Pharmacological and Toxicological Effects of Phytocannabinoids and Recreational Synthetic Cannabinoids: Increasing Risk of Public Health
Abstract
1. Introduction
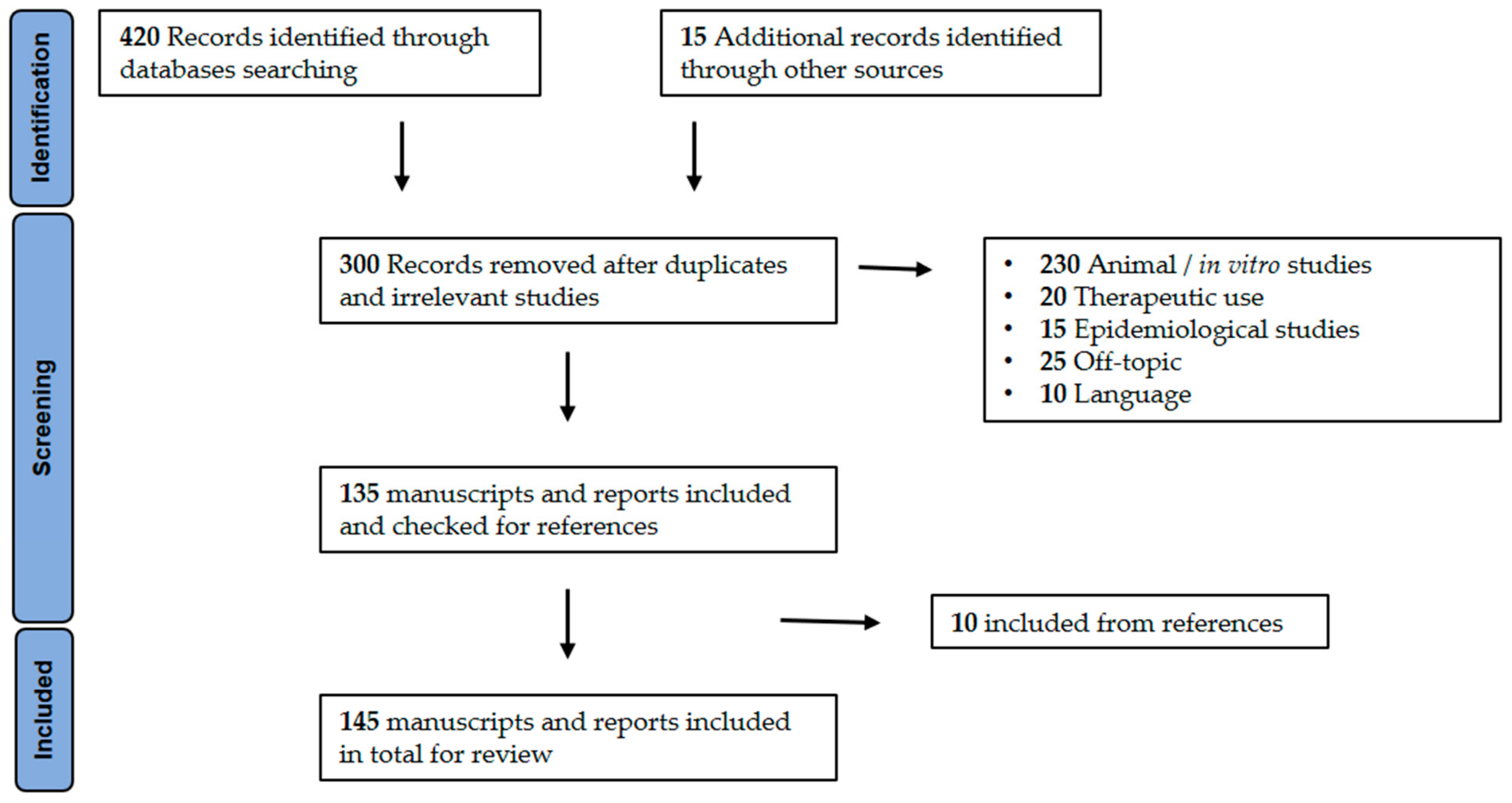
2. Methodology
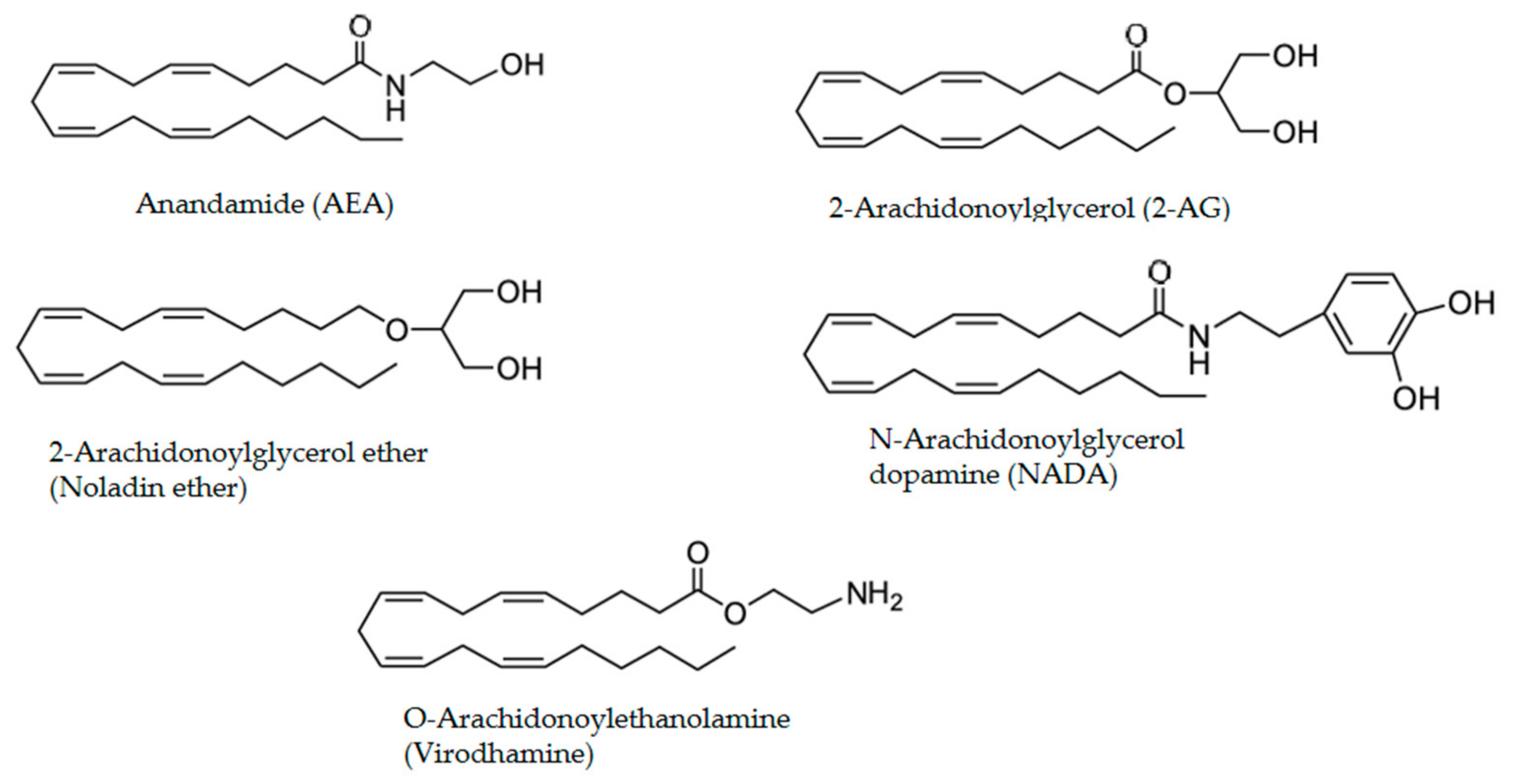
3. Endogenous Cannabinoids and Receptors
4. Cannabis sativa
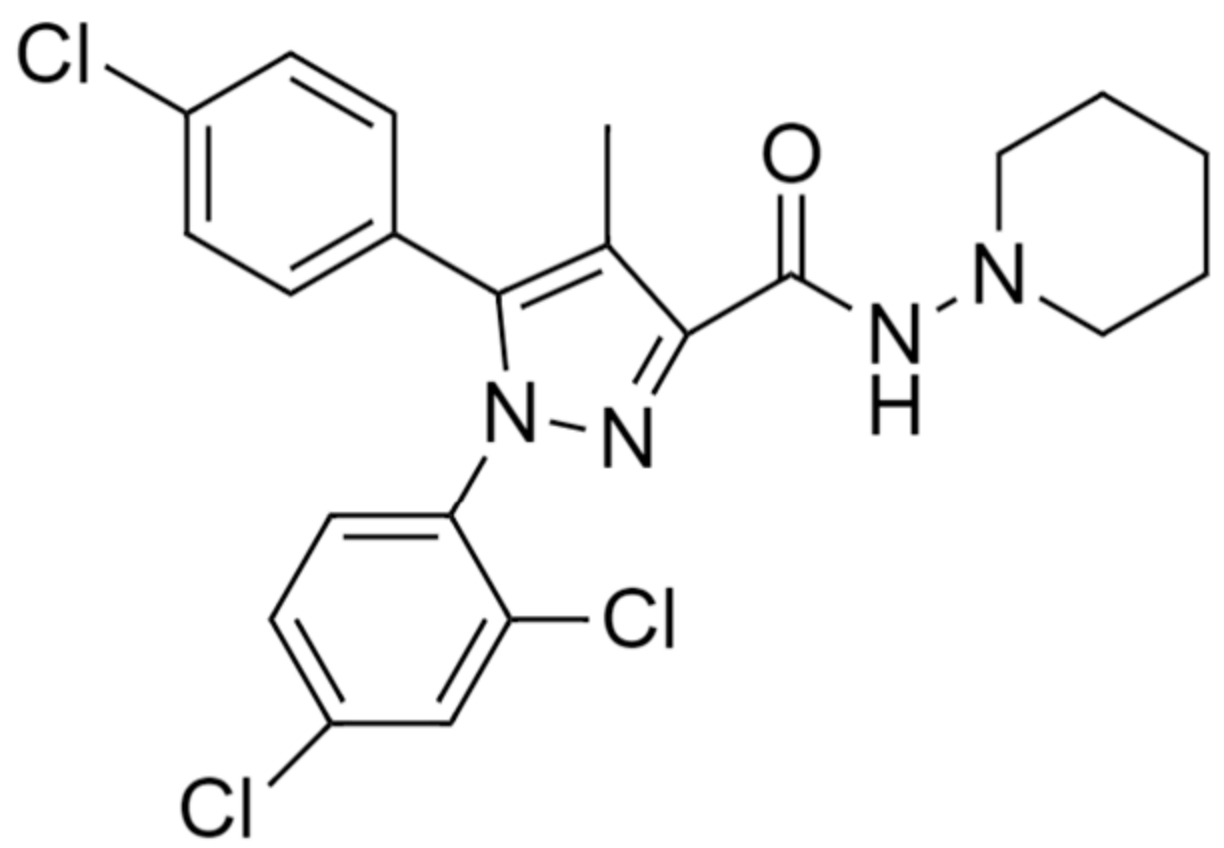
5. Therapeutic Effects of Phytocannabinoids and Synthetic Cannabinoids
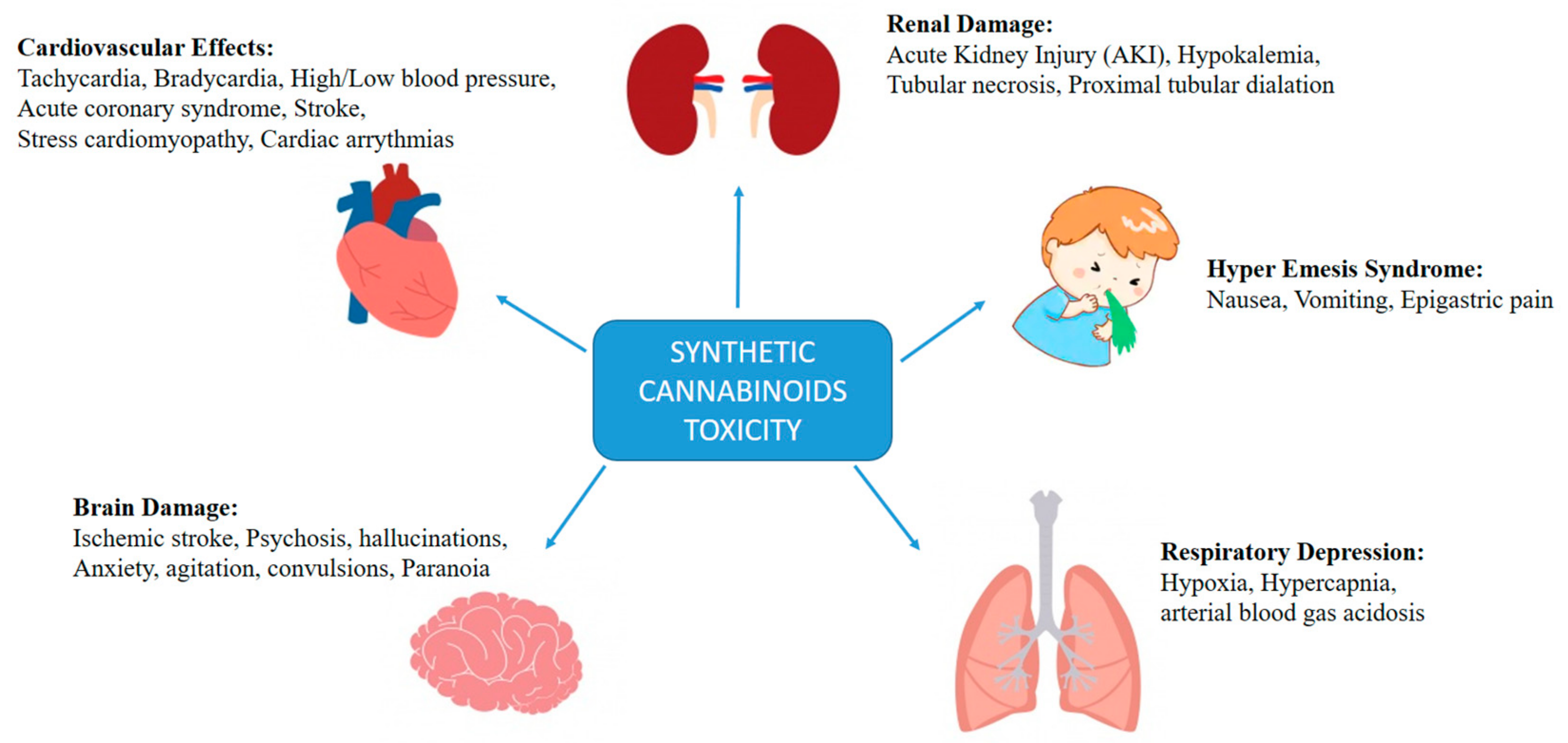
6. Synthetic Cannabinoids as Drugs of Abuse
7. Toxicological Effects of Synthetic Cannabinoids
7.1. Renal Injury
7.2. Cannabinoid Hyperemesis Syndrome
7.3. Cardiovascular Effects
7.4. Respiratory Depression
7.5. Effects on Brain
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mechoulam, R. The Pharmacohistory of Cannabis Sativa. In Cannabinoids as Therapeutic Agents; Chapman and Hall/CRC: Boca Raton, FL, USA, 2019; pp. 1–20. [Google Scholar] [CrossRef]
- Dos Santos, R.G.; Hallak, J.E.; Leite, J.P.; Zuardi, A.W.; Crippa, J.A. Phytocannabinoids and epilepsy. J. Clin. Pharm. Ther. 2015, 40, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Cassano, T.; Villani, R.; Pace, L.; Carbone, A.; Bukke, V.N.; Orkisz, S.; Avolio, C.; Serviddio, G. From Cannabis sativa to Cannabidiol: Promising Therapeutic Candidate for the Treatment of Neurodegenerative Diseases. Front. Pharmacol. 2020, 11, 124. [Google Scholar] [CrossRef]
- El-Alfy, A.T.; Ivey, K.; Robinson, K.; Ahmed, S.; Radwan, M.; Slade, D.; Khan, I.; ElSohly, M.; Ross, S. Antidepressant-like effect of delta9-tetrahydrocannabinol and other cannabinoids isolated from Cannabis sativa L. Pharmacol. Biochem. Behav. 2010, 95, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Pisanti, S.; Malfitano, A.M.; Ciaglia, E.; Lamberti, A.; Ranieri, R.; Cuomo, G.; Abate, M.; Faggiana, G.; Proto, M.C.; Fiore, D.; et al. Cannabidiol: State of the art and new challenges for therapeutic applications. Pharmacol. Ther. 2017, 175, 133–150. [Google Scholar] [CrossRef] [PubMed]
- Mills, B.; Yepes, A.; Nugent, K. Synthetic Cannabinoids. Am. J. Med Sci. 2015, 350, 59–62. [Google Scholar] [CrossRef]
- Wehrman, J. Fake Marijuana Spurs More Than 3,000 Calls to US Poison Centers. 2011. Available online: https://www.drugcaucus.senate.gov/sites/default/files/AAPCC%20National%20Press%20Release%20K2%2C%20Spice%203-28-2011.pdf (accessed on 10 July 2021).
- PUBLIC LAW 112–144—JULY 9. Title XI of the Food and Drug Administration Safety and Innovation Act. 2012. Available online: https://www.congress.gov/112/plaws/publ144/PLAW-112publ144.pdf (accessed on 21 June 2021).
- Law, R.; Schier, J.; Martin, C.; Chang, A.; Wolkin, A. Centers for Disease Control (CDC). Notes from the Field: Increase in Reported Adverse Health Effects Related to Synthetic Cannabinoid Use—United States, January–May 2015. MMWR. Morb. Mortal. Wkly. Rep. 2015, 64, 618–619. [Google Scholar]
- Williams, A.R.; Santaella-Tenorio, J.; Mauro, C.M.; Levin, F.R.; Martins, S.S. Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addiction 2017, 112, 1985–1991. [Google Scholar] [CrossRef]
- Lavi, E.; Rekhtman, D.; Berkun, Y.; Wexler, I. Sudden onset unexplained encephalopathy in infants: Think of cannabis intoxication. Eur. J. Pediatrics 2016, 175, 417–420. [Google Scholar] [CrossRef]
- Lindigkeit, R.; Boehme, A.; Eiserloh, I.; Luebbecke, M.; Wiggermann, M.; Ernst, L.; Beuerle, T. Spice: A never ending story? Forensic Sci. Int. 2009, 191, 58–63. [Google Scholar] [CrossRef]
- Griffiths, P.; Sedefov, R.; Gallegos, A.; Lopez, D. How globalization and market innovation challenge how we think about and respond to drug use: “Spice” a case study. Addiction 2010, 105, 951–953. [Google Scholar] [CrossRef]
- Harris, C.R.; Brown, A. Synthetic cannabinoid intoxication: A case series and review. J. Emerg. Med. 2013, 44, 360–366. [Google Scholar] [CrossRef]
- Lapoint, J.; James, L.P.; Moran, C.L.; Nelson, L.S.; Hoffman, R.S.; Moran, J.H. Severe toxicity following synthetic cannabinoid ingestion. Clin. Toxicol. 2011, 49, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Foley, J.D. Adolescent use and misuse of marijuana. Adolesc. Med. Clin. 2006, 17, 319–334. [Google Scholar] [CrossRef]
- United Nations Office on Drugs and Crime. World Drug Report. United Nations Publication, Sales No. E.18.XI.9. 2018. Available online: https://reliefweb.int/sites/reliefweb.int/files/resources/WDR18_Booklet_1_EXSUM.pdf (accessed on 26 June 2021).
- World Health Organization. The Health and Social Effects of Nonmedical Cannabis Use. WHO Document Production Services. 2016. Available online: https://www.who.int/substance_abuse/publications/msbcannabis.pdf (accessed on 21 July 2021).
- New Frontier Data. The Cannabis Industry Annual Report: 2017 Legal Marijuana Outlook. 2017. Available online: https://newfrontierdata.com/wp-content/uploads/2015/11/CIAR_Webinar_FINAL.pdf (accessed on 25 June 2021).
- United Nations Office on Drugs and Crime. World Drug Report. United Nations publication, Sales No. E.15.XI.6. 2015. Available online: http://www2.juridicas.unam.mx/marihuana-caso-mexico/wp-content/uploads/2016/02/World_Drug_Report_2015-ONU.pdf (accessed on 19 June 2021).
- Kasper, A.M.; Ridpath, A.D.; Arnold, J.K.; Chatham-Stephens, K.; Morrison, M.; Olayinka, O.; Parker, C.; Galli, R.; Cox, R.; Preacely, N.; et al. Severe Illness Associated with Reported Use of Synthetic Cannabinoids—Mississippi, April 2015. MMWR. Morb. Mortal. Wkly. Rep. 2015, 64, 1121–1122. [Google Scholar] [CrossRef] [PubMed]
- Devane, W.A.; Hanus, L.; Breuer, A.; Pertwee, R.G.; Stevenson, L.A.; Griffin, G.; Gibson, D.; Mandelbaum, A.; Etinger, A.; Mechoulam, R. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 1992, 258, 1946–1949. [Google Scholar] [CrossRef]
- Hanus, L.; Abu-Lafi, S.; Fride, E.; Breuer, A.; Vogel, Z.; Shalev, D.E.; Kustanovich, I.; Mechoulam, R. 2-arachidonyl glyceryl ether, an endogenous agonist of the cannabinoid CB1 receptor. Proc. Natl. Acad. Sci. USA 2001, 98, 3662–3665. [Google Scholar] [CrossRef] [PubMed]
- Huang, S.M.; Bisogno, T.; Trevisani, M.; Al-Hayani, A.; De Petrocellis, L.; Fezza, F.; Tognetto, M.; Petros, T.J.; Krey, J.F.; Chu, C.J.; et al. An endogenous capsaicin-like substance with high potency at recombinant and native vanilloid VR1 receptors. Proc. Natl. Acad. Sci. USA 2002, 99, 8400–8405. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.C.; Sauer, J.M.; Knierman, M.D.; Becker, G.W.; Berna, M.J.; Bao, J.; Nomikos, G.G.; Carter, P.; Bymaster, F.P.; Leese, A.B.; et al. Characterization of a novel endocannabinoid, virodhamine, with antagonist activity at the CB1 receptor. J. Pharmacol. Exp. Ther. 2002, 301, 1020–1024. [Google Scholar] [CrossRef]
- Basavarajappa, B.S. Critical enzymes involved in endocannabinoid metabolism. Protein Pept. Lett. 2007, 14, 237–246. [Google Scholar] [CrossRef]
- Long, J.Z.; Nomura, D.K.; Vann, R.E.; Walentiny, D.M.; Booker, L.; Jin, X.; Burston, J.J.; Sim-Selley, L.J.; Lichtman, A.H.; Wiley, J.L.; et al. Dual blockade of FAAH and MAGL identifies behavioral processes regulated by endocannabinoid crosstalk in vivo. Proc. Natl. Acad. Sci. USA 2009, 106, 20270–20275. [Google Scholar] [CrossRef]
- Bukke, V.N.; Archana, M.; Villani, R.; Romano, A.D.; Wawrzyniak, A.; Balawender, K.; Orkisz, S.; Beggiato, S.; Serviddio, G.; Cassano, T. The Dual Role of Glutamatergic Neurotransmission in Alzheimer’s Disease: From Pathophysiology to Pharmacotherapy. Int. J. Mol. Sci. 2020, 21, 7452. [Google Scholar] [CrossRef] [PubMed]
