Cholecystokinin-2 Receptor Targeting with Novel C-terminally Stabilized HYNIC-Minigastrin Analogs Radiolabeled with Technetium-99m
Abstract
1. Introduction
2. Results and Discussion
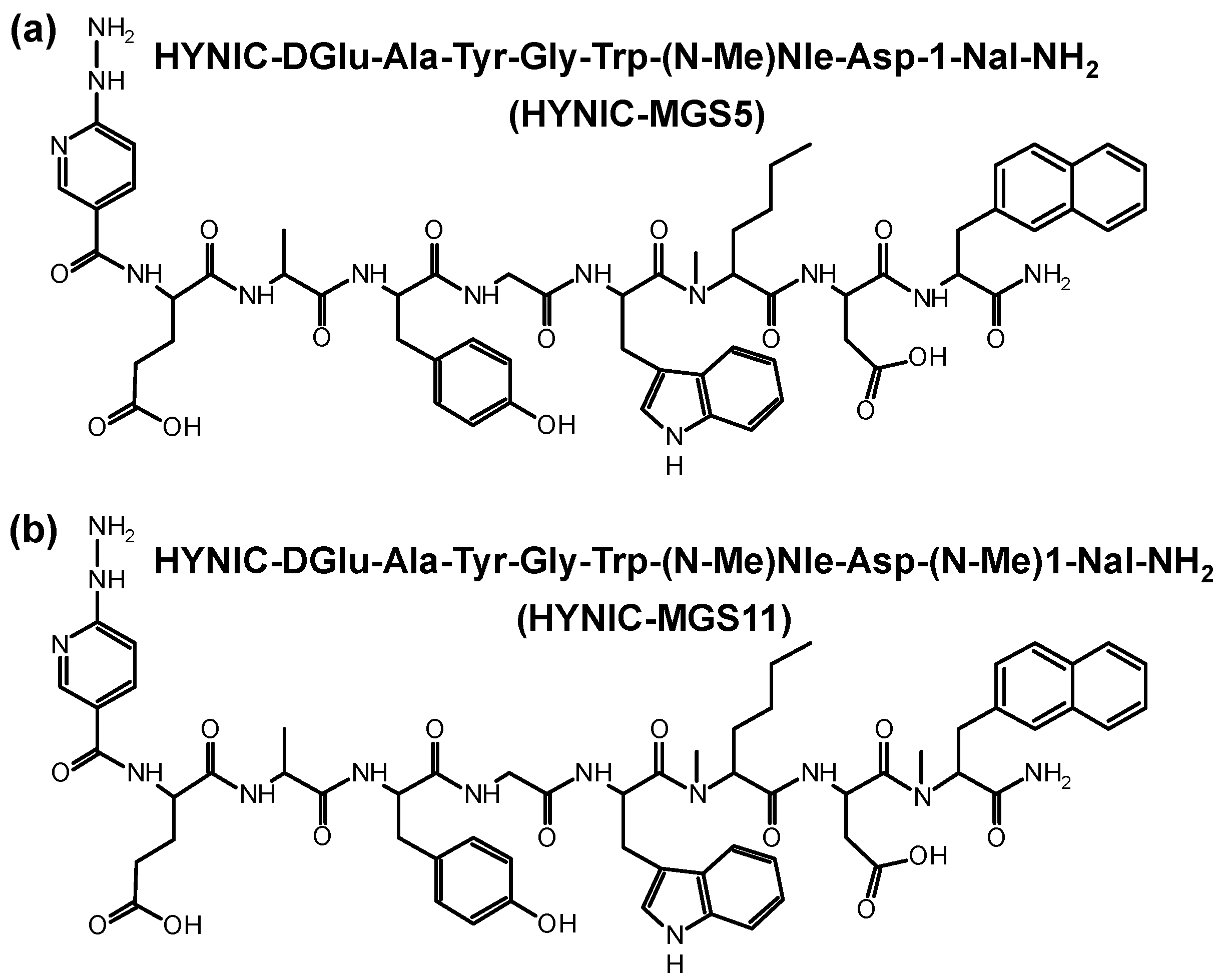
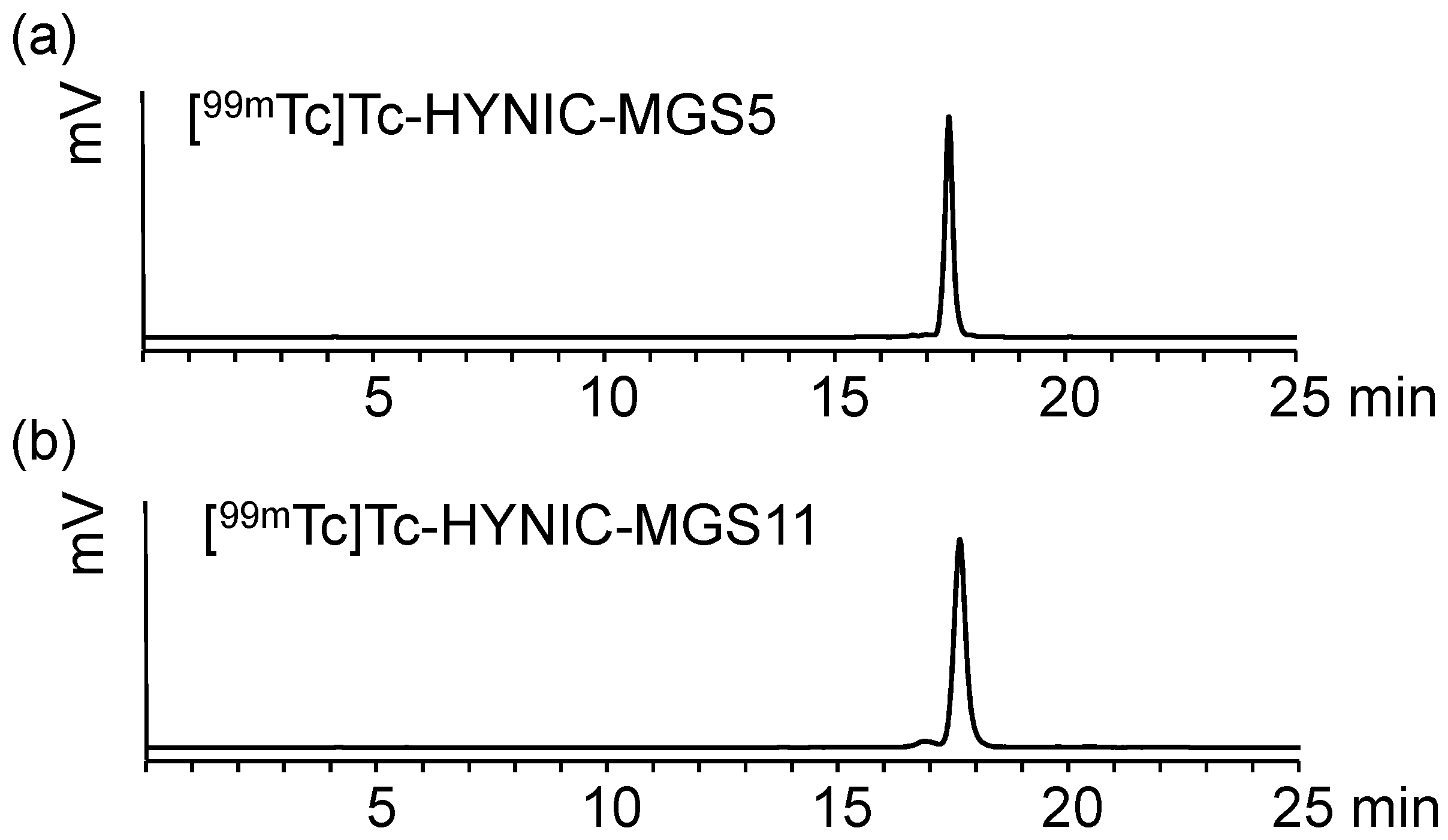
2.1. Peptide Synthesis and Radiolabeling
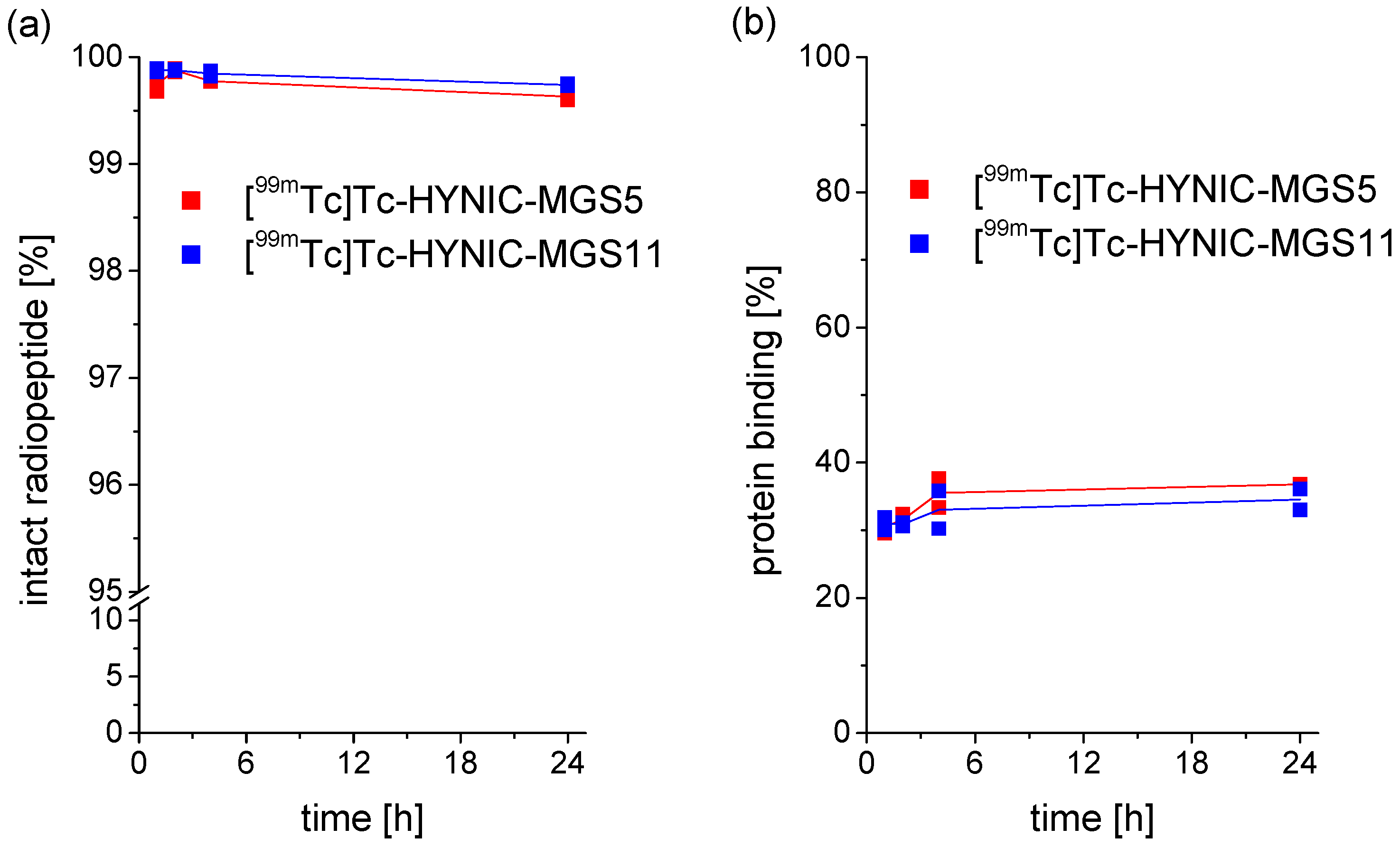
2.2. Characterization in Vitro
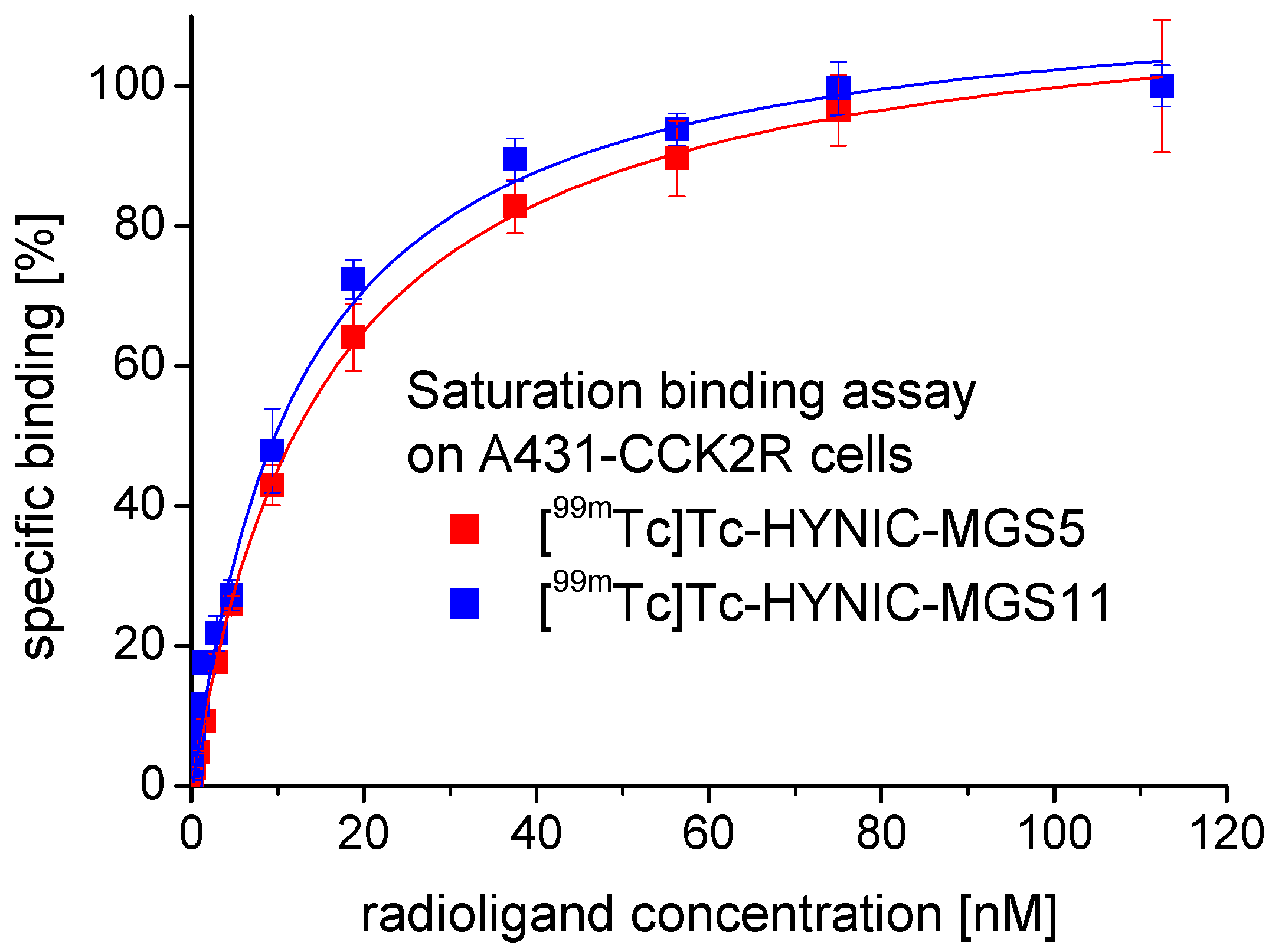
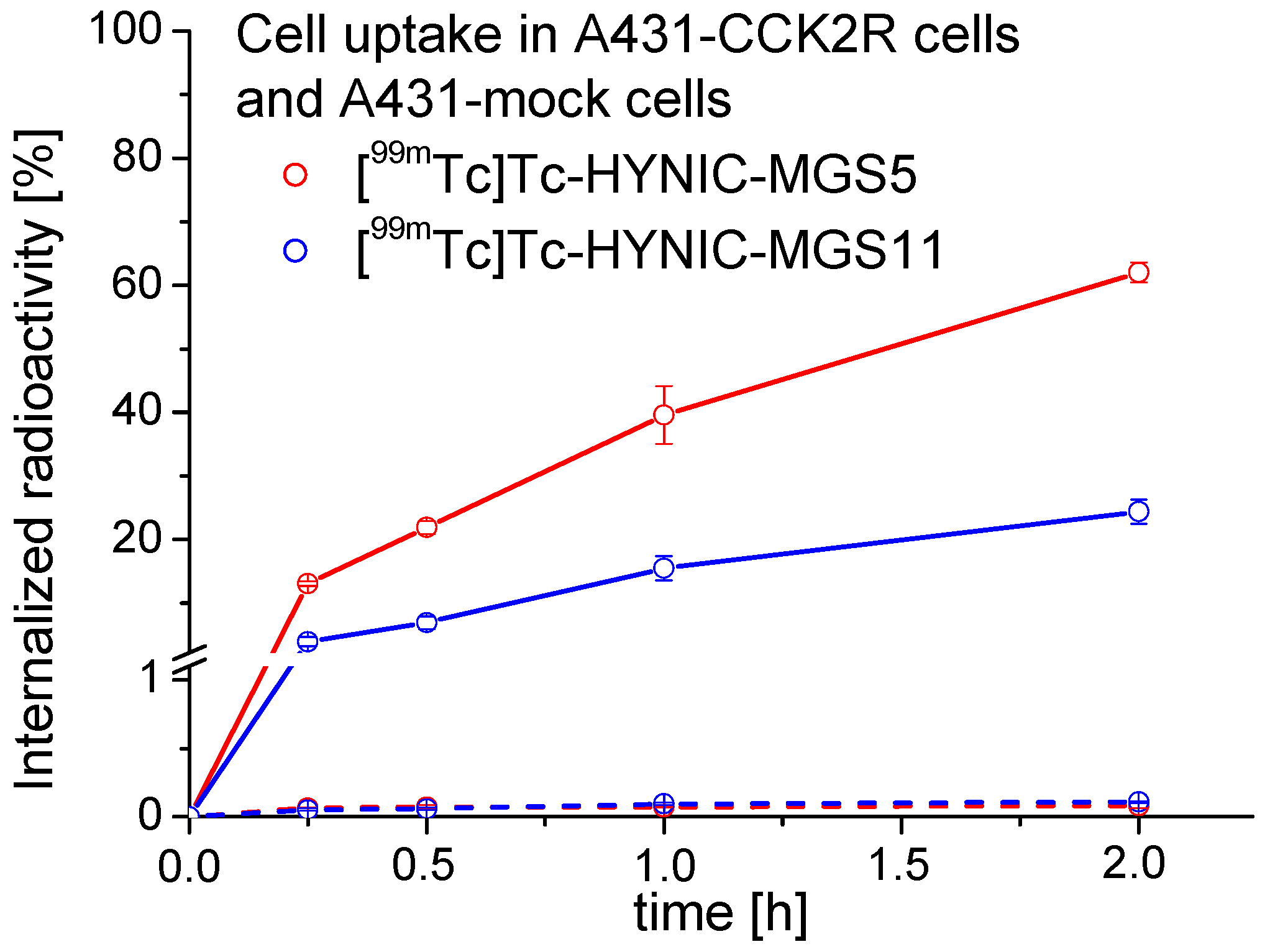
2.3. Receptor Binding and Cell Internalization Studies
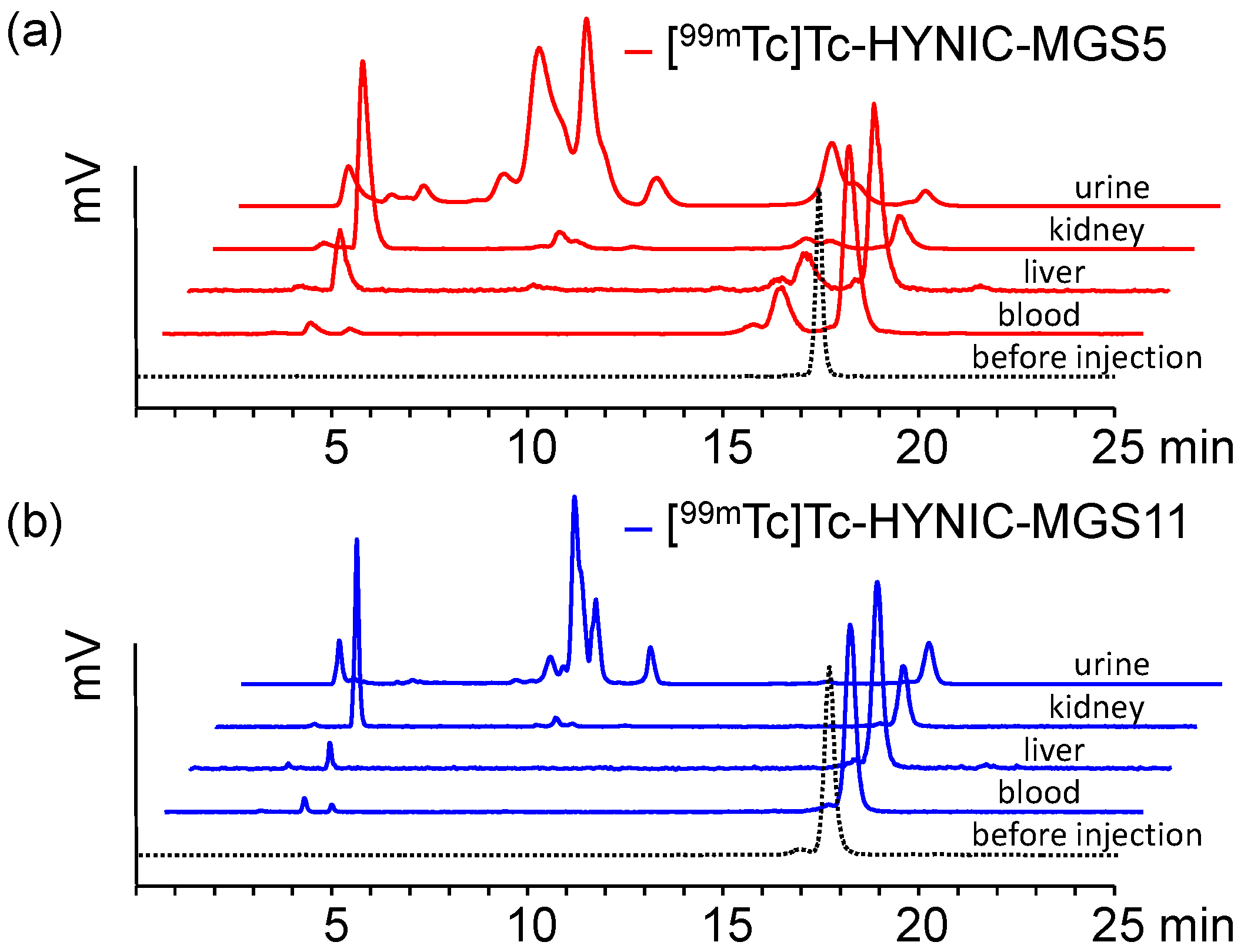
2.4. In Vivo Stability in BALB/c Mice
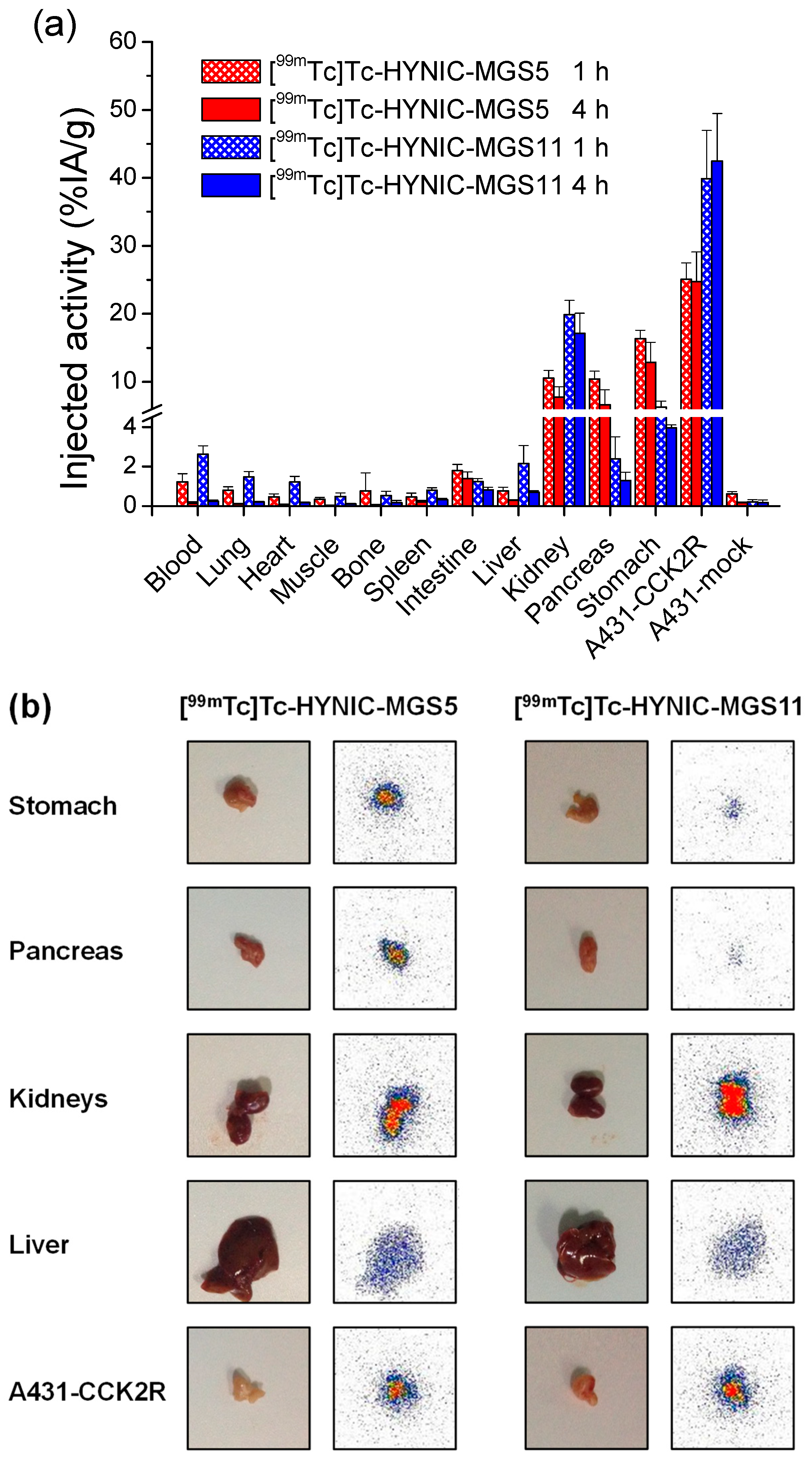
2.5. Biodistribution in Tumor-xenografted BALB/c Nude Mice
3. Materials and Methods
3.1. Materials
3.2. Peptide Synthesis
3.3. Analytical Systems and Methods
3.4. 99mTc-Radiolabeling Using the Tricine/EDDA Exchange Method
3.5. Evaluation of the in Vitro Properties
3.6. Receptor Binding and Cell Internalization Studies
3.7. Evaluation of the in Vivo Stability and Biodistribution
3.7.1. Metabolic Stability in BALB/c Mice
3.7.2. Biodistribution in Tumor-xenografted BALB/c Nude Mice
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Laverman, P.; Sosabowski, J.K.; Boerman, O.C.; Oyen, W.J.G. Radiolabelled peptides for oncological diagnosis. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 78–92. [Google Scholar] [CrossRef] [PubMed]
- Fani, M.; Maecke, H.R. Radiopharmaceutical development of radiolabelled peptides. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, S11–S30. [Google Scholar] [CrossRef] [PubMed]
- Fani, M.; Maecke, H.R.; Okarvi, S.M. Radiolabeled peptides: Valuable tools for the detection and treatment of cancer. Theranostics 2012, 2, 481–501. [Google Scholar] [CrossRef] [PubMed]
