Abstract
A dysregulated cellular Ca2+ homeostasis is involved in multiple pathologies including cancer. Changes in Ca2+ signaling caused by altered fluxes through ion channels and transporters (the transportome) are involved in all steps of the metastatic cascade. Cancer cells thereby “re-program” and “misuse” the cellular transportome to regulate proliferation, apoptosis, metabolism, growth factor signaling, migration and invasion. Cancer cells use their transportome to cope with diverse environmental challenges during the metastatic cascade, like hypoxic, acidic and mechanical cues. Hence, ion channels and transporters are key modulators of cancer progression. This review focuses on the role of transient receptor potential (TRP) channels in the metastatic cascade. After briefly introducing the role of the transportome in cancer, we discuss TRP channel functions in cancer cell migration. We highlight the role of TRP channels in sensing and transmitting cues from the tumor microenvironment and discuss their role in cancer cell invasion. We identify open questions concerning the role of TRP channels in circulating tumor cells and in the processes of intra- and extravasation of tumor cells. We emphasize the importance of TRP channels in different steps of cancer metastasis and propose cancer-specific TRP channel blockade as a therapeutic option in cancer treatment.
1. Introduction
Metastasis is the most important factor determining patient prognosis because most cancer patients die from the consequences of metastases [1]. This is particularly relevant for cancers which are usually asymptomatic in early stages and for which no easy screening tools are available such as the determination of prostate-specific antigen (PSA) levels in the plasma for prostate cancer. Thus, pancreatic ductal adenocarcinoma (PDAC) and non-small cell lung cancer (NSCLC) are two examples for cancers that are frequently diagnosed only in an advanced stage when macroscopic metastases have already developed. Accordingly, the prognosis of these cancers is extremely poor with 5-year survival rates of only 5% and 13% for European PDAC [2] and NSCLC patients [3], respectively. Disappointingly, the enormous gain of knowledge with respect to molecular and genetic mechanisms underlying these cancers has not yet led to therapeutic success. Thus, there still remains an unmet need for better understanding the pathophysiology of these diseases. Given the crucial role of metastasis for patient prognosis, it is particularly important to develop new concepts in the understanding of the mechanisms underlying metastasis.
Such a new concept, namely the involvement of ion-conducting transporters in neoplastic diseases has been emerging in recent years. Proteins involved in ion transport (the transportome) were found to contribute to essentially all “hallmarks of cancer” [4]. In this context, it is important to keep in mind that the transportome is the “working horse” of epithelial cells that are the origin of ~90% of all malignant tumors. The transportome is “misused” by cancer cells and regulates, among others, processes such as tumor cell proliferation, apoptosis, senescence, migration, invasion, metabolism and growth factor signaling. This is in part due to the dysregulated expression and function of transportome members in many tumors. Moreover, dysregulated expression frequently correlates with patient prognosis (see [5] for a series of reviews, e.g., [6,7,8,9]). The consistent presence of dysregulated ion channel expression and function in all cancers studied so far [10] has recently led to the provocative question of whether cancer hallmarks can be viewed as oncochannelopathies [11].
In the present review, we will focus on the contribution of transportome members to steps of the so-called metastatic cascade, i.e., on the mechanisms underlying the hematogenous or lymphatic spread of tumor cells from the primary tumor to distant organs. The literature on the cancer transportome has grown exponentially during the last years so that we will limit our discussion primarily to transient receptor potential (TRP) channels (see Table 1). The steps of the metastatic cascade are well defined. After leaving the primary tumor cancer cells invade into and migrate through the neighboring tissue to reach blood or lymph vessels that may have been newly formed (tumor angiogenesis). Following intravasation they are swept away with the bloodstream or the lymph. Within the bloodstream, circulating tumor cells (CTCs) interact with different blood cells such as platelets [12]. Platelet-CTC interactions seem to increase CTC survival, extravasation and metastasis [13,14]. Surviving CTCs adhere to endothelial cells lining the vessels, migrate intravascularly and penetrate the endothelial cell layer (extravasation). Alternatively, individual cancer cells or cell clusters may be trapped mechanically in small capillaries. Finally, the cells expand to form metastases in different parts of the body, and new vessels are formed to supply them with nutrients [1,15]. The extravasation of tumor cells bears many similarities with the recruitment of immune cells [16]. For example, some of the relevant adhesion molecules required for immune cell recruitment, such as LFA-1 or ICAM-1, have also been found in lung adenocarcinoma cells [17,18].

Table 1.
TRP channels and their impact in malignant phenotypes.
TRP channels are a large family of cation channels all showing sequence homology to the Drosophila TRP protein. Its subfamilies present in mammals are: the ankyrin subfamily TRPA, the canonical subfamily TRPC, the melastatin subfamily TRPM, the mucolypin subfamily TRPML, the polycystin subfamily TRPP and the vanilloid subfamily TRPV. They have varying selectivity ranging from nonselective cation channels to highly selective channels (e.g., for Ca2+). Their gating is also quite heterogeneous, as they can be gated by e.g., ligands, temperature or mechanical stimuli. [19,20]. TRP channels are involved in a wide variety of cellular processes. Some examples include Ca2+ homeostasis, nociception, inflammation, phagocytosis, or cell motility (e.g., reviewed in [21,22,23,24]). Their function can be described in very general terms as that of “cellular sensors”. Thereby, TRP channels confer the ability onto metastasizing cancer cells to respond to ambient physico-chemical signals. Microenvironmental stimuli are of central importance throughout the metastatic cascade. During the metastatic cascade cancer cell behavior is shaped by a wide variety of (harsh) microenvironmental stimuli [1]. Examples of such stimuli along the metastatic cascade and how their potential impact on TRP channel activity can regulate tumor and stromal cell behavior will be the main focus of this review.
There are numerous studies showing a clear correlation between cancer patient survival and TRP channel expression, e.g., TRPC1, TRPM2 and TRPV4 in breast cancer [25,26,27], TRPM7 in PDAC [28], TRPM8 in bladder cancer and osteosarcoma [29,30] and TRPV2 in breast and esophageal cancer [31,32] to name just a few examples (see also Table 2). Since cancer patients usually die from the consequences of metastases, the multitude of these observations strongly indicates that TRP channels have a significant share in the processes underlying the metastatic cascade. Thus, studying the role of TRP channels in steps of the metastatic cascade is a clinically relevant undertaking and bears great therapeutic potential.

Table 2.
TRP channel expression in different cancer types and its correlation with patient prognosis.
2. TRP Channels in Cancer Cell Migration and Invasion
Cell migration involves a large variety of temporally and spatially coordinated processes ranging from cell polarization, adhesion/de-adhesion to/from the surrounding matrix and/or neighboring cells, as well as extensive cytoskeletal and membrane dynamics [70,71,72]. Many components of the migration machinery are Ca2+-sensitive, including myosin-II [73], focal adhesions [74] or Ca2+-sensitive ion channels [72]. Hence, the intracellular Ca2+ concentration of migrating tumor (stroma) cells is tightly regulated, both spatially and temporally [75]. In fact, it is widely accepted that ion transport across the plasma membrane via numerous Na+, Ca2+ and K+ channels and transporters is crucial for cell migration [7,72,76]. Additionally, ion and H2O fluxes strongly depend on an appropriate plasma membrane potential (Vm). Vm as a key biophysical signal thereby regulates e.g., cell volume and migration and provides the driving force for Ca2+ influx. Hyperpolarization and depolarization can directly affect normal cell as well as cancer cell function. A depolarized Vm in many cancer types could be linked to e.g., cancer cell proliferation (reviewed in [77]). The following chapter will focus on the role of TRP channels in cancer cell migration and invasion.
Before summarizing recent findings in the field, we would like to critically discuss the experimental approaches. The gold standard is intravital microscopy because cells are migrating in their complex physiological environment. But it is not trivial to control and manipulate individual components of the tumor microenvironment such as pH or mechanical properties. Controlling the ambient conditions is more easily achieved in an in vitro setting, yet in a reductionist fashion. Boyden chambers for example are popular for in vitro assays of tumor cell invasion. A frequently used protocol is to coat the filter membranes with matrix proteins and induce “invasion” by applying a chemotactic gradient. However, under such experimental conditions it is impossible to distinguish “invasion” from chemotaxis. Inhibiting chemotaxis will lead to the same readout as inhibiting “invasion” since the steering mechanisms can be affected without impairing the migration motor [78,79]. Inhibiting either mechanism will lead to a reduced number of cells reaching the lower compartment of the Boyden chamber. Unfortunately, the proper control experiments, i.e., the use of Boyden chambers in the absence of chemotactic gradients are not always performed. Wound healing assays are also often used for migration analysis and can be a suitable approach to evaluate directionality of cell movement. Migration analysis within a 3D matrix as well can be a useful tool to analyze the matrix invasion of tumor cells; here, translocation as well as matrix digestion via e.g., MMP secretion should be taken into account. The papers cited below are mainly limited to studies considering the above-mentioned criteria.
2.1. TRPM7
TRPM7 is involved in several aspects of cell motility such as polarization [80], adhesion [81,82] and migration [83]. It is a Ca2+- and Mg2+-permeable channel with an α-kinase domain [84]. TRPM7 is essential for PDAC progression and invasion. TRPM7 expression in primary tumors is associated with PDAC lymph node metastasis [28]. Its over-expression correlates with increased tumor size and advanced tumor stages of pancreatic cancer and hence, inversely with patient prognosis [47,85]. Silencing of TRPM7 in PDAC cell lines leads to a reduction of cancer cell invasion [28]. TRPM7 function in PDAC invasion can be partly explained by TRMP7-mediated Mg2+ influx and subsequent kinase activation and heat shock protein secretion. Activation of TRPM7 and Hsp90a secretion could be linked to MMP-2 secretion which is an important step to degrade surrounding ECM and initiate cancer cell invasion [28]. In the non-small cell lung cancer (NSCLC) cell line A549 TRPM7 is upregulated after epidermal growth factor (EGF) stimulation and contributes to EGF-mediated increase in cell migration. Accordingly, shRNA-based silencing of TRPM7 attenuates the stimulation by EGF [48]. In breast cancer, myosin-II-based cell tensions and de-adhesion of cell-matrix contacts are TRPM7-dependent and TRPM7 is necessary for breast cancer metastasis into the lung in a murine model [49] (see also below). Silencing of TRPM7 in MDA-MB-435 breast cancer cells leads to a reduced migration. This can be accounted for a TRPM7-dependent regulation of Src and MAPK kinase pathways [51]. However, it should be noted that the origin of MDA-MB-435 cells has recently been questioned [65]. These findings suggest that at least part of the role of TRPM7 is calcium-independent. It rather involves its α-kinase domain which is needed for phosphorylation of myosin-IIA heavy chain [50,51,86]. A similar role of TRPM7 in cancer cell migration was found in a number of other tumors such as nasopharyngeal carcinoma and ovarian cancer [53,54]. In addition, TRPM7 is also known for its role in tumor cell proliferation [65,87,88].
2.2. TRPM8
There are numerous reports describing a role for TRPM8 in cancer cell migration and invasion. However, depending on the type of cancer its impact may be pro- or anti-migratory. In oral squamous cell carcinoma, activation of TRPM8 leads to an increase of MMP-9 activity and cell migration [55]. In breast cancer, TRPM8 promotes the aggressiveness of breast cancer cells by regulating epithelial-mesenchymal transition (EMT) via the activation of the AKT/GSK-3β pathway [56]. Silencing of TRPM8 decreases and over-expression increases the motility of MDA-MB-231 or MCF-7 breast cancer cells. Activation of TRPM8 in combination with TRPA1 leads to enhanced motility also in lung cancer cells, whereas knockdown shows the opposite effect [33]. In glioblastoma cells, TRPM8 inhibition reduces the migration and chemotaxis [57]. In contrast, in PDAC cells and in prostate cancer cells TRPM8 function and expression reduces cell motility [58,59,89]. TRPM8 function is also linked to cell survival in prostate cancer and TRMP8 suppression lead to oxidative stress and apoptosis [60]. TRPM8 channels are also regulated by intracellular proteins, so called TRP channel-associated factors (TCAFs). E.g.,TCAF1 leads to a reduction of prostate cancer cell velocity and migration directionality [90]. A modification of TRPM8 channels can also be mediated via N-glycosylation in HEK293 cells, but not in PDAC cell lines Panc-1, MiaPaCa2 or BxPc3, which express non-glycosylated channel isoforms [91]. Independently of its conductive function, TRPM8 acts as a Rap1 GTPase inhibitor, inhibiting endothelial cell migration [92].
2.3. TRPV2
Some TRPV channels have been found to be involved in cell proliferation, apoptosis, angiogenesis, migration, invasion, and generally in cancer progression [93]. The elevated expression of TRPV2 in metastatic prostate cancer points to a role of this channel in the metastatic cascade [61]. TRPV2 promotes cell migration and the invasive cancer cell phenotype [94]. Antimicrobial peptide LL-37, which is released from infiltrating immune cells, is able to activate TRPV2 and the Ca2+-activated K+ channel (KCa1.1) in different breast cancer cell lines leading to increased migration [62]. High TRPV2 expression is also correlated with a poor prognosis of esophageal squamous cell carcinoma (ESCC) [32].
2.4. TRPV4
TRPV4 is upregulated in breast cancer patients. TRPV4-mediated activation of protein kinase B leads to enhanced Akt and focal adhesion kinase (FAK) phosphorylation, which are both associated with cell migration. Pharmacological activation of TRPV4 in a breast cancer cell line causes downregulation of adhesion molecules like E-cadherin and β-catenin [26]. Upregulation of TRPV4 is accompanied by changes of the cytoskeletal network, enhanced blebability and reduced cell stiffness, facilitating cancer metastasis through neighboring tissues. It was suggested that TRPV4 activation thereby regulates breast cancer cell extravasation [63]. In gastric cancer, TRPV4 can be activated by co-localized calcium-sensing receptors, leading to Ca2+-induced proliferation, migration and invasion [64]. TRPV4 channels are also important players in tumor vascularization by regulating endothelial cell migration [95] (see chapter “TRP channels in tumor vascularization”). Moreover, they modulate the endothelial barrier permeability (see chapter “Extravasation of tumor cells” below).
