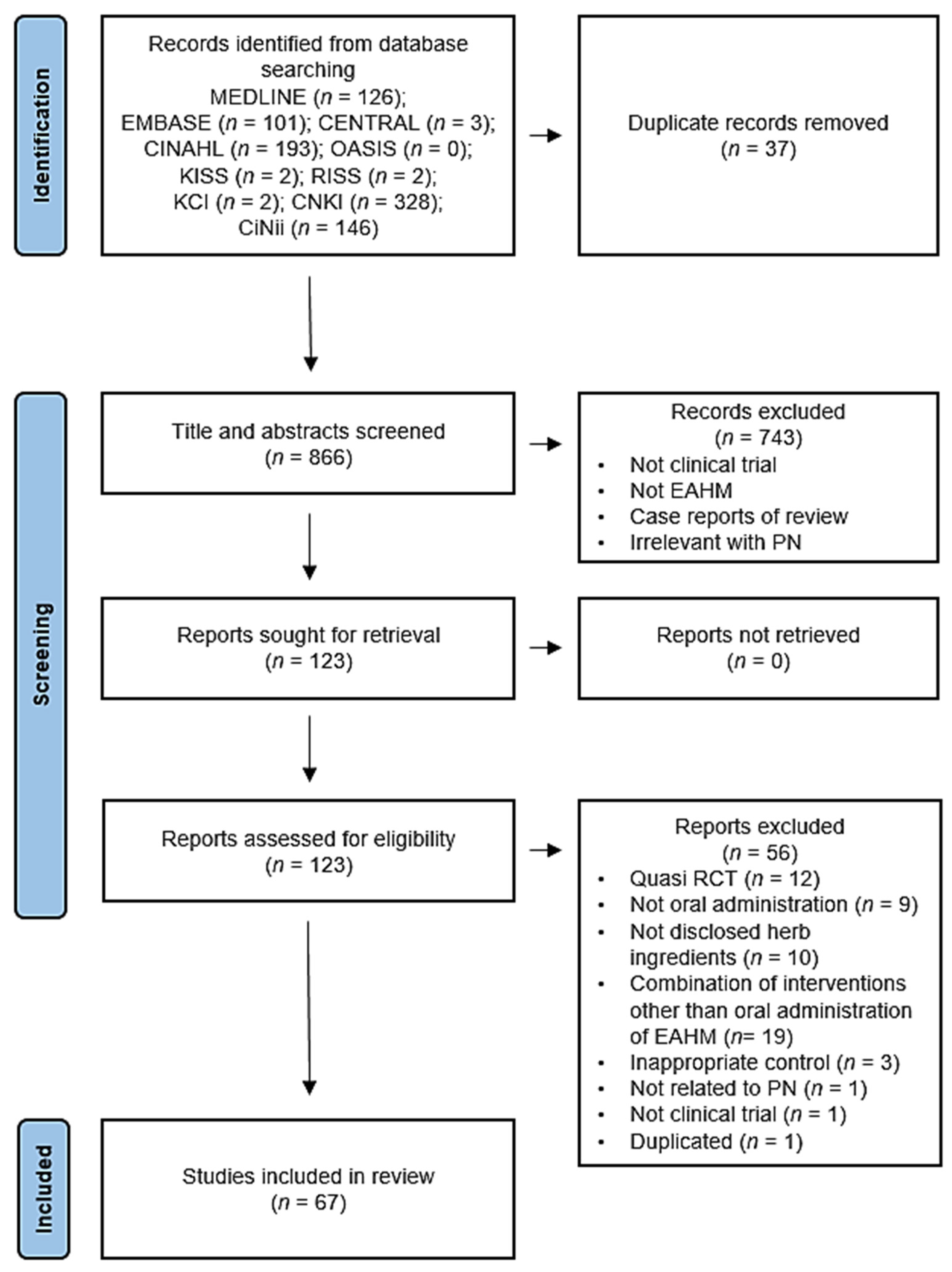
3.1. Study Selection
3.2. Study Characteristics
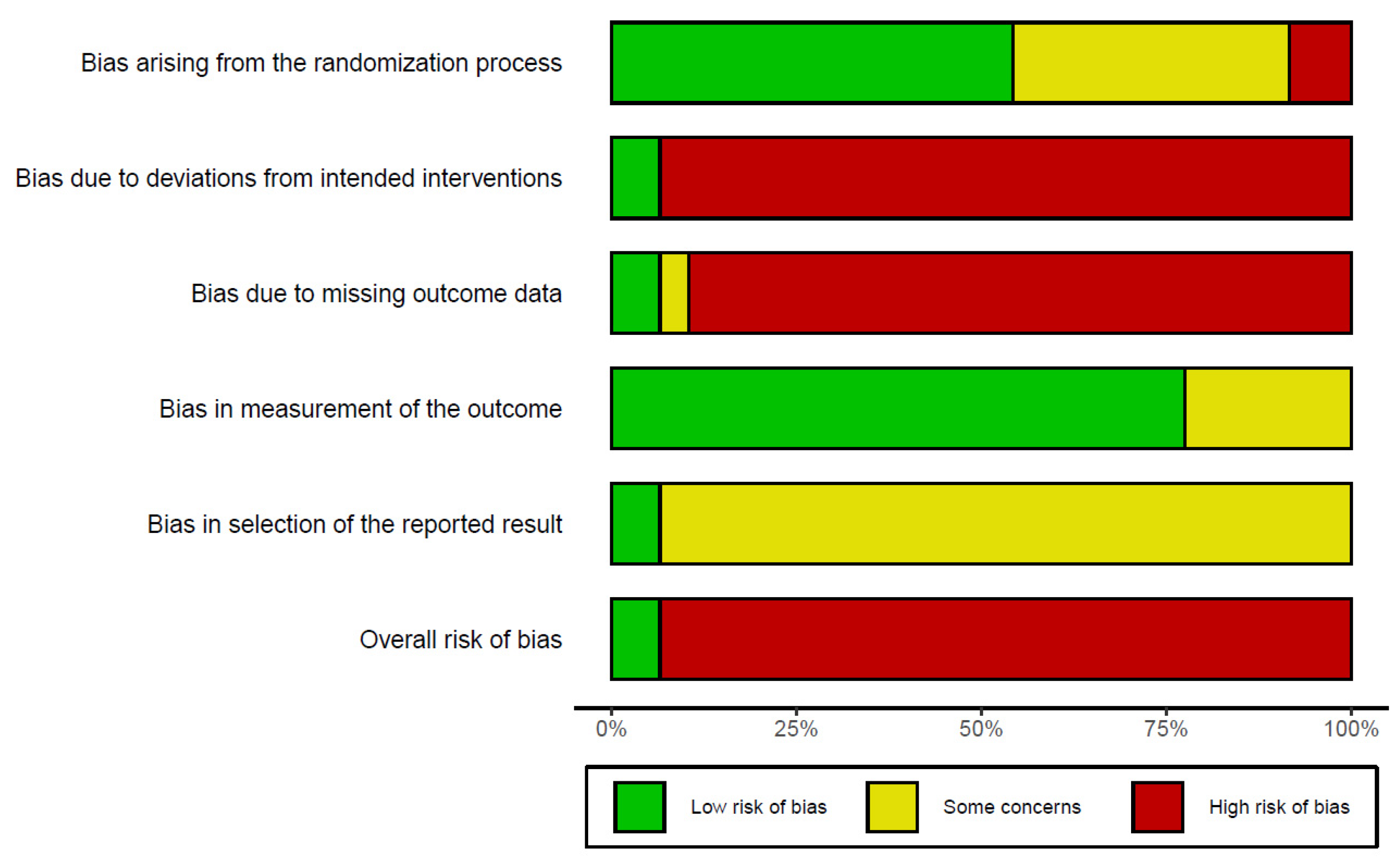
3.3. Risk of Bias
3.4. Efficacy
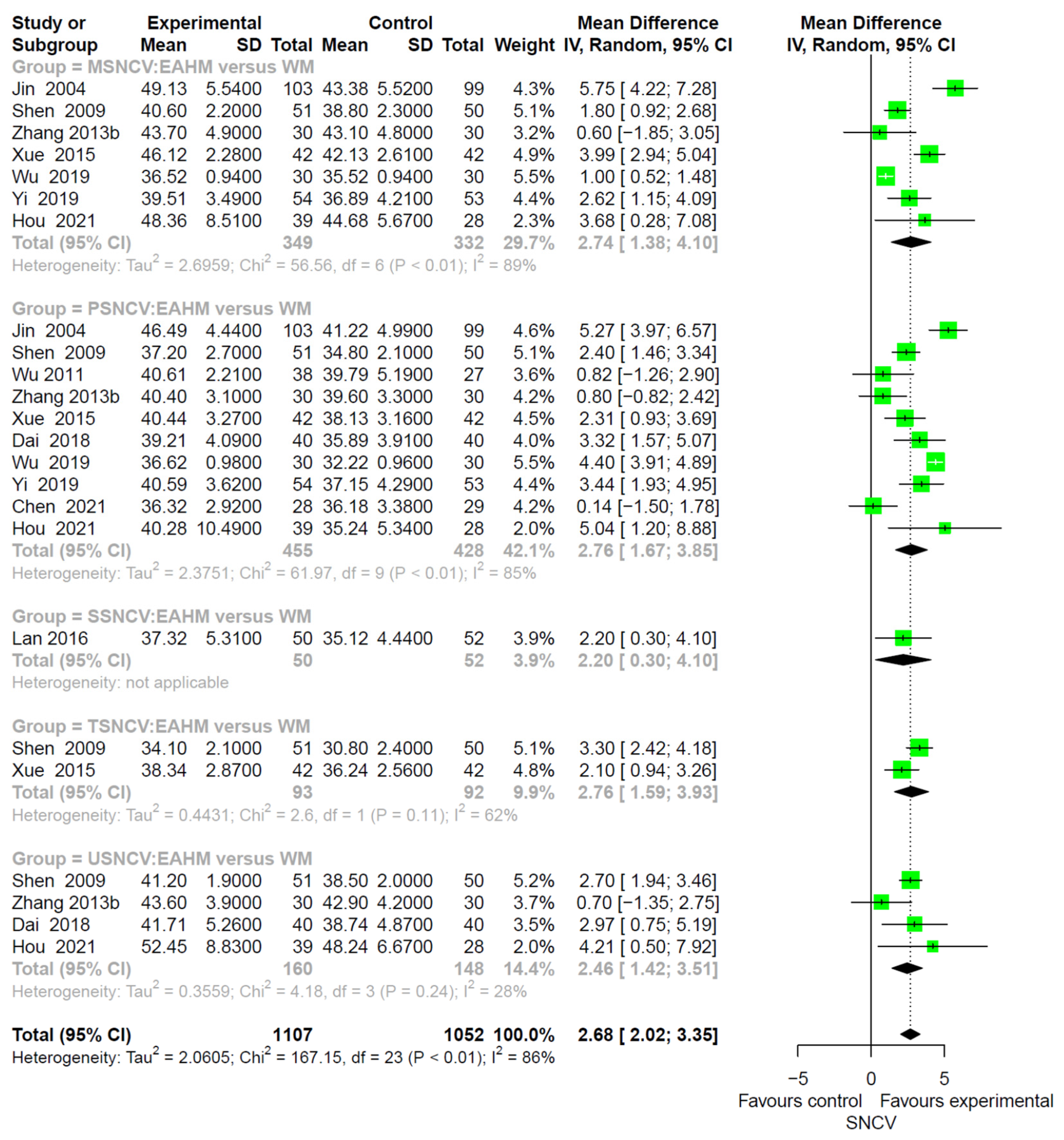
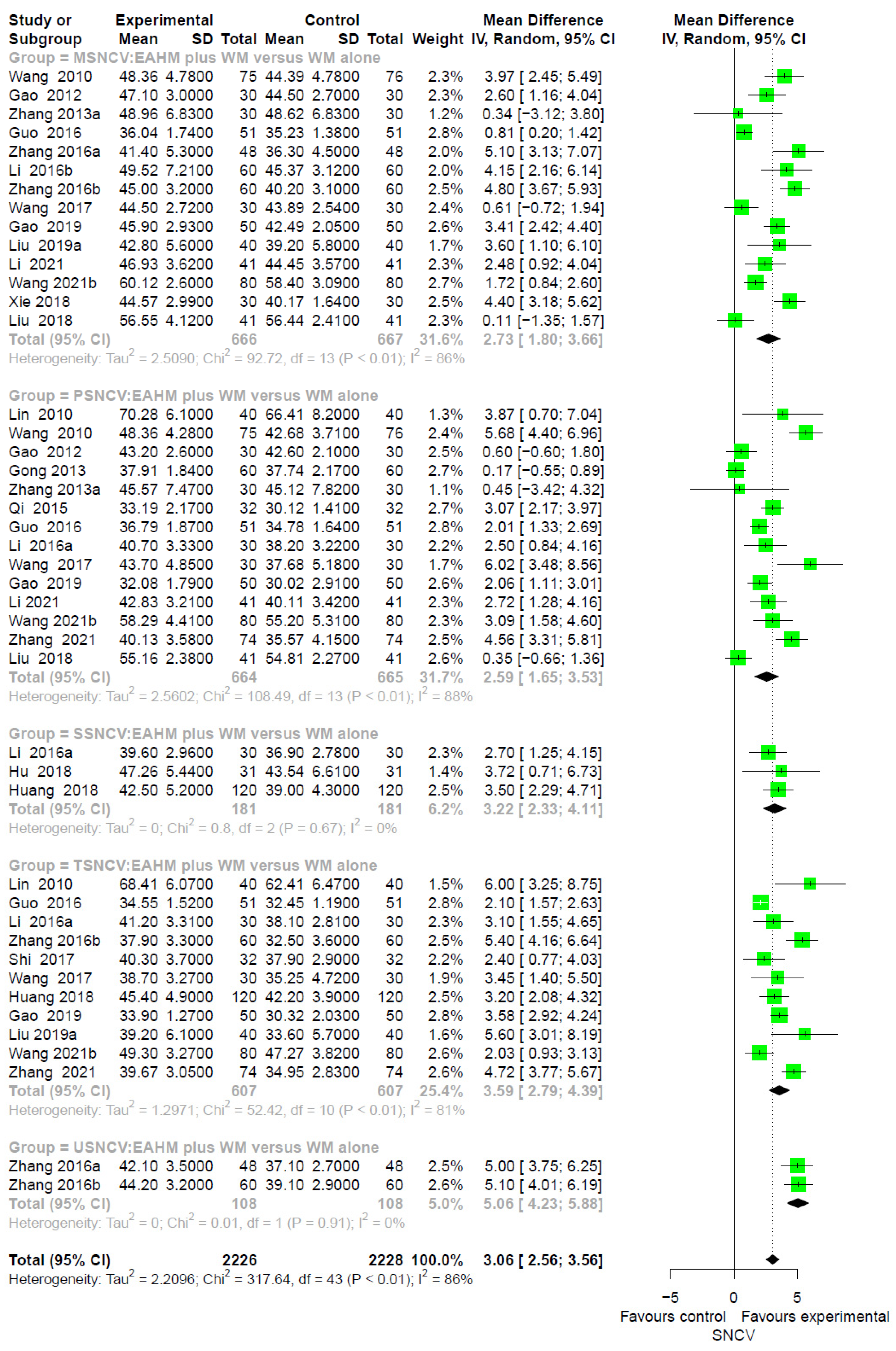
3.4.1. Primary Outcome: Sensory NCV (SNCV)
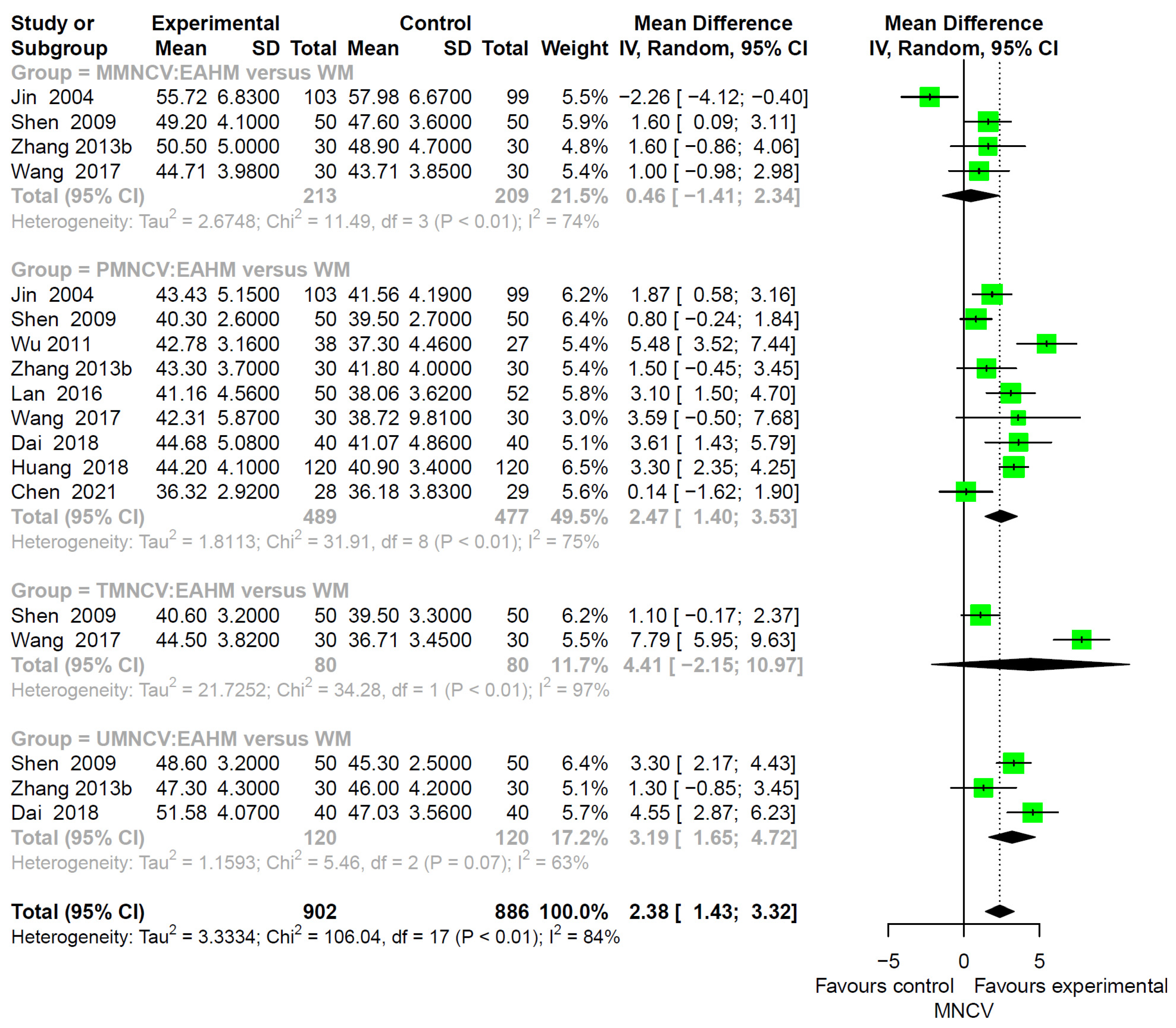
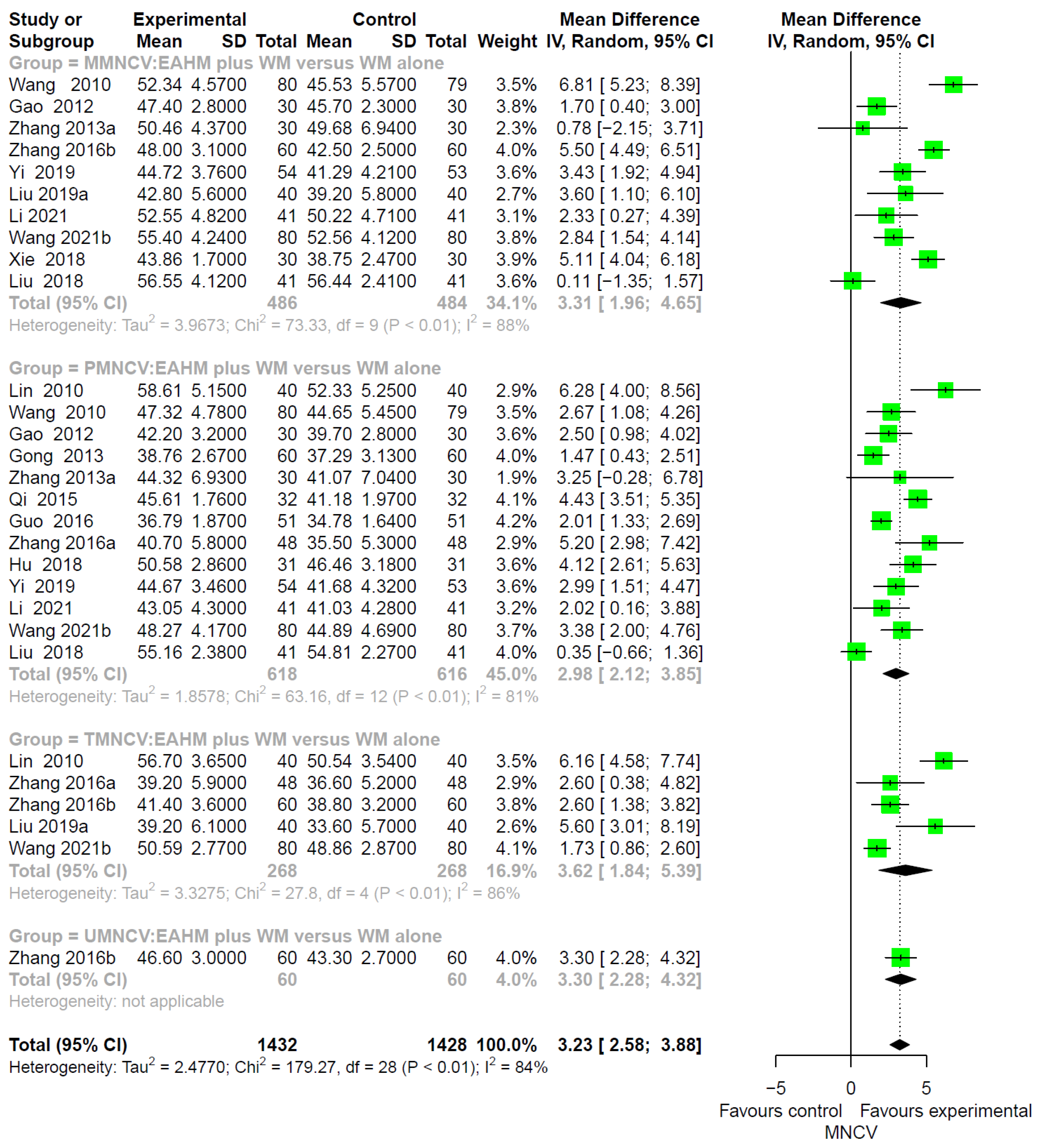
3.4.2. Primary Outcome: Motor NCV (MNCV)
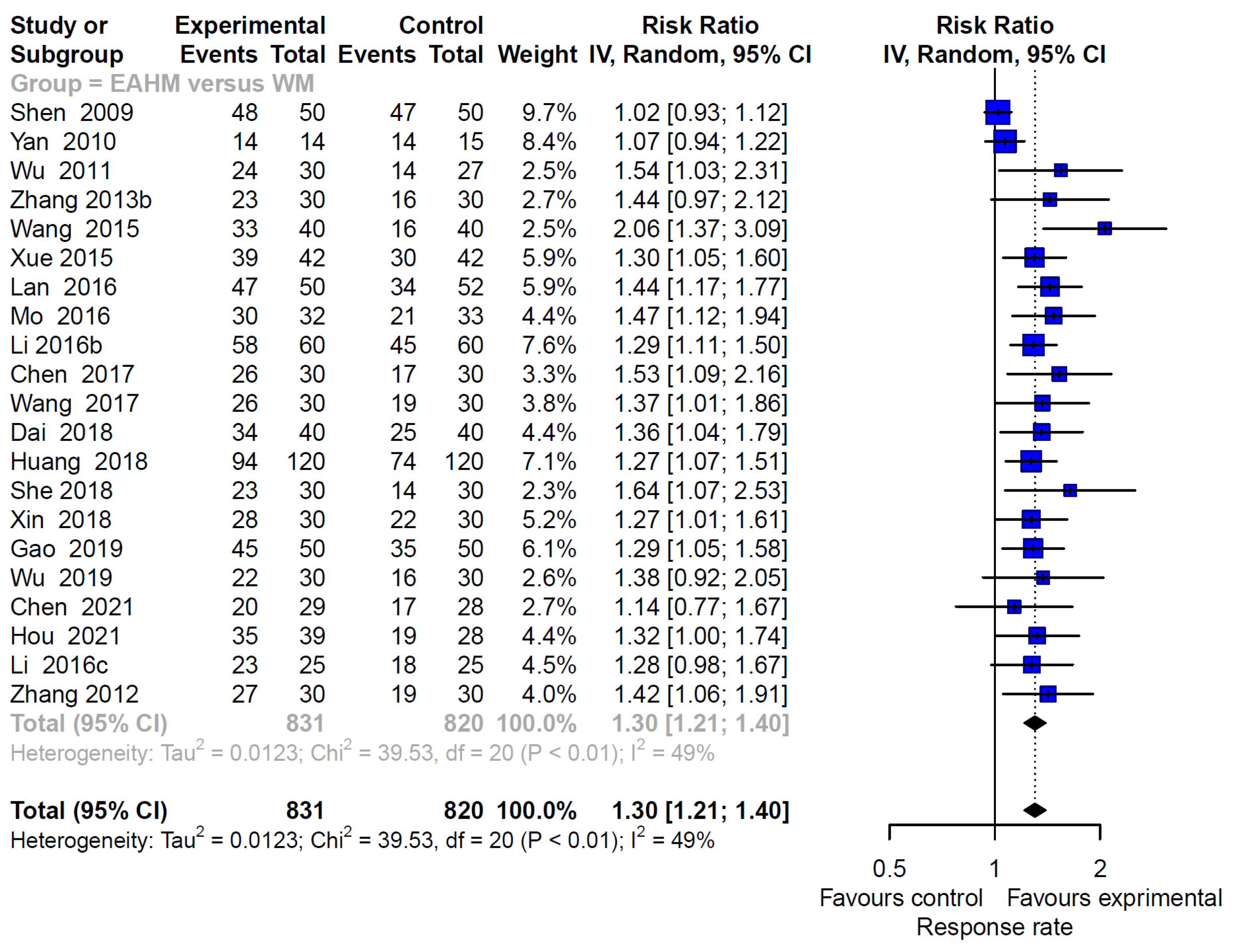
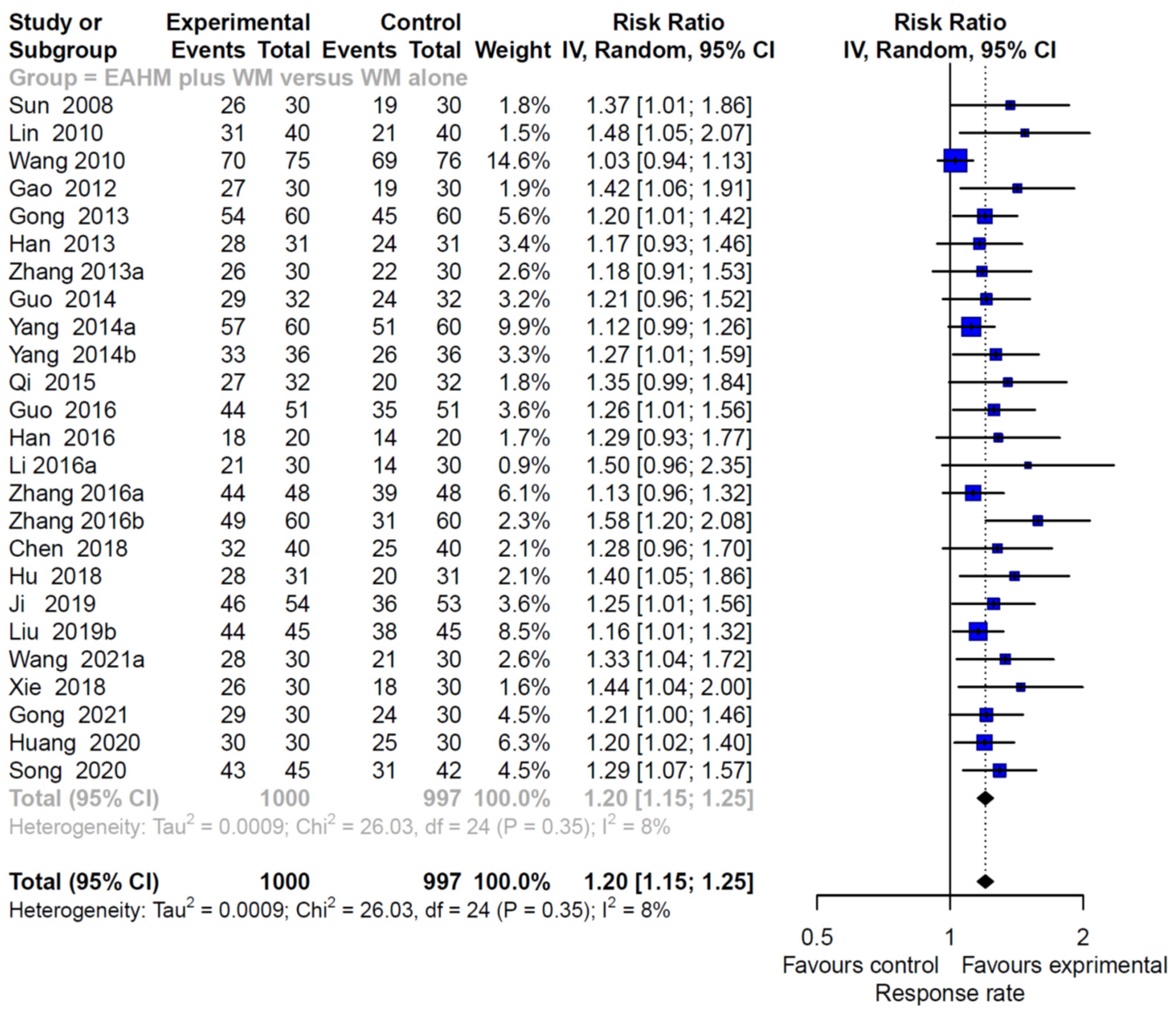
3.4.3. Primary Outcome: Response Rate
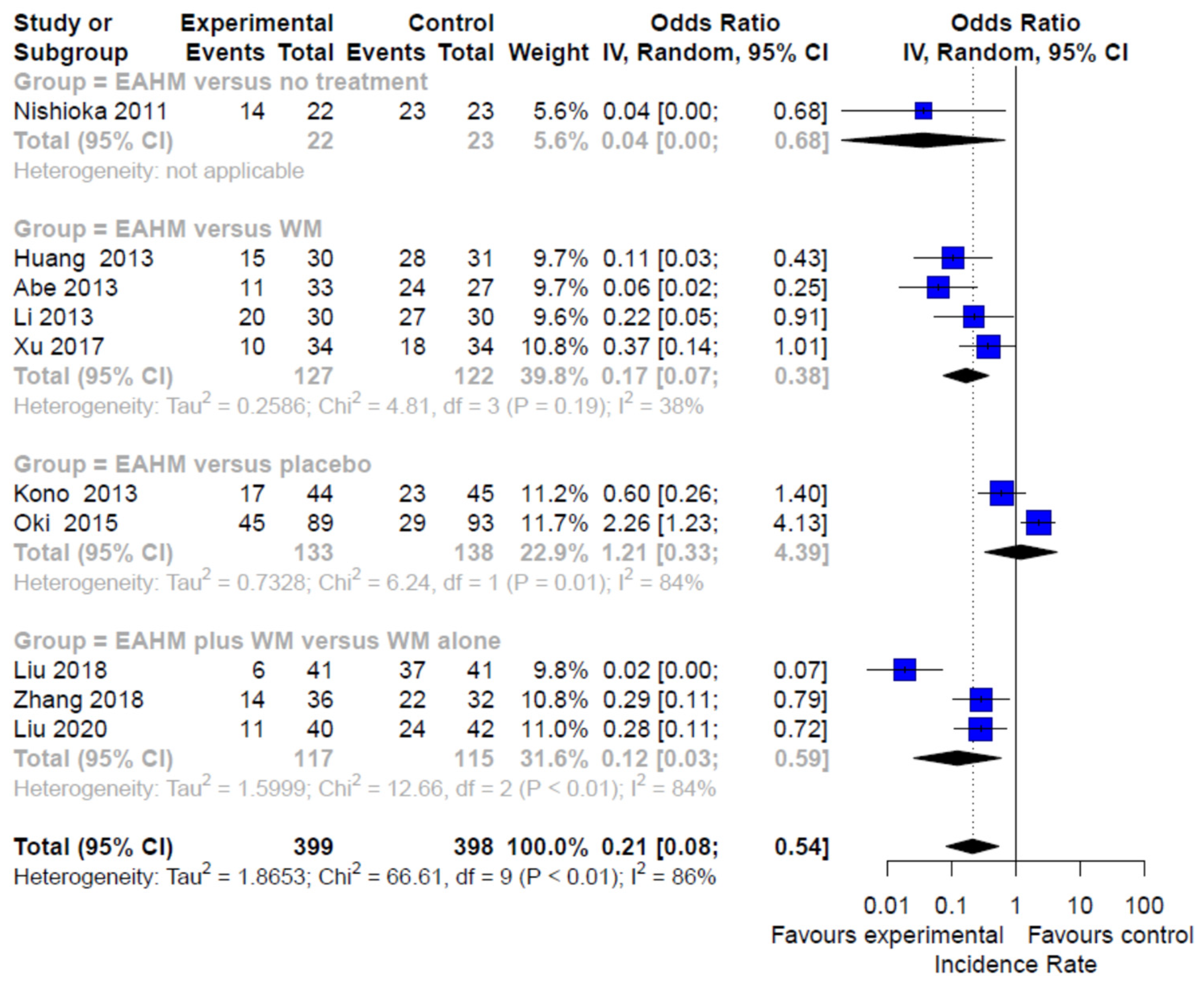
3.4.4. Secondary Outcome: Incidence Rate
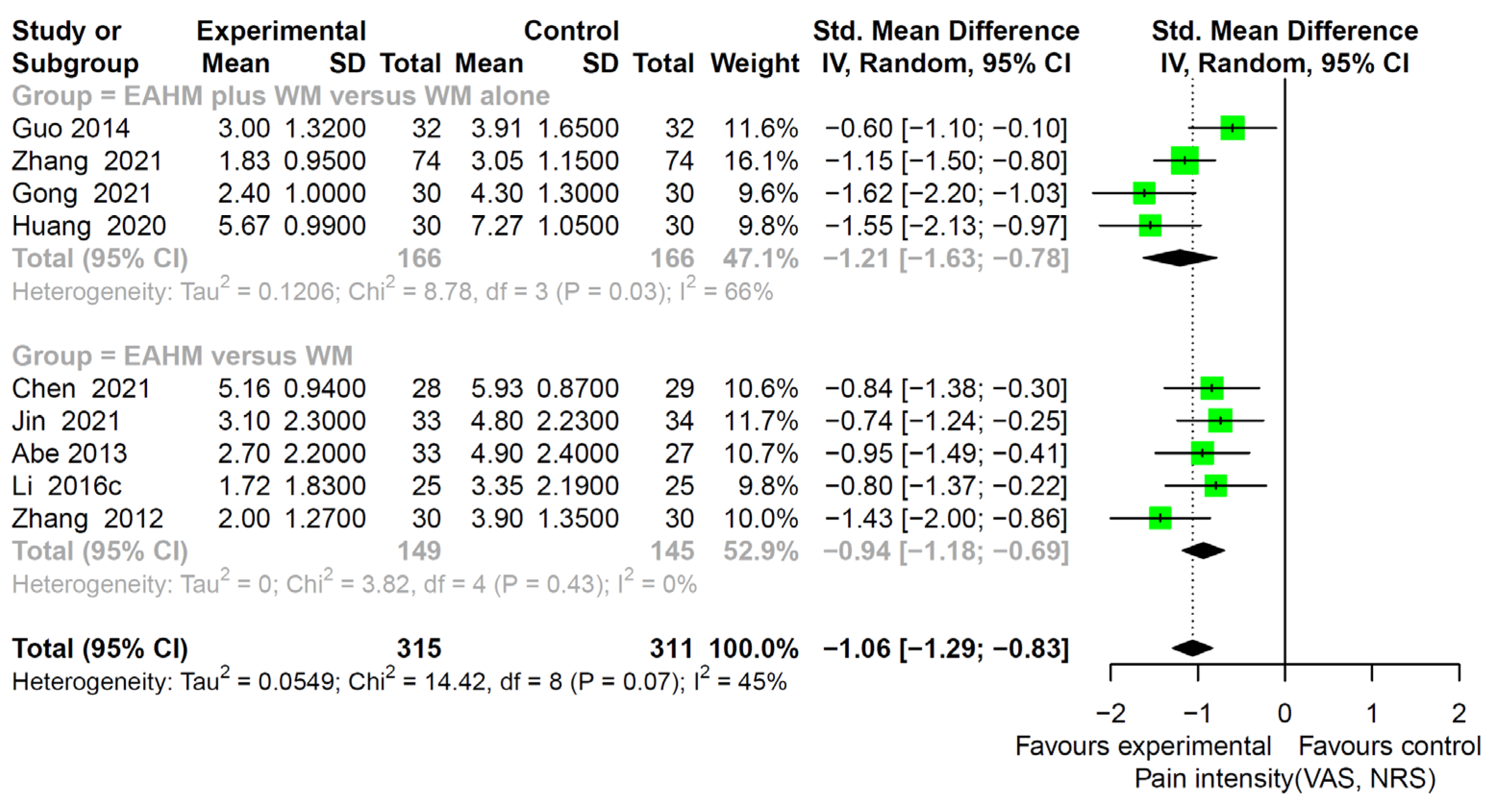
3.4.5. Secondary Outcome: Pain Intensity
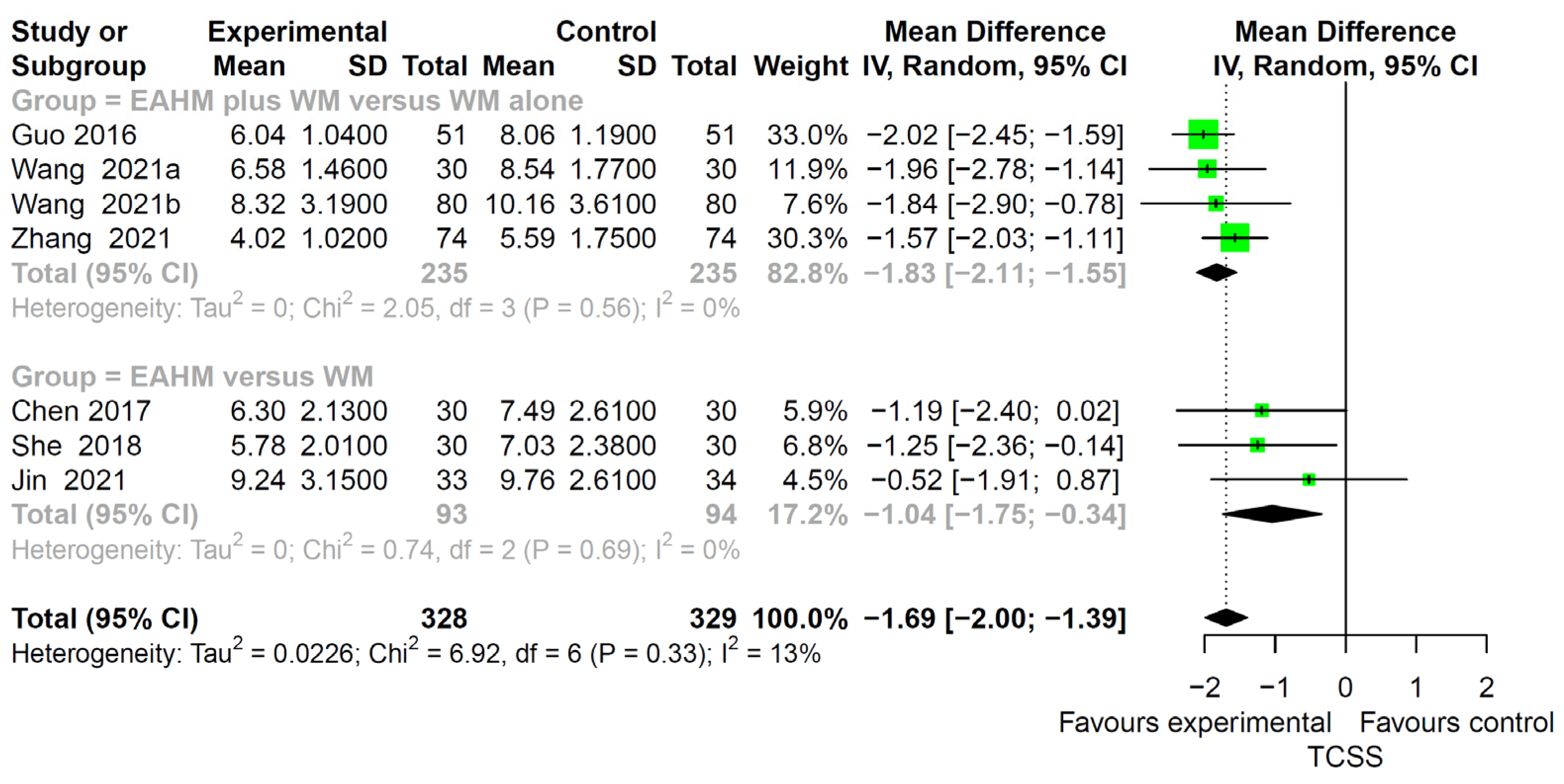
3.4.6. Secondary Outcome: TCSS
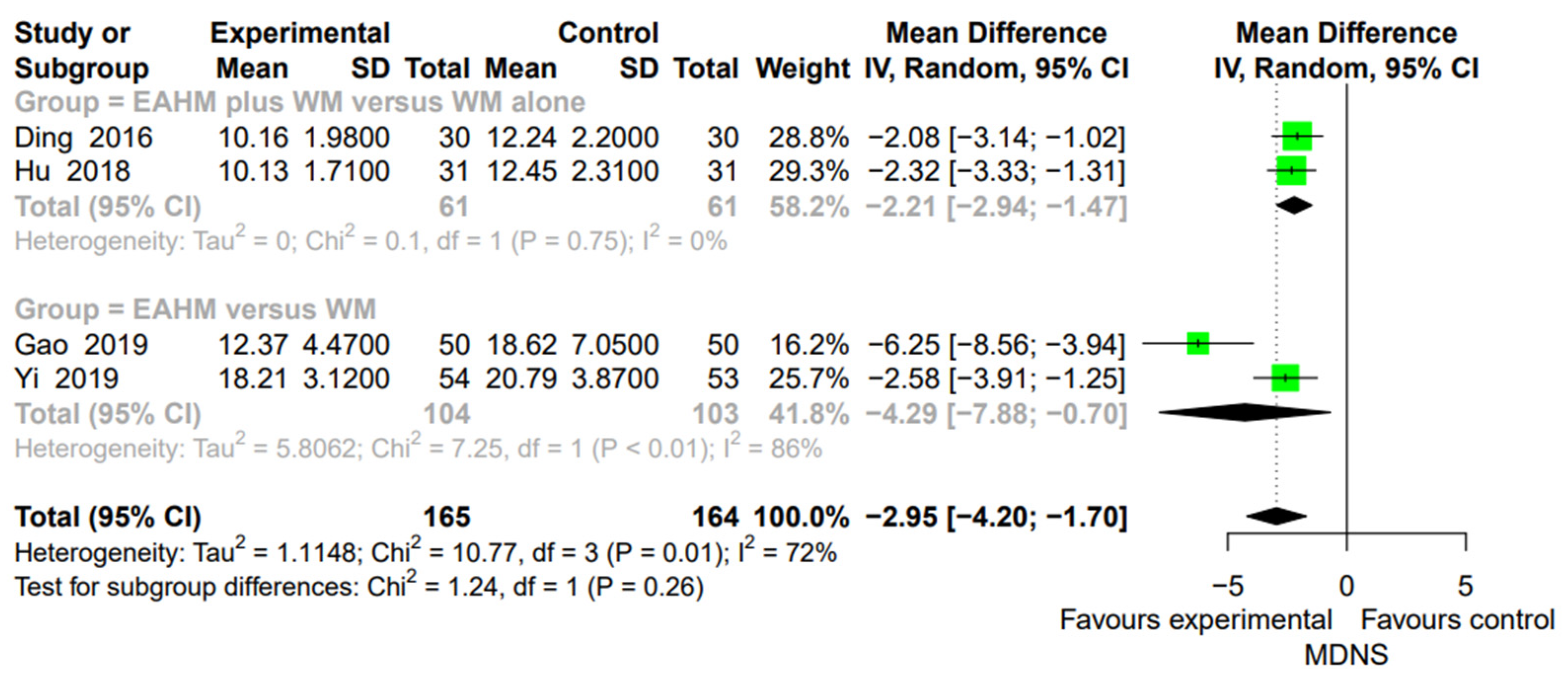
3.4.7. Secondary Outcome: MDNS
3.5. AEs
3.6. Subgroup Analysis
3.7. Further Analysis of EAHM Intervention
3.7.1. EAHM Composition Distribution
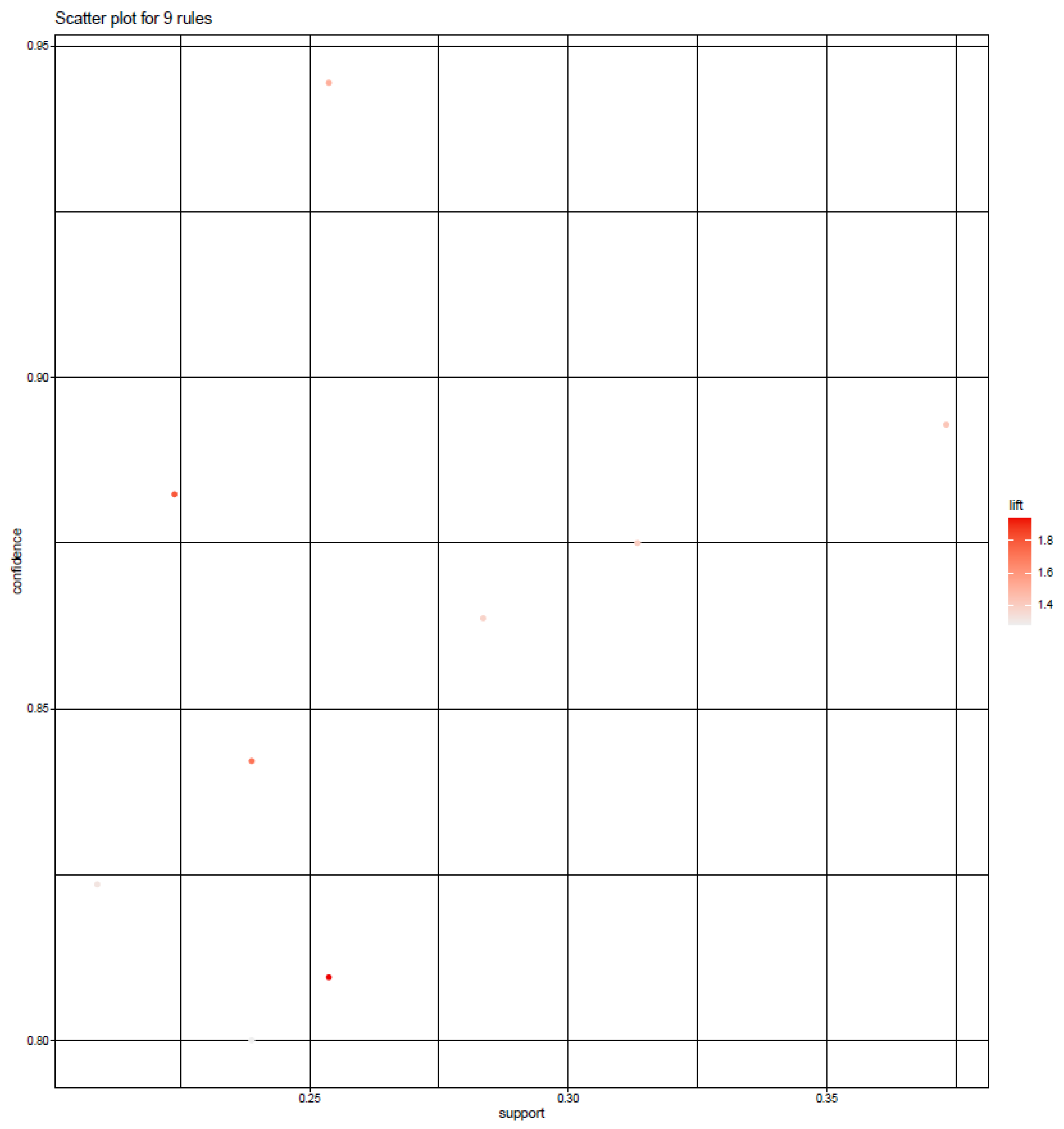
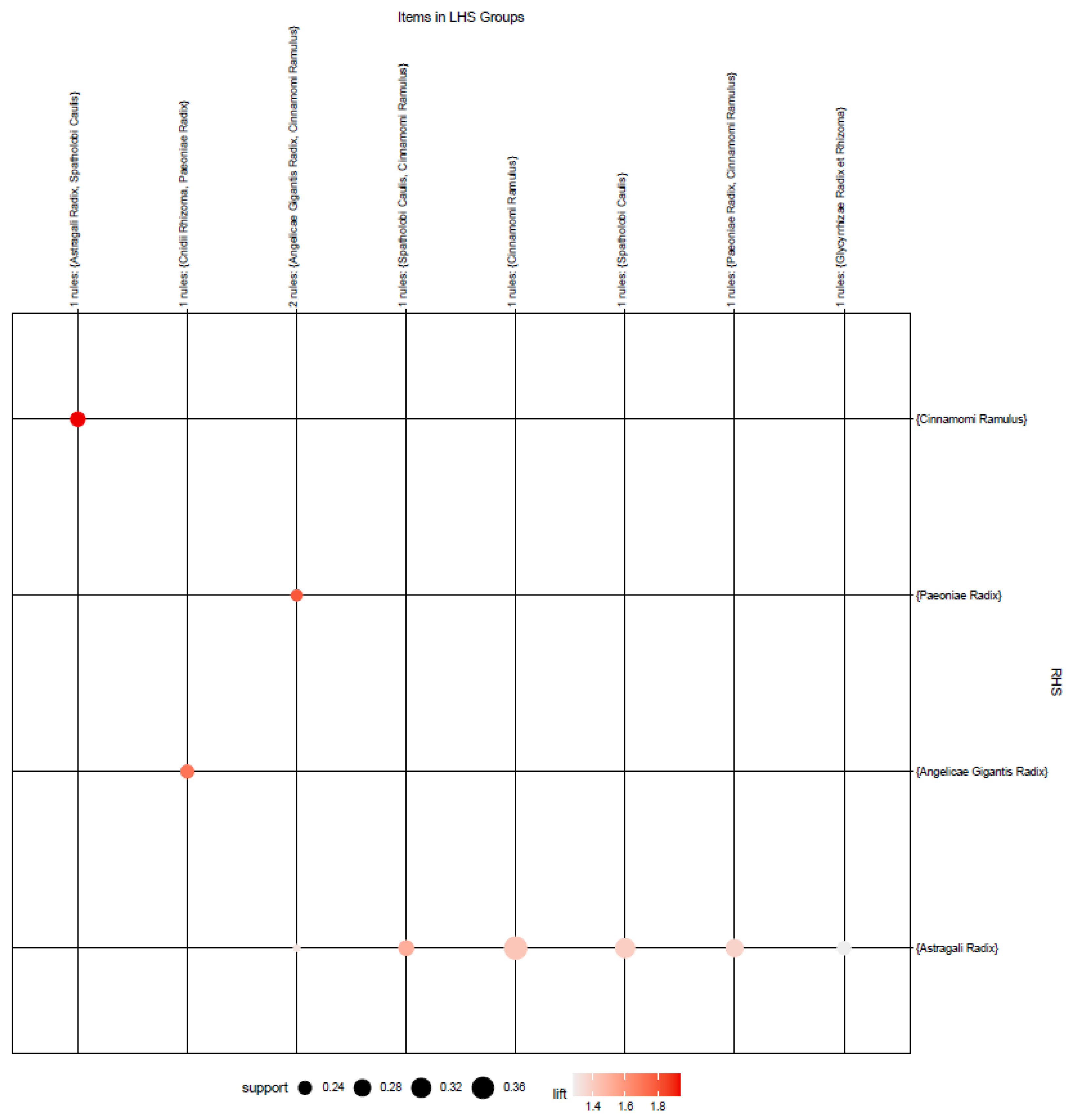
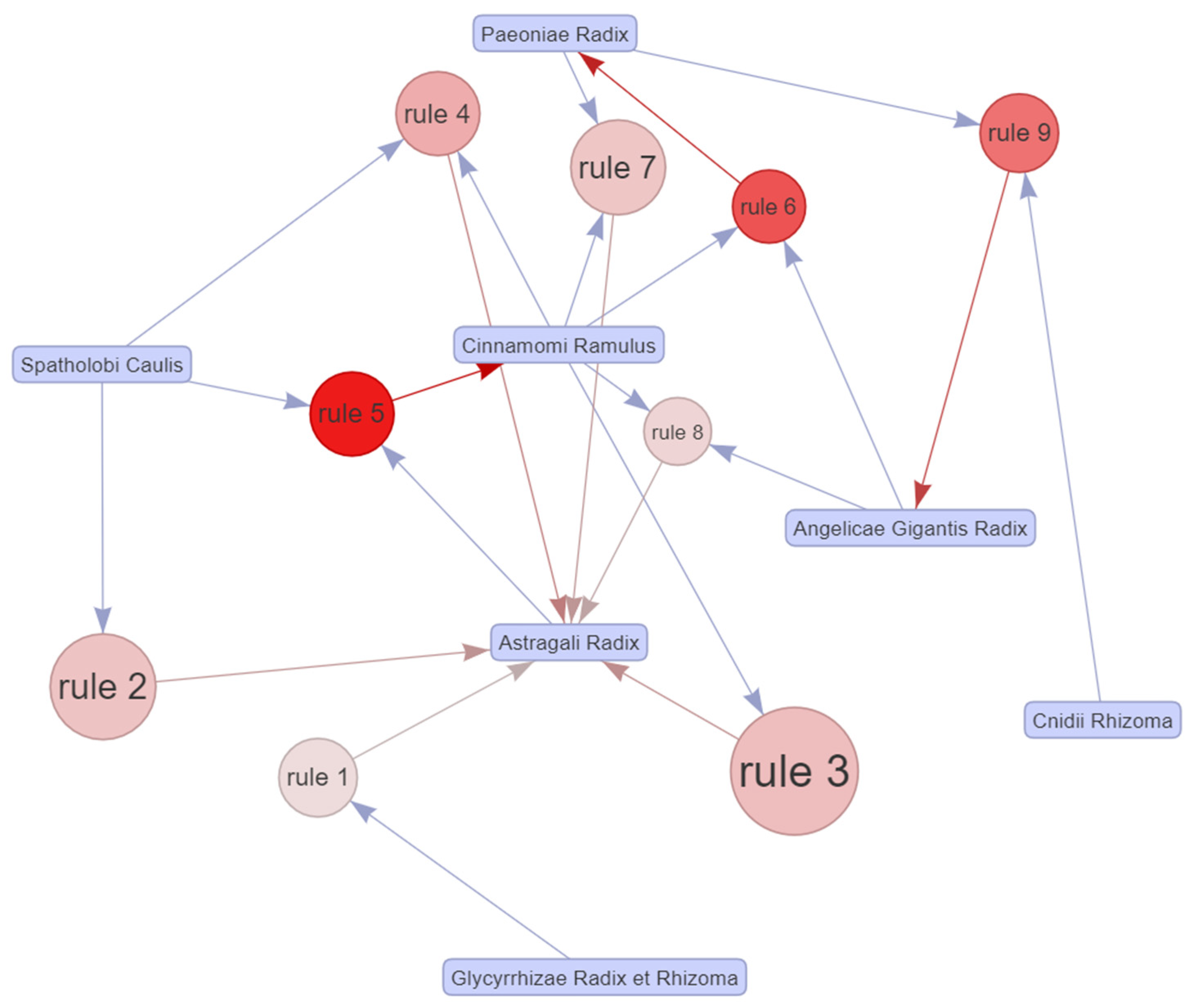
3.7.2. Apriori Algorithm-Based Association Rule Analysis
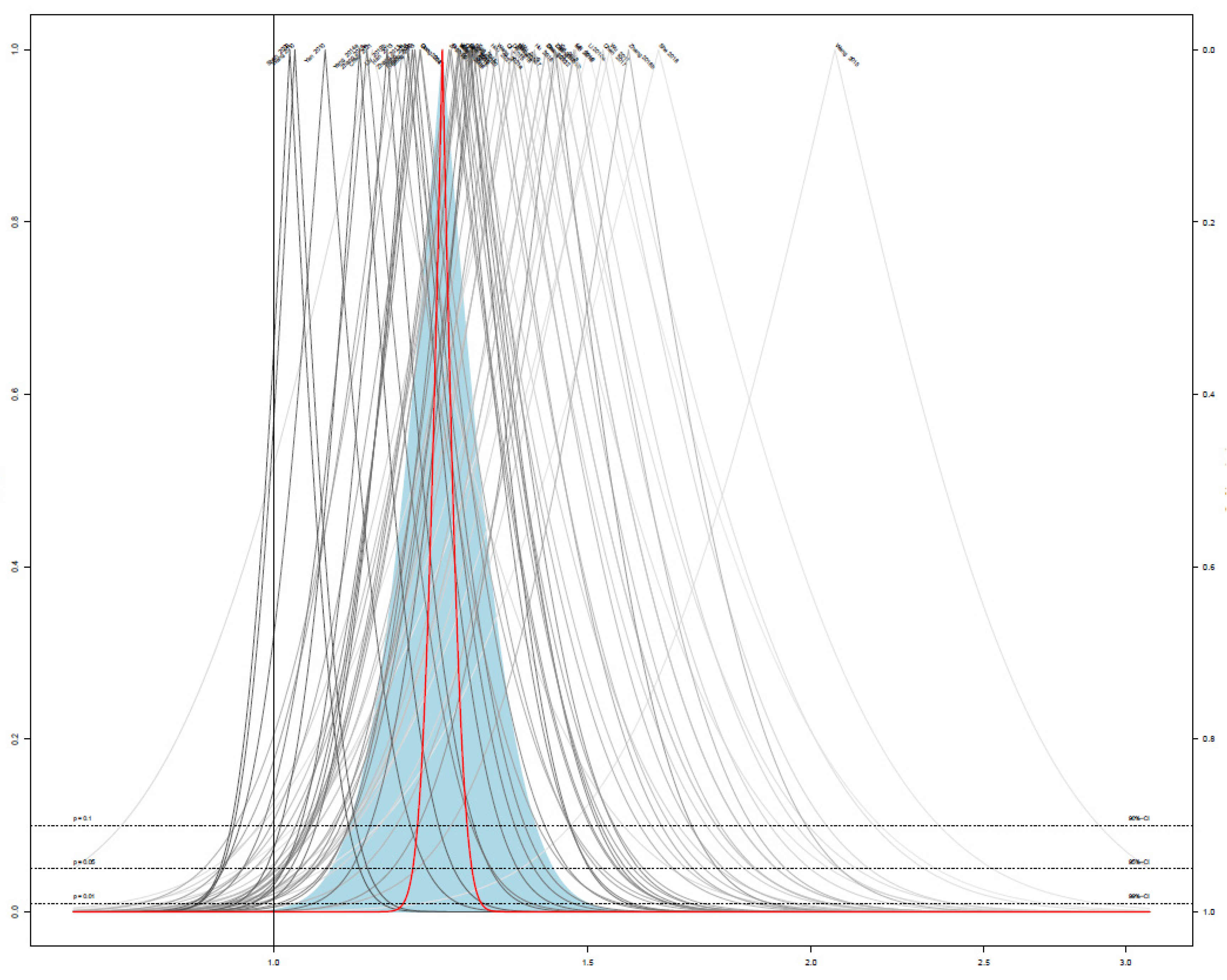
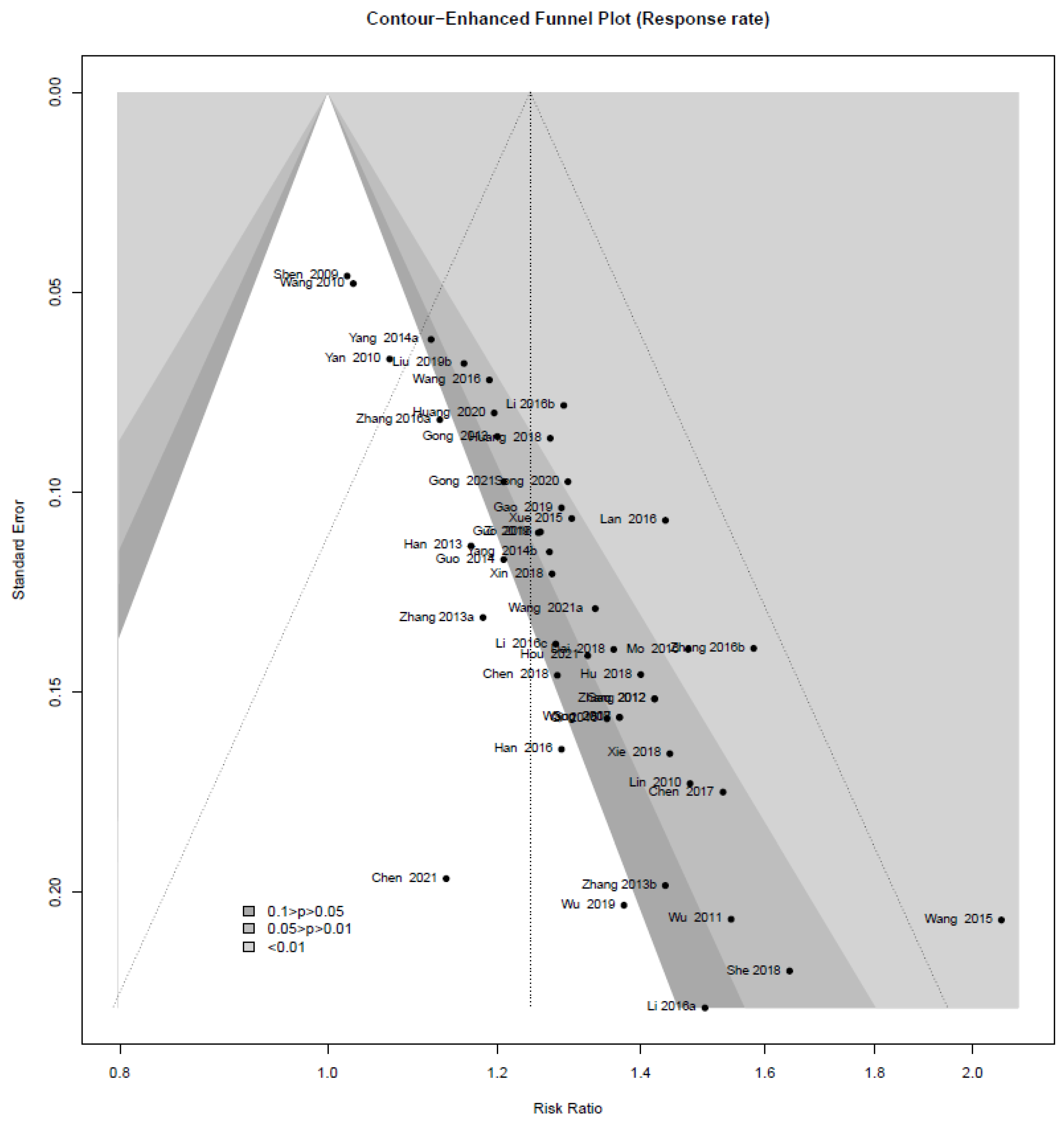
3.8. Publication Bias
3.9. Quality of Evidence According to the Outcome Measurements
4. Discussion
4.1. Summary of the Main Finding
4.2. Limitations
4.3. Implications of Clinical Practices
4.4. Implications of the Research
4.5. Challenges and Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Watson, J.C.; Dyck, P.J.B. Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management. Mayo Clin. Proc. 2015, 90, 940–951. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mallick-Searle, T.; Snodgrass, B.; Brant, J.M. Postherpetic neuralgia: Epidemiology, pathophysiology, and pain management pharmacology. J. Multidiscip. Healthc. 