- Koopmans, K.P.; Glaudemans, A.W.J.M. Rationale for the use of radiolabelled peptides in diagnosis and therapy. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Reubi, J.C.; Schaer, J.C.; Waser, B. Cholecystokinin(CCK)-A and CCK-B/gastrin receptors in human tumors. Cancer Res. 1997, 57, 1377–1386. [Google Scholar] [PubMed]
- Reubi, J.C. Targeting CCK receptors in human cancers. Curr. Top. Med. Chem. 2007, 7, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Kaloudi, A.; Nock, B.A.; Krenning, E.P.; Maina, T.; De Jong, M. Radiolabeled gastrin/CCK analogs in tumor diagnosis: Towards higher stability and improved tumor targeting. Q. J. Nucl. Med. Mol. Imaging 2015, 59, 287–302. [Google Scholar] [PubMed]
- Roosenburg, S.; Laverman, P.; van Delft, F.L.; Boerman, O.C. Radiolabeled CCK/gastrin peptides for imaging and therapy of CCK2 receptor-expressing tumors. Amino Acids 2011, 41, 1049–1058. [Google Scholar] [CrossRef]
- Fani, M.; Peitl, P.; Velikyan, I. Current status of radiopharmaceuticals for the theranostics of neuroendocrine neoplasms. Pharmaceuticals 2017, 10, 30. [Google Scholar] [CrossRef] [PubMed]
- Krošelj, M.; Mansi, R.; Reubi, J.C.; Maecke, H.R.; Kolenc Peitl, P. Comparison of DOTA-coupled minigastrin analogues and corresponding Nle congeners. Eur. J. Nuclear Med. Mol. Imaging 2012, 39, S533–S534. [Google Scholar] [CrossRef]
