Human Recombinant FSH and Its Biosimilars: Clinical Efficacy, Safety, and Cost-Effectiveness in Controlled Ovarian Stimulation for In Vitro Fertilization
Abstract
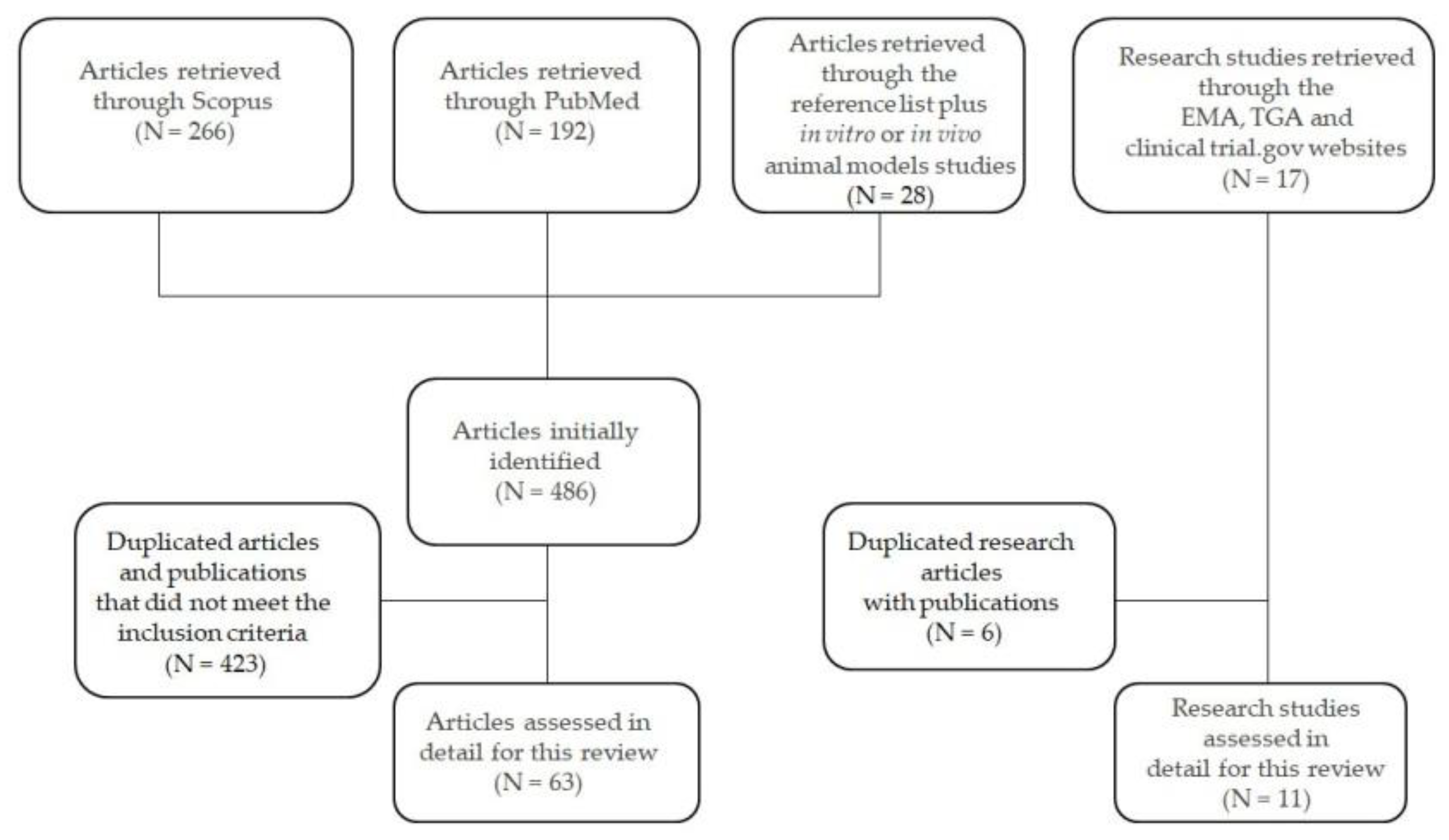
1. Introduction
2. Structure of hFSH
3. hFSH as a Medication: Historical Background
4. Recombinant Human FSH (r-hFSH)
5. Biosimilar r-hFSH (Follitropin α)
6. Clinical Trials Comparing Follitropin α Biosimilars vs. Originator
7. Cost-Effectiveness Evaluation of Follitropin α Biosimilars vs. Originator in the European Context
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Daya, S. Follicle-stimulating hormone in clinical practice: An update. Treat. Endocrinol. 2004, 3, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Santi, D.; Potì, F.; Simoni, M.; Casarini, L. Pharmacogenetics of G-protein-coupled receptors variants: FSH receptor and infertility treatment. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Leão, R.B.; Esteves, S.C. Gonadotropin therapy in assisted reproduction: An evolutionary perspective from biologics to biotech. Clinics 2014, 69, 279–293. [Google Scholar] [CrossRef]
- Cai, Q.; Wan, F.; Huang, K.; Zhang, H. Does the Number of Oocytes Retrieved Influence Pregnancy after Fresh Embryo Transfer? PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
- Sunkara, S.K.; Rittenberg, V.; Raine-Fenning, N.; Bhattacharya, S.; Zamora, J.; Coomarasamy, A. Association between the number of eggs and live birth in IVF treatment: An analysis of 400 135 treatment cycles. Hum. Reprod. Oxf. Engl. 2011, 26, 1768–1774. [Google Scholar] [CrossRef] [PubMed]
- Butnev, V.Y.; Butnev, V.Y.; May, J.V.; Shuai, B.; Tran, P.; White, W.K.; Brown, A.; Smalter Hall, A.; Harvey, D.J.; Bousfield, G.R. Production, purification, and characterization of recombinant hFSH glycoforms for functional studies. Mol. Cell. Endocrinol. 2015, 405, 42–51. [Google Scholar] [CrossRef]
- Olijve, W.; de Boer, W.; Mulders, J.W.; van Wezenbeek, P.M. Molecular biology and biochemistry of human recombinant follicle stimulating hormone (Puregon). Mol. Hum. Reprod. 1996, 2, 371–382. [Google Scholar] [CrossRef] [PubMed]
- Morell, A.G.; Gregoriadis, G.; Scheinberg, I.H.; Hickman, J.; Ashwell, G. The role of sialic acid in determining the survival of glycoproteins in the circulation. J. Biol. Chem. 1971, 246, 1461–1467. [Google Scholar] [PubMed]
- Andersen, C.Y.; Westergaard, L.G.; van Wely, M. FSH isoform composition of commercial gonadotrophin preparations: A neglected aspect? Reprod. Biomed. Online 2004, 9, 231–236. [Google Scholar] [CrossRef]
