Development and Usability of MSafe: A Fall Risk Application for Older Adults with Multiple Sclerosis
Abstract
1. Introduction
2. Materials and Methods
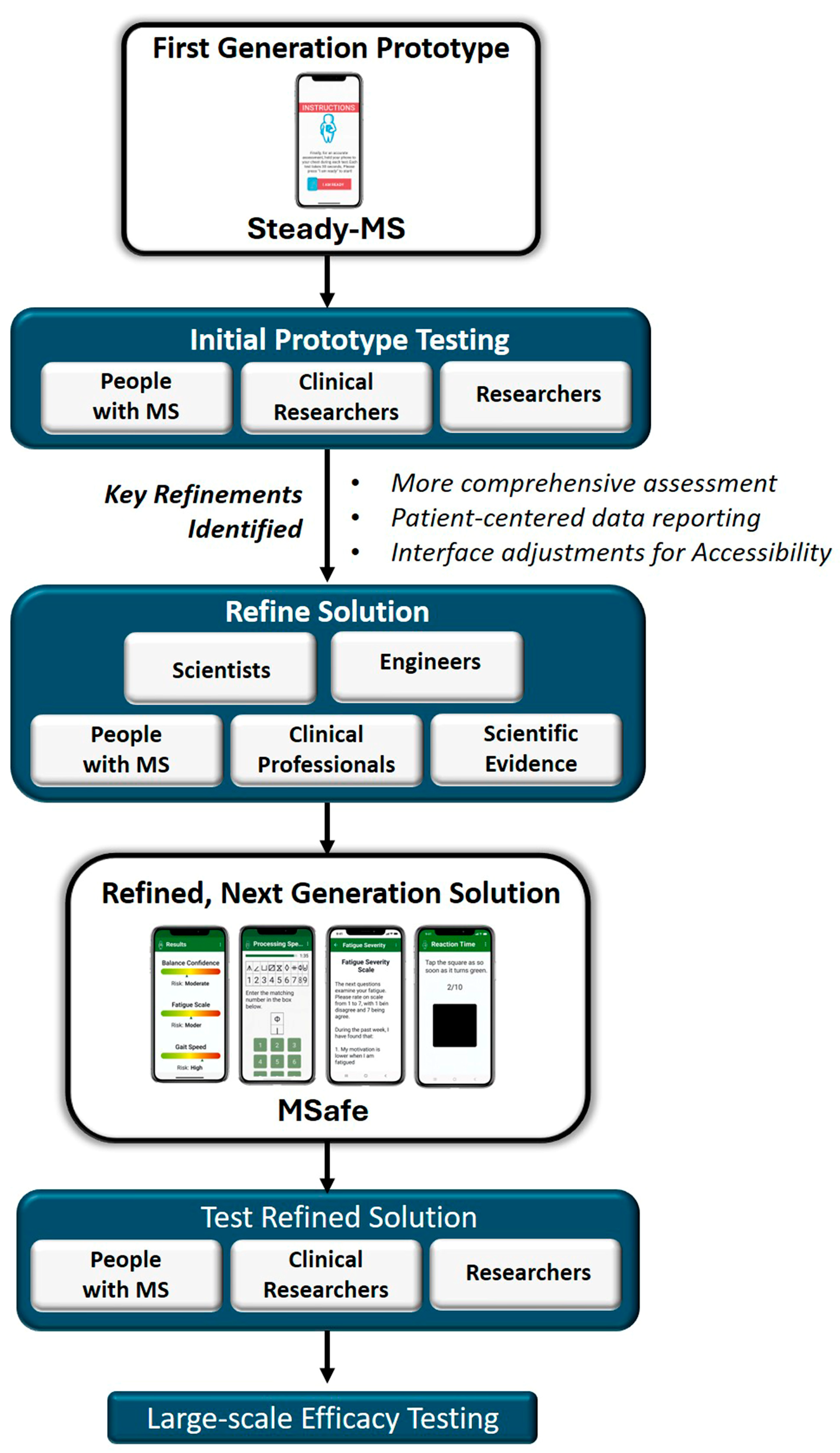
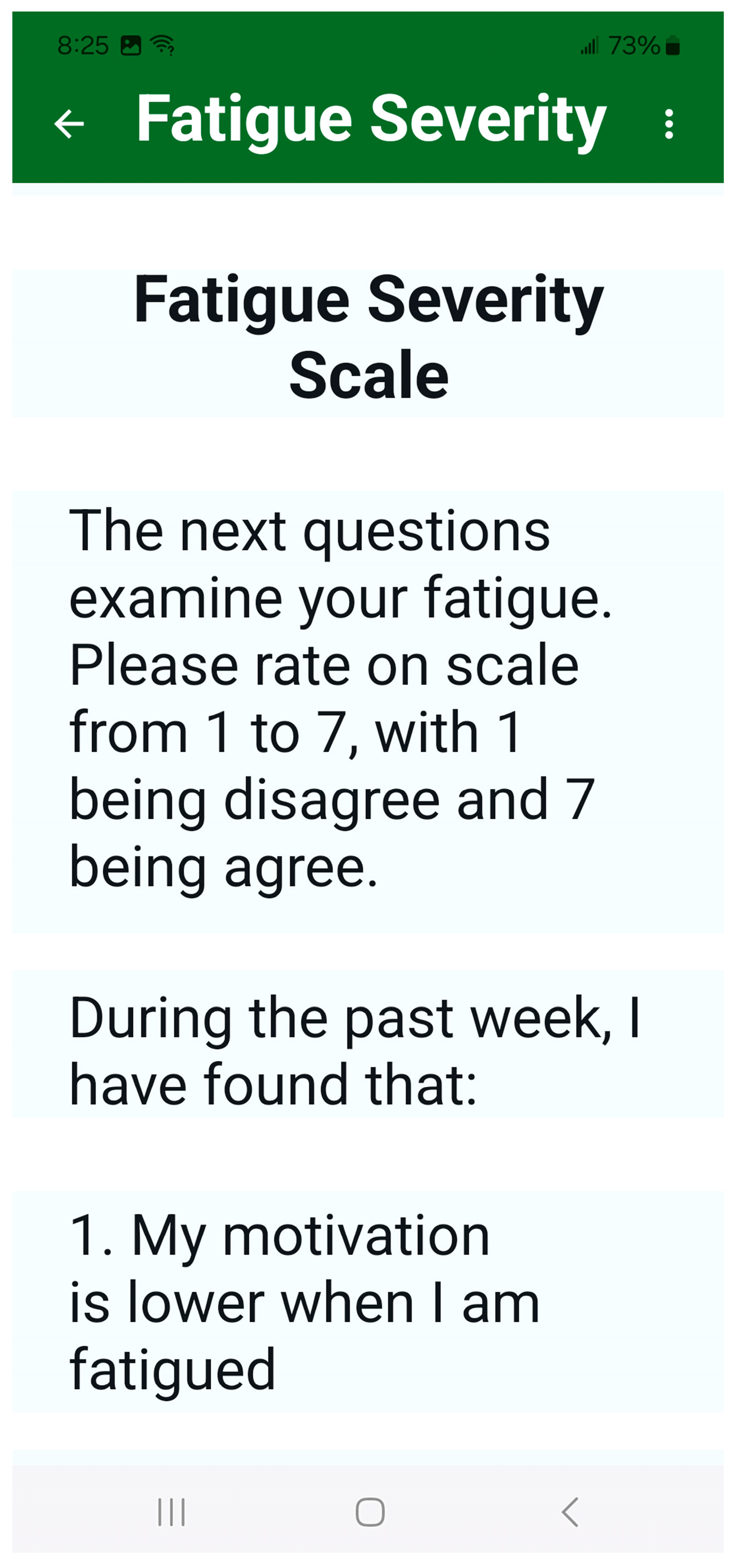
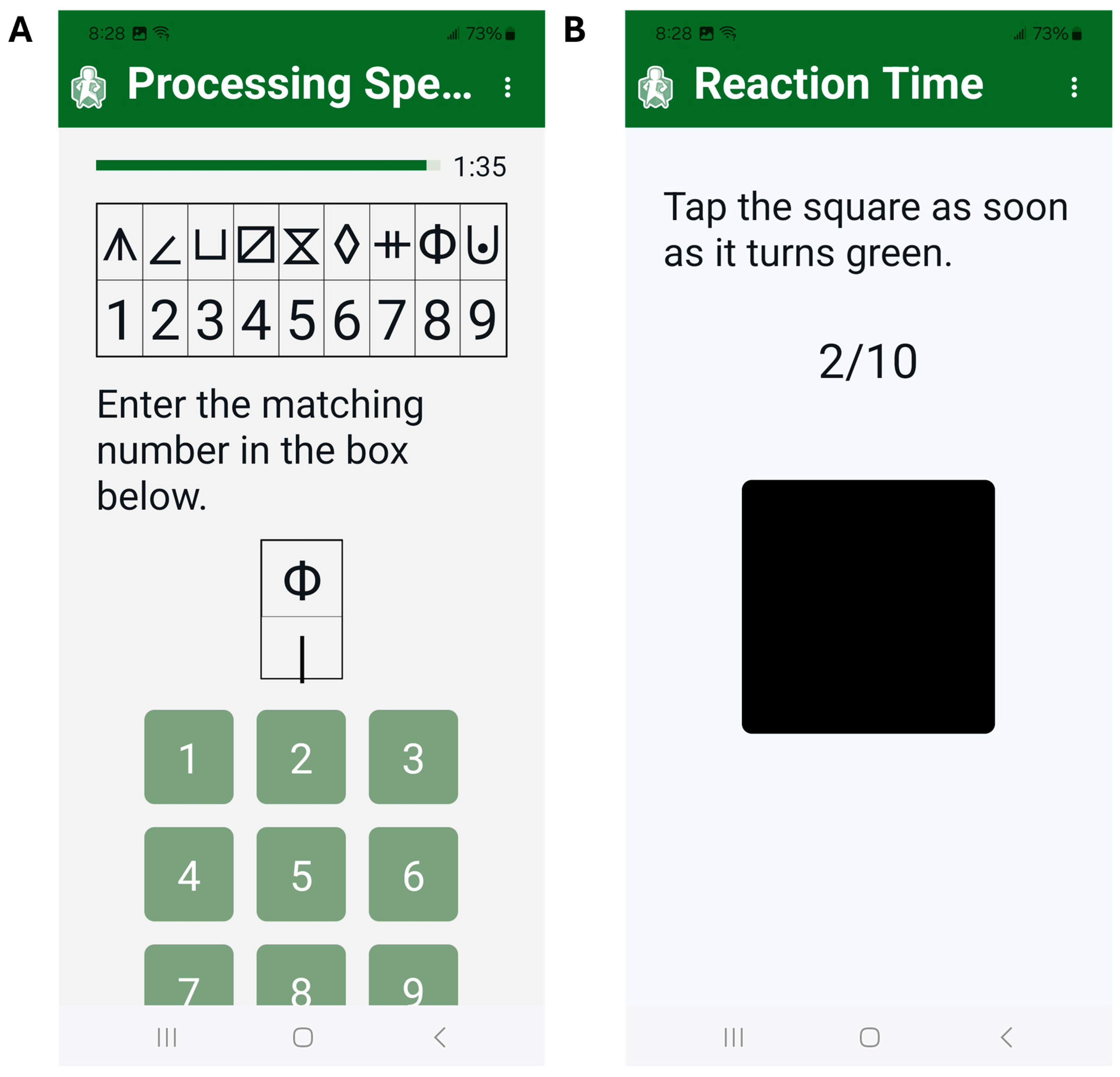
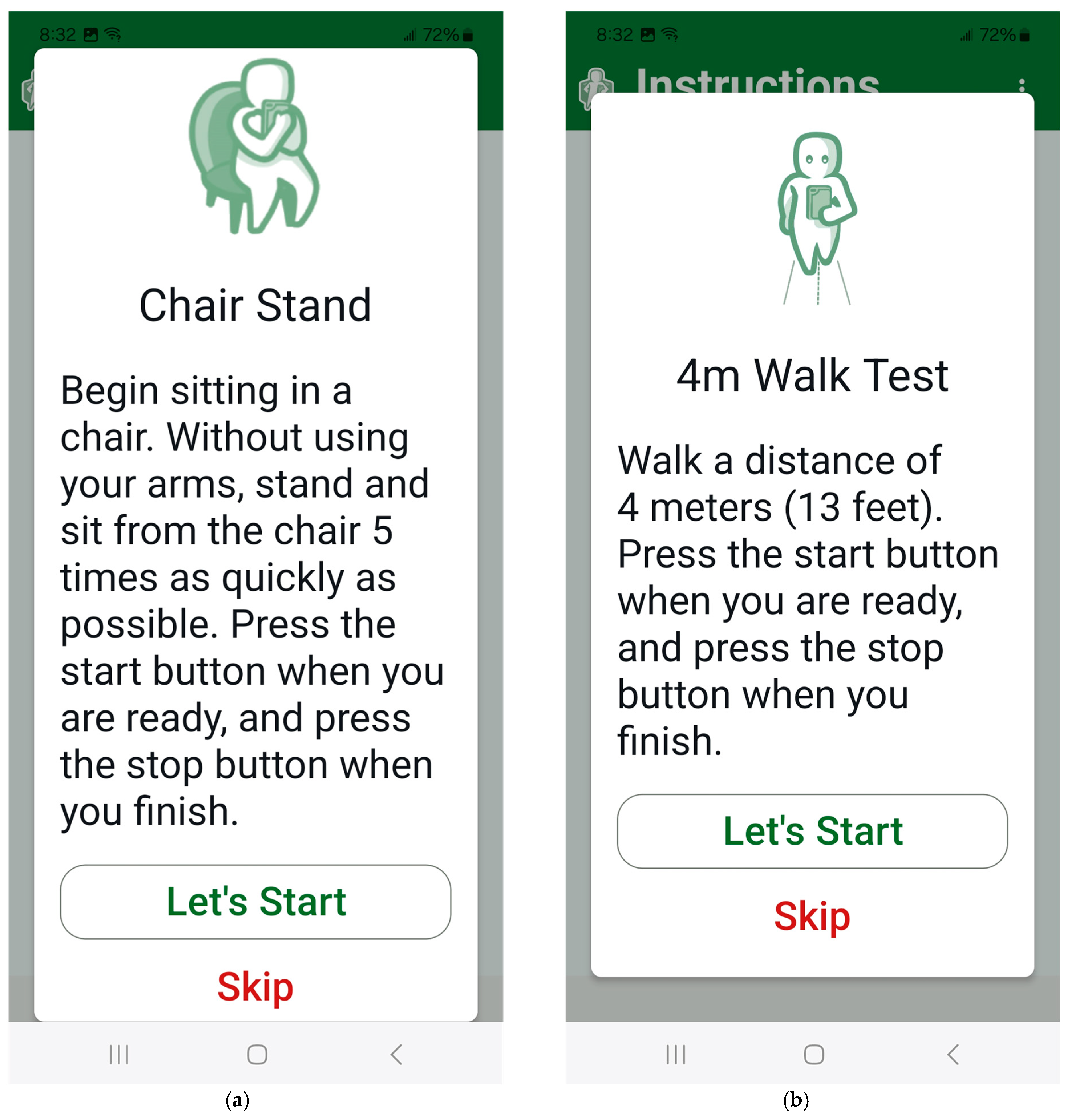
2.1. MSafe Development
2.2. MSafe Usability
2.3. Procedures
2.4. Statistical Analysis
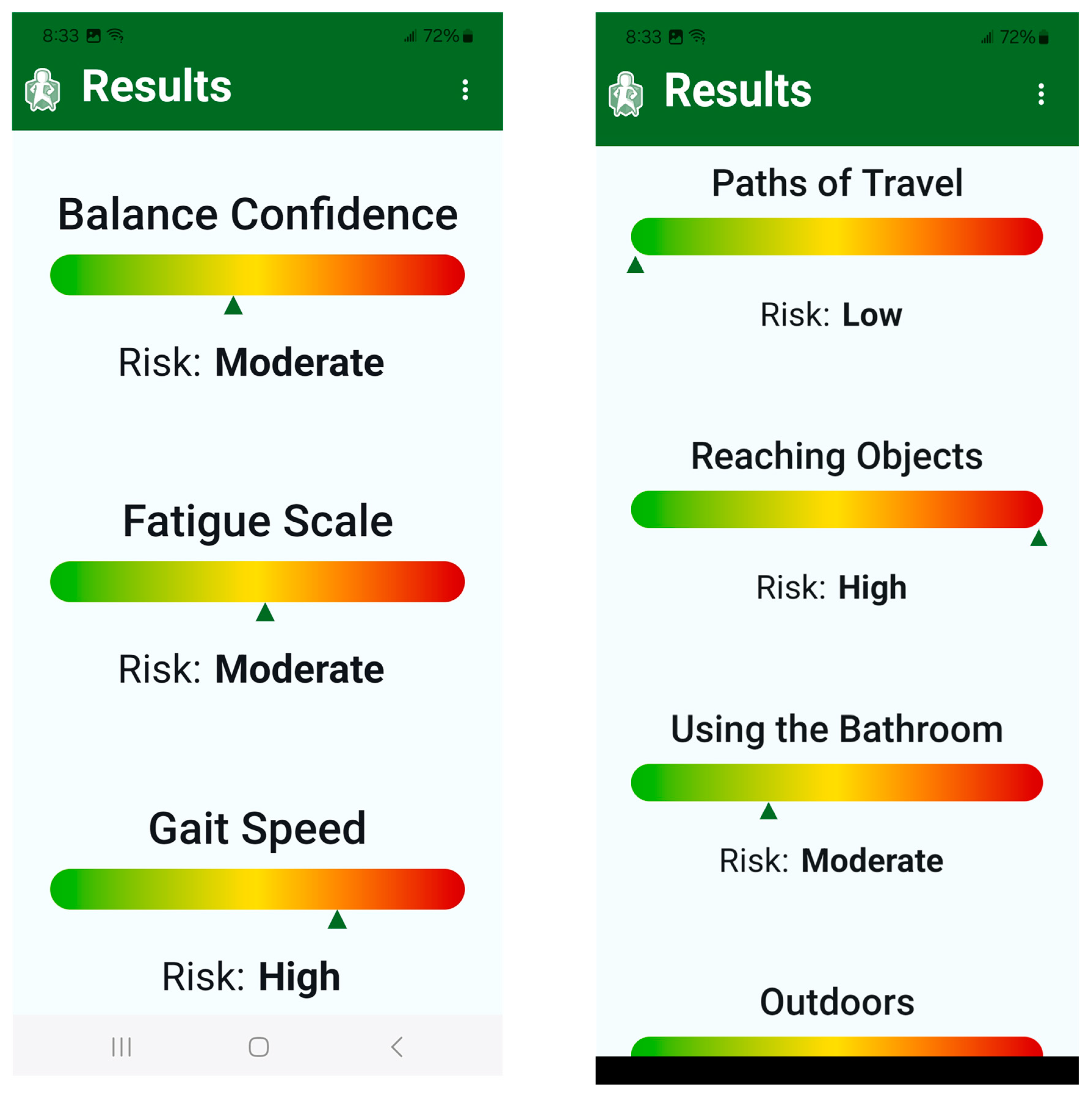
3. Results
3.1. Participants
3.2. System Usability Scale
3.3. Semi-Structured Interviews
3.4. Simplicity of Use
3.5. Progress Monitoring
3.6. Alignment and Awareness
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McGinley, M.P.; Goldschmidt, C.H.; Rae-Grant, A.D. Diagnosis and treatment of multiple sclerosis: A review. JAMA 2021, 325, 765–779. [Google Scholar] [CrossRef]
- Sanai, S.A.; Saini, V.; Benedict, R.H.; Zivadinov, R.; E Teter, B.; Ramanathan, M.; Weinstock-Guttman, B. Aging and multiple sclerosis. Mult. Scler. J. 2016, 22, 717–725. [Google Scholar] [CrossRef]
