Relationship Between Lower-Extremity Co-Contraction and Jerk During Gait
Abstract
Highlights
- Our study estimated the lower-extremity co-contractions from lower-leg jerks during gait.
- Our study showed that multiple regression analyses adjusted for age and gait speed revealed a relationship between jerks and co-contraction index.
- The study showed that reducing co-contraction reduces joint load, which is important for increasing lifespan.
- The gait analysis developed in this study can be a meaningful method for early preventive interventions for decreased gait speed.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Participants
2.3. Outcome Measures
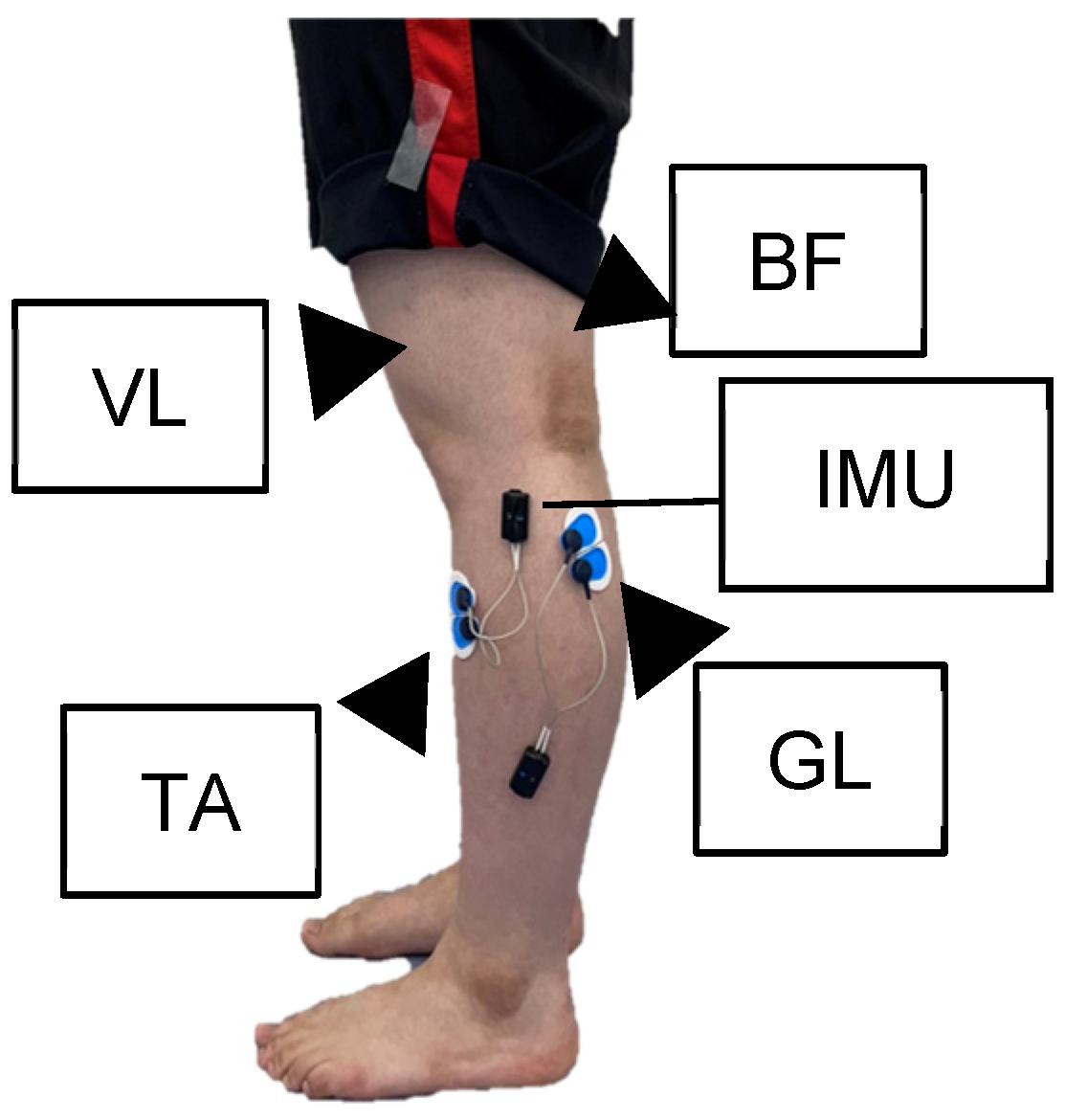
2.3.1. Surface EMG
Percent CCI
2.3.2. IMU Settings
Jerk
Estimated AP
STV
2.3.3. Gait Speed
2.4. Sample Size
2.5. Statistical Analysis
3. Results
3.1. General Characteristics and Outcomes
3.2. Correlation Between CCI, Age, Gait Speed and the Integral Value of Muscle Activities
3.3. Multiple Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CC | co-contractions |
| EMG | electromyography |
| TA | tibialis anterior |
| GL | gastrocnemius lateralis |
| VL | vastus lateralis |
| BF | biceps femoris |
| IMU | inertial measurement unit |
| CCI | co-contraction index |
| LS | Locomotive syndrome |
| AP | ankle plantar flexor power |
| STV | stride time variability |
| BMI | body mass index |
References
- Nakamura, K.; Ogata, T. Locomotive syndrome: Definition and management. Clin. Rev. Bone Miner. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef] [PubMed]
- Perry, J.; Garrett, M.; Gronley, J.K.; Mulroy, S.J. Classification of walking handicap in the stroke population. Stroke 1995, 26, 982–989. [Google Scholar] [CrossRef] [PubMed]
- Fulk, G.D.; He, Y.; Boyne, P.; Dunning, K. Predicting home and community walking activity poststroke. Stroke 2017, 48, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Fritz, S.; Lusardi, M. White paper: “Walking speed: The sixth vital sign”. J. Geriatr. Phys. Ther. 2009, 32, 2–9. [Google Scholar] [CrossRef]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture 2003, 18, 35–46. [Google Scholar] [CrossRef]
- Studenski, S.; Perera, S.; Patel, K.; Rosano, C.; Faulkner, K.; Inzitari, M.; Brach, J.; Chandler, J.; Cawthon, P.; Connor, E.B.; et al. Gait speed and survival in older adults. JAMA 2011, 305, 50–58. [Google Scholar] [CrossRef]
- Winter, D.A.; Patla, A.E.; Frank, J.S.; Walt, S.E. Biomechanical walking pattern changes in the fit and healthy elderly. Phys. Ther. 1990, 70, 340–347. [Google Scholar] [CrossRef]
- Judge, J.O.; Davis, R.B.; Ounpuu, S. Step length reductions in advanced age the role of ankle and hip kinetics. J. Gerontol. A Biol. Sci. Med. Sci. 1996, 51, M303–M312. [Google Scholar] [CrossRef]