- Lombardi, A.; Andreozzi, C.; Pavone, V.; Triglione, V.; Angiolini, L.; Caccia, P. Evaluation of the oligosaccharide composition of commercial follicle stimulating hormone preparations. Electrophoresis 2013, 34, 2394–2406. [Google Scholar] [CrossRef]
- Bousfield, G.R.; Butnev, V.Y.; Rueda-Santos, M.A.; Brown, A.; Hall, A.S.; Harvey, D.J. Macro- and Micro-heterogeneity in Pituitary and Urinary Follicle-Stimulating Hormone Glycosylation. J. Glycomics Lipidomics 2014, 4. [Google Scholar] [CrossRef]
- Jiang, C.; Hou, X.; Wang, C.; May, J.V.; Butnev, V.Y.; Bousfield, G.R.; Davis, J.S. Hypoglycosylated hFSH Has Greater Bioactivity Than Fully Glycosylated Recombinant hFSH in Human Granulosa Cells. J. Clin. Endocrinol. Metab. 2015, 100, E852–E860. [Google Scholar] [CrossRef] [PubMed]
- Riccetti, L.; Sperduti, S.; Lazzaretti, C.; Klett, D.; De Pascali, F.; Paradiso, E.; Limoncella, S.; Potì, F.; Tagliavini, S.; Trenti, T.; et al. Glycosylation Pattern and in vitro Bioactivity of Reference Follitropin alfa and Biosimilars. Front. Endocrinol. 2019, 10, 503. [Google Scholar] [CrossRef]
- Bousfield, G.R.; May, J.V.; Davis, J.S.; Dias, J.A.; Kumar, T.R. In Vivo and In Vitro Impact of Carbohydrate Variation on Human Follicle-Stimulating Hormone Function. Front. Endocrinol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Bassett, R.M.; Driebergen, R. Continued improvements in the quality and consistency of follitropin alfa, recombinant human FSH. Reprod. Biomed. Online 2005, 10, 169–177. [Google Scholar] [CrossRef]
- Revelli, A.; Pettinau, G.; Basso, G.; Carosso, A.; Ferrero, A.; Dallan, C.; Canosa, S.; Gennarelli, G.; Guidetti, D.; Filippini, C.; et al. Controlled Ovarian Stimulation with recombinant-FSH plus recombinant-LH vs. human Menopausal Gonadotropin based on the number of retrieved oocytes: Results from a routine clinical practice in a real-life population. Reprod. Biol. Endocrinol. RBE 2015, 13, 77. [Google Scholar] [CrossRef]
- Daya, S. Updated meta-analysis of recombinant follicle-stimulating hormone (FSH) versus urinary FSH for ovarian stimulation in assisted reproduction. Fertil. Steril. 2002, 77, 711–714. [Google Scholar] [CrossRef]
- Keene, J.L.; Matzuk, M.M.; Otani, T.; Fauser, B.C.; Galway, A.B.; Hsueh, A.J.; Boime, I. Expression of biologically active human follitropin in Chinese hamster ovary cells. J. Biol. Chem. 1989, 264, 4769–4775. [Google Scholar] [PubMed]
- Hugues, J.N.; Durnerin, I.C. Gonadotrophins--filled-by-mass versus filled-by-bioassay. Reprod. Biomed. Online 2005, 10 (Suppl. 3), 11–17. [Google Scholar] [CrossRef]
- GONAL-f. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/gonal-f (accessed on 21 May 2020).
