An Exploratory Study on Virtual Reality Technology for Fall Prevention in Older Adults with Mild Cognitive Impairment
Abstract
Highlights
- The Virtual Reality (VR) training program has positive training effects on fall prevention for older adults with MCI.
- The VR technology supports a useful cognitive-motor training on fall prevention for older population.
- Health professions can support the creation, inclusion, and adoption of accessible sensing technologies in aged care and rehabilitation services.
- Fall prevention assisted by the VR training can provide a new training approach in preventing falls for older adults with MCI.
Abstract
1. Introduction
2. Methods
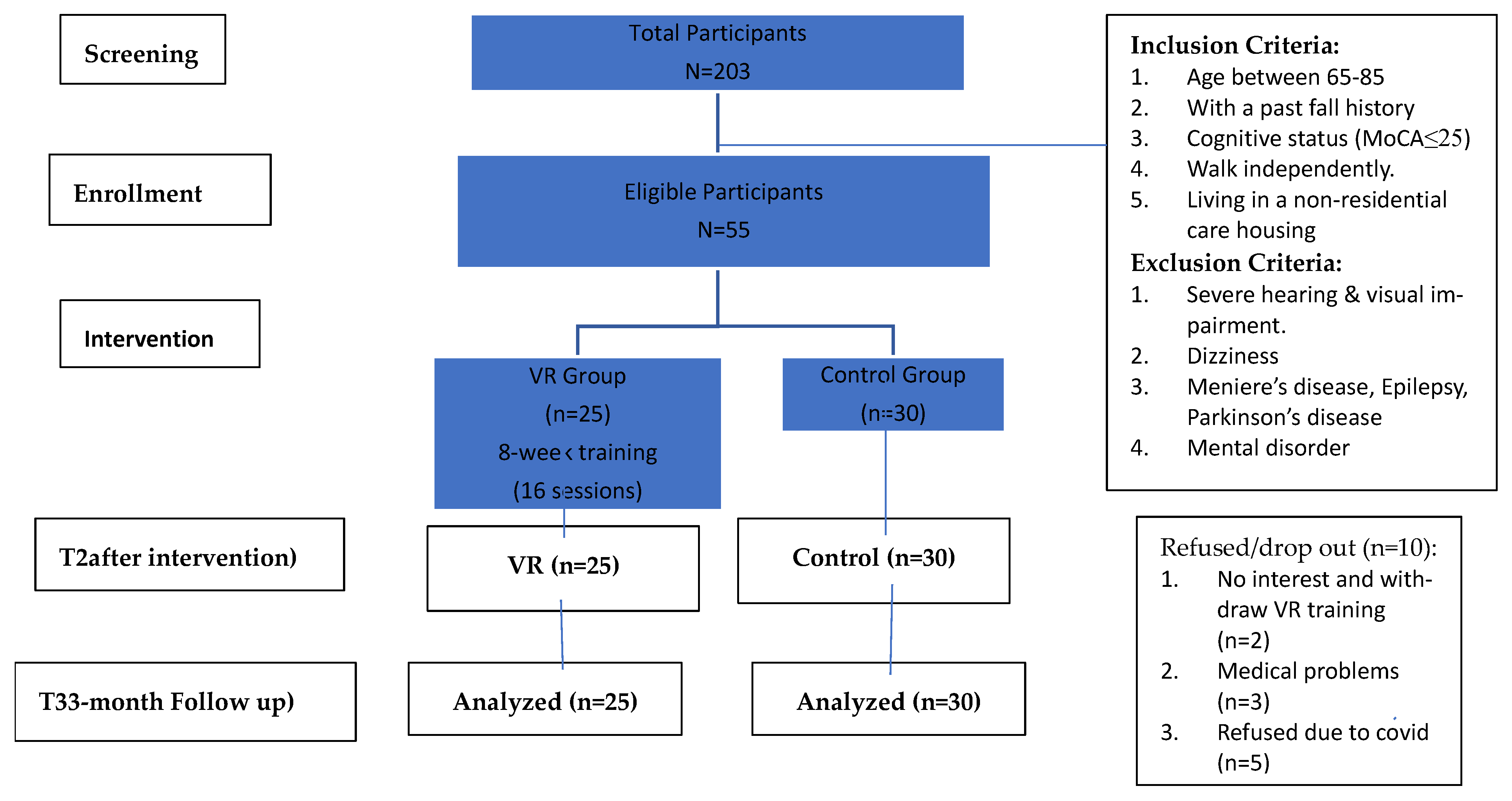
2.1. Participants
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Intervention
2.5. Procedure
2.6. Data Collection and Outcome Measures
2.7. Cognitive Measures
2.8. Physical Measures
2.9. Psychological Consideration
2.10. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Demographic Data (Health Outcomes)
4. Discussion
4.1. Overview
4.2. Full Immersive VR CAVE Training on Falls Prevention
4.3. Training Effects of VR Training for Fall Prevention
4.4. Challenges and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Montero-Odasso, M.; Van Der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Masud, T. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Step Safely: Strategies for Preventing and Managing Falls Across the Life-Course; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Myers, A.H.; Baker, S.P.; Van Natta, M.L.; Abbey, H.; Robinson, E.G. Risk factors associated with falls and injuries among elderly institutionalized persons. Am. J. Epidemiol. 1991, 133, 1179–1190. [Google Scholar] [CrossRef]
- Muir, S.W.; Gopaul, K.; Montero Odasso, M.M. The role of cognitive impairment in fall risk among older adults: A systematic review and meta-analysis. Age Ageing 2012, 41, 299–308. [Google Scholar] [CrossRef]
- Thapa, N.; Park, H.J.; Yang, J.; Son, H.; Lee, M.J.; Kang, S.W.; Park, K.W.; Park, H. The Effect of a Virtual Reality-Based Intervention Program on Cognitive in Older Adults with Mild Cognitive Impairment: A Randomized Control Trial. J. Clin. Med. 2020, 9, 1283. [Google Scholar] [CrossRef]