2.5. TRPV6
TRPV6 is associated with both pancreatic and breast cancer. TRPV6 is upregulated in human pancreatic cancer specimens and silencing of TRPV6 significantly inhibits invasion, proliferation and migration of pancreatic cancer cells [66]. In breast cancer, TRPV6 expression is higher in invasive areas of breast cancer tissues in comparison to the corresponding non-invasive areas. Moreover, TRPV6 silencing inhibits MDA-MB-231 and MCF-7 breast cancer cell migration. Therefore, TRPV6 is suggested to be involved in the metastatic process of breast cancer [65].
2.6. TRPC1
TRPC1 is required for PDGF- and EGF-mediated directional migration in glioma cells [39,96] by cooperating with chloride channels that are activated by TRPC1-mediated Ca2+ influx [97]. TRPC1 channels are also necessary for VEGF signaling and thyroid cancer migration and invasion [40]. TRPC1-mediated Ca2+ influx is needed for NSCLC proliferation in response to EGF signaling [37]. Transforming growth factor β1 (TGF-β1) induces Ca2+ entry likely via TRPC1 and NCX1 that raise cytosolic Ca2+ in pancreatic cancer cells so that knockdown of TRPC1 reverses TGF-β1-induced pancreatic cancer cell motility [36]. Silencing of TRPC1 or its activator STIM1 reduce TGF-β1 mediated calpain activation and subsequent cell migration, as well as expression of EMT markers such as N-cadherin and vimentin [34]. TRPC1 together with STIM1/Orai1 is also needed for colon cancer cell line (HCT-116) migration [98].
2.7. TRPC4
TRPC4 contributes to enhanced invasion and metastasis of granule precursor-derived human medulloblastoma [41]. Here, the authors use OGR1 to induce the expression of TRPC4 which promotes the migration of medulloblastoma cells.
2.8. TRPC5
It has been shown that overexpression of TRPC5 correlates with a poor prognosis in colon cancer by promoting tumor metastasis via the hypoxia-induced factor 1α (HIF-1α) -Twist signaling pathway [42].
2.9. TRPC6
TRPC6 is linked to several cancer types such as prostate, lung and colon cancer as well as glioblastoma. In prostate cancer, TRPC6 is suggested to be involved in cancer cell invasion into a “matrigel-based” matrix [99]. TRPC6 is detected in benign and malignant human prostate tumor tissues as well as in prostate cancer cell lines and its expression levels are associated with the histological grade [45]. Expression profiles of some TRP channels including TRPC6 are changing during the progression of prostate cancer towards the more aggressive and hormone-refractory stages [100]. TRPC6 also has been linked to lung cancer [44]: inhibition of TRPC6 channels lowers the intracellular Ca2+ concentration in A549 cells and strongly reduces the invasion of A549 cells. In human glioblastoma cells, TRPC6 expression is augmented by hypoxia and increases proliferation and cell invasion [43]. Here, TRPC6 is suggested to be a key mediator of Notch-driven glioblastoma invasiveness and angiogenesis. TRPC6 was also found to be upregulated in esophageal squamous cell carcinoma in which it negatively correlates with patients survival [68].
2.10. Other TRP Channels
The TRPA1 channel is involved in cellular invasion. It has been shown with transwell-invasion-assays that methyl syringate, a TRPA1 agonist inhibits induction of COX-2 and cell invasion of the NSCLC cell line A549 and of the fibrosarcoma cell line HT-1080 under hypoxic conditions [101].
To the best knowledge of the authors, there is no direct evidence linking TRPML channels to cancer invasiveness and metastasis, although the channel has an altered expression in glioblastoma and breast cancer [102]. This might be due to the subcellular localization of TRPML channels, as they are primarily expressed in endosomes and lysosomes, and they are not as easily investigated as channels residing in the plasma membrane. Moreover, the literature focuses on the effect of TRPML on autophagy and autophagy-related signaling that is independent of the calcium permeability of the channel [102]. However, these channels are key regulators of lysosomal calcium release, and moreover, their expression is linked to ERK1/2 and Akt signaling which plays a role in cell migration.
3. Influence of the Tumor Microenvironment on TRP Channels
The initial step of cancer cell invasion and migration out of the primary tumor is strongly regulated by a variety of tumor microenvironmental factors like pH, hypoxia, matrix stiffness, cytokines and the infiltrating cellular components such as fibroblasts and immune cells. The following chapter will link these factors to TRP channel function in tumor progression and invasion.
3.1. pH
Due to insufficient vascularization, limited supply of metabolic substrates, metabolic reprogramming towards the so-called aerobic glycolysis (Warburg effect) and-at least in later stages–tumor anemia, primary tumors and cancer cells export increased amounts of H+ and the tumor microenvironment (TME) becomes acidified [103,104,105,106]. In PDAC the extracellular pH landscape is superimposed by an intermittent postprandial acidification of the interstitium which is a consequence of the massive HCO3- secretion into the pancreatic ducts [107,108]. Similarly, the pH landscapes of stomach, bone or skin tumors are superimposed by the respective characteristic acid-base homeostasis of these organs. Several TRP channels are regulated by an extra-/intracellular acidosis [19,109]. They can either be activated, e.g., TRPV1/3 [20], TRPC5 [110] or inhibited by an acidosis such as TRPM2 [111] and TRPM8 [112], or their selectivity is regulated by pH (e.g., TRPM7; [113]). There is a close interrelation between the regulation of TRPM7 by protons and the divalent cations Ca2+ and Mg2+. On the one hand, the effect of the extracellular pH on TRPM7 activity depends on the presence of extracellular Ca2+ and Mg2+ [114]. On the other hand, the selectivity of TRPM7 channels for mono- or divalent cations is regulated by the extracellular pH. An acidification (e.g., pH 6) increases the permeability for monovalent cations [113]. For tumor cells, the impact of an intracellular alkalization (pH >7.2) is more relevant because tumor cells are frequently characterized by an alkaline intracellular pH [105]. TRMP7 channels are activated by an alkaline pH in these cells [115].
TRPV1 is a nonselective cation channel that is not only regulated by protons but also permeable for protons [20,116]. Low extracellular pH in lymphatic endothelial cells induces lymph-angiogenesis in a TRPV1-dependent manner [117]. This pH-dependent activation of TRPV1 also induces cytokine production (IL8) by endothelial cells.
The effect of pH on TRPV4 cells is controversially. Heterologously expressed TRPV4 channels can be activated by a drop of extracellular pH in CHO cells [118]. However, in esophageal epithelial cells TRPV4 activity is suppressed by an acidic pH [119].
TRPC4 and TRPC5 channels are already activated by a modest decrease of the extracellular pH (e.g., pH 7.0) when expressed in HEK293 cells [110].
TRPM2 channels are inhibited by extracellular acidification (pH 6.5) as protons compete with other cations like Ca2+ or Na+ for channel permeation and act as competitive TRPM2 antagonists [111]. Another possible mechanism for proton-dependent regulation of TRP channel activity was shown for TRPM8; the channel activity is reduced by extracellular divalent cations as well as by protons. The authors showed that this is due to a change in the membrane surface charge caused by an increased proton concentration [112].
3.2. Hypoxia
The high metabolic demand of the tumor cells and the insufficient blood and oxygen supply due the compression and inadequate number of vessels frequently cause hypoxia of the tumor stroma [120,121,122]. Hypoxia can be sensed by several TRP channels such as TRPM7 and TRPA1 [123], TRPC1 [25,40], TRPC6 [43,124,125,126], both in cancer cells and in stromal cells [126,127]. Hypoxia is commonly associated with increased production of reactive oxygen species (ROS) that can elicit both protumorigenic and antitumor effects [128]. TRPC6, TRPV1, TRPM2/4/7, TRPA1 are activated by ROS [19], and they are regulators of relevant steps of the metastatic cascade.
TRPM2 channels can be activated by hypoxia. They are expressed in several cancer types, for instance in breast cancer [129], neuroblastoma [130] and malignant melanoma [131]. In neuroblastoma cells, TRPM2 depletion leads to a suppressed HIF-1α signaling. Inhibiting TRPM2 function by mutating its pore region increases mitochondrial ROS production [132]. Accordingly, TRPM2 activation by oxidative stress in ischemic hearts prevents ROS production in the hypoxic heart [133]. A protective role of TRPM2 under hypoxia can also be found in neuroblastoma cells, in which activated TRPM2 channels lead to increased expression of superoxide dismutase 2 (SOD2) and reduced ROS levels [130,132].
TRPM7 as well as TRPA1 can be activated by hypoxia and increased ROS levels [123,134,135]. The prominent role of TRPM7 channels in cancer progression and cancer cell migration has already been discussed (see “TRP channels in cancer cell migration and invasion”).
TPRV1 and TRPV4 channels are activated under hypoxic conditions in pulmonary artery smooth muscle cells and induce migration [136].
In the follicular thyroid cancer cell line ML-1, knockdown of TRPC1 channels leads to decreased HIF-1α levels [40]. Corresponding results were found in breast cancer cells, in which hypoxia increases TRPC1 expression and TRPC1 regulates hypoxia-induced signaling [25].
In glioma cells, TRPC6 is upregulated and required for the hypoxia-mediated increase in proliferation and cell invasion [43]. Activated TRPC6 stabilizes HIF-1α in hypoxic glioma cells and supports hypoxic glucose metabolism of cancer cells via the GLUT1 transporter [124]. TRPC6 channels are also activated in a hypoxic environment in pancreatic stellate cells, which are the main producers of extracellular matrix proteins in PDAC [126,137]. Similar results were found in hepatic stellate cells, in which TRPC6 expression increases under hypoxic conditions [127].
3.3. Cytokines
The tumor microenvironment is a rich source of cytokines and growth factors secreted by tumor cells, stromal cells and infiltrating immune cells. Cytokine and growth factor receptors frequently trigger TRP channel-dependent signaling cascades [137]. In addition, TRP channels can also modify cytokine secretion of cancer and stroma cells and thereby modify the composition of the tumor microenvironment. However, it must be stated at this point that many of the studies investigating the role of TRP channels in cytokine secretion were not made with tumor cells. Nonetheless, they can be taken as proof-of-principle and studies made with immune cells are highly relevant because of the consistent immune cell infiltration of the tumor stroma.
TRPM2 is important for secretion of IL-2, IFNү and IL-17 in T-lymphocytes [138] as well as for IL-8 secretion in monocytes [139]. Stimulation of TRPM3 channels leads to activation of extracellular signal-regulated protein kinase (ERK1/2) and transcription of IL-8, a proinflammatory CXC chemokine important for proliferation, survival and migration of cancer cells in lung cancer and PDAC [140,141,142,143]. TRPM8 inhibition in murine peritoneal macrophages leads to a pro-inflammatory cytokine profile with increased TNFα and decreased IL-6 secretion [144]. TRPM8 activators like eucalyptol inhibit secretion of TNFα, IL-1β, IL-6 and IL-8 in monocytes [145]. In lung epithelial cells, TRPM8 activation increases transcription of IL-1α, IL-1β, IL-4, IL-6, IL-8, IL-13 and TNFα [146].
Ca2+ entry through TRPV2 was shown to be involved in IL-6 secretion in RAW264 and murine macrophages [147]. IL-8 secretion in human non-melanoma skin cancer can be stimulated by TRPV4, thereby leading to a possibly inhibitory autocrine circuitry, because IL-8 induces the downregulation of TRPV4 channels [148]. In human airway epithelial NCI-H292 cells, TRPV4 activation triggers Ca2+ entry and release of IL-8 and prostaglandin E2 (PGE2) in vitro and increases KC levels in in vivo murine bronchoalveolar lavage fluids [149].
3.4. Mechanical Properties of Tumor Cells and the Tumor Microenvironment
In addition to the above mentioned chemical stimuli, metastasizing tumor cells and stromal cells are also exposed to mechanical stimuli [150]. Altered mechanics is one of the main characteristics of most cancer types. In fact, the clinical detection of a tumor by palpation relies on the typical mechanical properties of the tumor tissue [150,151]. The elasticity of the tumor stroma [150,152] and the tissue pressure [121,153] are usually higher than those of the normal organs. PDAC and breast cancer may serve as prominent examples [154,155,156,157]. Altered mechanical properties not only stimulate the cancer cells. They have an equal impact on stromal cells as illustrated by the response of pancreatic stellate cells to a mechanical load. They are activated by an elevated tissue pressure and substrate rigidity [152,158].
Moreover, circulating tumor cells are exposed to massive shear forces while in the bloodstream and prior to extravasation. Finally, tumor and stroma cell migration itself also generates mechanical signals within the cells that–via TRP channel activation–modulate the migratory behavior [159]. There is ample evidence that TRP channels are involved in mechano-signaling [125]. TRPC1 [158,160], TRPM7 [161], TRPV4 [63], TRPA1 channels [162] are some of the relevant TRP channels that are also required for specific steps of the metastatic cascade.
TRPC1 channels are found at the rear end of polarized U2OS osteosarcoma cells. TRPC1 knockdown leads to disturbed cell polarity, decreased cell stiffness and disorganization of the actin filaments and microtubules [163]. In pancreatic stellate cells TRPC1 is involved in responding to an increase of the ambient pressure and its activation leads to increased migratory activity of pancreatic stellate cells [158]. TRPC1 also contributes to mechano-signaling during migration of MDCK-F cells and fibroblasts. Knockdown or knockout of TRPC1 attenuates calcium transients following mechanical stretch. Moreover, TRPC1 channels are needed for MDCK-F cells to respond to directional mechanical cues [160].
TRPM7 can be activated by mechanical stimuli like membrane stretch as well as through phospholipase C (PLC) signaling [164,165]. TRPM7 channels are involved in calpain signaling and myosin-II activation and modulate actomyosin cytoskeleton contraction [81,86]. In neuroblastoma cells TRPM7 modulates the cytoskeletal organization and affects the malignancy of tumor cells by regulating actomyosin dynamics and cell-matrix interactions [166].
