Aggregation Periods Influence Step Count Error in Low-Power Wearables
Highlights
- Aggregating step count into large aggregation periods significantly increases error and underestimation of step count in lower-power wearables
- Aggregation periods containing continuous walking bouts spanning the entire period are more accurate than aggregation periods containing multiple non-continuous walking bouts.
- Selection of the time aggregation period is critical for accurate step detection in a free-living environment, particularly for clinical and compliance monitoring.
- Optimizing aggregation periods for the metric of interest can improve wearable sensor performance without compromising battery life.
Abstract
1. Introduction
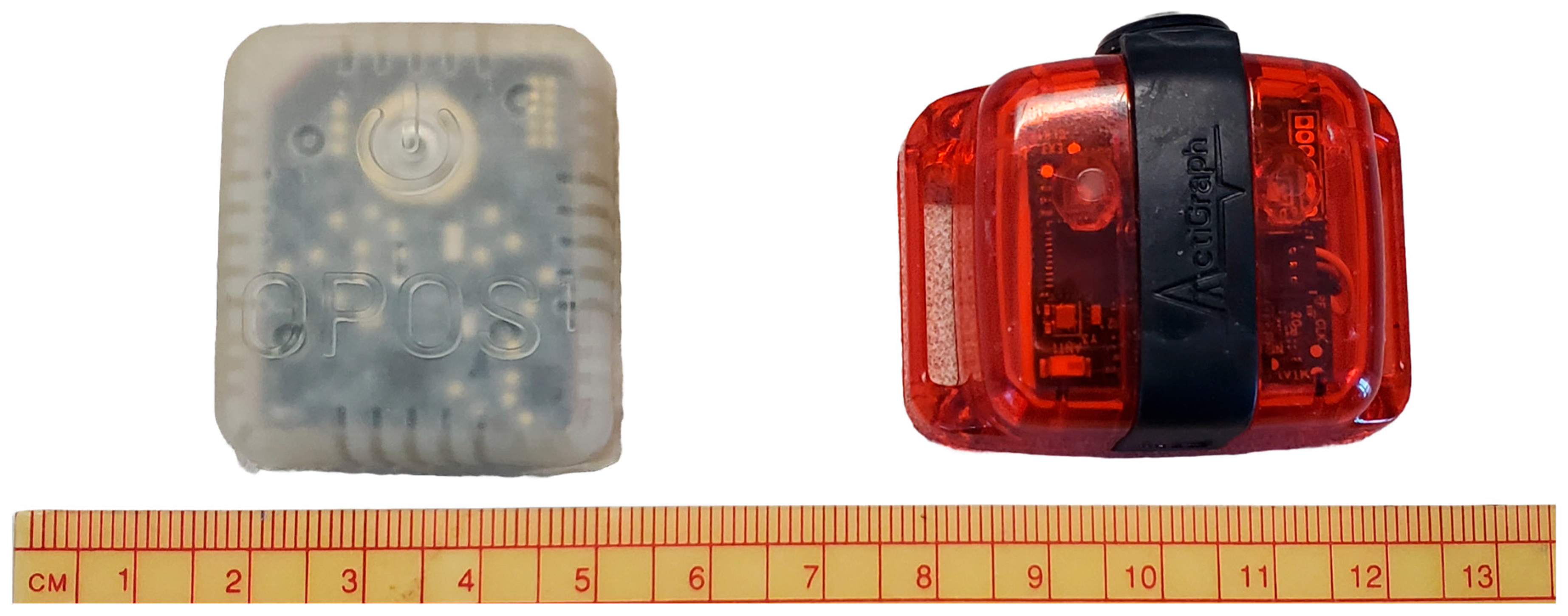
2. Materials and Methods
2.1. Data Collection
2.2. Data Processing
2.2.1. Wear Time
2.2.2. Total Step Count per Day
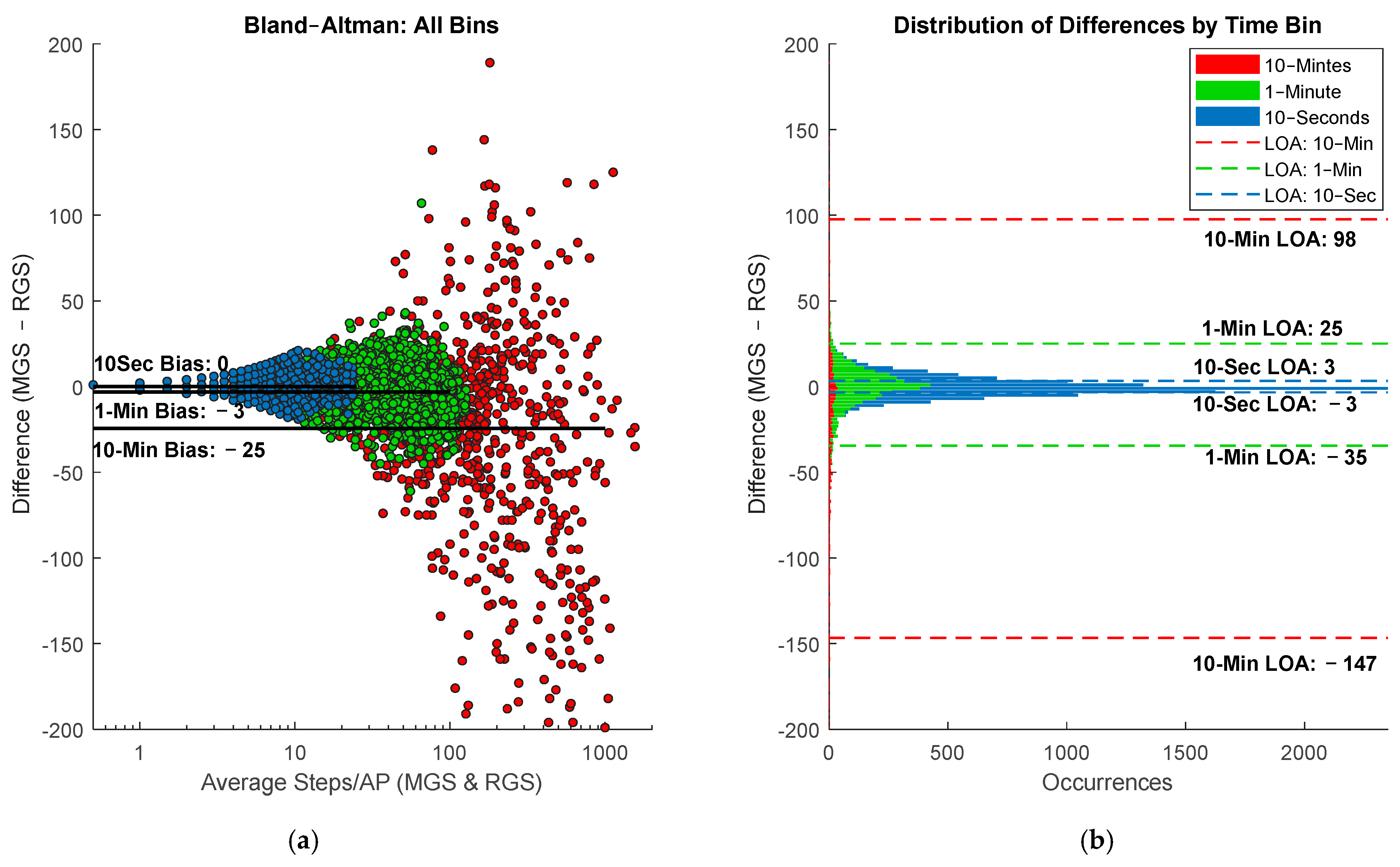
2.2.3. Aggregation Period Accuracy
2.2.4. Continuous and Non-Continuous Walking Bouts
3. Results
3.1. Wear Time
3.2. Total Steps per Day
3.3. Aggregation Period Accuracy
3.4. Continuous and Noncontinuous Walking Bouts
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AP | Aggregation Period |
| ADL | Activities of Daily Living |
| RGS | Research Grade Sensor |
| IMU | Inertial Measurement Unit |
| LCCC | Lin’s Concordance Correlation Coefficient |
| LOA | Limits of Agreement |
References
- Cooper, D.; Bhuskute, N.; Walsh, G. Exploring the Impact and Acceptance of Wearable Sensor Technology for Pre- and Postoperative Rehabilitation in Knee Replacement Patients. JBJS Open Access 2022, 7, e21. [Google Scholar] [CrossRef]
- Ghosh, A.; Nag, S.; Gomes, A.; Gosavi, A.; Ghule, G.; Kundu, A.; Purohit, B.; Srivastava, R. Applications of Smart Material Sensors and Soft Electronics in Healthcare Wearables for Better User Compliance. Micromachines 2022, 14, 121. [Google Scholar] [CrossRef]
- Adans-Dester, C.; Hankov, N.; O’bRien, A.; Vergara-Diaz, G.; Black-Schaffer, R.; Zafonte, R.; Dy, J.; Lee, S.I.; Bonato, P. Enabling precision rehabilitation interventions using wearable sensors and machine learning to track motor recovery. npj Digit. Med. 2020, 3, 121. [Google Scholar] [CrossRef]