- Wallin, M.T.; Culpepper, W.J.; Campbell, J.D.; Nelson, L.M.; Langer-Gould, A.; Marrie, R.A.; Cutter, G.R.; Kaye, W.E.; Wagner, L.; Tremlett, H.; et al. The prevalence of MS in the United States. Neurology 2019, 92, e1029–e1040. [Google Scholar] [CrossRef]
- Holm, R.P.; Wandall-Holm, M.F.; Sellebjerg, F.; Magyari, M. Comorbidity in the aging population with multiple sclerosis: A Danish nationwide study. Front. Neurol. 2023, 14, 1297709. [Google Scholar] [CrossRef] [PubMed]
- Graves, J.S.; Krysko, K.M.; Hua, L.H.; Absinta, M.; Franklin, R.J.M.; Segal, B.M. Ageing and multiple sclerosis. Lancet Neurol. 2023, 22, 66–77. [Google Scholar] [CrossRef] [PubMed]
- Coote, S.; Comber, L.; Quinn, G.; Santoyo-Medina, C.; Kalron, A.; Gunn, H. Falls in People with Multiple Sclerosis: Risk Identification, Intervention, and Future Directions. Int. J. MS Care 2020, 22, 247–255. [Google Scholar] [CrossRef]
- Cameron, M.H.; Nilsagard, Y. Balance, gait, and falls in multiple sclerosis. Handb. Clin. Neurol. 2018, 159, 237–250. [Google Scholar]
- Carling, A.; Forsberg, A.; Nilsagård, Y. Falls in people with multiple sclerosis: Experiences of 115 fall situations. Clin. Rehabil. 2018, 32, 526–535. [Google Scholar] [CrossRef]