- Puregon. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/puregon (accessed on 21 May 2020).
- Follistim AQ (follitropin beta) FDA Approval History. Available online: https://www.drugs.com/history/follistim-aq.html (accessed on 21 May 2020).
- Rekovelle | European Medicines Agency. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/rekovelle (accessed on 16 May 2020).
- Goa, K.L.; Wagstaff, A.J. Follitropin alpha in infertility: A review. BioDrugs Clin. Immunother. Biopharm. Gene Ther. 1998, 9, 235–260. [Google Scholar] [CrossRef]
- Olsson, H.; Sandström, R.; Grundemar, L. Different pharmacokinetic and pharmacodynamic properties of recombinant follicle-stimulating hormone (rFSH) derived from a human cell line compared with rFSH from a non-human cell line. J. Clin. Pharmacol. 2014, 54, 1299–1307. [Google Scholar] [CrossRef] [PubMed]
- Koechling, W.; Plaksin, D.; Croston, G.E.; Jeppesen, J.V.; Macklon, K.T.; Andersen, C.Y. Comparative pharmacology of a new recombinant FSH expressed by a human cell line. Endocr. Connect. 2017, 6, 297–305. [Google Scholar] [CrossRef]
- Mochtar, M.H.; Danhof, N.A.; Ayeleke, R.O.; Van der Veen, F.; van Wely, M. Recombinant luteinizing hormone (rLH) and recombinant follicle stimulating hormone (rFSH) for ovarian stimulation in IVF/ICSI cycles. Cochrane Database Syst. Rev. 2017, 5, CD005070. [Google Scholar] [CrossRef]
- Bordewijk, E.M.; Mol, F.; van der Veen, F.; Van Wely, M. Required amount of rFSH, HP-hMG and HP-FSH to reach a live birth: A systematic review and meta-analysis. Hum. Reprod. Open 2019, 2019, hoz008. [Google Scholar] [CrossRef]
- Mignini Renzini, M.; Brigante, C.; Coticchio, G.; Dal Canto, M.; Caliari, I.; Comi, R.; De Ponti, E.; Fadini, R. Retrospective analysis of treatments with recombinant FSH and recombinant LH versus human menopausal gonadotropin in women with reduced ovarian reserve. J. Assist. Reprod. Genet. 2017, 34, 1645–1651. [Google Scholar] [CrossRef] [PubMed]
- Weiss, N.S.; Nahuis, M.; Bayram, N.; Mol, B.W.J.; Van der Veen, F.; van Wely, M. Gonadotrophins for ovulation induction in women with polycystic ovarian syndrome. Cochrane Database Syst. Rev. 2015, CD010290. [Google Scholar] [CrossRef] [PubMed]
- Hugues, J.-N. Recombinant human follicle-stimulating hormone: A scientific step to clinical improvement. Reprod. Biomed. Online 2001, 2, 54–64. [Google Scholar] [CrossRef]
- Rekovelle. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/rekovelle (accessed on 17 May 2020).
- Administration, A.G.D. of H.T.G. Search the TGA Website. Available online: http://www.tga.gov.au/search/node (accessed on 21 May 2020).