- Van der Stelt, M.; Di Marzo, V. Anandamide as an intracellular messenger regulating ion channel activity. Prostaglandins Other Lipid Mediat. 2005, 77, 111–122. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, L.A.; Lolait, S.J.; Brownstein, M.J.; Young, A.C.; Bonner, T.I. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 1990, 346, 561–564. [Google Scholar] [CrossRef]
- Glass, M.; Dragunow, M.; Faull, R.L. Cannabinoid receptors in the human brain: A detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience 1997, 77, 299–318. [Google Scholar] [CrossRef]
- Szabo, B.; Schlicker, E. Effects of cannabinoids on neurotransmission. Handb. Exp. Pharmacol. 2005, 327–365. [Google Scholar] [CrossRef]
- Galiegue, S.; Mary, S.; Marchand, J.; Dussossoy, D.; Carriere, D.; Carayon, P.; Bouaboula, M.; Shire, D.; Le Fur, G.; Casellas, P. Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur. J. Biochem. 1995, 232, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Munro, S.; Thomas, K.L.; Abu-Shaar, M. Molecular characterization of a peripheral receptor for cannabinoids. Nature 1993, 365, 61–65. [Google Scholar] [CrossRef]
- Pertwee, R.G.; Howlett, A.C.; Abood, M.E.; Alexander, S.P.; Di Marzo, V.; Elphick, M.R.; Greasley, P.J.; Hansen, H.S.; Kunos, G.; Mackie, K.; et al. International Union of Basic and Clinical Pharmacology. LXXIX. Cannabinoid receptors and their ligands: Beyond CB(1) and CB(2). Pharmacol. Rev. 2010, 62, 588–631. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.M.; Wager-Miller, J.; Mackie, K. Cloning and molecular characterization of the rat CB2 cannabinoid receptor. Biochim. Biophys. Acta 2002, 1576, 255–264. [Google Scholar] [CrossRef]
- Antonelli, T.; Tomasini, M.C.; Tattoli, M.; Cassano, T.; Tanganelli, S.; Finetti, S.; Mazzoni, E.; Trabace, L.; Steardo, L.; Cuomo, V.; et al. Prenatal exposure to the CB1 receptor agonist WIN 55,212-2 causes learning disruption associated with impaired cortical NMDA receptor function and emotional reactivity changes in rat offspring. Cereb. Cortex 2005, 15, 2013–2020. [Google Scholar] [CrossRef]
- Castaldo, P.; Magi, S.; Cataldi, M.; Arcangeli, S.; Lariccia, V.; Nasti, A.A.; Ferraro, L.; Tomasini, M.C.; Antonelli, T.; Cassano, T.; et al. Altered regulation of glutamate release and decreased functional activity and expression of GLT1 and GLAST glutamate transporters in the hippocampus of adolescent rats perinatally exposed to Delta(9)-THC. Pharmacol. Res. 2010, 61, 334–341. [Google Scholar] [CrossRef] [PubMed]
- Castaldo, P.; Magi, S.; Gaetani, S.; Cassano, T.; Ferraro, L.; Antonelli, T.; Amoroso, S.; Cuomo, V. Prenatal exposure to the cannabinoid receptor agonist WIN 55,212-2 increases glutamate uptake through overexpression of GLT1 and EAAC1 glutamate transporter subtypes in rat frontal cerebral cortex. Neuropharmacology 2007, 53, 369–378. [Google Scholar] [CrossRef]
- Ferraro, L.; Tomasini, M.C.; Cassano, T.; Bebe, B.W.; Siniscalchi, A.; O’Connor, W.T.; Magee, P.; Tanganelli, S.; Cuomo, V.; Antonelli, T. Cannabinoid receptor agonist WIN 55,212-2 inhibits rat cortical dialysate gamma-aminobutyric acid levels. J. Neurosci. Res. 2001, 66, 298–302. [Google Scholar] [CrossRef]
- Alon, M.H.; Saint-Fleur, M.O. Synthetic cannabinoid induced acute respiratory depression: Case series and literature review. Respir. Med. Case Rep. 2017, 22, 137–141. [Google Scholar] [CrossRef]
- Jinwala, F.N.; Gupta, M. Synthetic cannabis and respiratory depression. J. Child Adolesc. Psychopharmacol. 2012, 22, 459–462. [Google Scholar] [CrossRef] [PubMed]
- Turcotte, C.; Blanchet, M.R.; Laviolette, M.; Flamand, N. The CB2 receptor and its role as a regulator of inflammation. Cell. Mol. Life Sci. CMLS 2016, 73, 4449–4470. [Google Scholar] [CrossRef] [PubMed]
- Zoratti, C.; Kipmen-Korgun, D.; Osibow, K.; Malli, R.; Graier, W.F. Anandamide initiates Ca(2+) signaling via CB2 receptor linked to phospholipase C in calf pulmonary endothelial cells. Br. J. Pharmacol. 2003, 140, 1351–1362. [Google Scholar] [CrossRef] [PubMed]
- Turner, S.E.; Williams, C.M.; Iversen, L.; Whalley, B.J. Molecular Pharmacology of Phytocannabinoids. Prog. Chem. Org. Nat. Prod. 2017, 103, 61–101. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, P.; Pichini, S.; Pacifici, R.; Busardo, F.P.; Del Rio, A. Herbal Preparations of Medical Cannabis: A Vademecum for Prescribing Doctors. Medicina 2020, 56, 237. [Google Scholar] [CrossRef]
- Flores-Sanchez, I.J.; Verpoorte, R. Secondary metabolism in cannabis. Phytochem. Rev. 2008, 7, 615–639. [Google Scholar] [CrossRef]
- Galal, A.M.; Slade, D.; Gul, W.; El-Alfy, A.T.; Ferreira, D.; Elsohly, M.A. Naturally occurring and related synthetic cannabinoids and their potential therapeutic applications. Recent Pat. CNS Drug Discov. 2009, 4, 112–136. [Google Scholar] [CrossRef]
- Eubanks, L.M.; Rogers, C.J.; Beuscher, A.E.t.; Koob, G.F.; Olson, A.J.; Dickerson, T.J.; Janda, K.D. A molecular link between the active component of marijuana and Alzheimer’s disease pathology. Mol. Pharm. 2006, 3, 773–777. [Google Scholar] [CrossRef]
- Atwal, N.; Casey, S.L.; Mitchell, V.A.; Vaughan, C.W. THC and gabapentin interactions in a mouse neuropathic pain model. Neuropharmacology 2019, 144, 115–121. [Google Scholar] [CrossRef]
- Rahn, E.J.; Hohmann, A.G. Cannabinoids as pharmacotherapies for neuropathic pain: From the bench to the bedside. Neurother. J. Am. Soc. Exp. Neurother. 2009, 6, 713–737. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.J.; Hartley, J.P.; Graham, J.D. Bronchodilator effect of delta1-tetrahydrocannabinol administered by aerosol of asthmatic patients. Thorax 1976, 31, 720–723. [Google Scholar] [CrossRef]
- Neff, G.W.; O’Brien, C.B.; Reddy, K.R.; Bergasa, N.V.; Regev, A.; Molina, E.; Amaro, R.; Rodriguez, M.J.; Chase, V.; Jeffers, L.; et al. Preliminary observation with dronabinol in patients with intractable pruritus secondary to cholestatic liver disease. Am. J. Gastroenterol. 2002, 97, 2117–2119. [Google Scholar] [CrossRef] [PubMed]
- Klahn, P. Cannabinoids-Promising Antimicrobial Drugs orIntoxicants with Benefits? Antibiotics 2020, 9, 297. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, J.D.; Williamson, E.M. Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis. J. Dermatol. Sci. 2007, 45, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.J.; Weston, S.E.; Jones, N.A.; Smith, I.; Bevan, S.A.; Williamson, E.M.; Stephens, G.J.; Williams, C.M.; Whalley, B.J. Delta(9)-Tetrahydrocannabivarin suppresses in vitro epileptiform and in vivo seizure activity in adult rats. Epilepsia 2010, 51, 1522–1532. [Google Scholar] [CrossRef] [PubMed]
- Wargent, E.T.; Kepczynska, M.; Zaibi, M.S.; Hislop, D.C.; Arch, J.R.S.; Stocker, C.J. High fat-fed GPR55 null mice display impaired glucose tolerance without concomitant changes in energy balance or insulin sensitivity but are less responsive to the effects of the cannabinoids rimonabant or Delta(9)-tetrahydrocannabivarin on weight gain. PeerJ 2020, 8, e9811. [Google Scholar] [CrossRef]
- Xi, Z.X.; Muldoon, P.; Wang, X.F.; Bi, G.H.; Damaj, M.I.; Lichtman, A.H.; Pertwee, R.G.; Gardner, E.L. Delta(8) -Tetrahydrocannabivarin has potent anti-nicotine effects in several rodent models of nicotine dependence. Br. J. Pharmacol. 2019, 176, 4773–4784. [Google Scholar] [CrossRef] [PubMed]
- Abioye, A.; Ayodele, O.; Marinkovic, A.; Patidar, R.; Akinwekomi, A.; Sanyaolu, A. Delta9-Tetrahydrocannabivarin (THCV): A commentary on potential therapeutic benefit for the management of obesity and diabetes. J. Cannabis Res. 2020, 2, 6. [Google Scholar] [CrossRef]
