Poppers Use and High Methaemoglobinaemia: ‘Dangerous Liaisons’
Abstract
:1. Introduction
2. Results
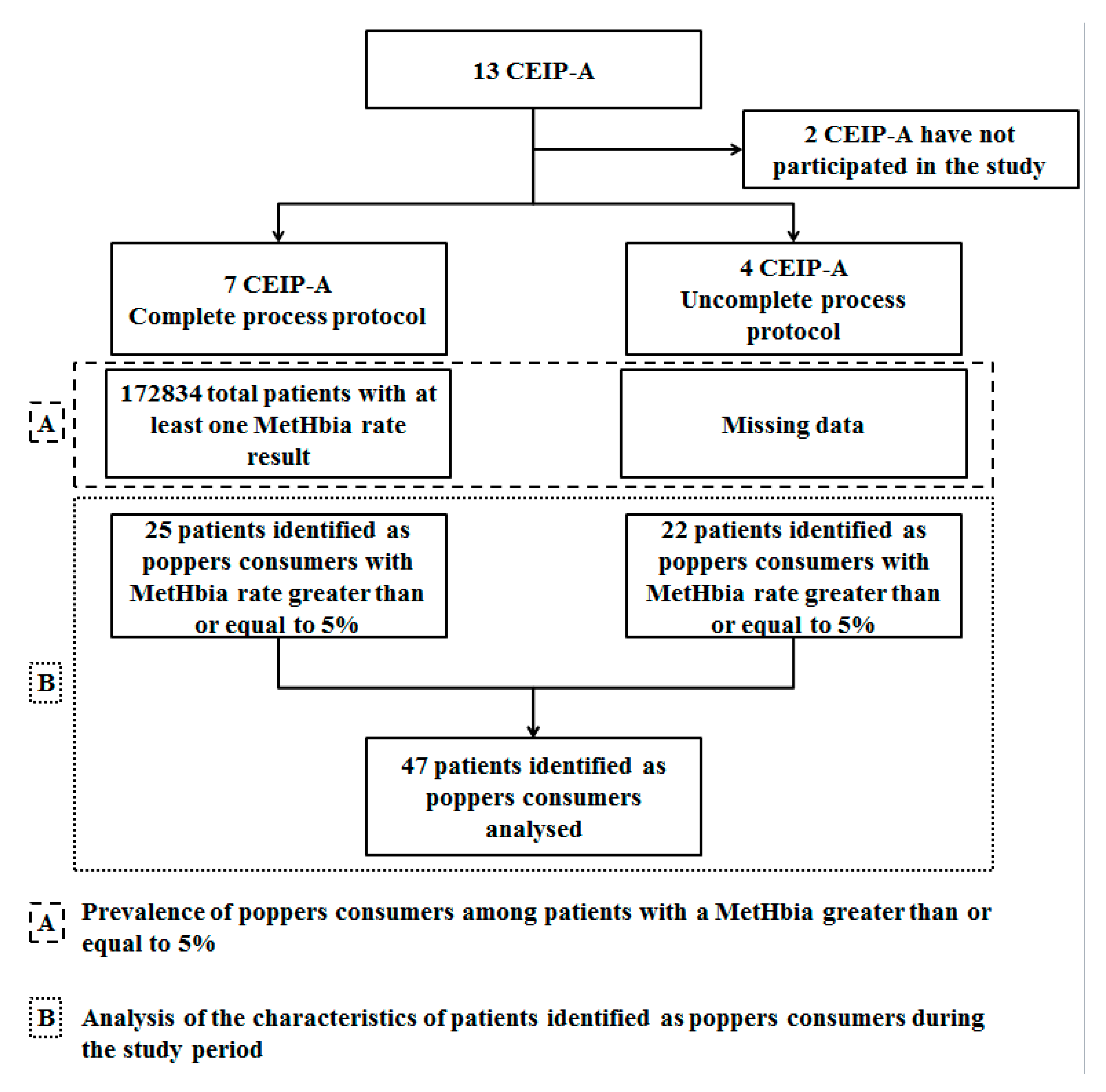
2.1. Stages of the Study
2.1.1. Part (A): Prevalence and Evolution of the Number of Cases of Poppers Consumers among Patients with a MetHbia Greater than or Equal to 5% Assessment
Primary Outcome
Evolution of the Prevalence before and after the Legalization of Poppers in France
Proportion of Poppers Consumers (Reported in Medical Records) According to the MetHbia Level
2.1.2. Part (B): Description of the Characteristics of Cases of Patients Identified as Consuming Poppers during the Study Period
3. Discussion
4. Methods
4.1. Study Oversight
4.2. Patients
4.3. Collected Data
4.3.1. Number of Patients with MetHbia Measurement
4.3.2. Number of Poppers Consumers among Patients with a MetHbia Greater than or Equal to 5%
4.4. Ethics
4.5. Outcomes
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Observatoire Français Des Drogues et Des Toxicomanies (OFDT) Poppers, Colles et Autres Solvants—Synthèse Des Connaissances—OFDT. Available online: https://www.ofdt.fr/produits-et-addictions/de-z/poppers-colles-et-autres-solvants/ (accessed on 30 August 2021).