- Lunenfeld, B.; Bilger, W.; Longobardi, S.; Alam, V.; D’Hooghe, T.; Sunkara, S.K. The Development of Gonadotropins for Clinical Use in the Treatment of Infertility. Front. Endocrinol. 2019, 10. [Google Scholar] [CrossRef]
- Cole, L.A. hCG, the wonder of today’s science. Reprod. Biol. Endocrinol. RBE 2012, 10, 24. [Google Scholar] [CrossRef]
- Sacchi, S.; Tenedini, E.; Tondelli, D.; Parenti, S.; Tagliasacchi, D.; Xella, S.; Marsella, T.; Tagliafico, E.; Marca, A.L. Gene expression profiles of human granulosa cells treated with bioequivalent doses of corifollitropin alfa (CFA) or recombinant human follicle-stimulating hormone (recFSH). Gynecol. Endocrinol. 2019, 35, 623–627. [Google Scholar] [CrossRef]
- Abd-Elaziz, K.; Duijkers, I.; Stöckl, L.; Dietrich, B.; Klipping, C.; Eckert, K.; Goletz, S. A new fully human recombinant FSH (follitropin epsilon): Two phase I randomized placebo and comparator-controlled pharmacokinetic and pharmacodynamic trials. Hum. Reprod. Oxf. Engl. 2017, 32, 1639–1647. [Google Scholar] [CrossRef] [PubMed]
- Griesinger, G.; Dietrich, B.; Stöckl, L.; Eckert, K.; Goletz, S.; Tandler-Schneider, A. Fully human glyco-optimized recombinant FSH (follitropin epsilon) – a randomized, comparator-controlled phase II clinical trial. Reprod. Biomed. Online 2020, 40, 331–341. [Google Scholar] [CrossRef] [PubMed]
- Harlin, J.; Csemiczky, G.; Wramsby, H.; Fried, G. Recombinant follicle stimulating hormone in in-vitro fertilization treatment-clinical experience with follitropin alpha and follitropin beta. Hum. Reprod. Oxf. Engl. 2000, 15, 239–244. [Google Scholar] [CrossRef] [PubMed]
- Brinsden, P.; Akagbosu, F.; Gibbons, L.M.; Lancaster, S.; Gourdon, D.; Engrand, P.; Loumaye, E. A comparison of the efficacy and tolerability of two recombinant human follicle-stimulating hormone preparations in patients undergoing in vitro fertilization-embryo transfer. Fertil. Steril. 2000, 73, 114–116. [Google Scholar] [CrossRef]
- Nyboe Andersen, A.; Nelson, S.M.; Fauser, B.C.J.M.; García-Velasco, J.A.; Klein, B.M.; Arce, J.-C.; ESTHER-1 Study Group. Individualized versus conventional ovarian stimulation for in vitro fertilization: A multicenter, randomized, controlled, assessor-blinded, phase 3 noninferiority trial. Fertil. Steril. 2017, 107, 387–396. [Google Scholar] [CrossRef] [PubMed]
- Beligotti, F. Commentary: The Development of Gonadotropins for Clinical Use in the Treatment of Infertility. Front. Endocrinol. 2020, 11, 151. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Sánchez, M.; Visnova, H.; Yuzpe, A.; Klein, B.M.; Mannaerts, B.; Arce, J.-C.; ESTHER-1 and ESTHER-2 Study Group. Individualization of the starting dose of follitropin delta reduces the overall OHSS risk and/or the need for additional preventive interventions: Cumulative data over three stimulation cycles. Reprod. Biomed. Online 2019, 38, 528–537. [Google Scholar] [CrossRef] [PubMed]
- Bosch, E.; Havelock, J.; Martin, F.S.; Rasmussen, B.B.; Klein, B.M.; Mannaerts, B.; Arce, J.-C.; ESTHER-2 Study Group. Follitropin delta in repeated ovarian stimulation for IVF: A controlled, assessor-blind Phase 3 safety trial. Reprod. Biomed. Online 2019, 38, 195–205. [Google Scholar] [CrossRef]
- Out, H.J.; Mannaerts, B.M.; Driessen, S.G.; Bennink, H.J. A prospective, randomized, assessor-blind, multicentre study comparing recombinant and urinary follicle stimulating hormone (Puregon versus Metrodin) in in-vitro fertilization. Hum. Reprod. Oxf. Engl. 1995, 10, 2534–2540. [Google Scholar] [CrossRef]
- Revelli, A.; Pittatore, G.; Casano, S.; Canosa, S.; Evangelista, F.; Benedetto, C. Efficacy and safety of late-start Corifollitropin-alfa administration for controlled ovarian hyperstimulation in IVF: A cohort, case-control study. J. Assist. Reprod. Genet. 2015, 32, 429–434. [Google Scholar] [CrossRef][Green Version]
- Revelli, A.; Gennarelli, G.; Sestero, M.; Canosa, S.; Carosso, A.; Salvagno, F.; Pittatore, G.; Filippini, C.; Benedetto, C. A prospective randomized trial comparing corifollitropin-α late-start (day 4) versus standard administration (day 2) in expected poor, normal, and high responders undergoing controlled ovarian stimulation for IVF. J. Assist. Reprod. Genet. 2020, 37, 1163–1170. [Google Scholar] [CrossRef] [PubMed]
- Weise, M.; Bielsky, M.-C.; De Smet, K.; Ehmann, F.; Ekman, N.; Narayanan, G.; Heim, H.-K.; Heinonen, E.; Ho, K.; Thorpe, R.; et al. Biosimilars-why terminology matters. Nat. Biotechnol. 2011, 29, 690–693. [Google Scholar] [CrossRef]
- Research, C. for D.E. and Scientific Considerations in Demonstrating Biosimilarity to a Reference Product. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/scientific-considerations-demonstrating-biosimilarity-reference-product (accessed on 5 May 2020).