2016, 9, 447–454. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Diabetes Statistics Report 2020. Estimates of Diabetes and Its Burden in the United States. Available online: https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf (accessed on 4 October 2021).
- Siao, P.; Kaku, M. A Clinician’s Approach to Peripheral Neuropathy. Semin. Neurol. 2019, 39, 519–530. [Google Scholar] [CrossRef]
- Attal, N.; Lanteri-Minet, M.; Laurent, B.; Fermanian, J.; Bouhassira, D. The specific disease burden of neuropathic pain: Results of a French nationwide survey. Pain 2011, 152, 2836–2843. [Google Scholar] [CrossRef] [PubMed]
- Torrance, N.; Ferguson, J.A.; Afolabi, E.; Bennett, M.I.; Serpell, M.G.; Dunn, K.M.; Smith, B.H. Neuropathic pain in the community: More under-treated than refractory? Pain 2013, 154, 690–699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Luo, Y.; Wang, C.-Z.; Sawadogo, R.; Tan, T.; Yuan, C.-S. Effects of Herbal Medicines on Pain Management. Am. J. Chin. Med. 2020, 48, 1–16. [Google Scholar] [CrossRef]
- Wu, X.; Hu, X.; Zhang, Q.; Liu, F.; Xiong, K. Regulatory Role of Chinese Herbal Medicine in Regulated Neuronal Death. CNS Neurol. Disord. Drug Targets 2021, 20, 228–248. [Google Scholar] [CrossRef]
- Ebrahimi, F.; Farzaei, M.H.; Bahramsoltani, R.; Heydari, M.; Naderinia, K.; Rahimi, R. Plant-derived medicines for neuropathies: A comprehensive review of clinical evidence. Rev. Neurosci. 2019, 30, 671–684. [Google Scholar] [CrossRef]
- Yang, D.; Liang, X.-C. Strategies and Research Progress of Chinese Medicine in Prevention and Treatment of Diabetic Peripheral Neuropathy. Chin. J. Integr. Med. 2018, 24, 794–800. [Google Scholar] [CrossRef]