- Hunter, L.; Gordge, L.; Dargan, P.I.; Wood, D.M. Methaemoglobinaemia Associated with the Use of Cocaine and Volatile Nitrites as Recreational Drugs: A Review. Br. J. Clin. Pharmacol. 2011, 72, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Observatoire français Des Drogues et Des Toxicomanies (OFDT) Evolution de L’usage Au Cours de La Vie de Substances Psychoactives (Hors Alcool, Tabac et Cannabis) Parmi Les 17—OFDT. Available online: https://www.ofdt.fr/statistiques-et-infographie/series-statistiques/evolution-de-l-usage-au-cours-de-la-vie-de-substances-psychoactives-hors-alcool-tabac-et-cannabis-parmi-les-17-ans/ (accessed on 30 August 2021).
- Gérome, C.; Cadet-Taïrou, A.; Gandilhon, M.; Milhet, M.; Martinez, M.; Néfau, T.; Observatoire Français Des Drogues et Des Toxicomanies (OFDT). Substances Psychoactives, Usagers et Marchés: Les Tendances Récentes (2017–2018). Tendances 2018, 129, 8p. [Google Scholar]
- Broady, T.; Mao, L.; Lee, E.; Bavinton, B.; Keen, P.; Bambridge, C.; Mackie, B.; Duck, T.; Cooper, C.; Prestage, G.; et al. Gay Community Periodic Survey: Sydney 2018. Available online: http://unsworks.unsw.edu.au/fapi/datastream/unsworks:52117/binae80f831-8458-4fec-8c2b-1f7ba7402409?view=true (accessed on 13 February 2020).
- Gruener, A.M.; Jeffries, M.A.R.; El Housseini, Z.; Whitefield, L. Poppers Maculopathy. Lancet Lond. Engl. 2014, 384, 1606. [Google Scholar] [CrossRef]
- Bradberry, S.M. Occupational Methaemoglobinaemia. Mechanisms of Production, Features, Diagnosis and Management Including the Use of Methylene Blue. Toxicol. Rev. 2003, 22, 13–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modarai, B.; Kapadia, Y.K.; Kerins, M.; Terris, J. Methylene Blue: A Treatment for Severe Methaemoglobinaemia Secondary to Misuse of Amyl Nitrite. Emerg. Med. J. EMJ 2002, 19, 270–271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranchon, G.; Mollard, F.; Lainé, N.; Malick, P.; Robert, D. Poppers-Induced Methemoglobinemia: An Unusual Cause of Cyanosis. Eur. J. Emerg. Med. 2008, 15, 361–362. [Google Scholar] [CrossRef] [PubMed]
- Davies, A.J.; Borschmann, R.; Kelly, S.P.; Ramsey, J.; Ferris, J.; Winstock, A.R. The Prevalence of Visual Symptoms in Poppers Users: A Global Survey. BMJ Open Ophthalmol. 2017, 1, e000015. [Google Scholar] [CrossRef] [Green Version]
- Hall, A.; Stessel, B.; Bergmans, D.; Schnabel, R. Two Cases of Acquired Methemoglobinemia. Acta Anaesthesiol. Belg. 2012, 63, 97–100. [Google Scholar]
- Janssens, U.; Hillen, S.; Janssens, T.; Grafe, J. Methämoglobinämie nach Inhalation von Poppers. Med. Klin.-Intensivmed. Notf. 2019, 114, 345–349. [Google Scholar] [CrossRef]
- Kragsfeldt, C.T.; Nissen, C.B.; Brandt, F. Methaemoglobinaemia induced by ingestion of alkyl nitrite, “poppers”. Ugeskr. Laeger 2016, 178, 34. [Google Scholar]
- Lefevre, T.; Nuzzo, A.; Mégarbane, B. Poppers-Induced Life-Threatening Methemoglobinemia. Am. J. Respir. Crit. Care Med. 2018, 198, e137–e138. [Google Scholar] [CrossRef] [PubMed]
- McCabe, A.; McCann, B.; Kelly, P. Pop Goes the O2: A Case of Popper-Induced Methaemoglobinamia. BMJ Case Rep. 2012, 2012. [Google Scholar] [CrossRef] [PubMed]
- Baumevieille, M.; Miremont, G.; Haramburu, F.; Maurain, C.; Bégaud, B. The French System of Evaluation of Dependence: Establishment in a Legal System. Therapie 2001, 56, 15–22. [Google Scholar] [PubMed]
- Agence Nationale de Sécurité Des Médicaments et Des Produits de Santé (ANSM), Comité Technique Des Centres d’évaluation et d’information Sur La Pharmacodépendence CT022016013:Résultats de l’enquête sur les poppers. Available online: https://archiveansm.integra.fr/var/ansm_site/storage/original/application/a8d567fe9271f990d0a0bdf42fe2c29f.pdf (accessed on 30 August 2021).