- Peterson, E.W.; Cho, C.C.; von Koch, L.; Finlayson, M.L. Injurious falls among middle aged and older adults with multiple sclerosis. Arch. Phys. Med. Rehabil. 2008, 89, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Peterson, E.W.; Cho, C.C.; Finlayson, M.L. Fear of falling and associated activity curtailment among middle aged and older adults with multiple sclerosis. Mult. Scler. J. 2007, 13, 1168–1175. [Google Scholar] [CrossRef]
- Gopal, A.; Gelfand, J.M.; Bove, R.; Block, V.J. Fall Assessment and Monitoring in People With Multiple Sclerosis: A Practical Evidence-Based Review for Clinicians. Neurol. Clin. Pract. 2023, 13, e200184. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.; Galvin, R.; Kennedy, C.; Finlayson, M.; McGuigan, C.; Walsh, C.D.; Coote, S. Interventions for preventing falls in people with multiple sclerosis. Cochrane Database Syst. Rev. 2019, 11, Cd012475. [Google Scholar] [CrossRef]
- Chiu, C.; Bishop, M.; Pionke, J.J.; Strauser, D.; Santens, R.L. Barriers to the Accessibility and Continuity of Health-Care Services in People with Multiple Sclerosis: A Literature Review. Int. J. MS Care 2017, 19, 313–321. [Google Scholar] [CrossRef]
