Emerging Applications of Augmented and Mixed Reality Technologies in Motor Rehabilitation: A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategy
2.4. Selection of Sources of Evidence
2.5. Data Charting
2.6. Data Items
2.7. Synthesis of Results
3. Results
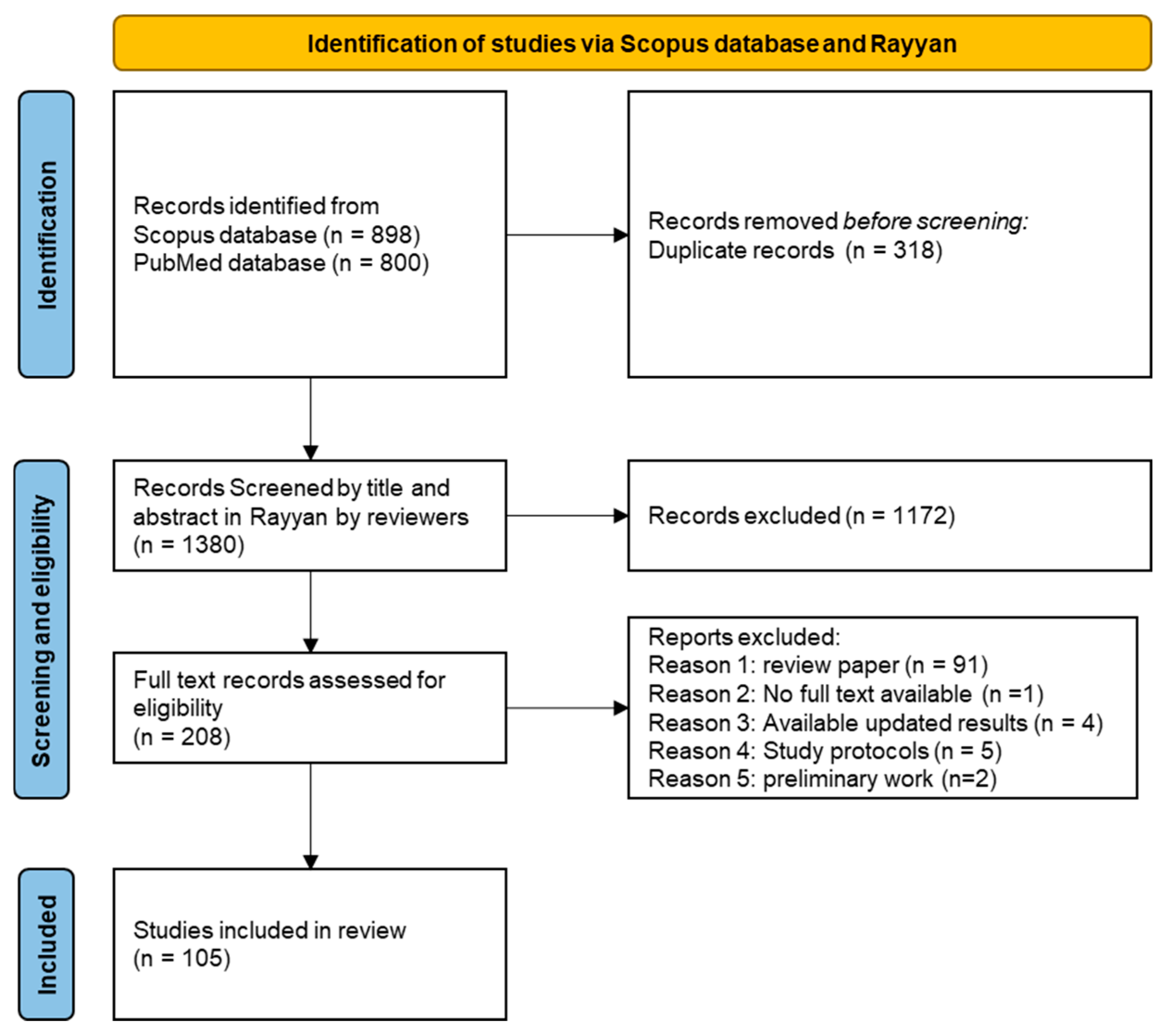
3.1. Selection of Sources of Evidence
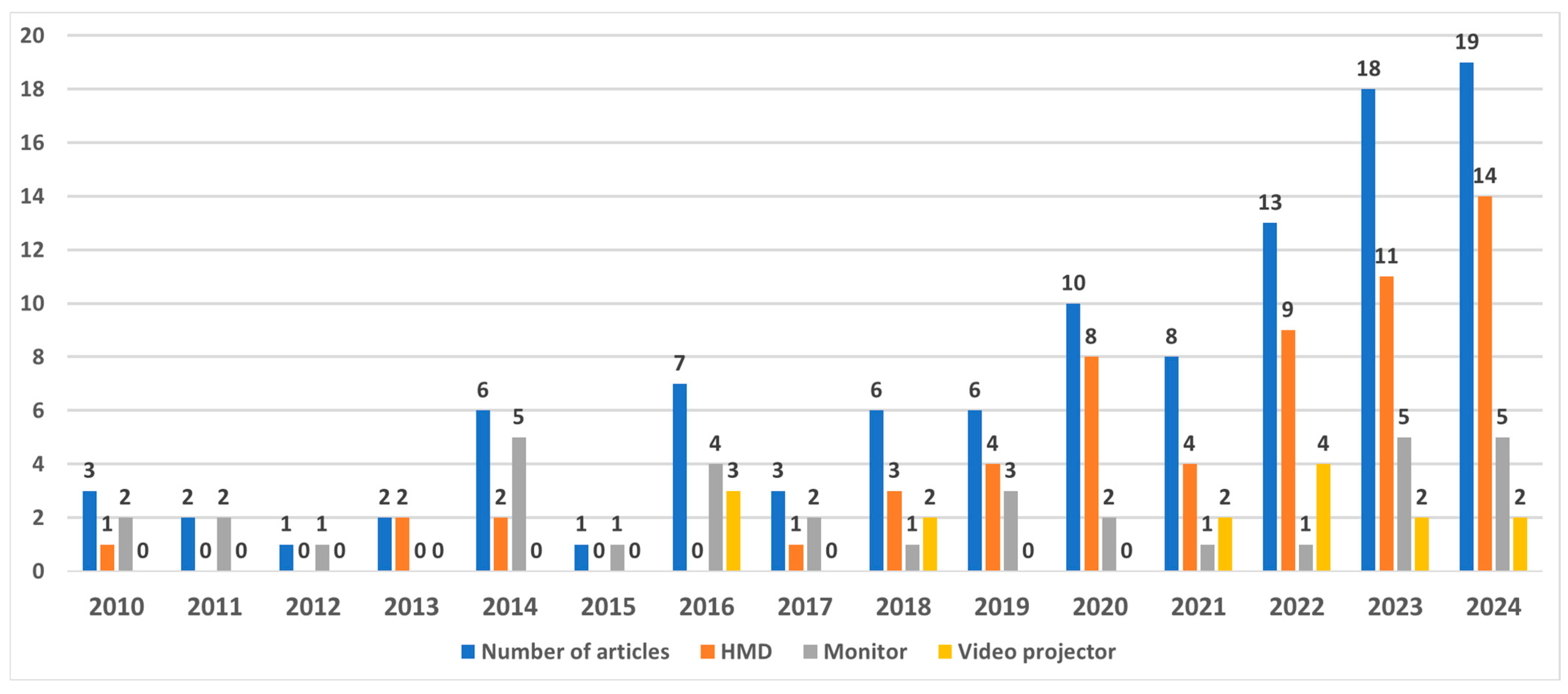
3.2. Characteristics of Sources of Evidence
3.3. Results of Individual Sources of Evidence
3.4. Synthesis of the Results
3.4.1. AR/MR Display Device
3.4.2. Source and Conveyed Information
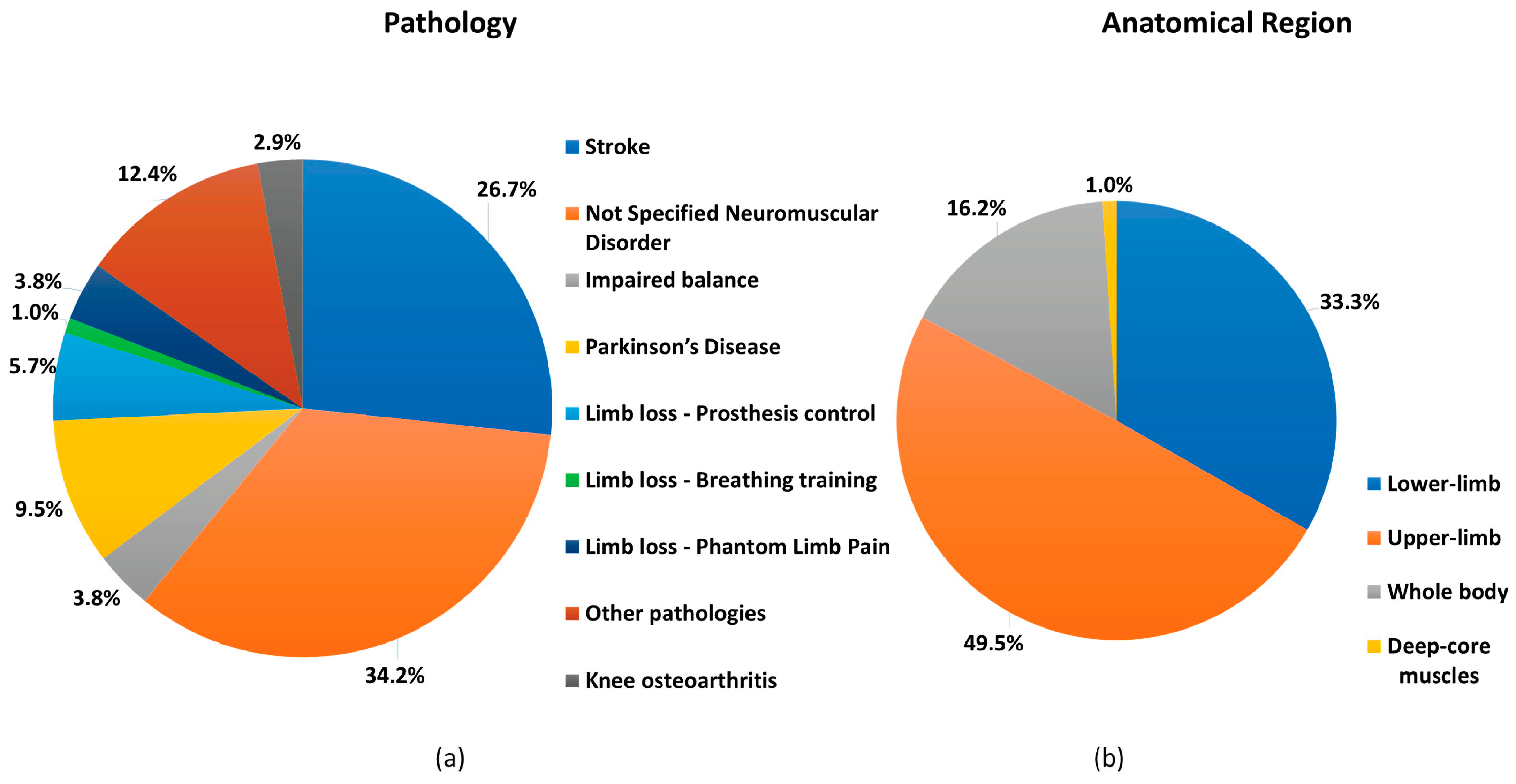
3.4.3. Pathology and Anatomical Region
3.4.4. Non-Specified Neuromuscular Disorders
3.4.5. Stroke Rehabilitation
3.4.6. Limb Loss
- Prosthesis Control: Five papers explored the use of AR/MR technology to enhance prosthetic limb control. Four papers [60,65,87,106] focused on upper limb prosthetics, and two [80,107] on the lower limb. Four studies [65,80,106,107] utilized HMDs to show the subject a virtual limb whose movement was controlled by the EMG signals from the residual muscles. One paper [60] used AR glasses to show a command window to control a virtual prosthesis. The interaction with the command window was realized by tracking the user’s head position. The user simultaneously received AR visual feedback about the command and, for example, grip strength or the degree of hand closure.