- Chien, T.-J.; Liu, C.-Y.; Fang, C.-J.; Kuo, C.-Y. The Efficacy of Acupuncture in Chemotherapy-Induced Peripheral Neuropathy: Systematic Review and Meta-Analysis. Integr. Cancer Ther. 2019, 18, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Dimitrova, A.; Murchison, C.; Oken, B. Acupuncture for the Treatment of Peripheral Neuropathy: A Systematic Review and Meta-Analysis. J. Altern. Complement. Med. 2017, 23, 164–179. [Google Scholar] [CrossRef]
- Deng, B.; Jia, L.; Cheng, Z. Radix Astragali-Based Chinese Herbal Medicine for Oxaliplatin-Induced Peripheral Neuropathy: A Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2016, 2016, 2421876. [Google Scholar] [CrossRef]
- Li, Z.; Jin, H.; Yan, Q.; Sun, L.; Wasan, H.S.; Shen, M.; Ruan, S. The Method of Activating Blood and Dredging Collaterals for Reducing Chemotherapy-Induced Peripheral Neuropathy: A Systematic Review and Meta-Analysis. Evid. Based Complement. Alternat. Med. 2019, 2019, 1029626. [Google Scholar] [CrossRef]
- Lee, G.; Kim, S.K. Therapeutic Effects of Phytochemicals and Medicinal Herbs on Chemotherapy-Induced Peripheral Neuropathy. Molecules 2016, 21, 1252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gu, J.-L.; Wei, G.-L.; Ma, Y.-Z.; Zhang, J.-Z.; Ji, Y.; Li, L.-C.; Yu, J.-L.; Hu, C.-H.; Huo, J.-G. Exploring the Possible Mechanism and Drug Targets of Huang-Qi-Gui-Zhi-Wu-Wu Decoction for the Treatment of Chemotherapy-Induced Peripheral Neuropathy on Network Pharmacology. Evid. Based Complement. Alternat. Med. 2020, 2020, 2363262. [Google Scholar] [CrossRef]
- Lu, M.-C.; Yao, C.-H.; Wang, S.-H.; Lai, Y.-L.; Tsai, C.-C.; Chen, Y.-S. Effect of Astragalus membranaceus in rats on peripheral nerve regeneration: In vitro and in vivo studies. J. Trauma Acute Care Surg. 2010, 68, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Chen, J. The mechanism of astragaloside IV promoting sciatic nerve regeneration. Neural Regen. Res. 2013, 8, 2256–2265. [Google Scholar] [CrossRef] [PubMed]