In tumor-derived endothelial cells TRPV4 expression levels are lowered. This leads to decreased mechanosensitivity and increased cell spreading on stiff matrices—an effect that is restored by overexpression of TRPV4. Prostate cancer-derived endothelial cells with low TRPV4 expression showed increased migration and abnormal angiogenesis [167]. TRPV4 is also required for breast cancer cell invasion. In breast cancer, TRPV4 overexpression leads to cancer cell softening, increased cell blebbing and actin reorganization. Altered mechanics were assessed indirectly with a micropipette aspiration technique. This was proposed to point to a role of TRPV4 channels in cancer cell extravasation by reducing cancer cell rigidity and improving the ability of cancer cells to infiltrate through the surrounding tissue [63].
3.5. Stroma Cells
The function of stromal cells such as fibroblast and immune cells, that are recruited and activated by cancer cells, is regulated by different TRP channels as well [137]. Our group has begun a systematic analysis of the (TRP) channels regulating the function of pancreatic stellate cells. These cells play a major role in PDAC progression by underlying the desmoplastic reaction within the tumor stroma and they are also involved in acute and chronic pancreatitis. Their functions rely on intracellular Ca2+ signaling [168,169]. Blockade of Ca2+-release-activated Ca2+-channels (CRAC) by GSK-7975A inhibits Ca2+ signaling in pancreatic stellate cells and attenuates pancreatitis [169].
Activation and migration of pancreatic stellate cells depend on TRPC1 channel expression. As mentioned in the preceding paragraph, TRPC1 is involved in the mechano-signaling of murine pancreatic stellate cells and needed for pressure-dependent activation [158]. TRPC3 channels are upregulated in the PDAC stroma. By cooperation with KCa3.1 channels they are necessary for pancreatic stellate cell migration and chemotaxis by mediating Ca2+ influx necessary for calpain stimulation [170]. TRPC6 channels are required for hypoxia-induced activation and autocrine stimulation of pancreatic stellate cells [126].
In hepatic stellate cells, TRPM7 is in involved in cell activation via the ERK and phosphoinositide 3-kinase (PI3K) pathway [171]. Inhibition or knockdown of TRPM7 lead to reduced proliferation and attenuated expression of activation markers like α-smooth muscle actin and Col1α1 in response to platelet-derived growth factor (PDGF) and TGF-β1 stimulation [171,172]. TRPM7 also underlies Ca2+ signaling at the leading edge of migrating lung fibroblasts [173]. In prostate cancer-associated fibroblasts, activation of TRPA1 leads to increased Ca2+ levels and elevated hepatocyte growth factor (HGF) and vascular endothelial growth factor (VEGF) secretion. Co-cultured prostate cancer cells are rescued from apoptosis by TRPA1 activation [174].
Infiltrating immune cells like neutrophils are important constituents of the tumor stroma in numerous tumors, including PDAC [175,176]. Neutrophils are recruited to the PDAC stroma via CXCR2 signaling [177] which in turn relies on TRPC6 channel activity [79]. It is discussed controversially whether TRPM2 channels contribute to neutrophil chemotaxis [139,178,179,180] Other neutrophilic TRP channels that are linked to chemotaxis or tissue infiltration include TRPM7 [139,178,179,180] and TRPV4 [181]. For a detailed overview of TRP channel function in neutrophil granulocytes we refer to a recent review from our group [23].
Taken together, the tumor microenvironment encompasses a wealth of different stimuli that shape cancer and stromal cell behavior. TRP channels are not only the sensors for these stimuli, they are also involved in transducing these external stimuli to altered cellular behavior and finally modify the tumor microenvironment by inducing e.g., cytokine secretion.
4. TRP Channels in Tumor Vascularization
Tumor cells must have access to blood or lymph vessels in order to spread within the body. They can either enter already existing vessels in the host organ, or they can enter newly formed vessels within the tumor. Thus, tumor angiogenesis is generally a prerequisite for metastasis. Tumor angiogenesis is initiated among others by growth factors secreted by tumor cells into the hypoxic tumor microenvironment such as VEGF, EGF and many others [95]. It strongly relies on intracellular Ca2+ signaling which may in part be mediated by TRP channels (reviewed in [95,182,183]). However, there are discrepancies between in vitro and in vivo studies. While the former reveal a participation of TRPC1 and TRPC6 channels in endothelial tube formation [184,185], the respective knockout mice appear to have a normal vasculature [3,186]. On the other hand, modulating TRPV4 channel activity pharmacologically (4α-PDD; [187]) or mechanically [188] elicits concordant effects in vivo and in vitro. It is interesting to note that altered expression of TRP channels is also observed in tumor-derived endothelial cells. This has been well documented for TRPV4 channels in breast cancer and prostate cancer-derived endothelial cells [167,189,190].
5. Extravasation of Tumor Cells
Extravasation of circulating tumor cells may originate from single tumor cells or cell clusters [12]. Prior to crossing the vessel wall, tumor cells have to adhere to endothelial cells. For extravasation of single tumor cells, analogies with immune cells are evident. Accordingly, adhesion molecules expressed by endothelial and tumor cells are crucial. Prominent examples are the family of cadherins, selectins, integrins or the Ig superfamily, including ICAM-1 or VCAM-1. There are several examples showing that the expression of adhesion molecules in endothelial cells is modulated by Ca2+-permeable ion channels. Overexpression of Orai1 potentiates the expression of ICAM-1 and VCAM-1 [191], silencing of TRPC1 attenuates cisplatin-induced ICAM-1 expression and endothelial dysfunction [192] and overexpression of TRPC3 enhances TNFα-induced VCAM-1 expression. Binding of selectins to their ligands is Ca2+-dependent. P-selectin has been identified to mediate adhesion of various leukocytes and certain types of cancer cells [193]. Its expression in endothelial cells is upregulated by TRPV4 agonists [194]. E-selectin with its ligands sialyl-Lewis-a or sialyl-Lewis-x and CD44 is important for the early attachment of cancer cells to endothelial cells [15]. Most studies only investigate the invasion of tumor cells which precedes intravasation and follows extravasation. We have referred to the role of TRP channels therein in one of the earlier sections of this review.
By analogy with the increased adhesion of monocytes to endothelial cells that is indirectly mediated by TRPC3 channels [195], one would expect a similar behavior for tumor cells as well. Channel-mediated upregulation of endothelial vascular cell adhesion molecule (VCAM)-1 should lead to an increase of adhesion of tumor cells to the endothelium. However, so far there are only very few studies investigating this aspect of the metastatic cascade. Using single cell force spectroscopy we recently measured cell-cell adhesion forces between A549 non-small cell lung cancer cells and human microvascular endothelial (HMEC-1) cells. We could show that inhibition or silencing of the Ca2+-activated potassium channel KCa3.1, which, by transporting positive charges to the extracellular space, provides electrical driving force for Ca2+ influx via TRP channels [170], increases ICAM-1-dependent adhesion between A549 and HMEC-1 cells [17]. One important conclusion of our study is that the adhesion of tumor cells to endothelial cells is largely regulated by endothelial KCa3.1 channels. Since inhibition of KCa3.1 channels leads to a decrease of the intracellular Ca2+ concentration [170,196], these channels must regulate ICAM-1 expression in a different manner than Orai1 or TRPC1 which mediate an increase of the intracellular Ca2+ concentration [184,185].
The limited knowledge on the role of ion channels in cell-cell adhesion contrasts with that on cell-matrix adhesion. Several studies have shown a role of TRP channels in this process. A few examples are listed in the following: inhibition of TRPC1 decreases adhesiveness of CNE2 nasopharyngeal tumor cells [38], TRPC2 channels regulate adhesion of rat thyroid FRTL-5 cells [197], silencing TRPM7 channels increases the adhesiveness of human umbilical vein endothelial (HUVEC) cells [82] and TRPM8 activation leads to inhibition of the GTPase Rap1 and impaired ß1 integrin-dependent adhesion and migration of endothelial cell line (HMECs) [92].
Once tumor cells are adherent to endothelial cells they will eventually breach the endothelial barrier and invade the underlying tissue. It is well known that cadherin-mediated cell-cell adhesion of endothelial cells is Ca2+-dependent [198]. The cadherin-mediated barrier integrity also depends on intracellular Ca2+ signaling that in turn is regulated, among others, by TRPV4 channels as shown for retinal endothelial cells [199] or for pulmonary vessels [12,200]. Endothelial TRPV4 channels cooperate with KCa3.1 channels in the regulation of the endothelial barrier integrity [201]. The barrier integrity can also be modulated by endothelial TRPM2 channels. When they are activated by oxidants generated by neutrophil granulocytes, endothelial cell junctions open and facilitate transmigration of neutrophils [202]. It remains to be seen whether such a mechanism also applies for tumor cell extravasation. Moreover, endothelial TRPC6 [203] and K2P2.1 channels [204] control the transendothelial migration of leukocytes. To the best of our knowledge, a role of TRP channels in transendothelial migration of tumor cells has not been directly shown. Our study showing that inhibition of endothelial KCa3.1 channels also impairs lung cancer cell transmigration [17] may serve as a further proof-of-principle for the role of ion channels in this process.
6. Pharmacologic Targeting of TRP Channels in Cancer
This review emphasizes the therapeutic potential of targeting TRP channels in cancer. TRP channels can already be used as prognostic and predictive clinical markers because TRP channel expression strongly correlates with patient survival (e.g., [205,206,207,208,209]). The pharmacological targeting of TRP channels offers the advantage that tumor, stroma and immune cells can be targeted simultaneously with potentially only one drug. For example, TRPC6 channels are expressed in hepatocellular carcinoma cells [210], in hepatic stellate cells [127], endothelial cells [203] and in neutrophil granulocytes [79]. Moreover, their inhibition is at least partially effective in tumors that are resistantt to chemotherapy [210]. Thus, TRP channel blockade may not only interrupt the mutual activation of tumor and stroma cells. When combined with conventional chemotherapeutics it also offers the opportunity to reduce their dosage and thereby lessen the severity of side effects. The challenge will be to selectively target TRP channel modulators to the tumor in order to avoid systemic side effects. We refer to the review by Gautier and colleagues for an overview of the pharmacological approach of targeting TRP channels in cancer [211].
Some approaches use the fact that TRP channels are upregulated in tumorigenic cells, so that targeted TRP channel activation leads to Ca2+ and Na+ influx, disruption of the ionic homeostasis and subsequent cell death. For the TRPM8 activator D3263, a clinical Phase 1 dose escalation study (NCT00839631) led to disease stabilization in prostate cancer patients. Another TRPM8 activator, WS-12, may be used as a diagnostic marker for prostate cancer by incorporating radiohalogens [212,213]. Another example is the Phase 1 trial of SOR-C13 (NCT01578564), a TRPV6 inhibitor. TRPV6 inhibition aims to suppress Ca2+-mediated cancer proliferation and metastasis e.g., in SCLC, prostate or pancreas cancer [66,214,215].
For ion channel inhibitors, the possible target is typically located in plasma membrane. The drug must only diffuse through the capillaries and the tissue to reach its target. Disease- and drug-derived factors (e.g., interstitial pH) significantly contribute to the differential distribution in the tissues. Therefore, relying solely on total drug concentration has the potential to introduce significant errors into the interpretation of drug delivery mechanisms. To assess the pharmacokinetic properties of potential drugs, it is crucial to also assess the free, unbound drug concentration, which refers to compounds that are for example not bound to plasma proteins [216]. In case of TRP channel inhibitors, it is still necessary to assess the amount of unbound drug concentration in the vicinity of the migrating cancer cells.
However, most of the cancer-associated TRP channels are far away from being targeted in clinical trials and developing suitable TRP channel modulators in combination with cancer-specific applications is urgently needed.
7. Conclusions and Open Questions
Recapitulating our knowledge on TRP channel regulation and function, it becomes obvious, that they play an important role in the dissemination of cancer cells and in disease progression (see Figure 1). In our view their contribution to cancer progression can be attributed at least in part to the fact that they are multimodal sensors and transducers/effectors of microenvironmental cues encountered by cancer cells during the metastatic cascade. They respond to many of the chemico-physical stimuli that are relevant for the metastatic spread of cancer cells. In light of the prognostic relevance of metastases, it is not surprising that there are strong correlations between TRP channel expression in tumors and the overall survival of the diseased patients. This review also shows that TRP channel functions in metastasis and cancer in general are still far from being fully understood. Many studies do not provide a detailed look on the mechanistic steps and signaling cascades regulated by TRP channels. Moreover, there is an almost complete lack of knowledge concerning the role of TRP channels in the processes of intra- and extravasation. It is equally unknown whether they play a role in circulating tumor cells. Circulating tumor cells are exposed to a massive mechanical stress so that one can expect a strong activation of mechanosensitive TRP and PIEZO channels potentially leading to a Ca2+ overload. While the overexpression of many TRP channels involved in mechano-signaling promotes aggressive tumor cell behavior, this may not be the case for the “success” of circulating tumor cells.
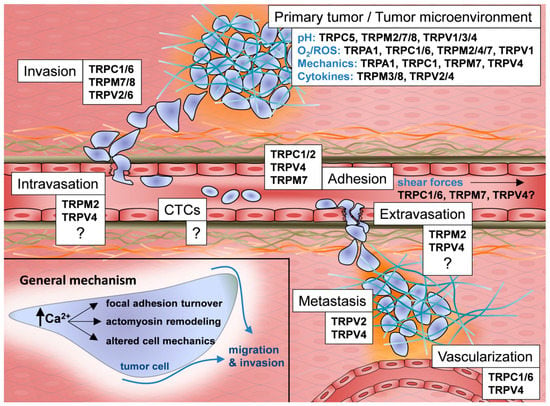
Figure 1.
TRP channels in the metastatic cascade.
During the metastatic cascade, cancer cells have to respond to various chemico-physical stimuli such as changes in pH, hypoxia, ROS, mechanical cues and growth factor and cytokine gradients. Cancer cells use TRP channels to sense, modify and regulate these stimuli during the different steps of the metastatic cascade/during tumor progression. This figure highlights important TRP channels within the metastatic cascade. Open questions are stressed with question marks.