- Mayo, C.D.; Farzam-Kia, N.; Ghahari, S. Identifying Barriers to and Facilitators of Health Service Access Encountered by Individuals with Multiple Sclerosis. Int. J. MS Care 2021, 23, 37–44. [Google Scholar] [CrossRef]
- Hsieh, K.L.; Chen, L.; Sosnoff, J.J. Mobile Technology for Falls Prevention in Older Adults. J. Gerontol. Ser. A 2023, 78, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Salimzadeh, Z.; Damanabi, S.; Kalankesh, L.R.; Ferdousi, R. Mobile Applications for Multiple Sclerosis: A Focus on Self-Management. Acta Inform. Medica 2019, 27, 12–18. [Google Scholar] [CrossRef]
- Foong, Y.C.; Bridge, F.; Merlo, D.; Gresle, M.; Zhu, C.; Buzzard, K.; Butzkueven, H.; van der Walt, A. Smartphone monitoring of cognition in people with multiple sclerosis: A systematic review. Mult. Scler. Relat. Disord. 2023, 73, 104674. [Google Scholar] [CrossRef]
- Yamada, M.; Aoyama, T.; Okamoto, K.; Nagai, K.; Tanaka, B.; Takemura, T. Using a Smartphone while walking: A measure of dual-tasking ability as a falls risk assessment tool. Age Ageing 2011, 40, 516–519. [Google Scholar] [CrossRef]
- Griffin, N.; Kehoe, M. A questionnaire study to explore the views of people with multiple sclerosis of using smartphone technology for health care purposes. Disabil. Rehabil. 2018, 40, 1434–1442. [Google Scholar] [CrossRef]
- Marrie, R.A.; Leung, S.; Tyry, T.; Cutter, G.R.; Fox, R.; Salter, A. Use of eHealth and mHealth technology by persons with multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 27, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, K.; Fanning, J.; Frechette, M.; Sosnoff, J. Usability of a fall risk mHealth app for people with multiple sclerosis: Mixed methods study. JMIR Hum. Factors 2021, 8, e25604. [Google Scholar] [CrossRef]
- Hsieh, K.L.; Sosnoff, J.J. Smartphone accelerometry to assess postural control in individuals with multiple sclerosis. Gait Posture 2021, 84, 114–119. [Google Scholar] [CrossRef]
- Digital Health Technologies for Remote Data Acquisition in Clinical Investigations US Food & Drug Administration. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/digital-health-technologies-remote-data-acquisition-clinical-investigations (accessed on 14 October 2025).