- Breathing Training: In one study [77], an AR headset was used to provide lower limb amputees with feedback about deep core muscle activity and thoracic excursion during breathing training for back pain reduction.
3.4.7. Parkinson’s Disease
3.4.8. Impaired Balance
3.4.9. Knee Osteoarthritis
3.4.10. Other Pathologies
- Cerebral Palsy [57]: visual cues indicative of walking speed were shown to the patient via smartglasses to improve walking capabilities.
- Cerebellar Ataxia [53]: two exergames were developed focusing on upper limb coordination. In the first game, participants had to move a virtual spaceship to different planets. The second game required following the spaceship’s square path with their hand, guided by a 3D wormhole visual that helps align hand-eye coordination, aiming to follow the wormhole’s central axis directly to the target.
- Ankle sprain [54]: an exergame for mobile devices was developed focusing on the lower limb, using Mobile Augmented Reality to deliver a range of motion exercises as well as monitor the user’s performance. In this game, the subject is seated with the edge of the heel on the floor whilst holding a mobile device and is instructed to pivot and mimic the foot based on the virtual cues displayed on the screen.
- Anterior Cruciate Ligament Reconstruction [81]: an AR-based telerehabilitation system was developed for patients recovering from Anterior Cruciate Ligament Reconstruction. The system provided real-time feedback and exercise tracking through a 3D motion capture camera, allowing patients to perform rehabilitation at home. A randomized controlled trial showed similar functional improvements to conventional rehabilitation, with faster quadriceps strength recovery in the AR group.
- Multiple Sclerosis [112]: an exergame was developed for individuals with Multiple Sclerosis to support upper limb rehabilitation. The game integrates bimanual tasks, requiring users to manipulate real objects while balancing virtual elements, aiming to improve motor coordination and functional abilities. Initial tests with healthy participants demonstrated feasibility, with future trials planned for patients with Multiple Sclerosis to assess therapeutic benefits.
- Pelvic Floor Dysfunction [84]: an exergame was developed for older women with pelvic floor dysfunction, incorporating platform-jumping mechanics and real-time motion tracking to support Pelvic Floor Dysfunction rehabilitation. The system provides interactive feedback to enhance motivation and adherence.
3.5. Usability and Acceptability Assessment
4. Discussion
4.1. How Is AR/MR Used in Rehabilitation?
4.2. AR/MR Display Technologies
4.3. Sensors Used to Add Augmented Information to the Real World
4.4. Target Pathology
4.5. Assessing Usability and Acceptance
4.6. Further Considerations
4.7. Future Directions in AR/MR Rehabilitation
- 1.
- Enhanced Treatment Assessment and Outcome Measures:
- Conduct rigorous comparative studies to evaluate the efficacy of AR/MR-based rehabilitation compared to traditional rehabilitation methods.
- Investigate the use of AR/MR in long-term rehabilitation treatments.
- Investigate the cost-effectiveness of AR/MR interventions in different clinical settings and patient populations.
- 2.
- Expanding Research into Specific Populations and Conditions:
- Extend studies to explore the application of AR/MR in the rehabilitation of specific patient populations and to address specific rehabilitation challenges, such as training of gait and upper limb function.
- 3.
- Addressing Medical device requirements, Visualization, and User Experience Challenges:
- Critically assess the suitability of off-the-shelf, consumer-grade hardware and commercial game engines for medical applications, given the stringent requirements and standards for medical devices.
- Develop innovative AR/MR display technologies to address current challenges and mitigate adverse effects associated with prolonged AR/MR use. This includes addressing limitations in the field of view, the Vergence–Accommodation conflict, the limited luminance/contrast, image registration accuracy, latency, and encumbrance.
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AR | Augmented reality |
| EMG | Electromyography |
| FOG | Freezing of gait |
| HMD | Head-mounted display |
| IMU | Inertial measurement unit |
| MR | Mixed reality |
| NSND | Not Specified Neuromuscular Disorders |
| PLP | Phantom limb pain |
| PRISMA-ScR | Systematic reviews and meta-analyses extension for scoping reviews |
| SLAM | Simultaneous localization and mapping |
| SUS | System usability scale |
| VR | Virtual reality |
| XR | Extended reality |
Appendix A
References
- Lederman, E. 14—Neuromuscular rehabilitation: Summary. In Neuromuscular Rehabilitation in Manual and Physical Therapy; Churchill Livingstone: Edinburgh, UK; Elsevier: Amsterdam, The Netherlands, 2010; pp. 169–171. [Google Scholar] [CrossRef]
- Ramesh, P.V.; Joshua, T.; Ray, P.; Devadas, A.K.; Raj, P.M.; Ramesh, S.V.; Ramesh, M.K.; Rajasekaran, R. Holographic elysium of a 4D ophthalmic anatomical and pathological metaverse with extended reality/mixed reality. Indian J. Ophthalmol. 2022, 70, 3116–3121. [Google Scholar] [PubMed]
- Ong, C.W.; Tan, M.C.J.; Lam, M.; Koh, V.T.C. Applications of Extended Reality in Ophthalmology: Systematic Review. J. Med. Internet Res. 2021, 23, e24152. [Google Scholar] [PubMed]
- Gazzoni, M.; Cerone, G.L. Augmented Reality Biofeedback for Muscle Activation Monitoring: Proof of Concept. In 8th European Medical and Biological Engineering Conference, Proceedings of the EMBEC 2020, Portorož, Slovenia, 29 November–3 December 2020; IFMBE Proceedings; Springer Science and Business Media Deutschland GmbH: Cham, Switzerland, 2021; pp. 143–150. [Google Scholar] [CrossRef]
- Milgram, P.; Kishino, F. A Taxonomy of Mixed Reality Visual Displays. IEICE Trans. Inf. Syst. 1994, E77-D, 1321–1329. Available online: https://search.ieice.org/bin/summary.php?id=e77-d_12_1321&category=D&year=1994&lang=E&abst= (accessed on 5 September 2023).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [PubMed]
- Devagiri, J.S.; Paheding, S.; Niyaz, Q.; Yang, X.; Smith, S. Augmented Reality and Artificial Intelligence in industry: Trends, tools, and future challenges. Expert Syst. Appl. 2022, 207, 118002. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [PubMed]
- Cadena, C.; Carlone, L.; Carrillo, H.; Latif, Y.; Scaramuzza, D.; Neira, J.; Reid, I.; Leonard, J.J. Past, Present, and Future of Simultaneous Localization and Mapping: Toward the Robust-Perception Age. IEEE Trans. Robot. 2016, 32, 1309–1332. [Google Scholar] [CrossRef]
- Vassallo, R.; Rankin, A.; Chen, E.C.S.; Peters, T.M. Hologram stability evaluation for Microsoft HoloLens. In Medical Imaging 2017: Image Perception, Observer Performance, and Technology Assessment, Proceedings of the SPIE MEDICAL IMAGING, Orlando, FL, USA, 11–16 February 2017; Kupinski, M.A., Nishikawa, R.M., Eds.; SPIE: Bellingham, WA, USA, 2017; p. 1013614. [Google Scholar] [CrossRef]
- Koroleva, E.S.; Tolmachev, I.V.; Alifirova, V.M.; Boiko, A.S.; Levchuk, L.A.; Loonen, A.J.M.; Ivanova, S.A. Serum BDNF’s Role as a Biomarker for Motor Training in the Context of AR-Based Rehabilitation after Ischemic Stroke. Brain Sci. 2020, 10, 623. [Google Scholar] [CrossRef]
- Guinet, A.-L.; Bouyer, G.; Otmane, S.; Desailly, E. Towards an AR game for walking rehabilitation: Preliminary study of the impact of augmented feedback modalities on walking speed. In Proceedings of the 2020 IEEE International Symposium on Mixed and Augmented Reality Adjunct (ISMAR-Adjunct), Recife, Brazil, 9–13 November 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 264–268. [Google Scholar] [CrossRef]