- Tou, W.I.; Chang, S.-S.; Lee, C.-C.; Chen, C.Y.-C. Drug design for neuropathic pain regulation from traditional Chinese medicine. Sci. Rep. 2013, 3, 844. [Google Scholar] [CrossRef] [Green Version]
- Noh, H.; Yoon, S.W.; Park, B. A Systematic Review of Herbal Medicine for Chemotherapy Induced Peripheral Neuropathy. Evid. Based Complement. Alternat. Med. 2018, 2018, 6194184. [Google Scholar] [CrossRef]
- Pang, B.; Zhao, T.-Y.; Zhao, L.-H.; Wan, F.; Ye, R.; Zhou, Q.; Tian, F.; Tong, X.-L. Huangqi Guizhi Wuwu Decoction for treating diabetic peripheral neuropathy: A meta-analysis of 16 randomized controlled trials. Neural Regen. Res. 2016, 11, 1347–1358. [Google Scholar] [CrossRef]
- Higgns, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, version 6.2 (updated February 2021); Cochrane: London, UK, 2021; Available online: https://training.cochrane.org/handbook (accessed on 2 September 2021).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Perkins, B.A.; Olaleye, D.; Zinman, B.; Bril, V. Simple screening tests for peripheral neuropathy in the diabetes clinic. Diabetes Care 2001, 24, 250–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldman, E.L.; Stevens, M.J.; Thomas, P.K.; Brown, M.B.; Canal, N.; Greene, D.A. A practical two-step quantitative clinical and electrophysiological assessment for the diagnosis and staging of diabetic neuropathy. Diabetes Care 1994, 17, 1281–1289. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencows, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [Green Version]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.r-project.org/ (accessed on 11 August 2021).