- Kuhlmann, M.; Covic, A. The protein science of biosimilars. Nephrol. Dial. Transplant. Off. Publ. Eur. Dial. Transpl. Assoc. Eur. Ren. Assoc. 2006, 21 (Suppl. 5), v4–v8. [Google Scholar] [CrossRef] [PubMed]
- Mellstedt, H.; Niederwieser, D.; Ludwig, H. The challenge of biosimilars. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2008, 19, 411–419. [Google Scholar] [CrossRef]
- Schiestl, M.; Stangler, T.; Torella, C.; Cepeljnik, T.; Toll, H.; Grau, R. Acceptable changes in quality attributes of glycosylated biopharmaceuticals. Nat. Biotechnol. 2011, 29, 310–312. [Google Scholar] [CrossRef]
- de Mora, F.; Fauser, B.C.J.M. Biosimilars to recombinant human FSH medicines: Comparable efficacy and safety to the original biologic. Reprod. Biomed. Online 2017, 35, 81–86. [Google Scholar] [CrossRef] [PubMed]
- Santi, D.; Simoni, M. Biosimilar recombinant follicle stimulating hormones in infertility treatment. Expert Opin. Biol. Ther. 2014, 14, 1399–1409. [Google Scholar] [CrossRef] [PubMed]
- Winstel, R.; Wieland, J.; Gertz, B.; Mueller, A.; Allgaier, H. Manufacturing of Recombinant Human Follicle-Stimulating Hormone Ovaleap® (XM17), Comparability with Gonal-f®, and Performance/Consistency. Drugs RD 2017, 17, 305–312. [Google Scholar] [CrossRef][Green Version]
- Anonymous Bemfola. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/bemfola (accessed on 9 May 2020).
- Announcements Richter acquires all Bemfola® rights in respect of US. Available online: https://www.richter.hu/en-US/investors/announcements/Pages/extraord180710.aspx (accessed on 26 May 2020).
- Gloaguen, P.; Crépieux, P.; Heitzler, D.; Poupon, A.; Reiter, E. Mapping the Follicle-Stimulating Hormone-Induced Signaling Networks. Front. Endocrinol. 2011, 2. [Google Scholar] [CrossRef]
- Ayoub, M.A.; Landomiel, F.; Gallay, N.; Jégot, G.; Poupon, A.; Crépieux, P.; Reiter, E. Assessing Gonadotropin Receptor Function by Resonance Energy Transfer-Based Assays. Front. Endocrinol. 2015, 6, 130. [Google Scholar] [CrossRef]
- Jonas, K.C.; Chen, S.; Virta, M.; Mora, J.; Franks, S.; Huhtaniemi, I.; Hanyaloglu, A.C. Temporal reprogramming of calcium signalling via crosstalk of gonadotrophin receptors that associate as functionally asymmetric heteromers. Sci. Rep. 2018, 8, 2239. [Google Scholar] [CrossRef] [PubMed]
- Orvieto, R.; Seifer, D.B. Biosimilar FSH preparations- are they identical twins or just siblings? Reprod. Biol. Endocrinol. RBE 2016, 14. [Google Scholar] [CrossRef] [PubMed]
- Ovaleap. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/ovaleap (accessed on 17 May 2020).
