Histological Effects of Intravitreal Injection of Antifungal Agents in New Zealand White Rabbits: An Electron Microscopic and Immunohistochemical Study
Abstract
1. Introduction
2. Results
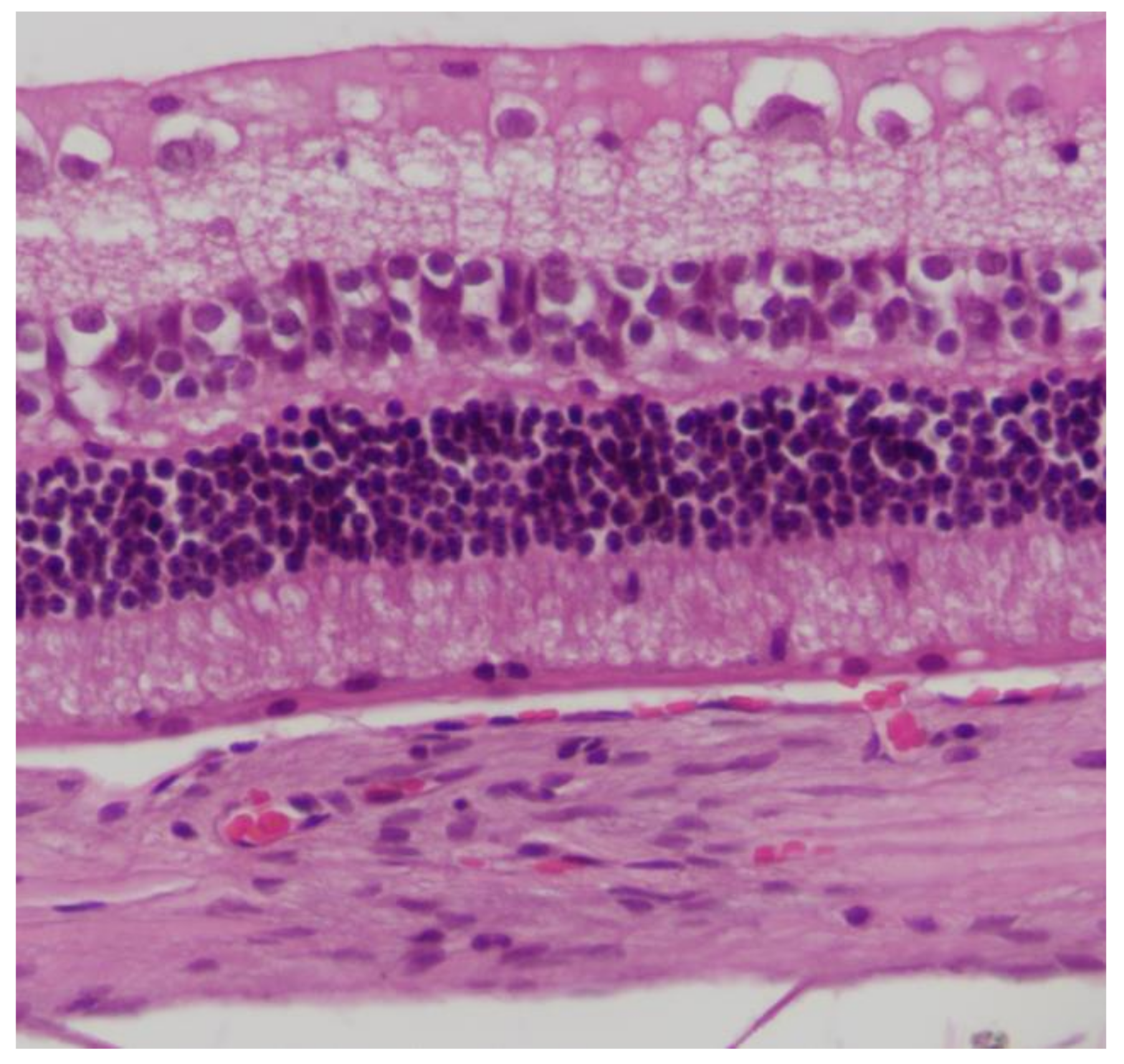
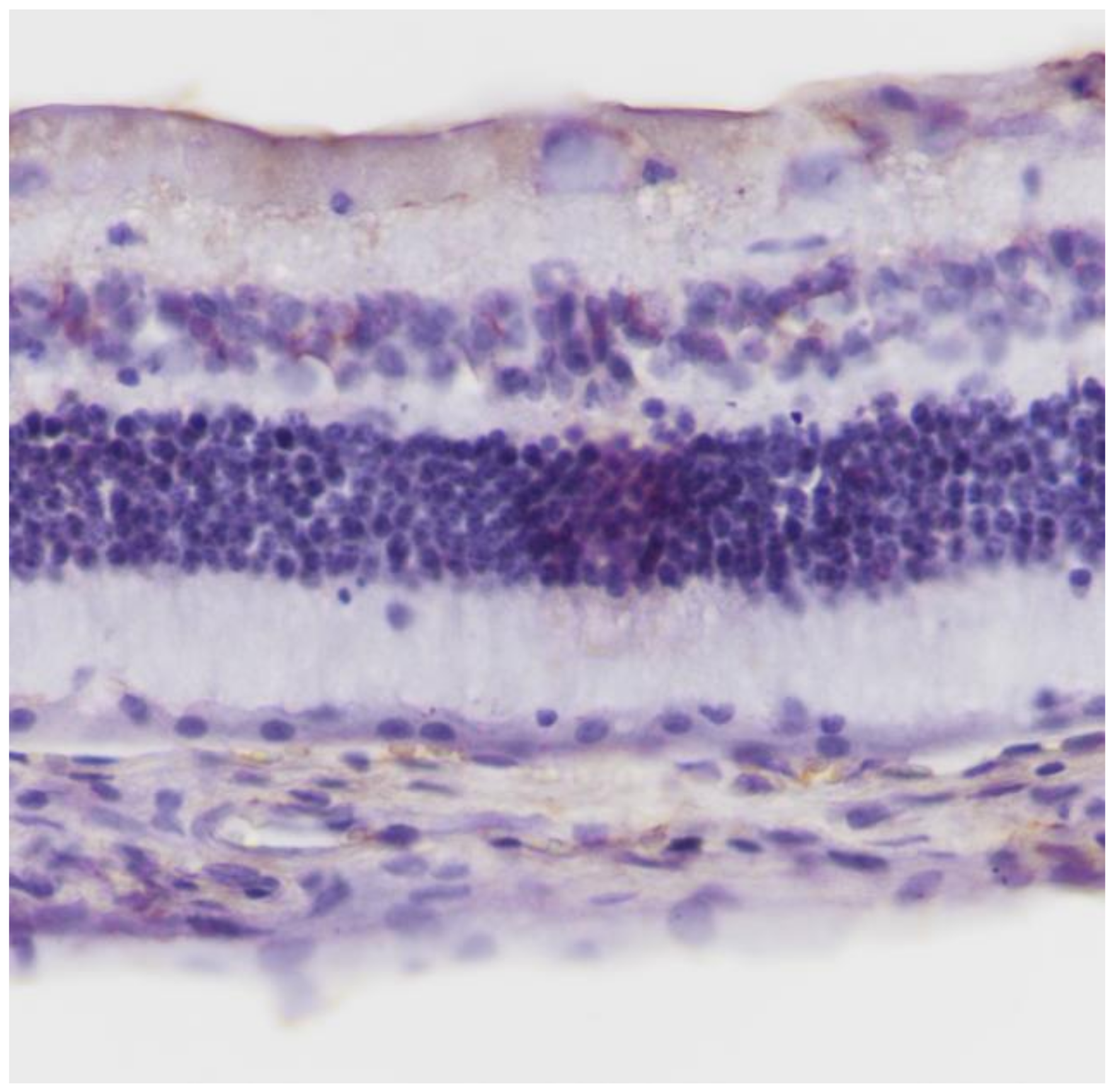
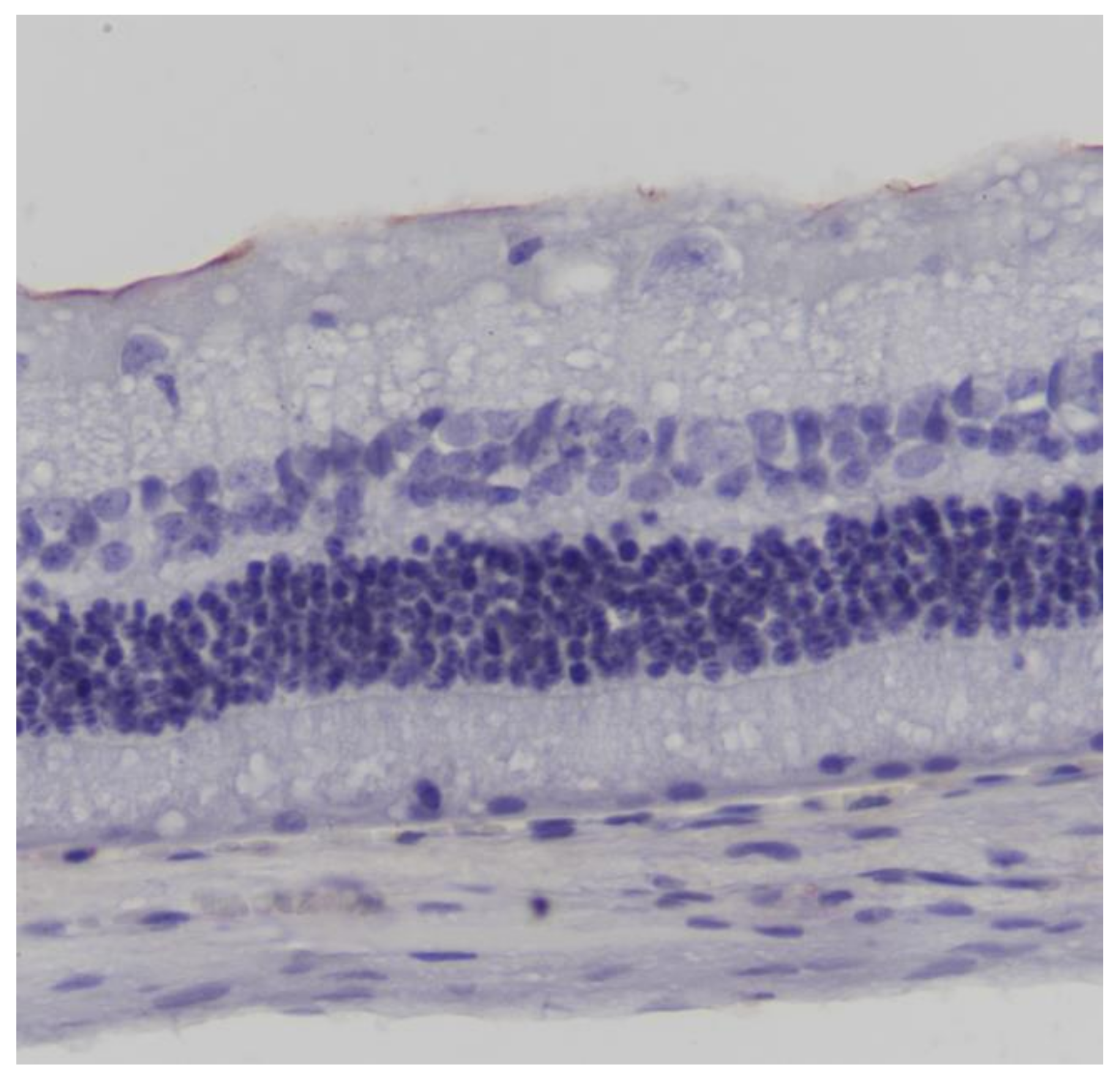
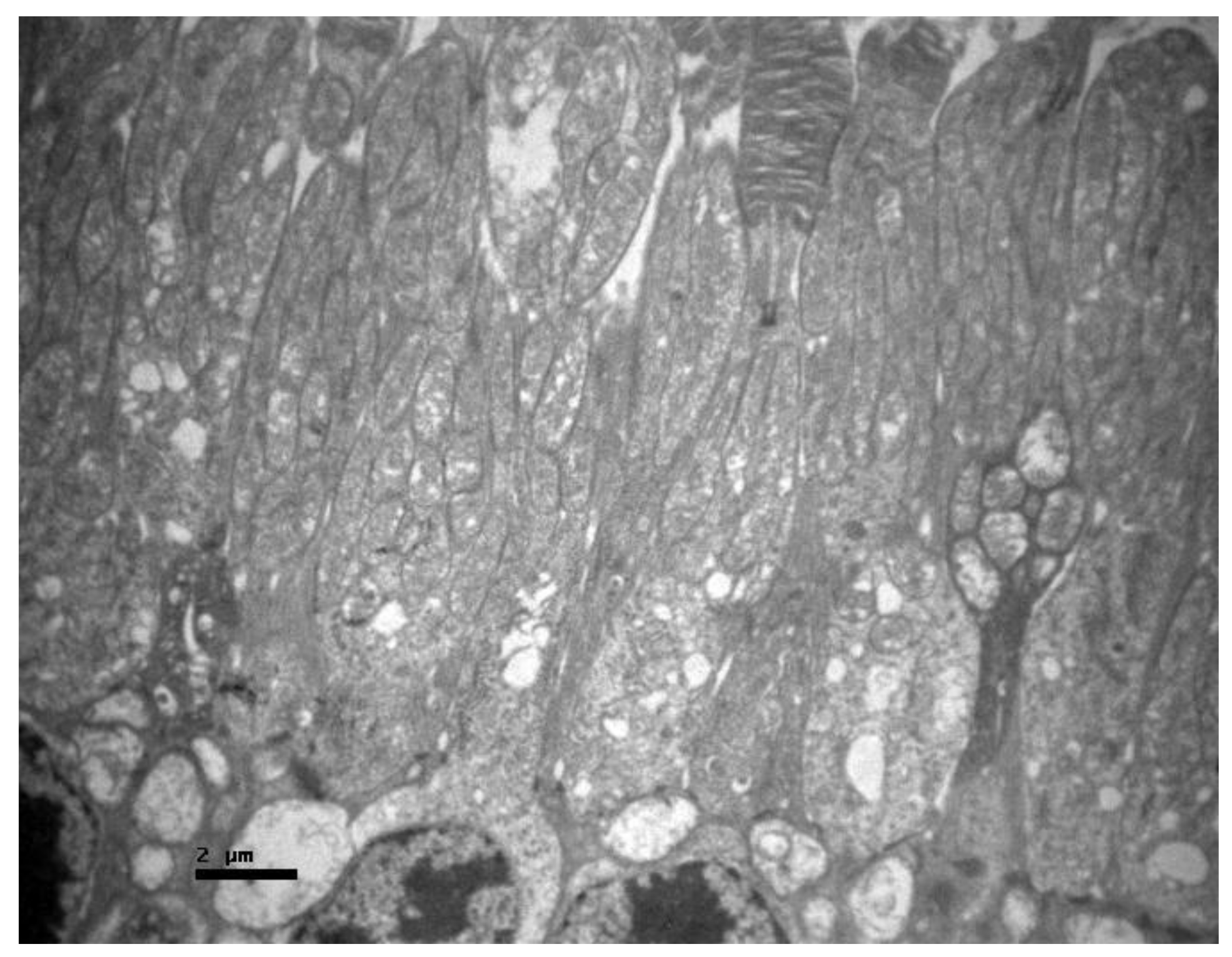
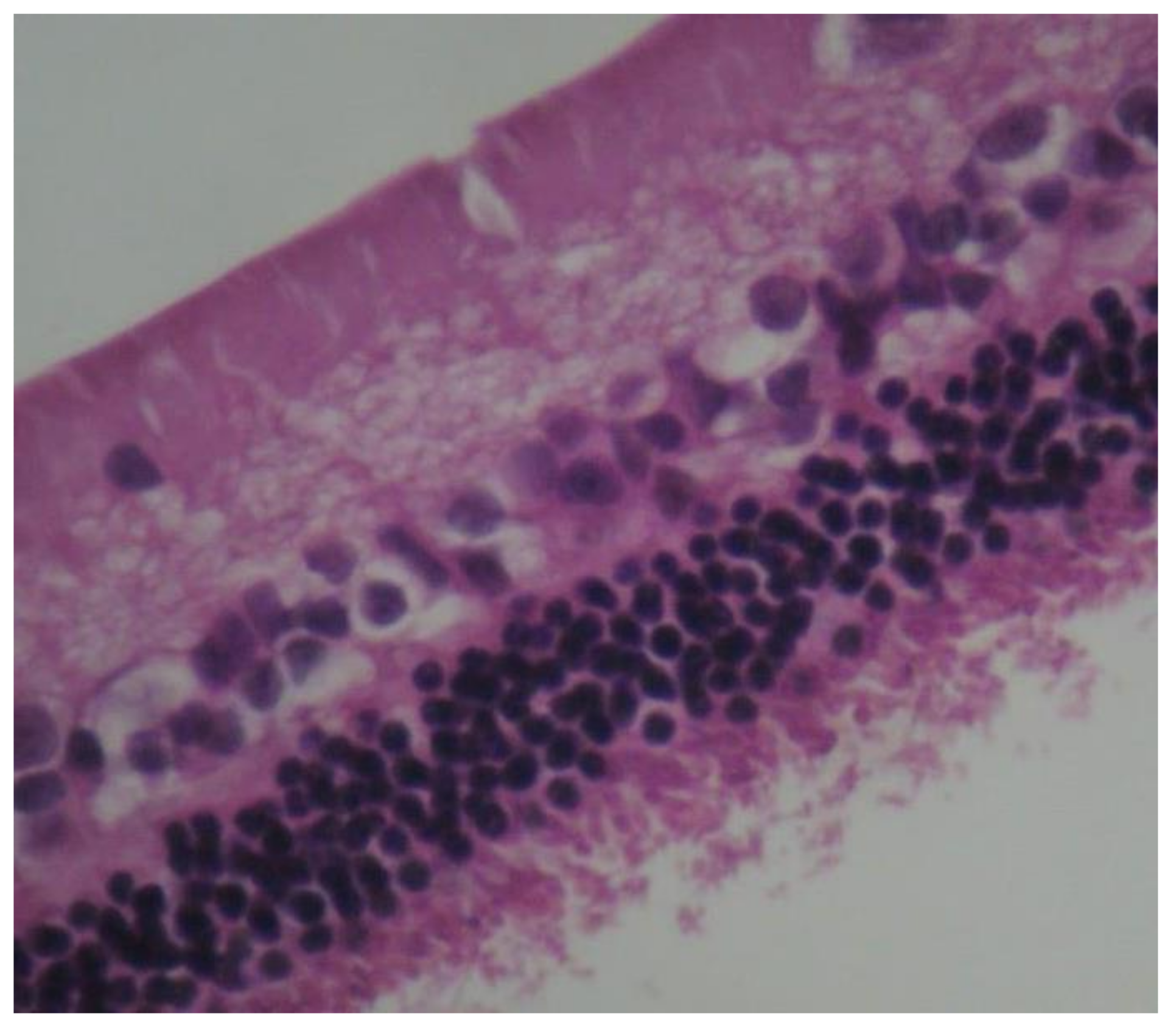
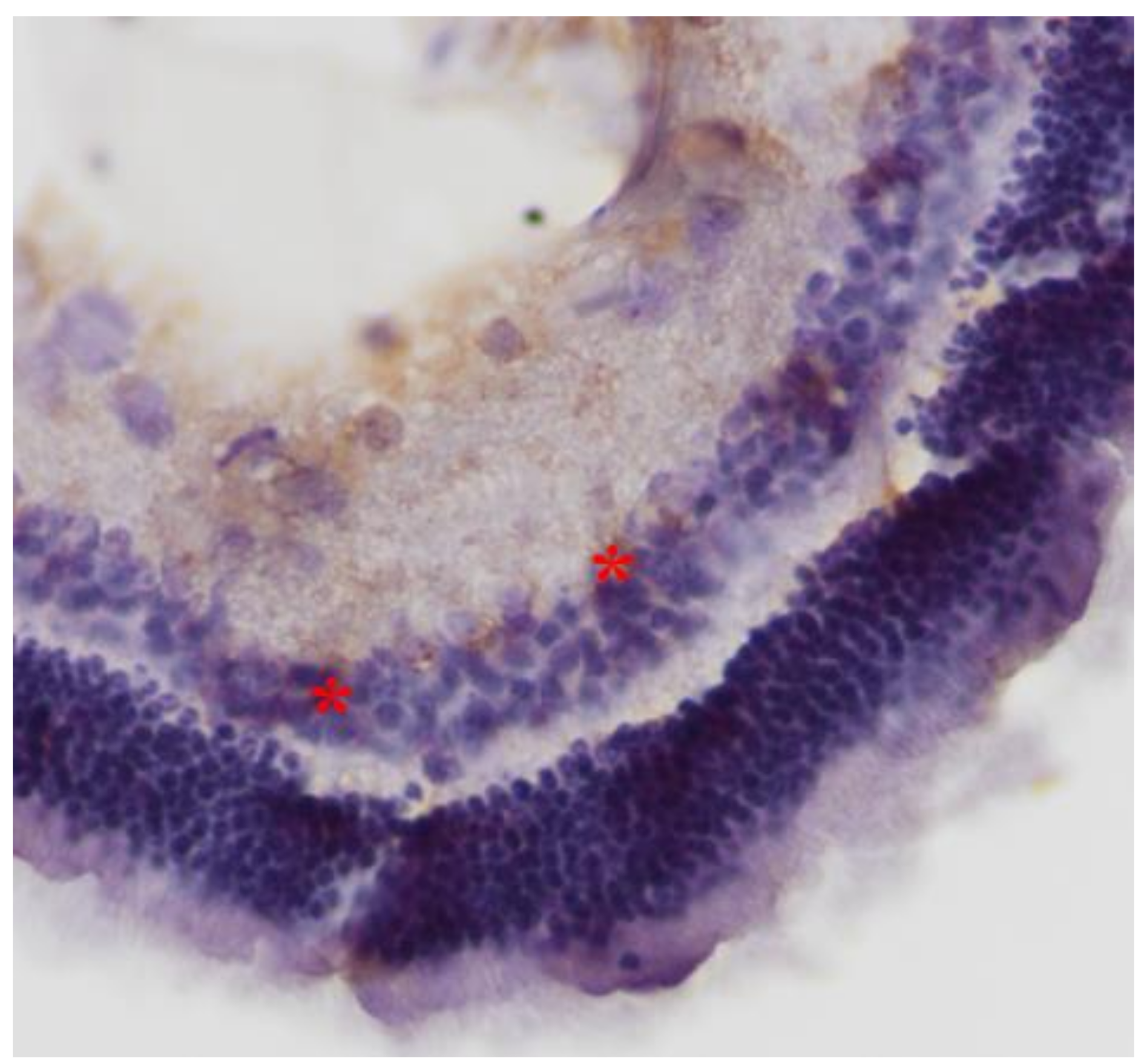
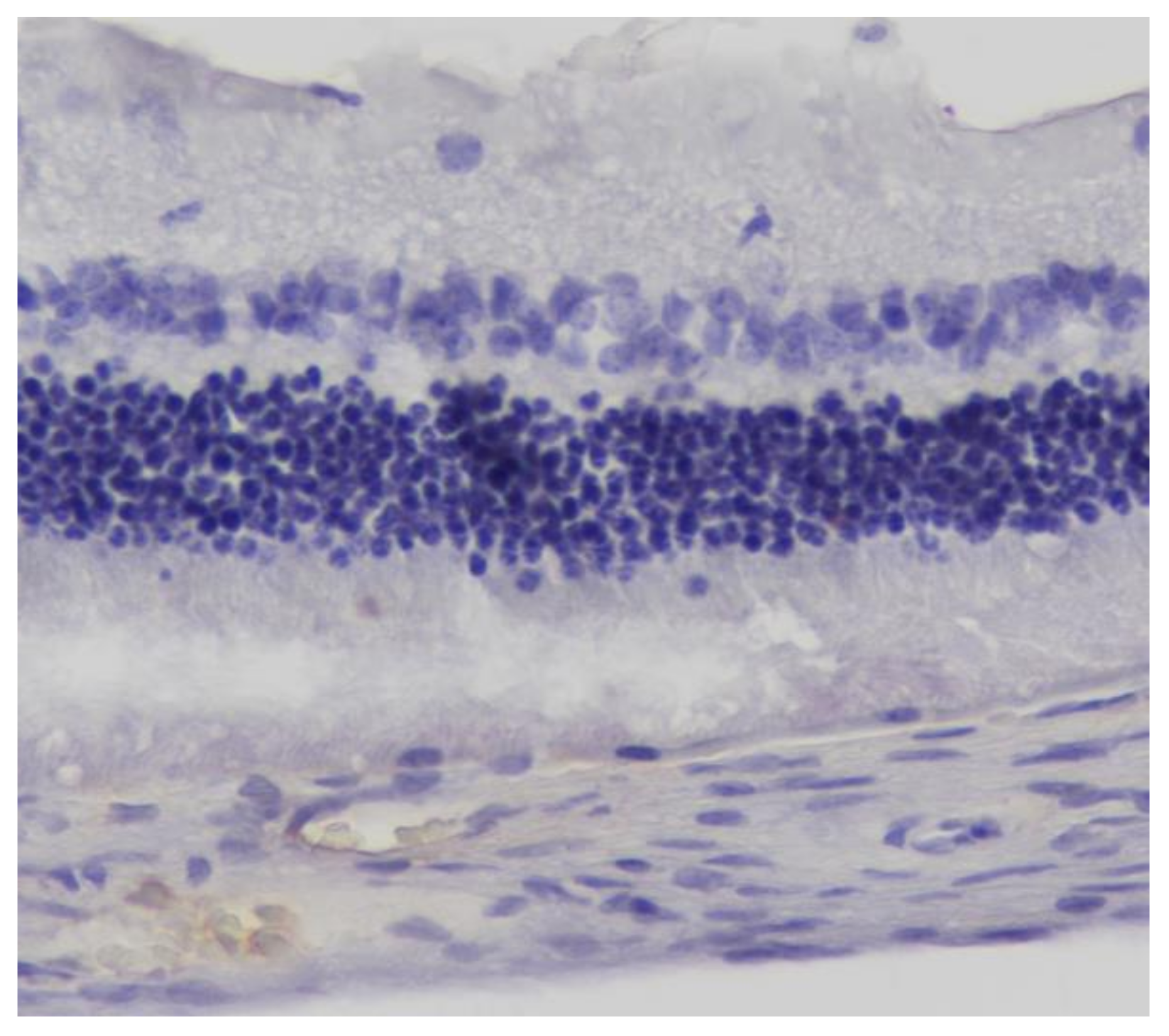
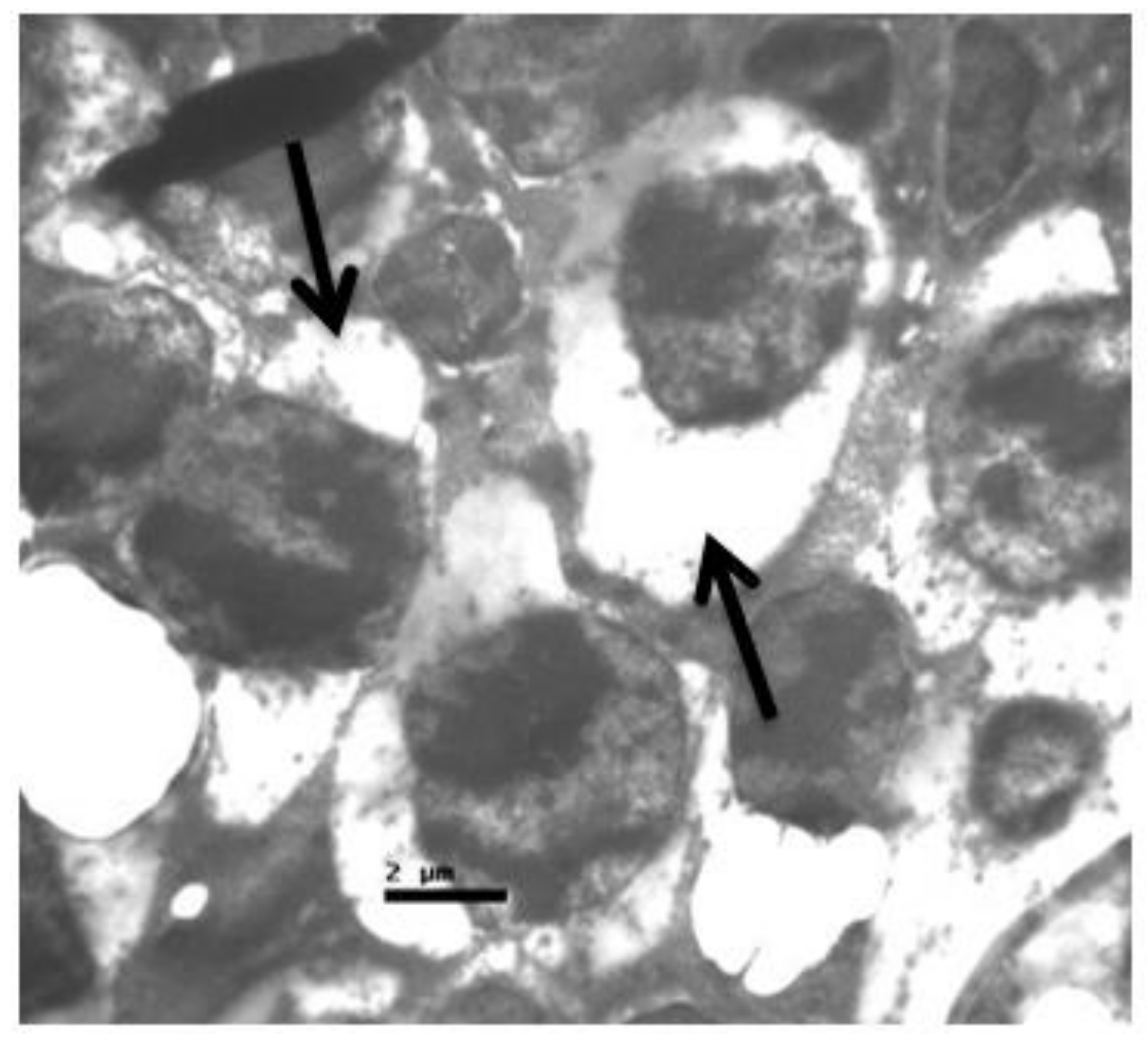
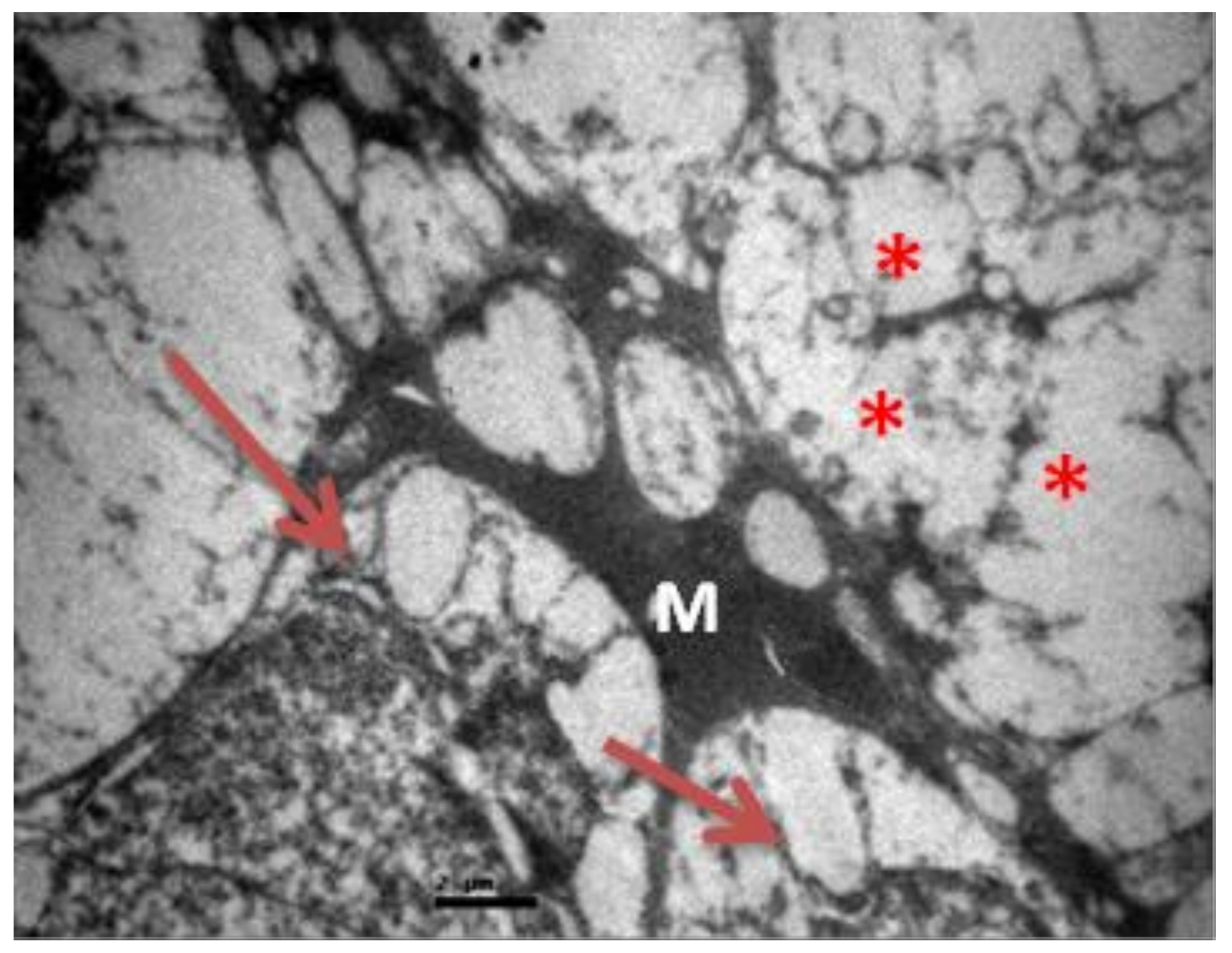
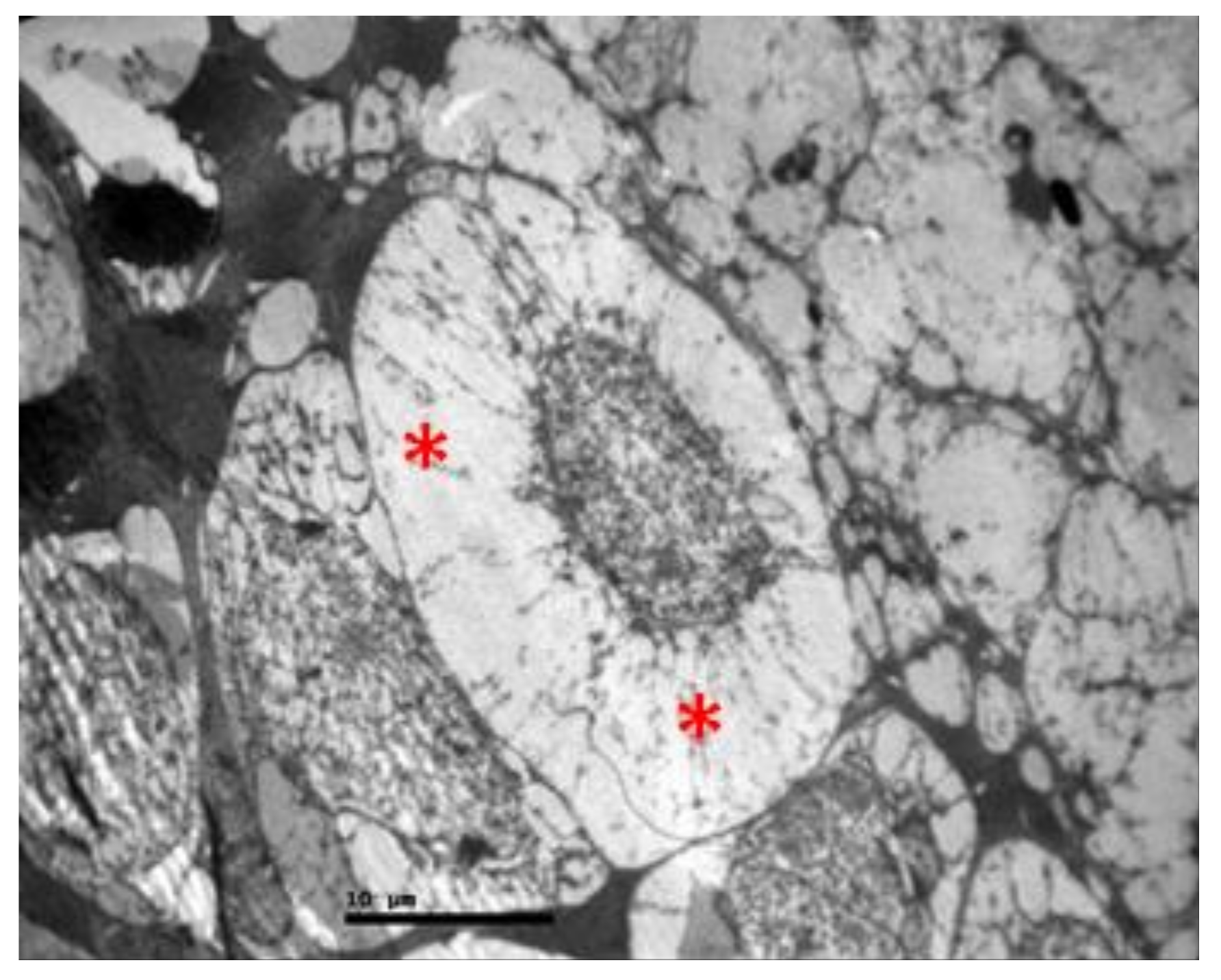
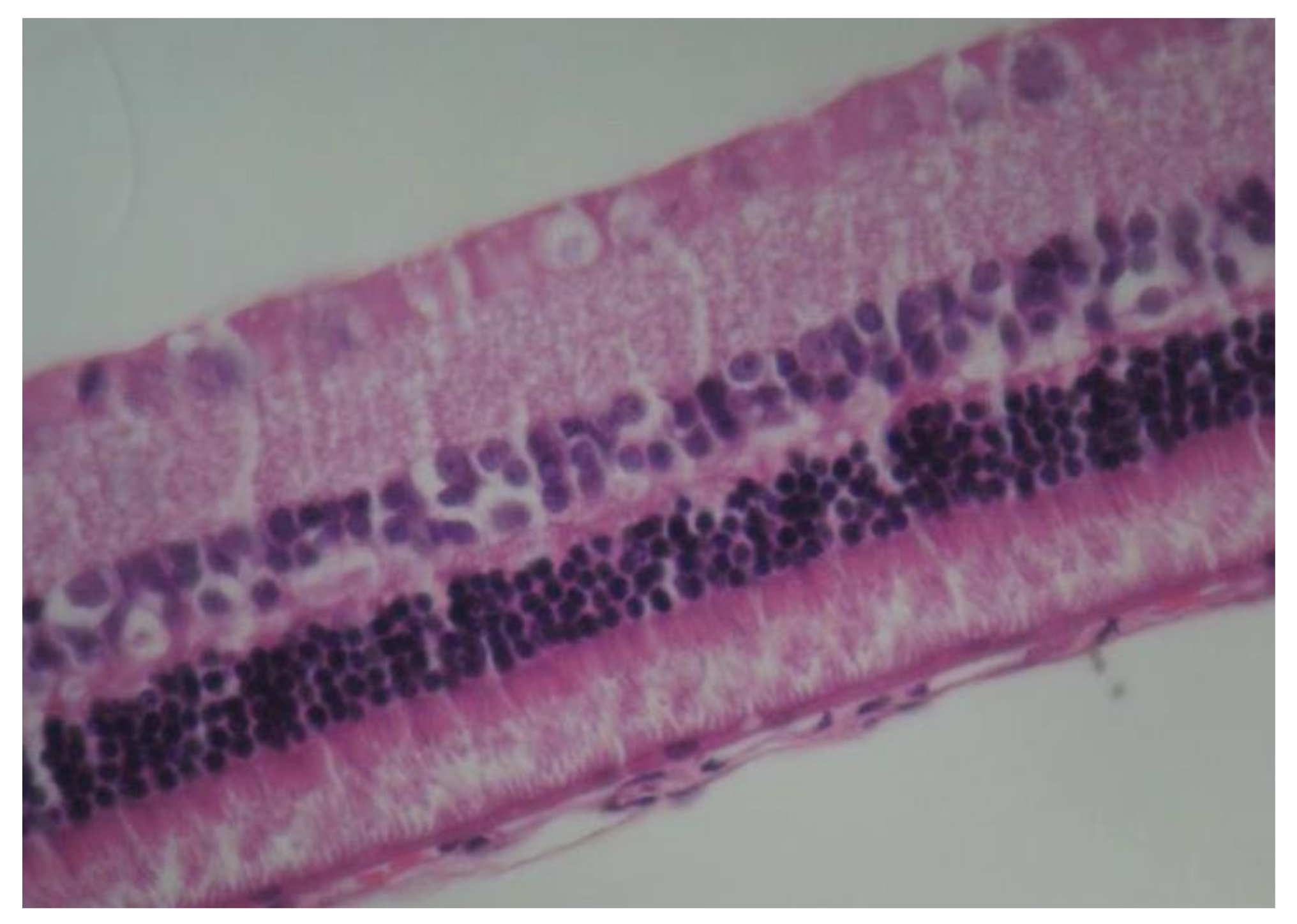
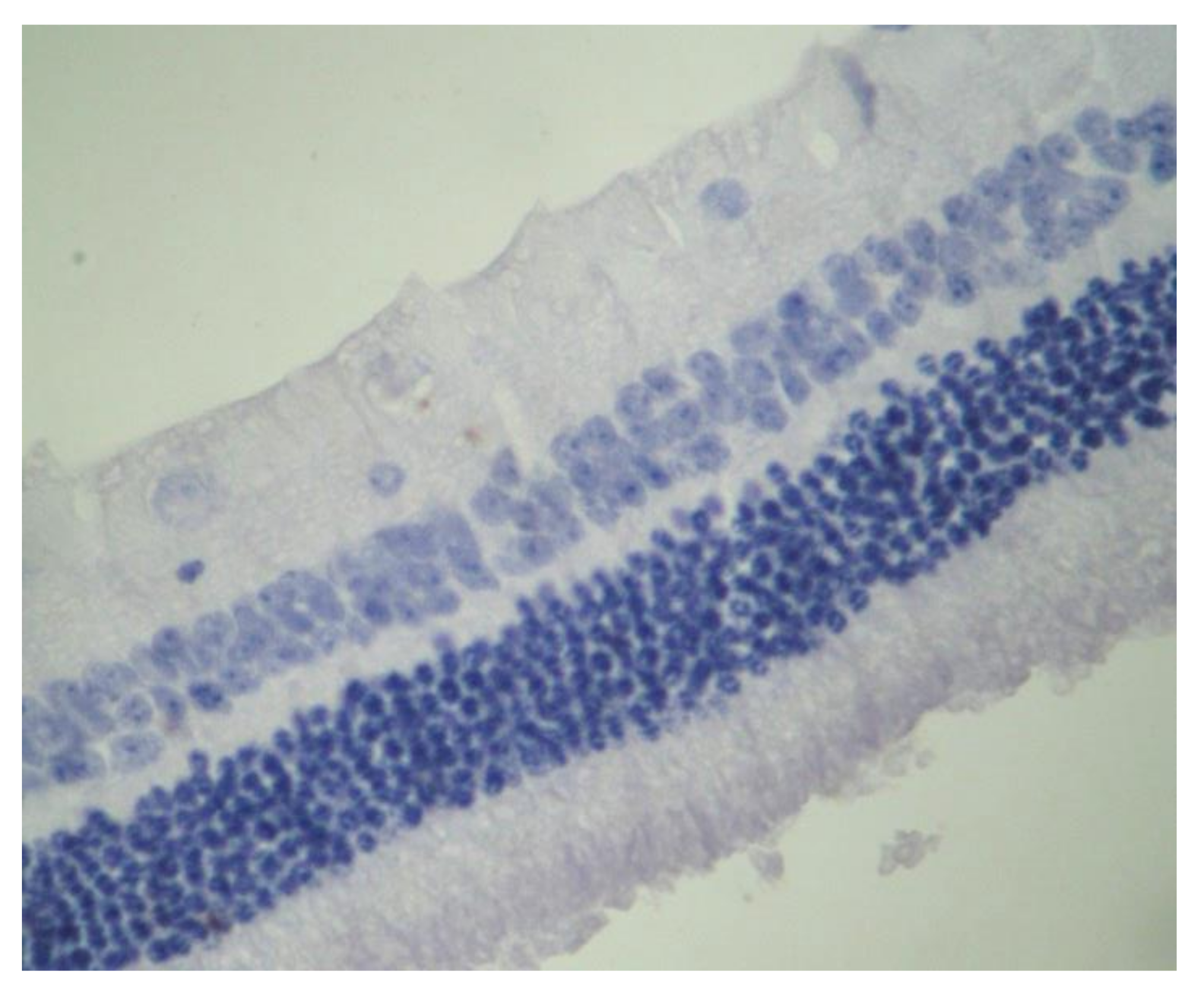
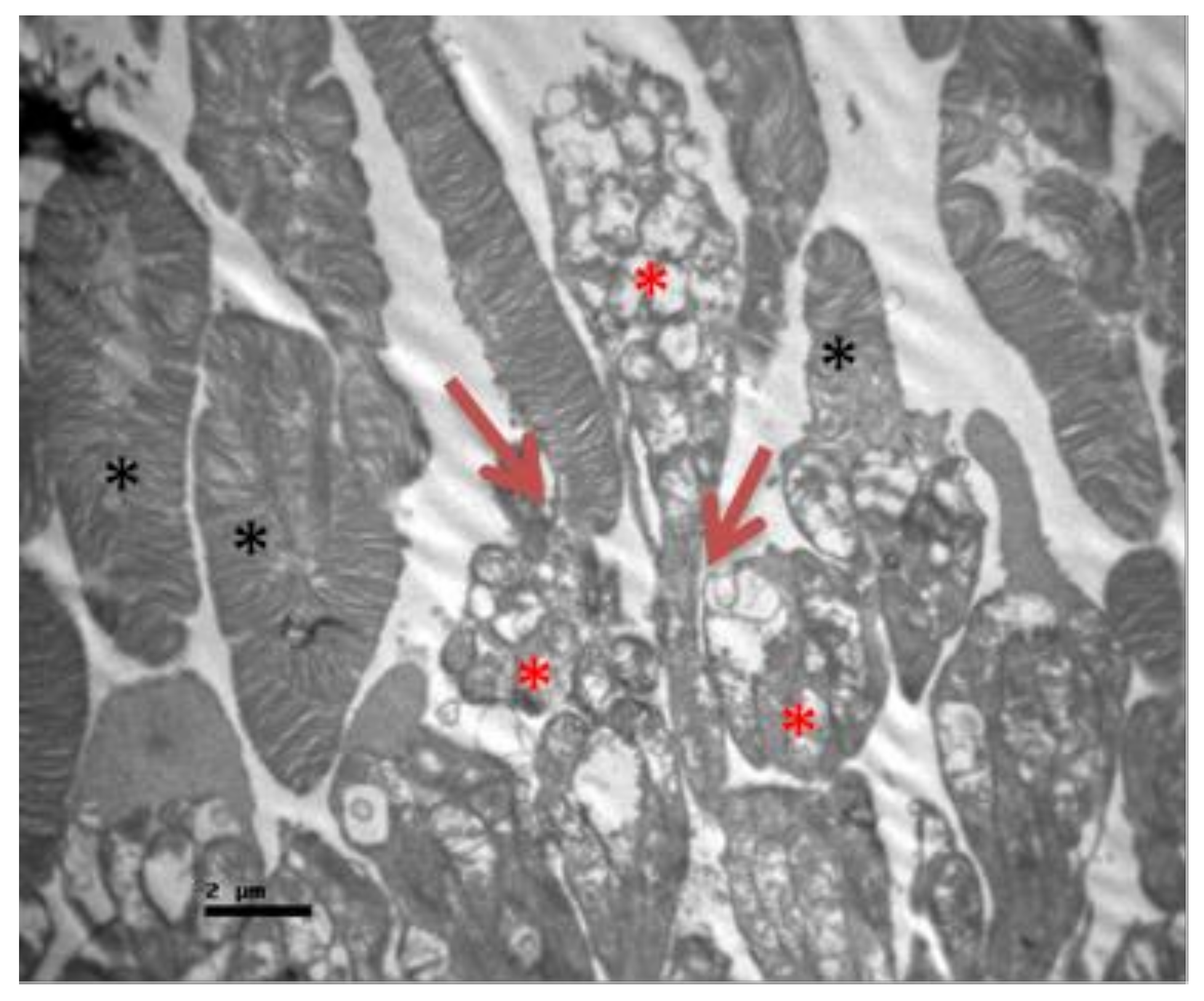
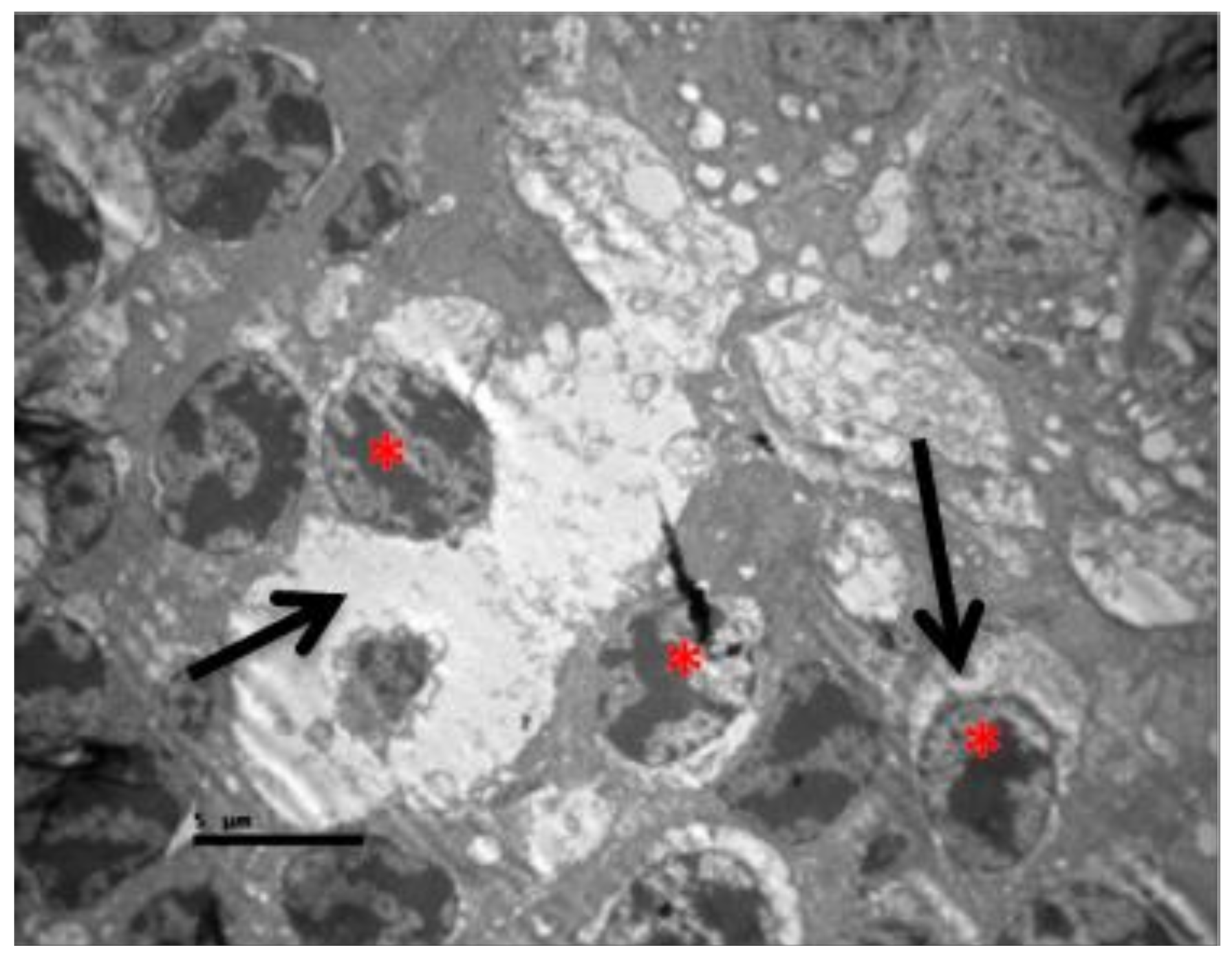
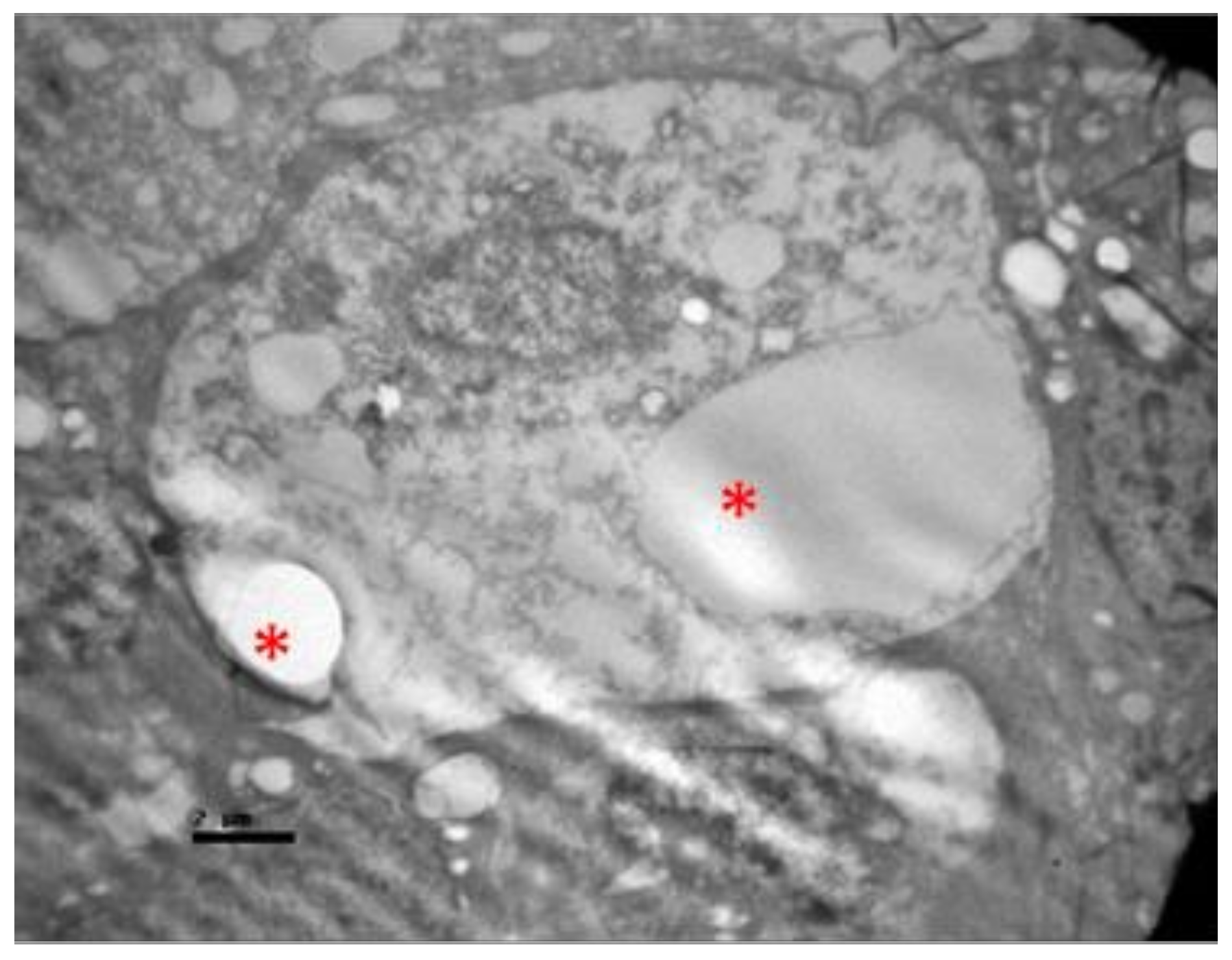
2.1. Group C
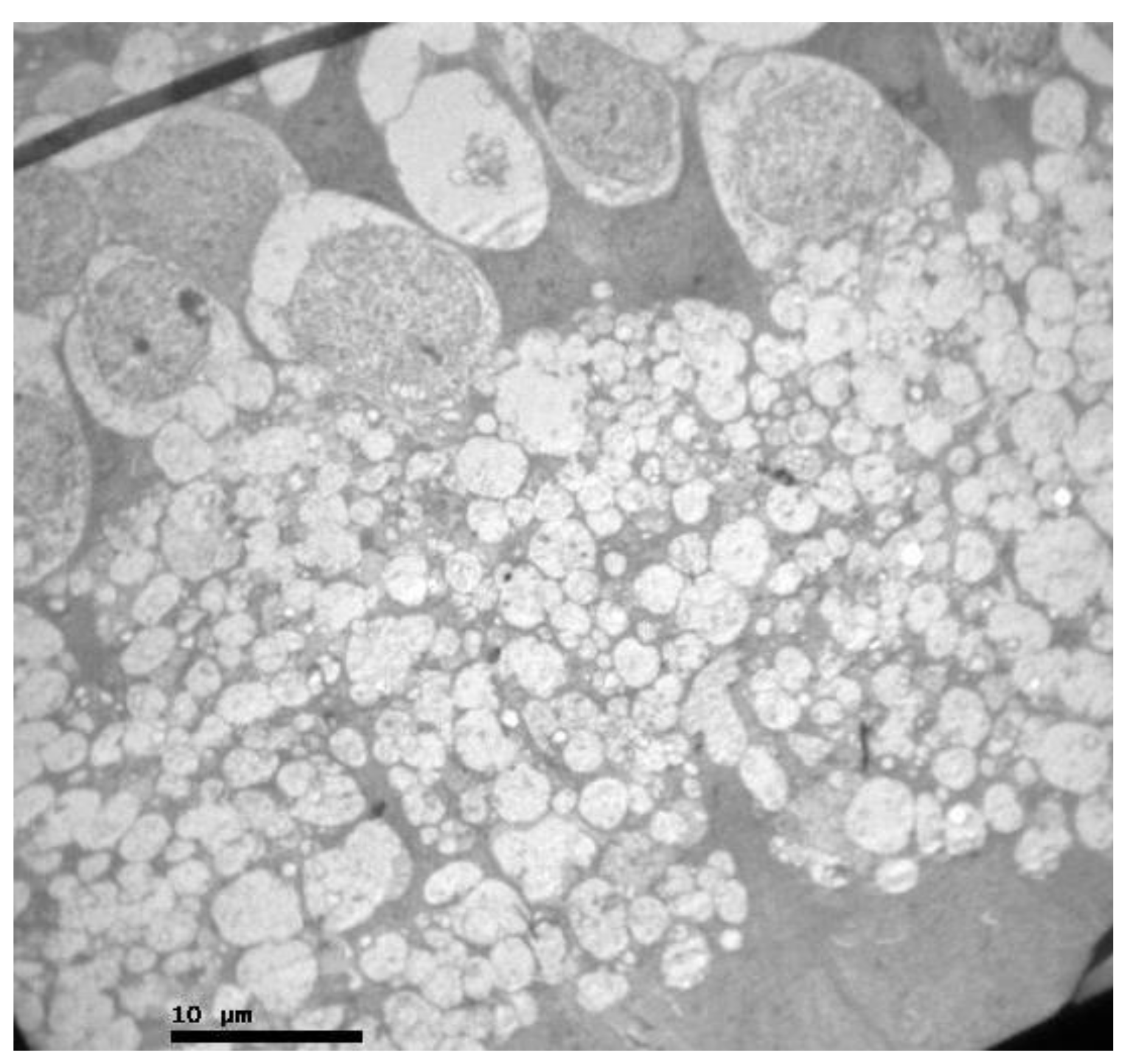
2.2. Group V
2.3. Group M
3. Discussion
4. Materials and Methods
4.1. Materials and Animals
4.2. Methods
4.2.1. Procedures
4.2.2. Preparation for Light Microscopy and Immunohistochemistry
4.2.3. Preparation for Transmission Electron Microscopy
4.2.4. Statistical Analysis
4.3. Ethical Approval
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Müller, G.G.; Kara-José, N.; Castro, R.S.D. Antifungals in eye infections: Drugs and routes of administration. Rev. Bras. De Oftalmol. 2013, 72, 132–141. [Google Scholar] [CrossRef][Green Version]
- Patil, A.; Majumdar, S. Echinocandins in ocular therapeutics. J. Ocul. Pharmacol. Ther. 2017, 33, 340–352. [Google Scholar] [CrossRef] [PubMed]
- Heralgi, M.M.; Badami, A.; Vokuda, H.; Venkatachalam, K. An Update on Voriconazole in Ophthalmology. Off. Sci. J. Delhi Ophthalmol. Soc. 2016, 27, 9–15. [Google Scholar] [CrossRef]
- Shen, Y.C.; Wang, M.Y.; Wang, C.Y.; Tsai, T.C.; Tsai, H.Y.; Lee, Y.F.; Wei, L.C. Clearance of intravitreal voriconazole. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2238–2241. [Google Scholar] [CrossRef]
- Gao, H.; Pennesi, M.E.; Shah, K.; Qiao, X.; Hariprasad, S.M.; Mieler, W.F.; Holz, E.R. Intravitreal voriconazole: An electroretinographic and histopathologic study. Arch. Ophthalmol. 2004, 122, 1687–1692. [Google Scholar] [CrossRef]
- Hua, G.; Pennesi, M.; Shah, K.; Qiao, X.; Hariprasad, S.M.; Mieler, W.F.; Holz, E.R. Safety of intravitreal voriconazole: Electroretinographic and histopathologic studies. Trans. Am. Ophthalmol. Soc. 2003, 101, 183. [Google Scholar]