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef]
- Lortie, C.J.; Filazzola, A. A contrast of meta and metafor packages for meta-analyses in R. Ecol. Evol. 2020, 10, 10916–10921. [Google Scholar] [CrossRef]
- Peters, J.L.; Sutton, A.J.; Jones, D.R.; Abrams, K.R.; Rushton, L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. J. Clin. Epidemiol. 2008, 61, 991–996. [Google Scholar] [CrossRef]
- Hahsler, M.; Grün, B.; Hornik, K. arules—A Computational Environment for Mining Association Rules and Frequent Item Sets. J. Stat. Softw. 2005, 14, 1–25. [Google Scholar] [CrossRef]
- Hahsler, M. arulesViz: Interactive Visualization of Association Rules with R. R J. 2017, 9, 163–175. [Google Scholar] [CrossRef]
- Agrawal, R.; Imieliński, T.; Swami, A. Mining association rules between sets of items in large databases. In Proceedings of the 1993 ACM SIGMOD International Conference on Management of Data, Washington, DC, USA, 26–28 May 1993; Volume 22, pp. 207–216. [Google Scholar] [CrossRef]
- Hsieh, P.-C.; Cheng, C.-F.; Wu, C.-W.; Tzeng, I.-S.; Kuo, C.-Y.; Hsu, P.-S.; Lee, C.-T.; Yu, M.-C.; Lann, C.-C. Combination of Acupoints in Treating Patients with Chronic Obstructive Pulmonary Disease: An Apriori Algorithm-Based Association Rule Analysis. Evid. Based Complement. Alternat. Med. 2020, 2020, 8165296. [Google Scholar] [CrossRef]
- Kuo, M.H.; Kushniruk, A.W.; Borycki, E.M.; Greig, D. Application of the Apriori algorithm for adverse drug reaction detection. Stud. Health Technol. Inform. 2009, 148, 95–101. [Google Scholar] [PubMed]
- Lu, P.-H.; Keng, J.-L.; Kuo, K.-L.; Wang, Y.-F.; Tai, Y.-C.; Kuo, C.-Y. An Apriori Algorithm-Based Association Rule Analysis to Identify Herb Combinations for Treating Uremic Pruritus Using Chinese Herbal Bath Therapy. Evid. Based Complement. Alternat. Med. 2020, 2020, 8854772. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J.; GRADE working group. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jin, J.; Chen, H.; Zhao, D.; Feng, Z.; Liu, Q.; Zhang, Z.; Qin, R. Clinical study on tangmaitong tablets in treating 103 cases of diabetic peripheral neuropathy. J. Tradit. Chin. Med. 2004, 45, 429–431. [Google Scholar]
- Sun, L. Clinical Observation on Treatment of 30 Cases of Peripheral Neuroapthy of Type 2 Diabetes with Nourishing Yin Bushen Huoxue Tongluo Decoction. Chin. J. Med. Drug Appl. 2008, 2, 39–40. [Google Scholar]
- Shen, J.; Shu, X. Clinical study of tangmaining capsule in the treatment of diabetic peripheral neuropathy. Chin. J. Exp. Trad. Med. Formul. 2009, 15, 74–76. [Google Scholar]
- Lin, M.; Yu, J.; Deng, Y.; Tan, S. Tongxinluo capsule combined with methyl vitamin B12 in the treatment of multiple diabetes observation of therapeutic effect of neuropathy. Chin. J. Clin. Ration. Drug Use 2010, 3, 31–32. [Google Scholar]
- Wang, Z.; Wang, J. Observation on curative effect of huangqi guizhi wuwu decoction in treating diabetic peripheral neuropathy. Qingdao Med. Health 2010, 42, 275–276. [Google Scholar]
- Yan, Q.; Yu, J. Evaluation of clinical therapeutic effect of the method for nourishing yin and activating blood circulation on diabetic peripheral neuropathy. Chin. Arch. TCM 2010, 28, 2372–2373. [Google Scholar]
- Wu, Y.; Zhang, J.; Qin, F. Modified yiqi huoxue decoction for the treatment of 30 cases of diabetic peripheral neuropathy. Chin. Foregin. Med. Treat. 2011, 18, 127–128. [Google Scholar]
- Gao, Z.; Wang, X. Clinical observation of diabetic peripheral neuropathy by the interfere of nourishing the liver to stop the wind and tonglu decoction. Chin. J. Basic Med. TCM 2012, 9, 998–1000. [Google Scholar]
- Gong, Y.; Wang, J.; Tan, Y.; Lu, J. Clinical effects of modified aconiti deccotion for diabetic perpheral neuropathy and its influences on the glucose level. J. Clin. Med. Pract. 2013, 17, 11–13. [Google Scholar]
- Han, J. Modified huangqi guizhi wuwu decoction combined with mecobalamin tablets in treating diabetes clinical observation of 62 cases of neuropathy. Anhui Med. Pharm. J. 2013, 17, 849–850. [Google Scholar]
- Zhang, J. Observation of mudan tongluo fang in the treatment of type 2 diabectic peripheral neuropathy. Clin. J. Tradit. Chin. Med. 2013, 25, 753–755. [Google Scholar]
- Zhang, Y. Observation on therapeutic effect of modified “Tangbaokang” on 60 cases of diabetic peripheral neuropathy. J. Med. Theor. Pract. 2013, 26, 747–749. [Google Scholar]
- Guo, Y.; Liu, Y.; Sun, Y.; Qin, B.; Cai, D. Clinical observation of modified “huangqi guizi wuwu decoction” for diabetic peripheral neuropathic pain. SH J. TCM 2014, 48, 40–42. [Google Scholar]
- Yang, Y. Shenqixuebi Decoction and Western Medicine Treat 60 Cases of Diabetic Peripheral Neuropathy. TCM Res. 2014, 27, 27–29. [Google Scholar]
- Yang, Q.; Chen, H. Treatment of 36 cases of diabetic peripheral neuropathy with modified huangqi guizi wuwu decoction. J. Aerospace Med. 2014, 25, 1009–1010. [Google Scholar]
- Qi, Y.; Yu, S. Effect of Mudan Granules on Oxidative Stress in Painful Diabetic Peripheral Neuropathy. Lishizhen Med. Mater. Med. Res. 2015, 26, 1561–1563. [Google Scholar]
- Wang, L.; Su, J.; Jiao, H.; Zhang, Y.; Liu, T.; Sin, L. 40 Cases of Senile Diabetic Peripheral Neuropathy Treated with Yixinshu Capsule and Maixuekang Capsule. J. Integr. TCWM Cardiovasc. Dis. 2015, 13, 939–940. [Google Scholar]
- Xue, L.; Chen, H.; Yang, Y.; Zhang, Z. Clinical observation on the treatment of 42 cases of diabetic peripheral neuropathy with modified liuteng shuilu shexian decoction. J. Sichuan TCM 2015, 33, 59–61. [Google Scholar]
- Ding, H.; Yuan, F. Clinical observation of buyang huanwu decoction combined with western medicine routine therapy in the treatment of diabectic peripheral neuropathy lesion. Chin. Med. Mod. Dis. Edu. Chin. 2016, 14, 1–3. [Google Scholar]
- Guo, H. Clinical research of the patients with type 2 diabetic peripheral neuropathy in the elderly treated by compound qiteng tongluo tang combined epalrestat. Acta Chin. Med. 2016, 31, 1874–1879. [Google Scholar]
- Han, L. Therapeutic effect of Zhanjintongluo Chinese medicine combined with mecobalamin in the treatment of patients with diabetic peripheral neuropathy. Diabetes New World 2016, 19, 50–51. [Google Scholar]
- Lan, B.; Wang, X.; Mi, J.; Wang, G. Clinic study of yiqi huoxue tongluo in treating diabetic peripheral neuropathy. Chin. Med. Mod. Dis. Edu. Chin. 2016, 14, 58–59. [Google Scholar]
- Mo, S.; Xiao, T. The observation on the clinical effect of yangyin jiedu decoction in the treatment of diabetic perpheral neuropathy of qi and yin deficiency with blood stasis type. World J. Integr. Trad. West Med. 2016, 11, 692–695. [Google Scholar]
- Wang, Z.; An, X.; Chen, L.; Aihua, C.; Wen, H.; Lin, N. Clinical study on modified tangbitong recipe for treatment of type 2 diabetes distal symmetric polyneuropathy. Guangxi TCM 2016, 39, 19–21. [Google Scholar]
- Li, G.; Huang, D.; Li, M.; Lin, L. Effects of wenyang huoxue tongbi fang on nerve conduction velocity and plasma hcy of diabetic peripheral neurophathy with yang-deficiency, congealing cold and blood stasis syndrome. J. Tradit. Chin. Med. 2016, 57, 1486–1489. [Google Scholar]
- Zhang, J.; Zhi, D.; Xie, H. Treatment of 48 cases of diabetic peripheral neuropathy with huangqichifeng decoction combined danggisini decoction. World Latest Med. Info. 2016, 16, 26–27. [Google Scholar]
- Li, H.; Zhong, Q. Clinical observatyion of huangzhi tonglnaoluo capsule in treating diabetic periphral neuropathy. Yunnan J. TCM Mater. Med. 2016, 37, 37–38. [Google Scholar]
- Zhang, H.; Su, H.; Wang, Y.; Zhang, B. Observation of the clinical effect of nimodipine combined with qiming granule in the treatment of diabetic peripheral neuropathy. Inf. TCM 2016, 33, 97–100. [Google Scholar]
- Chen, H.; Wu, J.; Tan, H. Clinical observation of danggui sini tang for diabetic peripheral neuropathy. J. New Chin. Med. 2017, 49, 56–58. [Google Scholar]
- Shi, Z.; Li, L.; Wang, K.; Lu, Y. Effect of compound danshen dripping pills on early peripheral neuropathy in patients with type 2 diabetes. Diabetes New World 2017, 4, 174–176. [Google Scholar]
- Wang, P.; Cui, P.; Hong, Y. Effect of danggui sini deccotion on treatment of diabetic peripheral neuropathy with cold congealing and blood stasis. Chin. Arch. TCM 2017, 35, 661–664. [Google Scholar]
- Chen, X. Clinical study on danggui sini tang in treatment of peripheral neuropathy of diabetes mellitus with cold and dampness obstraction spleen syndrome. Acta Chin. Med. 2018, 33, 756–759. [Google Scholar]
- Dai, Q.; Xu, X. Clinical study of huangqi guizhi wuwu decoction combined with yunu decoction in the treatment of diabectic peripheral neuropathy. Shaanxi TCM 2018, 39, 482–484. [Google Scholar]
- Hu, Y.; Liu, H.; Liu, M.; Wang, T. Clinical observation of modified jiajian huangqi guizhi wuwu decoction in treating diabetic peripheral neuropahty patients with Qi deficiency and blood stasis type. Clin. J. TCM 2018, 30, 105–107. [Google Scholar]
- Huang, X.; Lin, X.; Chen, C. Clinical study on matong powder in treating 120 cases of diabetic peripheral neuritis. Mod. Hosp. 2018, 18, 288–290. [Google Scholar]
- She, Y.; Yu, J.; Li, R.; Wang, Y.; Zhang, S. Observations on curative effect of huangqi guizhi wuwu granules combined with acupucnture and moxibustion in treating diabetic peripheral neuropathy. J. Guangxi Univ. TCM 2018, 21, 11–13. [Google Scholar]
- Xin, Y.; Ma, D. Observation on the clinical curative effect of mongolian medicine garidi-13 weiwan in the treatment of diabetic peripheral neuropathy. J. Med. Pharm. Chin. Minorities 2018, 24, 15–16. [Google Scholar]
- Gao, S.; Tian, X.; Jinag, W.; Ma, Y. Clinical study on the treatment of 50 cases of diabetic peripheral neuropathy with shengmai powder combined with basic therapy. Jiangsu TCM 2018, 51, 28–30. [Google Scholar]
- Wu, G.; Meng, C.; Zhang, D. A randomized controlled study of acupuncture combined with taohong siwu decocotion in treating diabetic peripheral neuropathy. J. Gansu Univ. Chin. Med. 2019, 36, 64–67. [Google Scholar]
- Yi, W.; Zhang, F.; Wang, Y.; Sun, H.; Hu, Y.; Wu, S.; Liu, T. Clinical observation on 54 cases of diabetic peripheral neuropathy with phlegm and static blood syndrome treated with mongolian medicine zhenbao pills. J. Tradit. Chin. Med. 2019, 60, 42–46. [Google Scholar]
- Ji, W.; Hua, W. Efficacy of yangyin zhuyu decoction with epalrestat in the treatment of bi disease with yin deficiency and blood stasis syndrome caused by consumptive thirst. J. Changchun Univ. Chin. Med. 2019, 35, 460–463. [Google Scholar]
- Liu, L.; Bin, J.; Kong, F. Clinical observation on treating diabetic peripheral neuropathy with shengjiang san and taohong yin. Clin. J. Chin. Med. 2019, 11, 61–65. [Google Scholar]
- Liu, M. Huangqi guizhi wuwu decoction combined with western Medicine treat peripheral neuropathy in type 2 diabetes mellitus randomized parallel controlled study. J. Pract. TCIM 2019, 33, 10–12. [Google Scholar]
- Chen, J.; Zhang, Y.; Hu, C.; Feng, Z.; Liu, M.; Shi, J.; Shen, Y.; Jiang, J.; Yan, J. Clinical research on TCM directional penetration combined with zicui juanbi decoction in treating painful diabetic peripheral neuropathy. Mod. J. Integr. Trad. Chin. West Med. 2021, 30, 1844–1848. [Google Scholar]
- Hou, Y.; Guo, L.; Zhang, Y.; Li, X. Clinical study of jiuchongdan in the treatment of diabetic peripheral neuropathy. Chin. TCM Tech. 2021, 19, 9–10. [Google Scholar]
- Jin, S.; Chen, Q.; Yao, Z.; Lu, H. Clinical obseravation of shenxie zhitong capsule in treating diabetic peripheral neuroapthy of stagnant blockade of collaterals. Chin. J. Exp. Trad. Med. Formul. 2021, 27, 81–87. [Google Scholar]
- Li, Q.; Zhang, B. Exploration of the effect of Huanquizhiwuwu decoction combined with mudan granules in 41 cases of diabetic peripheral neuropathy (Qi deficiency and blood stasis syndrome). Anhui Med. Pharm. J. 2021, 25, 1052–1056. [Google Scholar]
- Wang, Y.; Tang, L.; Song, H. Clinical observation of yiqi yangyin tongluo decoction in treating diabetic peripheral neuropathy. Chin. TCM Sci. Tech. 2021, 28, 289–291. [Google Scholar]
- Wang, R. Clinical effect of taohong siwu decoction combined with mecobalamin on diabetic peripheral neuropathy. Diabetes New World 2021, 24, 181–183. [Google Scholar]
- Zhang, R.; Zhong, Y.; Zhao, L. The influence of buqi huoxue zhitong tang and A-lipoic acid in patients with diabetic peripheral neuropathy on inflammatory response and neurological function of lower extremity. Chin. Prim. Health Care 2021, 35, 92–94. [Google Scholar]
- Nishioka, M.; Shimada, M.; Kurita, N.; Iwata, T.; Morimoto, S.; Yoshikawa, K.; Higashijima, J.; Mayatani, T.; Kono, T. The Kampo medicine, Goshajinkigan, prevents neuropathy in patients treated by FOLFOX regimen. Int. J. Clin. Oncol. 2011, 16, 322–327. [Google Scholar] [CrossRef]
- Huang, J.; Lin, Q.; Qiu, Z.; Liu, H.; Huang, Y.; Liang, Y.; Tu, F. Clinical study of protective effect of yiqi wenjing yangxue huoxue recipe combined with reduced gluthathione on oxaliplatin-induced chronic neurotoxicity. Chin. J. Exp. Trad. Med. Formul. 2013, 19, 312–315. [Google Scholar]
- Abe, H.; Kawai, Y.; Mori, T.; Tomida, K.; Kubota, Y.; Umeda, T.; Tani, T. The Kampo medicine Goshajinkigan prevents neuropathy in breast cancer patients treated with docetaxel. Asian Pac. J. Cancer Prev. 2013, 14, 6351–6356. [Google Scholar] [CrossRef] [Green Version]
- Kono, T.; Hata, T.; Morita, S.; Munemoto, Y.; Matsui, T.; Kojima, H.; Takemoto, H.; Fukunaga, M.; Nagata, N.; Shimata, M.; et al. Goshajinkigan oxaliplatin neurotoxicity evaluation (GONE): A phase 2, multicenter, randomized, double-blind, placebo-controlled trial of goshajinkigan to prevent oxaliplatin-induced neuropathy. Cancer Chemother. Pharmacol. 2013, 72, 1283–1290. [Google Scholar] [CrossRef] [Green Version]
- Li, Z.; Dai, A.; Yang, H.; Li, S.; Wan, Y.; Yang, W. The random parallel control study of protective effect of rongjin fang on oxaliplatin-induced chronic neurotoxicity in treating colorectal cancer. J. Pract. TCIM 2013, 27, 46–49. [Google Scholar]