- Agence Nationale de Sécurité Des Médicaments et Des Produits de Santé (ANSM), Comité Technique Des Centres d’Évaluation et d’Information Sur La Pharmacodépendance-Addictovigilance—CT022018033. Available online: https://ansm.sante.fr/var/ansm_site/storage/original/application/ceb01e99d7d498f9182ed4574d4b10eb.pdf (accessed on 27 April 2020).
- Victorri-Vigneau, C.; Trewick, D.; Dejoie, T.; Masson, D.; Bulteau, S.; Rousselet, M.; Sauvaget, A.; Grall-Bronnec, M.; Jolliet, P. Poppers Regulation for Public Sale: No Measure in France Yet. Therapie 2018, 73, 217–221. [Google Scholar] [CrossRef] [PubMed]
- Gerada, C.; Ashworth, M. ABC of Mental Health. Addiction and Dependence—I: Illicit Drugs. BMJ 1997, 315, 297–300. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fonberg, J.D.; Sinha, M. National Cannabis Survey, First Quarter 2019. Available online: https://www150.statcan.gc.ca/n1/daily-quotidien/190502/dq190502a-eng.htm (accessed on 6 October 2021).
- Pain, S.; Chavant, F.; Fauconneau, B.; Guenezan, J.; Marjanovic, N.; Lardeur, J.-Y.; Brunet, B.; Perault-Pochat, M.-C. Dangerous Intoxication after Oral Ingestion of Poppers (Alkyl Nitrites): Two Case Reports. Therapie 2017, 72, 397–399. [Google Scholar] [CrossRef] [PubMed]
- Foroozan, M.; Studer, M.; Splingard, B.; Cuny, J.F.; Barbaud, A.; Schmutz, J.L. Facial dermatitis due to inhalation of Poppers. Ann. Dermatol. Venereol. 2009, 136, 298–299. [Google Scholar] [CrossRef] [PubMed]
- Docherty, G.; Eslami, M.; O’Donnell, H. “Poppers Maculopathy”: A Case Report and Literature Review. Can. J. Ophthalmol. J. Can. Ophtalmol. 2018, 53, e154–e156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Total | Before Regulation Change | After Regulation Change | |||||
|---|---|---|---|---|---|---|---|
| n (%) | January 2012 to December 2017 | From January 2012 to May 2013 | From June 2013 to December 2014 | From January 2015 to December 2015 | From January 2016 to December 2016 | From January 2017 to December 2017 | From June 2013 to December 2017 |
| Total number of patients | 172,834 (100%) | 30,480 (17.63) | 39,817 (23.04) | 30,117 (17.42) | 33,164 (19.19) | 39,196 (22.68) | 142,354 (82.36) |
| Total number of patients with MetHbia ≥ 5% | 239 (0.14) | 42 (0.14) | 57 (0.14) | 41 (0.14) | 48 (0.14) | 51 (0.13) | 197 (0.14) |
| Identified poppers consumption | 25 (10.46) | 2 (4.76) | 9 (15.79) | 3 (7.32) | 5 (7.32) | 6 (11.76) | 23 (11.67) |
| ≥5% and <25% Identified poppers consumption | 220 (92.05) 12/220 | 40 (95.24) | 52 (91.23) | 37 (90.24) | 46 (95.83) | 45 (88.24) | 180 (91.37) |
| ≥25% Identified poppers consumption | 19 (7.95) 13/19 | 2 (4.76) | 5 (8.77) | 4 (9.76) | 2 (4.17) | 6 (11.76) | 17 (8.63) |
| Total Poppers Consumers (n = 47) | Consumers with MetHbia <25% (n = 20) | Consumers with MetHbia ≥25% (n = 27) | |
|---|---|---|---|
| Male Sex, n (%) | 42 (89.4) | 18 (90) | 24 (88.9) |
| Age (years), mean (sd) Min–Max | 35 (10.3) 19–54 | 34 (9.9) 19–54 | 36 (10.5) 19–52 |
| Median of maximum MetHbia level per patient [IQR] Min–Max | 25.1% [20.8–37.7%] 5.4–87.8% | 17.6% [12.625–23.15%] 5.4–24.9% | 31.7% [27–54.4%] b 25–87.8% |
| Mode of administration | |||