- Collier, S.; Gronostaj, M.; MacGurn, A.; Cope, J.; Yoder, J.; Beach, M. Estimated Burden of Keratitis—United States. Morb. Mortal. Wkl. Rep. 2010, 63, 1027–1030. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Notes from the field: Multistate outbreak of postprocedural fungal endophthalmitis associated with a single compounding pharmacy—United States, March–April. Morb. Mortal. Wkl. Rep. 2012, 61, 310–311. [Google Scholar]
- Jeng, B.H.; Gritz, D.C.; Kumar, A.B.; Holsclaw, D.S.; Porco, T.C.; Smith, S.D.; Whitcher, J.P.; Margolis, T.P.; Wong, I.G. Epidemiology of ulcerative keratitis in Northern California. Arch. Ophthalmol. (Chicago Ill 1960) 2010, 128, 1022–1028. [Google Scholar] [CrossRef]
- CDC. Fusarium keratitis-multiple states. Morb. Mortal. Wkl. Rep. 2006, 55, 400–401. [Google Scholar]
- Thomas, P.; Kaliamurthy, J. Mycotic keratitis: Epidemiology, diagnosis and management. Clin. Microbiol. Infect. 2013, 19, 210–220. [Google Scholar] [CrossRef] [PubMed]
- Keay, L.; Gower, E.W.; Iovieno, A.; Oechsler, R.A.; Alfonso, E.C.; Matoba, A.; Colby, K.; Tuli, S.S.; Hammersmith, K.; Cavanagh, D.; et al. Clinical and microbiological characteristics of fungal keratitis in the United States, 2001–2007: A multicenter study. Ophthalmology 2011, 118, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Thomas, P. Fungal infections of the cornea. Eye 2003, 17, 852–862. [Google Scholar] [CrossRef]
- Bennett, J. Agentes antimicrobianos, agentes antifúngicos. In Goodman & Gilman: As Bases Farmacológicas da Terapêutica, 11th ed.; Brunton, L., Ed.; McGraw-Hill: Rio de Janeiro, Brazil, 2007; pp. 1103–1117. [Google Scholar]
- Kernt, M.; Neubauer, A.S.; De Kaspar, H.M.; Kampik, A. Intravitreal voriconazole: In vitro safety-profile for fungal endophthalmitis. Retina 2009, 29, 362–370. [Google Scholar] [CrossRef]
- Martinez, R. Atualização no uso de agentes antifúngicos. J. Bras. Pneumol. 2006, 32, 449–460. [Google Scholar] [CrossRef][Green Version]
- Amaral, V.C.S.; Nunes Junior, G.P. Ketoconazole- and fluconazole-induced embryotoxicity and skeletal anomalies in wistar rats: A comparative study. Braz. Arch. Biol. Technol. 2008, 51, 1153–1161. [Google Scholar] [CrossRef]
- Haddad, R.; El-Mollayess, G. Combination of Intracameral and Intrastromal Voriconazole in the Treatment of Recalcitrant Acremonium Fungal Keratitis. Middle East Afr. J. Ophthalmol. 2012, 19, 265–268. [Google Scholar] [CrossRef]
- Kalaiselvi, G.; Narayana, S.; Krishnan, T.; Sengupta, S. Intrastromal voriconazole for deep recalcitrant fungal keratitis: A case series. Br. J. Ophthalmol. 2014, 99, 195–198. [Google Scholar] [CrossRef]
- Lekhanont, K.; Nonpassopon, M.; Nimvorapun, N.; Santanirand, P. Treatment With Intrastromal and Intracameral Voriconazole in 2 Eyes With Lasiodiplodia theobromae Keratitis: Case reports. Medicine (Baltimore) 2015, 94, e541. [Google Scholar] [CrossRef]