- Oki, E.; Emi, Y.; Kojima, H.; Higashijima, J.; Kato, T.; Miyake, Y.; Kon, M.; Ogata, Y.; Takahashi, K.; Ishida, H.; et al. Preventive effect of Goshajinkigan on peripheral neurotoxicity of FOLFOX therapy (GENIUS trial): A placebo-controlled, double-blind, randomized phase III study. Int. J. Clin. Oncol. 2015, 20, 767–775. [Google Scholar] [CrossRef]
- Xu, C.; Hu, X.; Xu, S. Clinical observation of modified huangqi guizhi wuwu decoction in the prevention and treatment of peripheral neurotoxicity induced by oxaliplatin. Shanghai J. TCM 2017, 51, 53–63. [Google Scholar]
- Xie, B. Effect of yiqihuoxue decoction on peripheral neuropathy caused by chemotherapy. Chin. Fore Med. Res. 2018, 16, 118–119. [Google Scholar]
- Liu, K.; Sun, T.; Xu, X.; Que, X. Clinical observation of yiqi wenyang tongluo chinese medicine combined with amifostine in preventing oxaliplatin neurotoxicityin patients with gastrointestinal cancer. Clin. J. TCM 2018, 30, 1240–1242. [Google Scholar]
- Zhang, W. Clinical analysis on tradtional chinese meidcine in preventing neurotoxicity induced by oxaliplatitn chemotherapy. CJGMCM 2018, 33, 3676–3678. [Google Scholar]
- Liu, Y.; Jiang, J.; Zhang, Q.; Jin, W.; Lan, Y.; Zhou, Z.; Fang, B. Clinical observation on “bushen huoxue method” in the preveintion of peripheral neuropathy induced by bortezomib for multiple myeloma patient. Chin. J. Gen. Pract. 2020, 18, 374–375. [Google Scholar]
- Li, J. Clinical observation on treatment of postherpetic neuralgia with jingdu tongluo decoction. J. Sichuan TCM 2016, 34, 156–157. [Google Scholar]
- Zhang, G.; Wang, X.; Wang, X. Observation on the therapeutic effect of modified chushiweiling decoction for the treatment of 30 cases of zoster neuralgia. Chin. J. Diffic. Compl. Cas. 2012, 11, 550–551. [Google Scholar]
- Zhao, L.; Yang, J. Randomized controlled observation of shugan zhuyu zhentong decoction combined with oxycodone hydrochloride sustained release tablets in the treatment of neuralgia after herpes zoster. Chin. TCM Sci. Tech. 2018, 25, 371–375. [Google Scholar]
- Gong, Q. Clinical observation on 60 cases of occipital neuralgia treated by chuanxiogng cha tiaosan combined with gabapentin capsules. Shanxi Med. J. 2021, 50, 216–218. [Google Scholar]
- Huang, Y.; Zhang, Z.; Li, C.; Xie, C.; Tan, Q.; Zhan, Q. Observation of curative effect of xiongzhi yufeng decoction on primary trigeminal neuralgia. West J. TCM 2020, 33, 110–113. [Google Scholar]
- Song, M. Clinical observation of yangxue shugan decoction in treating supraorbital neuralgia in perimenopausal women. Strait. Pharm. J. 2020, 32, 126–127. [Google Scholar]
- Zhao, J.; Li, Y.; Xin, L.; Sun, M.; Yu, C.; Shi, G.; Bao, T.; Liu, J.; Ni, Y.; Lu, R.; et al. Clinical Features and Rules of Chinese Herbal Medicine in Diabetic Peripheral Neuropathy Patients. Evid. Based Complement. Alternat. Med. 2020, 2020, 5795264. [Google Scholar] [CrossRef]
- Fu, Q.; Yang, H.; Zhang, L.; Liu, Y.; Li, X.; Dai, M.; Yang, Y.; Xie, Y.; Liu, Y.; Fu, L.; et al. Traditional Chinese medicine foot bath combined with acupoint massage for the treatment of diabetic peripheral neuropathy: A systematic review and meta-analysis of 31 RCTs. Diabetes Metab. Res. Rev. 2020, 36, e3218. [Google Scholar] [CrossRef]
- Kim, H.U.; Ryu, J.Y.; Lee, J.O.; Lee, S.Y. A systems approach to traditional oriental medicine. Nat. Biotechnol. 2015, 33, 264–268. [Google Scholar] [CrossRef] [Green Version]
- Zhou, X.; Seto, S.W.; Chang, D.; Kiat, H.; Razmovski-Naumovski, V.; Chan, K.; Bensoussan, A. Synergistic Effects of Chinese Herbal Medicine: A Comprehensive Review of Methodology and Current Research. Front. Pharmacol. 2016, 7, 201. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Hu, Y.; Tan, W.; Wu, X.; Chen, R.; Cao, J.; Chen, M.; Wang, Y. Compatibility art of traditional Chinese medicine: From the perspective of herb pairs. J. Ethnopharmacol. 2012, 143, 412–423. [Google Scholar] [CrossRef]
- Xie, G.; Peng, W.; Li, P.; Xia, Z.; Zhong, Y.; He, F.; Tulake, Y.; Feng, D.; Wang, Y.; Xing, Z.; et al. A Network Pharmacology Analysis to Explore the Effect of Astragali Radix-Radix Angelica Sinensis on Traumatic Brain Injury. BioMed Res. Int. 2018, 2018, 3951783. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.; Sun, L.; Gu, L.; Zhang, Y.; Zhao, S.; Zhao, L.-S.; Chen, X. The comparative pharmacokinetics of four bioactive ingredients after administration of Ramulus Cinnamomi-Radix Glycyrrhizae herb pair extract, Ramulus Cinnamomi extract and Radix Glycyrrhizae extract. Biomed. Chromatogr. 2016, 30, 1270–1277. [Google Scholar] [CrossRef]
- Dewanjee, S.; Das, S.; Das, A.K.; Bhattacharjee, N.; Dihingia, A.; Dua, T.K.; Kalita, J.; Manna, P. Molecular mechanism of diabetic neuropathy and its pharmacotherapeutic targets. Eur. J. Pharmacol. 2018, 833, 472–523. [Google Scholar] [CrossRef]
- Di Cesare Mannelli, L.; Pacini, A.; Micheli, L.; Femia, A.P.; Maresca, M.; Zanardelli, M.; Vannacci, A.; Gallo, E.; Bilia, A.R.; Caderni, G.; et al. Astragali radix: Could it be an adjuvant for oxaliplatin-induced neuropathy? Sci. Rep. 2017, 7, 42021. [Google Scholar] [CrossRef] [Green Version]
- Zheng, Z.; Zhao, B. Astragalus polysaccharide protects hypoxia-induced injury by up-regulation of miR-138 in rat neural stem cells. Biomed. Pharmacother. 2018, 102, 295–301. [Google Scholar] [CrossRef]
- Sun, L.; Zong, S.-B.; Li, J.-C.; Lv, Y.-Z.; Liu, L.-N.; Wang, Z.-Z.; Zhou, J.; Cao, L.; Kou, J.-P.; Xiao, W. The essential oil from the twigs of Cinnamomum cassia Presl alleviates pain and inflammation in mice. J. Ethnopharmacol. 2016, 194, 904–912. [Google Scholar] [CrossRef]
- Zheng, F.-H.; Wei, P.; Huo, H.-L.; Xing, X.-F.; Chen, F.-L.; Tan, X.-M.; Luo, J.-B. Neuroprotective effect of gui zhi (Ramulus cinnamomi) on ma huang- (Herb ephedra-) induced toxicity in rats treated with a ma huang-gui zhi herb pair. Evid. Based Complement. Alternat. Med. 2015, 2015, 913461. [Google Scholar] [CrossRef] [Green Version]
- Hou, C.; Zhang, R.; Zhang, K.; Chen, X. Total glycosides of Paeony shows Neuroprotective effects against Semen Strychni-induced neurotoxicity by recovering secretion of hormones and improving brain energy metabolism. Metab. Brain Dis. 2017, 32, 2033–2044. [Google Scholar] [CrossRef]
- Zhang, Y.; Sun, D.; Meng, Q.; Guo, W.; Chen, Q.; Zhang, Y. Calcium channels contribute to albiflorin-mediated antinociceptive effects in mouse model. Neurosci. Lett. 2016, 628, 105–109. [Google Scholar] [CrossRef]
- Park, H.R.; Lee, H.; Lee, J.-J.; Yim, N.-H.; Gu, M.-J.; Ma, J.Y. Protective Effects of Spatholobi Caulis Extract on Neuronal Damage and Focal Ischemic Stroke/Reperfusion Injury. Mol. Neurobiol. 2018, 55, 4650–4666. [Google Scholar] [CrossRef]
- Li, F.-S.; Weng, J.-K. Demystifying Traditional Herbal Medicine with Modern Approach. Nat. Plants 2017, 3, 17109. [Google Scholar] [CrossRef]
- Li, L.; Zhang, L.; Yang, C. Multi-Target Strategy and Experimental Studies of Traditional Chinese Medicine for Alzheimer’s Disease Therapy. Curr. Top. Med. Chem. 2016, 16, 537–548. [Google Scholar] [CrossRef]
- Choi, Y.; Kim, Y.-E.; Jerng, U.M.; Kim, H.; Lee, S.I.; Kim, G.-N.; Cho, S.-H.; Kang, H.W.; Jung, I.C.; Han, K.; et al. Korean Traditional Medicine in Treating Patients with Mild Cognitive Impairment: A Multicenter Prospective Observational Case Series. Evid. Based Complement. Alternat. Med. 2020, 2020, 4323989. [Google Scholar] [CrossRef]
- Chen, J.; Wang, Y.-K.; Gao, Y.; Hu, L.-S.; Yang, J.-W.; Wang, J.-R.; Sun, W.-J.; Liang, Z.-Q.; Cao, Y.-M.; Cao, Y.-B. Protection against COVID-19 Injury by Qingfei Paidu Decoction via Anti-Viral, Anti-Inflammatory Activity and Metabolic Programming. Biomed. Pharmacother. 2020, 129, 110281. [Google Scholar] [CrossRef]
- Yoon, S.W.; Jeong, J.S.; Kim, J.H.; Aggarwal, B.B. Cancer Prevention and Therapy: Integrating Traditional Korean Medicine Into Modern Cancer Care. Integr. Cancer Ther. 2014, 13, 310–331. [Google Scholar] [CrossRef] [Green Version]
- Wong, V.K.-W.; Law, B.Y.-K.; Yao, X.-J.; Chen, X.; Xu, S.W.; Liu, L.; Leung, E.L.-H. Advanced Research Technology for Discovery of New Effective Compounds from Chinese Herbal Medicine and Their Molecular Targets. Pharmacol. Res. 2016, 111, 546–555. [Google Scholar] [CrossRef]
- Lee, W.-Y.; Lee, C.-Y.; Kim, Y.-S.; Kim, C.-E. The Methodological Trends of Traditional Herbal Medicine Employing Network Pharmacology. Biomolecules 2019, 9, 362. [Google Scholar] [CrossRef] [Green Version]
- Huang, J.; Tao, G.; Liu, J.; Cai, J.; Huang, Z.; Chen, J.-X. Current Prevention of COVID-19: Natural Products and Herbal Medicine. Front. Pharmacol. 2020, 11, 588508. [Google Scholar] [CrossRef]
- Takanashi, K.; Dan, K.; Kanzaki, S.; Hasegawa, H.; Watanabe, K.; Ogawa, K. The Preventive Effect of the Traditional Japanese Herbal Medicine, Hochuekkito, against Influenza A Virus via Autophagy In Vitro. Pharmacology 2017, 99, 99–105. [Google Scholar] [CrossRef]
- Lemões, J.S.; Lemons e Silva, C.F.; Avila, S.P.F.; Montero, C.R.S.; e Silva, S.D.d.A.; Samios, D.; Peralba, M.d.C.R. Chemical Pretreatment of Arundo donax L. for Second-Generation Ethanol Production. Electron. J. Biotechnol. 2018, 31, 67–74. [Google Scholar] [CrossRef]
- Zhao, C.; Qiao, X.; Shao, Q.; Hassan, M.; Ma, Z. Evolution of the Lignin Chemical Structure during the Bioethanol Production Process and Its Inhibition to Enzymatic Hydrolysis. Energy Fuels 2020, 34, 5938–5947. [Google Scholar] [CrossRef]
- Zhang, M.; Zhao, C.; Shao, Q.; Yang, Z.; Zhang, X.; Xu, X.; Hassan, M. Determination of Water Content in Corn Stover Silage Using Near-Infrared Spectroscopy. Int. J. Agric. Biol. Eng. 2019, 12, 143–148. [Google Scholar] [CrossRef]
- Wei, H.; Liu, S.; Liao, Y.; Ma, C.; Wang, D.; Tong, J.; Feng, J.; Yi, T.; Zhu, L. A Systematic Review of the Medicinal Potential of Mulberry in Treating Diabetes Mellitus. Am. J. Chin. Med. 2018, 46, 1743–1770. [Google Scholar] [CrossRef] [Green Version]
| First Author (Year) [Reference] | Type of Condition | Trial Design | Number of Participants (Male/Female); Age (Mean ± SD) | Interventions | Morbidity Period (Mean ± SD or Range) | Outcome Index (Intergroup Differences p-Value) | Course of Treatment | Adverse Event (Case/Symptom) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Trial | Control | Trial | Control | Trial | Control | ||||||
| Jin (2004) [38] | DPN | RCT | 103(54/49) 59.4 ± 5.61 y | 99(51/48) 58.81 ± 6.01 y | Tangmaitong tablets (0.5 g × 4 t, t.i.d.) | Mecobalamin tablets (500 μg, t.i.d.) | 3.31 ± 1.25 y | 3.82 ± 1.17 y | 1. MMNCV (p > 0.05) 2. MSNCV (p < 0.01) 3. PMNCV (p < 0.05) 4. PSNCV (p < 0.01) | 8 w | Trial: 1 AE/diarrhea Control: 3 AEs/abdominal pain with diarrhea |
| Sun (2008) [39] | DPN | RCT | 30(18/12) 40–70 y | 30(16/14) 43–69 y | 1. Ziyinbushenhuoxuetonglou fang decoction (300 mL, b.i.d.) 2. Mecobalamin tablets (500 μg, t.i.d.) | Mecobalamin tablets (500 μg, t.i.d.) | 1–33 m | 1–34 m | 1. CER (p < 0.05) | 4 w | NR |
| Shen (2009) [40] | DPN | RCT | 50(21/29) 60 ± 4.2 y | 50(27/23) 58.81 ± 6.01 y | Tangmaining capsule (4.5 g × 5 c, b.i.d.) | Mecobalamin tablets (500 μg, t.i.d.) | 8.5 y | 7.9 y | 1. CER (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p < 0.05) 4. UMNCV (p < 0.01) 5. USNCV (p < 0.01) 6. PMNCV (p < 0.05) 7. PSNCV (p > 0.05) 8. TMNCV (p > 0.05) 9. TSNCV (p < 0.01) | 8 w | Trial: No AE Control: No AE |
| Lin (2010) [41] | DPN | RCT | 40(22/18) median 55.6 y | 40(23/19) median 54.2 y | 1. Tongxinluo capsule (3 c, t.i.d.) 2. Mecobalamin tablets (500 μg, t.i.d.) | Mecobalamin tablets (500 μg, t.i.d.) | NR | NR | 1. CER (p < 0.05) 2. PMNCV (p < 0.01) 3. PSNCV (p < 0.01) 4. TMNCV (p < 0.01) 5. TSNCV (p < 0.01) | 4 w | NR |
| Wang (2010) [42] | DPN | RCT | 80(45/35) 62.68 ± 7.35 y | 79(43/36) 62.78 ± 7.57 y | 1. Huangqiguizhiwuwu decoction (300 mL, b.i.d.) 2. Mecobalamin injection (0.5 mg, q.d., i.m.) | Mecobalamin injection (0.5 mg, q.d., i.m.) | 7.12 ± 4.25 y | 6.98 ± 4.62 y | 1. CER (p < 0.01) 2. MMNCV (p < 0.01) 3. MNSCV (p < 0.01) 4. PMNCV (p < 0.01) 5. PSNCV (p < 0.01) | 12 w | NR |
| Yan (2010) [43] | DPN | RCT | 14(7/7) 57.79 ± 6.73 y | 15(6/9) 52.53 ± 8.0 y | Shutangluofang granule (b.i.d.) | Methylcobalamine (500 μg, t.i.d.) | 13.14 ± 10.58 m | 10.67 ± 11.14 m | 1. CER (p < 0.05) | 12 w | NR |
| Wu (2011) [44] | DPN | RCT | 30(16/14) mean 49.9 y | 27(15/12) mean 48 y | Modified yiqihuoxue decoction (300 mL, b.i.d.) | Vitamin B1 (20 mg, t.i.d.) Vitamin B6 (20 mg, t.i.d.) | mean 12 m | mean 11.4 m | 1. CER (p < 0.01) 2. PMNCV (p < 0.01) 3. PSNCV (p < 0.01) | 6 w | NR |
| Gao (2012) [45] | DPN | RCT | 30(16/14) NR | 30(17/13) NR | 1. Nourishing the liver to stop the wind and tongluo decoction 2. Methylcobalamine (0.5 mg, t.i.d.) | Methylcobalamine (0.5 mg, t.i.d.) | NR | NR | 1. CER (p < 0.05) 2. MMNCV (p < 0.01) 3. MSNCV (p < 0.01) 4. PMNCV (p < 0.01) 5. PSNCV (p < 0.01) | 8 w | Trial: 2 AEs/nausea, upper abdominal discomfort Control: No AE |
| Gong (2013) [46] | DPN | RCT | 60(32/28) 56.42 ± 5.28 y | 60(33/27) 57.16 ± 5.34 y | 1. Modified aconite decoction (400 mL, b.i.d.) 2. Methylcobalamine (500 μg, t.i.d.) | Methylcobalamine (500 μg, t.i.d.) | 7.65 ± 3.84 m | 7.83 ± 3.29 m | 1. CER (p < 0.05) 2. PMNCV (p < 0.01) 3. PSNCV (p > 0.05) | 30 d | Trial: No AE Control: No AE |
| Han (2013) [47] | DPN | RCT | 31(17/14) 54.2 ± 9.6 y | 31(16/15) 55.3 ± 10.1 y | 1. Modified huangqiguizhiwuwu decoction (400 mL, b.i.d.) 2. Methylcobalamine (0.5 mg, t.i.d.) | Methylcobalamine (0.5 mg, t.i.d.) | NR | NR | 1. CER (p < 0.05) | 8 w | Trial: No AE Control: No AE |
| Zhang (2013a) [48] | DPN | RCT | 30(16/14) 54.32 ± 7.14 y | 30(15/15) 56.24 ± 7.40 y | 1. Mudan tong luo fang (b.i.d.) 2. α-Lipoic acid injection (600 mg, q.d., i.v. drip) | α-Lipoic acid injection (600 mg, q.d., i.v. drip) | 8.3 ± 1.67 y | 8.5 ± 1.54 y | 1. CER (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p < 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) | 3 w | NR |
| Zhang (2013b) [49] | DPN | RCT | 30 Total 60(36/14) 56 ± 8 y | 30 Total 60(36/14) 56 ± 8 y | Tang bao kang (20 pills, t.i.d.) | 1. Methylcobalamine (500 μg, t.i.d.) 2. Vitamin B1 (30 mg, t.i.d.) 3. Vitamin B6 (30 mg, t.i.d.) | Total 5–10 y | Total 5–10 y | 1. CER (p < 0.01) 2. MMNCV (p < 0.01) 3. MSNCV (p < 0.01) 4. UMNCV (p < 0.01) 5. USNCV (p < 0.01) 6. PMNCV (p < 0.01) 7. PSNCV (p < 0.01) | 24 w | Trial: No AE Control: 1 AE/skin rash |