- Franz, J.R.; Kram, R. Advanced age affects the individual leg mechanics of level, uphill, and downhill walking. J. Biomech. 2013, 46, 535–540. [Google Scholar] [CrossRef]
- Kulmala, J.-P.; Korhonen, M.T.; Kuitunen, S.; Suominen, H.; Heinonen, A.; Mikkola, A.; Avela, J. Which muscles compromise human locomotor performance with age? J. R. Soc. Interface 2014, 11, 20140858. [Google Scholar] [CrossRef]
- Kerrigan, D.C.; Todd, M.K.; Della Croce, U.; Lipsitz, L.A.; Collins, J.J. Biomechanical gait alterations independent of speed in the healthy elderly: Evidence for specific limiting impairments. Arch. Phys. Med. Rehabil. 1998, 79, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Chang, W.H.; Choi, B.O.; Ryu, G.H.; Kim, Y.H. Age-related differences in muscle co-activation during locomotion and their relationship with gait speed: A pilot study. BMC Geriatr. 2017, 17, 44. [Google Scholar] [CrossRef] [PubMed]
- Hausdorff, J.M.; Nelson, M.E.; Kaliton, D.; Layne, J.E.; Bernstein, M.J.; Nuernberger, A.; Singh, M.A. Etiology and modification of gait instability in older adults: A randomized controlled trial of exercise. J. Appl. Physiol. 2001, 90, 2117–2129. [Google Scholar] [CrossRef] [PubMed]
- Brognara, L.; Palumbo, P.; Grimm, B.; Palmerini, L. Assessing gait in Parkinson’s disease using wearable motion sensors: A systematic review. Diseases 2019, 7, 18. [Google Scholar] [CrossRef]
- Weygers, I.; Kok, M.; Konings, M.; Hallez, H.; De Vroey, H.; Claeys, K. Inertial sensor-based lower limb joint kinematics: A methodological systematic review. Sensors 2020, 20, 673. [Google Scholar] [CrossRef]
- Kobsar, D.; Charlton, J.M.; Tse, C.T.F.; Esculier, J.F.; Graffos, A.; Krowchuk, N.M.; Thatcher, D.; Hunt, M.A. Validity and reliability of wearable inertial sensors in healthy adult walking: A systematic review and meta-analysis. J. Neuroeng. Rehabil. 2020, 17, 62. [Google Scholar] [CrossRef]
- Lee, C.J.; Lee, J.K. Inertial motion capture-based wearable systems for estimation of joint kinetics: A systematic review. Sensors 2022, 22, 2507. [Google Scholar] [CrossRef]
- Prasanth, H.; Caban, M.; Keller, U.; Courtine, G.; Ijspeert, A.; Vallery, H.; von Zitzewitz, J. Wearable sensor-based real-time gait detection: A systematic review. Sensors 2021, 21, 2727. [Google Scholar] [CrossRef]
- Miyashita, T.; Kudo, S.; Maekawa, Y. Estimation of the ankle power during the terminal stance of gait using an inertial sensor. J. Phys. Ther. Sci. 2019, 31, 354–359. [Google Scholar] [CrossRef]
- Hortobágyi, T.; DeVita, P. Muscle pre- and coactivity during downward stepping are associated with leg stiffness in aging. J. Electromyogr. Kinesiol. 2000, 10, 117–126. [Google Scholar] [CrossRef]