- Miranda-Duro, M.D.C.; Nieto-Riveiro, L.; Concheiro-Moscoso, P.; Groba, B.; Pousada, T.; Canosa, N.; Pereira, J. Occupational therapy and the use of technology on older adult fall prevention: A scoping review. Int. J. Environ. Res. Public Health 2021, 18, 702. [Google Scholar] [CrossRef] [PubMed]
- Mirelman, A.; Rochester, L.; Maidan, I.; Del Din, S.; Alcock, L.; Nieuwhof, F.; Hausdorff, J.M. Addition of a non-immersive virtual reality component to treadmill training to reduce fall risk in older adults (V-TIME): A randomized controlled trial. Lancet 2016, 388, 1170–1182. [Google Scholar] [CrossRef] [PubMed]
- Elliott, S.; Leland, N.E. Occupational therapy falls prevention interventions for community-dwelling older adults: A systematic review. Am. J. Occup. Ther. 2018, 72, 7204190040p1–7204190040p11. [Google Scholar] [CrossRef] [PubMed]
- Liddle, J. Considering inclusion in digital technology: An occupational therapy role and responsibility. Aust. Occup. Ther. J. 2023, 70, 157–158. [Google Scholar] [CrossRef]
- Gao, Z.; Lee, J.; McDonough, D. Virtual Reality Exercise a Coping Strategy for Health and Wellness Promotion in Older Adults during the COVID-19 Pandemic. J. Clin. Med. 2020, 9, 1986. [Google Scholar] [CrossRef]
- Baus, O.; Bouchard, S. Moving from virtual reality exposure-based therapy to augmented reality exposure-based therapy: A review. Front. Hum. Neurosci. 2014, 8, 112. [Google Scholar] [CrossRef]
- Mirelman, A.; Maidan, I.; Shiratzky, S.S.; Hausdorff, J.M. Virtual Reality Training as an Intervention to Reduce Falls. In Falls and Cognition in Older Persons; Montero-Odasso, M., Camicioli, R., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Boulton, E.; Hawley-Hague, H.; French, D.P.; Mellone, S.; Zacchi, A.; Clemson, L.; Todd, C. Implementing behaviour change theory and techniques to increase physical activity and prevent functional decline among adults aged 61–70: The PreventIT project. Prog. Cardiovasc. Dis. 2019, 62, 147–156. [Google Scholar] [CrossRef]