- Sharma, N.; Agarwal, P.; Sinha, R.; Titiyal, J.; Velpandian, T.; Vajpayee, R. Evaluation of intrastromal voriconazole injection in recalcitrant deep fungal keratitis: Case series. Br. J. Ophthalmol. 2011, 95, 1735–1737. [Google Scholar] [CrossRef]
- Lee, S.; Lee, J.; Kim, S. Topical and Oral Voriconazole in the Treatment of Fungal Keratitis. Korean J. Ophthalmol. 2009, 23, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.; Kramer, M.; Blau, H.; Bishara, J.; AxerSiegel, R.; Weinberger, D. Intravitreal voriconazole for the treatment of endogenous Aspergillus endophthalmitis. Ophthalmology 2006, 113, 1184–1186. [Google Scholar] [CrossRef]
- Vila Arteaga, J.; Suriano, M.; Stirbu, O. Intravitreal voriconazole for the treatment of Aspergillus chorioretinitis. Int. Ophthalmol. 2011, 31, 341–344. [Google Scholar] [CrossRef]
- Klont, R.; Eggink, C.; Rijs, A.; Wesseling, P.; Verweij, P. Successful Treatment of Fusarium Keratitis with Cornea Transplantation and Topical and Systemic Voriconazole. Clin. Infect. Dis. 2005, 40, e110–e112. [Google Scholar] [CrossRef] [PubMed]
- Varma, D.; Thaker, H.; Moss, P.; Wedgwood, K.; Innes, J. Use of voriconazole in Candida retinitis. Eye 2004, 19, 485–487. [Google Scholar] [CrossRef]
- Al-Badriyeh, D.; Neoh, C.; Stewart, K.; Kong, D. Clinical utility of voriconazole eye drops in ophthalmic fungal keratitis. Clin. Ophthalmol. 2010, 4, 391–405. [Google Scholar]
- Bachmann, S.P.; VandeWalle, K.; Ramage, G.; Patterson, T.F.; Wickes, B.L.; Graybill, J.R.; López-Ribot, J.L. In vitro activity of caspofungin against Candida albicans biofilms. Antimicrob. Agents Chemother. 2002, 46, 3591–3596. [Google Scholar] [CrossRef]
- Lalitha, P.; Shapiro, B.L.; Srinivasan, M.; Prajna, N.V.; Acharya, N.R.; Fothergill, A.W.; Ruiz, J.; Chidambaram, J.D.; Maxey, K.J.; Hong, K.C.; et al. Antimicrobial susceptibility of Fusarium, Aspergillus, and other filamentous fungi isolated from keratitis. Arch. Ophthalmol. 2007, 125, 789–793. [Google Scholar] [CrossRef]
- Wagner, C.; Graninger, W.; Presterl, E.; Joukhadar, C. The echinocandins: Comparison of their pharmacokinetics, pharmacodynamics and clinical applications. Pharmacology 2006, 78, 161–177. [Google Scholar] [CrossRef]
- Katsikas, G.; Tzima, S. The Role of Interleukin-6 in the Systemic and Extra-articular manifestations of Rheumatoid Arthritis. Hell. Rheumatol. 2009, 20, 36–47. [Google Scholar]