- Hortobágyi, T.; Finch, A.; Solnik, S.; Rider, P.; DeVita, P. Association between muscle activation and metabolic cost of walking in Young and old adults. J. Gerontol. A Biol. Sci. Med. Sci. 2011, 66, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.W.; Kerrigan, D.C. Identification of Kinetic Differences between Fallers and Nonfallers in the Elderly. Am. J. Phys. Med. Rehabil. 1999, 78, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, P.; Vanswearingen, J.; Godfrey, A.; Redfern, M.; Montero-Odasso, M.; Sejdic, E. Acceleration gait measures as proxies for motor skill of walking: A narrative review. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Kawanishi, K.; Fukuda, D.; Niwa, H.; Okuno, T.; Miyashita, T.; Kitagawa, T.; Kudo, S. Relationship between tissue gliding of the lateral thigh and gait parameters after trochanteric fractures. Sensors 2022, 22, 3842. [Google Scholar] [CrossRef]
- Villagrán, I.; Moënne-Loccoz, C.; Aguilera, V.; García, V.; Reyes, J.T.; Rodríguez, S.; Miranda, C.; Altermatt, F.; Fuentes-López, E.; Delgado, M.; et al. Biomechanical analysis of expert anesthesiologists and novice residents performing a simulated central venous access procedure. PLoS ONE 2021, 16, e0250941. [Google Scholar] [CrossRef]
- Fukaya, T.; Mutsuzaki, H.; Nakano, W.; Mori, K. Smoothness of the knee joint movement during the stance phase in patients with severe knee osteoarthritis. Asia Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2018, 14, 1–5. [Google Scholar] [CrossRef]
- Mirelman, A.; Bernad-Elazari, H.; Nobel, T.; Thaler, A.; Peruzzi, A.; Plotnik, M.; Giladi, N.; Hausdorff, J.M. Effects of Aging on Arm Swing during Gait: The Role of Gait Speed and Dual Tasking. PLoS ONE 2015, 10, e0136043. [Google Scholar] [CrossRef]
- Lo, J.; Lo, O.-Y.; Olson, E.A.; Habtemariam, D.; Iloputaife, I.; Gagnon, M.M.; Manor, B.; Lipsitz, L.A. Functional implications of muscle co-contraction during gait in advanced age. Gait Posture 2017, 53, 110–114. [Google Scholar] [CrossRef]
- Craig, J.J.; Bruetsch, A.P.; Huisinga, J.M. Coordination of Trunk and Foot Acceleration during Gait Is Affected by Walking Velocity and Fall History in Elderly Adults. Aging Clin. Exp. Res. 2019, 31, 943–950. [Google Scholar] [CrossRef]
- Na, A.; Buchanan, T.S. Self-reported walking difficulty and knee osteoarthritis influences limb dynamics and muscle co-contraction during gait. Hum. Mov. Sci. 2019, 64, 409–419. [Google Scholar] [CrossRef]
- Minami, I.; Oogai, K.; Nemoto, T.; Nakamura, T.; Igarashi, Y.; Wakabayashi, N. Measurement of jerk-cost using a triaxial piezoelectric accelerometer for the evaluation of jaw movement smoothness. J. Oral Rehabil. 2010, 37, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Brodie, M.A.; Lovell, N.H.; Canning, C.G.; Menz, H.B.; Delbaere, K.; Redmond, S.J.; Latt, M.; Sturnieks, D.L.; Menant, J.; Smith, S.T.; et al. Gait as a biomarker? Accelerometers reveal that reduced movement quality while walking is associated with Parkinson’s disease, ageing and fall risk. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2014, 2014, 5968–5971. [Google Scholar] [CrossRef] [PubMed]