- Kaloudi, A.; Nock, B.A.; Lymperis, E.; Krenning, E.P.; de Jong, M.; Maina, T. Improving the In Vivo Profile of Minigastrin Radiotracers: A Comparative Study Involving the Neutral Endopeptidase Inhibitor Phosphoramidon. Cancer Biother. Radiopharm. 2016, 31, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Pawlak, D.; Rangger, C.; Kolenc Peitl, P.; Garnuszek, P.; Maurin, M.; Ihli, L.; Kroselj, M.; Maina, T.; Maecke, H.; Erba, P.; et al. From preclinical development to clinical application: Kit formulation for radiolabelling the minigastrin analogue CP04 with In-111 for a first-in-human clinical trial. Eur. J. Pharm. Sci. 2016, 85, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Grob, N.M.; Behe, M.; von Guggenberg, E.; Schibli, R.; Mindt, T.L. Methoxinine—An alternative stable amino acid substitute for oxidation-sensitive methionine in radiolabelled peptide conjugates. J. Pept. Sci. 2017, 23, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Rangger, C.; Klingler, M.; Balogh, L.; Pöstényi, Z.; Polyak, A.; Pawlak, D.; Mikołajczak, R.; von Guggenberg, E. 177Lu Labeled Cyclic Minigastrin Analogues with Therapeutic Activity in CCK2R Expressing Tumors: Preclinical Evaluation of a Kit Formulation. Mol. Pharm. 2017, 14, 3045–3058. [Google Scholar] [CrossRef] [PubMed]
- Klingler, M.; Decristoforo, C.; Rangger, C.; Summer, D.; Foster, J.; Sosabowski, J.K.; von Guggenberg, E. Site-specific stabilization of minigastrin analogs against enzymatic degradation for enhanced cholecystokinin-2 receptor targeting. Theranostics 2018, 8, 2896–2908. [Google Scholar] [CrossRef] [PubMed]
- Klingler, M.; Summer, D.; Rangger, C.; Haubner, R.; Foster, J.; Sosabowski, J.; Decristoforo, C.; Virgolini, I.; von Guggenberg, E. DOTA-MGS5, a new cholecystokinin-2 receptor targeting peptide analog with optimized targeting profile for theranostic use. J. Nucl. Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Konijnenberg, M.; Erba, P.A.; Mikolajczak, R.; Decristoforo, C.; Maecke, H.; Maina-Nock, T.; Zaletel, K.; Kolenc-Peitl, P.; Virgolini, I.; Przybylik-Mazurek, E.; et al. First biosafety, biodistribution and dosimetry study of the gastrin analogue 111In-CP04 in medullary thyroid cancer. Phase I clinical trial, GRANT-T-MTC. Eur. J. Nucl. Med. Mol. Imaging 2017, 44, S258. [Google Scholar]
- Sauter, A.W.; Mansi, R.; Hassiepen, U.; Muller, L.; Panigada, T.; Wiehr, S.; Wild, A.-M.; Geistlich, S.; Béhé, M.; Rottenburger, C.; et al. Targeting of the cholecystokinin-2 receptor with the minigastrin analog 177Lu-DOTA-PP-F11N: Does the use of protease inhibitors further improve in vivo distribution? J. Nucl. Med. 2018. [Google Scholar] [CrossRef]
- Nock, B.; Maina, T. Tetraamine-coupled peptides and resulting 99mTc-radioligands: An effective route for receptor-targeted diagnostic imaging of human tumors. Curr. Top. Med. Chem. 2012, 12, 2655–2667. [Google Scholar] [CrossRef]
- Povoski, S.R.; Neff, R.L.; Mojzisik, C.M.; O’Malley, D.M.; Hinkle, G.H.; Hall, N.C.; Murrey, D.A.; Knopp, M.V.; Martin, E.W. A comprehensive overview of radioguided surgery using gamma detection probe technology. World J. Surg. Oncol. 2009, 7, 11. [Google Scholar] [CrossRef]
- Von Guggenberg, E.; Dietrich, H.; Skvortsova, I.; Gabriel, M.; Virgolini, I.J.; Decristoforo, C. 99mTc-labelled HYNIC-minigastrin with reduced kidney uptake for targeting of CCK-2 receptor-positive tumours. Eur. J. Nucl. Med. Mol. Imaging 2007, 34, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Von Guggenberg, E.; Sallegger, W.; Helbok, A.; Ocak, M.; King, R.; Mather, S.J.; Decristoforo, C. Cyclic minigastrin analogues for gastrin receptor scintigraphy with technetium-99m: Preclinical evaluation. J. Med. Chem. 2009, 52, 4786–4793. [Google Scholar] [CrossRef] [PubMed]