- Wood, T.A.; Wajda, D.A.; Sosnoff, J.J. Use of a short version of the activities-specific balance confidence scale in multiple sclerosis. Int. J. MS Care 2019, 21, 15–21. [Google Scholar] [CrossRef]
- Rooney, S.; McFadyen, A.; Wood, L.; Moffat, F.; Paul, L. Minimally important difference of the fatigue severity scale and modified fatigue impact scale in people with multiple sclerosis. Mult. Scler. Relat. Disord. 2019, 35, 158–163. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.T.P.; Matsuda, P.N.; Fritz, N.E.P.; Allen, D.D.; Yorke, A.M.P.; Widener, G.L.; Jewell, S.T.M.; Potter, K. Self-Report Measures of Fatigue for People With Multiple Sclerosis: A Systematic Review. J. Neurol. Phys. Ther. 2024, 48, 6–14. [Google Scholar] [CrossRef]
- Ziebart, C.; Dewan, N.; Tuazon, J.; MacDermid, J. Development of the Home Fall Hazard Checklist. Rehabil. Res. Pract. 2021, 2021, 5362197. [Google Scholar] [CrossRef]
- Benedict, R.H.; DeLuca, J.; Phillips, G.; LaRocca, N.; Hudson, L.D.; Rudick, R. Validity of the Symbol Digit Modalities Test as a cognition performance outcome measure for multiple sclerosis. Mult. Scler. J. 2017, 23, 721–733. [Google Scholar] [CrossRef]
- Sosnoff, J.J.; Balantrapu, S.; Pilutti, L.A.; Sandroff, B.M.; Morrison, S.; Motl, R.W. Cognitive processing speed is related to fall frequency in older adults with multiple sclerosis. Arch. Phys. Med. Rehabil. 2013, 94, 1567–1572. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R.; Clark, R.D. Simple physiological and clinical tests for the accurate prediction of falling in older people. Gerontology 1996, 42, 199–203. [Google Scholar] [CrossRef]
- Tijsma, M.; Vister, E.; Hoang, P.; Lord, S.R. A simple test of choice stepping reaction time for assessing fall risk in people with multiple sclerosis. Disabil. Rehabil. 2017, 39, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Antoniadou, E.; Kalivioti, X.; Stolakis, K.; Koloniari, A.; Megas, P.; Tyllianakis, M.; Panagiotopoulos, E. Reliability and validity of the mCTSIB dynamic platform test to assess balance in a population of older women living in the community. J. Musculoskelet. Neuronal Interact. 2020, 20, 185–193. [Google Scholar]
- Özüdoğru, A.; Canlı, M.; Gürses, Ö.A.; Alkan, H.; Yetiş, A. Determination of five times-sit-to-stand test performance in patients with multiple sclerosis: Validity and reliability. Somatosens. Mot. Res. 2023, 40, 72–77. [Google Scholar] [CrossRef]
- Ozkan, T.; Unluer, N.O.; Ates-Sari, Y.; Hangun, S.F.; Vural, G. Reliability and validity of the 4-meter walk test in patients with multiple sclerosis. Mult. Scler. Relat. Disord. 2024, 87, 105679. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.-A.; DuMontier, C.; Yu, W.; Ask, L.; Zhou, J.; Testa, M.A.; Kim, D.; Abel, G.; Travison, T.; Manor, B.; et al. Validity and Reliability of a Smartphone Application for Home Measurement of Four-Meter Gait Speed in Older Adults. Bioengineering 2024, 11, 257. [Google Scholar] [CrossRef]
- Abou, L.; Peters, J.; Fritz, N.E.; Sosnoff, J.J.; Kratz, A.L. Motor Cognitive Dual-Task Testing to Predict Future Falls in Multiple Sclerosis: A Systematic Review. Neurorehabil. Neural Repair 2022, 36, 757–769. [Google Scholar] [CrossRef] [PubMed]
- Wajda, D.A.; Motl, R.W.; Sosnoff, J.J. Dual task cost of walking is related to fall risk in persons with multiple sclerosis. J. Neurol. Sci. 2013, 335, 160–163. [Google Scholar] [CrossRef]
- Reelick, M.F.; Kessels, R.P.; Faes, M.C.; Weerdesteyn, V.; Esselink, R.A.; Olde Rikkert, M.G. Increased intra-individual variability in stride length and reaction time in recurrent older fallers. Aging Clin. Exp. Res. 2011, 23, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Abasıyanık, Z.; Kahraman, T.; Baba, C.; Sağıcı, Ö.; Ertekin, Ö.; Özakbaş, S. Discriminative ability of the original and short form of the Activities-specific Balance Confidence scale and its individual items for falls in people with multiple sclerosis. Acta Neurol. Belg. 2024, 124, 957–964. [Google Scholar] [CrossRef]