There are clearly two major quests for the field of TRP channels in cancer. One is to delineate in more detail the contribution of TRP channels to the metastatic cascade. A molecular understanding of the role of TRP channels therein is a prerequisite for developing new (TRP channel-targeting) therapeutic concepts. Novel microfluidic techniques as well as biophysical techniques such as atomic force microscopy will be valuable approaches for deciphering the role of TRP channels in intra- and extravasation of tumor cells and also in circulating tumor cells. The second challenge is to continue the development of new and specific TRP channel modulators so that the therapeutic potential of aberrant TRP channel function in the metastatic cascade can be evaluated pharmacologically and eventually be translated clinically. In our view, the responsiveness of TRP channels to cues from the tumor microenvironment makes them very attractive targets. Their attractiveness is reinforced by the fact that they allow simultaneous targeting of both tumor and stromal cells. Moreover, there is growing evidence that TRP channel modulation constitutes a new approach to overcome resistance to “conventional” cancer therapeutics (e.g., [210,217]). Thereby, the vicious cycle of mutual activation of tumor and stromal cells can potentially be interrupted.
Acknowledgement
The authors wish to thank past and present members of their laboratory whose enthusiastic work contributed largely to developing the concepts described in this review. A.S. acknowledges support from the Deutsche Forschungsgemeinschaft (DFG; SCHW 407/17-1), Cells-in-Motion Cluster of Excellence (EXC 1003-CiM), University of Münster, Germany and IZKF Münster (Schw2/020/18). B.F. received support from Cells-in-Motion Cluster of Excellence (EXC 1003-CiM; PP 2016-12).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Riggi, N.; Aguet, M.; Stamenkovic, I. Cancer Metastasis: A Reappraisal of Its Underlying Mechanisms and Their Relevance to Treatment. Annu. Rev. Pathol. 2018, 13, 117–140. [Google Scholar] [CrossRef] [PubMed]
- Carrato, A.; Falcone, A.; Ducreux, M.; Valle, J.W.; Parnaby, A.; Djazouli, K.; Alnwick-Allu, K.; Hutchings, A.; Palaska, C.; Parthenaki, I. A Systematic Review of the Burden of Pancreatic Cancer in Europe: Real-World Impact on Survival, Quality of Life and Costs. J. Gastrointest. Cancer 2015, 46, 201–211. [Google Scholar] [CrossRef] [PubMed]
- De Angelis, R.; Sant, M.; Coleman, M.P.; Francisci, S.; Baili, P.; Pierannunzio, D.; Trama, A.; Visser, O.; Brenner, H.; Ardanaz, E.; et al. EUROCARE-5 Working Group Cancer survival in Europe 1999–2007 by country and age: Results of EUROCARE--5-a population-based study. Lancet Oncol. 2014, 15, 23–34. [Google Scholar] [CrossRef]
- Hanahan, D.; Weinberg, R.A. Hallmarks of cancer: The next generation. Cell 2011, 144, 646–674. [Google Scholar] [CrossRef] [PubMed]
- Djamgoz, M.B.A.; Coombes, R.C.; Schwab, A. Ion transport and cancer: From initiation to metastasis. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2014, 369, 20130092. [Google Scholar] [CrossRef] [PubMed]
- Andersen, A.P.; Moreira, J.M.A.; Pedersen, S.F. Interactions of ion transporters and channels with cancer cell metabolism and the tumour microenvironment. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369. [Google Scholar] [CrossRef] [PubMed]
- Schwab, A.; Stock, C. Ion channels and transporters in tumour cell migration and invasion. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2014, 369, 20130102. [Google Scholar] [CrossRef] [PubMed]
- Urrego, D.; Tomczak, A.P.; Zahed, F.; Stühmer, W.; Pardo, L.A. Potassium channels in cell cycle and cell proliferation. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369. [Google Scholar] [CrossRef] [PubMed]
- Wanitchakool, P.; Wolf, L.; Koehl, G.E.; Sirianant, L.; Schreiber, R.; Kulkarni, S.; Duvvuri, U.; Kunzelmann, K. Role of anoctamins in cancer and apoptosis. Philos. Trans. R. Soc. Lond. B. Biol. Sci. 2014, 369, 20130096. [Google Scholar] [CrossRef] [PubMed]
- Bernardini, M.; Fiorio Pla, A.; Prevarskaya, N.; Gkika, D. Human transient receptor potential (TRP) channel expression profiling in carcinogenesis. Int. J. Dev. Biol. 2015, 59, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Prevarskaya, N.; Skryma, R.; Shuba, Y. Ion Channels in Cancer: Are Cancer Hallmarks Oncochannelopathies? Physiol. Rev. 2018, 98, 559–621. [Google Scholar] [CrossRef] [PubMed]
- Micalizzi, D.S.; Maheswaran, S.; Haber, D.A. A conduit to metastasis: Circulating tumor cell biology. Genes Dev. 2017, 31, 1827–1840. [Google Scholar] [CrossRef] [PubMed]
- Franco, A.T.; Corken, A.; Ware, J. Platelets at the interface of thrombosis, inflammation, and cancer. Blood 2015, 126, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Velez, J.; Enciso, L.J.; Suarez, M.; Fiegl, M.; Grismaldo, A.; López, C.; Barreto, A.; Cardozo, C.; Palacios, P.; Morales, L.; et al. Platelets promote mitochondrial uncoupling and resistance to apoptosis in leukemia cells: A novel paradigm for the bone marrow microenvironment. Cancer Microenviron. 2014, 7, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Reymond, N.; d’Água, B.B.; Ridley, A.J. Crossing the endothelial barrier during metastasis. Nat. Rev. Cancer 2013, 13, 858–870. [Google Scholar] [CrossRef] [PubMed]
- Pick, R.; Brechtefeld, D.; Walzog, B. Intraluminal crawling versus interstitial neutrophil migration during inflammation. Mol. Immunol. 2013, 55, 70–75. [Google Scholar] [CrossRef] [PubMed]
- Bulk, E.; Kramko, N.; Liashkovich, I.; Glaser, F.; Schillers, H.; Schnittler, H.-J.; Oberleithner, H.; Schwab, A. KCa3.1 channel inhibition leads to an ICAM-1 dependent increase of cell-cell adhesion between A549 lung cancer and HMEC-1 endothelial cells. Oncotarget 2017, 8, 112268–112282. [Google Scholar] [CrossRef] [PubMed]
- Soto, M.S.; O’Brien, E.R.; Andreou, K.; Scrace, S.F.; Zakaria, R.; Jenkinson, M.D.; O’Neill, E.; Sibson, N.R. Disruption of tumour-host communication by downregulation of LFA-1 reduces COX-2 and e-NOS expression and inhibits brain metastasis growth. Oncotarget 2016, 7, 52375–52391. [Google Scholar] [CrossRef] [PubMed]
- Nilius, B.; Szallasi, A. Transient receptor potential channels as drug targets: From the science of basic research to the art of medicine. Pharmacol. Rev. 2014, 66, 676–814. [Google Scholar] [CrossRef] [PubMed]
- Szolcsányi, J.; Sándor, Z. Multisteric TRPV1 nocisensor: A target for analgesics. Trends Pharmacol. Sci. 2012, 33, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Khalil, M.; Alliger, K.; Weidinger, C.; Yerinde, C.; Wirtz, S.; Becker, C.; Engel, M.A. Functional Role of Transient Receptor Potential Channels in Immune Cells and Epithelia. Front. Immunol. 2018, 9, 174. [Google Scholar] [CrossRef] [PubMed]
- van Goor, M.K.C.; Hoenderop, J.G.J.; van der Wijst, J. TRP channels in calcium homeostasis: From hormonal control to structure-function relationship of TRPV5 and TRPV6. Biochim. Biophys. Acta 2017, 1864, 883–893. [Google Scholar] [CrossRef] [PubMed]
- Najder, K.; Musset, B.; Lindemann, O.; Bulk, E.; Schwab, A.; Fels, B. The function of TRP channels in neutrophil granulocytes. Pflüg. Arch. 2018. [Google Scholar] [CrossRef] [PubMed]
- Vrenken, K.S.; Jalink, K.; van Leeuwen, F.N.; Middelbeek, J. Beyond ion-conduction: Channel-dependent and -independent roles of TRP channels during development and tissue homeostasis. Biochim. Biophys. Acta 2016, 1863, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Azimi, I.; Milevskiy, M.J.G.; Kaemmerer, E.; Turner, D.; Yapa, K.T.D.S.; Brown, M.A.; Thompson, E.W.; Roberts-Thomson, S.J.; Monteith, G.R. TRPC1 is a differential regulator of hypoxia-mediated events and Akt signalling in PTEN-deficient breast cancer cells. J. Cell Sci. 2017, 130, 2292–2305. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.H.; Choong, L.Y.; Jin, T.H.; Mon, N.N.; Chong, S.; Liew, C.S.; Putti, T.; Lu, S.Y.; Harteneck, C.; Lim, Y.P. TRPV4 plays a role in breast cancer cell migration via Ca2+-dependent activation of AKT and downregulation of E-cadherin cell cortex protein. Oncogenesis 2017, 6, e338. [Google Scholar] [CrossRef] [PubMed]
- Sumoza-Toledo, A.; Espinoza-Gabriel, M.I.; Montiel-Condado, D. Evaluation of the TRPM2 channel as a biomarker in breast cancer using public databases analysis. Bol. Méd. Hosp. Infant. México 2016, 73, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Rybarczyk, P.; Vanlaeys, A.; Brassart, B.; Dhennin-Duthille, I.; Chatelain, D.; Sevestre, H.; Ouadid-Ahidouch, H.; Gautier, M. The Transient Receptor Potential Melastatin 7 Channel Regulates Pancreatic Cancer Cell Invasion through the Hsp90α/uPA/MMP2 pathway. Neoplasia 2017, 19, 288–300. [Google Scholar] [CrossRef] [PubMed]
- Xiao, N.; Jiang, L.M.; Ge, B.; Zhang, T.Y.; Zhao, X.K.; Zhou, X. Over-expression of TRPM8 is associated with poor prognosis in urothelial carcinoma of bladder. Tumour Biol. 2014, 35, 11499–11504. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Xu, H. High expression of TRPM8 predicts poor prognosis in patients with osteosarcoma. Oncol. Lett. 2016, 12, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- Elbaz, M.; Ahirwar, D.; Xiaoli, Z.; Zhou, X.; Lustberg, M.; Nasser, M.W.; Shilo, K.; Ganju, R.K. TRPV2 is a novel biomarker and therapeutic target in triple negative breast cancer. Oncotarget 2016, 5. [Google Scholar] [CrossRef]
- Zhou, K.; Zhang, S.-S.; Yan, Y.; Zhao, S. Overexpression of transient receptor potential vanilloid 2 is associated with poor prognosis in patients with esophageal squamous cell carcinoma. Med. Oncol. 2014, 31, 17. [Google Scholar] [CrossRef] [PubMed]
- Du, G.-J.; Li, J.-H.; Liu, W.-J.; Liu, Y.-H.; Zhao, B.; Li, H.-R.; Hou, X.-D.; Li, H.; Qi, X.-X.; Duan, Y.-J. The combination of TRPM8 and TRPA1 expression causes an invasive phenotype in lung cancer. Tumour Biol. 2014, 35, 1251–1261. [Google Scholar] [CrossRef] [PubMed]
- Schaar, A.; Sukumaran, P.; Sun, Y.; Dhasarathy, A.; Singh, B.B. TRPC1-STIM1 activation modulates transforming growth factor β-induced epithelial-to-mesenchymal transition. Oncotarget 2016, 7, 80554–80567. [Google Scholar] [CrossRef] [PubMed]
- Faouzi, M.; Hague, F.; Geerts, D.; Ay, A.-S.; Potier-Cartereau, M.; Ahidouch, A.; Ouadid-Ahidouch, H. Functional cooperation between KCa3.1 and TRPC1 channels in human breast cancer: Role in cell proliferation and patient prognosis. Oncotarget 2016, 7, 36419–36435. [Google Scholar] [CrossRef] [PubMed]
- Dong, H.; Shim, K.-N.; Li, J.M.J.; Estrema, C.; Ornelas, T.A.; Nguyen, F.; Liu, S.; Ramamoorthy, S.L.; Ho, S.; Carethers, J.M.; et al. Molecular mechanisms underlying Ca2+-mediated motility of human pancreatic duct cells. Am. J. Physiol. Cell Physiol. 2010, 299, C1493–1503. [Google Scholar] [CrossRef] [PubMed]
- Tajeddine, N.; Gailly, P. TRPC1 protein channel is major regulator of epidermal growth factor receptor signaling. J. Biol. Chem. 2012, 287, 16146–16157. [Google Scholar] [CrossRef] [PubMed]
- He, B.; Liu, F.; Ruan, J.; Li, A.; Chen, J.; Li, R.; Shen, J.; Zheng, D.; Luo, R. Silencing TRPC1 expression inhibits invasion of CNE2 nasopharyngeal tumor cells. Oncol. Rep. 2012, 27, 1548–1554. [Google Scholar] [CrossRef] [PubMed]
