The Antiarrhythmic Activity of Novel Pyrrolidin-2-one Derivative S-75 in Adrenaline-Induced Arrhythmia
Abstract
1. Introduction
2. Results
2.1. S-75 Showed Low Affinity toward Sodium, Potassium, and Calcium Channels
2.2. S-75 Prolonged the PQ and Decreased Heart Rate in the Normal ECG in Rats
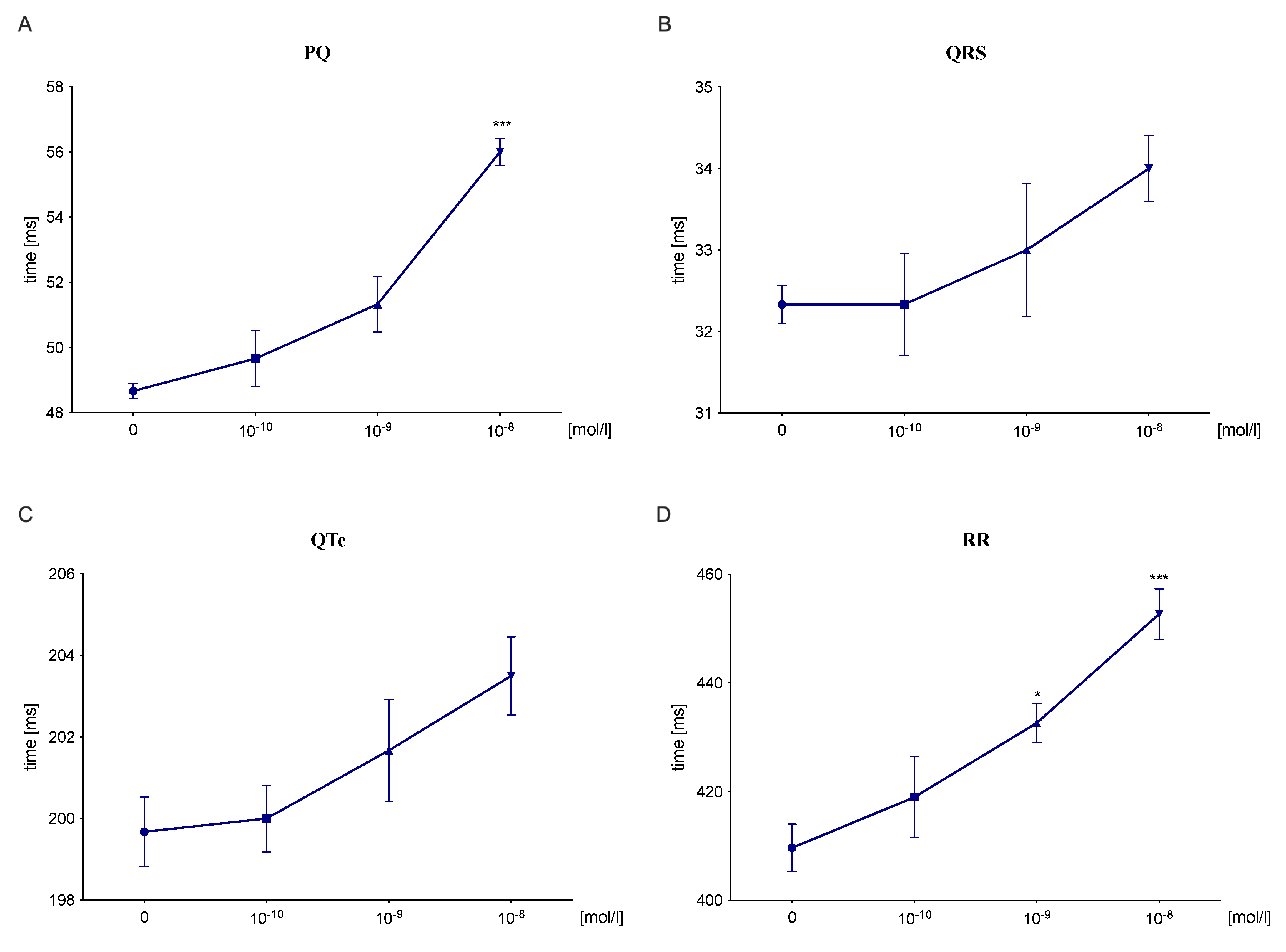
2.3. S-75 Prolonged the PQ and RR Interval in an Isolated Rat’s Heart
2.4. S-75 Showed Prophylactic Antiarrhythmic Properties in Arrythmia Models Caused by Adrenaline, but Not Calcium Chloride and Aconitine
2.5. S-75 Did Not Possess the Antiarrhythmic Activity in the Post-Reperfusion Model in Isolated Rat Heart
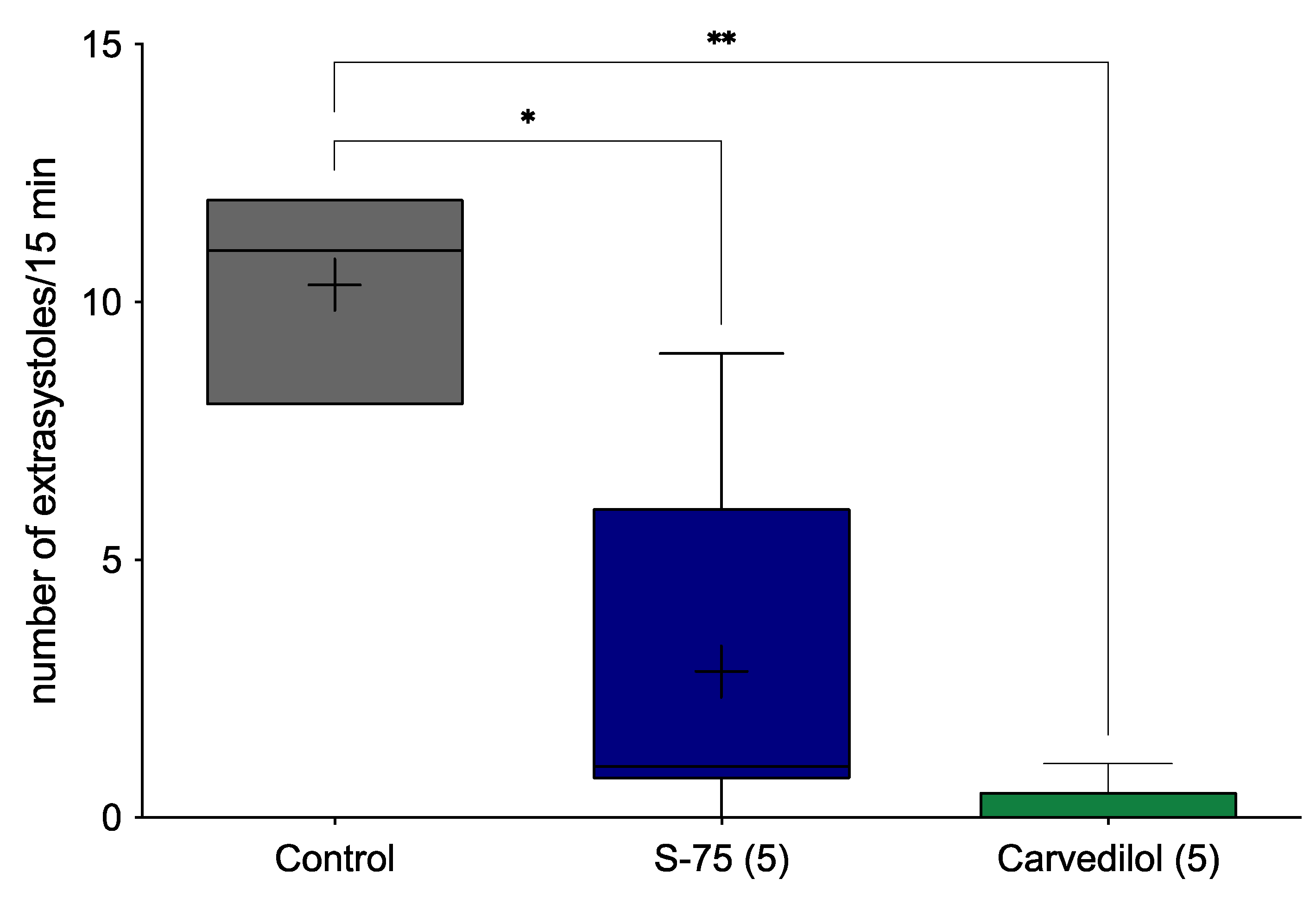
2.6. S-75 Showed Therapeutic Antiarrhythmic Properties in Adrenaline-Induced Arrythmia Model
3. Discussion
4. Materials and Methods
4.1. Drugs
4.2. Animals
4.3. Affinity for β1-Adrenergic Receptors
4.4. Effect on Sodium, Potassium, and Calcium Channels
4.5. Effect on Normal Electrocardiogram in Rats
4.6. Effect on Normal ECG of Isolated Rat Heart
4.7. Prophylactic Antiarrhythmic Activity in Adrenaline-, Aconitine-, and Calcium Chloride-Induced Arrhythmias
4.8. Antiarrhythmic Activity in the Post-Reperfusion Model in Isolated Rat Heart
- occurrence of less than 10 extrasystoles—1 point;
- occurrence of more than 10 extrasystoles—2 points;
- presence of ventricular tachycardia—3 points;
- presence of fibrillation—4 points.