- Breeman, W.A.P.; Fröberg, A.C.; de Blois, E.; van Gameren, A.; Melis, M.; de Jong, M.; Maina, T.; Nock, B.A.; Erion, J.L.; Mäcke, H.R.; et al. Optimised labeling, preclinical and initial clinical aspects of CCK-2 receptor-targeting with 3 radiolabeled peptides. Nucl. Med. Biol. 2008, 35, 839–849. [Google Scholar] [CrossRef] [PubMed]
- Fröberg, A.C.; De Jong, M.; Nock, B.A.; Breeman, W.A.P.; Erion, J.L.; Maina, T.; Verdijsseldonck, M.; De Herder, W.W.; Van Der Lugt, A.; Kooij, P.P.M.; et al. Comparison of three radiolabelled peptide analogues for CCK-2 receptor scintigraphy in medullary thyroid carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2009, 36, 1265–1272. [Google Scholar] [CrossRef] [PubMed]
- Kosowicz, J.; Mikołajczak, R.; Czepczyński, R.; Ziemnicka, K.; Gryczyńska, M.; Sowiński, J. Two Peptide Receptor Ligands 99mTc-EDDA/HYNIC-Tyr3-Octreotide and 99mTc-EDDA/HYNIC-D Glu-Octagastrin for Scintigraphy of Medullary Thyroid Carcinoma. Cancer Biother. Radiopharm. 2007, 22, 613–628. [Google Scholar] [CrossRef] [PubMed]
- Ocak, M.; Helbok, A.; Rangger, C.; Peitl, P.K.; Nock, B.A.; Morelli, G.; Eek, A.; Sosabowski, J.K.; Breeman, W.A.P.; Reubi, J.C.; et al. Comparison of biological stability and metabolism of CCK2 receptor targeting peptides, a collaborative project under COST BM0607. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 1426–1435. [Google Scholar] [CrossRef] [PubMed]