- Debarba, H.G.; de Oliveira, M.E.; Ladermann, A.; Chague, S.; Charbonnier, C. Augmented Reality Visualization of Joint Movements for Physical Examination and Rehabilitation. In Proceedings of the 2018 IEEE Conference on Virtual Reality and 3D User Interfaces (VR), Tuebingen/Reutlingen, Germany, 18–22 March 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 537–538. [Google Scholar] [CrossRef]
- Chang, W.-C.; Ko, L.-W.; Yu, K.-H.; Ho, Y.-C.; Chen, C.-H.; Jong, Y.-J.; Huang, Y.-P. EEG analysis of mixed-reality music rehabilitation system for post-stroke lower limb therapy. J. Soc. Inf. Disp. 2019, 27, 372–380. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.; Jo, S.; Lee, K.; Kim, J.; Song, C. Video augmented mirror therapy for upper extremity rehabilitation after stroke: A randomized controlled trial. J. Neurol. 2023, 270, 831–842. [Google Scholar] [PubMed]
- Correa-Agudelo, E.; Hernández, A.M.; Ferrin, C.; Gomez, J.D. ViLimbs: Improving phantom limb treatment through multisensory feedback. In CHI EA ’15, Proceedings of the 33rd Annual ACM Conference Extended Abstracts on Human Factors in Computing Systems, Seoul, Republic of Korea, 18–23 April 2015; Association for Computing Machinery: New York, NY, USA, 2015; Volume 18, pp. 1313–1318. [Google Scholar] [CrossRef]
- Yeo, S.M.; Lim, J.Y.; Do, J.G.; Lim, J.-Y.; Lee, J.I.; Hwang, J.H. Effectiveness of interactive augmented reality-based telerehabilitation in patients with adhesive capsulitis: Protocol for a multi-center randomized controlled trial. BMC Musculoskelet. Disord. 2021, 22, 386. [Google Scholar] [PubMed]
- van de Venis, L.; van de Warrenburg, B.P.C.; Weerdesteyn, V.; van Lith, B.J.H.; Geurts, A.C.H.; Nonnekes, J. Improving gait adaptability in patients with hereditary spastic paraplegia (Move-HSP): Study protocol for a randomized controlled trial. Trials 2021, 22, 32. [Google Scholar] [PubMed]
- Lendaro, E.; Hermansson, L.; Burger, H.; Van Der Sluis, C.K.; McGuire, B.E.; Pilch, M.; Bunketorp-Käll, L.; Kulbacka-Ortiz, K.; Rignér, I.; Stockselius, A.; et al. Phantom motor execution as a treatment for phantom limb pain: Protocol of an international, double-blind, randomised controlled clinical trial. BMJ Open 2018, 8, e021039. [Google Scholar] [PubMed]
- Timmermans, C.; Roerdink, M.; van Ooijen, M.W.; Meskers, C.G.; Janssen, T.W.; Beek, P.J. Walking adaptability therapy after stroke: Study protocol for a randomized controlled trial. Trials 2016, 17, 425. [Google Scholar] [PubMed]
- Liston, M.; Genna, G.; Maurer, C.; Kikidis, D.; Gatsios, D.; Fotiadis, D.; Bamiou, D.E.; Pavlou, M. Investigating the feasibility and acceptability of the HOLOBalance system compared with standard care in older adults at risk for falls: Study protocol for an assessor blinded pilot randomised controlled study. BMJ Open 2021, 11, e039254. [Google Scholar] [PubMed]
- Rossano, C.; Terrier, P. Visually-guided gait training in paretic patients during the first rehabilitation phase: Study protocol for a randomized controlled trial. Trials 2016, 17, 523. [Google Scholar] [PubMed]
- Shim, G.Y.; Kim, E.H.; Lee, S.J.; Chang, C.B.; Lee, Y.S.; Lee, J.I.; Hwang, J.H.; Lim, J.-Y. Postoperative rehabilitation using a digital healthcare system in patients with total knee arthroplasty: A randomized controlled trial. Arch. Orthop. Trauma Surg. 2023, 143, 6361–6370. [Google Scholar] [CrossRef]
- Everard, G.; Burton, Q.; Van de Sype, V.; Bibentyo, T.N.; Auvinet, E.; Edwards, M.G.; Batcho, C.S.; Lejeune, T. Extended reality to assess post-stroke manual dexterity: Contrasts between the classic box and block test, immersive virtual reality with controllers, with hand-tracking, and mixed-reality tests. J. NeuroEng. Rehabil. 2024, 21, 36. [Google Scholar] [PubMed]
- Shim, G.Y.; Kim, E.H.; Baek, Y.J.; Chang, W.K.; Kim, B.R.; Oh, J.H.; Lee, J.I.; Hwang, J.H.; Lim, J.-Y. A randomized controlled trial of postoperative rehabilitation using digital healthcare system after rotator cuff repair. NPJ Digit. Med. 2023, 6, 95. [Google Scholar] [CrossRef] [PubMed]
- Pavlou, M.; Flavell, C.A.; Gourtani, F.M.; Nikitas, C.; Kikidis, D.; Bibas, A.; Gatsios, D.; Tsakanikas, V.; Fotiadis, D.I.; Koutsouris, D.; et al. Feasibility and acceptability of the HOLObalance telerehabilitation system compared with standard care for older adults at risk of falls: The HOLOBalance assessor blinded pilot randomised controlled study. Age Ageing 2024, 53, afae214. [Google Scholar] [CrossRef]
- Ahn, D.; Chung, H.; Lee, H.-W.; Kang, K.; Ko, P.-W.; Kim, N.S.; Park, T. Smart Gait-Aid Glasses for Parkinson’s Disease Patients. IEEE Trans. Biomed. Eng. 2017, 64, 2394–2402. [Google Scholar] [PubMed]
- Aung, Y.M.; Al-Jumaily, A. Real time biosignal-Driven illusion system for upper limb rehabilitation. In Biomedical Engineering/817: Robotics Applications, Proceedings of the IASTED International Conference on Biomedical Engineering, Zurich, Switzerland, 23–25 June 2014; Acta Press: Calgary, AB, Canada, 2014; pp. 286–293. [Google Scholar] [CrossRef]
- Barioni, R.R.; Chaves, T.M.; Figueiredo, L.; Teichrieb, V.; Neto, E.V.; Da Gama, A.E.F. ARkanoidAR: An Augmented Reality System to Guide Biomechanical Movements at Sagittal Plane. In Proceedings of the 2017 19th Symposium on Virtual and Augmented Reality (SVR), Curitiba, Brazil, 1–4 November 2017; IEEE: Piscataway, NJ, USA, 2017; pp. 207–214. [Google Scholar] [CrossRef]
- Bennour, S.; Ulrich, B.; Legrand, T.; Jolles, B.M.; Favre, J. A gait retraining system using augmented-reality to modify footprint parameters: Effects on lower-limb sagittal-plane kinematics. J. Biomech. 2018, 66, 26–35. [Google Scholar] [PubMed]
- Blomqvist, S.; Seipel, S.; Engström, M. Using augmented reality technology for balance training in the older adults: A feasibility pilot study. BMC Geriatr. 2021, 21, 144. [Google Scholar] [PubMed]
- Boucher, D.B.; Roberts-South, A.; Garcia, A.A.; Katchabaw, M.; Jog, M.S. Immersive augmented reality: Investigating a new tool for Parkinson disease rehabilitation. In Proceedings of the 2013 6th International IEEE/EMBS Conference on Neural Engineering (NER), San Diego, CA, USA, 6–8 November 2013; pp. 1570–1573. [Google Scholar] [CrossRef]
- Burke, J.W.; McNeill, M.D.J.; Charles, D.K.; Morrow, P.J.; Crosbie, J.H.; McDonough, S.M. Augmented reality games for upper-limb stroke rehabilitation. In Proceedings of the 2010 Second International Conference on Games and Virtual Worlds for Serious Applications, Braga, Portugal, 25–26 March 2010; pp. 75–78. [Google Scholar] [CrossRef]
- Cavalcanti, V.C.; de Santana Ferreira, M.I.; Teichrieb, V.; Barioni, R.R.; Correia, W.F.M.; Da Gama, A.E.F. Usability and effects of text, image and audio feedback on exercise correction during augmented reality based motor rehabilitation. Comput. Graph. 2019, 85, 100–110. [Google Scholar] [CrossRef]
- Chen, Y.; Baran, M.; Sundaram, H.; Rikakis, T. A low cost, adaptive mixed reality system for home-based stroke rehabilitation. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 1827–1830. [Google Scholar] [PubMed]
- Colomer, C.; Llorens, R.; Noé, E.; Alcañiz, M. Effect of a mixed reality-based intervention on arm, hand, and finger function on chronic stroke. J. NeuroEng. Rehabil. 2016, 13, 45. [Google Scholar] [PubMed]
- Condino, S.; Turini, G.; Viglialoro, R.; Gesi, M.; Ferrari, V. Wearable Augmented Reality Application for Shoulder Rehabilitation. Electronics 2019, 8, 1178. [Google Scholar] [CrossRef]
- Da Gama, A.E.F.; Chaves, T.M.; Figueiredo, L.S.; Baltar, A.; Meng, M.; Navab, N.; Teichrieb, V.; Fallavollita, P. MirrARbilitation: A clinically-related gesture recognition interactive tool for an AR rehabilitation system. Comput. Methods Programs Biomed. 2016, 135, 105–114. [Google Scholar] [PubMed]
- de Assis, G.A.; Corrêa, A.G.D.; Martins, M.B.R.; Pedrozo, W.G.; Lopes R de, D. An augmented reality system for upper-limb post-stroke motor rehabilitation: A feasibility study. Disabil. Rehabil. Assist. Technol. 2016, 11, 521–528. [Google Scholar] [PubMed]