- Ohman, H.; Savikko, N.; Strandberg, T.E. Effects of exercise on cognition: The Finnish Alzheimer disease exercise trial: A randomized, controlled trial. J. Am. Geriatr. Soc. 2016, 64, 731–738. [Google Scholar] [CrossRef] [PubMed]
- Montero-Odasso, M.; Camicioli, R. Falls and Cognition in Older Persons: Fundamentals, Assessment and Therapeutic Options; Springer Nature: Berlin, Germany, 2019. [Google Scholar]
- Bourrelier, J.; Ryard, J. Use of a virtual environment to engage motor and postural abilities in elderly subjects with and without mild cognitive impairment (MAAMI Project). IRBM 2016, 37, 75–80. [Google Scholar] [CrossRef]
- Hamm, J.; Money, A.G.; Atwal, A.; Paraskevopoulos, I. Fall prevention intervention technologies: A conceptual framework and survey of the state of the art. J. Biomed. Inform. 2016, 59, 319–345. [Google Scholar] [CrossRef] [PubMed]
- Theodoropoulos, A.; Stavropoulou, D.; Papadopoulos, P.; Platis, N.; Lepouras, G. Developing an interactive VR CAVE for immersive shared gaming experiences. Virtual Worlds 2023, 2, 162–181. [Google Scholar] [CrossRef]
- Ip, W.K.; Soar, J.; James, C.; Wang, Z.; Fong, K.N. Innovative virtual reality (VR) application for preventing of falls among Chinese older adults: A usability and acceptance exploratory study. Hum. Behav. Emerg. Technol. 2024, 2024, 5556767. [Google Scholar] [CrossRef]
- Tuena, C.; Serino, S.; Stramba-Badiale, C.; Pedroli, E.; Goulene, K.M.; Stramba-Badiale, M.; Riva, G. Usability of an embodied CAVE system for spatial navigation training in mild cognitive impairment. J. Clin. Med. 2023, 12, 1949. [Google Scholar] [CrossRef]
- Ip, W.K.; Soar, J.; James, C.; Wang, S.Y.; Fong, K.N. Virtual reality game-based training for preventing falls among community-dwelling older adults with mild cognitive impairment: A pilot randomized control trial study. Virtual Real. 2025, 29, 18. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Report on Falls Prevention in Older Age. World Health Organization. 2008. Available online: https://apps.who.int/iris/handle/10665/43811 (accessed on 17 March 2008).