- Kishimoto, T. The biology of interleukin-6. Blood 1989, 74, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, H. Roles of IL-6 in Ocular Inflammation: A Review. Ocul. Immunol. Inflamm. 2017, 26, 37–50. [Google Scholar] [CrossRef]
- Pascual-Camps, Ι.; Hernández-Martínez, P.; Monje-Fernández, L.; Dolz-Marco, R.; Gallego-Pinazo, R.; Wu, L.; Arévalo, J.F.; Díaz-Llopis, M. Update on intravitreal anti-tumor necrosis factor alpha therapies for ocular disorders. J. Ophthalmic Inflamm. Infect. 2014, 4, 26. [Google Scholar] [CrossRef] [PubMed]
- Theodossiadis, P.G.; Markomichelakis, N.N.; Sfikakis, P.P. Tumor necrosis factor antagonists: Preliminary evidence for an emerging approach in the treatment of ocular inflammation. Retina 2007, 27, 399–413. [Google Scholar] [CrossRef]
- Idriss, H.T.; Naismith, J.H. TNF alpha and the TNF receptor superfamily: Structure-function relationship(s). Microsc. Res. Tech. 2000, 50, 184–195. [Google Scholar] [CrossRef]
- Horiuchi, T.; Mitoma, H.; Harashima, S.; Tsukamoto, H.; Shimoda, T. Transmembrane TNF-a: Structure, function and interaction with anti-TNF agents. Rheumatology 2010, 49, 1215–1228. [Google Scholar] [CrossRef] [PubMed]
- Wallace, W.; Hahn, B. Pathomechanisms of Cutaneous Lupus Erythematosus. In Dubois’ Lupus Erythematosus and Related Syndromes, 8th ed.; Saunders Elsevier: Philadelphia, PA, USA, 2013; Volume 23, pp. 310–318. [Google Scholar]
- Ayadi, A.E.; Herndon, D.N.; Finnerty, C.C. Biomarkers in Burn Patient Care. In Total Burn Care, 5th ed.; Saunders Elsevier: Philadelphia, PA, USA, 2018; Volume 21, pp. 232–235. [Google Scholar]
- Ravussin, E.; Smith, S.R. Role of the Adipocyte in Metabolism and Endocrine Function. In Endocrinology: Adult and Pediatric, 7th ed.; Saunders Elsevier: Philadelphia, PA, USA, 2016; Volume 36, pp. 627–647. [Google Scholar]
- Yao, M.; Brummer, G.; Acevedo, D.; Cheng, N. Cytokine Regulation of Metastasis and Tumorigenicity. Adv. Cancer Res. 2016, 132, 265–367. [Google Scholar] [PubMed]
- Kinne, R.W.; Stuhlmüller, B.; Burmester, G.R. Macrophages. Rheum. Arthritis 2009, 8C, 107–115. [Google Scholar]
- Hariprasad, S.M.; Mieler, W.F.; Holz, E.R.; Gao, H.; Kim, J.E.; Chi, J.; Prince, R.A. Determination of vitreous, aqueous, and plasma concentration of orally administered voriconazole in humans. Arch. Ophthalmol. 2004, 122, 42–47. [Google Scholar] [CrossRef] [PubMed]
- Alfonso, E.C.; Miller, G.A. Fungal keratitis, D. In Cornea: Fundamentals, Diagnosis and Management, 3rd ed.; Krachmer, J.H., Mannis, M.J., Holland, E.J., Eds.; Mosby Elsevier: New York, NY, USA, 2011. [Google Scholar]