4.9. Therapeutic Antiarrhythmic Activity in Adrenaline-Induced Arrhythmia
4.10. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Cardiovascular Diseases. Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 26 August 2021).
- Institute of Medicine (US) Committee on Social Security. Cardiovascular Disability Criteria, D. Arrhythmias. In Cardiovascular Disability: Updating the Social Security Listings; National Academies Press (US): Washington, DC, USA, 2010; ISBN 978-0-309-15698-1. [Google Scholar]
- Feld, G.K.; Chen, P.S.; Nicod, P.; Fleck, R.P.; Meyer, D. Possible atrial proarrhythmic effects of class 1C antiarrhythmic drugs. Am. J. Cardiol. 1990, 66, 378–383. [Google Scholar] [CrossRef]
- Wang, D.; Patel, C.; Cui, C.; Yan, G.-X. Preclinical assessment of drug-induced proarrhythmias: Role of the arterially perfused rabbit left ventricular wedge preparation. Pharmacol. Ther. 2008, 119, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Cardiac Arrhythmia Suppression Trial (CAST) Investigators. Preliminary report: Effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N. Engl. J. Med. 1989, 321, 406–412. [Google Scholar] [CrossRef] [PubMed]
- Naccarelli, G.V.; Wolbrette, D.L.; Khan, M.; Bhatta, L.; Hynes, J.; Samii, S.; Luck, J. Old and new antiarrhythmic drugs for converting and maintaining sinus rhythm in atrial fibrillation: Comparative efficacy and results of trials. Am. J. Cardiol. 2003, 91, 15D–26D. [Google Scholar] [CrossRef]
- Gillis, A.M. Effects of antiarrhythmic drugs on QT interval dispersion--relationship to antiarrhythmic action and proarrhythmia. Prog. Cardiovasc. Dis. 2000, 42, 385–396. [Google Scholar] [CrossRef]
- Jaszczyszyn, E.; Panaszek, B. Podstawy elektrofizjologiczne, przyczyny i klasyfikacja zaburzeń rytmu serca—Implikacje rokownicze i terapeutyczne. Fam. Med. Prim. Care Rev. 2013, 15, 573–579. [Google Scholar]
- O’Connell, T.D.; Jensen, B.C.; Baker, A.J.; Simpson, P.C. Cardiac alpha1-adrenergic receptors: Novel aspects of expression, signaling mechanisms, physiologic function, and clinical importance. Pharmacol. Rev. 2014, 66, 308–333. [Google Scholar] [CrossRef]
- Ikeda, U.; Tsuruya, Y.; Yaginuma, T. Alpha 1-adrenergic stimulation is coupled to cardiac myocyte hypertrophy. Am. J. Physiol. 1991, 260, H953-6. [Google Scholar] [CrossRef]
- Fuller, S.J.; Gaitanaki, C.J.; Sugden, P.H. Effects of catecholamines on protein synthesis in cardiac myocytes and perfused hearts isolated from adult rats. Stimulation of translation is mediated through the alpha 1-adrenoceptor. Biochem. J. 1990, 266, 727–736. [Google Scholar] [CrossRef]
- Simpson, P. Stimulation of hypertrophy of cultured neonatal rat heart cells through an alpha 1-adrenergic receptor and induction of beating through an alpha 1- and beta 1-adrenergic receptor interaction. Evidence for independent regulation of growth and beating. Circ. Res. 1985, 56, 884–894. [Google Scholar] [CrossRef]
- Simpson, P. Norepinephrine-stimulated hypertrophy of cultured rat myocardial cells is an alpha 1 adrenergic response. J. Clin. Investig. 1983, 72, 732–738. [Google Scholar] [CrossRef]
- Simpson, P.; McGrath, A.; Savion, S. Myocyte hypertrophy in neonatal rat heart cultures and its regulation by serum and by catecholamines. Circ. Res. 1982, 51, 787–801. [Google Scholar] [CrossRef]
- Milano, C.A.; Dolber, P.C.; Rockman, H.A.; Bond, R.A.; Venable, M.E.; Allen, L.F.; Lefkowitz, R.J. Myocardial expression of a constitutively active alpha 1B-adrenergic receptor in transgenic mice induces cardiac hypertrophy. Proc. Natl. Acad. Sci. USA 1994, 91, 10109–10113. [Google Scholar] [CrossRef]