- Germanotta, M.; Vasco, G.; Petrarca, M.; Rossi, S.; Carniel, S.; Bertini, E.; Cappa, P.; Castelli, E. Robotic and clinical evaluation of upper limb motor performance in patients with Friedreich’s ataxia: An observational study. J. Neuroeng. Rehabil. 2015, 12, 41. [Google Scholar] [CrossRef] [PubMed]
- Brunner, R.; Frigo, C.A. Control of tibial advancement by the plantar flexors during the stance phase of gait depends on knee flexion with respect to the ground reaction force. Bioengineering 2023, 11, 41. [Google Scholar] [CrossRef]
- Favre, J.; Erhart-Hledik, J.C.; Andriacchi, T.P. Age-related differences in sagittal-plane knee function at Heel-Strike of walking are increased in osteoarthritic patients. Osteoarthr. Cartil. 2014, 22, 464–471. [Google Scholar] [CrossRef]
- Brunner, R.; Rutz, E. Biomechanics and muscle function during gait. J. Child. Orthop. 2013, 7, 367–371. [Google Scholar] [CrossRef]
- Trepczynski, A.; Kutzner, I.; Schwachmeyer, V.; Heller, M.O.; Pfitzner, T.; Duda, G.N. Impact of antagonistic muscle co-contraction on in vivo knee contact forces. J. Neuroeng. Rehabil. 2018, 15, 101. [Google Scholar] [CrossRef]
- Brunner, R.; Romkes, J. Abnormal EMG muscle activity during gait in patients without neurological disorders. Gait Posture 2008, 27, 399–407. [Google Scholar] [CrossRef]
- Mengarelli, A.; Maranesi, E.; Burattini, L.; Fioretti, S.; Di Nardo, F. Co-Contraction Activity of Ankle Muscles during Walking: A Gender Comparison. Biomed. Signal Process. Control 2017, 33, 1–9. [Google Scholar] [CrossRef]
- Craig, C.E.; Goble, D.J.; Doumas, M. Proprioceptive Acuity Predicts Muscle Co-Contraction of the tibialis anterior and gastrocnemius Medialis in Older Adults’ Dynamic Postural Control. Neuroscience 2016, 322, 251–261. [Google Scholar] [CrossRef]



| Variable | n = 30 (Female: 22, Male: 8) |
|---|---|
| Age (year) | 66.0 (12.0) |
| Height (cm) | 159.9 (9.8) |
| Weight (kg) | 61.5 (10.8) |
| BMI | 24.0 (3.7) |
| Gait speed (m/s) | 1.22 (0.22) |
| Estimated AP (W/kg) | 0.065 (0.010) |
| STV (%) | 2.18 (0.92) |
| TAGL (%) | 62.2 (11.6) |
| VLBF (%) | 64.4 (10.1) |
| VLGL (%) | 59.8 (12.3) |
| First Half of Stance Phase | Second Half of Stance Phase | Variables | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jerk x | Jerk y | Jerk z | Jerk x | Jerk y | Jerk z | AP | GS | Age | |||
| CCI | Entire stance phase | TAGL | 0.17 | 0.02 | −0.002 | 0.24 | 0.003 | −0.08 | −0.009 | −0.23 | 0.11 |
| VLBF | 0.05 | −0.32 | −0.27 | 0.18 | −0.28 | −0.09 | −0.007 | −0.04 | 0.13 | ||
| VLGL | 0.30 | 0.003 | 0.15 | 0.59 *** | −0.20 | 0.02 | −0.004 | −0.36 * | 0.27 | ||
| First half of stance phase | TAGL | 0.31 | 0.13 | 0.05 | 0.27 | −0.02 | −0.06 | 0.01 | −0.09 | 0.11 | |
| VLBF | 0.05 | −0.22 | −0.12 | 0.12 | −0.16 | 0.06 | 0.05 | −0.09 | 0.13 | ||
| VLGL | 0.23 | 0.02 | 0.26 | 0.44 * | 0.01 | 0.20 | 0.15 | −0.11 | 0.10 | ||