- Hariprasad, S.M.; Mieler, W.F.; Lin, T.K.; E Sponsel, W.; Graybill, J.R. Voriconazole in the treatment of fungal eye infections: A review of current literature. Br. J. Ophthalmol. 2008, 92, 871–878. [Google Scholar] [CrossRef]
- Anderson, K.L.; Mitra, S.; Salouti, R.; Pham, T.-A.; Taylor, H.R. Fungal keratitis caused by Paecilomyces lilacinus associated with a retained intracorneal hair. Cornea 2004, 23, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Bunya, V.Y.; Hammersmith, K.M.; Rapuano, C.J.; Ayres, B.D.; Cohen, E.J. Topical and oral voriconazole in the treatment of fungal keratitis. Am. J. Ophthalmol. 2007, 143, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Nulens, E.; Eggink, C.; Rijs, A.J.M.M.; Wesseling, P.; E Verweij, P. Keratitis caused by Scedosporium apiospermum successfully treated with a cornea transplant and voriconazole. J. Clin. Microbiol. 2003, 41, 2261–2264. [Google Scholar] [CrossRef]
- Polizzi, A.; Siniscalchi, C.; Mastromarino, A.; Saccà, S.C. Effect of voriconazole on a corneal abscess caused by fusarium. Acta Ophthalmol. Scand. 2004, 82, 762–764. [Google Scholar] [CrossRef]
- Clode, A.B.; Davis, J.L.; Salmon, J.; Michau, T.M.; Gilger, B.C. Evaluation of concentration of voriconazole in aqueous humor after topical and oral administration in horses. Am. J. Vet. Res. 2006, 67, 296–301. [Google Scholar] [CrossRef] [PubMed]
- Prakash, G.; Sharma, N.; Goel, M.; Titiyal, J.S.; Vajpayee, R.B. Evaluation of intrastromal injection of voriconazole as a therapeutic adjunctive for the management of deep recalcitrant fungal keratitis. Am. J. Ophthalmol. 2008, 146, 56–59. [Google Scholar] [CrossRef]
- Siatiri, H.; Daneshgar, F.; Siatiri, N.; Khodabande, A. The effects of intrastromal voriconazole injection and topical voriconazole in the treatment of recalcitrant Fusarium keratitis. Cornea 2011, 30, 872–875. [Google Scholar] [CrossRef] [PubMed]
- Prajna, N.V.; Mascarenhas, J.; Krishnan, T.; Reddy, P.R.; Prajna, L.; Srinivasan, M.; Vaitilingam, C.M.; Hong, K.C.; Lee, S.M.; McLeod, S.D.; et al. Comparison of natamycin and voriconazole for the treatment of fungal keratitis. Arch. Ophthalmol. 2010, 128, 672–678. [Google Scholar] [CrossRef]
- Giaconi, J.A.; Marangon, F.B.; Miller, D.; Alfonso, E.C. Voriconazole and fungal keratitis: A report of two treatment failures. J. Ocul. Pharm. 2006, 22, 437–439. [Google Scholar] [CrossRef]
- Diekema, D.J.; Messer, S.A.; Hollis, R.J.; Jones, R.N.; Pfaller, M.A. Activities of caspofungin, itraconazole, posaconazole, ravuconazole, voriconazole, and amphotericin B against 448 recent clinical isolates of filamentous fungi. J. Clin. Microbiol. 2003, 41, 3623–3626. [Google Scholar] [CrossRef]