- O’Connell, T.D.; Ishizaka, S.; Nakamura, A.; Swigart, P.M.; Rodrigo, M.C.; Simpson, G.L.; Cotecchia, S.; Rokosh, D.G.; Grossman, W.; Foster, E.; et al. The alpha(1A/C)- and alpha(1B)-adrenergic receptors are required for physiological cardiac hypertrophy in the double-knockout mouse. J. Clin. Investig. 2003, 111, 1783–1791. [Google Scholar] [CrossRef]
- Papay, R.S.; Shi, T.; Piascik, M.T.; Naga Prasad, S.V.; Perez, D.M. α₁A-adrenergic receptors regulate cardiac hypertrophy in vivo through interleukin-6 secretion. Mol. Pharmacol. 2013, 83, 939–948. [Google Scholar] [CrossRef] [PubMed]
- Chaulet, H.; Lin, F.; Guo, J.; Owens, W.A.; Michalicek, J.; Kesteven, S.H.; Guan, Z.; Prall, O.W.; Mearns, B.M.; Feneley, M.P.; et al. Sustained augmentation of cardiac alpha1A-adrenergic drive results in pathological remodeling with contractile dysfunction, progressive fibrosis and reactivation of matricellular protein genes. J. Mol. Cell. Cardiol. 2006, 40, 540–552. [Google Scholar] [CrossRef] [PubMed]
- Du, X.-J.; Gao, X.-M.; Kiriazis, H.; Moore, X.-L.; Ming, Z.; Su, Y.; Finch, A.M.; Hannan, R.A.; Dart, A.M.; Graham, R.M. Transgenic alpha1A-adrenergic activation limits post-infarct ventricular remodeling and dysfunction and improves survival. Cardiovasc. Res. 2006, 71, 735–743. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, Y.; Wright, C.D.; Merkwan, C.L.; Baye, N.L.; Liang, Q.; Simpson, P.C.; O’Connell, T.D. An alpha1A-adrenergic-extracellular signal-regulated kinase survival signaling pathway in cardiac myocytes. Circulation 2007, 115, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; McElwee-Witmer, S.; Perrone, M.; Clark, K.L.; Zilberstein, A. Phenylephrine protects neonatal rat cardiomyocytes from hypoxia and serum deprivation-induced apoptosis. Cell Death Differ. 2000, 7, 773–784. [Google Scholar] [CrossRef][Green Version]
- Terzic, A.; Pucéat, M.; Clément, O.; Scamps, F.; Vassort, G. Alpha 1-adrenergic effects on intracellular pH and calcium and on myofilaments in single rat cardiac cells. J. Physiol. 1992, 447, 275–292. [Google Scholar] [CrossRef]
- Hirano, S.; Kusakari, Y.; O-Uchi, J.; Morimoto, S.; Kawai, M.; Hongo, K.; Kurihara, S. Intracellular mechanism of the negative inotropic effect induced by alpha1-adrenoceptor stimulation in mouse myocardium. J. Physiol. Sci. 2006, 56, 297–304. [Google Scholar] [CrossRef]
- Lin, F.; Owens, W.A.; Chen, S.; Stevens, M.E.; Kesteven, S.; Arthur, J.F.; Woodcock, E.A.; Feneley, M.P.; Graham, R.M. Targeted alpha(1A)-adrenergic receptor overexpression induces enhanced cardiac contractility but not hypertrophy. Circ. Res. 2001, 89, 343–350. [Google Scholar] [CrossRef]
- Kitakaze, M.; Hori, M.; Sato, H.; Iwakura, K.; Gotoh, K.; Inoue, M.; Kitabatake, A.; Kamada, T. Beneficial effects of alpha 1-adrenoceptor activity on myocardial stunning in dogs. Circ. Res. 1991, 68, 1322–1339. [Google Scholar] [CrossRef]
- Kitakaze, M.; Hori, M.; Morioka, T.; Minamino, T.; Takashima, S.; Sato, H.; Shinozaki, Y.; Chujo, M.; Mori, H.; Inoue, M. Alpha 1-adrenoceptor activation mediates the infarct size-limiting effect of ischemic preconditioning through augmentation of 5′-nucleotidase activity. J. Clin. Investig. 1994, 93, 2197–2205. [Google Scholar] [CrossRef]
- Tsuchida, A.; Liu, Y.; Liu, G.S.; Cohen, M.V.; Downey, J.M. alpha 1-adrenergic agonists precondition rabbit ischemic myocardium independent of adenosine by direct activation of protein kinase C. Circ. Res. 1994, 75, 576–585. [Google Scholar] [CrossRef]