- Holland, M.L.; Allen, J.D.; Arnold, J.C. Interaction of plant cannabinoids with the multidrug transporter ABCC1 (MRP1). Eur. J. Pharmacol. 2008, 591, 128–131. [Google Scholar] [CrossRef] [PubMed]
- Iuvone, T.; Esposito, G.; Esposito, R.; Santamaria, R.; Di Rosa, M.; Izzo, A.A. Neuroprotective effect of cannabidiol, a non-psychoactive component from Cannabis sativa, on beta-amyloid-induced toxicity in PC12 cells. J. Neurochem. 2004, 89, 134–141. [Google Scholar] [CrossRef]
- Esposito, G.; De Filippis, D.; Carnuccio, R.; Izzo, A.A.; Iuvone, T. The marijuana component cannabidiol inhibits beta-amyloid-induced tau protein hyperphosphorylation through Wnt/beta-catenin pathway rescue in PC12 cells. J. Mol. Med. 2006, 84, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, P.; Lo Faro, A.F.; Pirani, F.; Berretta, P.; Pacifici, R.; Pichini, S.; Busardo, F.P. Pharmacology and legal status of cannabidiol. Ann. Istituto Super. Sanita. 2020, 56, 285–291. [Google Scholar] [CrossRef]
- Lowin, T.; Tingting, R.; Zurmahr, J.; Classen, T.; Schneider, M.; Pongratz, G. Cannabidiol (CBD): A killer for inflammatory rheumatoid arthritis synovial fibroblasts. Cell Death Dis. 2020, 11, 714. [Google Scholar] [CrossRef]
- Breuer, A.; Haj, C.G.; Fogaca, M.V.; Gomes, F.V.; Silva, N.R.; Pedrazzi, J.F.; Del Bel, E.A.; Hallak, J.C.; Crippa, J.A.; Zuardi, A.W.; et al. Fluorinated Cannabidiol Derivatives: Enhancement of Activity in Mice Models Predictive of Anxiolytic, Antidepressant and Antipsychotic Effects. PLoS ONE 2016, 11, e0158779. [Google Scholar] [CrossRef]
- Hayakawa, K.; Mishima, K.; Irie, K.; Hazekawa, M.; Mishima, S.; Fujioka, M.; Orito, K.; Egashira, N.; Katsurabayashi, S.; Takasaki, K.; et al. Cannabidiol prevents a post-ischemic injury progressively induced by cerebral ischemia via a high-mobility group box1-inhibiting mechanism. Neuropharmacology 2008, 55, 1280–1286. [Google Scholar] [CrossRef]
- Zamberletti, E.; Gabaglio, M.; Piscitelli, F.; Brodie, J.S.; Woolley-Roberts, M.; Barbiero, I.; Tramarin, M.; Binelli, G.; Landsberger, N.; Kilstrup-Nielsen, C.; et al. Cannabidivarin completely rescues cognitive deficits and delays neurological and motor defects in male Mecp2 mutant mice. J. Psychopharmacol. 2019, 33, 894–907. [Google Scholar] [CrossRef] [PubMed]
- Hill, T.D.; Cascio, M.G.; Romano, B.; Duncan, M.; Pertwee, R.G.; Williams, C.M.; Whalley, B.J.; Hill, A.J. Cannabidivarin-rich cannabis extracts are anticonvulsant in mouse and rat via a CB1 receptor-independent mechanism. Br. J. Pharmacol. 2013, 170, 679–692. [Google Scholar] [CrossRef] [PubMed]
- Giacoppo, S.; Gugliandolo, A.; Trubiani, O.; Pollastro, F.; Grassi, G.; Bramanti, P.; Mazzon, E. Cannabinoid CB2 receptors are involved in the protection of RAW264.7 macrophages against the oxidative stress: An in vitro study. Eur. J. Histochem. EJH 2017, 61, 2749. [Google Scholar] [CrossRef]
- Borrelli, F.; Fasolino, I.; Romano, B.; Capasso, R.; Maiello, F.; Coppola, D.; Orlando, P.; Battista, G.; Pagano, E.; Di Marzo, V.; et al. Beneficial effect of the non-psychotropic plant cannabinoid cannabigerol on experimental inflammatory bowel disease. Biochem. Pharmacol. 2013, 85, 1306–1316. [Google Scholar] [CrossRef] [PubMed]
- Granja, A.G.; Carrillo-Salinas, F.; Pagani, A.; Gomez-Canas, M.; Negri, R.; Navarrete, C.; Mecha, M.; Mestre, L.; Fiebich, B.L.; Cantarero, I.; et al. A cannabigerol quinone alleviates neuroinflammation in a chronic model of multiple sclerosis. J. Neuroimmune Pharmacol. Off. J. Soc. NeuroImmune Pharmacol. 2012, 7, 1002–1016. [Google Scholar] [CrossRef] [PubMed]
- Aguareles, J.; Paraiso-Luna, J.; Palomares, B.; Bajo-Graneras, R.; Navarrete, C.; Ruiz-Calvo, A.; Garcia-Rincon, D.; Garcia-Taboada, E.; Guzman, M.; Munoz, E.; et al. Oral administration of the cannabigerol derivative VCE-003.2 promotes subventricular zone neurogenesis and protects against mutant huntingtin-induced neurodegeneration. Transl. Neurodegener. 2019, 8, 9. [Google Scholar] [CrossRef] [PubMed]
- Carrillo-Salinas, F.J.; Navarrete, C.; Mecha, M.; Feliu, A.; Collado, J.A.; Cantarero, I.; Bellido, M.L.; Munoz, E.; Guaza, C. A cannabigerol derivative suppresses immune responses and protects mice from experimental autoimmune encephalomyelitis. PLoS ONE 2014, 9, e94733. [Google Scholar] [CrossRef] [PubMed]
- Valdeolivas, S.; Navarrete, C.; Cantarero, I.; Bellido, M.L.; Munoz, E.; Sagredo, O. Neuroprotective properties of cannabigerol in Huntington’s disease: Studies in R6/2 mice and 3-nitropropionate-lesioned mice. Neurother. J. Am. Soc. Exp. Neurother. 2015, 12, 185–199. [Google Scholar] [CrossRef]
- Wirth, P.W.; Watson, E.S.; ElSohly, M.; Turner, C.E.; Murphy, J.C. Anti-inflammatory properties of cannabichromene. Life Sci. 1980, 26, 1991–1995. [Google Scholar] [CrossRef]
- De Luca, M.A.; Fattore, L. Therapeutic Use of Synthetic Cannabinoids: Still an OpenIssue? Clin. Ther. 2018, 40, 1457–1466. [Google Scholar] [CrossRef]
- Johnston, L.D.; Miech, R.A.; O’Malley, P.M.; Bachman, J.G.; Schulenberg, J.E.; Patrick, M.E. Monitoring the Future National Survey Results on Drug Use 1975–2018: Overview, Key Findings on Adolescent Drug Use; Institute for Social Research, University of Michigan: Ann Arbor, MI, USA, 2019. [Google Scholar]
- Watson, S.J.; Benson, J.A., Jr.; Joy, J.E. Marijuana and medicine: Assessing the science base: A summary of the 1999 Institute of Medicine report. Arch. Gen. Psychiatry 2000, 57, 547–552. [Google Scholar] [CrossRef]
- Campbell, F.A.; Tramer, M.R.; Carroll, D.; Reynolds, D.J.; Moore, R.A.; McQuay, H.J. Are cannabinoids an effective and safe treatment option in the management of pain? A qualitative systematic review. BMJ 2001, 323, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Badowski, M.E.; Perez, S.E. Clinical utility of dronabinol in the treatment of weight loss associated with HIV and AIDS. HIV AIDS 2016, 8, 37–45. [Google Scholar] [CrossRef] [PubMed][Green Version]
- De Lago, E.; Moreno-Martet, M.; Cabranes, A.; Ramos, J.A.; Fernandez-Ruiz, J. Cannabinoids ameliorate disease progression in a model of multiple sclerosis in mice, acting preferentially through CB1 receptor-mediated anti-inflammatory effects. Neuropharmacology 2012, 62, 2299–2308. [Google Scholar] [CrossRef]
- Ramer, R.; Hinz, B. Antitumorigenic targets of cannabinoids-current status and implications. Expert Opin. Ther. Targets 2016, 20, 1219–1235. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, T.; Tomasini, M.C.; Tattoli, M.; Cassano, T.; Finetti, S.; Mazzoni, E.; Trabace, L.; Carratu, M.R.; Cuomo, V.; Tanganelli, S.; et al. Prenatal exposure to the cannabinoid receptor agonist WIN 55,212-2 and carbon monoxide reduces extracellular glutamate levels in primary rat cerebral cortex cell cultures. Neurochem. Int. 2006, 49, 568–576. [Google Scholar] [CrossRef]
- Croxford, J.L. Therapeutic potential of cannabinoids in CNS disease. CNS Drugs 2003, 17, 179–202. [Google Scholar] [CrossRef] [PubMed]
- Ferraro, L.; Tomasini, M.C.; Beggiato, S.; Gaetani, S.; Cassano, T.; Cuomo, V.; Amoroso, S.; Tanganelli, S.; Antonelli, T. Short- and long-term consequences of prenatal exposure to the cannabinoid agonist WIN55,212-2 on rat glutamate transmission and cognitive functions. J. Neural Transm. 2009, 116, 1017–1027. [Google Scholar] [CrossRef]
- Tomasini, M.C.; Ferraro, L.; Bebe, B.W.; Tanganelli, S.; Cassano, T.; Cuomo, V.; Antonelli, T. Delta(9)-tetrahydrocannabinol increases endogenous extracellular glutamate levels in primary cultures of rat cerebral cortex neurons: Involvement of CB(1) receptors. J. Neurosci. Res. 2002, 68, 449–453. [Google Scholar] [CrossRef]