| Second half of stance phase | TAGL | 0.19 | −0.02 | −0.19 | 0.38 * | −0.17 | −0.26 | −0.06 | −0.30 | 0.24 | |
| VLBF | 0.21 | −0.32 | −0.38 * | 0.17 | −0.27 | −0.20 | 0.05 | 0.10 | 0.06 | ||
| VLGL | 0.23 | 0.05 | −0.03 | 0.39 * | −0.31 | −0.25 | −0.18 | −0.53 ** | 0.50 ** | ||
| Entire Stance Phase | First Half of Stance Phase | Second Half of Stance Phase | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| TAGL | VLBF | VLGL | TAGL | VLBF | VLGL | TAGL | VLBF | VLGL | |||
| The integral value of each muscle activity | Entire stance phase | TA | −0.14 | −0.1 | −0.01 | −0.15 | −0.31 | 0.13 | 0.07 | −0.02 | 0.01 |
| GL | −0.15 | −0.50 ** | −0.22 | 0.08 | −0.47 ** | 0.13 | −0.33 | −0.35 | −0.31 | ||
| VL | 0.02 | −0.21 | −0.42 * | −0.01 | −0.39 * | −0.53 | −0.11 | −0.21 | 0.01 | ||
| BF | −0.05 | −0.28 | −0.42 * | −0.05 | −0.32 | −0.40 ** | −0.1 | −0.22 | −0.42 * | ||
| First half of stance phase | TA | −0.21 | −0.19 | 0.03 | −0.22 | −0.35 | 0.15 | 0.01 | −0.11 | 0.10 | |
| GL | 0.15 | −0.18 | 0.15 | 0.35 | −0.29 | 0.09 | −0.08 | −0.16 | 0.14 | ||
| VL | −0.05 | −0.24 | −0.44 * | −0.04 | −0.45 * | −0.55 ** | −0.16 | −0.21 | −0.05 | ||
| BF | −0.07 | −0.06 | −0.33 | −0.09 | −0.27 | −0.39 ** | −0.03 | −0.02 | −0.33 | ||
| Second half of stance phase | TA | 0.09 | −0.07 | −0.16 | 0.02 | −0.21 | 0.15 | 0.23 | 0.02 | 0.02 | |
| GL | −0.3 | −0.56 ** | −0.25 | −0.12 | −0.39 * | −0.15 | −0.38 * | −0.43 * | −0.41 * | ||
| VL | 0.02 | −0.14 | −0.42 * | 0.03 | −0.25 | −0.48 ** | −0.11 | −0.19 | −0.11 | ||
| BF | −0.05 | −0.40 * | −0.44 * | −0.03 | −0.32 | −0.37 * | −0.15 | −0.37 * | −0.44 | ||
| Unstandardized Coefficients | Standardized Coefficients β | 95% Confidence Interval | p-Value | VIF | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| (Constant) | 39.510 | 7.245 | 71.775 | 0.018 | ||
| Second half of stance Ax jerk | 27.105 | 0.393 | 8.049 | 46.161 | 0.007 | 1.116 |
| Age | 0.343 | 0.348 | 0.072 | 0.613 | 0.015 | 1.106 |
| gait speed | −17.511 | −0.328 | −32.423 | −2.599 | 0.023 | 1.142 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miyashita, T.; Kawanishi, K.; Kudo, S. Relationship Between Lower-Extremity Co-Contraction and Jerk During Gait. Sensors 2025, 25, 2327. https://doi.org/10.3390/s25072327
Miyashita T, Kawanishi K, Kudo S. Relationship Between Lower-Extremity Co-Contraction and Jerk During Gait. Sensors. 2025; 25(7):2327. https://doi.org/10.3390/s25072327
Chicago/Turabian StyleMiyashita, Toshinori, Kengo Kawanishi, and Shintarou Kudo. 2025. "Relationship Between Lower-Extremity Co-Contraction and Jerk During Gait" Sensors 25, no. 7: 2327. https://doi.org/10.3390/s25072327
APA StyleMiyashita, T., Kawanishi, K., & Kudo, S. (2025). Relationship Between Lower-Extremity Co-Contraction and Jerk During Gait. Sensors, 25(7), 2327. https://doi.org/10.3390/s25072327