- Bankwala, Z.; Hale, S.L.; Kloner, R.A. Alpha-adrenoceptor stimulation with exogenous norepinephrine or release of endogenous catecholamines mimics ischemic preconditioning. Circulation 1994, 90, 1023–1028. [Google Scholar] [CrossRef]
- Heusch, G. Alpha-adrenergic mechanisms in myocardial ischemia. Circulation 1990, 81, 1–13. [Google Scholar] [CrossRef]
- Corr, P.B.; Witkowski, F.X. Arrhythmias associated with reperfusion: Basic insights and clinical relevance. J. Cardiovasc. Pharmacol. 1984, 6 (Suppl. S6), S903–S909. [Google Scholar] [CrossRef] [PubMed]
- Lamontagne, D.; Yamaguchi, N.; Nadeau, R.; De Champlain, J.; Godin, D.; Campeau, N. Effects of sotalol, (-)-propranolol and prazosin on reperfusion-induced arrhythmias and increased cardiac norepinephrine release. Eur. J. Pharmacol. 1986, 123, 1–10. [Google Scholar] [CrossRef]
- Colucci, W.S. Alpha-adrenergic receptor blockade with prazosin. Consideration of hypertension, heart failure, and potential new applications. Ann. Intern. Med. 1982, 97, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Tölg, R.; Kurz, T.; Ungerer, M.; Schreieck, J.; Görge, B.; Richardt, G. Influence of alpha- and beta-adrenoceptor antagonists on ventricular fibrillation in ischemic rat hearts. Naunyn Schmiedebergs Arch. Pharmacol. 1997, 356, 62–68. [Google Scholar] [CrossRef]
- Bralet, J.; Didier, J.; Moreau, D.; Opie, L.H.; Rochette, L. Effect of alpha-adrenoceptor antagonists (phentolamine, nicergoline and prazosin) on reperfusion arrhythmias and noradrenaline release in perfused rat heart. Br. J. Pharmacol. 1985, 84, 9–18. [Google Scholar]
- Bernauer, W.; Ernenputsch, I. Antagonistic effects of alpha-adrenoceptor blocking agents on arrhythmias, enzyme release, and myocardial necrosis in isolated rat hearts with coronary occlusion and reperfusion. Naunyn Schmiedebergs Arch. Pharmacol. 1988, 338, 88–95. [Google Scholar] [CrossRef]
- Kubacka, M.; Mogilski, S.; Filipek, B.; Marona, H. Antiarrhythmic properties of some 1,4-disubstituted piperazine derivatives with α1-adrenoceptor affinities. Eur. J. Pharmacol. 2013, 720, 237–246. [Google Scholar] [CrossRef]
- Kubacka, M.; Szkaradek, N.; Mogilski, S.; Pańczyk, K.; Siwek, A.; Gryboś, A.; Filipek, B.; Żmudzki, P.; Marona, H.; Waszkielewicz, A.M. Design, synthesis and cardiovascular evaluation of some aminoisopropanoloxy derivatives of xanthone. Bioorgan. Med. Chem. 2018, 26, 3773–3784. [Google Scholar] [CrossRef]
- Handzlik, J.; Bajda, M.; Zygmunt, M.; MacIg, D.; Dybała, M.; Bednarski, M.; Filipek, B.; Malawska, B.; Kieć-Kononowicz, K. Antiarrhythmic properties of phenylpiperazine derivatives of phenytoin with α 1-adrenoceptor affinities. Bioorgan. Med. Chem. 2012, 20, 2290–2303. [Google Scholar] [CrossRef]
- Sapa, J.; Nowaczyk, A.; Kulig, K. Antiarrhythmic and antioxidant activity of novel pyrrolidin-2-one derivatives with adrenolytic properties. Naunyn Schmiedebergs Arch. Pharmacol. 2011, 383, 13–25. [Google Scholar] [CrossRef]
- Malawska, B.; Kulig, K.; Filipek, B.; Sapa, J.; Macia̧g, D.; Zygmunt, M.; Antkiewicz-Michaluk, L. Synthesis, antiarrhythmic, and antihypertensive effects of novel 1-substituted pyrrolidin-2-one and pyrrolidine derivatives with adrenolytic activity. Eur. J. Med. Chem. 2002, 37, 183–195. [Google Scholar] [CrossRef]