- Vister, E.; Tijsma, M.E.; Hoang, P.D.; Lord, S.R. Fatigue, physical activity, quality of life, and fall risk in people with multiple sclerosis. Int. J. MS Care 2017, 19, 91–98. [Google Scholar] [CrossRef]
- Khalil, H.; Rehan, R.; Al-Sharman, A.; El-Salem, K. The clinical correlates of the chair sit to stand performance in people with multiple sclerosis. Physiother. Theory Pract. 2022, 38, 2884–2895. [Google Scholar] [CrossRef]
- Bilgin, Y.O.U.; Koskderelioglu, A.; Gedizlioglu, M. Fall risk is related to cognitive functioning in ambulatory multiple sclerosis patients. Neurol. Sci. 2023, 44, 3233–3242. [Google Scholar] [CrossRef]
- Hobson, J. The montreal cognitive assessment (MoCA). Occup. Med. 2015, 65, 764–765. [Google Scholar] [CrossRef]
- Powell, L.E.; Myers, A.M. The activities-specific balance confidence (ABC) scale. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 1995, 50, M28–M34. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Lewis, J.R. The system usability scale: Past, present, and future. Int. J. Hum.–Comput. Interact. 2018, 34, 577–590. [Google Scholar] [CrossRef]
- Brooke, J. SUS-A quick and dirty usability scale. Usability Eval. Ind. 1996, 189, 4–7. [Google Scholar]
- Hyzy, M.; Bond, R.; Mulvenna, M.; Bai, L.; Dix, A.; Leigh, S.; Hunt, S. System Usability Scale Benchmarking for Digital Health Apps: Meta-analysis. JMIR Mhealth Uhealth 2022, 10, e37290. [Google Scholar] [CrossRef] [PubMed]
- Gromisch, E.S.; Turner, A.P.; Haselkorn, J.K.; Lo, A.C.; Agresta, T. Mobile health (mHealth) usage, barriers, and technological considerations in persons with multiple sclerosis: A literature review. JAMIA Open 2020, 4, ooaa067. [Google Scholar] [CrossRef] [PubMed]
- Montalban, X.; Graves, J.; Midaglia, L.; Mulero, P.; Julian, L.; Baker, M.; Schadrack, J.; Gossens, C.; Ganzetti, M.; Scotland, A.; et al. A smartphone sensor-based digital outcome assessment of multiple sclerosis. Mult. Scler. J. 2022, 28, 654–664. [Google Scholar] [CrossRef] [PubMed]
- Maillart, E.; Labauge, P.; Cohen, M.; Maarouf, A.; Vukusic, S.; Donzé, C.; Gallien, P.; De Sèze, J.; Bourre, B.; Moreau, T.; et al. MSCopilot, a new multiple sclerosis self-assessment digital solution: Results of a comparative study versus standard tests. Eur. J. Neurol. 2020, 27, 429–436. [Google Scholar] [CrossRef]
- Antonioni, A.; Baroni, A.; Fregna, G.; Ahmed, I.; Straudi, S. The effectiveness of home-based transcranial direct current stimulation on chronic pain: A systematic review and meta-analysis. Digit. Health 2024, 10, 20552076241292677. [Google Scholar] [CrossRef]
- de Moura, M.C.D.S.; Hazime, F.A.; Marotti Aparicio, L.V.; Grecco, L.A.C.; Brunoni, A.R.; Hasue, R.H. Effects of transcranial direct current stimulation (tDCS) on balance improvement: A systematic review and meta-analysis. Somatosens. Mot. Res. 2019, 36, 122–135. [Google Scholar] [CrossRef] [PubMed]
- Kalron, A.; Aloni, R.; Allali, G. The relationship between depression, anxiety and cognition and its paradoxical impact on falls in multiple sclerosis patients. Mult. Scler. Relat. Disord. 2018, 25, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Kasser, S.L.; Goldstein, A.; Wood, P.K.; Sibold, J. Symptom variability, affect and physical activity in ambulatory persons with multiple sclerosis: Understanding patterns and time-bound relationships. Disabil. Health J. 2017, 10, 207–213. [Google Scholar] [CrossRef]
- Kratz, A.L.; Murphy, S.L.; Braley, T.J. Ecological Momentary Assessment of Pain, Fatigue, Depressive, and Cognitive Symptoms Reveals Significant Daily Variability in Multiple Sclerosis. Arch. Phys. Med. Rehabil. 2017, 98, 2142–2150. [Google Scholar] [CrossRef] [PubMed]
| Domain | MSafe Design Element | Validated Construct (Key Refs) |
|---|---|---|
| Balance confidence | ABC-6 (6 items) | Activities-specific Balance Confidence short form [24] |
| Fatigue | FSS (9 items) | Fatigue Severity Scale [25,26] |
| Environmental hazards (home/outdoor) | CDC STEADI-adapted questions | STEADI ‘Check for Safety’ home safety checklist [27] |
| Vision risk | Self-report prompts | Vision impairment as falls-risk factor [7] |