- Little, J.P.; Villanueva, E.B.; Klegeris, A. Therapeutic potential of cannabinoids in the treatment of neuroinflammation associated with Parkinson’s disease. Mini Rev. Med. Chem. 2011, 11, 582–590. [Google Scholar] [CrossRef][Green Version]
- Morgese, M.G.; Cassano, T.; Cuomo, V.; Giuffrida, A. Anti-dyskinetic effects of cannabinoids in a rat model of Parkinson’s disease: Role of CB(1) and TRPV1 receptors. Exp. Neurol. 2007, 208, 110–119. [Google Scholar] [CrossRef]
- Morgese, M.G.; Cassano, T.; Gaetani, S.; Macheda, T.; Laconca, L.; Dipasquale, P.; Ferraro, L.; Antonelli, T.; Cuomo, V.; Giuffrida, A. Neurochemical changes in the striatum of dyskinetic rats after administration of the cannabinoid agonist WIN55,212-2. Neurochem. Int. 2009, 54, 56–64. [Google Scholar] [CrossRef]
- Seillier, A.; Advani, T.; Cassano, T.; Hensler, J.G.; Giuffrida, A. Inhibition of fatty-acid amide hydrolase and CB1 receptor antagonism differentially affect behavioural responses in normal and PCP-treated rats. Int. J. Neuropsychopharmacol. 2010, 13, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Ramer, R.; Hinz, B. Cannabinoids as Anticancer Drugs. Adv. Pharmacol. 2017, 80, 397–436. [Google Scholar] [CrossRef]
- Carracedo, A.; Lorente, M.; Egia, A.; Blazquez, C.; Garcia, S.; Giroux, V.; Malicet, C.; Villuendas, R.; Gironella, M.; Gonzalez-Feria, L.; et al. The stress-regulated protein p8 mediates cannabinoid-induced apoptosis of tumor cells. Cancer Cell 2006, 9, 301–312. [Google Scholar] [CrossRef]
- McAllister, S.D.; Murase, R.; Christian, R.T.; Lau, D.; Zielinski, A.J.; Allison, J.; Almanza, C.; Pakdel, A.; Lee, J.; Limbad, C.; et al. Pathways mediating the effects of cannabidiol on the reduction of breast cancer cell proliferation, invasion, and metastasis. Breast Cancer Res. Treat. 2011, 129, 37–47. [Google Scholar] [CrossRef]
- Ortega, A.; Garcia-Hernandez, V.M.; Ruiz-Garcia, E.; Meneses-Garcia, A.; Herrera-Gomez, A.; Aguilar-Ponce, J.L.; Montes-Servin, E.; Prospero-Garcia, O.; Del Angel, S.A. Comparing the effects of endogenous and synthetic cannabinoid receptor agonists on survival of gastric cancer cells. Life Sci. 2016, 165, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Nithipatikom, K.; Endsley, M.P.; Isbell, M.A.; Falck, J.R.; Iwamoto, Y.; Hillard, C.J.; Campbell, W.B. 2-arachidonoylglycerol: A novel inhibitor of androgen-independent prostate cancer cell invasion. Cancer Res. 2004, 64, 8826–8830. [Google Scholar] [CrossRef] [PubMed]
- McKallip, R.J.; Jia, W.; Schlomer, J.; Warren, J.W.; Nagarkatti, P.S.; Nagarkatti, M. Cannabidiol-induced apoptosis in human leukemia cells: A novel role of cannabidiol in the regulation of p22phox and Nox4 expression. Mol. Pharmacol. 2006, 70, 897–908. [Google Scholar] [CrossRef] [PubMed]
- Casanova, M.L.; Blazquez, C.; Martinez-Palacio, J.; Villanueva, C.; Fernandez-Acenero, M.J.; Huffman, J.W.; Jorcano, J.L.; Guzman, M. Inhibition of skin tumor growth and angiogenesis in vivo by activation of cannabinoid receptors. J. Clin. Investig. 2003, 111, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Lukhele, S.T.; Motadi, L.R. Cannabidiol rather than Cannabis sativa extracts inhibit cell growth and induce apoptosis in cervical cancer cells. BMC Complementary Altern. Med. 2016, 16, 335. [Google Scholar] [CrossRef] [PubMed]
- Patsos, H.A.; Greenhough, A.; Hicks, D.J.; Al Kharusi, M.; Collard, T.J.; Lane, J.D.; Paraskeva, C.; Williams, A.C. The endogenous cannabinoid, anandamide, induces COX-2-dependent cell death in apoptosis-resistant colon cancer cells. Int. J. Oncol. 2010, 37, 187–193. [Google Scholar] [CrossRef]
- Ramer, R.; Heinemann, K.; Merkord, J.; Rohde, H.; Salamon, A.; Linnebacher, M.; Hinz, B. COX-2 and PPAR-gamma confer cannabidiol-induced apoptosis of human lung cancer cells. Mol. Cancer Ther. 2013, 12, 69–82. [Google Scholar] [CrossRef]
- Pourkhalili, N.; Ghahremani, M.H.; Farsandaj, N.; Tavajohi, S.; Majdzadeh, M.; Parsa, M.; Lavasani, N.J.; Ostad, S.N. Evaluation of anti-invasion effect of cannabinoids on human hepatocarcinoma cells. Toxicol. Mech. Methods 2013, 23, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Bettiga, A.; Aureli, M.; Colciago, G.; Murdica, V.; Moschini, M.; Luciano, R.; Canals, D.; Hannun, Y.; Hedlund, P.; Lavorgna, G.; et al. Bladder cancer cell growth and motility implicate cannabinoid 2 receptor-mediated modifications of sphingolipids metabolism. Sci. Rep. 2017, 7, 42157. [Google Scholar] [CrossRef]
- Barbado, M.V.; Medrano, M.; Caballero-Velazquez, T.; Alvarez-Laderas, I.; Sanchez-Abarca, L.I.; Garcia-Guerrero, E.; Martin-Sanchez, J.; Rosado, I.V.; Piruat, J.I.; Gonzalez-Naranjo, P.; et al. Cannabinoid derivatives exert a potent anti-myeloma activity both in vitro and in vivo. Int. J. Cancer 2017, 140, 674–685. [Google Scholar] [CrossRef] [PubMed]
- Galve-Roperh, I.; Sanchez, C.; Cortes, M.L.; Gomez del Pulgar, T.; Izquierdo, M.; Guzman, M. Anti-tumoral action of cannabinoids: Involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation. Nat. Med. 2000, 6, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Tiedra, S.; Fabrias, G.; Davila, D.; Salanueva, I.J.; Casas, J.; Montes, L.R.; Anton, Z.; Garcia-Taboada, E.; Salazar-Roa, M.; Lorente, M.; et al. Dihydroceramide accumulation mediates cytotoxic autophagy of cancer cells via autolysosome destabilization. Autophagy 2016, 12, 2213–2229. [Google Scholar] [CrossRef]
- De Petrocellis, L.; Melck, D.; Palmisano, A.; Bisogno, T.; Laezza, C.; Bifulco, M.; Di Marzo, V. The endogenous cannabinoid anandamide inhibits human breast cancer cell proliferation. Proc. Natl. Acad. Sci. USA 1998, 95, 8375–8380. [Google Scholar] [CrossRef] [PubMed]
- Pertwee, R.G. Emerging strategies for exploiting cannabinoid receptor agonists as medicines. Br. J. Pharmacol. 2009, 156, 397–411. [Google Scholar] [CrossRef] [PubMed]
- Sano, K.; Mishima, K.; Koushi, E.; Orito, K.; Egashira, N.; Irie, K.; Takasaki, K.; Katsurabayashi, S.; Iwasaki, K.; Uchida, N.; et al. Delta 9-tetrahydrocannabinol-induced catalepsy-like immobilization is mediated by decreased 5-HT neurotransmission in the nucleus accumbens due to the action of glutamate-containing neurons. Neuroscience 2008, 151, 320–328. [Google Scholar] [CrossRef]
- Bedse, G.; Romano, A.; Cianci, S.; Lavecchia, A.M.; Lorenzo, P.; Elphick, M.R.; Laferla, F.M.; Vendemiale, G.; Grillo, C.; Altieri, F.; et al. Altered expression of the CB1 cannabinoid receptor in the triple transgenic mouse model of Alzheimer’s disease. J. Alzheimer’s Dis. JAD 2014, 40, 701–712. [Google Scholar] [CrossRef]
- Bedse, G.; Romano, A.; Lavecchia, A.M.; Cassano, T.; Gaetani, S. The role of endocannabinoid signaling in the molecular mechanisms of neurodegeneration in Alzheimer’s disease. J. Alzheimer’s Dis. JAD 2015, 43, 1115–1136. [Google Scholar] [CrossRef]
- Cassano, T.; Calcagnini, S.; Pace, L.; De Marco, F.; Romano, A.; Gaetani, S. Cannabinoid Receptor 2 Signaling in Neurodegenerative Disorders: From Pathogenesis to a Promising Therapeutic Target. Front. Neurosci. 2017, 11, 30. [Google Scholar] [CrossRef] [PubMed]
- Consroe, P.; Sandyk, R.; Snider, S.R. Open label evaluation of cannabidiol in dystonic movement disorders. Int. J. Neurosci. 1986, 30, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Ruiz, J.; Moreno-Martet, M.; Rodriguez-Cueto, C.; Palomo-Garo, C.; Gomez-Canas, M.; Valdeolivas, S.; Guaza, C.; Romero, J.; Guzman, M.; Mechoulam, R.; et al. Prospects for cannabinoid therapies in basal ganglia disorders. Br. J. Pharmacol. 2011, 163, 1365–1378. [Google Scholar] [CrossRef]