- Stavropoulos, T.G.; Papastergiou, A.; Mpaltadoros, L.; Nikolopoulos, S.; Kompatsiaris, I. IoT Wearable Sensors and Devices in Elderly Care: A Literature Review. Sensors 2020, 20, 2826. [Google Scholar] [CrossRef]
- Strain, T.; Flaxman, S.; Guthold, R.; Semenova, E.; Cowan, M.; Riley, L.M.; Bull, F.C.; Stevens, G.A.; Raheem, R.A.; Agoudavi, K.; et al. National, regional, and global trends in insufficient physical activity among adults from 2000 to 2022: A pooled analysis of 507 population-based surveys with 5·7 million participants. Lancet Glob. Health 2024, 12, e1232–e1243. [Google Scholar] [CrossRef]
- Thatipelli, S.; Arun, A.; Chung, P.; Etemadi, M.; Heller, J.A.; Kwiat, D.; Imamura-Ching, J.; Harrison, M.R.; Roy, S. Review of Existing Brace Adherence Monitoring Methods to Assess Adherence. JPO J. Prosthetics Orthot. 2016, 28, 126–135. [Google Scholar] [CrossRef]
- Wang, X.; Yu, H.; Kold, S.; Rahbek, O.; Bai, S. Wearable sensors for activity monitoring and motion control: A review. Biomim. Intell. Robot. 2023, 3, 100089. [Google Scholar] [CrossRef]
- Toth, L.P.; Park, S.; Pittman, W.L.; Sarisaltik, D.; Hibbing, P.R.; Morton, A.L.; Springer, C.M.; Crouter, S.E.; Bassett, D.R. Effects of Brief Intermittent Walking Bouts on Step Count Accuracy of Wearable Devices. J. Meas. Phys. Behav. 2019, 2, 13–21. [Google Scholar] [CrossRef]
- Pan, J.; Wei, S. Accuracy and reliability of accelerometer-based pedometers in step counts during walking, running, and stair climbing in different locations of attachment. Sci. Rep. 2024, 14, 27761. [Google Scholar] [CrossRef]
- Lundell, S.; Kaufman, K.R. Mechanical Method for Rapid Determination of Step Count Sensor Settings. Bioengineering 2024, 11, 547. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef]
- Toth, L.P.; Park, S.; Pittman, W.L.; Sarisaltik, D.; Hibbing, P.R.; Morton, A.L.; Springer, C.M.; Crouter, S.E.; Bassett, D.R. Validity of Activity Tracker Step Counts during Walking, Running, and Activities of Daily Living. Transl. J. Am. Coll. Sports Med. 2018, 3, 52–59. [Google Scholar] [CrossRef]