- Malawska, B.; Kulig, K.; Gippert, A.; Filipek, B.; Sapa, J.; Maciag, D. Synthesis and development of new 2-substituted 1-[3-(4-arylpiperazin-1-yl)propyl]-pyrrolidin-2-one derivatives with antiarrhythmic, hypotensive, and alpha-adrenolytic activity. Farmaco 2005, 60, 793–803. [Google Scholar] [CrossRef] [PubMed]
- Kulig, K.; Sapa, J.; Maciag, D.; Filipek, B.; Malawska, B. Synthesis and pharmacological evaluation of new 1-[3-(4-arylpiperazin-1-yl)-2-hydroxypropyl]-pyrrolidin-2-one derivatives with anti-arrhythmic, hypotensive, and alpha-adrenolytic activity. Arch. Pharm. Weinh. 2007, 340, 466–475. [Google Scholar] [CrossRef] [PubMed]
- Kulig, K.; Sapa, J.; Nowaczyk, A.; Filipek, B.; Malawska, B. Design, synthesis and pharmacological evaluation of new 1-[3-(4-arylpiperazin-1-yl)-2-hydroxy-propyl]-3,3-diphenylpyrrolidin-2-one derivatives with antiarrhythmic, antihypertensive, and alpha-adrenolytic activity. Eur. J. Med. Chem. 2009, 44, 3994–4003. [Google Scholar] [CrossRef]
- Kulig, K.; Sapa, J.; Nowaczyk, A.; Filipek, B.; Malawska, B. Synthesis and pharmacological evaluation of new 1-[3-(4-phenylpiperazin-1-yl)-propyl]- and 1-[3-(4-phenylpiperidine)-propyl]-3-aryl-3-alkyl-pyrrolidin-2-one derivatives with antiarrhythmic and antihypertensive activity. Acta Pol. Pharm. 2009, 66, 649–662. [Google Scholar]
- Kulig, K.; Spieces, C.; Sapa, J.; Caspers, C.; Filipek, B.; Malawska, B. Synthesis and pharmacological evaluation of pyrrolidin-2-one derivatives as antiarrhythmic, antihypertensive and alpha-adrenolytic agents. Pharmacol. Rep. 2010, 62, 68–85. [Google Scholar] [CrossRef]
- Sapa, J. Antiarrhythmic activity of novel S-enantiomers of pyrrolidin-2-one derivatives with adrenolytic properties. Acta Pol. Pharm. 2010, 67, 537–542. [Google Scholar]
- Betti, L.; Zanelli, M.; Giannaccini, G.; Manetti, F.; Schenone, S.; Strappaghetti, G. Synthesis of new piperazine-pyridazinone derivatives and their binding affinity toward alpha1-, alpha2-adrenergic and 5-HT1A serotoninergic receptors. Bioorgan. Med. Chem. 2006, 14, 2828–2836. [Google Scholar] [CrossRef]
- Li, M.-Y.; Tsai, K.-C.; Xia, L. Pharmacophore identification of alpha(1A)-adrenoceptor antagonists. Bioorgan. Med. Chem. Lett. 2005, 15, 657–664. [Google Scholar] [CrossRef] [PubMed]
- Li, M.-Y.; Fang, H.; Xia, L. Pharmacophore-based design, synthesis, biological evaluation, and 3D-QSAR studies of aryl-piperazines as alpha(1)-adrenoceptor antagonists. Bioorgan. Med. Chem. Lett. 2005, 15, 3216–3219. [Google Scholar] [CrossRef]
- Zaręba, P.; Dudek, M.; Lustyk, K.; Siwek, A.; Starowicz, G.; Bednarski, M.; Nowiński, L.; Raźny, K.; Sapa, J.; Malawska, B.; et al. α-Adrenoceptor antagonistic and hypotensive properties of novel arylpiperazine derivatives of pyrrolidin-2-one. Bioorgan. Med. Chem. 2015, 23, 2104–2111. [Google Scholar] [CrossRef]
- Cheng, Y.; Prusoff, W.H. Relationship between the inhibition constant (K1) and the concentration of inhibitor which causes 50 percent inhibition (I50) of an enzymatic reaction. Biochem. Pharmacol. 1973, 22, 3099–3108. [Google Scholar] [PubMed]
- De Clerck, F.; Van de Water, A.; D’Aubioul, J.; Lu, H.R.; van Rossem, K.; Hermans, A.; Van Ammel, K. In vivo measurement of QT prolongation, dispersion and arrhythmogenesis: Application to the preclinical cardiovascular safety pharmacology of a new chemical entity. Fundam. Clin. Pharmacol. 2002, 16, 125–140. [Google Scholar] [CrossRef]
- Nichols, A.J.; Sulpizio, A.C.; Ashton, D.J.; Hieble, J.P.; Ruffolo, R.R.J. In vitro pharmacologic profile of the novel beta-adrenoceptor antagonist and vasodilator, carvedilol. Pharmacology 1989, 39, 327–336. [Google Scholar] [CrossRef]