- Garcia-Arencibia, M.; Gonzalez, S.; de Lago, E.; Ramos, J.A.; Mechoulam, R.; Fernandez-Ruiz, J. Evaluation of the neuroprotective effect of cannabinoids in a rat model of Parkinson’s disease: Importance of antioxidant and cannabinoid receptor-independent properties. Brain Res. 2007, 1134, 162–170. [Google Scholar] [CrossRef]
- Maroon, J.; Bost, J. Review of the neurological benefits of phytocannabinoids. Surg. Neurol. Int. 2018, 9, 91. [Google Scholar] [CrossRef] [PubMed]
- Uribe-Marino, A.; Francisco, A.; Castiblanco-Urbina, M.A.; Twardowschy, A.; Salgado-Rohner, C.J.; Crippa, J.A.; Hallak, J.E.; Zuardi, A.W.; Coimbra, N.C. Anti-aversive effects of cannabidiol on innate fear-induced behaviors evoked by an ethological model of panic attacks based on a prey vs the wild snake Epicrates cenchria crassus confrontation paradigm. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2012, 37, 412–421. [Google Scholar] [CrossRef]
- Baker, D.; Pryce, G.; Croxford, J.L.; Brown, P.; Pertwee, R.G.; Huffman, J.W.; Layward, L. Cannabinoids control spasticity and tremor in a multiple sclerosis model. Nature 2000, 404, 84–87. [Google Scholar] [CrossRef] [PubMed]
- Mecha, M.; Torrao, A.S.; Mestre, L.; Carrillo-Salinas, F.J.; Mechoulam, R.; Guaza, C. Cannabidiol protects oligodendrocyte progenitor cells from inflammation-induced apoptosis by attenuating endoplasmic reticulum stress. Cell Death Dis. 2012, 3, e331. [Google Scholar] [CrossRef] [PubMed]
- Consroe, P.; Musty, R.; Rein, J.; Tillery, W.; Pertwee, R. The perceived effects of smoked cannabis on patients with multiple sclerosis. Eur. Neurol. 1997, 38, 44–48. [Google Scholar] [CrossRef]
- Iskedjian, M.; Bereza, B.; Gordon, A.; Piwko, C.; Einarson, T.R. Meta-analysis of cannabis based treatments for neuropathic and multiple sclerosis-related pain. Curr. Med. Res. Opin. 2007, 23, 17–24. [Google Scholar] [CrossRef]
- Abuhasira, R.; Shbiro, L.; Landschaft, Y. Medical use of cannabis and cannabinoids containing products—Regulations in Europe and North America. Eur. J. Intern. Med. 2018, 49, 2–6. [Google Scholar] [CrossRef]
- Cahn, R.S. Cannabis indica resin, Part III. The constitution of Cannabinol. J. Chem. Soc. 1932, 1342–1353. [Google Scholar] [CrossRef]
- Mechoulam, R.; Gaoni, Y. A Total Synthesis of Dl-Delta-1-Tetrahydrocannabinol, the Active Constituent of Hashish. J. Am. Chem. Soc. 1965, 87, 3273–3275. [Google Scholar] [CrossRef]
- Auwarter, V.; Dresen, S.; Weinmann, W.; Muller, M.; Putz, M.; Ferreiros, N. ‘Spice’ and other herbal blends: Harmless incense or cannabinoid designer drugs? J. Mass Spectrom. JMS 2009, 44, 832–837. [Google Scholar] [CrossRef]
- New Psychoactive Substances Briefing for Professionals: Spice, Synthetic Cannabinoids, Manchester Health and Care Commissioning. 2017. Available online: https://www.mhcc.nhs.uk/wp-content/uploads/2017/08/MMU2278-SUAB-New-psychoactive-substance-use-in-Manchester.pdf (accessed on 10 June 2021).
- Piggee, C. Investigating a not-so-natural high. Anal. Chem. 2009, 81, 3205–3207. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, C.D.; Carreiro, S.P.; Babu, K.M. Here today, gone tomorrow…and back again? A review of herbal marijuana alternatives (K2, Spice), synthetic cathinones (bath salts), kratom, Salvia divinorum, methoxetamine, and piperazines. J. Med. Toxicol. Off. J. Am. Coll. Med. Toxicol. 2012, 8, 15–32. [Google Scholar] [CrossRef] [PubMed]
- Seely, K.A.; Prather, P.L.; James, L.P.; Moran, J.H. Marijuana-based drugs: Innovative therapeutics or designer drugs of abuse? Mol. Interv. 2011, 11, 36–51. [Google Scholar] [CrossRef] [PubMed]
- Dresen, S.; Ferreiros, N.; Putz, M.; Westphal, F.; Zimmermann, R.; Auwarter, V. Monitoring of herbal mixtures potentially containing synthetic cannabinoids as psychoactive compounds. J. Mass Spectrom. JMS 2010, 45, 1186–1194. [Google Scholar] [CrossRef] [PubMed]
- Barratt, M.J.; Cakic, V.; Lenton, S. Patterns of synthetic cannabinoid use in Australia. Drug Alcohol Rev. 2013, 32, 141–146. [Google Scholar] [CrossRef]
- Uchiyama, N.; Kikura-Hanajiri, R.; Kawahara, N.; Haishima, Y.; Goda, Y. Identification of a cannabinoid analog as a new type of designer drug in a herbal product. Chem. Pharm. Bull. 2009, 57, 439–441. [Google Scholar] [CrossRef]
- Shevyrin, V.A.; Morzherin, Y.Y. Cannabinoids: Structures, effects, and classification. Russ. Chem. Bull. 2015, 64, 1249–1266. [Google Scholar] [CrossRef]
- Gurney, S.M.; Scott, K.S.; Kacinko, S.L.; Presley, B.C.; Logan, B.K. Pharmacology, Toxicology, and Adverse Effects of Synthetic Cannabinoid Drugs. Forensic Sci. Rev. 2014, 26, 53–78. [Google Scholar]
- Giorgetti, A.; Busardo, F.P.; Tittarelli, R.; Auwarter, V.; Giorgetti, R. Post-Mortem Toxicology: A Systematic Review of Death Cases Involving Synthetic Cannabinoid Receptor Agonists. Front. Psychiatry 2020, 11, 464. [Google Scholar] [CrossRef]
- Freeman, M.J.; Rose, D.Z.; Myers, M.A.; Gooch, C.L.; Bozeman, A.C.; Burgin, W.S. Ischemic stroke after use of the synthetic marijuana “spice”. Neurology 2013, 81, 2090–2093. [Google Scholar] [CrossRef] [PubMed]
- Wolff, V.; Schlagowski, A.I.; Rouyer, O.; Charles, A.L.; Singh, F.; Auger, C.; Schini-Kerth, V.; Marescaux, C.; Raul, J.S.; Zoll, J.; et al. Tetrahydrocannabinol induces brain mitochondrial respiratory chain dysfunction and increases oxidative stress: A potential mechanism involved in cannabis-related stroke. BioMed Res. Int. 2015, 2015, 323706. [Google Scholar] [CrossRef]
- Seely, K.A.; Lapoint, J.; Moran, J.H.; Fattore, L. Spice drugs are more than harmless herbal blends: A review of the pharmacology and toxicology of synthetic cannabinoids. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2012, 39, 234–243. [Google Scholar] [CrossRef] [PubMed]
- Steup, C. Untersuchung des Handelsproduktes “Spice”. THC PHARM GmbH-The Health Concept. 2008. Available online: https://docplayer.org/45061257-Untersuchung-des-handelsproduktes-spice.html (accessed on 18 July 2021).
- Brents, L.K.; Zimmerman, S.M.; Saffell, A.R.; Prather, P.L.; Fantegrossi, W.E. Differential drug-drug interactions of the synthetic Cannabinoids JWH-018 and JWH-073: Implications for drug abuse liability and pain therapy. J. Pharmacol. Exp. Ther. 2013, 346, 350–361. [Google Scholar] [CrossRef]
- Norman, C.; Walker, G.; McKirdy, B.; McDonald, C.; Fletcher, D.; Antonides, L.H.; Sutcliffe, O.B.; Nic Daeid, N.; McKenzie, C. Detection and quantitation of synthetic cannabinoid receptor agonists in infused papers from prisons in a constantly evolving illicit market. Drug Test. Anal. 2020, 12, 538–554. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. Fentanils and Synthetic Cannabinoids: Driving Greater Complexity into the Drug Situation. An Update from the EU Early Warning System; Publications Office of the European Union: Luxembourg, 2018. [Google Scholar]
- Graziano, S.; Anzillotti, L.; Mannocchi, G.; Pichini, S.; Busardò, F.P. Screening methods for rapid determination of new psychoactive substances (NPS) in conventional and non-conventional biological matrices. J. Pharm. Biomed. Anal. 2019, 163, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Kidson, S. Doctor Slams Synthetic Cannabis. Nelson Mail. 2011. Available online: http://www.stuff.co.nz/nelson-mail/5162284/Doctor-slams-synthetic-cannabis (accessed on 15 June 2021).