- Von Guggenberg, E.; Behe, M.; Behr, T.M.; Saurer, M.; Seppi, T.; Decristoforo, C. 99mTc-labeling and in vitro and in vivo evaluation of HYNIC- and (Nalpha-His)acetic acid-modified [D-Glu1]-minigastrin. Bioconjug. Chem. 2004, 15, 864–871. [Google Scholar] [CrossRef]
- Von Guggenberg, E.; Sarg, B.; Lindner, H.; Melendez Alafort, L.; Mather, S.J.; Moncayo, R.; Decristoforo, C. Preparation via coligand exchange and characterization of [99mTc-EDDA-HYNIC-D-Phe1,Tyr3]Octreotide (99mTc-EDDA/HYNIC-TOC). J. Label. Compd. Radiopharm. 2003, 46, 307–318. [Google Scholar] [CrossRef]
- Surfraz, M.B.; King, R.; Mather, S.J.; Biagini, S.C.G.; Blower, P.J. Trifluoroacetyl-HYNIC Peptides: Synthesis and 99mTc Radiolabeling. J. Med. Chem. 2007, 50, 1418–1422. [Google Scholar] [CrossRef] [PubMed]
- King, R.C.; Surfraz, M.B.; Biagini, S.C.G.; Blower, P.J.; Mather, S.J. How do HYNIC-conjugated peptides bind technetium? Insights from LC-MS and stability studies. Dalton Trans. 2007, 4998–5007. [Google Scholar] [CrossRef]
- Lay, J.M.; Jenkins, C.; Friis-Hansen, L.; Samuelson, L.C. Structure and developmental expression of the mouse CCK-B receptor gene. Biochem. Biophys. Res. Commun. 2000, 272, 837–842. [Google Scholar] [CrossRef] [PubMed]
- Kossatz, S.; Béhé, M.; Mansi, R.; Saur, D.; Czerney, P.; Kaiser, W.A.; Hilger, I. Multifactorial diagnostic NIR imaging of CCK2R expressing tumors. Biomaterials 2013, 34, 5172–5180. [Google Scholar] [CrossRef] [PubMed]
- Aloj, L.; Aurilio, M.; Rinaldi, V.; D’ambrosio, L.; Tesauro, D.; Peitl, P.K.; Maina, T.; Mansi, R.; von Guggenberg, E.; Joosten, L.; et al. Comparison of the binding and internalization properties of 12 DOTA-coupled and 111In-labelled CCK2/gastrin receptor binding peptides: A collaborative project under COST Action BM0607. Eur. J. Nucl. Med. Mol. Imaging. 2011, 38, 1417–1425. [Google Scholar] [CrossRef] [PubMed]