| Inhaled only a, n (%) Median of maximum MetHbia level per patient [IQR] Min–Max | 37 (78.7) 25.0% [20.8–28.6%] 5.4–87.8% | 18 (90.0) 19.7% [13.375–23.45%] 5.4–24.9% | 19 (70.4) 28.6% [26.5–48.85%] 25–87.8% |
| Oral only, n (%) Median of maximum MetHbia level per patient [IQR] Min–Max | 9 (19.1) 30.6% [20–57.35%] 11.5–76.9% | 2 (10.0) 12.3% [11.875–12.625%] 11.5–13% | 7 (25.9) 38.8% [30.6–75.9%] b 27–76.9% |
| Combined oral and inhaled, n (%) Median of maximum MetHbia level per patient | 1 (2.1) 31.2% | 0 | 1 (3.7) 31.2% |
| Associated substances consumption, n (%) At least one substance Alcohol Amphetamines Sildenafil Benzodiazepines Cocaine Cannabis NPS | 16 (30.0) 13 (27.7) 4 (8.5) 2 (4.3) 1 (2.1) 1 (2.1) 1 (2.1) 1 (2.1) | 5 (25.0) 4 (20.0) 2 (10.0) 0 0 0 1 (5.0) 1 (5.0) | 11 (40.7) 9 (33.3) 2 (7.4) 2 (7.4) 1 (3.7) 1 (3.7) 0 0 |
| Symptoms, n (%) Cyanosis and/or discoloration Desaturation Respiratory dysfunction Consciousness disorder Malaise Coma Cardiac dysfunction Psychiatric symptoms Dizziness | 32 (68.1) 21 (44.7) 13 (27.7) 12 (25.5) 8 (17.0) 5 (10.6) 6 (12.8) 2 (4.25) c 2 (4.25) | 9 (45.0) 8 (40.0) 5 (25.0) 1 (5.0) 1 (5.0) 2 (10.0) 3 (15.0) 2 (10.0) 0 | 23 (85.2) 13 (48.1) 8 (29.6) 11 (40.7) 7 (25.9) 3 (11.1) 3 (11.1) 0 2 (7.4) |
| Complications n (%) Rhabdomyolysis Hemolytic anemia Serotoninergic syndrome Pulmonary embolism Syncope Cardiorespiratory arrest Toxic encephalopathy | 8 (17.0) 2 (4.3) 2 (4.3) 2 (4.3) 1 (2.1) 1 (2.1) 1 (2.1) 1 (2.1) | 6 (30.0) 2 (10.0) 2 (10.0) 2 (10.0) 1 (5.0) 0 0 1 (5.0) | 2 (7.4) 0 0 0 0 1 (3.7) 1 (3.7) 0 |
| Support, n (%) Methylene blue Oxygen therapy Specialized department Simple monitoring or rehydration Unspecified | 32 (68.1) 27 (57.4) 10 (21.3) 5 (10.6) 1 (2.1) | 11 (55.0) 10 (50.0) 7 (35.0) 3 (15.0) 0 | 21 (77.8) 17 (62.9) 3 (11.1) 2 (7.4) 1 (3.7) |
| Evolution, n (%) Favorable Deceased Unspecified | 43 (91.5) 1 (2.1) 3 (6.4) | 19 (95.0) 0 1 (5.0) | 24 (88.9) 1 (3.7) 2 (7.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrangou-Poueys-Darlas, M.; Gerardin, M.; Deheul, S.; Istvan, M.; Guerlais, M.; FAN; Jolliet, P.; Dejoie, T.; Victorri-Vigneau, C. Poppers Use and High Methaemoglobinaemia: ‘Dangerous Liaisons’. Pharmaceuticals 2021, 14, 1061. https://doi.org/10.3390/ph14101061
Barrangou-Poueys-Darlas M, Gerardin M, Deheul S, Istvan M, Guerlais M, FAN, Jolliet P, Dejoie T, Victorri-Vigneau C. Poppers Use and High Methaemoglobinaemia: ‘Dangerous Liaisons’. Pharmaceuticals. 2021; 14(10):1061. https://doi.org/10.3390/ph14101061
Chicago/Turabian StyleBarrangou-Poueys-Darlas, Malcolm, Marie Gerardin, Sylvie Deheul, Marion Istvan, Marylène Guerlais, FAN, Pascale Jolliet, Thomas Dejoie, and Caroline Victorri-Vigneau. 2021. "Poppers Use and High Methaemoglobinaemia: ‘Dangerous Liaisons’" Pharmaceuticals 14, no. 10: 1061. https://doi.org/10.3390/ph14101061
APA StyleBarrangou-Poueys-Darlas, M., Gerardin, M., Deheul, S., Istvan, M., Guerlais, M., FAN, Jolliet, P., Dejoie, T., & Victorri-Vigneau, C. (2021). Poppers Use and High Methaemoglobinaemia: ‘Dangerous Liaisons’. Pharmaceuticals, 14(10), 1061. https://doi.org/10.3390/ph14101061