- Vardakou, I.; Pistos, C.; Spiliopoulou, C. Spice drugs as a new trend: Mode of action, identification and legislation. Toxicol. Lett. 2010, 197, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Dargan, P.I.; Hudson, S.; Ramsey, J.; Wood, D.M. The impact of changes in UK classification of the synthetic cannabinoid receptor agonists in “Spice”. Int. J. Drug Policy 2011, 22, 274–277. [Google Scholar] [CrossRef]
- Fattore, L.; Fratta, W. Beyond THC: The New Generation of Cannabinoid Designer Drugs. Front. Behav. Neurosci. 2011, 5, 60. [Google Scholar] [CrossRef] [PubMed]
- Porteous, D. Ban on Tai High “Legal Highs”. Otago Daily Times. 2011. Available online: https://www.odt.co.nz/news/national/ban-tai-high-legal-highs (accessed on 15 July 2021).
- U.S. Department of Justice, D.E.A. Title 21 Code of Federal Regulations. Part. 1308-Schedules of Controlled Substances. 11 Schedule I. 2018. Available online: https://www.deadiversion.usdoj.gov/21cfr/cfr/1308/1308_11.htm (accessed on 19 July 2021).
- Ozturk, H.M.; Yetkin, E.; Ozturk, S. Synthetic Cannabinoids and Cardiac Arrhythmia Risk: Review of the Literature. Cardiovasc. Toxicol. 2019, 19, 191–197. [Google Scholar] [CrossRef]
- Vandrey, R.; Dunn, K.E.; Fry, J.A.; Girling, E.R. A survey study to characterize use of Spice products (synthetic cannabinoids). Drug Alcohol Depend. 2012, 120, 238–241. [Google Scholar] [CrossRef] [PubMed]
- Every-Palmer, S. Synthetic cannabinoid JWH-018 and psychosis: An explorative study. Drug Alcohol Depend. 2011, 117, 152–157. [Google Scholar] [CrossRef]
- Aung, M.M.; Griffin, G.; Huffman, J.W.; Wu, M.; Keel, C.; Yang, B.; Showalter, V.M.; Abood, M.E.; Martin, B.R. Influence of the N-1 alkyl chain length of cannabimimetic indoles upon CB(1) and CB(2) receptor binding. Drug Alcohol Depend. 2000, 60, 133–140. [Google Scholar] [CrossRef]
- Kronstrand, R.; Roman, M.; Andersson, M.; Eklund, A. Toxicological findings of synthetic cannabinoids in recreational users. J. Anal. Toxicol. 2013, 37, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Noble, C.; Cannaert, A.; Linnet, K.; Stove, C.P. Application of an activity-based receptor bioassay to investigate the in vitro activity of selected indole- and indazole-3-carboxamide-based synthetic cannabinoids at CB1 and CB2 receptors. Drug Test. Anal. 2019, 11, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Coppola, M.; Mondola, R. JWH-122 Consumption Adverse Effects: A Case of Hallucinogen Persisting Perception Disorder Five-Year Follow-up. J. Psychoact. Drugs 2017, 49, 262–265. [Google Scholar] [CrossRef]
- De Freitas, G.B.; da Silva, L.L.; Romeiro, N.C.; Fraga, C.A. Development of CoMFA and CoMSIA models of affinity and selectivity for indole ligands of cannabinoid CB1 and CB2 receptors. Eur. J. Med. Chem. 2009, 44, 2482–2496. [Google Scholar] [CrossRef] [PubMed]
- McQuade, D.; Hudson, S.; Dargan, P.I.; Wood, D.M. First European case of convulsions related to analytically confirmed use of the synthetic cannabinoid receptor agonist AM-2201. Eur. J. Clin. Pharmacol. 2013, 69, 373–376. [Google Scholar] [CrossRef] [PubMed]
- Lonati, D.; Buscaglia, E.; Papa, P.; Valli, A.; Coccini, T.; Giampreti, A.; Petrolini, V.M.; Vecchio, S.; Serpelloni, G.; Locatelli, C.A. MAM-2201 (analytically confirmed) intoxication after “Synthacaine” consumption. Ann. Emerg. Med. 2014, 64, 629–632. [Google Scholar] [CrossRef]
- Bertol, E.; Vaiano, F.; Di Milia, M.G.; Mari, F. In vivo detection of the new psychoactive substance AM-694 and its metabolites. Forensic Sci. Int. 2015, 256, 21–27. [Google Scholar] [CrossRef]
- European Monitoring Centre for Drugs and Drug Addiction. New Psychoactive Substances: Global Markets, Glocal Threats and the COVID-19 Pandemic. An. Update from the EU Early Warning System; EMCDDA: Lisbon, Portugal, 2020. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. EMCDDA Initial Report on the New Psychoactive Substance Methyl 3,3-dimethyl-2-(1-(pent-4-en-1-yl)-1H-indazole-3- carboxamido)butanoate (MDMB-4en-PINACA), Initial Reports; EMCDDA: Lisbon, Portugal, 2020. [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction. EMCDDA Initial Report on the New Psychoactive Substance Methyl 2-({[1-(4-fluorobutyl)-1H-indol-3-yl]carbonyl}amino)- 3,3-dimethylbutanoate (4F-MDMB-BICA), Initial Reports; EMCDDA: Lisbon, Portugal, 2020. [Google Scholar]
- Cannaert, A.; Sparkes, E.; Pike, E.; Luo, J.L.; Fang, A.; Kevin, R.C.; Ellison, R.; Gerona, R.; Banister, S.D.; Stove, C.P. Synthesis and in Vitro Cannabinoid Receptor 1 Activity of Recently Detected Synthetic Cannabinoids 4F-MDMB-BICA, 5F-MPP-PICA, MMB-4en-PICA, CUMYL-CBMICA, ADB-BINACA, APP-BINACA, 4F-MDMB-BINACA, MDMB-4en-PINACA, A-CHMINACA, 5F-AB-P7AICA, 5F-MDMB-P7AICA, and 5F-AP7AICA. ACS Chem. Neurosci. 2020, 11, 4434–4446. [Google Scholar] [CrossRef]
- Baumann, M.H.; Solis, E., Jr.; Watterson, L.R.; Marusich, J.A.; Fantegrossi, W.E.; Wiley, J.L. Baths salts, spice, and related designer drugs: The science behind the headlines. J. Neurosci. Off. J. Soc. Neurosci. 2014, 34, 15150–15158. [Google Scholar] [CrossRef]
- Seely, K.A.; Patton, A.L.; Moran, C.L.; Womack, M.L.; Prather, P.L.; Fantegrossi, W.E.; Radominska-Pandya, A.; Endres, G.W.; Channell, K.B.; Smith, N.H.; et al. Forensic investigation of K2, Spice, and “bath salt” commercial preparations: A three-year study of new designer drug products containing synthetic cannabinoid, stimulant, and hallucinogenic compounds. Forensic Sci. Int. 2013, 233, 416–422. [Google Scholar] [CrossRef]
- Meijer, K.A.; Russo, R.R.; Adhvaryu, D.V. Smoking synthetic marijuana leads to self-mutilation requiring bilateral amputations. Orthopedics 2014, 37, e391–e394. [Google Scholar] [CrossRef]
- Bhanushali, G.K.; Jain, G.; Fatima, H.; Leisch, L.J.; Thornley-Brown, D. AKI associated with synthetic cannabinoids: A case series. Clin. J. Am. Soc. Nephrol. CJASN 2013, 8, 523–526. [Google Scholar] [CrossRef] [PubMed]
- Ukaigwe, A.; Karmacharya, P.; Donato, A. A Gut Gone to Pot: A Case of Cannabinoid Hyperemesis Syndrome due to K2, a Synthetic Cannabinoid. Case Rep. Emerg. Med. 2014, 2014, 167098. [Google Scholar] [CrossRef] [PubMed]
- Mir, A.; Obafemi, A.; Young, A.; Kane, C. Myocardial infarction associated with use of the synthetic cannabinoid K2. Pediatrics 2011, 128, e1622–e1627. [Google Scholar] [CrossRef]
- Sevinc, M.M.; Kinaci, E.; Bayrak, S.; Yardimci, A.H.; Cakar, E.; Bektas, H. Extraordinary cause of acute gastric dilatation and hepatic portal venous gas: Chronic use of synthetic cannabinoid. World J. Gastroenterol. 2015, 21, 10704–10708. [Google Scholar] [CrossRef]
- Takematsu, M.; Hoffman, R.S.; Nelson, L.S.; Schechter, J.M.; Moran, J.H.; Wiener, S.W. A case of acute cerebral ischemia following inhalation of a synthetic cannabinoid. Clin. Toxicol. 2014, 52, 973–975. [Google Scholar] [CrossRef]
- Barutta, F.; Bruno, G.; Mastrocola, R.; Bellini, S.; Gruden, G. The role of cannabinoid signaling in acute and chronic kidney diseases. Kidney Int. 2018, 94, 252–258. [Google Scholar] [CrossRef]
- Koura, Y.; Ichihara, A.; Tada, Y.; Kaneshiro, Y.; Okada, H.; Temm, C.J.; Hayashi, M.; Saruta, T. Anandamide decreases glomerular filtration rate through predominant vasodilation of efferent arterioles in rat kidneys. J. Am. Soc. Nephrol. JASN 2004, 15, 1488–1494. [Google Scholar] [CrossRef] [PubMed]
- Barutta, F.; Corbelli, A.; Mastrocola, R.; Gambino, R.; Di Marzo, V.; Pinach, S.; Rastaldi, M.P.; Perin, P.C.; Gruden, G. Cannabinoid receptor 1 blockade ameliorates albuminuria in experimental diabetic nephropathy. Diabetes 2010, 59, 1046–1054. [Google Scholar] [CrossRef] [PubMed]
- Silva, G.B.; Atchison, D.K.; Juncos, L.I.; Garcia, N.H. Anandamide inhibits transport-related oxygen consumption in the loop of Henle by activating CB1 receptors. Am. J. Physiol. Ren. Physiol. 2013, 304, F376–F381. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.C.; Lim, S.K.; Han, H.J.; Park, S.H. Cannabinoid receptor 1 mediates palmitic acid-induced apoptosis via endoplasmic reticulum stress in human renal proximal tubular cells. J. Cell. Physiol. 2010, 225, 654–663. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.C.; Lim, S.K.; Park, M.J.; Kim, G.Y.; Han, H.J.; Park, S.H. Cannabinoid receptor 1 mediates high glucose-induced apoptosis via endoplasmic reticulum stress in primary cultured rat mesangial cells. Am. J. Physiol. Ren. Physiol. 2011, 301, F179–F188. [Google Scholar] [CrossRef] [PubMed]
- Park, F.; Potukuchi, P.K.; Moradi, H.; Kovesdy, C.P. Cannabinoids and the kidney: Effects in health and disease. Am. J. Physiol. Ren. Physiol. 2017, 313, F1124–F1132. [Google Scholar] [CrossRef]
- Barutta, F.; Piscitelli, F.; Pinach, S.; Bruno, G.; Gambino, R.; Rastaldi, M.P.; Salvidio, G.; Di Marzo, V.; Cavallo Perin, P.; Gruden, G. Protective role of cannabinoid receptor type 2 in a mouse model of diabetic nephropathy. Diabetes 2011, 60, 2386–2396. [Google Scholar] [CrossRef] [PubMed]
- Jenkin, K.A.; McAinch, A.J.; Grinfeld, E.; Hryciw, D.H. Role for cannabinoid receptors in human proximal tubular hypertrophy. Cell. Physiol. Biochem. Int. J. Exp. Cell. Physiol. Biochem. Pharmacol. 2010, 26, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, D.G.; Goligorsky, M.S.; Schmid, P.C.; Krebsbach, R.J.; Schmid, H.H.; Das, S.K.; Dey, S.K.; Arreaza, G.; Thorup, C.; Stefano, G.; et al. Production and physiological actions of anandamide in the vasculature of the rat kidney. J. Clin. Investig. 1997, 100, 1538–1546. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, P.; Pan, H.; Rajesh, M.; Batkai, S.; Patel, V.; Harvey-White, J.; Mukhopadhyay, B.; Hasko, G.; Gao, B.; Mackie, K.; et al. CB1 cannabinoid receptors promote oxidative/nitrosative stress, inflammation and cell death in a murine nephropathy model. Br. J. Pharmacol. 2010, 160, 657–668. [Google Scholar] [CrossRef]
- Mukhopadhyay, P.; Baggelaar, M.; Erdelyi, K.; Cao, Z.; Cinar, R.; Fezza, F.; Ignatowska-Janlowska, B.; Wilkerson, J.; van Gils, N.; Hansen, T.; et al. The novel, orally available and peripherally restricted selective cannabinoid CB2 receptor agonist LEI-101 prevents cisplatin-induced nephrotoxicity. Br. J. Opharmacol. 2016, 173, 446–458. [Google Scholar] [CrossRef]