- Lepannetier, S.; Zanou, N.; Yerna, X.; Emeriau, N.; Dufour, I.; Masquelier, J.; Muccioli, G.; Tajeddine, N.; Gailly, P. Sphingosine-1-phosphate-activated TRPC1 channel controls chemotaxis of glioblastoma cells. Cell Calcium 2016, 60, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Asghar, M.Y.; Magnusson, M.; Kemppainen, K.; Sukumaran, P.; Löf, C.; Pulli, I.; Kalhori, V.; Törnquist, K. Transient Receptor Potential Canonical 1 (TRPC1) Channels as Regulators of Sphingolipid and VEGF Receptor Expression: Implications for thyroid cancer cell migration and proliferation. J. Biol. Chem. 2015, 290, 16116–16131. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.-C.; Huang, W.-C.; Lin, Y.-P.; Becker, E.B.E.; Ansorge, O.; Flockerzi, V.; Conti, D.; Cenacchi, G.; Glitsch, M.D. Functional expression of calcium-permeable canonical transient receptor potential 4-containing channels promotes migration of medulloblastoma cells. J. Physiol. 2017, 595, 5525–5544. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Zhu, Y.; Dong, Y.; Zhang, P.; Han, X.; Jin, J.; Ma, X. Overexpression of TrpC5 promotes tumor metastasis via the HIF-1α-Twist signaling pathway in colon cancer. Clin. Sci. Lond. Engl. 1979 2017, 131, 2439–2450. [Google Scholar] [CrossRef] [PubMed]
- Chigurupati, S.; Venkataraman, R.; Barrera, D.; Naganathan, A.; Madan, M.; Paul, L.; Pattisapu, J.V.; Kyriazis, G.A.; Sugaya, K.; Bushnev, S.; et al. Receptor channel TRPC6 is a key mediator of Notch-driven glioblastoma growth and invasiveness. Cancer Res. 2010, 70, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.-L.; Liu, B.-C.; Lu, X.-Y.; Yan, Y.; Zhai, Y.-J.; Bao, Q.; Doetsch, P.W.; Deng, X.; Thai, T.L.; Alli, A.A.; et al. Inhibition of TRPC6 reduces non-small cell lung cancer cell proliferation and invasion. Oncotarget 2017, 8, 5123–5134. [Google Scholar] [CrossRef] [PubMed]
- Yue, D.; Wang, Y.; Xiao, J.-Y.; Wang, P.; Ren, C.-S. Expression of TRPC6 in benign and malignant human prostate tissues. Asian J. Androl. 2009, 11, 541–547. [Google Scholar] [CrossRef] [PubMed]
- El Boustany, C.; Bidaux, G.; Enfissi, A.; Delcourt, P.; Prevarskaya, N.; Capiod, T. Capacitative calcium entry and transient receptor potential canonical 6 expression control human hepatoma cell proliferation. Hepatology 2008, 47, 2068–2077. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Kazi, A.A.; Li, Q.; Yang, Z.; Berg, A.; Yee, R.K. Aberrant over-expression of TRPM7 ion channels in pancreatic cancer: Required for cancer cell invasion and implicated in tumor growth and metastasis. Biol. Open 2015, 4, 507–514. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Chen, X.; Du, X.; Guan, B.; Liu, Y.; Zhang, H. EGF enhances the migration of cancer cells by up-regulation of TRPM7. Cell Calcium 2011, 50, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Middelbeek, J.; Kuipers, A.J.; Henneman, L.; Visser, D.; Eidhof, I.; van Horssen, R.; Wieringa, B.; Canisius, S.V.; Zwart, W.; Wessels, L.F.; et al. TRPM7 is required for breast tumor cell metastasis. Cancer Res. 2012, 72, 4250–4261. [Google Scholar] [CrossRef] [PubMed]
- Guilbert, A.; Gautier, M.; Dhennin-Duthille, I.; Rybarczyk, P.; Sahni, J.; Sevestre, H.; Scharenberg, A.M.; Ouadid-Ahidouch, H. Transient receptor potential melastatin 7 is involved in oestrogen receptor-negative metastatic breast cancer cells migration through its kinase domain. Eur. J. Cancer 2013, 49, 3694–3707. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Cai, C.; Wu, J.; Cai, S.; Ye, C.; Chen, H.; Yang, Z.; Zeng, H.; Shen, Q.; Zou, F. TRPM7 mediates breast cancer cell migration and invasion through the MAPK pathway. Cancer Lett. 2013, 333, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.M.; Azimi, I.; Faville, R.A.; Peters, A.A.; Jalink, K.; Putney, J.W.; Goodhill, G.J.; Thompson, E.W.; Roberts-Thomson, S.J.; Monteith, G.R. Induction of epithelial-mesenchymal transition (EMT) in breast cancer cells is calcium signal dependent. Oncogene 2014, 33, 2307–2316. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.-P.; Luan, Y.; You, C.-X.; Chen, X.-H.; Luo, R.-C.; Li, R. TRPM7 regulates the migration of human nasopharyngeal carcinoma cell by mediating Ca2+ influx. Cell Calcium 2010, 47, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Liao, Q.-J.; Zhang, Y.; Zhou, H.; Luo, C.-H.; Tang, J.; Wang, Y.; Tang, Y.; Zhao, M.; Zhao, X.-H.; et al. TRPM7 is required for ovarian cancer cell growth, migration and invasion. Biochem. Biophys. Res. Commun. 2014, 454, 547–553. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, Y.; Ohkubo, T.; Ikebe, T.; Yamazaki, J. Blockade of TRPM8 activity reduces the invasion potential of oral squamous carcinoma cell lines. Int. J. Oncol. 2012, 40, 1431–1440. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Chen, Y.; Shuai, S.; Ding, D.; Li, R.; Luo, R. TRPM8 promotes aggressiveness of breast cancer cells by regulating EMT via activating AKT/GSK-3β pathway. Tumour Biol. 2014, 35, 8969–8977. [Google Scholar] [CrossRef] [PubMed]
- Klumpp, D.; Frank, S.C.; Klumpp, L.; Sezgin, E.C.; Eckert, M.; Edalat, L.; Bastmeyer, M.; Zips, D.; Ruth, P.; Huber, S.M. TRPM8 is required for survival and radioresistance of glioblastoma cells. Oncotarget 2017, 8, 95896–95913. [Google Scholar] [CrossRef] [PubMed]
- Cucu, D.; Chiritoiu, G.; Petrescu, S.; Babes, A.; Stanica, L.; Duda, D.G.; Horii, A.; Dima, S.O.; Popescu, I. Characterization of functional transient receptor potential melastatin 8 channels in human pancreatic ductal adenocarcinoma cells. Pancreas 2014, 43, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.-H.; Wang, X.-H.; Wang, H.-P.; Hu, L.-Q. Effects of TRPM8 on the proliferation and motility of prostate cancer PC-3 cells. Asian J. Androl. 2009, 11, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Bidaux, G.; Borowiec, A.-S.; Dubois, C.; Delcourt, P.; Schulz, C.; Vanden Abeele, F.; Lepage, G.; Desruelles, E.; Bokhobza, A.; Dewailly, E.; et al. Targeting of short TRPM8 isoforms induces 4TM-TRPM8-dependent apoptosis in prostate cancer cells. Oncotarget 2016, 7, 29063–29080. [Google Scholar] [CrossRef] [PubMed]
- Monet, M.; Lehen’kyi, V. ’yacheslav; Gackiere, F.; Firlej, V.; Vandenberghe, M.; Roudbaraki, M.; Gkika, D.; Pourtier, A.; Bidaux, G.; Slomianny, C.; Delcourt, P.; et al. Role of cationic channel TRPV2 in promoting prostate cancer migration and progression to androgen resistance. Cancer Res. 2010, 70, 1225–1235. [Google Scholar] [CrossRef] [PubMed]
- Gambade, A.; Zreika, S.; Guéguinou, M.; Chourpa, I.; Fromont, G.; Bouchet, A.M.; Burlaud-Gaillard, J.; Potier-Cartereau, M.; Roger, S.; Aucagne, V.; et al. Activation of TRPV2 and BKCa channels by the LL-37 enantiomers stimulates calcium entry and migration of cancer cells. Oncotarget 2016, 7, 23785–23800. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.H.; Choong, L.Y.; Mon, N.N.; Lu, S.; Lin, Q.; Pang, B.; Yan, B.; Krishna, V.S.R.; Singh, H.; Tan, T.Z.; et al. TRPV4 Regulates Breast Cancer Cell Extravasation, Stiffness and Actin Cortex. Sci. Rep. 2016, 6, 27903. [Google Scholar] [CrossRef] [PubMed]
- Xie, R.; Xu, J.; Xiao, Y.; Wu, J.; Wan, H.; Tang, B.; Liu, J.; Fan, Y.; Wang, S.; Wu, Y.; et al. Calcium Promotes Human Gastric Cancer via a Novel Coupling of Calcium-Sensing Receptor and TRPV4 Channel. Cancer Res. 2017, 77, 6499–6512. [Google Scholar] [CrossRef] [PubMed]
- Dhennin-Duthille, I.; Gautier, M.; Faouzi, M.; Guilbert, A.; Brevet, M.; Vaudry, D.; Ahidouch, A.; Sevestre, H.; Ouadid-Ahidouch, H. High expression of transient receptor potential channels in human breast cancer epithelial cells and tissues: Correlation with pathological parameters. Cell. Physiol. Biochem. 2011, 28, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Dong, M.; Zhou, J.; Sheng, W.; Li, X.; Gao, W. Expression and prognostic significance of TRPV6 in the development and progression of pancreatic cancer. Oncol. Rep. 2018, 39, 1432–1440. [Google Scholar] [CrossRef] [PubMed]
- Rae, J.M.; Creighton, C.J.; Meck, J.M.; Haddad, B.R.; Johnson, M.D. MDA-MB-435 cells are derived from M14 Melanoma cells––a loss for breast cancer, but a boon for melanoma research. Breast Cancer Res. Treat. 2007, 104, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.-S.; Wen, J.; Yang, F.; Cai, X.-L.; Yang, H.; Luo, K.-J.; Liu, Q.W.; Hu, R.-G.; Xie, X.; Huang, Q.-Y.; et al. High expression of transient potential receptor C6 correlated with poor prognosis in patients with esophageal squamous cell carcinoma. Med. Oncol. 2013, 30, 607. [Google Scholar] [CrossRef] [PubMed]
- Rybarczyk, P.; Gautier, M.; Hague, F.; Dhennin-Duthille, I.; Chatelain, D.; Kerr-Conte, J.; Pattou, F.; Regimbeau, J.-M.; Sevestre, H.; Ouadid-Ahidouch, H. Transient receptor potential melastatin-related 7 channel is overexpressed in human pancreatic ductal adenocarcinomas and regulates human pancreatic cancer cell migration. Int. J. Cancer 2012, 131, E851–E861. [Google Scholar] [CrossRef] [PubMed]
- Fife, C.M.; McCarroll, J.A.; Kavallaris, M. Movers and shakers: Cell cytoskeleton in cancer metastasis. Br. J. Pharmacol. 2014, 171, 5507–5523. [Google Scholar] [CrossRef] [PubMed]
- Friedl, P.; Mayor, R. Tuning Collective Cell Migration by Cell-Cell Junction Regulation. Cold Spring Harb. Perspect. Biol. 2017, 9. [Google Scholar] [CrossRef] [PubMed]
- Schwab, A.; Fabian, A.; Hanley, P.J.; Stock, C. Role of ion channels and transporters in cell migration. Physiol. Rev. 2012, 92, 1865–1913. [Google Scholar] [CrossRef] [PubMed]
- Betapudi, V.; Rai, V.; Beach, J.R.; Egelhoff, T. Novel regulation and dynamics of myosin II activation during epidermal wound responses. Exp. Cell Res. 2010, 316, 980–991. [Google Scholar] [CrossRef] [PubMed]
- Giannone, G.; Rondé, P.; Gaire, M.; Beaudouin, J.; Haiech, J.; Ellenberg, J.; Takeda, K. Calcium rises locally trigger focal adhesion disassembly and enhance residency of focal adhesion kinase at focal adhesions. J. Biol. Chem. 2004, 279, 28715–28723. [Google Scholar] [CrossRef] [PubMed]
- Iamshanova, O.; Fiorio Pla, A.; Prevarskaya, N. Molecular mechanisms of tumour invasion: Regulation by calcium signals. J. Physiol. 2017, 595, 3063–3075. [Google Scholar] [CrossRef] [PubMed]
- Stock, C.; Ludwig, F.T.; Hanley, P.J.; Schwab, A. Roles of ion transport in control of cell motility. Compr. Physiol. 2013, 3, 59–119. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Brackenbury, W.J. Membrane potential and cancer progression. Front. Physiol. 2013, 4. [Google Scholar] [CrossRef] [PubMed]
- Kronlage, M.; Song, J.; Sorokin, L.; Isfort, K.; Schwerdtle, T.; Leipziger, J.; Robaye, B.; Conley, P.B.; Kim, H.-C.; Sargin, S.; et al. Autocrine Purinergic Receptor Signaling Is Essential for Macrophage Chemotaxis. Sci. Signal 2010, 3, ra55. [Google Scholar] [CrossRef] [PubMed]
- Lindemann, O.; Umlauf, D.; Frank, S.; Schimmelpfennig, S.; Bertrand, J.; Pap, T.; Hanley, P.J.; Fabian, A.; Dietrich, A.; Schwab, A. TRPC6 regulates CXCR2-mediated chemotaxis of murine neutrophils. J. Immunol. 2013, 190, 5496–5505. [Google Scholar] [CrossRef] [PubMed]
- Schilling, T.; Miralles, F.; Eder, C. TRPM7 regulates proliferation and polarisation of macrophages. J. Cell Sci. 2014, 127, 4561–4566. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.; Langeslag, M.; van Leeuwen, B.; Ran, L.; Ryazanov, A.G.; Figdor, C.G.; Moolenaar, W.H.; Jalink, K.; van Leeuwen, F.N. TRPM7, a novel regulator of actomyosin contractility and cell adhesion. EMBO J. 2006, 25, 290–301. [Google Scholar] [CrossRef] [PubMed]
- Nishitani, W.S.; Alencar, A.M.; Wang, Y. Rapid and Localized Mechanical Stimulation and Adhesion Assay: TRPM7 Involvement in Calcium Signaling and Cell Adhesion. PLoS ONE 2015, 10, e0126440. [Google Scholar] [CrossRef]