| Guo (2014) [50] | DPN | RCT | 32(19/13) 64.78 ± 8.90 y | 32(15/17) 65.59 ± 8.35 y | 1. Modified huangqiguizhiwuwu decoction (b.i.d.) 2. Mecobalamin tablets (0.5 mg, t.i.d.) 3. Gabapentin (600 mg, t.i.d.) | 1. Mecobalamin tablets (0.5 mg, t.i.d.) 2. Gabapentin (600 mg, t.i.d.) | NR | NR | 1. CER (p < 0.01) 2. VAS (p < 0.05) | 8 w | NR |
| Yang (2014a) [51] | DPN | RCT | 60(35/25) 51.30 ± 6.03 y | 60(37/23) 51.26 ± 5.38 y | 1. Shenqixuebi feng (b.i.d.) 2. α-Lipoic acid injection (0.3 g, q.d., i.v. drip) 3. Mecobalamin injection (0.5 mg, q.d., i.v. drip) | 1. α-Lipoic acid injection (0.3 g, q.d., i.v. drip) 2. Mecobalamin injection (0.5 mg, q.d., i.v. drip) | 3.65 ± 1.12 y | 3.36 ± 1.18 y | 1. CER (p < 0.05) | 4 w | NR |
| Yang (2014b) [52] | DPN | RCT | 36(23/13) 47.8 ± 8.3 y | 36(20/16) 46.5 ± 8.1 y | 1. Modified huangqiguizhiwuwu decoction (200 mL, q.d.) 2. Methylcobalamine injection (500 μg, q.d., i.m.) | 1. Methylcobalamine injection (500 μg, q.d., i.m.) | 4.1 ± 1.3 m | 3.9 ± 1.4 m | 1. CER (p < 0.05) | 4 w | NR |
| Qi (2015) [53] | DPN | RCT | 32(17/15) 53.2 ± 7.1 y | 32(16/16) 52.4 ± 7.0 y | 1. Mudan granule (7 g, t.i.d.) 2. 0.9% Sodium chloride 200 mL and α-Lipoic acid injection (450 mg, q.d., i.v. drip) | 1. 0.9% Sodium chloride 200 mL and αLipoic acid injection (450 mg, q.d., i.v. drip) | 2.3 ± 2.1 y | 2.6 ± 1.9 y | 1. CER (p < 0.05) 2. PMNCV (p < 0.01) 3. PSNCV (p < 0.01) | 4 w | Trial: No AE Control: No AE |
| Wang (2015) [54] | DPN | RCT | 40(20/20) mean 68.5 y | 40(23/17) mean 71.2 y | 1. Yinxinshu capsule (3 c, t.i.d.) 2. Maixuekang capsule (3 c, t.i.d.) | 1. Oryzanol (20 mg, t.i.d.) 2. Vitamin B1 (10 mg, t.i.d.) 3. Adenosylcobalamin (1 mg, t.i.d.) | 10–12 y | 10–12 y | 1. CER (p < 0.05) | 4 w | Trial: No AE Control: No AE |
| Xue (2015) [55] | DPN | RCT | 42(23/19) 36–78 y | 42(22/20) 35–78 y | 1. Modified liutengshuilushexian decoction (150 mL, q.d.) | 1. Methylcobalamine tablet (0.5 mg, t.i.d.) | 28–73 d | 30–73 d | 1. CER (p < 0.01) 2. MSNCV (p < 0.01) 3. TSNCV (p < 0.01) 4. PSNCV (p < 0.01) | 3 w | Trial: No AE Control: No AE |
| Ding (2016) [56] | DPN | RCT | 30(12/18) 55.16 ± 11.78 y | 30(16/14) 54.97 ± 12.05 y | 1. Buyanghuanwu decoction (b.i.d.) 2. Methylcobalamine (0.5 mg t.i.d.) 3. Alprostadil injection (10 ug, q.d., i.v.) 4. α-Lipoic acid injection (0.3 mg, q.d., i.v. drip) | 1. Methylcobalamine (0.5 mg, t.i.d.) 2. Alprostadil injection (10 ug, q.d., i.v.) 3. α-Lipoic acid injection (0.3 mg, q.d., i.v. drip) | 7.51 ± 2.12 y | 6.59 ± 1.91 y | 1. MDNS (p < 0.05) | 8 w | NR |
| Guo (2016) [57] | DPN | RCT | 51(26/25) 69.54 ± 5.06 y | 51(28/23) 69.78 ± 5.96 y | 1. Qitengtongluo decoction (b.i.d.) 2. Epalrestat (50 mg, 1 t, t.i.d.) | 1. Epalrestat (50 mg, 1 t, t.i.d.) | 1.91 ± 2.09 y | 6.59 ± 1.91 y | 1. CER (p < 0.05) 2. NCSS (p < 0.05) 3. MSNCV (p < 0.05) 4. TSNCV (p < 0.05) 5. PMNCV (p < 0.05) 6. PSNCV (p < 0.05) | 12 w | NR |
| Han (2016) [58] | DPN | RCT | 20(12/8) 54.3 ± 7.2 y | 20(11/9) 53.7 ± 6.8 y | 1. Zhanjin tongluo chinese medicine (b.i.d.) 2. Mecobalamin tablets (500 μg, t.i.d.) | 1. Mecobalamin tablets (500 μg, t.i.d.) | 2.4 ± 1.2 y | 2.6 ± 1.3 y | 1. CER (p < 0.05) | 4 w | NR |
| Lan (2016) [59] | DPN | RCT | 54 Other information NR | 54 Other information NR | Yiqihuoxue tongluo capsule (1.2 g, t.i.d.) | Epalrestat tablets (50 mg, t.i.d.) | NR | NR | 1. CER (p < 0.05) 2. PMNCV (p < 0.05) 3. SSNCV (p < 0.05) | 12 w | Trial: No AE Control: No AE |
| Mo (2016) [60] | DPN | RCT | 33(19/14) 65.28 ± 9.098 y | 32(17/15) 62.34 ± 8.168 y | Yangyinjiedudecoction (300 mL, b.i.d.) | Methylcobalamine (0.5 mg t.i.d.) | 2–23 y | 2–19 y | 1. CER (p < 0.01) | 8 w | NR |
| Wang (2016) [61] | DPN | RCT | 124(72/52) 57.3 ± 6.8 y | 103(58/45) 58.1 ± 7.2 y | Modified tangbitong feng (150 mL, b.i.d.) | No treatment | 22.1 ± 5.4 m | 23.5 ± 4.8 m | 1. CER (p < 0.01) | 8 w | Trial: No AE Control: No AE |
| Li (2016a) [62] | DPN | RCT | 30(18/12) 49.6 ± 5.6 y | 30(17/13) 50.3 ± 5.4 y | 1. Wenyanghuoxuetongbi feng (b.i.d.) 2. Methylcobalamine (0.5 mg, t.i.d.) | 1. Methylcobalamine (0.5 mg, t.i.d.) | 18.21 ± 12.37 m | 17.97 ± 12.54 m | 1. CER (p < 0.01) 2. TSNCV (p < 0.01) 3. SSNCV (p < 0.05) 4. PSNCV (p < 0.05) | 8 w | Trial: No AE Control: No AE |
| Zhang (2016a) [63] | DPN | RCT | 48(26/22) 54.6 y | 48(28/20) 55.2 y | 1. Huangichifeng decoction combined Dangguisini decoction (q.d.) 2. Methylcobalamine injection (500 μg, q.d., i.m.) | 1. Methylcobalamine injection (500 μg, q.d., i.v.) | 2.8 y | 3.2 y | 1. CER (p < 0.01) 2. MSNCV (p < 0.01) 3. USNCV (p < 0.01) 4. PMNCV (p < 0.01) 5. TMNCV (p < 0.01) | 4 w | NR |
| Li (2016b) [64] | DPN | RCT | 60(37/23) 57 y | 60(35/25) 56 y | Huangzhitongnaoluo capsule (3 c, t.i.d.) | Mecobalamin dispersible tablets (500 mg, t.i.d.) | 1–13 y | 1–12 y | 1. CER (p < 0.05) 2. MSNCV (p < 0.05) 3. TMNCV (p < 0.05) | 12 w | NR |
| Zhang (2016b) [65] | DPN | RCT | 60(36/24) 55.3 ± 6.4 y | 60(35/25) 55.6 ± 5.5 y | 1. Qiming granule (4.5 g, t.i.d.) 2. Nimodipine injection (8 mg, q.d., i.v. drip) | 1. Nimodipine injection (8 mg, q.d., i.v. drip) | 2.0 ± 1.1 y | 2.2 ± 1.0 y | 1. CER (p < 0.01) 2. MMNCV (p < 0.01) 3. MSNCV (p < 0.01) 4. UMNCV (p < 0.05) 5. USNCV (p < 0.01) 6. TMNCV (p < 0.05) 7. TSNCV (p < 0.01) | 12 w | Trial: No AE Control: 1 AE/mild dizziness |
| Chen (2017) [66] | DPN | RCT | 30(14/16) 38.72 ± 20.02 y | 30(13/17) 39.11 ± 19.57 y | Dagguisini decoction (300 mL, b.i.d.) | Epalrestat capsule (50 mg, t.i.d.) | 4.32 ± 2.05 y | 4.20 ± 2.01 y | 1. CER (p < 0.05) 2. TCSS (p < 0.05) | 12 w | Trial: No AE Control: No AE |
| Shi (2017) [67] | DPN | RCT | 32(20/12) 38.7 ± 8.1 y | 32(22/10) 40.3 ± 10.1 y | Fufang danshen dripping pill (10 pills, t.i.d.) | 1. Methylcobalamine (0.5 mg, t.i.d.) 2. Epalrestat (50 mg, t.i.d.) | 3.87 ± 1.5 y | 3.69 ± 1.3 y | 1. TSNCV (p < 0.01) | 15 w | NR |
| Wang (2017) [68] | DPN | RCT | 30(15/15) 58.76 ± 4.32 y | 30(16/14) 57.21 ± 3.56 y | Dangguisini decoction (200 mL, b.i.d.) | Mecobalamin tablets (500 μg, t.i.d.) | 3.56 ± 1.21 y | 3.84 ± 1.36 y | 1. CER (p < 0.05) 2. MMNCV (p > 0.05) 3. MSNCV (p > 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) 6. TMNCV (p < 0.05) 7. TSNCV (p < 0.05) | 8 w | NR |
| Chen (2018) [69] | DPN | RCT | 40(19/21) 55.8 ± 4.7 y | 40(20/20) 56.2 ± 2.8 y | 1. Dangguisinin decoction (b.i.d.) 2. Mecobalamin tablets (500 μg, t.i.d.) | Mecobalamin tablets (500 μg, t.i.d.) | 3.6 ± 1.8 y | 2.4 ± 2.1 y | 1. CER (p < 0.05) | 4 w | Trial: 2 AEs/skin rash, gastrointestinal discomfort Control: 3 AEs/diarrhea (2), skin rash |
| Dai (2018) [70] | DPN | RCT | 40 45–85 y Other information NR | 40 45–85 y Other information NR | Modified huangqiguizhiwuwu decoction (500 mL, b.i.d.) | Epalrestat capsule (50 mg, t.i.d.) | NR | NR | 1. CER (p < 0.05) 2. UMNCV (p < 0.05) 3. USNCV (p < 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) | 3 w | NR |
| Hu (2018) [71] | DPN | RCT | 31(13/18) 55.45 ± 11.52 y | 31(15/16) 53.76 ± 2.03 y | 1. Modified Jiajianhuangqiguizhiwuwu decoction (200 mL, b.i.d.) 2. Methylcobalamine (0.5 mg, t.i.d.) | 1. Methylcobalamine tablet (0.5 mg, t.i.d.) | 7.13 ± 2.01 y | 6.52 ± 1.95 y | 1. CER (p < 0.05) 2. SMNCV (p < 0.05) 3. SSNCV (p < 0.05) 4. MDNS (p < 0.05) | 8 w | NR |
| Huang (2018) [72] | DPN | RCT | 120(52/68) 51.3 ± 11.4 y | 120(51/69) 50.9 ± 11.6 y | Matong powder (7 g, t.i.d.) | Methylcobalamine tablet (0.5 mg, t.i.d.) | 8.92 ± 8.6 m | 8.97 ± 8.5 m | 1. CER (p < 0.05) 2. PMNCV (p < 0.05) 3. TSNCV (p < 0.05) 4. SSNCV (p < 0.05) | 8 w | Trial: 3 AEs/ Abdominal bloating with anorexia (3) Control: 2 AEs/Abdominal bloating with anorexia (2) |
| She (2018) [73] | DPN | RCT | 30(18/12) 63.35 ± 7.12 y | 30(17/13) 65.13 ± 6.21 y | 1. Huangqiguizhiwuwu granule (b.i.d.) 2. Mecobalamin tablet (1 mg, t.i.d.) | Mecobalamin tablet (1 mg, t.i.d.) | 3.31 ± 2.06 y | 3.82 ± 1.97 y | 1. CER (p < 0.05) 2. TCSS (p < 0.05) | 6 w | NR |
| Xin (2018) [74] | DPN | RCT | 30 Total 60(36/24) 55.3 y | 30 Total 60(36/24) 55.3 y | 1. Mongolian medicine garidi-13 weiwan (3 g, q.d.) | Mecobalamin tablet (0.5 mg, t.i.d.) | Total 4.2 y | Total 4.2 y | 1. CER (p < 0.05) | 4 w | NR |
| Gao (2019) [75] | DPN | RCT | 50(26/24) 60.83 ± 5.26 y | 50(25/25) 61.17 ± 6.05 y | 1. Modified shengmaisan (300 mL, b.i.d.) 2. Mecobalamin tablet (500 μg, t.i.d.) | Mecobalamin tablet (500 μg, t.i.d.) | 3.82 ± 1.04 y | 3.77 ± 1.12 y | 1. CER (p < 0.05) 2. MDNS (p < 0.01) 2. MMNCV (p > 0.05) 3. MSNCV (p > 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) 6. TMNCV (p < 0.05) 7. TSNCV (p < 0.05) | 8 w | Trial: No AE Control: No AE |
| Wu (2019) [76] | DPN | RCT | 30(16/14) 57.60 ± 7.20 y | 30(16/14) 57.03 ± 7.63 y | Taohongsiwu decoction (t.i.d.) | Epalrestat tablet (50 mg, t.i.d.) | 4.3 y | 4.3 y | 1. CER (p < 0.05) 2. MSNCV (p < 0.05) 3. PSNCV (p < 0.05) | 4 w | Trial: No AE Control: No AE |
| Yi (2019) [77] | DPN | RCT | 60(31/29) 61.36 ± 4.37 y | 60(29/31) 61.53 ± 4.64 y | Mongolian medicine zhenbo pill (0.2 g × 15 p, b.i.d.) | α-Lipoic acid tablet (0.3 g × 2 c, q.d.) | 8.23 ± 3.21 y | 8.23 ± 3.12 y | 1. MDNS (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p < 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) | 24 w | Trial: 5 AEs/nausea (2), anorexia (3) Control: 6 AEs/ nausea (2), gastric pain (2) |
| Ji (2019) [78] | DPN | RCT | 54(32/22) 54.47 ± 9.81 y | 53(33/20) 54.81 ± 9.44 y | 1. Yangyinzhuyu decoction (150 mL, b.i.d.) 2. Epalrestat tablet (50 mg, t.i.d.) | Epalrestat tablet (50 mg, t.i.d.) | 10.24 ± 3.08 y | 10.53 ± 2.66 y | 1. CER (p < 0.05) | 90 d | Trial: No AE Control: No AE |
| Liu (2019a) [79] | DPN | RCT | 40 Other information NR | 40 Other information NR | 1. Shengjinsan combined Taohongyin (200 mL, b.i.d.) 2. Mecobalamin tablet (500 mg, t.i.d.) | Mecobalamin tablet (500 mg, t.i.d.) | NR | NR | 1. MMNCV (p < 0.05) 2. MSNCV (p < 0.05) 3. TMNCV (p < 0.05) 4. TSNCV (p < 0.05) | 4 w | NR |
| Liu (2019b) [80] | DPN | RCT | 45(27/18) 58.77 ± 4.26 y | 45(26/19) 59.46 ± 4.77 y | 1. Huangqiguizhiwuwu decoction (400 mL, b.i.d.) 2. Epalrestat tablets (t.i.d.) 3. Mecobalamin tablet (t.i.d.) | 1. Epalrestat tablets (t.i.d.) 2. Mecobalamin tablet (t.i.d.) | 3.28 ± 1.45 m | 3.31 ± 1.13 m | 1. CER (p < 0.05) | 8 w | NR |
| Chen (2021) [81] | DPN | RCT | 28(15/13) 57.2 ± 8.1 y | 29(16/13) 56.5 ± 7.6 y | 1. Zicuijuanbi decoction (150 mL, b.i.d.) 2. Normal saline injection (250 mL, i.v.) | 1. gabapentin capsule (0.3 g, t.i.d.) 2. Normal saline injection (250 mL, i.v.) | 15.57 ± 3.68 y | 14.59 ± 4.35 y | 1. VAS (p < 0.05) 2. PSNCV (p < 0.05) 3. CER (p < 0.05) | 10 w | NR |
| Hou (2021) [82] | DPN | RCT | 39(24/15) 56.74 ± 11.79 y | 28(18/10) 55.83 ± 10.60 y | Jiuchongdan (40 pills, t.i.d.) | Mecobalamin tablet (500 μg, t.i.d.) | 15.28 ± 11.23 m | 16.72 ± 10.96 m | 1. CER (p < 0.05) 2. PSNCV (p < 0.05) 3. MSNCV (p < 0.05) 4. USNCV (p < 0.05) | 12 w | NR |
| Jin (2021) [83] | DPN | RCT | 51(NR) 64.36 ± 7.08 y | 53(NR) 62.23 ± 7.32 y | Shenxiezhitoing capsule (3 c, t.i.d.) | α-Lipoic acid tablet (0.3 g × 2 t, q.d.) | 173.48 ± 84.97 m | 145.67 ± 70.68 m | 1. TCSS (p < 0.01) 2. VAS (p < 0.05) | 12 w | NR |
| Li (2021) [84] | DPN | RCT | 41(22/19) 59.81 ± 5.63 y | 41(23/18) 60.20 ± 5.62 y | 1. Huangqiguizhiwuwu decoction (200 mL, t.i.d.) combined Mudan granule (7 g, t.i.d.) 2. Mecobalamin tablet (500 mg, t.i.d.) | 1. Mecobalamin tablet (500 mg, t.i.d.) | 3.15 ± 0.45 y | 3.12 ± 0.43 y | 1. CER (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p < 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) | 8 w | Trial: 5 AEs/diarrhea (1), nausea (1), constipation (2), dizziness (1) Control: 1 AE/ nausea (1) |
| Wang (2021a) [85] | DPN | RCT | 30(16/14) 64.63 ± 4.72 y | 30(17/13) 64.71 ± 4.68 y | 1. Yiqiyangyintongluo decoction (200 mL, b.i.d.) 2. Epalrestat tablets (50 mg, t.i.d.) | 1. Epalrestat tablets (50 mg, t.i.d.) | 6.14 ± 1.24 y | 6.12 ± 1.22 y | 1. CER (p < 0.05) 2. TCSS (p < 0.05) | 12 w | NR |
| Wang (2021b) [86] | DPN | RCT | 50(34/16) 67.13 ± 6.29 y | 50(32/18) 67.13 ± 6.29 y | 1. Taohongsiwu decoction (b.i.d.) 2. Mecobalamin capsule (0.5 mg, t.i.d.) | 1. Mecobalamin capsule (0.5 mg, t.i.d.) | 1.57 ± 0.51 y | 1.42 ± 0.83 y | 1. TCSS (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p < 0.05) 4. PMNCV (p < 0.05) 5. PSNCV (p < 0.05) 6. TMNCV (p < 0.05) 7. TSNCV (p < 0.05) | 4 w | NR |
| Zhang (2021) [87] | DPN | RCT | 74 Total 148(78/70) 59.64 ± 8.94 y | 74 Total 148(78/70) 59.64 ± 8.94 y | 1. Buqizhitoing decoction (b.i.d.) 2. α-Lipoic acid injection (0.6 g, q.d.) combined 0.9% Sodium chrolide injection (250 mL, q.d.) | 1. α-Lipoic acid injection (0.6 g, q.d.) combined 0.9% Sodium chloride injection (250 mL, q.d.) | Total 9.33 ± 1.25 y | Total 9.33 ± 1.25 y | 1. TSNCV (p < 0.05) 2. PSNCV (p < 0.05) 3. TCSS (p < 0.05) 4. NRS (p < 0.05) | 8 w | NR |
| Nishioka (2011) [88] | CIPN | RCT | 22(14/8) 67(48–77) | 23(8/15) 65(52–80) | Goshajinkigan (2.5 g, t.i.d.) | No treatment | NR | NR | Incidence rate (p-value NR) | 20 course chemotherapy | Adverse events unrelated to EAHM were reported. |
| Huang (2013) [89] | CIPN | RCT | 30(17/13) 62.30 ± 8.29 y | 31(21/10) 60.00 ± 8.88 y | Yiqiwenjingyangxuehuoxue recipe (200 mL, b.i.d.) | No treatment | NR | NR | Incidence rate (p < 0.05) | 4 w | NR |
| Abe (2013) [90] | CIPN | RCT | 33(NR) median 58(35–70) | 27(NR) median 55(33–69) | Goshajinkigan (2.5 g, b.i.d. or t.i.d.) | Mecobalamin tablet (500 μg, t.i.d.) | NR | NR | Incidence rate (p < 0.01) 2. VAS (p < 0.01) | 18 w | Adverse events unrelated to EAHM were reported. |
| Kono (2013) [91] | CIPN | RCT | 44(23/21) median 67(40–88) | 45(25/20) median 61(36–82) | Goshajinkigan (2.5 g, b.i.d. or t.i.d.) | Placebo | NR | NR | Incidence rate (p-value NR) | 26 w | Adverse events unrelated to EAHM were reported. |
| Li (2013) [92] | CIPN | RCT | 30(9/21) 52.1 ± 11.50 y | 45(25/20) 54.4 ± 11.09 | Rongjin fang decoction (200 mL, b.i.d.) | Glutathione injection (1500 mg/m2, q.d., i.v. drip) | 9.1 ± 2.42m | 8.3 ± 3.02m | Incidence rate (p < 0.005) | 24 w | Adverse events unrelated to EAHM were reported. |
| Oki (2015) [93] | CIPN | RCT | 89(48/41) 62.4 ± 10.6 y | 93(51/42) 60.4 ± 11.5 y | Goshajinkigan (2.5 g, b.i.d. or t.i.d.) | Placebo | NR | NR | Incidence rate (p < 0.05) | 12 course chemotherapy | Adverse events unrelated to EAHM were reported. |