- De Cecco, M.; Luchetti, A.; Butaslac, I.; Pilla, F.; Guandalini, G.M.A.; Bonavita, J.; Mazzucato, M.; Hirokazu, K. Sharing Augmented Reality between a Patient and a Clinician for Assessment and Rehabilitation in Daily Living Activities. Information 2023, 14, 204. [Google Scholar] [CrossRef]
- de Crignis, A.C.; Ruhnau, S.T.; Hösl, M.; Lefint, J.; Amberger, T.; Dressnandt, J.; Brunner, H.; Müller, F. Robotic arm training in neurorehabilitation enhanced by augmented reality—A usability and feasibility study. J. Neuroeng. Rehabil. 2023, 20, 105. [Google Scholar] [CrossRef] [PubMed]
- De Leon, N.I.; Bhatt, S.K.; Al-Jumaily, A. Augmented reality game based multi-usage rehabilitation therapist for stroke patients. Int. J. Smart Sens. Intell. Syst. 2014, 7, 1044–1058. [Google Scholar] [CrossRef]
- Debarba, H.G.; Oliveira ME de Ladermann, A.; Chague, S.; Charbonnier, C. Augmented Reality Visualization of Joint Movements for Rehabilitation and Sports Medicine. In Proceedings of the 2018 20th Symposium on Virtual and Augmented Reality (SVR), Foz do Iguacu, Brazil, 28–30 October 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 114–121. [Google Scholar] [CrossRef]
- Duff, M.; Chen, Y.; Cheng, L.; Liu, S.M.; Blake, P.; Wolf, S.L.; Rikakis, T. Adaptive mixed reality rehabilitation improves quality of reaching movements more than traditional reaching therapy following stroke. Neurorehabilit. Neural Repair 2013, 27, 306–315. [Google Scholar] [CrossRef] [PubMed]
- Enam, N.; Veerubhotla, A.; Ehrenberg, N.; Kirshblum, S.; Nolan, K.J.; Pilkar, R. Augmented-reality guided treadmill training as a modality to improve functional mobility post-stroke: A proof-of-concept case series. Top. Stroke Rehabil. 2021, 28, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Escalona, F.; Martinez-Martin, E.; Cruz, E.; Cazorla, M.; Gomez-Donoso, F. EVA: EVAluating at-home rehabilitation exercises using augmented reality and low-cost sensors. Virtual Real. 2020, 24, 567–581. [Google Scholar] [CrossRef]
- Espay, A.J.; Baram, Y.; Dwivedi, A.K.; Shukla, R.; Gartner, M.; Gaines, L.; Duker, A.P.; Revilla, F.J. At-home training with closed-loop augmented-reality cueing device for improving gait in patients with Parkinson disease. J. Rehabil. Res. Dev. 2010, 47, 573–582. [Google Scholar] [CrossRef] [PubMed]
- Evans, E.; Dass, M.; Muter, W.M.; Tuthill, C.; Tan, A.Q.; Trumbower, R.D. A Wearable Mixed Reality Platform to Augment Overground Walking: A Feasibility Study. Front. Hum. Neurosci. 2022, 16, 868074. [Google Scholar] [CrossRef]
- Fang, Y.; Luo, Z.; Huang, F.; Wang, Z.; Li, D.; Hua, X. Developing a Mixed Reality-Based Game for Post-Stroke Motor Rehabilitation: Combining Training and Assessment. In Proceedings of the 2023 9th International Conference on Virtual Reality (ICVR), Xianyang, China, 12–14 May 2023; IEEE: Piscataway, NJ, USA, 2023; pp. 393–399. [Google Scholar] [CrossRef]
- Franzò, M.; Pica, A.; Pascucci, S.; Serrao, M.; Marinozzi, F.; Bini, F. A Proof of Concept Combined Using Mixed Reality for Personalized Neurorehabilitation of Cerebellar Ataxic Patients. Sensors 2023, 23, 1680. [Google Scholar] [CrossRef] [PubMed]
- Franzo, M.; Pascucci, S.; Serrao, M.; Marinozzi, F.; Bini, F. Breakthrough in Occupational Therapy with Mixed-Reality exergaming for cerebellar ataxia patients. In Proceedings of the 2023 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Jeju, Republic of Korea, 14–16 June 2023; IEEE: Piscataway, NJ, USA, 2023. [Google Scholar] [CrossRef]
- Garcia, J.A.; Navarro, K.F. The mobile RehAppTM: An AR-based mobile game for ankle sprain rehabilitation. In Proceedings of the 2014 IEEE 3rd International Conference on Serious Games and Applications for Health (SeGAH), Rio de Janeiro, Brazil, 14–16 May 2014; IEEE: Piscataway, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Garcia Hernandez, N.V.; Buccelli, S.; Laffranchi, M.; de Michieli, L. Mixed Reality-based Exergames for Upper Limb Robotic Rehabilitation. In HRI ’23, Proceedings of the Companion of the 2023 ACM/IEEE International Conference on Human-Robot Interaction, Stockholm, Sweden, 13–16 March 2023; Association for Computing Machinery: New York, NY, USA, 2023; pp. 447–451. [Google Scholar] [CrossRef]
- Gmez-Portes, C.; Carneros-Prado, D.; Albusac, J.; Castro-Schez, J.J.; Glez-Morcillo, C.; Vallejo, D. PhyRe Up! A System Based on Mixed Reality and Gamification to Provide Home Rehabilitation for Stroke Patients. IEEE Access 2021, 9, 139122–139137. [Google Scholar] [CrossRef]
- Guinet, A.-L.; Bouyer, G.; Otmane, S.; Desailly, E. Visual Feedback in Augmented Reality to Walk at Predefined Speed Cross-Sectional Study Including Children with Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 2322–2331. [Google Scholar] [PubMed]
- Gulcan, K.; Guclu-Gunduz, A.; Yasar, E.; Ar, U.; Sucullu Karadag, Y.; Saygili, F. The effects of augmented and virtual reality gait training on balance and gait in patients with Parkinson’s disease. Acta Neurol. Belg. 2023, 123, 1917–1925. [Google Scholar] [PubMed]
- Ham, Y.; Yang, D.S.; Choi, Y.; Shin, J.H. Effectiveness of mixed reality-based rehabilitation on hands and fingers by individual finger-movement tracking in patients with stroke. J. NeuroEng. Rehabil. 2024, 21, 140. [Google Scholar] [PubMed]
- Hazubski, S.; Hoppe, H.; Otte, A. Electrode-free visual prosthesis/exoskeleton control using augmented reality glasses in a first proof-of-technical-concept study. Sci. Rep. 2020, 10, 16279. [Google Scholar] [PubMed]
- He, Y.; Sawada, I.; Fukuda, O.; Shima, R.; Yamaguchi, N.; Okumura, H. Development of an evaluation system for upper limb function using AR technology. In GECCO ’18, Proceedings of the Genetic and Evolutionary Computation Conference, Kyoto, Japan, 15–19 July 2018; Association for Computing Machinery: New York, NY, USA, 2018; pp. 1835–1840. [Google Scholar] [CrossRef]
- Held, J.P.O.; Yu, K.; Pyles, C.; Veerbeek, J.M.; Bork, F.; Heining, S.-M.; Navab, N.; Luft, A.R. Augmented Reality–Based Rehabilitation of Gait Impairments: Case Report. JMIR mHealth uHealth 2020, 8, e17804. [Google Scholar] [PubMed]
- Hoda, M.; Dong, H.; Ahmed, D.; El Saddik, A. Cloud-based rehabilitation exergames system. In Proceedings of the 2014 IEEE International Conference on Multimedia and Expo Workshops (ICMEW), Chengdu, China, 14–18 July 2014; IEEE: Piscataway, NJ, USA, 2014. [Google Scholar] [CrossRef]
- Hossain, M.S.; Hardy, S.; Alamri, A.; Alelaiwi, A.; Hardy, V.; Wilhelm, C. AR-based serious game framework for post-stroke rehabilitation. Multimed. Syst. 2016, 22, 659–674. [Google Scholar] [CrossRef]
- Hunt, C.L.; Sun, Y.; Wang, S.; Shehata, A.W.; Hebert, J.S.; Gonzalez-Fernandez, M.; Kaliki, R.R.; Thakor, N.V. Limb loading enhances skill transfer between augmented and physical reality tasks during limb loss rehabilitation. J. NeuroEng. Rehabil. 2023, 20, 16. [Google Scholar] [PubMed]
- Im, D.J.; Ku, J.; Kim, Y.J.; Cho, S.; Cho, Y.K.; Lim, T.; Lee, H.S.; Kim, H.J.; Kang, Y.J. Utility of a Three-Dimensional Interactive Augmented Reality Program for Balance and Mobility Rehabilitation in the Elderly: A Feasibility Study. Ann. Rehabil. Med. 2015, 39, 462–472. [Google Scholar] [CrossRef]
- Janssen, S.; de Ruyter van Steveninck, J.; Salim, H.S.; Cockx, H.M.; Bloem, B.R.; Heida, T.; van Wezel, R.J.A. The Effects of Augmented Reality Visual Cues on Turning in Place in Parkinson’s Disease Patients with Freezing of Gait. Front. Neurol. 2020, 11, 185. [Google Scholar] [CrossRef]
- Jeon, S.; Kim, J. Effects of Augmented-Reality-Based Exercise on Muscle Parameters, Physical Performance, and Exercise Self-Efficacy for Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 3260. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Monge, J.; Postolache, O.; Niu, W. Augmented Reality with Application in Physical Rehabilitation. In Proceedings of the 2019 International Conference on Sensing and Instrumentation in IoT Era (ISSI), Lisbon, Portugal, 29–30 August 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1–6. [Google Scholar] [CrossRef]