- Brodie, M.A.D.; Coppens, M.J.M.; Lord, S.R.; Lovell, N.H.; Gschwind, Y.J.; Redmond, S.J.; Del Rosario, M.B.; Wang, K.; Sturnieks, D.L.; Persiani, M.; et al. Wearable pendant device monitoring using new wavelet-based methods shows daily life and laboratory gaits are different. Med. Biol. Eng. Comput. 2016, 54, 663–674. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.J.; Zhong, W.H.; Liu, Y.X.; Miao, H.Z.; Li, Y.C.; Ji, M.H. Sample Size for Assessing Agreement between Two Methods of Measurement by Bland−Altman Method. Int. J. Biostat. 2016, 39, 20150039. [Google Scholar] [CrossRef] [PubMed]
- Fortune, E.; Lugade, V.; Morrow, M.; Kaufman, K. Validity of using tri-axial accelerometers to measure human movement—Part II: Step counts at a wide range of gait velocities. Med. Eng. Phys. 2014, 36, 659–669. [Google Scholar] [CrossRef]
- Kruskal, W.H.; Wallis, W.A. Use of Ranks in One-Criterion Variance Analysis. J. Am. Stat. Assoc. 1952, 47, 583–621. [Google Scholar] [CrossRef]
- Smith, M.W.; Ma, J.; Stafford, R.S. Bar charts enhance Bland–Altman plots when value ranges are limited. J. Clin. Epidemiology 2010, 63, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Orendurff, M.S. How humans walk: Bout duration, steps per bout, and rest duration. J. Rehabilitation Res. Dev. 2008, 45, 1077–1090. [Google Scholar] [CrossRef]
- Gomersall, S.R.; Ng, N.; Burton, N.W.; Pavey, T.G.; Gilson, N.D.; Brown, W.J. Estimating Physical Activity and Sedentary Behavior in a Free-Living Context: A Pragmatic Comparison of Consumer-Based Activity Trackers and ActiGraph Accelerometry. J. Med. Internet Res. 2016, 18, e239. [Google Scholar] [CrossRef]
- An, H.; Jones, G.C.; Kang, S.; Welk, G.J.; Lee, J. How valid are wearable physical activity trackers for measuring steps? Eur. J. Sport Sci. 2017, 17, 360–368. [Google Scholar] [CrossRef]