- Sapa, J.; Filipek, B.; Nowiński, L. Antiarrhythmic and hypotensive activities of 1-[2-hydroxy-3-(4-phenyl-1-piperazinyl)propyl]-pyrrolidin-2-one (MG-1(R,S)) and its enantiomers. Pharmacol. Rep. 2011, 63, 455–463. [Google Scholar] [CrossRef]
- Ruffolo, R.R.J.; Nichols, A.J.; Stadel, J.M.; Hieble, J.P. Structure and function of alpha-adrenoceptors. Pharmacol. Rev. 1991, 43, 475–505. [Google Scholar] [PubMed]
- Vaughan Williams, E.M. Classification of antidysrhythmic drugs. Pharmacol. Ther. B 1975, 1, 115–138. [Google Scholar] [CrossRef] [PubMed]
- Amin, A.S.; Asghari-Roodsari, A.; Tan, H.L. Cardiac sodium channelopathies. Pflug. Arch. 2010, 460, 223–237. [Google Scholar] [CrossRef] [PubMed]
- Clancy, C.E.; Zhu, Z.I.; Rudy, Y. Pharmacogenetics and anti-arrhythmic drug therapy: A theoretical investigation. Am. J. Physiol. Heart Circ. Physiol. 2007, 292, H66–H75. [Google Scholar] [CrossRef]
- Raschi, E.; Vasina, V.; Poluzzi, E.; De Ponti, F. The hERG K+ channel: Target and antitarget strategies in drug development. Pharmacol. Res. 2008, 57, 181–195. [Google Scholar] [CrossRef]
- Brown, A.M. Drugs, hERG and sudden death. Cell Calcium 2004, 35, 543–547. [Google Scholar] [CrossRef]
- Landstrom, A.P.; Dobrev, D.; Wehrens, X.H.T. Calcium Signaling and Cardiac Arrhythmias. Circ. Res. 2017, 120, 1969–1993. [Google Scholar] [CrossRef]
- Krumpl, G.; Todt, H.; Krejcy, K.; Raberger, G. Antiarrhythmic efficacy of labetalol as assessed by programmed electrical stimulation. Br. J. Pharmacol. 1990, 100, 855–861. [Google Scholar] [CrossRef]
- Hieble, J.P. Adrenoceptor subclassification: An approach to improved cardiovascular therapeutics. Pharm. Acta Helv. 2000, 74, 163–171. [Google Scholar] [CrossRef]
- Billman, G.E. Effect of alpha 1-adrenergic receptor antagonists on susceptibility to malignant arrhythmias: Protection from ventricular fibrillation. J. Cardiovasc. Pharmacol. 1994, 24, 394–402. [Google Scholar] [CrossRef]
- Pytka, K.; Lustyk, K.; Żmudzka, E.; Kotańska, M.; Siwek, A.; Zygmunt, M.; Dziedziczak, A.; Śniecikowska, J.; Olczyk, A.; Gałuszka, A.; et al. Chemically Homogenous Compounds with Antagonistic Properties at All α1-Adrenoceptor Subtypes but not β1-Adrenoceptor Attenuate Adrenaline-Induced Arrhythmia in Rats. Front. Pharmacol. 2016, 7, 229. [Google Scholar] [CrossRef] [PubMed]
- Corr, P.B.; Heathers, G.P.; Yamada, K.A. Mechanisms contributing to the arrhythmogenic influences of alpha 1-adrenergic stimulation in the ischemic heart. Am. J. Med. 1989, 87, 19S–25S. [Google Scholar] [CrossRef]
- Callaway, J.K.; Castillo-Melendez, M.; Giardina, S.F.; Krstew, E.K.; Beart, P.M.; Jarrott, B. Sodium channel blocking activity of AM-36 and sipatrigine (BW619C89): In vitro and in vivo evidence. Neuropharmacology 2004, 47, 146–155. [Google Scholar] [CrossRef]
- Reynolds, I.J.; Snowman, A.M.; Snyder, S.H. (-)-[3H] desmethoxyverapamil labels multiple calcium channel modulator receptors in brain and skeletal muscle membranes: Differentiation by temperature and dihydropyridines. J. Pharmacol. Exp. Ther. 1986, 237, 731–738. [Google Scholar] [PubMed]
- Huang, X.-P.; Mangano, T.; Hufeisen, S.; Setola, V.; Roth, B.L. Identification of human Ether-à-go-go related gene modulators by three screening platforms in an academic drug-discovery setting. Assay Drug Dev. Technol. 2010, 8, 727–742. [Google Scholar] [CrossRef]
- Szekeres, L.; Papp, J. Experimental cardiac arrhythmias. In Experimental Production of Diseases, Part 3, Heart and Circulation, Handbook of Experimental Pharmacology; Springer: Berlin/Heidelberg, Germany, 1975. [Google Scholar]