- Strowitzki, T.; Kuczynski, W.; Mueller, A.; Bias, P. Randomized, active-controlled, comparative phase 3 efficacy and safety equivalence trial of Ovaleap® (recombinant human follicle-stimulating hormone) in infertile women using assisted reproduction technology (ART). Reprod. Biol. Endocrinol. RBE 2016, 14, 1. [Google Scholar] [CrossRef] [PubMed]
- Wolzt, M.; Gouya, G.; Sator, M.; Hemetsberger, T.; Irps, C.; Rettenbacher, M.; Vcelar, B. Comparison of pharmacokinetic and safety profiles between Bemfola(®) and Gonal-f(®) after subcutaneous application. Eur. J. Drug Metab. Pharmacokinet. 2016, 41, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Rettenbacher, M.; Andersen, A.N.; Garcia-Velasco, J.A.; Sator, M.; Barri, P.; Lindenberg, S.; van der Ven, K.; Khalaf, Y.; Bentin-Ley, U.; Obruca, A.; et al. A multi-centre phase 3 study comparing efficacy and safety of Bemfola(®) versus Gonal-f(®) in women undergoing ovarian stimulation for IVF. Reprod. Biomed. Online 2015, 30, 504–513. [Google Scholar] [CrossRef]
- Mastrangeli, R.; Satwekar, A.; Cutillo, F.; Ciampolillo, C.; Palinsky, W.; Longobardi, S. In-vivo biological activity and glycosylation analysis of a biosimilar recombinant human follicle-stimulating hormone product (Bemfola) compared with its reference medicinal product (GONAL-f). PLoS ONE 2017, 12, e0184139. [Google Scholar] [CrossRef] [PubMed]
- Biosimilar Versus Urinary Gonadotropins—Full Text View—ClinicalTrials.gov. Available online: https://clinicaltrials.gov/ct2/show/NCT02503605 (accessed on 17 May 2020).
- Barakhoeva, Z.; Vovk, L.; Fetisova, Y.; Marilova, N.; Ovchinnikova, M.; Tischenko, M.; Scherbatyuk, Y.; Kolotovkina, A.; Miskun, A.; Kasyanova, G.; et al. A multicenter, randomized, phase III study comparing the efficacy and safety of follitropin alpha biosimilar and the original follitropin alpha. Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 241, 6–12. [Google Scholar] [CrossRef]
- Moon, S.Y.; Choi, Y.S.; Ku, S.-Y.; Kim, S.H.; Choi, Y.M.; Kang, I.S.; Kim, C.H. Comparison of the efficacy and safety of a new recombinant human follicle-stimulating hormone (DA-3801) with follitropin-alpha (Gonal-F) in women undergoing controlled ovarian hyperstimulation for assisted reproductive technology. J. Obstet. Gynaecol. Res. 2007, 33, 305–315. [Google Scholar] [CrossRef]
- Gizzo, S.; Garcia-Velasco, J.A.; Heiman, F.; Ripellino, C.; Bühler, K. A cost-effectiveness evaluation comparing originator follitropin alfa to the biosimilar for the treatment of infertility. Int. J. Womens Health 2016, 8, 683–689. [Google Scholar] [CrossRef]
- Grynberg, M.; Murphy, C.; Doré, C.; Fresneau, L.; Paillet, S.; Petrica, N.; Frédérique, M.; Ravonimbola, H. A cost-effectiveness analysis comparing the originator follitropin alfa to its biosimilars in patients undergoing a medically assisted reproduction program from a French perspective. J. Med. Econ. 2018, 1–15. [Google Scholar] [CrossRef]
- Xue, W.; Lloyd, A.; Falla, E.; Roeder, C.; Papsch, R.; Bühler, K. A cost-effectiveness evaluation of the originator follitropin alpha compared to the biosimilars for assisted reproduction in Germany. Int. J. Womens Health 2019, 11, 319–331. [Google Scholar] [CrossRef] [PubMed]
- Christianson, M.S.; Shoham, G.; Tobler, K.J.; Zhao, Y.; Monseur, B.; Leong, M.; Shoham, Z. Use of various gonadotropin and biosimilar formulations for in vitro fertilization cycles: Results of a worldwide Web-based survey. J. Assist. Reprod. Genet. 2017, 34, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- Ulloa-Aguirre, A.; Reiter, E.; Crépieux, P. FSH Receptor Signaling: Complexity of Interactions and Signal Diversity. Endocrinology 2018, 159, 3020–3035. [Google Scholar] [CrossRef] [PubMed]
| Drug Name | NCT Number | Title | Status/Country | Study Results | Study Design | Outcome Measures |
|---|---|---|---|---|---|---|