- Johnson, L.B.; Kauffman, C.A.; Saravolatz, L.D. Voriconazole: A new triazole antifungal agent. Clin. Infect. Dis. 2003, 36, 630–637. [Google Scholar] [CrossRef] [PubMed]
- Espinel-Ingroff, A.; Boyle, K.; Sheehan, D.J. In vitro antifungal activities of voriconazole and reference agents as determined by NCCLS methods: Review of the literature. Mycopathologia 2001, 150, 101–115. [Google Scholar] [CrossRef] [PubMed]
- Marco, F.; Pfaller, M.A.; Messer, S.A.; Jones, R.N. Antifungal activity of a new triazole, voriconazole (UK-109,496), compared with three other antifungal agents tested against clinical isolates of filamentous fungi. Med. Mycol. 1998, 36, 433–436. [Google Scholar] [CrossRef] [PubMed]
- Marangon, F.B.; Miller, D.; Giaconi, J.A.; Alfonso, E.C. In vitro investigation of voriconazole susceptibility for keratitis and endophthalmitis fungal pathogens. Am. J. Ophthalmol. 2004, 137, 820–825. [Google Scholar] [CrossRef]
- Harrison, J.M.; Glickman, R.D.; Ballentine, C.S.; Trigo, Y.; Pena, M.A.; Kurian, P.; Graybill, J.R. Retinal function assessed by ERG before and after induction of ocular aspergillosis and treatment by the anti-fungal, micafungin, in rabbits. Doc. Ophthalmol. 2005, 110, 37–55. [Google Scholar] [CrossRef]
- Trujillo, F.; Paris, G.; Woodward, L.; Graybill, J.; Pena, M.; Najvar, L.; Trigo, Y.; Sponsel, W.E. Comparison of Two Antifungal Agents, Natamycin and Micafungin, for Fungal Keratitis. Investig. Ophthalmol. Vis. Sci. 2004, 45, 113. [Google Scholar]
- Paris, G.; Trujillo, F.; Woodward, L.; Trigo, Y.; Ballentine, C.S.; Najvar, L.K.; Glickman, R.D.; Harrison, J.M.; Graybill, J.; Sponsel, W.E. Micafungin vs Amphotericin B in the Treatment of Experimental Aspergillosis Endophthalmitis. Investig. Ophthalmol. Vis. Sci. 2004, 45, 4014. [Google Scholar]
- Hiraoka, T.; Wakabayashi, T.; Kaji, Y.; Nanbu, P.N.; Okamoto, F.; Kiuchi, T.; Fu, B.; Oshika, T. Toxicological Evaluation of Micafungin Ophthalmic Solution in Rabbit Eyes. J. Ocul. Pharmacol. Ther. 2005, 21, 149–156. [Google Scholar] [CrossRef]
- Suzuki, T.; Uno, T.; Chen, G.; Ohashi, Y. Ocular distribution of intravenously administered micafungin in rabbits. J. Infect. Chemother. 2008, 14, 204–2017. [Google Scholar] [CrossRef]
- Toshikuni, N.; Ujike, K.; Yanagawa, T.; Suga, T.; Shimizu, T.; Kusuda, Y.; Okamoto, M.; Ogawa, T.; Yuasa, S. Candida albicans endophthalmitis after extracorporeal shock wave lithotripsy in a patient with liver cirrhosis. Int. Med. (Tokyo Jpn.) 2006, 45, 1327–1332. [Google Scholar] [CrossRef]