- Scheffer, A.C.; Schuurmans, M.J.; van Dijk, N.; van der Hooft, T.; de Rooij, S.E. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing 2008, 37, 19–24. [Google Scholar] [CrossRef]
- Yardley, L.; Beyer, N.; Hauer, K.; Kempen, G.; Piot-Ziegler, C.; Todd, C. Development and initial validation of the Falls Efficacy Scale-International (FES-I). Age Ageing 2005, 34, 614–619. [Google Scholar] [CrossRef]
- Yeung, P.Y.; Wong, L.L.; Chan, C.C.; Yung, C.Y.; Leung, L.J.; Tam, Y.Y.; Lau, M.L. Montreal cognitive assessment—Single cutoff achieves screening purpose. Neuropsychiatr. Dis. Treat. 2020, 2020, 2681–2687. [Google Scholar] [CrossRef]
- Lei, L.; Erin, D.B. Performance on Original and a Chinese Version of Trail Making Test Part B: A Normative Bilingual Sample. Appl. Neuropsychol. 2000, 7, 243–246. [Google Scholar] [CrossRef]
- Beck Jepsen, D.; Robinson, K.; Ogliari, G.; Montero-Odasso, M.; Kamkar, N.; Ryg, J.; Freiberger, E. Predicting falls in older adults: An umbrella review of instruments assessing gait, balance, and functional mobility. BMC Geriatr. 2022, 22, 615. [Google Scholar] [CrossRef]
- Muir, S.W.; Berg, K.; Chesworth, B.; Speechley, M. Use of the Berg Balance Scale for predicting multiple falls in community-dwelling elderly people: A prospective study. Phys. Ther. 2008, 88, 449–459. [Google Scholar] [CrossRef]
- Bischoff, H.A.; Stähelin, H.B.; Monsch, A.U.; Iversen, M.D.; Weyh, A.; Von Dechend, M.; Theiler, R. Identifying a cut-off point for normal mobility: A comparison of the timed ‘up and go’ test in community-dwelling and institutionalized elderly women. Age Ageing 2003, 32, 315–320. [Google Scholar] [CrossRef]
- Nieminen, P. Ten points for high-quality statistical reporting and data presentation. Appl. Sci. 2020, 10, 3885. [Google Scholar] [CrossRef]
- Sarah, A.C.; Jodi, M.H.; Jacob, D.; Bolzenius, L.E.; Salminen, L.M.; Baker, S.S.; Robert, H.P. Longitudinal Change in Performance on the Montreal Cognitive Assessment in Older Adults. Clin. Neuropsychol. 2015, 29, 824–835. [Google Scholar] [CrossRef]
- Kim, O.; Pang, Y.; Kim, J.H. The effectiveness of virtual reality for people with mild cognitive impairment or dementia: A meta-analysis. BMC Psychiatry 2019, 19, 219. [Google Scholar] [CrossRef]
- Kwan, R.Y.C.; Liu, J.Y.W.; Fong, K.N.K.; Qin, J.; Leung, P.K.; Sin, O.S.K.; Lai, C.K. Feasibility and Effects of Virtual Reality Motor-Cognitive Training in Community-Dwelling Older People With Cognitive Frailty: Pilot Randomized Controlled Trial. JMIR Serious Games 2021, 9, e28400. [Google Scholar] [CrossRef]
- Ng, Y.L.; Ma, F.; Ho, F.K.; Ip, P.; Fu, K.W. Effectiveness of virtual and augmented reality-enhanced exercise on physical activity, psychological outcomes, and physical performance: A systematic review and meta-analysis of randomized controlled trials. Comput. Hum. Behav. 2019, 99, 278–291. [Google Scholar] [CrossRef]
- Law, L.L.; Barnett, F.; Yau, M.K.; Gray, M.A. Effects of combined cognitive and exercise interventions on cognition in older adults with and without cognitive impairment: A systematic review. Ageing Res. Rev. 2014, 15, 61–75. [Google Scholar] [CrossRef] [PubMed]