- Litchfield, J.T.; Wilcoxon, F. A simplified method of evaluating dose-effect experiments. J. Pharmacol. Exp. Ther. 1949, 96, 99–113. [Google Scholar]
| Treatment | β1 a,c (pKi [nM]) | Na+ a,d (IC50 [μM]) | K+ hERG b,e (IC50 [μM]) | Ca2+ a,f (IC50 [μM]) |
|---|---|---|---|---|
| S-75 | n.c. | 58 | 29.3 | 0.757 |
| Propranolol | 15.0 | - | - | - |
| Veratridine | - | 16.7 | - | - |
| Terfenadine | - | - | 0.025 | - |
| D-600 | - | - | - | 0.037 |
| Parameters | Time of Observation [min] | |||
|---|---|---|---|---|
| 0 | 5 | 10 | 15 | |
| PQ | 46.44 ± 1.352 | 47.00 ± 1.537 | 49.78 ± 1.042 | 52.11 ± 2.061 ** |
| QRS | 33.78 ± 1.384 | 35.56 ± 1.701 | 33.89 ± 1.628 | 37.22 ± 1.637 |
| QTc | 182.9 ± 4.805 | 192.3 ± 6.176 | 189.3 ± 9.543 | 190.9 ± 11.46 |
| QT | 81.57 ± 1.356 | 81.53 ± 1.812 | 82.47 ± 2.186 | 83.90 ± 1.730 |
| Rate | 310.8 ± 17.07 | 307.9 ± 18.93 | 287.8 ± 22.94 ** | 284.0 ± 23.50 ** |
| Treatment | Dose (mg/kg) | Fibrillations (%) | Extrasystoles (%) | Bradycardia (%) | Blocks (%) | Mortality (%) |
|---|---|---|---|---|---|---|
| Adrenaline-Induced Arrythmia | ||||||
| Control | - | - | 100 | 100 | 100 | 100 |
| S-75 | 0.5 | - | 16.7 | 0 | 33.3 | 0 |
| 0.25 | - | 66.7 | 16.7 | 50 | 0 | |
| 0.125 | - | 66.7 | 33.3 | 33.3 | 50 | |
| 0.06 | - | 83.3 | 100 | 50 | 0 | |
| 0.03 | - | 100 | 100 | 100 | 33.3 | |
| Carvedilol | 0.25 | - | 100 | 16.6 | 100 | 66.7 |
| Calcium Chloride-Induced Arrythmia | ||||||
| Control | - | 100 | 100 | 100 | 100 | 100 |
| S-75 | 5 | 66.7 | 100 | 100 | 100 | 83.3 |
| Verapamil | 2.5 | 33.3 | 66.7 | 100 | 83.3 | 16.7 |
| Aconitine-Induced Arrythmia | ||||||
| Control | - | 100 | 100 | 100 | 100 | 100 |
| S-75 | 5 | 100 | 100 | 100 | 100 | 100 |
| Propafenone | 5 | 33.3 | 66.7 | 100 | 83.3 | 16.6 |
| Treatment | Concentration (M) | Extrasystoles (%) | Tachycardia (%) | Fibrillations (%) | Arrhythmia Severity Index |
|---|---|---|---|---|---|
| Control | - | 100 | 100 | 33.3 | 6.3 |
| S-75 | 10−10 | 100 | 100 | 100 | 9 |
| Amiodarone | 10−9 | 100 | 100 | 66.7 | 7.7 |
| Propafenone | 10−11 | 100 | 66.7 | 33.3 | 6.7 |
| Quinidine | 10−6 | 83.3 | 50 | 0 | 2.3 * |
| Treatment | Dose (mg/kg) | Bradycardia (%) | Blocks (%) | Mortality (%) |
|---|---|---|---|---|
| Control | - | 100 | 100 | 67.7 |
| S-75 | 5 | 33.3 | 33.3 | 16.7 |
| Carvedilol | 5 | 67.7 | 83.3 | 16.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lustyk, K.; Sałaciak, K.; Zaręba, P.; Siwek, A.; Sapa, J.; Pytka, K. The Antiarrhythmic Activity of Novel Pyrrolidin-2-one Derivative S-75 in Adrenaline-Induced Arrhythmia. Pharmaceuticals 2021, 14, 1065. https://doi.org/10.3390/ph14111065
Lustyk K, Sałaciak K, Zaręba P, Siwek A, Sapa J, Pytka K. The Antiarrhythmic Activity of Novel Pyrrolidin-2-one Derivative S-75 in Adrenaline-Induced Arrhythmia. Pharmaceuticals. 2021; 14(11):1065. https://doi.org/10.3390/ph14111065
Chicago/Turabian StyleLustyk, Klaudia, Kinga Sałaciak, Paula Zaręba, Agata Siwek, Jacek Sapa, and Karolina Pytka. 2021. "The Antiarrhythmic Activity of Novel Pyrrolidin-2-one Derivative S-75 in Adrenaline-Induced Arrhythmia" Pharmaceuticals 14, no. 11: 1065. https://doi.org/10.3390/ph14111065
APA StyleLustyk, K., Sałaciak, K., Zaręba, P., Siwek, A., Sapa, J., & Pytka, K. (2021). The Antiarrhythmic Activity of Novel Pyrrolidin-2-one Derivative S-75 in Adrenaline-Induced Arrhythmia. Pharmaceuticals, 14(11), 1065. https://doi.org/10.3390/ph14111065