- Gao, S.-L.; Kong, C.-Z.; Zhang, Z.; Li, Z.-L.; Bi, J.-B.; Liu, X.-K. TRPM7 is overexpressed in bladder cancer and promotes proliferation, migration, invasion and tumor growth. Oncol. Rep. 2017, 38, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Chubanov, V.; Mittermeier, L.; Gudermann, T. Role of kinase-coupled TRP channels in mineral homeostasis. Pharmacol. Ther. 2018, 184, 159–176. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Chan, A.S.; Yee, J.D.; Yee, R.K. TRPM7 and TRPM8 Ion Channels in Pancreatic Adenocarcinoma: Potential Roles as Cancer Biomarkers and Targets. Scientifica 2012, 2012, 415158. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.; Middelbeek, J.; Lasonder, E.; Dulyaninova, N.G.; Morrice, N.A.; Ryazanov, A.G.; Bresnick, A.R.; Figdor, C.G.; van Leeuwen, F.N. TRPM7 regulates myosin IIA filament stability and protein localization by heavy chain phosphorylation. J. Mol. Biol. 2008, 378, 790–803. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Li, M.-H.; Inoue, K.; Chu, X.-P.; Seeds, J.; Xiong, Z.-G. Transient Receptor Potential Melastatin 7–like Current in Human Head and Neck Carcinoma Cells: Role in Cell Proliferation. Cancer Res. 2007, 67, 10929–10938. [Google Scholar] [CrossRef] [PubMed]
- Yee, N.S.; Zhou, W.; Liang, I.-C. Transient receptor potential ion channel Trpm7 regulates exocrine pancreatic epithelial proliferation by Mg2+-sensitive Socs3a signaling in development and cancer. Dis. Model. Mech. 2011, 4, 240–254. [Google Scholar] [CrossRef] [PubMed]
- Gkika, D.; Flourakis, M.; Lemonnier, L.; Prevarskaya, N. PSA reduces prostate cancer cell motility by stimulating TRPM8 activity and plasma membrane expression. Oncogene 2010, 29, 4611–4616. [Google Scholar] [CrossRef] [PubMed]
- Gkika, D.; Lemonnier, L.; Shapovalov, G.; Gordienko, D.; Poux, C.; Bernardini, M.; Bokhobza, A.; Bidaux, G.; Degerny, C.; Verreman, K.; et al. TRP channel-associated factors are a novel protein family that regulates TRPM8 trafficking and activity. J. Cell Biol. 2015, 208, 89–107. [Google Scholar] [CrossRef] [PubMed]
- Ulăreanu, R.; Chiriţoiu, G.; Cojocaru, F.; Deftu, A.; Ristoiu, V.; Stănică, L.; Mihăilescu, D.F.; Cucu, D. N-glycosylation of the transient receptor potential melastatin 8 channel is altered in pancreatic cancer cells. Tumour Biol. 2017, 39. [Google Scholar] [CrossRef] [PubMed]
- Genova, T.; Grolez, G.P.; Camillo, C.; Bernardini, M.; Bokhobza, A.; Richard, E.; Scianna, M.; Lemonnier, L.; Valdembri, D.; Munaron, L.; et al. TRPM8 inhibits endothelial cell migration via a non-channel function by trapping the small GTPase Rap1. J. Cell Biol. 2017, 216, 2107–2130. [Google Scholar] [CrossRef] [PubMed]
- Santoni, G.; Farfariello, V.; Amantini, C. TRPV channels in tumor growth and progression. Adv. Exp. Med. Biol. 2011, 704, 947–967. [Google Scholar] [CrossRef] [PubMed]
- Oulidi, A.; Bokhobza, A.; Gkika, D.; Vanden Abeele, F.; Lehen’kyi, V.; Ouafik, L.H.; Mauroy, B.; Prevarskaya, N. TRPV2 mediates adrenomedullin stimulation of prostate and urothelial cancer cell adhesion, migration and invasion. PLoS ONE 2013, 8, e64885. [Google Scholar] [CrossRef] [PubMed]
- Moccia, F. Endothelial Ca2+ Signaling and the Resistance to Anticancer Treatments: Partners in Crime. Int. J. Mol. Sci. 2018, 19, 217. [Google Scholar] [CrossRef] [PubMed]
- Bomben, V.C.; Turner, K.L.; Barclay, T.-T.C.; Sontheimer, H. Transient receptor potential canonical channels are essential for chemotactic migration of human malignant gliomas. J. Cell. Physiol. 2011, 226, 1879–1888. [Google Scholar] [CrossRef] [PubMed]
- Cuddapah, V.A.; Turner, K.L.; Sontheimer, H. Calcium entry via TRPC1 channels activates chloride currents in human glioma cells. Cell Calcium 2013, 53, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Guéguinou, M.; Harnois, T.; Crottes, D.; Uguen, A.; Deliot, N.; Gambade, A.; Chantôme, A.; Haelters, J.P.; Jaffrès, P.A.; Jourdan, M.L.; et al. SK3/TRPC1/Orai1 complex regulates SOCE-dependent colon cancer cell migration: A novel opportunity to modulate anti-EGFR mAb action by the alkyl-lipid Ohmline. Oncotarget 2016, 7, 36168–36184. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Li, X.; Liu, J.; Li, J.; Li, L.-J.; Qiu, M.-X. Effects of TRPC6 on invasibility of low-differentiated prostate cancer cells. Asian Pac. J. Trop. Med. 2014, 7, 44–47. [Google Scholar] [CrossRef]
- Gkika, D.; Prevarskaya, N. TRP channels in prostate cancer: The good, the bad and the ugly? Asian J. Androl. 2011, 13, 673–676. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Shim, M.K.; Jin, M.; Rhyu, M.-R.; Lee, Y. Methyl syringate, a TRPA1 agonist represses hypoxia-induced cyclooxygenase-2 in lung cancer cells. Phytomedicine 2016, 23, 324–329. [Google Scholar] [CrossRef] [PubMed]
- Morelli, M.B.; Nabissi, M.; Amantini, C.; Tomassoni, D.; Rossi, F.; Cardinali, C.; Santoni, M.; Arcella, A.; Oliva, M.A.; Santoni, A.; et al. Overexpression of transient receptor potential mucolipin-2 ion channels in gliomas: Role in tumor growth and progression. Oncotarget 2016, 7, 43654–43668. [Google Scholar] [CrossRef] [PubMed]
- Estrella, V.; Chen, T.; Lloyd, M.; Wojtkowiak, J.; Cornnell, H.H.; Ibrahim-Hashim, A.; Bailey, K.; Balagurunathan, Y.; Rothberg, J.M.; Sloane, B.F.; et al. Acidity generated by the tumor microenvironment drives local invasion. Cancer Res. 2013, 73, 1524–1535. [Google Scholar] [CrossRef] [PubMed]
- Helmlinger, G.; Yuan, F.; Dellian, M.; Jain, R.K. Interstitial pH and pO2 gradients in solid tumors in vivo: High-resolution measurements reveal a lack of correlation. Nat. Med. 1997, 3, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Reshkin, S.J.; Cardone, R.A.; Harguindey, S. Na+-H+ exchanger, pH regulation and cancer. Recent Pat. Anticancer Drug Discov. 2013, 8, 85–99. [Google Scholar] [CrossRef] [PubMed]
- Vaupel, P.; Kallinowski, F.; Okunieff, P. Blood flow, oxygen and nutrient supply, and metabolic microenvironment of human tumors: A review. Cancer Res. 1989, 49, 6449–6465. [Google Scholar] [PubMed]
- Novak, I.; Haanes, K.A.; Wang, J. Acid-base transport in pancreas—New challenges. Front. Physiol. 2013, 4. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, S.F.; Novak, I.; Alves, F.; Schwab, A.; Pardo, L.A. Alternating pH landscapes shape epithelial cancer initiation and progression: Focus on pancreatic cancer. Bioessays 2017. [Google Scholar] [CrossRef] [PubMed]
- Holzer, P. Acid-Sensitive Ion Channels and Receptors. In Sensory Nerves; Canning, B.J., Spina, D., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; Volume 194, pp. 283–332. ISBN 978-3-540-79089-1. [Google Scholar]
- Semtner, M.; Schaefer, M.; Pinkenburg, O.; Plant, T.D. Potentiation of TRPC5 by Protons. J. Biol. Chem. 2007, 282, 33868–33878. [Google Scholar] [CrossRef] [PubMed]
- Starkus, J.G.; Fleig, A.; Penner, R. The calcium-permeable non-selective cation channel TRPM2 is modulated by cellular acidification. J. Physiol. 2010, 588, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Mahieu, F.; Janssens, A.; Gees, M.; Talavera, K.; Nilius, B.; Voets, T. Modulation of the cold-activated cation channel TRPM8 by surface charge screening. J. Physiol. 2010, 588, 315–324. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Li, M.; Yue, L. Potentiation of TRPM7 inward currents by protons. J. Gen. Physiol. 2005, 126, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Mačianskienė, R.; Almanaitytė, M.; Jekabsone, A.; Mubagwa, K. Modulation of Human Cardiac TRPM7 Current by Extracellular Acidic pH Depends upon Extracellular Concentrations of Divalent Cations. PLoS ONE 2017, 12, e0170923. [Google Scholar] [CrossRef] [PubMed]
- Chokshi, R.; Matsushita, M.; Kozak, J.A. Detailed examination of Mg2+ and pH sensitivity of human TRPM7 channels. Am. J. Physiol. Cell Physiol. 2012, 302, C1004–C1011. [Google Scholar] [CrossRef] [PubMed]
- Hellwig, N.; Plant, T.D.; Janson, W.; Schäfer, M.; Schultz, G.; Schaefer, M. TRPV1 acts as proton channel to induce acidification in nociceptive neurons. J. Biol. Chem. 2004, 279, 34553–34561. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, M.; Morita, Y.; Hata, K.; Muragaki, Y. Acidic microenvironments induce lymphangiogenesis and IL-8 production via TRPV1 activation in human lymphatic endothelial cells. Exp. Cell Res. 2016, 345, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, M.; Mizuno, A.; Kodaira, K.; Imai, M. Impaired pressure sensation in mice lacking TRPV4. J. Biol. Chem. 2003, 278, 22664–22668. [Google Scholar] [CrossRef] [PubMed]
- Shikano, M.; Ueda, T.; Kamiya, T.; Ishida, Y.; Yamada, T.; Mizushima, T.; Shimura, T.; Mizoshita, T.; Tanida, S.; Kataoka, H.; et al. Acid inhibits TRPV4-mediated Ca2+ influx in mouse esophageal epithelial cells. Neurogastroenterol. Motil. 2011, 23, 1020–1028. [Google Scholar] [CrossRef] [PubMed]
- Muz, B.; de la Puente, P.; Azab, F.; Azab, A.K. The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia 2015, 3, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Provenzano, P.P.; Cuevas, C.; Chang, A.E.; Goel, V.K.; Von Hoff, D.D.; Hingorani, S.R. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell 2012, 21, 418–429. [Google Scholar] [CrossRef] [PubMed]
- Semenza, G.L. The hypoxic tumor microenvironment: A driving force for breast cancer progression. Biochim. Biophys. Acta 2016, 1863, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Mori, Y.; Takahashi, N.; Polat, O.K.; Kurokawa, T.; Takeda, N.; Inoue, M. Redox-sensitive transient receptor potential channels in oxygen sensing and adaptation. Pflüg. Arch. 2016, 468, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, J.; Wei, Y.; Liu, Y.; Ding, X.; Dong, B.; Xu, Y.; Wang, Y. Crucial role of TRPC6 in maintaining the stability of HIF-1α in glioma cells under hypoxia. J. Cell Sci. 2015, 128, 3317–3329. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Montell, C. Forcing open TRP channels: Mechanical gating as a unifying activation mechanism. Biochem. Biophys. Res. Commun. 2015, 460, 22–25. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.F.B.; Mortensen, M.B.; Detlefsen, S. Identification of markers for quiescent pancreatic stellate cells in the normal human pancreas. Histochem. Cell Biol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Iyer, S.C.; Kannan, A.; Devaraj, N.; Halagowder, D. Receptor channel TRPC6 orchestrate the activation of human hepatic stellate cell under hypoxia condition. Exp. Cell Res. 2015. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Karakhanova, S.; Werner, J.; Bazhin, A.V. Reactive oxygen species in cancer biology and anticancer therapy. Curr. Med. Chem. 2013, 20, 3677–3692. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.A.; Cheung, J.Y. TRPM2 protects against tissue damage following oxidative stress and ischaemia-reperfusion. J. Physiol. 2016, 594, 4181–4191. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Hoffman, N.E.; Shanmughapriya, S.; Bao, L.; Keefer, K.; Conrad, K.; Merali, S.; Takahashi, Y.; Abraham, T.; Hirschler-Laszkiewicz, I.; et al. A splice variant of the human ion channel TRPM2 modulates neuroblastoma tumor growth through hypoxia-inducible factor (HIF)-1/2α. J. Biol. Chem. 2014, 289, 36284–36302. [Google Scholar] [CrossRef] [PubMed]