- Stanmore, E.K.; Mavroeidi, A.; de Jong, L.D.; Skelton, D.A.; Sutton, C.J.; Benedetto, V.; Todd, C. The effectiveness and cost-effectiveness of strength and balance Exergames to reduce falls risk for people aged 55 years and older in UK assisted living facilities: A multi-centre, cluster randomized controlled trial. BMC Med. 2019, 17, 49. [Google Scholar] [CrossRef]
- Yang, C.M.; Hsieh, J.S.C.; Chen, Y.C.; Yang, S.Y.; Lin, H.C.K. Effects of Kinect exergames on balance training among community older adults: A randomized controlled trial. Medicine 2020, 99, e21228. [Google Scholar] [CrossRef] [PubMed]
- Irazoki, E.; Contreras-Somoza, L.M.; Toribio-Guzman, J.M.; Jenaro-Rio, C.; van der Roest, H.; Franco-Martin, M.A. Technologies for Cognitive Training and Cognitive Rehabilitation for People With Mild Cognitive Impairment and Dementia. A Systematic Review. Front. Psychol. 2020, 11, 648. [Google Scholar] [CrossRef] [PubMed]
- Delbaere, K.; Kochan, N.A.; Close, J.C.; Menant, J.C.; Sturnieks, D.L.; Brodaty, H.; Lord, S.R. Mild cognitive impairment as a predictor of falls in community-dwelling older people. Am. J. Geriatr. Psychiatry 2012, 20, 845–853. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Speechley, M. Falls in cognitively impaired older adults: Implications for risk assessment and prevention. J. Am. Geriatr. Soc. 2018, 66, 367–375. [Google Scholar] [CrossRef]
- Fu, A.S.; Gao, K.L.; Tung, A.K.; Tsang, W.W.; Kwan, M.M. Effectiveness of exergaming training in reducing risk and incidence of falls in frail older adults with a history of falls. Arch. Phys. Med. Rehabil. 2015, 96, 2096–2102. [Google Scholar] [CrossRef]
- Welmer, A.K.; Rizzuto, D.; Laukka, E.J.; Johnell, K.; Fratiglioni, L. Cognitive and physical function in relation to the risk of injurious falls in older adults: A population-based study. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 2017, 72, 669–675. [Google Scholar] [CrossRef]
- Chau, P.H.; Kwok, Y.Y.J.; Chan, M.K.M.; Kwan, K.Y.D.; Wong, K.L.; Tang, Y.H.; Leung, M.K. Feasibility, acceptability, and efficacy of virtual reality training for older adults and people with disabilities: Single-arm pre-post study. J. Med. Internet Res. 2021, 23, e27640. [Google Scholar] [CrossRef]
- Zahabi, M.; Abdul Razak, A.M. Adaptive virtual reality-based training: A systematic literature review and framework. Virtual Real. 2020, 24, 725–752. [Google Scholar] [CrossRef]
- Nikolopoulou, K. What Is Convenience Sampling?|Definition & Examples. Scribbr. 2022. Available online: https://www.scribbr.com/methodology/convenience-sampling/ (accessed on 8 August 2022).
- World Health Organization. Falls. Geneva, Switzerland. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 21 June 2021).
- Morello, R.T.; Soh, S.E.; Behm, K.; Egan, A.; Ayton, D.; Hill, K.; Barker, A.L. Multifactorial falls prevention programs for older adults presenting to the emergency department with a fall: Systematic review and meta-analysis. Inj. Prev. 2019, 25, 557–564. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Intervention (n = 25) | Control (n = 30) | * p Value |
|---|---|---|---|
| Age (years), M (SD) | 71.96 (5.11) | 77.23 (4.59) | 0.067 |
| Gender n (%) | 0.180 | ||
| Male | 20% | ||
| Female | 100% | 80% | |
| Education Level (years), n (%) | 0.179 | ||
| Primary or below | 40% | 53.3% | |
| 60% | 46.7% | ||
| Living Status, n (%) | 0.208 | ||
| Alone | 24% | 40% | |
| With family | 76% | 60% | |
| History of Fall, n (%) | 0.218 | ||