- Buser, G.L.; Gerona, R.R.; Horowitz, B.Z.; Vian, K.P.; Troxell, M.L.; Hendrickson, R.G.; Houghton, D.C.; Rozansky, D.; Su, S.W.; Leman, R.F. Acute kidney injury associated with smoking synthetic cannabinoid. Clin. Toxicol. 2014, 52, 664–673. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Acute kidney injury associated with synthetic cannabinoid use--multiple states, 2012. MMWR Morb. Mortal. Wkly. Rep. 2013, 62, 93–98. [Google Scholar]
- Alp, A.; Akdam, H.; Avcioglu, B.Y.; Ersan, S. Synthetic cannabinoids in the kidneys. Rev. Assoc. Med. Bras. 2017, 63, 10–12. [Google Scholar] [CrossRef][Green Version]
- Allen, J.H.; de Moore, G.M.; Heddle, R.; Twartz, J.C. Cannabinoid hyperemesis: Cyclical hyperemesis in association with chronic cannabis abuse. Gut 2004, 53, 1566–1570. [Google Scholar] [CrossRef]
- Sorensen, C.J.; DeSanto, K.; Borgelt, L.; Phillips, K.T.; Monte, A.A. Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment-a Systematic Review. J. Med. Toxicol. Off. J. Am. Coll. Med. Toxicol. 2017, 13, 71–87. [Google Scholar] [CrossRef]
- Darmani, N.A. Cannabinoid-Induced Hyperemesis: A Conundrum-From Clinical Recognition to Basic Science Mechanisms. Pharmaceuticals 2010, 3, 2163–2177. [Google Scholar] [CrossRef] [PubMed]
- Bick, B.L.; Szostek, J.H.; Mangan, T.F. Synthetic cannabinoid leading to cannabinoid hyperemesis syndrome. Mayo Clin. Proc. 2014, 89, 1168–1169. [Google Scholar] [CrossRef]
- Woods, J.A.; Wright, N.J.; Gee, J.; Scobey, M.W. Cannabinoid Hyperemesis Syndrome: An Emerging Drug-Induced Disease. Am. J. Ther. 2016, 23, e601–e605. [Google Scholar] [CrossRef]
- Panikashvili, D.; Mechoulam, R.; Beni, S.M.; Alexandrovich, A.; Shohami, E. CB1 cannabinoid receptors are involved in neuroprotection via NF-kappa B inhibition. J. Cereb. Blood Flow Metab. Off. J. Int. Soc. Cereb. Blood Flow Metab. 2005, 25, 477–484. [Google Scholar] [CrossRef] [PubMed]
- Del Mar Ramirez Fernandez, M.; De Boeck, G.; Wood, M.; Lopez-Rivadulla, M.; Samyn, N. Simultaneous analysis of THC and its metabolites in blood using liquid chromatography-tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2008, 875, 465–470. [Google Scholar] [CrossRef]
- Patterson, D.A.; Smith, E.; Monahan, M.; Medvecz, A.; Hagerty, B.; Krijger, L.; Chauhan, A.; Walsh, M. Cannabinoid hyperemesis and compulsive bathing: A case series and paradoxical pathophysiological explanation. J. Am. Board Fam. Med. JABFM 2010, 23, 790–793. [Google Scholar] [CrossRef] [PubMed]
- Simonetto, D.A.; Oxentenko, A.S.; Herman, M.L.; Szostek, J.H. Cannabinoid hyperemesis: A case series of 98 patients. Mayo Clin. Proc. 2012, 87, 114–119. [Google Scholar] [CrossRef]
- Iversen, L. Cannabis and the brain. Brain J. Neurol. 2003, 126, 1252–1270. [Google Scholar] [CrossRef]
- Gash, A.; Karliner, J.S.; Janowsky, D.; Lake, C.R. Effects of smoking marihuana on left ventricular performance and plasma norepinephrine: Studies in normal men. Ann. Intern. Med. 1978, 89, 448–452. [Google Scholar] [CrossRef]
- Karschner, E.L.; Darwin, W.D.; McMahon, R.P.; Liu, F.; Wright, S.; Goodwin, R.S.; Huestis, M.A. Subjective and physiological effects after controlled Sativex and oral THC administration. Clin. Pharmacol. Ther. 2011, 89, 400–407. [Google Scholar] [CrossRef]
- Charbonney, E.; Sztajzel, J.M.; Poletti, P.A.; Rutschmann, O. Paroxysmal atrial fibrillation after recreational marijuana smoking: Another “holiday heart”? Swiss Med. Wkly. 2005, 135, 412–414. [Google Scholar]
- Wu, T.C.; Tashkin, D.P.; Djahed, B.; Rose, J.E. Pulmonary hazards of smoking marijuana as compared with tobacco. N. Engl. J. Med. 1988, 318, 347–351. [Google Scholar] [CrossRef]
- Lipina, C.; Hundal, H.S. Modulation of cellular redox homeostasis by the endocannabinoid system. Open Biol. 2016, 6, 150276. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Saluja, S.; Kumar, A.; Agrawal, S.; Thind, M.; Nanda, S.; Shirani, J. Cardiovascular Complications of Marijuana and Related Substances: A Review. Cardiol. Ther. 2018, 7, 45–59. [Google Scholar] [CrossRef] [PubMed]
- Mittleman, M.A.; Lewis, R.A.; Maclure, M.; Sherwood, J.B.; Muller, J.E. Triggering myocardial infarction by marijuana. Circulation 2001, 103, 2805–2809. [Google Scholar] [CrossRef]
- Bonz, A.; Laser, M.; Kullmer, S.; Kniesch, S.; Babin-Ebell, J.; Popp, V.; Ertl, G.; Wagner, J.A. Cannabinoids acting on CB1 receptors decrease contractile performance in human atrial muscle. J. Cardiovasc. Pharmacol. 2003, 41, 657–664. [Google Scholar] [CrossRef]
- Baranchuk, A.; Johri, A.M.; Simpson, C.S.; Methot, M.; Redfearn, D.P. Ventricular fibrillation triggered by marijuana use in a patient with ischemic cardiomyopathy: A case report. Cases J. 2008, 1, 373. [Google Scholar] [CrossRef] [PubMed]
- Fisher, B.A.; Ghuran, A.; Vadamalai, V.; Antonios, T.F. Cardiovascular complications induced by cannabis smoking: A case report and review of the literature. Emerg. Med. J. EMJ 2005, 22, 679–680. [Google Scholar] [CrossRef] [PubMed]
- Rumalla, K.; Reddy, A.Y.; Mittal, M.K. Association of Recreational Marijuana Use with Aneurysmal Subarachnoid Hemorrhage. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2016, 25, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Schmid, K.; Niederhoffer, N.; Szabo, B. Analysis of the respiratory effects of cannabinoids in rats. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2003, 368, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Orsini, J.; Blaak, C.; Tam, E.; Rajayer, S.; Morante, J.; Yeh, A.; Butala, A. The Wide and Unpredictable Scope of Synthetic Cannabinoids Toxicity. Case Rep. Crit. Care 2015, 2015, 542490. [Google Scholar] [CrossRef]
- Aygün, A.; Katipoğlu, B.; İmamoğlu, M.; Kılıç, M.; Karapolat, B.S.; Türkyılmaz, A. Acute Respiratory Distress Syndrome and Pneumothorax after Synthetic Cannabinoid Intoxication. Eurasian J. Emerg. Med. 2017, 16, 86–87. [Google Scholar] [CrossRef]
- Tai, S.; Fantegrossi, W.E. Synthetic Cannabinoids: Pharmacology, Behavioral Effects, and Abuse Potential. Curr. Addict. Rep. 2014, 1, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Paronis, C.A.; Nikas, S.P.; Shukla, V.G.; Makriyannis, A. Delta(9)-Tetrahydrocannabinol acts as a partial agonist/antagonist in mice. Behav. Pharmacol. 2012, 23, 802–805. [Google Scholar] [CrossRef]
- Helyes, Z.; Kemeny, A.; Cseko, K.; Szoke, E.; Elekes, K.; Mester, M.; Sandor, K.; Perkecz, A.; Kereskai, L.; Mark, L.; et al. Marijuana smoke induces severe pulmonary hyperresponsiveness, inflammation, and emphysema in a predictive mouse model not via CB1 receptor activation. Am. J. Physiol. Lung Cell. Mol. Physiol. 2017, 313, L267–L277. [Google Scholar] [CrossRef]
- Yirgin, G.; Ates, I.; Katipoglu, B.; Demir, B.F.; Yilmaz, N. Pulmonary embolism due to synthetic cannabinoid use: Case report. Turk. Kardiyol. Dern. Ars. Turk. Kardiyol. Dern. Yayin. Organidir 2018, 46, 411–413. [Google Scholar] [CrossRef]
- Raheemullah, A.; Laurence, T.N. Repeated Thrombosis after Synthetic Cannabinoid Use. J. Emerg. Med. 2016, 51, 540–543. [Google Scholar] [CrossRef] [PubMed]
- Burns, H.D.; Van Laere, K.; Sanabria-Bohorquez, S.; Hamill, T.G.; Bormans, G.; Eng, W.S.; Gibson, R.; Ryan, C.; Connolly, B.; Patel, S.; et al. [18F]MK-9470, a positron emission tomography (PET) tracer for in vivo human PET brain imaging of the cannabinoid-1 receptor. Proc. Natl. Acad. Sci. USA 2007, 104, 9800–9805. [Google Scholar] [CrossRef] [PubMed]
- Gruber, S.A.; Silveri, M.M.; Dahlgren, M.K.; Yurgelun-Todd, D. Why so impulsive? White matter alterations are associated with impulsivity in chronic marijuana smokers. Exp. Clin. Psychopharmacol. 2011, 19, 231–242. [Google Scholar] [CrossRef]
- Zalesky, A.; Solowij, N.; Yucel, M.; Lubman, D.I.; Takagi, M.; Harding, I.H.; Lorenzetti, V.; Wang, R.; Searle, K.; Pantelis, C.; et al. Effect of long-term cannabis use on axonal fibre connectivity. Brain J. Neurol. 2012, 135, 2245–2255. [Google Scholar] [CrossRef] [PubMed]
- Campolongo, P.; Trezza, V.; Cassano, T.; Gaetani, S.; Morgese, M.G.; Ubaldi, M.; Soverchia, L.; Antonelli, T.; Ferraro, L.; Massi, M.; et al. Perinatal exposure to delta-9-tetrahydrocannabinol causes enduring cognitive deficits associated with alteration of cortical gene expression and neurotransmission in rats. Addict. Biol. 2007, 12, 485–495. [Google Scholar] [CrossRef] [PubMed]
- Trezza, V.; Campolongo, P.; Cassano, T.; Macheda, T.; Dipasquale, P.; Carratu, M.R.; Gaetani, S.; Cuomo, V. Effects of perinatal exposure to delta-9-tetrahydrocannabinol on the emotional reactivity of the offspring: A longitudinal behavioral study in Wistar rats. Psychopharmacology 2008, 198, 529–537. [Google Scholar] [CrossRef]
- Battistella, G.; Fornari, E.; Annoni, J.M.; Chtioui, H.; Dao, K.; Fabritius, M.; Favrat, B.; Mall, J.F.; Maeder, P.; Giroud, C. Long-term effects of cannabis on brain structure. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2014, 39, 2041–2048. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, J.G.; Block, R.I.; O’Leary, D.S.; Ponto, L.B.; Ghoneim, M.M.; Bechara, A. Effects of chronic marijuana use on brain activity during monetary decision-making. Neuropsychopharmacol. Off. Publ. Am. Coll. Neuropsychopharmacol. 2012, 37, 618–629. [Google Scholar] [CrossRef]
- Cohen-Cory, S. The developing synapse: Construction and modulation of synaptic structures and circuits. Science 2002, 298, 770–776. [Google Scholar] [CrossRef]
- Casu, M.A.; Pisu, C.; Sanna, A.; Tambaro, S.; Spada, G.P.; Mongeau, R.; Pani, L. Effect of delta9-tetrahydrocannabinol on phosphorylated CREB in rat cerebellum: An immunohistochemical study. Brain Res. 2005, 1048, 41–47. [Google Scholar] [CrossRef]
- Bossong, M.G.; Niesink, R.J. Adolescent brain maturation, the endogenous cannabinoid system and the neurobiology of cannabis-induced schizophrenia. Prog. Neurobiol. 2010, 92, 370–385. [Google Scholar] [CrossRef]
- Creagh, S.; Warden, D.; Latif, M.A.; Paydar, A. The New Classes of Synthetic Illicit Drugs Can Significantly Harm the Brain: A Neuro Imaging Perspective with Full Review of MRI Findings. Clin. Radiol. Imaging J. 2018, 2, 000116. [Google Scholar] [CrossRef]
- Drugs of Abuse. A DEA Resource Guide. Drug Enforcement Administration, U.S. Department of Justice. 2017. Available online: https://www.dea.gov/sites/default/files/drug_of_abuse.pdf (accessed on 12 June 2021).