- Orfanelli, U.; Wenke, A.-K.; Doglioni, C.; Russo, V.; Bosserhoff, A.K.; Lavorgna, G. Identification of novel sense and antisense transcription at the TRPM2 locus in cancer. Cell Res. 2008, 18, 1128–1140. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Chen, S.-J.; Conrad, K.; Keefer, K.; Abraham, T.; Lee, J.P.; Wang, J.; Zhang, X.-Q.; Hirschler-Laszkiewicz, I.; Wang, H.-G.; et al. Depletion of the Human Ion Channel TRPM2 in Neuroblastoma Demonstrates Its Key Role in Cell Survival through Modulation of Mitochondrial Reactive Oxygen Species and Bioenergetics. J. Biol. Chem. 2016, 291, 24449–24464. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.A.; Hoffman, N.E.; Merali, S.; Zhang, X.-Q.; Wang, J.; Rajan, S.; Shanmughapriya, S.; Gao, E.; Barrero, C.A.; Mallilankaraman, K.; et al. TRPM2 channels protect against cardiac ischemia-reperfusion injury: Role of mitochondria. J. Biol. Chem. 2014, 289, 7615–7629. [Google Scholar] [CrossRef] [PubMed]
- Aarts, M.; Iihara, K.; Wei, W.-L.; Xiong, Z.-G.; Arundine, M.; Cerwinski, W.; MacDonald, J.F.; Tymianski, M. A key role for TRPM7 channels in anoxic neuronal death. Cell 2003, 115, 863–877. [Google Scholar] [CrossRef]
- Takahashi, N.; Kuwaki, T.; Kiyonaka, S.; Numata, T.; Kozai, D.; Mizuno, Y.; Yamamoto, S.; Naito, S.; Knevels, E.; Carmeliet, P.; et al. TRPA1 underlies a sensing mechanism for O2. Nat. Chem. Biol. 2011, 7, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Parpaite, T.; Cardouat, G.; Mauroux, M.; Gillibert-Duplantier, J.; Robillard, P.; Quignard, J.-F.; Marthan, R.; Savineau, J.-P.; Ducret, T. Effect of hypoxia on TRPV1 and TRPV4 channels in rat pulmonary arterial smooth muscle cells. Pflüg. Arch. 2016, 468, 111–130. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, N.; Lindemann, O.; Schwab, A. TRP channels and STIM/ORAI proteins: Sensors and effectors of cancer and stroma cell migration. Br. J. Pharmacol. 2014, 171, 5524–5540. [Google Scholar] [CrossRef] [PubMed]
- Melzer, N.; Hicking, G.; Göbel, K.; Wiendl, H. TRPM2 cation channels modulate T cell effector functions and contribute to autoimmune CNS inflammation. PLoS ONE 2012, 7, e47617. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Shimizu, S.; Kiyonaka, S.; Takahashi, N.; Wajima, T.; Hara, Y.; Negoro, T.; Hiroi, T.; Kiuchi, Y.; Okada, T.; et al. TRPM2-mediated Ca2+ influx induces chemokine production in monocytes that aggravates inflammatory neutrophil infiltration. Nat. Med. 2008, 14, 738–747. [Google Scholar] [CrossRef] [PubMed]
- Luppi, F.; Longo, A.M.; de Boer, W.I.; Rabe, K.F.; Hiemstra, P.S. Interleukin-8 stimulates cell proliferation in non-small cell lung cancer through epidermal growth factor receptor transactivation. Lung Cancer 2007, 56, 25–33. [Google Scholar] [CrossRef] [PubMed]
- Rubil, S.; Lesch, A.; Mukaida, N.; Thiel, G. Stimulation of transient receptor potential M3 (TRPM3) channels increases interleukin-8 gene promoter activity involving AP-1 and extracellular signal-regulated protein kinase. Cytokine 2018, 103, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Takamori, H.; Oades, Z.G.; Hoch, O.C.; Burger, M.; Schraufstatter, I.U. Autocrine growth effect of IL-8 and GROalpha on a human pancreatic cancer cell line, Capan-1. Pancreas 2000, 21, 52–56. [Google Scholar] [CrossRef] [PubMed]
- Waugh, D.J.J.; Wilson, C. The interleukin-8 pathway in cancer. Clin. Cancer Res. 2008, 14, 6735–6741. [Google Scholar] [CrossRef] [PubMed]
- Khalil, M.; Babes, A.; Lakra, R.; Försch, S.; Reeh, P.W.; Wirtz, S.; Becker, C.; Neurath, M.F.; Engel, M.A. Transient receptor potential melastatin 8 ion channel in macrophages modulates colitis through a balance-shift in TNF-alpha and interleukin-10 production. Mucosal Immunol. 2016, 9, 1500–1513. [Google Scholar] [CrossRef] [PubMed]
- Juergens, U.R.; Engelen, T.; Racké, K.; Stöber, M.; Gillissen, A.; Vetter, H. Inhibitory activity of 1,8-cineol (eucalyptol) on cytokine production in cultured human lymphocytes and monocytes. Pulm. Pharmacol. Ther. 2004, 17, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Sabnis, A.S.; Reilly, C.A.; Veranth, J.M.; Yost, G.S. Increased transcription of cytokine genes in human lung epithelial cells through activation of a TRPM8 variant by cold temperatures. Am. J. Physiol. Lung Cell. Mol. Physiol. 2008, 295, L194–200. [Google Scholar] [CrossRef] [PubMed]
- Yamashiro, K.; Sasano, T.; Tojo, K.; Namekata, I.; Kurokawa, J.; Sawada, N.; Suganami, T.; Kamei, Y.; Tanaka, H.; Tajima, N.; et al. Role of transient receptor potential vanilloid 2 in LPS-induced cytokine production in macrophages. Biochem. Biophys. Res. Commun. 2010, 398, 284–289. [Google Scholar] [CrossRef] [PubMed]
- Fusi, C.; Materazzi, S.; Minocci, D.; Maio, V.; Oranges, T.; Massi, D.; Nassini, R. Transient receptor potential vanilloid 4 (TRPV4) is downregulated in keratinocytes in human non-melanoma skin cancer. J. Investig. Dermatol. 2014, 134, 2408–2417. [Google Scholar] [CrossRef] [PubMed]
- Henry, C.O.; Dalloneau, E.; Pérez-Berezo, M.-T.; Plata, C.; Wu, Y.; Guillon, A.; Morello, E.; Aimar, R.-F.; Potier-Cartereau, M.; Esnard, F.; et al. In vitro and in vivo evidence for an inflammatory role of the calcium channel TRPV4 in lung epithelium: Potential involvement in cystic fibrosis. Am. J. Physiol. Lung Cell. Mol. Physiol. 2016, 311, L664–675. [Google Scholar] [CrossRef] [PubMed]
- Northey, J.J.; Przybyla, L.; Weaver, V.M. Tissue Force Programs Cell Fate and Tumor Aggression. Cancer Discov. 2017, 7, 1224–1237. [Google Scholar] [CrossRef] [PubMed]
- Pickup, M.W.; Mouw, J.K.; Weaver, V.M. The extracellular matrix modulates the hallmarks of cancer. EMBO Rep. 2014, 15, 1243–1253. [Google Scholar] [CrossRef] [PubMed]
- Lachowski, D.; Cortes, E.; Pink, D.; Chronopoulos, A.; Karim, S.A.; Morton, J.; del Río Hernández, A.E. Substrate Rigidity Controls Activation and Durotaxis in Pancreatic Stellate Cells. Sci. Rep. 2017, 7, 2506. [Google Scholar] [CrossRef] [PubMed]
- Stylianopoulos, T.; Martin, J.D.; Chauhan, V.P.; Jain, S.R.; Diop-Frimpong, B.; Bardeesy, N.; Smith, B.L.; Ferrone, C.R.; Hornicek, F.J.; Boucher, Y.; et al. Causes, consequences, and remedies for growth-induced solid stress in murine and human tumors. Proc. Natl. Acad. Sci. USA 2012, 109, 15101–15108. [Google Scholar] [CrossRef] [PubMed]
- Acerbi, I.; Cassereau, L.; Dean, I.; Shi, Q.; Au, A.; Park, C.; Chen, Y.Y.; Liphardt, J.; Hwang, E.S.; Weaver, V.M. Human breast cancer invasion and aggression correlates with ECM stiffening and immune cell infiltration. Integr. Biol. 2015, 7, 1120–1134. [Google Scholar] [CrossRef] [PubMed]
- Paszek, M.J.; Zahir, N.; Johnson, K.R.; Lakins, J.N.; Rozenberg, G.I.; Gefen, A.; Reinhart-King, C.A.; Margulies, S.S.; Dembo, M.; Boettiger, D.; et al. Tensional homeostasis and the malignant phenotype. Cancer Cell 2005, 8, 241–254. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.E.; Kay, E.J.; Neilson, L.J.; Henze, A.; Serneels, J.; McGhee, E.J.; Dhayade, S.; Nixon, C.; Mackey, J.B.; Santi, A.; et al. Tumor matrix stiffness promotes metastatic cancer cell interaction with the endothelium. EMBO J. 2017, 36, 2373–2389. [Google Scholar] [CrossRef] [PubMed]
- Rice, A.J.; Cortes, E.; Lachowski, D.; Cheung, B.C.H.; Karim, S.A.; Morton, J.P.; del Río Hernández, A. Matrix stiffness induces epithelial–mesenchymal transition and promotes chemoresistance in pancreatic cancer cells. Oncogenesis 2017, 6, e352. [Google Scholar] [CrossRef] [PubMed]
- Fels, B.; Nielsen, N.; Schwab, A. Role of TRPC1 channels in pressure-mediated activation of murine pancreatic stellate cells. Eur. Biophys. J. 2016, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Mrkonjić, S.; Garcia-Elias, A.; Pardo-Pastor, C.; Bazellières, E.; Trepat, X.; Vriens, J.; Ghosh, D.; Voets, T.; Vicente, R.; Valverde, M.A. TRPV4 participates in the establishment of trailing adhesions and directional persistence of migrating cells. Pflüg. Arch. 2015, 467, 2107–2119. [Google Scholar] [CrossRef] [PubMed]
- Fabian, A.; Bertrand, J.; Lindemann, O.; Pap, T.; Schwab, A. Transient receptor potential canonical channel 1 impacts on mechanosignaling during cell migration. Pflüg. Arch. 2012, 464, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-S.; Liu, Y.-A.; Huang, C.-J.; Yen, M.-H.; Tseng, C.-T.; Chien, S.; Lee, O.K. Mechanosensitive TRPM7 mediates shear stress and modulates osteogenic differentiation of mesenchymal stromal cells through Osterix pathway. Sci. Rep. 2015, 5, 16522. [Google Scholar] [CrossRef] [PubMed]
- Lennertz, R.C.; Kossyreva, E.A.; Smith, A.K.; Stucky, C.L. TRPA1 Mediates Mechanical Sensitization in Nociceptors during Inflammation. PLoS ONE 2012, 7, e43597. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.-W.; Chang, S.-J.; Harn, H.I.-C.; Huang, H.-T.; Lin, H.-H.; Shen, M.-R.; Tang, M.-J.; Chiu, W.-T. Mechanosensitive store-operated calcium entry regulates the formation of cell polarity. J. Cell. Physiol. 2015, 230, 2086–2097. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.M.; Choi, S.; Park, K. TRPM7 Is Involved in Volume Regulation in Salivary Glands. J. Dent. Res. 2017, 96, 1044–1050. [Google Scholar] [CrossRef] [PubMed]
- Won, J.; Vang, H.; Kim, J.H.; Lee, P.R.; Kang, Y.; Oh, S.B. TRPM7 Mediates Mechanosensitivity in Adult Rat Odontoblasts. J. Dent. Res. 2018, 22034518759947. [Google Scholar] [CrossRef] [PubMed]
- Middelbeek, J.; Vrenken, K.; Visser, D.; Lasonder, E.; Koster, J.; Jalink, K.; Clark, K.; van Leeuwen, F.N. The TRPM7 interactome defines a cytoskeletal complex linked to neuroblastoma progression. Eur. J. Cell Biol. 2016, 95, 465–474. [Google Scholar] [CrossRef] [PubMed]
- Adapala, R.K.; Thoppil, R.J.; Ghosh, K.; Cappelli, H.C.; Dudley, A.C.; Paruchuri, S.; Keshamouni, V.; Klagsbrun, M.; Meszaros, J.G.; Chilian, W.M.; et al. Activation of mechanosensitive ion channel TRPV4 normalizes tumor vasculature and improves cancer therapy. Oncogene 2015. [Google Scholar] [CrossRef] [PubMed]
- Ferdek, P.E.; Jakubowska, M.A. Biology of pancreatic stellate cells-more than just pancreatic cancer. Pflüg. Arch. 2017. [Google Scholar] [CrossRef]
- Gryshchenko, O.; Gerasimenko, J.V.; Gerasimenko, O.V.; Petersen, O.H. Ca(2+) signals mediated by bradykinin type 2 receptors in normal pancreatic stellate cells can be inhibited by specific Ca(2+) channel blockade. J. Physiol. 2015. [Google Scholar] [CrossRef]
- Storck, H.; Hild, B.; Schimmelpfennig, S.; Sargin, S.; Nielsen, N.; Zaccagnino, A.; Budde, T.; Novak, I.; Kalthoff, H.; Schwab, A. Ion channels in control of pancreatic stellate cell migration. Oncotarget 2017. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Zhan, S.; Huang, C.; Cheng, X.; Lv, X.; Si, H.; Li, J. TRPM7 channel regulates PDGF-BB-induced proliferation of hepatic stellate cells via PI3K and ERK pathways. Toxicol. Appl. Pharmacol. 2013, 272, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Huang, C.; Meng, X.; Wu, B.; Ma, T.; Liu, X.; Zhu, Q.; Zhan, S.; Li, J. TGF-β1-elevated TRPM7 channel regulates collagen expression in hepatic stellate cells via TGF-β1/Smad pathway. Toxicol. Appl. Pharmacol. 2014, 280, 335–344. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.; Wang, X.; Chen, M.; Ouyang, K.; Song, L.-S.; Cheng, H. Calcium flickers steer cell migration. Nature 2009, 457, 901–905. [Google Scholar] [CrossRef] [PubMed]
- Vancauwenberghe, E.; Noyer, L.; Derouiche, S.; Lemonnier, L.; Gosset, P.; Sadofsky, L.R.; Mariot, P.; Warnier, M.; Bokhobza, A.; Slomianny, C.; et al. Activation of mutated TRPA1 ion channel by resveratrol in human prostate cancer associated fibroblasts (CAF). Mol. Carcinog. 2017, 56, 1851–1867. [Google Scholar] [CrossRef] [PubMed]