- Wong, C.K.; Mentis, H.M.; Kuber, R. The bit doesn’t fit: Evaluation of a commercial activity-tracker at slower walking speeds. Gait Posture 2018, 59, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Orendurff, M.S.; Segal, A.D.; Berge, J.S.; Flick, K.C.; Spanier, D.; Klute, G.K. The kinematics and kinetics of turning: Limb asymmetries associated with walking a circular path. Gait Posture 2006, 23, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Himann, J.E.; Cunningham, D.A.; Rechnitzer, P.A.; Paterson, D.H. Age-related changes in speed of walking. Med. Sci. Sports Exerc. 1988, 20, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Han, H.; Kim, H.; Sun, W.; Malaska, M.; Miller, B. Validation of wearable activity monitors for real-time cadence. J. Sports Sci. 2020, 38, 383–389. [Google Scholar] [CrossRef]



| Range of Total Steps/Bin | All Bins Bias (LOA) | 10-Min Bias (LOA) | 1-Min & 10-Min Bias (LOA) | 1-Min Bias (LOA) | 10-s & 1-Min Bias (LOA) | 10-s Bias (LOA) | 10-Min & 10-s Bias (LOA) |
|---|---|---|---|---|---|---|---|
| 0–10 | 0 (−10, 9) | −1 (−9, 7) | 0 † (−12, 11) | 0 * (−12, 11) | −2 (−11, 8) | −2 (−11, 8) | −2 (−11, 8) |
| 10–20 | 0 (−11, 11) | −1 (−25, 24) | 1 (−14, 16) | 1 (−14, 15) | −1 (−20, 11) | −1 (−10, 8) | −1 (−10, 8) |
| 20–40 | 1 (−24, 27) | −8 (−43.0, 27) | 1 (−26, 28) | 3 (−22, 27) | 3 (−20, 25) | 3 (−7, 11) | −3 (−31, 25) |
| 40–100 | −4 (−49, 40) | −13 * (−81, 45) | −4 (−49, 40) | −1 (−33, 30) | −1 † (−33, 30) | NA | −13 † (−81, 54) |
| 100–200 | −15 (−95, 66) | −19.0 (−123, 85) | −14.8 (−95.5, 66) | −9.0 (−36, 8) | −9.0 † (−36, 8) | NA | −19 † (−123, 85) |
| 200–400 | −30 † (−162, 101) | −30 (−162,101) | −30 † (−162, 101) | NA | NA | NA | −30 † (−162, 101) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lundell, S.; Kaufman, K.R. Aggregation Periods Influence Step Count Error in Low-Power Wearables. Sensors 2025, 25, 6998. https://doi.org/10.3390/s25226998
Lundell S, Kaufman KR. Aggregation Periods Influence Step Count Error in Low-Power Wearables. Sensors. 2025; 25(22):6998. https://doi.org/10.3390/s25226998
Chicago/Turabian StyleLundell, Sydney, and Kenton R. Kaufman. 2025. "Aggregation Periods Influence Step Count Error in Low-Power Wearables" Sensors 25, no. 22: 6998. https://doi.org/10.3390/s25226998
APA StyleLundell, S., & Kaufman, K. R. (2025). Aggregation Periods Influence Step Count Error in Low-Power Wearables. Sensors, 25(22), 6998. https://doi.org/10.3390/s25226998