- Walia, H.; Tucci, V.; Greene, J.; Tordilla-Wadia, J.; Kelty, P.; Walia, S. A case of endogenous Trichosporon endophthalmitis treated with micafungin and voriconazole. J. Global Infect. Dis. 2009, 1, 71–74. [Google Scholar]
- Matsumoto, Y.; Murat, D.; Kojima, T.; Shimazaki, J.; Tsubota, K. The comparison of solitary topical micafungin or fluconazole application in the treatment of Candida fungal keratitis. Br. J. Ophthalmol. 2010, 95, 1406–1409. [Google Scholar] [CrossRef]
- Mochizuki, K.; Suemori, S.; Udo, K.; Komori, S.; Ohkusu, K.; Yamada, N.; Ogura, S. Intraocular penetration of micafungin in patient with Candida albicans endophthalmitis. J. Ocul. Pharm. 2011, 27, 531–533. [Google Scholar] [CrossRef]
- Mochizuki, K.; Sawada, A.; Suemori, S.; Kawakami, H.; Niwa, Y.; Kondo, Y.; Ohkusu, K.; Yamada, N.; Ogura, S.; Yaguchi, T.; et al. Intraocular Penetration of Intravenous Micafungin in Inflamed Human Eyes. Antimicrob. Agents Chemother. 2013, 57, 4027–4030. [Google Scholar] [CrossRef] [PubMed]
- Mochizuki, K.; Murase, H.; Yasuda, Y.; Suematsu, H.; Yamagishi, Y.; Mikamo, H. Discrepancy of in-vitro data and clinical efficacy of micafungin against Candida tropicalis endophthalmitis. J. Infect. Chemother. 2012, 18, 786–789. [Google Scholar] [CrossRef] [PubMed]
- Chamilos, G.; Lewis, R.; Albert, N.; Kontoyiannis, D. Paradoxical Effect of Echinocandins across Candida Species In Vitro: Evidence for Echinocandin-Specific and Candida Species-Related Differences. Antimicrob. Agents Chemother. 2007, 51, 2257–2259. [Google Scholar] [CrossRef]
- Monden, Y.; Yamamoto, S.; Yamakawa, R.; Sunada, A.; Asari, S.; Makimura, K.; Inoue, Y. First case of fungal keratitis caused by Pestalotiopsis clavispora. Clin. Ophthalmol. 2013, 7, 2261–2264. [Google Scholar] [CrossRef]
- Mitani, A.; Shiraishi, A.; Miyamoto, H.; Sunada, A.; Ueda, A.; Asari, S.; Zheng, X.; Yamamoto, Y.; Hara, Y.; Ohashi, Y. Fungal keratitis caused by Beauveria bassiana: Drug and temperature sensitivity profiles: A case report. BMC Res. Notes 2014, 7, 677. [Google Scholar] [CrossRef] [PubMed]
- Kokuzawa, S.; Suemori, S.; Mochizuki, K.; Hirose, Y.; Yaguchi, T. Aspergillus tubingenesis endophthalmitis after cataract surgery with implantation of preloaded intraocular lens. Semin. Ophthalmol. 2013, 29, 218–221. [Google Scholar] [CrossRef]
- Kamoshita, M.; Matsumoto, Y.; Nishimura, K.; Katono, Y.; Murata, M.; Ozawa, Y.; Shimmura, S.; Tsubota, K. Wickerhamomyces anomalus fungal keratitis responds to topical treatment with antifungal micafungin. J. Infect. Chemother. 2014, 21, 141–143. [Google Scholar] [CrossRef]