- Jung, G.U.; Moon, T.H.; Park, G.W.; Lee, J.Y.; Lee, B.H. Use of augmented reality-based training with EMG-triggered functional electric stimulation in stroke rehabilitation. J. Phys. Ther. Sci. 2013, 25, 147–151. [Google Scholar] [CrossRef]
- Karatsidis, A.; Richards, R.E.; Konrath, J.M.; Van Den Noort, J.C.; Schepers, H.M.; Bellusci, G.; Harlaar, J.; Veltink, P.H. Validation of wearable visual feedback for retraining foot progression angle using inertial sensors and an augmented reality headset. J. Neuroeng. Rehabil. 2018, 15, 78. [Google Scholar] [PubMed]
- Ko, L.-W.; Stevenson, C.; Chang, W.-C.; Yu, K.-H.; Chi, K.-C.; Chen, Y.-J.; Chen, C.-H. Integrated Gait Triggered Mixed Reality and Neurophysiological Monitoring as a Framework for Next-Generation Ambulatory Stroke Rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 2435–2444. [Google Scholar] [PubMed]
- Kong, B.S.H.; Lim, W.N. Advancing Stroke Rehabilitation: Designing an Augmented Reality System for Enhanced User Engagement and Recovery. In Proceedings of the 2024 IEEE 14th Symposium on Computer Applications & Industrial Electronics (ISCAIE), Penang, Malaysia, 24–25 May 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 440–445. [Google Scholar] [CrossRef]
- Koroleva, E.S.; Kazakov, S.D.; Tolmachev, I.V.; Loonen, A.J.M.; Ivanova, S.A.; Alifirova, V.M. Clinical Evaluation of Different Treatment Strategies for Motor Recovery in Poststroke Rehabilitation during the First 90 Days. J. Clin. Med. 2021, 10, 3718. [Google Scholar] [CrossRef]
- Ku, J.; Kim, Y.J.; Cho, S.; Lim, T.; Lee, H.S.; Kang, Y.J. Three-Dimensional Augmented Reality System for Balance and Mobility Rehabilitation in the Elderly: A Randomized Controlled Trial. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 132–141. [Google Scholar] [PubMed]
- Kuijpers, R.; Smulders, E.; Groen, B.E.; Smits-Engelsman, B.C.M.; Nijhuis-van der Sanden, M.W.G.; Weerdesteyn, V. Walking adaptability improves after treadmill training in children with Developmental Coordination Disorder: A proof-of-concept study. Gait Posture 2022, 92, 258–263. [Google Scholar] [PubMed]
- Lancere, L.; Jürgen, M.; Gapeyeva, H. Mixed reality and sensor real-time feedback to increase muscle engagement during deep core exercising. Virtual Real. 2023, 27, 3435–3449. [Google Scholar] [CrossRef]
- Lee, E.-Y.; Tran, V.T.; Kim, D. A Novel Head Mounted Display Based Methodology for Balance Evaluation and Rehabilitation. Sustainability 2019, 11, 6453. [Google Scholar] [CrossRef]
- Li, C.; Song, X.; Chen, S.; Wang, C.; He, J.; Zhang, Y.; Xu, S.; Yan, Z.; Jia, J.; Shull, P. Long-term Effectiveness and Adoption of a Cellphone Augmented Reality System on Patients with Stroke: Randomized Controlled Trial. JMIR Serious Games 2021, 9, e30184. [Google Scholar] [CrossRef]
- Lim, G.; Youn, H.; Kim, H.; Jeong, H.; Cho, J.; Lee, S.; Pak, C.; Kwon, S. Impact of Mixed Reality-Based Rehabilitation on Muscle Activity in Lower-Limb Amputees: An EMG Analysis. IEEE Access 2024, 12, 106415–106431. [Google Scholar] [CrossRef]
- Lim, J.Y.; Yu, H.J.; Kim, S.H.; Lee, J.I.; Lim, J.Y.; Wang, J.H.; Hwang, J.H. Effectiveness of In-Home, Augmented Reality–Based Telerehabilitation After Anterior Cruciate Ligament Reconstruction: A Randomized Controlled Trial. Orthop. J. Sports Med. 2024, 12. [Google Scholar] [CrossRef]
- Lin, J.K.; Cheng, P.H.; Su, Y.; Luh, J.J.; Wang, S.Y.; Lin, H.W.; Hou, H.C.; Chiang, W.C.; Wu, S.W.; Su, M.J. Augmented reality serious game framework for rehabilitation with personal health records. In Proceedings of the 2011 IEEE 13th International Conference on e-Health Networking, Applications and Services, Columbia, MO, USA, 13–15 June 2011; pp. 197–200. [Google Scholar] [CrossRef]
- Liu, J.; Mei, J.; Zhang, X.; Lu, X.; Huang, J. Augmented reality-based training system for hand rehabilitation. Multimed. Tools Appl. 2017, 76, 14847–14867. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, Z.; Chen, Z.; Zhang, Y.; Diao, Y.; Liu, G. A Female Pelvic Floor Dysfunction Rehealthy Training Exergame Designed for the Older Women. In CSCW Companion ’24, Proceedings of the Companion Publication of the 2024 Conference on Computer-Supported Cooperative Work and Social Computing, San Jose, Costa Rica, 9–13 November 2024; Association for Computing Machinery: New York, NY, USA, 2024; pp. 398–402. [Google Scholar] [CrossRef]
- Luchetti, A.; Parolin, E.; Butaslac, I.; Fujimoto, Y.; Kanbara, M.; Bosetti, P.; De Cecco, M.; Kato, H. Stepping over Obstacles with Augmented Reality based on Visual Exproprioception. In Proceedings of the 2020 IEEE International Symposium on Mixed and Augmented Reality Adjunct (ISMAR-Adjunct), Recife, Brazil, 9–13 November 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 96–101. [Google Scholar] [CrossRef]
- Mahmood, N.; Anello, A.; Kim, J.W.; Kim, K.; Smith, B.E.; Ridgel, A. Haptic-Enhanced Mixed Reality for Upper Limb Rehabilitation in Parkinson’s Disease. In Proceedings of the 2024 46th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 15–19 July 2024; IEEE: Piscataway, NJ, USA, 2024. [Google Scholar] [CrossRef]
- Markovic, M.; Dosen, S.; Cipriani, C.; Popovic, D.; Farina, D. Stereovision and augmented reality for closed-loop control of grasping in hand prostheses. J. Neural Eng. 2014, 11, 046001. [Google Scholar] [PubMed]
- McCarty, T.; Surender, S.; Shu, C.; Huang, Z.; Chen, J.; Kokkoni, E. Integrating Mixed Reality and Body Weight Support Technology for Immersive Pediatric Rehabilitation. In Proceedings of the 2024 46th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 15–19 July 2024; IEEE: Piscataway, NJ, USA, 2024. [Google Scholar] [CrossRef]
- Miller, D.A.L.; Ogata, T.; Sasabe, G.; Shan, L.; Tsumura, N.; Miyake, Y. Spatiotemporal Gait Guidance Using Audiovisual Cues of Synchronized Walking Avatar in Augmented Reality. IEEE Access 2022, 10, 90498–90506. [Google Scholar] [CrossRef]
- Miller, D.A.L.; Uchitomi, H.; Miyake, Y. Effects of Gradual Spatial and Temporal Cues Provided by Synchronized Walking Avatar on Elderly Gait. Appl. Sci. 2024, 14, 8374. [Google Scholar] [CrossRef]
- Mousavi Hondori, H.; Khademi, M.; Dodakian, L.; McKenzie, A.; Lopes, C.V.; Cramer, S.C. Choice of Human–Computer Interaction Mode in Stroke Rehabilitation. Neurorehabilit. Neural Repair 2016, 30, 258–265. [Google Scholar] [PubMed]
- Nam, J.-Y.; Lee, S.-H.; Song, W.-K. Comparison of Reaching Motion in Mixed Reality Headset and End-effector-based Robotic Arm with Flat Panel Display. In Proceedings of the 2022 9th IEEE RAS/EMBS International Conference for Biomedical Robotics and Biomechatronics (BioRob), Seoul, Republic of Korea, 21–24 August 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 1–6. [Google Scholar] [CrossRef]
- Nam, Y.-G.; Park, S.Y.; Kwon, B.S. Rehabilitation Exercise Using a Smart-Bar Device with Augmented Reality Guide Function. Int. J. Precis. Eng. Manuf. 2023, 24, 1263–1270. [Google Scholar] [CrossRef]
- Nekar, D.M.; Lee, D.Y.; Hong, J.H.; Kim, J.S.; Kim, S.G.; Nam, Y.G.; Yu, J.H. Effects of Pseudo-Weight Resistance Training Using Mixed-Reality Technology on Muscle Activation in Healthy Adults: A Preliminary Study. Appl. Sci. 2023, 13, 10021. [Google Scholar] [CrossRef]
- Ortiz-Catalan, M.; Guðmundsdóttir, R.A.; Kristoffersen, M.B.; Zepeda-Echavarria, A.; Caine-Winterberger, K.; Kulbacka-Ortiz, K.; Widehammar, C.; Eriksson, K.; Stockselius, A.; Ragnö, C.; et al. Phantom motor execution facilitated by machine learning and augmented reality as treatment for phantom limb pain: A single group, clinical trial in patients with chronic intractable phantom limb pain. Lancet 2016, 388, 2885–2894. [Google Scholar] [PubMed]