| OVALEAP® | NCT02809989 | A study to evaluate the effect of Ovaleap® on the pregnancy rate and clinical effects as well as the user-friendliness of the Ovaleap®-Pen | Completed in 2018 Germany | Results available [63] | Study Type: Observational Observational model: Single group prospective treatment cohort Enrolment: 507 participants (18–40 years) Drug: Ovaleap® |
|
| AFOLIA® | NCT02459418 | Comparative pharmacokinetics of AFOLIA and US Gonal-F® RFF redi-ject after single subcutaneous application | Completed in 2016 United Kingdom | Results available [64] | Study Type: Interventional Phase: Phase I Allocation: Randomized Intervention model: Crossover assignment Masking: None (Open Label) Enrolment: 42 participants (18-42 years) Drugs: Afolia, Gonal-F® |
|
| FOLIA® | NCT01687712 | Phase III study comparing efficacy and safety of AFOLIA vs. Gonal-F® RFF in women (35 to 42) undergoing IVF | Completed in 2016 United States | Results available, not published yet | Study Type: Interventional Phase: Phase III Allocation: Randomized Intervention model: Parallel Assignment Masking: Double (Investigator, Outcomes Assessor) Enrolment: 1100 participants (35–42 years) Drugs: Afolia, Gonal- F® |
|
| AFOLIA® | NCT01141270 | Comparative pharmacokinetics of AFOLIA and Gonal-F® | Completed in 2010 Austria | No results available | Study Type: Interventional Phase: Phase I Allocation: Randomized Intervention model: Crossover assignment Masking: None (Open Label) Enrolment: 32 participants (18–38 years) Drugs: Afolia, Gonal-F® |
|
| AFOLIA® | NCT01121666 | Multi-centre study to compare efficacy and safety of AFOLIA and Gonal-F® in women | Completed in 2013 Austria, Germany | Results available [65] | Study Type: Interventional Phase: Phase III Allocation: Randomized Intervention model: Parallel Assignment Masking: Single (Outcomes Assessor) Enrolment: 460 participants (20–38 years) Drugs: Afolia, Gonal- F® |
|
| BEMFOLA® | NCT02942849 | Post-authorisation study on the use of Bemfola® in human assisted reproductive technology | Completed in 2018 Germany | No results available | Study Type: Observational Observational model: cohort, prospective Enrolment: 1195 participants (≥18 years) Drug: Bemfola® |
|
| BEMFOLA® | NCT03767218 | Ignition of ovarian stimulation with recombinant human FSH (Bemfola) in the late follicular phase | Recruitment completed in 2020 | No results available | Study Type: Interventional Phase: Phase III Allocation: Randomized Intervention model: Two-arm design with 1:1 Masking: None (Open Label) Enrolment: 40 participants (18–36 years) Drug: Bemfola® |
|
| BEMFOLA® | NCT02941341 | Observational post- authorisation study on the use of Bemfola® in human assisted reproductive techniques in Spain | Completed in 2020 Germany | No results available | Study Type: Observational Observational model: cohort, prospective Enrolment: 1222participants (≥18 years) Drug: Bemfola® |
|
| BEMFOLA® | NCT02503605 | Biosimilar versus urinary gonadotropins study documents | Unknown Spain | No results available | Study Type: Interventional Phase: Phase IV Allocation: Randomized Intervention model: Parallel Assignment Masking: None (Open Label) Enrolment: 130 participants (18–35 years) Drugs: Bemfola®, urinary FSH |
|
| BEMFOLA® | NCT02625519 | Efficacy of urinary vs. recombinant FSH in oocyte donors based on receptor N680S FSH gene polymorphism (genodon trial) | Completed in 2019 Spain | No results available | Study Type: Interventional Phase: Phase IV Allocation: Randomized Intervention model: Parallel Assignment Masking: None (Open Label) Enrolment: 180 participants (18-30 years) Drugs: Bemfola®, urinary hFSH, |
|
| FOSTIPUR® | NCT02785822 | Study to Compare hFSH- HP (Fostipur) and hMG HP (Meriofert) in patients with polycystic ovary under a IVF/CSI cycle | Completed in 2018 Spain | No results available | Study Type: Interventional Phase: Phase IV Allocation: Randomized Intervention model: Parallel assignment Masking: Single (Investigator) Enrolment: 19 participants (18–38 years) Drugs: Fostipur®, hMG-HP |