| Cognitive processing speed | Symbol–Digit matching (120 s; 10 s practice) | Symbol Digit Modalities Test analog [28,29] |
| Simple reaction time | 10 trials; mean ms | Reaction/choice stepping RT [30,31] |
| Standing balance | Eyes open/closed feet apart; tandem eyes open; single-leg open (≤30 s) with phone; tri-axial acceleration | mCTSIB and IMU postural sway [22,32] |
| Lower-limb strength | 5 Times Sit-to-Stand (user-timed) | 5 time sit-to-stand [33] |
| Gait speed | 4 m walk (single-task; user-timed) | 4 m walk test/4 m gait speed [34,35] |
| Dual-task gait cost | 4 m walk with serial 3 s from 87 | Dual-task gait cost [36,37] |
| Variable | Participants (n = 21) |
|---|---|
| Age (years) | 61.4 (4.6) |
| Sex | |
| Female | 20 (95.2%) |
| Male | 1 (4.8%) |
| Race | |
| African American or Black | 18 (85.7%) |
| White | 3 (14.3) |
| Education | |
| High school graduate or equivalent | 2 (9.5%) |
| Vocational training | 1 (4.8%) |
| Some or in-progress college/associate’s degree | 5 (23.8%) |
| Bachelor’s degree | 8 (38.1%) |
| Master’s degree | 5 (23.8%) |
| MS Type | |
| Relapse Remitting | 19 (90.5%) |
| Primary Progressive | 2 (9.5%) |
| MS Duration (years) | 19.8 (8.6) |
| Walking Aid | 9 (42.8%) |
| Cane | 9 (42.8%) |
| Walker/rollator | 4 (19%) |
| Expanded Disability Status Scale | 5.1 (1.0) |
| Activities Balance Confidence Scale (%) | 62.1 (25.4) |
| Falls Efficacy Scale International | 35.9 (12.7) |
| Montreal Cognitive Assessment | 23.1 (2.7) |
| Theme | Example Quotes |
|---|---|
| Simplicity of Use | “It’s easy to use. It’s user friendly.” |
| “It’s pretty much self-explanatory”. | |
| “It’s very, very easy”. | |
| “Everything was pretty much clear”. | |
| “I like how simple it is. You push on that and then the numbers pop up. That’s wonderful”. | |
| Progress Monitoring | “MS things are always changing by the literal minute. If I were to do this first thing in the morning, I’d probably be running up or down that hall because I feel better in the morning.” |
| “It’s a reinforcement for to see that you started here and you’ve gone there in a month, two months, three months”. | |
| “I like being able to share the information [results] with my doctor. I can share and don’t have to guess.” | |
| “It’s helpful to explain it [fall risk] to me knowing that I could actually track what’s going on, especially the part with the balance score.” | |
| “It would help to share the information with my doctor. In my case, I’m already concerned about staying upright and not falling, but I think I’ve had this disease for 20 years, and it would be nice to show the difference. It’s hard to explain—over six months, you feel like your walking has changed, but you can’t really identify how. This would tell them how.” | |
| Alignment and Awareness | “I like the fact that it kind of gives you an idea of the [fall risk] areas, and I was actually in agreement with most of it.” |
| “It reconfirmed some of the kind of things I thought were going on with me”. | |
| “I think I have strong legs. I really do think I have strong legs, but in this particular situation, I couldn’t do that [five time sit to stand].” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsieh, K.L.; Backus, D.; Willingham, T.B.; Sanford, J. Development and Usability of MSafe: A Fall Risk Application for Older Adults with Multiple Sclerosis. Sensors 2025, 25, 7075. https://doi.org/10.3390/s25227075
Hsieh KL, Backus D, Willingham TB, Sanford J. Development and Usability of MSafe: A Fall Risk Application for Older Adults with Multiple Sclerosis. Sensors. 2025; 25(22):7075. https://doi.org/10.3390/s25227075
Chicago/Turabian StyleHsieh, Katherine L., Deborah Backus, T. Bradley Willingham, and Jon Sanford. 2025. "Development and Usability of MSafe: A Fall Risk Application for Older Adults with Multiple Sclerosis" Sensors 25, no. 22: 7075. https://doi.org/10.3390/s25227075
APA StyleHsieh, K. L., Backus, D., Willingham, T. B., & Sanford, J. (2025). Development and Usability of MSafe: A Fall Risk Application for Older Adults with Multiple Sclerosis. Sensors, 25(22), 7075. https://doi.org/10.3390/s25227075