- Pezzera, M.; Chitti, E.; Borghese, N.A. MIRARTS: A mixed reality application to support postural rehabilitation. In Proceedings of the 2020 IEEE 8th International Conference on Serious Games and Applications for Health (SeGAH), Vancouver, BC, Canada, 12–14 August 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 1–7. [Google Scholar] [CrossRef]
- Pillai, A.; Sunny, M.S.H.; Shahria, M.T.; Banik, N.; Rahman, M.H. Gamification of Upper Limb Rehabilitation in Mixed-Reality Environment. Appl. Sci. 2022, 12, 12260. [Google Scholar] [CrossRef]
- Pinto-Fernandez, D.; Gomez, M.; Rodrigues, C.; Rojo, A.; Raya, R.; Rocon, E.; Moreno, J.C.; Torricelli, D. Augmented Reality Feedback for Exoskeleton-Assisted Walking. A Feasibility Study. In Proceedings of the 2023 International Conference on Rehabilitation Robotics (ICORR), Singapore, 24–28 September 2023; IEEE Computer Society: Washington, DC, USA, 2023. [Google Scholar] [PubMed]
- Pisano, F.; Mellace, D.; Fugatti, A.; Aiello, E.N.; Diotti, S.; Curti, B.; Giust, A.; Marfoli, A.; Perin, C.; De Sandi, A.; et al. Cerebellar tDCS combined with augmented reality treadmill for freezing of gait in Parkinson’s disease: A randomized controlled trial. J. NeuroEng. Rehabil. 2024, 21, 173. [Google Scholar] [CrossRef]
- Prahm, C.; Bressler, M.; Eckstein, K.; Kuzuoka, H.; Daigeler, A.; Kolbenschlag, J. Developing a wearable Augmented Reality for treating phantom limb pain using the Microsoft Hololens 2. In AHs ’22, Proceedings of the Augmented Humans International Conference 2022, Kashiwa, Japan, 13–15 March 2022; Association for Computing Machinery: New York, NY, USA, 2022; pp. 309–312. [Google Scholar] [CrossRef]
- Retzinger, G.R.; Golbarg, B.; Pham, W.T.; Lachica, I.J.; Chan, T.; Hinkel-Lipsker, J.W. Holographic Hintways: A systems feasibility and usability study of augmented reality cueing for gait adaptation. Gait Posture 2024, 107, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, J.; D’Antona, A.; Proto, A.; Piva, G.; Lamberti, N.; Bonfè, M.; Farsoni, S. A Framework Integrating Augmented Reality and Wearable Sensors for the Autonomous Execution of Rehabilitation Exercises. Electronics 2023, 12, 4958. [Google Scholar] [CrossRef]
- Roumpi, M.; Gatsios, D.; Tsakanikas, V.D.; Tsiouris, K.M.; Georga, E.I.; Bamiou, D.-E.; Pavlou, M.; Nikitas, C.; Kikidis, D.; Walz, I.; et al. Analysis of the sentiments of the participants in a clinical study to evaluate a balance rehabilitation intervention delivered by a Virtual Coach. In Proceedings of the 2022 IEEE 21st Mediterranean Electrotechnical Conference (MELECON), Palermo, Italy, 14–16 June 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 103–107. [Google Scholar] [CrossRef]
- Scheermesser, M.; Baumgartner, D.; Nast, I.; Bansi, J.; Kool, J.; Bischof, P.; Bauer, C.M. Therapists and patients perceptions of a mixed reality system designed to improve trunk control and upper extremity function. Sci. Rep. 2024, 14, 6598. [Google Scholar] [CrossRef] [PubMed]
- Sekhavat, Y.A.; Namani, M.S. Projection-Based AR: Effective Visual Feedback in Gait Rehabilitation. IEEE Trans. Hum.-Mach. Syst. 2018, 48, 626–636. [Google Scholar] [CrossRef]
- Sharma, A.; Hunt, C.L.; Maheshwari, A.; Osborn, L.; Levay, G.; Kaliki, R.R.; Soares, A.B.; Thakor, N. A Mixed-Reality Training Environment for Upper Limb Prosthesis Control. In Proceedings of the 2018 IEEE Biomedical Circuits and Systems Conference (BioCAS), Cleveland, OH, USA, 17–19 October 2018; IEEE: Piscataway, NJ, USA, 2018; pp. 1–4. [Google Scholar] [CrossRef]
- Shim, W.; Kim, H.; Lim, G.; Lee, S.; Kim, H.; Hwang, J.; Lee, E.; Cho, J.; Jeong, H.; Pak, C.; et al. Implementation of the XR Rehabilitation Simulation System for the Utilization of Rehabilitation with Robotic Prosthetic Leg. Appl. Sci. 2022, 12, 12659. [Google Scholar] [CrossRef]
- Sousa, M.; Vieira, J.; Medeiros, D.; Arsénio, A.; Jorge, J. SleeveAR: Augmented reality for rehabilitation using realtime feedback. In IUI ’16, Proceedings of the 21st International Conference on Intelligent User Interfaces, Sonoma, CA, USA, 7–10 March 2016; Association for Computing Machinery: New York, NY, USA, 2016; pp. 175–185. [Google Scholar] [CrossRef]
- Tada, K.; Kutsuzawa, K.; Owaki, D.; Hayashibe, M. Quantifying Motor and Cognitive Function of the Upper Limb Using Mixed Reality Smartglasses. In Proceedings of the 2022 44th Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Glasgow, UK, 11–15 July 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 2556–2559. [Google Scholar] [PubMed]
- Tada, K.; Sorimachi, Y.; Kutsuzawa, K.; Owaki, D.; Hayashibe, M. Integrated Quantitative Evaluation of Spatial Cognition and Motor Function with HoloLens Mixed Reality. Sensors 2024, 24, 528. [Google Scholar] [CrossRef] [PubMed]
- Tan, G.; Uchitomi, H.; Isobe, R.; Miyake, Y. Sense of embodiment with synchronized avatar during walking in mixed reality. Sci. Rep. 2024, 14, 21198. [Google Scholar] [CrossRef]
- Tanda, M.; Prattico, F.G.; Podda, J.; Grange, E.; Brichetto, G.; De Michieli, L.; Lamberti, F.; Barresi, G. Rehabilitative Exergaming in Multiple Sclerosis: Bimanual Tasks in Mixed Reality. In Proceedings of the 2024 IEEE Gaming, Entertainment, and Media Conference (GEM), Turin, Italy, 5–7 June 2024; IEEE: Piscataway, NJ, USA, 2024. [Google Scholar] [CrossRef]
- Thinh, N.T.; Quoc, N.A.; Tam Toan, N.V.; Luc, T.T. Implementation of Rehabilitation Platform based on Augmented Reality Technology. In Proceedings of the 2021 21st International Conference on Control, Automation and Systems (ICCAS), Jeju, Republic of Korea, 12–15 October 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 1926–1931. [Google Scholar] [CrossRef]
- Thøgersen, M.; Andoh, J.; Milde, C.; Graven-Nielsen, T.; Flor, H.; Petrini, L. Individualized Augmented Reality Training Reduces Phantom Pain and Cortical Reorganization in Amputees: A Proof of Concept Study. J. Pain 2020, 21, 1257–1269. [Google Scholar] [PubMed]
- Timmermans, C.; Roerdink, M.; Meskers, C.G.M.; Beek, P.J.; Janssen, T.W.J. Walking-adaptability therapy after stroke: Results of a randomized controlled trial. Trials 2021, 22, 923. [Google Scholar] [CrossRef] [PubMed]
- Trojan, J.; Diers, M.; Fuchs, X.; Bach, F.; Bekrater-Bodmann, R.; Foell, J.; Kamping, S.; Rance, M.; Maaß, H.; Flor, H. An augmented reality home-training system based on the mirror training and imagery approach. Behav. Res. Methods 2014, 46, 634–640. [Google Scholar] [CrossRef] [PubMed]
- Tykhyi, R.; Tsapiv, Y.; Dyvak, M.; Popovych, D.; Havrylenko, A.; Husieva, T. Software System for Supporting Art Therapy Processes using Augmented Reality Technologies. In Proceedings of the 2024 14th International Conference on Advanced Computer Information Technologies (ACIT), Ceske Budejovice, Czech Republic, 19–21 September 2024; IEEE: Piscataway, NJ, USA, 2024; pp. 660–664. [Google Scholar] [CrossRef]
- Vaida, C.; Rus, G.; Tucan, P.; Machado, J.; Pisla, A.; Zima, I.; Birlescu, I.; Pisla, D. Enhancing Robotic-Assisted Lower Limb Rehabilitation Using Augmented Reality and Serious Gaming. Appl. Sci. 2024, 14, 12029. [Google Scholar] [CrossRef]
- van de Venis, L.; van de Warrenburg, B.; Weerdesteyn, V.; Geurts, A.C.H.; Nonnekes, J. Gait-Adaptability Training in People with Hereditary Spastic Paraplegia: A Randomized Clinical Trial. Neurorehabilit. Neural Repair 2023, 37, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Viglialoro, R.M.; Turini, G.; Carbone, M.; Condino, S.; Mamone, V.; Coluccia, N.; Dell’Agli, S.; Morucci, G.; Ryskalin, L.; Ferrari, V.; et al. A Projected AR Serious Game for Shoulder Rehabilitation Using Hand-Finger Tracking and Performance Metrics: A Preliminary Study on Healthy Subjects. Electronics 2023, 12, 2516. [Google Scholar] [CrossRef]