- Vegt, E.; de Jong, M.; Wetzels, J.F.; Masereeuw, R.; Melis, M.; Oyen, W.J.; Gotthardt, M.; Boerman, O.C. Renal toxicity of radiolabeled peptides and antibody fragments: Mechanisms, impact on radionuclide therapy, and strategies for prevention. J. Nucl. Med. 2010, 51, 1049–1058. [Google Scholar] [CrossRef] [PubMed]
- Vegt, E.; Melis, M.; Eek, A.; de Visser, M.; Brom, M.; Oyen, W.J.; Gotthardt, M.; de Jong, M.; Boerman, O.C. Renal uptake of different radiolabelled peptides is mediated by megalin: SPECT and biodistribution studies in megalin-deficient mice. Eur. J. Nucl. Med. Mol. Imaging 2011, 38, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Laverman, P.; Joosten, L.; Eek, A.; Roosenburg, S.; Kolenc Peitl, P.; Maina, T.; Mäcke, H.; Aloj, L.; von Guggenberg, E.; Sosabowski, J.K.; et al. Comparative biodistribution of 12 111In-labelled gastrin/CCK2 receptor-targeting peptides. Eur. J. Nucl. Mol. Imaging 2011, 38, 1410–1416. [Google Scholar] [CrossRef] [PubMed]
- Kaloudi, A.; Nock, B.A.; Lymperis, E.; Krenning, E.P.; de Jong, M.; Maina, T. 99mTc-labeled gastrins of varying peptide chain length: Distinct impact of NEP/ACE-inhibition on stability and tumor uptake in mice. Nucl. Med. Biol. 2016, 43, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Maina, T.; Kaloudi, A.; Nock, B.A. 99mTc-DGA1, a new radiotracer derived from a non-peptidic CCK2R-antagonist, showing excellent prospects for diagnostic imaging of CCK2R-positive human tumors with SPECT. Nucl. Med. Biol. in press.