| <12 months | 53.6% | 33% | |
| >12 months | 46.4% | 67% | |
| History of Chronic Pain, n (%) | 0.418 | ||
| Yes | 44% | 33% | |
| No | 56% | 67% | |
| History of Fracture, n (%) | 0.104 | ||
| Yes | 40% | 20% | |
| No | 60% | 80% | |
| History of Osteoporosis, n (%) | 0.311 | ||
| Yes | 35.3% | 50% | |
| No. | 64.7% | 50% |
| Outcomes, M a + SD b | ||||
|---|---|---|---|---|
| Variables | All (N = 55) | Intervention (n = 25) | Control (n = 30) | p Value < 0.05 |
| Cognition: HK-MoCA c | 21.22 | 22.68 (0.69) | 20.00 (0.63) | 0.006 |
| Executive Function | ||||
| Trail Making Test A (TMT-A) | 67.91 | 65.84 (8.45) | 69.63 (7.71) | 0.742 |
| Trail Making Test B (TMT-B) | 112.64 | 104.28 (75.44) | 119.61 (69.60) | 0.421 |
| Time Up and Go Test (TUG) | 13.41 | 11.48 (0.93) | 15.01 (0.85) | 0.007 |
| Berg Balance Scale (BBS) | 50.71 | 50.71 (0.98) | 50.70 (0.90) | 0.988 |
| 6-min walk test (6 MWT) | 310.51 | 318.52 (12.18) | 303.84 (12.03) | 0.415 |
| Fall Efficacy Scale International (FES-I) | 40.11 | 43.04 (2.31) | 37.16 (2.10) | 0.043 |
| Outcome Measures | Group | Pre-Test | M + SD Post-Test | Follow Up | Multivariate | Univariate Within Group | * p < 0.05 Between Group |
|---|---|---|---|---|---|---|---|
| Cognition (HK-MoCA) | VR Control | 22.68 (0.69) 20.00 (0.63) | 25.72 (0.79) 20.97 (0.72) | 25.96 (0.81) 21.2 (0.74) | 0.008 ** | 0.000 ** | 0.000 ** |
| Executive Function TMT-A TMT-B | VR Control VR Control | 65.85 (8.45) 69.63 (7.14) 104.28 (13.96) 119.61 (12.74) | 47.29 (6.93) 61.68 (6.32) 83.16 (14.49) 109.83 (13.22) | 42.94 (6.24) 64.52 (6.07) 72.88 (15.41) 140.01 (14.66) | 0.038 * 0.006 ** | 0.000 ** 0.172 | 0.038 * 0.041 * |
| Balance Level BBS | VR Control | 50.72 (0.98) 50.70 (0.90) | 52.84 (1.65) 47.33 (1.15) | 53.21 (1.16) 50.13 (1.05) | 0.032 * | 0.311 | 0.047 * |
| Walk Speed 6 MWT | VR Control | 318.51 (13.18) 303.84 (12.03) | 365.10 (12.82) 298.42 (11.07) | 373.68 (13.02) 305.19 (11.89) | 0.001 ** | 0.002 ** | 0.002 ** |
| Functional Mobility TUG | VR Control | 11.48 (0.93) 15.01 (0.85) | 9.27 (0.56) 12.61 (0.51) | 8.46 (0.71) 12.07 (0.66) | 0.938 | 0.000 ** | 0.000 ** |
Fear of Fall (FES-I) | VR Control | 43.64 (2.31) 37.16 (2.10) | 39.00 (2.35) 38.80 (2.15) | 33.48 (2.01) 33.53 (1.84) | 0.148 | 0.001 ** | 0.299 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ip, W.K.; Soar, J.; Fong, K.; Wang, S.-Y.; James, C. An Exploratory Study on Virtual Reality Technology for Fall Prevention in Older Adults with Mild Cognitive Impairment. Sensors 2025, 25, 3123. https://doi.org/10.3390/s25103123
Ip WK, Soar J, Fong K, Wang S-Y, James C. An Exploratory Study on Virtual Reality Technology for Fall Prevention in Older Adults with Mild Cognitive Impairment. Sensors. 2025; 25(10):3123. https://doi.org/10.3390/s25103123
Chicago/Turabian StyleIp, Wing Keung, Jeffrey Soar, Kenneth Fong, Szu-Yao Wang, and Christina James. 2025. "An Exploratory Study on Virtual Reality Technology for Fall Prevention in Older Adults with Mild Cognitive Impairment" Sensors 25, no. 10: 3123. https://doi.org/10.3390/s25103123
APA StyleIp, W. K., Soar, J., Fong, K., Wang, S.-Y., & James, C. (2025). An Exploratory Study on Virtual Reality Technology for Fall Prevention in Older Adults with Mild Cognitive Impairment. Sensors, 25(10), 3123. https://doi.org/10.3390/s25103123