- Wang, Y.-W.; Chen, C.-H.; Lin, Y.-C. Balance Rehabilitation System for Parkinson’s Disease Patients based on Augmented Reality. In Proceedings of the 2020 IEEE Eurasia Conference on IOT, Communication and Engineering (ECICE), Yunlin, Taiwan, 23–25 October 2020; IEEE: Piscataway, NJ, USA, 2020; pp. 191–194. [Google Scholar] [CrossRef]
- Wang, Y.; Gao, L.; Yan, H.; Jin, Z.; Fang, J.; Qi, L.; Zhen, Q.; Liu, C.; Wang, P.; Liu, Y.; et al. Efficacy of C-Mill gait training for improving walking adaptability in early and middle stages of Parkinson’s disease. Gait Posture 2022, 91, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Tan, D.; Li, Z.; Sun, Z. Supporting Tremor Rehabilitation Using Optical See-Through Augmented Reality Technology. Sensors 2023, 23, 3924. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Luo, C.; Yang, S.; Xu, S.; Yang, Y.; Jia, J.; Yu, B. MRehab: A Mixed Reality Rehabilitation System Supporting Integrated Speech and Hand Training. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2024, 8, 1–23. [Google Scholar] [CrossRef]
- Wenk, N.; Penalver-Andres, J.; Palma, R.; Buetler, K.A.; Muri, R.; Nef, T.; Marchal-Crespo, L. Reaching in Several Realities: Motor and Cognitive Benefits of Different Visualization Technologies. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1037–1042. [Google Scholar] [PubMed]
- Yang, Z.-Q.; Du, D.; Wei, X.-Y.; Tong, R.K.-Y. Augmented reality for stroke rehabilitation during COVID-19. J. NeuroEng. Rehabil. 2022, 19, 136. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.-H.; Nekar, D.M.; Kang, H.-Y.; Lee, J.-W.; Oh, S.-Y. Comparison of Physical Activity Training Using Augmented Reality and Conventional Therapy on Physical Performance following a Total Knee Replacement: A Randomized Controlled Trial. Appl. Sci. 2023, 13, 894. [Google Scholar] [CrossRef]
- Zhang, D.; Shen, Y.; Ong, S.K.; Nee, A.Y.C. An affordable augmented reality based rehabilitation system for hand motions. In Proceedings of the 2010 International Conference on Cyberworlds, Singapore, 20–22 October 2010; pp. 346–353. [Google Scholar] [CrossRef]
- Hoffman, D.M.; Girshick, A.R.; Akeley, K.; Banks, M.S. Vergence–accommodation conflicts hinder visual performance and cause visual fatigue. J. Vis. 2008, 8, 33. [Google Scholar] [CrossRef]
- Condino, S.; Turini, G.; Parchi, P.D.; Viglialoro, R.M.; Piolanti, N.; Gesi, M.; Ferrari, M.; Ferrari, V. How to build a patient-specific hybrid simulator for orthopaedic open surgery: Benefits and limits of mixed-reality using the Microsoft hololens. J. Healthc. Eng. 2018, 2018, 5435097. [Google Scholar] [CrossRef] [PubMed]
| Author | AR/MR Visualization Device | AR/MR | Source of Information in AR/MR | Pathology | Anatomical District | Number of Participants | Acceptability and/or Usability Analysis |
|---|---|---|---|---|---|---|---|
| Ahn et al., 2017 [29] | HMD 1 (Epson Moverio) | AR | •Accelerometer •Gyroscope | Parkinson | Lower-limb | P 5: 10 | No |
| Aung et al., 2014 [30] | Monitor | AR | •Camera •EMG sensor | Stroke | Upper-limb | H 6: 7 | No |
| Barioni et al., 2017 [31] | Monitor | AR | RGB-D camera | NSND 3 | Upper-limb | H: 9 | Yes |
| Bennour et al., 2018 [32] | Video Projector | AR | Infrared camera | NSND | Lower-limb | H: 10 | No |
| Blomqvist et al., 2021 [33] | HMD (Microsoft HoloLens) | AR | SLAM 2 | Impaired balance | Whole body | P: 7 | Yes |
| Boucher et al., 2013 [34] | HMD (VUZIX iWear) | AR | RGB-D camera | Parkinson | Whole body | 33 (H: 11, P: 22) | Yes |
| Burke et al., 2010 [35] | Monitor | AR | Camera | Stroke | Upper-limb | No info | No |
| Cavalcanti et al., 2019 [36] | Monitor | AR | RGB-D camera | NSND | Upper-limb | H: 45 | Yes |
| Chen et al., 2011 [37] | Monitor | MR | •Infrared camera •Pressure sensor | Stroke | Upper-limb | H: 3 | No |
| Colomer et al., 2016 [38] | Video Projector | AR | RGB-D camera | Stroke | Upper-limb | P: 30 | Yes |
| Condino et al., 2019 [39] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Upper-limb | H: 25 | Yes |
| Da Gama et al., 2016 [40] | Monitor | AR | RGB-D camera | NSND | Upper-limb | 33 (H: 22, P:11) | Yes |
| de Assis et al., 2016 [41] | Monitor | AR | •EMG sensor •Camera | Stroke | Upper-limb | P: 8 | No |
| De Cecco et al., 2023 [42] | HMD (Microsoft HoloLens) | MR | •RGB-D camera •Force platform •ECG sensor | NSND | Upper-limb | 8 (H: 5, P: 3) | No |
| de Crignis et al., 2023 [43] | HMD (Microsoft HoloLens) | AR | SLAM | Stroke | Upper-limb | P: 11 | Yes |
| De Leon et al., 2014 [44] | Monitor | AR | RGB-D camera | Stroke | Upper-limb | H:4 | Yes |
| Debarba et al., 2018 [45] | HMD (Microsoft HoloLens) | AR | •SLAM •Infrared camera | NSND | Lower-limb | H: 5 | Yes |
| Duff et al., 2012 [46] | Monitor | MR | Infrared camera | Stroke | Upper-limb | P:25 | No |
| Enam et al., 2021 [47] | Video Projector | AR | Force platform | Stroke | Lower-limb | 3 (H: 1, P: 2) | Yes |
| Escalona et al., 2020 [48] | Monitor | AR | RGB-D camera | NSND | Whole body | H: 10 | Yes |
| Espay et al., 2010 [49] | HMD (N/A) | AR | •Accelerometer •Force platform | Parkinson | Lower-limb | P: 13 | No |
| Evans et al., 2022 [50] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Lower-limb | H: 12 | No |
| Everard, et al., 2024 [26] | Monitor | MR | •EMG sensor •Camera | PLP 4 | Upper-limb | P: 81 | Yes |
| Fang et al., 2023 [51] | Monitor | MR | RGB-D camera | Stroke | Upper-limb | P: 5 | No |
| Franzò et al., 2023 [52] | HMD (Microsoft HoloLens) | MR | SLAM | Cerebellar Ataxic | Upper-limb | H: 1 | No |
| Franzo et al., 2023 [53] | HMD (Microsoft HoloLens) | MR | SLAM | Cerebellar Ataxic | Upper-limb | No info | No |
| Garcia et al., 2014 [54] | Monitor | AR | RGB-D camera | Ankle sprain | Lower-limb | No info | No |
| Garcia Hernandez et al., 2023 [55] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Upper-limb | H: 3 | No |
| Gazzoni et al., 2021 [4] | HMD (Epson Moverio) | AR | EMG sensor | NSND | Whole body | No info | No |
| Gmez-Portes et al., 2021 [56] | HMD (Microsoft HoloLens) | MR | SLAM | Stroke | Upper-limb | H: 25 | No |
| Guinet et al., 2022 [57] | HMD (Microsoft HoloLens) | AR | SLAM | Cerebral Palsy | Lower-limb | P: 25 | Yes |
| Gulcan et al., 2022 [58] | Video Projector | AR | Force platform | Parkinson | Lower-limb | P: 30 | No |
| Ham et al., 2024 [59] | Monitor | MR | •Infrared camera •Camera | Stroke | Upper-limb | P: 21 | No |
| Hazubski et al., 2020 [60] | HMD (Epson Moverio) | AR | •Infrared camera •Accelerometer | Limb loss—Prosthesis control | Upper-limb | No info | No |
| He et al., 2018 [61] | Monitor | AR | •IMU sensor •Camera •LDR Sensor | NSND | Upper-limb | H: 5 | No |
| Held et al., 2020 [62] | HMD (Microsoft HoloLens) | AR | SLAM | Stroke | Lower-limb | P: 1 | Yes |
| Hoda et al., 2014 [63] | Monitor | MR | •Infrared camera •Accelerometer | Stroke | Upper-limb | H: 6 | Yes |
| Hossain et al., 2016 [64] | Monitor | AR | •Camera •Accelerometer •Vibrotactile actuators | Stroke | Upper-limb | 36 (H: 25, P: 11) | Yes |
| Hunt et al., 2023 [65] | HMD (Custom made, VIVE Pro HTC) | AR | •HTC Vive Tracker •EMG sensor •Camera | Limb loss—Prosthesis control | Upper-limb | H: 12 | No |
| Im et al., 2015 [66] | Monitor | AR | RGB-D camera | NSND | Lower-limb | H: 18 | Yes |
| Janssen et al., 2020 [67] | HMD (Microsoft HoloLens) | MR | SLAM | Parkinson | Whole body | P: 16 | Yes |
| Jeon et al., 2020 [68] | Monitor | AR | RGB-D camera | sarcopenia | Whole body | H: 27 | Yes |
| Jin et al., 2019 [69] | HMD (Custom made) | AR | •Force platform •RGB-D camera | Stroke | Lower-limb | H: 3 | No |
| Jung et al., 2013 [70] | HMD (SVGA i-visor) | AR | •EMG sensor •Electronic goniometer | Stroke | Upper-limb | P: 10 | No |
| Karatsidis et al., 2018 [71] | HMD (Microsoft HoloLens) | AR | •IMU sensor •SLAM | Knee osteoarthritis | Lower-limb | H: 11 | No |
| Ko et al., 2021 [72] | HMD (Microsoft HoloLens) | MR | SLAM | Stroke | Lower-limb | P: 9 | No |