|
| PRIMAPUR® | NCT03857230 | The safety and pharmacokinetics of Primapur® and Gonal-F® | Completed in 2019 Russia | Results available [68] | Study Type: Interventional Phase: Phase I Allocation: Randomized Intervention model: Crossover Assignment Masking: None (Open Label) Enrolment: 28 participants (18–40 years) Drugs: Primapur®, Gonal- F® |
|
| PRIMAPUR® | NCT03088137 | Study to compare efficacy and safety of Primapur® and Gonal-F® in women for assisted reproductive treatment | Completed in 2018 Russia | Results available [68] | Study Type: Interventional Phase: Phase III Allocation: Randomized Intervention model: Parallel Assignment Masking: Single (Outcomes Assessor) Enrolment: 118 participants (20–35 years) Drugs: Primapur®, Gonal- F® |
|
| DA-3801® | NCT01820728 | A Phase III clinical study to compare the efficac and safety of DA-3801 and that of Gonal-F® | Completed in 2012 Korea | Results available [69] | Study Type: Interventional Phase: Phase III Allocation: Randomized Intervention model: Parallel Assignment Masking: None (Open Label) Enrollment: 93 participants (20–38 years) Drugs: DA-3801, Gonal-F® |
|
| FOLITIME® | NCT02454556 | A randomized, multicentre, open label, evaluator blinded study to evaluate safety and efficacy of Folitime® of Gemabiotech S.A. versus Gonal-F® of Merck Serono, in patients with infertility undergoing ART | Completed in 2016 Argentina | No results available | Study Type: Interventional Phase: Phase III Allocation: Randomized Intervention model: Parallel Assignment Masking: Single (Outcomes Assessor) Enrollment: 106 participants (18–37 years) Drugs: FOLITIME®, Gonal-F® |
|
| LM-001® | NCT03535103 | Study on the safety and pharmacokinetics of LM001 and Gonal-F® in healthy women | Unknown Argentina | No results available | Study Type: Interventional Phase: Phase I Allocation: Randomized Intervention model: Crossover Assignment Masking: None (Open Label) Enrollment: 32 participants (18–40 years) Drugs: LM001, Gonal-F® |
|
| GONAPUR® | NCT03057574 | Gonapure® in multifollicular stimulation in Egyptian women undergoing IVF/ICSI | Unknown Egypt | No results available | Study Type: Interventional Phase: Phase 4 Allocation: N/A Intervention model: Single Group Assignment Masking: None (Open Label) Enrollment: 200 participants (18–38 years) Drug: Gonapure® |
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bergandi, L.; Canosa, S.; Carosso, A.R.; Paschero, C.; Gennarelli, G.; Silvagno, F.; Benedetto, C.; Revelli, A. Human Recombinant FSH and Its Biosimilars: Clinical Efficacy, Safety, and Cost-Effectiveness in Controlled Ovarian Stimulation for In Vitro Fertilization. Pharmaceuticals 2020, 13, 136. https://doi.org/10.3390/ph13070136
Bergandi L, Canosa S, Carosso AR, Paschero C, Gennarelli G, Silvagno F, Benedetto C, Revelli A. Human Recombinant FSH and Its Biosimilars: Clinical Efficacy, Safety, and Cost-Effectiveness in Controlled Ovarian Stimulation for In Vitro Fertilization. Pharmaceuticals. 2020; 13(7):136. https://doi.org/10.3390/ph13070136
Chicago/Turabian StyleBergandi, Loredana, Stefano Canosa, Andrea Roberto Carosso, Carlotta Paschero, Gianluca Gennarelli, Francesca Silvagno, Chiara Benedetto, and Alberto Revelli. 2020. "Human Recombinant FSH and Its Biosimilars: Clinical Efficacy, Safety, and Cost-Effectiveness in Controlled Ovarian Stimulation for In Vitro Fertilization" Pharmaceuticals 13, no. 7: 136. https://doi.org/10.3390/ph13070136
APA StyleBergandi, L., Canosa, S., Carosso, A. R., Paschero, C., Gennarelli, G., Silvagno, F., Benedetto, C., & Revelli, A. (2020). Human Recombinant FSH and Its Biosimilars: Clinical Efficacy, Safety, and Cost-Effectiveness in Controlled Ovarian Stimulation for In Vitro Fertilization. Pharmaceuticals, 13(7), 136. https://doi.org/10.3390/ph13070136