- Kapur, R.; Kim, B.; Tu, E.Y.; Birnbaum, A.; Fiscella, R.; Navare, S.; Lim, J.I. The Safe and Non-Toxic Dose of Intravitreal Micafungin and Caspofungin in a Rabbit Model. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3324. [Google Scholar]
- Missel, P.J. Simulating Intravitreal Injections in Anatomically Accurate Models for Rabbit, Monkey, and Human Eyes. Pharm. Res. 2012, 29, 3251–3272. [Google Scholar] [CrossRef] [PubMed]
- Del Amo, E.M.; Urtti, A. Rabbit as an animal model for intravitreal pharmacokinetics: Clinical predictability and quality of the published data. Exp. Eye Res. 2015, 137, 111e124. [Google Scholar] [CrossRef] [PubMed]
- Kyriakopoulos, G.; Tsaroucha, A.K.; Valsami, G.; Lambropoulou, M.; Kostomitsopoulos, N.; Christodoulou, E.; Kakazanis, Z.; Anagnostopoulos, C.; Tsalikidis, C.; Simopoulos, C.E. Silibinin Improves TNF-α and M30 Expression and Histological Parameters in Rat Kidneys After Hepatic Ischemia/Reperfusion. J. Investig. Surg. 2018, 31, 201–209. [Google Scholar] [CrossRef] [PubMed]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karachrysafi, S.; Sioga, A.; Komnenou, A.; Karamitsos, A.; Xioteli, M.; Dori, I.; Delis, G.; Kofidou, E.; Anastasiadou, P.; Sotiriou, S.; et al. Histological Effects of Intravitreal Injection of Antifungal Agents in New Zealand White Rabbits: An Electron Microscopic and Immunohistochemical Study. Pharmaceuticals 2020, 13, 267. https://doi.org/10.3390/ph13100267
Karachrysafi S, Sioga A, Komnenou A, Karamitsos A, Xioteli M, Dori I, Delis G, Kofidou E, Anastasiadou P, Sotiriou S, et al. Histological Effects of Intravitreal Injection of Antifungal Agents in New Zealand White Rabbits: An Electron Microscopic and Immunohistochemical Study. Pharmaceuticals. 2020; 13(10):267. https://doi.org/10.3390/ph13100267
Chicago/Turabian StyleKarachrysafi, Sofia, Antonia Sioga, Anastasia Komnenou, Athanasios Karamitsos, Maria Xioteli, Ioanna Dori, Georgios Delis, Evangelia Kofidou, Penelope Anastasiadou, Sotiris Sotiriou, and et al. 2020. "Histological Effects of Intravitreal Injection of Antifungal Agents in New Zealand White Rabbits: An Electron Microscopic and Immunohistochemical Study" Pharmaceuticals 13, no. 10: 267. https://doi.org/10.3390/ph13100267
APA StyleKarachrysafi, S., Sioga, A., Komnenou, A., Karamitsos, A., Xioteli, M., Dori, I., Delis, G., Kofidou, E., Anastasiadou, P., Sotiriou, S., Karampatakis, V., & Papamitsou, T. (2020). Histological Effects of Intravitreal Injection of Antifungal Agents in New Zealand White Rabbits: An Electron Microscopic and Immunohistochemical Study. Pharmaceuticals, 13(10), 267. https://doi.org/10.3390/ph13100267