| Kong et al. [73] | Monitor | AR | RGB-D camera | Stroke | Whole body | 10 (H: 8, P: 2) | Yes |
| Koroleva et al., 2021 [74] | HMD (Epson Moverio) | AR | •Infrared camera •RGB-D camera | Stroke | Whole body | P: 50 | No |
| Ku et al., 2019 [75] | Monitor | AR | RGB-D camera | NSND | Lower-limb | H: 34 | No |
| Kuijpers et al., 2022 [76] | Video Projector | AR | Force platform | Developmental Coordination Disorder | Lower-limb | P: 27 | Yes |
| Lancere et al., 2023 [77] | HMD (Microsoft HoloLens) | MR | •EMG sensor •Respiratory Sensor | Limb loss—Breathing training | Deep core muscles | P: 13 | Yes |
| Lee et al., 2019 [78] | HMD (Microsoft HoloLens) | MR | •SLAM •Force platform | Impaired balance | Whole body | H: 8 | Yes |
| Li et al., 2021 [79] | Monitor | AR | Camera | Stroke | Upper-limb | P: 30 | Yes |
| Lim G et al., 2024 [80] | HMD (Meta Quest Pro) | MR | •EMG sensor •RGB-D camera | Amputees—Prosthesis control | Lower-limb | 15 (H: 5, P: 10) | No |
| Lim JY et al. [81] | Monitor | AR | RGB-D camera | Anterior Cruciate Ligament | Lower-limb | P: 28 | Yes |
| Lin et al., 2011 [82] | Monitor | AR | RGB-D camera | NSND | Upper-limb | No info | No |
| Liu et al., 2017 [83] | Monitor | AR | Camera | NSND | Upper-limb | H: 20 | Yes |
| Liu et al., 2024 [84] | HMD/Monitor (N/A) | MR | •SLAM •RGB-D camera | Pelvic Floor Dysfunction | Lower-limb | P: 1 | No |
| Luchetti et al., 2020 [85] | HMD (Microsoft HoloLens) | AR | SLAM | NSND | Lower-limb | H: 27 | Yes |
| Mahmood et al. [86] | HMD (Microsoft HoloLens) | MR | SLAM | Parkinson | Upper-limb | 31 (H: 22, P: 9) | Yes |
| Markovic et al., 2014 [87] | HMD (VUZIX iWear) | AR | •EMG sensor •Camera | Amputees—Prosthesis control | Upper-limb | H: 13 | No |
| McCarty, T et al., 2024 [88] | HMD (Microsoft HoloLens) | MR | •IMU sensor •SLAM •RGB-D camera •Force platform •RGB-D camera | NSND | Whole body | No info | No |
| Miller et al., 2022 [89] | HMD (Microsoft HoloLens) | AR | SLAM | NSND | Lower-limb | H: 8 | No |
| Miller et al., 2024 [90] | HMD (Microsoft HoloLens) | AR | SLAM | NSND | Lower-limb | H: 19 | No |
| Mousavi Hondori et al., 2016 [91] | Video Projector | AR | •Camera | Stroke | Upper-limb | P: 18 | No |
| Nam et al., 2022 [92] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Upper-limb | H: 4 | Yes |
| Nam et al., 2023 [93] | Monitor | AR | IMU sensor | Adolescent idiopathic scoliosis | Upper-limb | 13 (H: 10, P: 3) | No |
| Nekar et al., 2023 [94] | HMD (Microsoft HoloLens) | MR | •IMU sensor •EMG sensor •SLAM | NSND | Upper-limb | H: 32 | Yes |
| Ortiz-Catalan et al., 2016 [95] | Monitor | AR | •Camera •EMG sensor | PLP | Upper-limb | P: 14 | No |
| Pavlou et al., 2024 [28] | HMD/Video Projector (N/A) | MR | •IMU sensor •Pressure-based insole •RGB-D camera | Impaired balance | Whole body | H: 120 | Yes |
| Pezzera et al., 2020 [96] | HMD (Microsoft HoloLens) | MR | •RGB-D camera •Force platform | NSND | Whole body | No info | No |
| Pillai et al., 2022 [97] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Upper-limb | H: 10 | Yes |
| Pinto-Fern’andez et al., 2023 [98] | HMD (Microsoft HoloLens) | AR | IMU sensor | NSND | Lower-limb | H: 5 | Yes |
| Pisano et al., 2024 [99] | Video Projector | AR | •Force platform •RGB-D camera | Parkinson | Lower-limb | P: 17 | No |
| Prahm et al., 2022 [100] | HMD (Microsoft HoloLens) | AR | •SLAM •EMG sensor | PLP | Upper-limb | No info | No |
| Retzinger et al., 2024 [101] | HMD (Magic Leap) | AR | IMU sensor | Parkinson | Lower-limb | H: 20 | Yes |
| Rizzi et al., 2023 [102] | HMD (Microsoft HoloLens) | AR | •IMU sensor •Respiratory Sensor | NSND | Whole body | H: 10 | Yes |
| Roumpi et al., 2022 [103] | HMD/Video Projector (N/A) | AR | •IMU sensor •Pressure-based insole •RGB-D camera | Impaired balance | Whole body | H: 47 | Yes |
| Scheermesser et al., 2024 [104] | HMD (Microsoft HoloLens) | MR | SLAM | Stroke | Upper-limb | P: 15 | Yes |
| Sekhavat et al., 2018 [105] | Video Projector | AR | RGB-D camera | NSND | Lower-limb | 32 (H: 24, P: 8) | Yes |
| Sharma et al., 2018 [106] | HMD (Microsoft HoloLens) | MR | •SLAM •EMG sensor | Limb loss—Prosthesis control | Upper-limb | H: 2 | No |
| Shim et al., 2022 [107] | HMD (Microsoft HoloLens) | MR | •EMG sensor •SLAM | Limb loss—Prosthesis control | Lower-limb | 15 (H: 8, P: 7) | Yes |
| Shim et al., 2023 [25] | Monitor | AR | RGB-D camera | Knee osteoarthritis | Lower-limb | P: 56 | Yes |
| Shim et al., 2023 [27] | Monitor | AR | RGB-D camera | Rotator cuff tear | Upper-limb | P: 115 | Yes |
| Sousa et al., 2016 [108] | Video Projector | AR | Infrared camera | NSND | Upper-limb | H: 18 | Yes |
| Tada et al., 2022 [109] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Upper-limb | H: 7 | No |
| Tada et al., 2024 [110] | HMD (Microsoft HoloLens) | MR | SLAM | NSND | Upper-limb | H: 10 | Yes |
| Tan et al., 2024 [111] | HMD (Microsoft HoloLens) | MR | •RGB-D camera •SLAM •IMU sensor | NSND | Lower-limb | H: 10 | Yes |
| Tanda et al., 2024 [112] | HMD (Microsoft HoloLens) | MR | •SLAM •Camera | Multiple Sclerosis | Upper-limb | H: 13 | Yes |
| Thinh et al., 2021 [113] | Monitor | AR | •Camera •Torque sensor | Stroke | Whole body | P: 10 | Yes |
| Thøgersen et al., 2020 [114] | HMD (HTC Vive) | AR | •HTC Vive Tracker •EMG sensor | PLP | Upper-limb | P: 7 | No |
| Timmermans et al., 2021 [115] | Video Projector | AR | •Force platform •RGB-D camera | Stroke | Lower-limb | P: 33 | Yes |
| Trojan et al., 2014 [116] | HMD/Monitor (eMagin) | AR | •Camera •Infrared camera | NSND | Upper-limb | H: 7 | No |
| Tykhyi et al., 2024 [117] | HMD (Magic leap) | AR | SLAM | NSND | Upper-limb | P: 1 | No |
| Vaida et al., 2024 [118] | HMD (Microsoft HoloLens) | AR | •SLAM •Electronic goniometer | NSND | Lower-limb | H:12 | Yes |
| van de Venis et al., 2023 [119] | Video Projector | AR | Force platform | HSP 7 | Lower-limb | P: 36 | No |
| Viglialoro et al., 2023 [120] | Video Projector | AR | Infrared camera | NSND | Upper-limb | H: 16 | Yes |
| Wang et al., 2020 [121] | HMD (HTC Vive) | AR | •HTC Vive Tracker •Camera | Parkinson | Lower-limb | P: 5 | Yes |
| Wang et al., 2022 [122] | Video Projector | AR | Force platform | Parkinson | Lower-limb | P: 52 | No |
| Wang et al., 2023 [123] | HMD (Oculus Quest) | AR | Infrared camera | Tremor | Whole body | H: 13 | Yes |
| Wang et al., 2024 [124] | HMD (Microsoft HoloLens) | MR | SLAM | Stroke | Upper-limb | P:12 | Yes |
| Wenk et al., 2019 [125] | HMD/Monitor (HTC Vive) | AR | HTC Vive Tracker | NSND | Upper-limb | H: 20 | No |
| Yang et al., 2022 [126] | Monitor | AR | RGB-D camera | Stroke | Whole body | P: 39 | Yes |
| Yu et al., 2023 [127] | Monitor | AR | RGB-D camera | Knee osteoarthritis | Lower-limb | P: 24 | No |
| Zhang et al., 2010 [128] | Monitor | AR | •RGB-D camera •Flex sensor | Stroke | Upper-limb | No info | No |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farsi, A.; Cerone, G.L.; Falla, D.; Gazzoni, M. Emerging Applications of Augmented and Mixed Reality Technologies in Motor Rehabilitation: A Scoping Review. Sensors 2025, 25, 2042. https://doi.org/10.3390/s25072042
Farsi A, Cerone GL, Falla D, Gazzoni M. Emerging Applications of Augmented and Mixed Reality Technologies in Motor Rehabilitation: A Scoping Review. Sensors. 2025; 25(7):2042. https://doi.org/10.3390/s25072042
Chicago/Turabian StyleFarsi, Arman, Giacinto Luigi Cerone, Deborah Falla, and Marco Gazzoni. 2025. "Emerging Applications of Augmented and Mixed Reality Technologies in Motor Rehabilitation: A Scoping Review" Sensors 25, no. 7: 2042. https://doi.org/10.3390/s25072042
APA StyleFarsi, A., Cerone, G. L., Falla, D., & Gazzoni, M. (2025). Emerging Applications of Augmented and Mixed Reality Technologies in Motor Rehabilitation: A Scoping Review. Sensors, 25(7), 2042. https://doi.org/10.3390/s25072042