- Kramer, C.L.; Wetzel, D.R.; Wijdicks, E.F. Devastating Delayed Leukoencephalopathy Associated with Bath Salt Inhalation. Neurocritical Care 2016, 24, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Prosser, J.M.; Nelson, L.S. The toxicology of bath salts: A review of synthetic cathinones. J. Med. Toxicol. Off. J. Am. Coll. Med. Toxicol. 2012, 8, 33–42. [Google Scholar] [CrossRef]
- D’Souza, D.C.; Kosten, T.R. Cannabinoid antagonists: A treatment in search of an illness. Arch. Gen. Psychiatry 2001, 58, 330–331. [Google Scholar] [CrossRef]
- Compton, D.R.; Aceto, M.D.; Lowe, J.; Martin, B.R. In vivo characterization of a specific cannabinoid receptor antagonist (SR141716A): Inhibition of delta 9-tetrahydrocannabinol-induced responses and apparent agonist activity. J. Pharmacol. Exp. Ther. 1996, 277, 586–594. [Google Scholar]
- DeSanty, K.P.; Dar, M.S. Cannabinoid-induced motor incoordination through the cerebellar CB(1) receptor in mice. Pharmacol. Biochem. Behav. 2001, 69, 251–259. [Google Scholar] [CrossRef]
- Hampson, R.E.; Deadwyler, S.A. Cannabinoids, hippocampal function and memory. Life Sci. 1999, 65, 715–723. [Google Scholar] [CrossRef]
- Robinson, L.; Goonawardena, A.V.; Pertwee, R.G.; Hampson, R.E.; Riedel, G. The synthetic cannabinoid HU210 induces spatial memory deficits and suppresses hippocampal firing rate in rats. Br. J. Pharmacol. 2007, 151, 688–700. [Google Scholar] [CrossRef] [PubMed]
| Name | Structure | Ki/µM | Key Findings |
|---|---|---|---|
| Δ9-trans-Tetrahydrocannabinol | 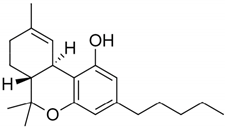 | CB1—0.005 a 0.008 b 0.013 c CB2—0.003 a 0.0017 b 0.0068 c [45] | THC inhibits Alzheimer’s disease (AD) pathology (by competitively inhibiting acetylcholinesterase enzyme and beta-amyloid (Aβ) peptide aggregation) [49] As analgesic for neuropathic pain [50,51] Bronchodialator effect on asthma patients [52] Effective to treat intractable cholestatic pruritus [53] Potent against methicillin-resistant Staphylococcus aureus (MRSA) strains (MIC- 2 µg/mL) * [54] Inhibit the proliferation of a hyper-proliferating human keratinocyte cell line in the treatment of psoriasis [55] |
| Δ9-Tetrahydrocannabivarin | 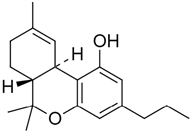 | CB1—0.075 d 0.0047 e CB2—0.225 a 0.145 a [45] | Exerts antiepileptiform and anticonvulsant properties in adult rats [56] Ameliorates insulin sensitivity and can be used to treat obesity-associated glucose intolerance [57] Δ8-Tetrahydrocannabivarin has potent anti-nicotine effects [58] Potent against MRSA strains (MIC—4 µg/mL) * [54] As a potential therapeutic benefit for the management of obesity and diabetes [59] |
| Cannabinol | 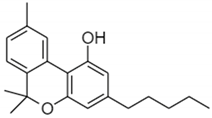 | CB1—0.069 f 0.012 g CB2—0.016 g 0.07 f [45] | Potent against MRSA strains (MIC—2 µg/mL) * [54] Inhibit the proliferation of a hyper-proliferating human keratinocyte cell line in the treatment of psoriasis [55] |
| Cannabidiol |  | CB1—4.3 e 1.45 g CB2—2.86 f 0.37 g [45] | Potent against MRSA strains (MIC—2 µg/mL) * [54] Inhibit the proliferation of a hyper-proliferating human keratinocyte cell line in the treatment of psoriasis [55] Potent inhibitor of transporter ABCC1 or MRP1 that helps in accumulation of anticancer drugs in cells [60] Protect against Aβ neurotoxicity in AD [61] Inhibits tau hyperphosphorylation in AD [62] Anti-arthritic by targeting synovial fibroblasts [63,64] Fluorinated derivatives of cannabidiol shows therapeutic activity as anxiolytic, antidepressant, antipsychotic, and anticompulsive [65] Prevents post-ischemic injury via HMGB1-inhibiting mechanism [66] |
| Cannabidivarin | 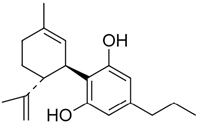 | CB1—14.7 g CB2—0.57 g [45] | Ameliorates autism-like behaviours, restores endocannabinoid signaling and neuroinflammation [67] Anti-convulsant [68] Potent against MRSA strains (MIC—8 µg/mL) * [54] |
| Cannabigerol | 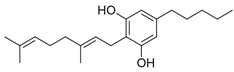 | CB1—0.896 g CB2—0.153 g [45] | Anti-oxidant properties in macrophages [69] Can be used to treat inflammatory bowel disease [70] Potent anti-inflammatory agent in a model of multiple sclerosis (MS) [71] Cannabigerol derivative VCE-003.2 protects against mutant huntingtin-induced neurodegeneration [72] Cannabigerol derivative VCE-003 can be used in the treatment of human immune diseases [73] Potent against MRSA strains (MIC—2 µg/mL) * [54] Plays a neuroprotective role in the treatment of Huntington’s disease (HD) [74] |
| Cannabichromene | 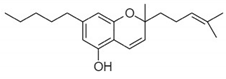 | CB1—0.71 g CB2—0.256 g [45] | Potent against MRSA strains (MIC—8 µg/mL) * [54] Inhibit the proliferation of a hyper-proliferating human keratinocyte cell line in the treatment of psoriasis [55] Anti-inflammatory properties [75] |
| Name | Structure | Receptors | Adverse Effects |
|---|---|---|---|
| CP47,497 (5-(1,1-dimethylheptyl)-2-[(1R,3S)-3-hydroxycyclohexyl]-phenol) | 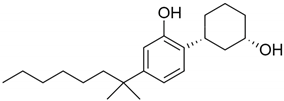 | CB1 and CB2 agonist [149] | Increased heart rate, high/low blood pressure, coughing, and, vomiting [150] |
| JWH-018 (1-pentyl-3-(1-naphthoyl)indole) |  | CB1 and CB2 agonist [149] | Psychosis [151], hallucinations, vertigo, paresthesias, shaking, shivering, hypertension, dry mouth, vomiting, mydriasis, hypokalemia, extrasystoles, tachycardia, conjunctival hyperemia [134], and ischemic stroke [135] |
| JWH-073 (1-butyl-3-(1-naphthoyl)indole) |  | CB1 and CB2 agonist [149,152] | Altered mood and perception, red or bloodshot eyes, nausea, vomiting, listlessness, fever, sweating, and dryness of the mouth [150] |
| JWH-019 (1-hexyl-3-(1-naphthoyl)indole) | 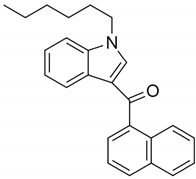 | CB1 and CB2 agonist [152] | Confused speech, unstable appearance [150] |
| JWH-250 (1-pentyl-3-(2-methoxyphenylacetyl)indole) | 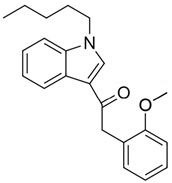 | CB1 and CB2 agonist [149] | Dilated unresponsive pupils and bloodshot eyes [153] |
| JWH-081 (1-pentyl-3-[1-(4-methoxynaphthoyl)]indole) | 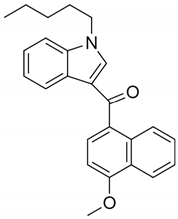 | CB1 and CB2 agonist [152] | Slurred speech [153] |
| JWH-122 (1-pentyl-3-(4-methyl-1-naphthoyl)indole) | 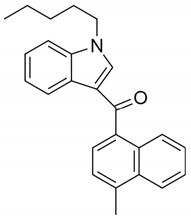 | Agonist at CB1 and CB2 [154] | Hallucinations, disorientation, sedation, anxiety, agitation, tachycardia, hypertension, dyspnea, nausea, vomiting, hyperglycemia, and hypokalemia [155] |
| AM2201 (1-(5-fluoropentyl)-3-(1-naphthoyl)indole) |  | Agonist at CB1 and CB2 [156] | Convulsions [157], Excitatory behavior, xerostomia, chest pain, severe dyspnea, tachycardia (150 beats/min), and mild hypertension [158] |
| AM694 (1-(5-fluoropentyl)-3-(2-iodobenzoyl)indole) | 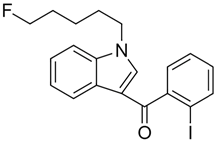 | Agonist at CB1 [159] | Agitation, hallucination, anxiety, and paranoia [159] |
| JWH-203 (1-pentyl-3-(2-chlorophenylacetyl)indole) | 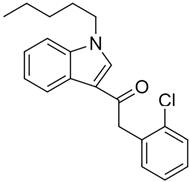 | Agonist at CB1 and CB2 [156] | Head twitching, slurred speech, hallucination, dilated unresponsive pupils and bloodshot eyes [153] |
| MDMB-4en-PINACA | 4F-MDMB-BICA | |
|---|---|---|
| Structure | 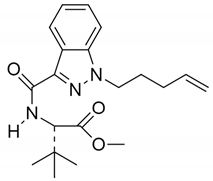 | 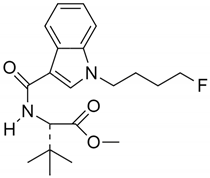 |
| Molecular Formula | C20H27N3O3 | C20H27FN2O3 |
| Form | Yellow powder | White powder [163] |
| Availability | Since 2017 | Since 2020 |
| Cases reported | 768 seizures as of October 2020. 11 acute non-fatal poisonings in the United Kingdom (UK) 4 confirmed deaths were reported in total by Sweden and UK | 108 seizures as of October 2020 21 deaths reported by Hungary between May and August 2020 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bukke, V.N.; Archana, M.; Villani, R.; Serviddio, G.; Cassano, T. Pharmacological and Toxicological Effects of Phytocannabinoids and Recreational Synthetic Cannabinoids: Increasing Risk of Public Health. Pharmaceuticals 2021, 14, 965. https://doi.org/10.3390/ph14100965
Bukke VN, Archana M, Villani R, Serviddio G, Cassano T. Pharmacological and Toxicological Effects of Phytocannabinoids and Recreational Synthetic Cannabinoids: Increasing Risk of Public Health. Pharmaceuticals. 2021; 14(10):965. https://doi.org/10.3390/ph14100965
Chicago/Turabian StyleBukke, Vidyasagar Naik, Moola Archana, Rosanna Villani, Gaetano Serviddio, and Tommaso Cassano. 2021. "Pharmacological and Toxicological Effects of Phytocannabinoids and Recreational Synthetic Cannabinoids: Increasing Risk of Public Health" Pharmaceuticals 14, no. 10: 965. https://doi.org/10.3390/ph14100965
APA StyleBukke, V. N., Archana, M., Villani, R., Serviddio, G., & Cassano, T. (2021). Pharmacological and Toxicological Effects of Phytocannabinoids and Recreational Synthetic Cannabinoids: Increasing Risk of Public Health. Pharmaceuticals, 14(10), 965. https://doi.org/10.3390/ph14100965