- Wayua, C.; Low, P.S. Evaluation of a nonpeptidic ligand for imaging of cholecystokinin 2 receptor-expressing cancers. J. Nucl. Med. 2015, 56, 113–119. [Google Scholar] [CrossRef]
- Hubalewska-Dydejczyk, A.; Kulig, J.; Szybinski, P.; Mikolajczak, R.; Pach, D.; Sowa-Staszczak, A.; Fröss-Baron, K.; Huszno, B. Radio-guided surgery with the use of [99mTc-EDDA/HYNIC]octreotate in intra-operative detection of neuroendocrine tumours of the gastrointestinal tract. Eur. J. Nucl. Med. Mol. Imaging 2007, 34, 1545–1555. [Google Scholar] [CrossRef]
- Robu, S.; Schottelius, M.; Eiber, M.; Maurer, T.; Gschwend, J.; Schwaiger, M.; Wester, H.-J. Preclinical Evaluation and First Patient Application of 99mTc-PSMA-I&S for SPECT Imaging and Radioguided Surgery in Prostate Cancer. J. Nucl. Med. 2017, 58, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Aloj, L.; Caracò, C.; Panico, M.; Zannetti, A.; Del Vecchio, S.; Tesauro, D.; De Luca, S.; Arra, C.; Pedone, C.; Morelli, G.; et al. In vitro and in vivo evaluation of 111In-DTPAGlu-G-CCK8 for cholecystokinin-B receptor imaging. J Nucl. Med. 2004, 45, 485–494. [Google Scholar] [PubMed]
- Chatterjee, J.; Gilon, C.; Hoffman, A.; Kessler, H. N-methylation of peptides: A new perspective in medicinal chemistry. Acc. Chem. Res. 2008, 41, 1331–1342. [Google Scholar] [CrossRef] [PubMed]
| [99mTc]Tc-HYNIC-MGS5 | [99mTc]Tc-HYNIC-MGS11 | |||
|---|---|---|---|---|
| 1 h p.i. | 4 h p.i. | 1 h p.i. | 4 h p.i. | |
| Tumor/blood | 21.6 ± 5.1 | 273 ± 151 | 15.6 ± 4.5 | 177 ± 55 |
| Tumor/kidney | 2.4 ± 0.3 | 3.3 ± 1.1 | 2.0 ± 0.6 | 2.6 ± 0.8 |
| Tumor/stomach | 1.5 ± 0.2 | 2.0 ± 0.4 | 6.5 ± 1.9 | 10.7 ± 1.4 |
| Tumor/pancreas | 2.4 ± 0.3 | 4.2 ± 2.0 | 20.6 ± 11.7 | 34.8 ± 9.7 |
| Tumor/intestine | 14.2 ± 1.7 | 19.2 ± 7.5 | 32.3 ± 5.0 | 61.1 ± 14.3 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klingler, M.; Rangger, C.; Summer, D.; Kaeopookum, P.; Decristoforo, C.; von Guggenberg, E. Cholecystokinin-2 Receptor Targeting with Novel C-terminally Stabilized HYNIC-Minigastrin Analogs Radiolabeled with Technetium-99m. Pharmaceuticals 2019, 12, 13. https://doi.org/10.3390/ph12010013
Klingler M, Rangger C, Summer D, Kaeopookum P, Decristoforo C, von Guggenberg E. Cholecystokinin-2 Receptor Targeting with Novel C-terminally Stabilized HYNIC-Minigastrin Analogs Radiolabeled with Technetium-99m. Pharmaceuticals. 2019; 12(1):13. https://doi.org/10.3390/ph12010013
Chicago/Turabian StyleKlingler, Maximilian, Christine Rangger, Dominik Summer, Piriya Kaeopookum, Clemens Decristoforo, and Elisabeth von Guggenberg. 2019. "Cholecystokinin-2 Receptor Targeting with Novel C-terminally Stabilized HYNIC-Minigastrin Analogs Radiolabeled with Technetium-99m" Pharmaceuticals 12, no. 1: 13. https://doi.org/10.3390/ph12010013
APA StyleKlingler, M., Rangger, C., Summer, D., Kaeopookum, P., Decristoforo, C., & von Guggenberg, E. (2019). Cholecystokinin-2 Receptor Targeting with Novel C-terminally Stabilized HYNIC-Minigastrin Analogs Radiolabeled with Technetium-99m. Pharmaceuticals, 12(1), 13. https://doi.org/10.3390/ph12010013