- Mayer, P.; Dinkic, C.; Jesenofsky, R.; Klauss, M.; Schirmacher, P.; Dapunt, U.; Hackert, T.; Uhle, F.; Hänsch, G.M.; Gaida, M.M. Changes in the microarchitecture of the pancreatic cancer stroma are linked to neutrophil-dependent reprogramming of stellate cells and reflected by diffusion-weighted magnetic resonance imaging. Theranostics 2018, 8, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Powell, D.R.; Huttenlocher, A. Neutrophils in the Tumor Microenvironment. Trends Immunol. 2016, 37, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Nywening, T.M.; Belt, B.A.; Cullinan, D.R.; Panni, R.Z.; Han, B.J.; Sanford, D.E.; Jacobs, R.C.; Ye, J.; Patel, A.A.; Gillanders, W.E.; et al. Targeting both tumour-associated CXCR2+neutrophils and CCR2+macrophages disrupts myeloid recruitment and improves chemotherapeutic responses in pancreatic ductal adenocarcinoma. Gut 2017. [Google Scholar] [CrossRef] [PubMed]
- Di, A.; Gao, X.-P.; Qian, F.; Kawamura, T.; Han, J.; Hecquet, C.; Ye, R.D.; Vogel, S.M.; Malik, A.B. The redox-sensitive cation channel TRPM2 modulates phagocyte ROS production and inflammation. Nat. Immunol. 2011, 13, 29–34. [Google Scholar] [CrossRef] [PubMed]
- Haraguchi, K.; Kawamoto, A.; Isami, K.; Maeda, S.; Kusano, A.; Asakura, K.; Shirakawa, H.; Mori, Y.; Nakagawa, T.; Kaneko, S. TRPM2 contributes to inflammatory and neuropathic pain through the aggravation of pronociceptive inflammatory responses in mice. J. Neurosci. 2012, 32, 3931–3941. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-H.; Rong, M.-Y.; Wang, L.; Ren, Z.; Chen, L.-N.; Jia, J.-F.; Li, X.-Y.; Wu, Z.-B.; Chen, Z.-N.; Zhu, P. CD147 up-regulates calcium-induced chemotaxis, adhesion ability and invasiveness of human neutrophils via a TRPM-7-mediated mechanism. Rheumatology 2014, 53, 2288–2296. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Michalick, L.; Tang, C.; Tabuchi, A.; Goldenberg, N.; Dan, Q.; Awwad, K.; Wang, L.; Erfinanda, L.; Nouailles, G.; et al. Role of Transient Receptor Potential Vanilloid 4 in Neutrophil Activation and Acute Lung Injury. Am. J. Respir. Cell Mol. Biol. 2016, 54, 370–383. [Google Scholar] [CrossRef] [PubMed]
- Earley, S.; Brayden, J.E. Transient receptor potential channels in the vasculature. Physiol. Rev. 2015, 95, 645–690. [Google Scholar] [CrossRef] [PubMed]
- Fiorio Pla, A.; Gkika, D. Emerging role of TRP channels in cell migration: From tumor vascularization to metastasis. Front. Physiol. 2013, 4. [Google Scholar] [CrossRef] [PubMed]
- Hamdollah Zadeh, M.A.; Glass, C.A.; Magnussen, A.; Hancox, J.C.; Bates, D.O. VEGF-mediated elevated intracellular calcium and angiogenesis in human microvascular endothelial cells in vitro are inhibited by dominant negative TRPC6. Microcirculation 2008, 15, 605–614. [Google Scholar] [CrossRef] [PubMed]
- Kini, V.; Chavez, A.; Mehta, D. A new role for PTEN in regulating transient receptor potential canonical channel 6-mediated Ca2+ entry, endothelial permeability, and angiogenesis. J. Biol. Chem. 2010, 285, 33082–33091. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, K.; Dubrovska, G.; Nielsen, G.; Fesüs, G.; Uhrenholt, T.R.; Hansen, P.B.; Gudermann, T.; Dietrich, A.; Gollasch, M.; de Wit, C.; Köhler, R. Amplification of EDHF-type vasodilatations in TRPC1-deficient mice. Br. J. Pharmacol. 2010, 161, 1722–1733. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-K.; Hsu, P.-Y.; Wang, T.-M.; Miao, Z.-F.; Lin, R.-T.; Juo, S.-H.H. TRPV4 Activation Contributes Functional Recovery from Ischemic Stroke via Angiogenesis and Neurogenesis. Mol. Neurobiol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Thodeti, C.K.; Matthews, B.; Ravi, A.; Mammoto, A.; Ghosh, K.; Bracha, A.L.; Ingber, D.E. TRPV4 channels mediate cyclic strain-induced endothelial cell reorientation through integrin-to-integrin signaling. Circ. Res. 2009, 104, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Fiorio Pla, A.; Ong, H.L.; Cheng, K.T.; Brossa, A.; Bussolati, B.; Lockwich, T.; Paria, B.; Munaron, L.; Ambudkar, I.S. TRPV4 mediates tumor-derived endothelial cell migration via arachidonic acid-activated actin remodeling. Oncogene 2012, 31, 200–212. [Google Scholar] [CrossRef] [PubMed]
- Thoppil, R.J.; Cappelli, H.C.; Adapala, R.K.; Kanugula, A.K.; Paruchuri, S.; Thodeti, C.K. TRPV4 channels regulate tumor angiogenesis via modulation of Rho/Rho kinase pathway. Oncotarget 2016, 7, 25849–25861. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.-X.; Yuan, J.-N.; Zhang, F.-R.; Liu, Y.-Y.; Zhang, T.-T.; Li, K.; Lv, X.-F.; Zhou, J.-G.; Huang, L.-Y.; Shang, J.-Y.; et al. Inhibition of Orai1-mediated Ca2+ entry limits endothelial cell inflammation by suppressing calcineurin-NFATc4 signaling pathway. Biochem. Biophys. Res. Commun. 2018, 495, 1864–1870. [Google Scholar] [CrossRef] [PubMed]
- Bodiga, V.L.; Kudle, M.R.; Bodiga, S. Silencing of PKC-α, TRPC1 or NF-κB expression attenuates cisplatin-induced ICAM-1 expression and endothelial dysfunction. Biochem. Pharmacol. 2015, 98, 78–91. [Google Scholar] [CrossRef] [PubMed]
- Kaytes, P.S.; Geng, J.G. P-selectin mediates adhesion of the human melanoma cell line NKI-4: Identification of glycoprotein ligands. Biochemistry 1998, 37, 10514–10521. [Google Scholar] [CrossRef] [PubMed]
- Bihari, S.; Dixon, D.-L.; Lawrence, M.D.; De Bellis, D.; Bonder, C.S.; Dimasi, D.P.; Bersten, A.D. Fluid-induced lung injury-role of TRPV4 channels. Pflüg. Arch. 2017, 469, 1121–1134. [Google Scholar] [CrossRef] [PubMed]
- Smedlund, K.; Tano, J.-Y.; Vazquez, G. The constitutive function of native TRPC3 channels modulates vascular cell adhesion molecule-1 expression in coronary endothelial cells through nuclear factor kappaB signaling. Circ. Res. 2010, 106, 1479–1488. [Google Scholar] [CrossRef] [PubMed]
- Bulk, E.; Ay, A.-S.; Hammadi, M.; Ouadid-Ahidouch, H.; Schelhaas, S.; Hascher, A.; Rohde, C.; Thoennissen, N.H.; Wiewrodt, R.; Schmidt, E.; et al. Epigentic dysregulation of KCa 3.1 channels induces poor prognosis in lung cancer. Int. J. Cancer J. Int. Cancer 2015. [Google Scholar] [CrossRef] [PubMed]
- Sukumaran, P.; Löf, C.; Pulli, I.; Kemppainen, K.; Viitanen, T.; Törnquist, K. Significance of the transient receptor potential canonical 2 (TRPC2) channel in the regulation of rat thyroid FRTL-5 cell proliferation, migration, adhesion and invasion. Mol. Cell. Endocrinol. 2013, 374, 10–21. [Google Scholar] [CrossRef] [PubMed]
- Nagafuchi, A.; Takeichi, M. Cell binding function of E-cadherin is regulated by the cytoplasmic domain. EMBO J. 1988, 7, 3679–3684. [Google Scholar] [PubMed]
- Phuong, T.T.T.; Redmon, S.N.; Yarishkin, O.; Winter, J.M.; Li, D.Y.; Križaj, D. Calcium influx through TRPV4 channels modulates the adherens contacts between retinal microvascular endothelial cells. J. Physiol. 2017, 595, 6869–6885. [Google Scholar] [CrossRef] [PubMed]
- Simonsen, U.; Wandall-Frostholm, C.; Oliván-Viguera, A.; Köhler, R. Emerging roles of calcium-activated K channels and TRPV4 channels in lung oedema and pulmonary circulatory collapse. Acta Physiol. Oxf. Engl. 2017, 219, 176–187. [Google Scholar] [CrossRef] [PubMed]
- Wandall-Frostholm, C.; Dalsgaard, T.; Bajoriūnas, V.; Oliván-Viguera, A.; Sadda, V.; Beck, L.; Mogensen, S.; Stankevicius, E.; Simonsen, U.; Köhler, R. Genetic deficit of KCa 3.1 channels protects against pulmonary circulatory collapse induced by TRPV4 channel activation. Br. J. Pharmacol. 2015. [Google Scholar] [CrossRef] [PubMed]
- Mittal, M.; Nepal, S.; Tsukasaki, Y.; Hecquet, C.M.; Soni, D.; Rehman, J.; Tiruppathi, C.; Malik, A.B. Neutrophil Activation of Endothelial Cell-Expressed TRPM2 Mediates Transendothelial Neutrophil Migration and Vascular Injury. Circ. Res. 2017, 121, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Weber, E.W.; Han, F.; Tauseef, M.; Birnbaumer, L.; Mehta, D.; Muller, W.A. TRPC6 is the endothelial calcium channel that regulates leukocyte transendothelial migration during the inflammatory response. J. Exp. Med. 2015, 212, 1883–1899. [Google Scholar] [CrossRef] [PubMed]
- Bittner, S.; Ruck, T.; Schuhmann, M.K.; Herrmann, A.M.; Maati, H.M.; ou Bobak, N.; Göbel, K.; Langhauser, F.; Stegner, D.; Ehling, P.; Borsotto, M.; et al. Endothelial TWIK-related potassium channel-1 (TREK1) regulates immune-cell trafficking into the CNS. Nat. Med. 2013, 19, 1161–1165. [Google Scholar] [CrossRef] [PubMed]
- Cui, C.; Merritt, R.; Fu, L.; Pan, Z. Targeting calcium signaling in cancer therapy. Acta Pharm. Sin. B 2017, 7, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Barritt, G.J. TRPM8 in prostate cancer cells: A potential diagnostic and prognostic marker with a secretory function? Endocr. Relat. Cancer 2006, 13, 27–38. [Google Scholar] [CrossRef] [PubMed]
- Ouadid-Ahidouch, H.; Dhennin-Duthille, I.; Gautier, M.; Sevestre, H.; Ahidouch, A. TRP channels: Diagnostic markers and therapeutic targets for breast cancer? Trends Mol. Med. 2013, 19, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Peters, A.A.; Simpson, P.T.; Bassett, J.J.; Lee, J.M.; Da Silva, L.; Reid, L.E.; Song, S.; Parat, M.-O.; Lakhani, S.R.; Kenny, P.A.; et al. Calcium channel TRPV6 as a potential therapeutic target in estrogen receptor-negative breast cancer. Mol. Cancer Ther. 2012, 11, 2158–2168. [Google Scholar] [CrossRef] [PubMed]
- Alptekin, M.; Eroglu, S.; Tutar, E.; Sencan, S.; Geyik, M.A.; Ulasli, M.; Demiryurek, A.T.; Camci, C. Gene expressions of TRP channels in glioblastoma multiforme and relation with survival. Tumour Biol. 2015, 36, 9209–9213. [Google Scholar] [CrossRef] [PubMed]
- Wen, L.; Liang, C.; Chen, E.; Chen, W.; Liang, F.; Zhi, X.; Wei, T.; Xue, F.; Li, G.; Yang, Q.; et al. Regulation of Multi-drug Resistance in hepatocellular carcinoma cells is TRPC6/Calcium Dependent. Sci. Rep. 2016, 6, 23269. [Google Scholar] [CrossRef] [PubMed]
- Gautier, M.; Dhennin-Duthille, I.; Ay, A.S.; Rybarczyk, P.; Korichneva, I.; Ouadid-Ahidouch, H. New insights into pharmacological tools to TR(i)P cancer up. Br. J. Pharmacol. 2014, 171, 2582–2592. [Google Scholar] [CrossRef] [PubMed]
- Beck, B.; Bidaux, G.; Bavencoffe, A.; Lemonnier, L.; Thebault, S.; Shuba, Y.; Barrit, G.; Skryma, R.; Prevarskaya, N. Prospects for prostate cancer imaging and therapy using high-affinity TRPM8 activators. Cell Calcium 2007, 41, 285–294. [Google Scholar] [CrossRef] [PubMed]
- Boonstra, M.C.; de Geus, S.W.L.; Prevoo, H.A.J.M.; Hawinkels, L.J.A.C.; van de Velde, C.J.H.; Kuppen, P.J.K.; Vahrmeijer, A.L.; Sier, C.F.M. Selecting Targets for Tumor Imaging: An Overview of Cancer-Associated Membrane Proteins. Biomark. Cancer 2016, 8, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Lehen’Kyi, V.; Flourakis, M.; Skryma, R.; Prevarskaya, N. TRPV6 channel controls prostate cancer cell proliferation via Ca(2+)/NFAT-dependent pathways. Oncogene 2007, 26, 7380–7385. [Google Scholar] [CrossRef] [PubMed]
- Lau, J.K.; Brown, K.C.; Dom, A.M.; Witte, T.R.; Thornhill, B.A.; Crabtree, C.M.; Perry, H.E.; Brown, J.M.; Ball, J.G.; Creel, R.G.; et al. Capsaicin induces apoptosis in human small cell lung cancer via the TRPV6 receptor and the calpain pathway. Apoptosis 2014, 19, 1190–1201. [Google Scholar] [CrossRef] [PubMed]
- Stern, S.T.; Martinez, M.N.; Stevens, D.M. When Is It Important to Measure Unbound Drug in Evaluating Nanomedicine Pharmacokinetics? Drug Metab. Dispos. 2016, 44, 1934–1939. [Google Scholar] [CrossRef] [PubMed]
- Nabissi, M.; Morelli, M.B.; Santoni, M.; Santoni, G. Triggering of the TRPV2 channel by cannabidiol sensitizes glioblastoma cells to cytotoxic chemotherapeutic agents. Carcinogenesis 2013, 34, 48–57. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).