| Xu (2017) [94] | CIPN | RCT | 34(19/15) 52.4 ± 8.1 y | 34(20/14) 51.8 ± 7.6 y | Modified huangqiguizhiwuwu decoction (b.i.d.) | Mecobalamin tablet (500 μg, t.i.d.) | NR | NR | Incidence rate (p < 0.05) | 4 course chemotherapy/56d | NR |
| Xie (2018) [95] | CIPN | RCT | 30(16/14) 57.92 ± 7.33 y | 30(17/13) 58.97 ± 6.20 y | 1. Yiqihuoxue decoction (500 mL, t.i.d.) 2. Duloxetine (30 mg, t.i.d.) 3. Gabapentine (600 mg, t.i.d.) | 1. Duloxetine (30 mg, t.i.d.) 2. Gabapentine (600 mg, t.i.d.) | 27.65 ± 9.06 d | 28.16 ± 7.53 d | 1. CER (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p < 0.05) | 12 w | NR |
| Liu (2018) [96] | CIPN | RCT | 41(25/16) 62.54 ± 7.86 y | 41(22/19) 61.69 ± 8.34 y | Yiqiwenyangtougluo decoction (300 mL, b.i.d.) | Amifostine injection (500 mg/m2, i.v. drip) | NR | NR | 1. Incidence rate (p < 0.05) 2. MMNCV (p < 0.05) 3. MSNCV (p > 0.05) 4. SMNCV (p < 0.05) 5. SSNCV (p > 0.05) | 24 w | NR |
| Zhang (2018) [97] | CIPN | RCT | 40(24/16) 56.27 ± 9.22 y | 40(23/17) 56.80 ± 9.42 y | Self-prescribed herbal medicine (q.d.) | No treatment | NR | NR | Incidence rate (p < 0.05) | 4 course chemotherapy/4 w | NR |
| Liu (2020) [98] | CIPN | RCT | 40(28/12) 56.2 ± 8.4 y | 42(30/12) 52.8 ± 10.5 y | Bushenhuoxue herbal medicine (b.i.d.) | Dexamethasone injection (40 mg, i.v. drip) | NR | NR | Incidence rate (p < 0.05) | 6 course chemotherapy/18 w | NR |
| Li (2016c) [99] | PHN | RCT | 25(12/13) 58.31 ± 7.95 y | 25(13/12) 58.31 ± 8.11 y | Self-prescribed Jingdutongluo decoction (t.i.d.) | Cobamamide injection (1.5 mg, q.d., i.m.) | 7.52 ± 2.16 m | 7.58 ± 2.38 m | 1. CER (p < 0.05) 2. VAS (p < 0.05) | 4 w | NR |
| Zhang (2012) [100] | PHN | RCT | 30(16/14) median 58.32 y | 30(17/13) median 59.38 y | Modified chushiweiling decoction (b.i.d.) | 1. Vitamin B1 (10 mg, t.i.d.) 2. Mecobalamin tablet (0.5 mg, t.i.d.) | 6.8 d | 7.5 d | 1. CER (p < 0.05) 2. VAS (p < 0.05) | 4 w | Trial: No AE Control: No AE |
| Zhao (2018) [101] | PHN | RCT | 47(29/18) 48.2 ± 9.4 y | 46(24/22) 48.5 ± 9.6 y | Shuganzhuyuzhentong decoction (300 mL, b.i.d.) | 1. Calamine lotion 2. Diclofenac sodium emulsion 3. Vitamin B 4. Mecobalamin 5. Oxycodoen hydrochloride sustained release tablet (10 mg, b.i.d.) | 52.4 ± 10.9 d | 48.5 ± 9.6 d | VAS improvement rate (p < 0.05) | 4 w | Trial: 10 AEs constipation (3) nausea and vomiting (2) dizziness (2) xerostomia (2) Control: 14 AEs constipation (9) nausea and vomiting (1) dizziness (1) xerostomia(3) |
| Gong (2021) [102] | Occipital neuralgia | RCT | 30 (16/14) 42.6 ± 6.1 y | 30 (17/13) 43.2 ± 6.4 y | 1. Modified chuanxiongchadio san 2. Gabapentin capsule (0.3 g, t.i.d.) | 1. Gabapentin capsule (0.3 g, t.i.d.) | 4.2 ± 1.1 d | 4.6 ± 1.3 d | 1. CER (p < 0.05) 2. VAS (p < 0.05) | 2 w | NR |
| Huang (2020) [103] | Trigeminal neuralgia | RCT | 30 (15/15) 58.50 ± 10.72 y | 30 (9/21) 60.07 ± 13.57 y | 1. Xiongzhiyufeng decoction (b.i.d.) 2. Carbamazepine (0.1 g, b.i.d.) | 1. Carbamazepine (0.1 g, b.i.d.) | 2.95 ± 3.19 y | 2.12 ± 2.46 y | 1. CER (p < 0.05) 2. VAS (p < 0.05) | 20 d | NR |
| Song (2020) [104] | Supraorbital neuralgia | RCT | 45(NR) 52.2 ± 3.5 y | 42(NR) 50.1 ± 4.2 y | Yangxueshugan decoction (b.i.d.) | 1. Mecobalamin tablet (500 μg, t.i.d.) 2. Citicoline sodium (q.d.) | NR | NR | 1. CER (p < 0.05) | 2 w | NR |
| Author (Year) [Reference] | D1 | D2 | D3 | D4 | D5 | Overall |
|---|---|---|---|---|---|---|
| Jin (2004) [38] | Sc | H | H | L | Sc | H |
| Sun (2008) [39] | Sc | H | H | Sc | Sc | H |
| Shen (2009) [40] | L | H | H | L | Sc | H |
| Lin (2010) [41] | Sc | H | H | L | Sc | H |
| Wang (2010) [42] | L | H | H | L | Sc | H |
| Yan (2010) [43] | Sc | H | H | Sc | Sc | H |
| Wu (2011) [44] | Sc | H | H | L | Sc | H |
| Gao (2012) [45] | Sc | H | H | L | Sc | H |
| Gong (2013) [46] | Sc | H | H | L | Sc | H |
| Han (2013) [47] | L | H | H | Sc | Sc | H |
| Zhang (2013a) [48] | L | H | H | L | Sc | H |
| Zhang (2013b) [49] | Sc | H | H | L | Sc | H |
| Guo (2014) [50] | Sc | H | H | Sc | Sc | H |
| Yang (2014a) [51] | Sc | H | H | Sc | Sc | H |
| Yang (2014b) [52] | L | H | H | Sc | Sc | H |
| Qi (2015) [53] | Sc | H | H | L | Sc | H |
| Wang (2015) [54] | Sc | H | H | Sc | Sc | H |
| Xue (2015) [55] | L | H | H | L | Sc | H |
| Ding (2016) [56] | Sc | H | H | L | Sc | H |
| Guo (2016) [57] | L | H | H | L | Sc | H |
| Han (2016) [58] | Sc | H | H | L | Sc | H |
| Lan (2016) [59] | H | H | H | L | Sc | H |
| Mo (2016) [60] | L | H | H | Sc | Sc | H |
| Wang (2016) [61] | L | H | H | Sc | Sc | H |
| Li (2016a) [62] | L | H | H | L | Sc | H |
| Zhang (2016a) [63] | L | H | H | L | Sc | H |
| Li (2016b) [64] | Sc | H | H | L | Sc | H |
| Zhang (2016b) [65] | L | H | H | L | Sc | H |
| Chen (2017) [66] | L | H | H | L | Sc | H |
| Shi (2017) [67] | Sc | H | H | L | Sc | H |
| Wang (2017) [68] | L | H | H | L | Sc | H |
| Chen (2018) [69] | L | H | H | Sc | Sc | H |
| Dai (2018) [70] | H | H | H | L | Sc | H |
| Hu (2018) [71] | Sc | H | H | L | Sc | H |
| Huang (2018) [72] | L | H | H | L | Sc | H |
| She (2018) [73] | L | H | H | L | Sc | H |
| Xin (2018) [74] | H | H | H | Sc | Sc | H |
| Gao (2019) [75] | Sc | H | H | L | Sc | H |
| Wu (2019) [76] | L | H | H | L | Sc | H |
| Yi (2019) [77] | L | H | H | L | Sc | H |
| Ji (2019) [78] | L | H | H | Sc | Sc | H |
| Liu (2019a) [79] | Sc | H | H | L | Sc | H |
| Liu (2019b) [80] | Sc | H | H | Sc | Sc | H |
| Chen (2021) [81] | Sc | H | Sc | L | Sc | H |
| Hou (2021) [82] | Sc | H | H | L | Sc | H |
| Jin (2021) [83] | L | H | Sc | L | Sc | H |
| Li (2021) [84] | L | H | H | L | Sc | H |
| Wang (2021a) [85] | L | H | H | L | Sc | H |
| Wang (2021b) [86] | L | H | H | L | Sc | H |
| Zhang (2021) [87] | H | H | H | L | Sc | H |
| Nishioka (2011) [88] | L | L | L | L | L | L |
| Huang (2013) [89] | L | H | Sc | L | Sc | H |
| Abe (2013) [90] | L | L | L | L | L | L |
| Kono (2013) [91] | L | L | L | L | L | L |
| Li (2013) [92] | L | H | H | L | Sc | H |
| Oki (2015) [93] | L | L | L | L | L | L |
| Xu (2017) [94] | Sc | H | H | L | Sc | H |
| Xie (2018) [95] | L | H | H | L | Sc | H |
| Liu (2018) [96] | L | H | H | L | Sc | H |
| Zhang (2018) [97] | Sc | H | H | L | Sc | H |
| Liu (2020) [98] | Sc | H | H | L | Sc | H |
| Li (2016c) [99] | L | H | H | L | Sc | H |
| Zhang (2012) [100] | Sc | H | H | L | Sc | H |
| Zhao (2018) [101] | L | H | H | Sc | Sc | H |
| Gong (2021) [102] | Sc | H | H | L | Sc | H |
| Huang (2020) [103] | Sc | H | H | L | Sc | H |
| Song (2020) [104] | H | H | H | Sc | Sc | H |
| Intervention and Comparator | Outcomes | Subgroup Analysis | Number of Participants (Studies) | Mean Difference (95% CI) | Heterogeneity | ||
|---|---|---|---|---|---|---|---|
| I2, % | p | ||||||
| EAHM in combination with the other treatment vs. active control | MSNCV | Main analysis | 1333(14) | 2.73 (1.80 to 3.66) | 86% | p < 0.01 | |
| Patient types | DPN | 1191(12) | 2.80 (1.83 to 3.78) | 85% | p < 0.01 | ||
| CIPN | 142(2) | 2.27 (−1.93 to 6.48) | 95% | p < 0.01 | |||
| Duration of treatment | ≤4 weeks | 635(6) | 3.01 (1.20 to 4.82) | 93% | p < 0.01 | ||
| >4 weeks, ≤11 weeks | 302(4) | 2.31 (1.05 to 3.56) | 73% | p = 0.01 | |||
| >11 weeks | 396(4) | 2.81 (0.84 to 4.78) | 74% | p < 0.01 | |||
| PSNCV | Main analysis | 1329(14) | 2.59 (1.65 to 3.53) | 88% | p < 0.01 | ||
| Patient types | DPN | 1247(13) | 2.79 (1.81 to 3.76) | 88% | p < 0.01 | ||
| CIPN | 82(1) | 0.35 (−0.66 to 1.36) | - | - | |||
| Duration of treatment | ≤4 weeks | 364(4) | 3.02 (2.29 to 3.76) | 0% | p = 0.57 | ||
| >4 weeks, ≤11 weeks | 235(3) | 2.64 (0.10 to 5.19) | 95% | p < 0.01 | |||
| >11 weeks | 630(7) | 2.49 (1.09 to 3.89) | 89% | p < 0.01 | |||
| TSNCV | Main analysis | 1214(11) | 3.59 (2.79 to 4.39) | 81% | p < 0.01 | ||
| Patient types | Only DPN | - | - | - | - | ||
| Duration of treatment | ≤4 weeks | 440(4) | 4.60 (2.38 to 6.82) | 85% | p < 0.01 | ||
| >4 weeks, ≤11 weeks | 166(2) | 2.13 (1.62 to 2.63) | 0% | p = 0.73 | |||
| >11 weeks | 608(5) | 3.72 (3.11 to 4.32) | 33% | p = 0.20 | |||
| MMNCV | Main analysis | 980(10) | 3.31 (1.96 to 4.65) | 88% | p < 0.01 | ||
| Patient types | DPN | 828(8) | 3.49 (2.10 to 4.89) | 84% | p < 0.01 | ||
| CIPN | 142(2) | 2.64 (−2.26 to 7.54) | 97% | p < 0.01 | |||
| Duration of treatment | >11 weeks | 528(5) | 4.21 (2.18 to 6.24) | 92% | p < 0.01 | ||
| >4 weeks, ≤11 weeks | 142(2) | 1.88 (0.78 to 2.98) | 0% | p = 0.61 | |||
| ≤4 weeks | 300(3) | 2.68 (1.51 to 3.85) | 9% | p = 0.33 | |||
| PMNCV | Main analysis | 1234(13) | 2.98 (2.12 to 3.85) | 81% | p < 0.01 | ||
| Patient types | DPN | 1152(12) | 3.22 (2.43 to 4.01) | 73% | p < 0.01 | ||
| CIPN | 82(1) | 0.35 (−0.66 to 1.36) | - | - | |||
| Duration of treatment | ≤4 weeks | 460(5) | 4.42 (3.51 to 5.33) | 29% | p = 0.23 | ||
| >4 weeks, ≤11 weeks | 450(4) | 1.91 (0.79 to 3.02) | 75% | p < 0.01 | |||
| >11 weeks | 324(4) | 2.48 (1.29 to 3.68) | 63% | p = 0.04 | |||
| EAHM monotherapy vs. active control | MSNCV | Main analysis | 681(7) | 2.74 (1.38 to 4.10) | 89% | p < 0.01 | |
| Patient types | Only DPN | - | - | - | - | ||
| Duration of treatment | ≤4 weeks | 144(2) | 2.46 (−0.47 to 5.39) | 96% | p < 0.01 | ||
| >4 weeks, ≤11 weeks | 303(2) | 3.72 (−0.15 to 7.59) | 95% | p < 0.01 | |||
| >11 weeks | 234(3) | 2.23 (0.75 to 3.71) | 25% | p = 0.26 | |||
| PSNCV | Main analysis | 883(10) | 2.76 (1.67 to 3.85) | 85% | |||
| Patient types | Only DPN | - | - | - | - | ||
| Duration of treatment | ≤4 weeks | 224(3) | 3.46 (2.04 to 4.88) | 77% | p = 0.01 | ||
| >4 weeks, ≤11 weeks | 425(4) | 2.23 (0.09 to 4.38) | 89% | p < 0.01 | |||
| >11 weeks | 234(3) | 2.73 (0.45 to 5.02) | 73% | p = 0.02 | |||
| PMNCV | Main analysis | 967(9) | 2.47 (1.40 to 3.53) | 75% | p < 0.01 | ||
| Patient types | Only DPN | - | - | - | - | ||
| Duration of treatment | ≤4 weeks | 80(1) | 3.61 (1.43 to 5.79) | - | - | ||
| >4 weeks, ≤11 weeks | 725(6) | 2.37 (0.91 to 3.83) | 83% | p < 0.01 | |||
| >11 weeks | 162(2) | 2.40 (0.85 to 3.96) | 35% | p = 0.21 | |||
| EAHM (Latin Name) | Frequency of Utilization | Relative Frequency (%) | Cumulative Percentiles (%) |
|---|---|---|---|
| Astragali Radix | 42 | 6.27 | 6.27 |
| Angelicae Gigantis Radix | 33 | 4.93 | 11.20 |
| Paeoniae Radix | 33 | 4.93 | 16.13 |
| Cnidii Rhizoma | 29 | 4.33 | 20.46 |
| Cinnamomi Ramulus | 28 | 4.18 | 24.64 |
| Spatholobi Caulis | 24 | 3.58 | 28.22 |
| Achyranthis Radix | 20 | 2.99 | 31.21 |
| Glycyrrhyziae Radix et Rhizoma | 20 | 2.99 | 34.20 |
| Salviae Miltiorrhizae Radix | 20 | 2.99 | 37.19 |
| Carthami Flos | 18 | 2.69 | 39.88 |
| No. | Associations Rules | Support | Confidence | Lift |
|---|---|---|---|---|
| 1 | {Glycyrrhizae Radix et Rhizoma} => {Astragali Radix} | 0.239 | 0.800 | 1.276 |
| 2 | {Spatholobi Caulis} => {Astragali Radix} | 0.313 | 0.875 | 1.396 |
| 3 | {Cinnamomi Ramulus} => {Astragali Radix} | 0.373 | 0.893 | 1.424 |
| 4 | {Cinnamomi Ramulus, Spatholobi Caulis} => {Astragali Radix} | 0.254 | 0.944 | 1.507 |
| 5 | {Astragali Radix, Spatholobi Caulis} => {Cinnamomi Ramulus} | 0.254 | 0.810 | 1.937 |
| 6 | {Angelicae Gigantis Radix, Cinnamomi Ramulus} => {Paeoniae Radix} | 0.224 | 0.882 | 1.791 |
| 7 | {Cinnamomi Ramulus, Paeoniae Radix} => {Astragali Radix} | 0.284 | 0.864 | 1.378 |
| 8 | {Angelicae Gigantis Radix, Cinnamomi Ramulus} => {Astragali Radix} | 0.209 | 0.824 | 1.314 |
| 9 | {Cnidii Rhizoma, Paeoniae Radix} => {Angelicae Gigantis Radix} | 0.239 | 0.842 | 1.710 |
| Intervention and Comparator Intervention | Outcomes | Number of Participants (Studies) | Anticipated Absolute of Relative Effects (95% CI) | Quality of the Evidence (GRADE) |
|---|---|---|---|---|
| EAHM combination of WM compared to WM for peripheral neuropathy | SNCV | 4454 (21 RCTs) | MD 3.06 higher (2.56 higher to 3.56 higher) | ⨁⨁⨁◯ MODERATE |
| MNCV | 2860 (16 RCTs) | MD 3.23 higher (2.58 higher to 3.88 higher) | ⨁⨁⨁◯ MODERATE | |
| Response rate | 1997 (25 RCTs) | RR 1.20 (1.15 to 1.25) | ⨁⨁⨁◯ MODERATE | |
| Incidence rate | 232 (3 RCTs) | OR 0.12 (0.03 to 0.59) | ⨁⨁◯◯ LOW | |
| Pain intensity | 332 (4 RCTs) | SMD 1.21 SD lower (1.29 lower to 0.83 lower) | ⨁⨁⨁◯ MODERATE | |
| TCSS | 470 (4 RCTs) | MD 1.83 lower (2.11 lower to 1.55 lower) | ⨁⨁◯◯ LOW | |
| MDNS | 122 (2 RCTs) | MD 2.21 lower (2.94 lower to 1.47 lower) | ⨁⨁◯◯ LOW | |
| EAHM monotherapy compared WM for peripheral neuropathy | SNCV | 2159 (10 RCTs) | MD 2.68 higher (2.02 higher to 3.35 higher) | ⨁⨁⨁◯ MODERATE |
| MNCV | 1788 (9 RCTs) | MD 2.38 higher (1.43 higher to 3.32 higher) | ⨁⨁⨁◯ MODERATE | |
| Response rate | 1651 (21 RCTs) | RR 1.30 (1.20 to 1.29) | ⨁⨁◯◯ LOW | |
| Incidence rate | 249 (4 RCTs) | OR 0.17 (0.07 to 0.38) | ⨁⨁◯◯ LOW | |
| Pain intensity | 294 (4 RCTs) | SMD 0.94 SD lower (1.18 lower to 0.69 lower) | ⨁⨁⨁◯ MODERATE | |
| TCSS | 187 (3 RCTs) | MD 1.04 lower (1.75 lower to 0.34 lower) | ⨁⨁◯◯ LOW | |
| MDNS | 207 (2 RCTs) | MD 2.95 lower (4.2 lower to 1.7 lower) | ⨁⨁◯◯ LOW |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jo, H.-G.; Lee, D. Oral Administration of East Asian Herbal Medicine for Peripheral Neuropathy: A Systematic Review and Meta-Analysis with Association Rule Analysis to Identify Core Herb Combinations. Pharmaceuticals 2021, 14, 1202. https://doi.org/10.3390/ph14111202
Jo H-G, Lee D. Oral Administration of East Asian Herbal Medicine for Peripheral Neuropathy: A Systematic Review and Meta-Analysis with Association Rule Analysis to Identify Core Herb Combinations. Pharmaceuticals. 2021; 14(11):1202. https://doi.org/10.3390/ph14111202
Chicago/Turabian StyleJo, Hee-Geun, and Donghun Lee. 2021. "Oral Administration of East Asian Herbal Medicine for Peripheral Neuropathy: A Systematic Review and Meta-Analysis with Association Rule Analysis to Identify Core Herb Combinations" Pharmaceuticals 14, no. 11: 1202. https://doi.org/10.3390/ph14111202
APA StyleJo, H.-G., & Lee, D. (2021). Oral Administration of East Asian Herbal Medicine for Peripheral Neuropathy: A Systematic Review and Meta-Analysis with Association Rule Analysis to Identify Core Herb Combinations. Pharmaceuticals, 14(11), 1202. https://doi.org/10.3390/ph14111202







