Ballistocardial Signal-Based Personal Identification Using Deep Learning for the Non-Invasive and Non-Restrictive Monitoring of Vital Signs
Abstract
1. Introduction
2. Materials and Methods
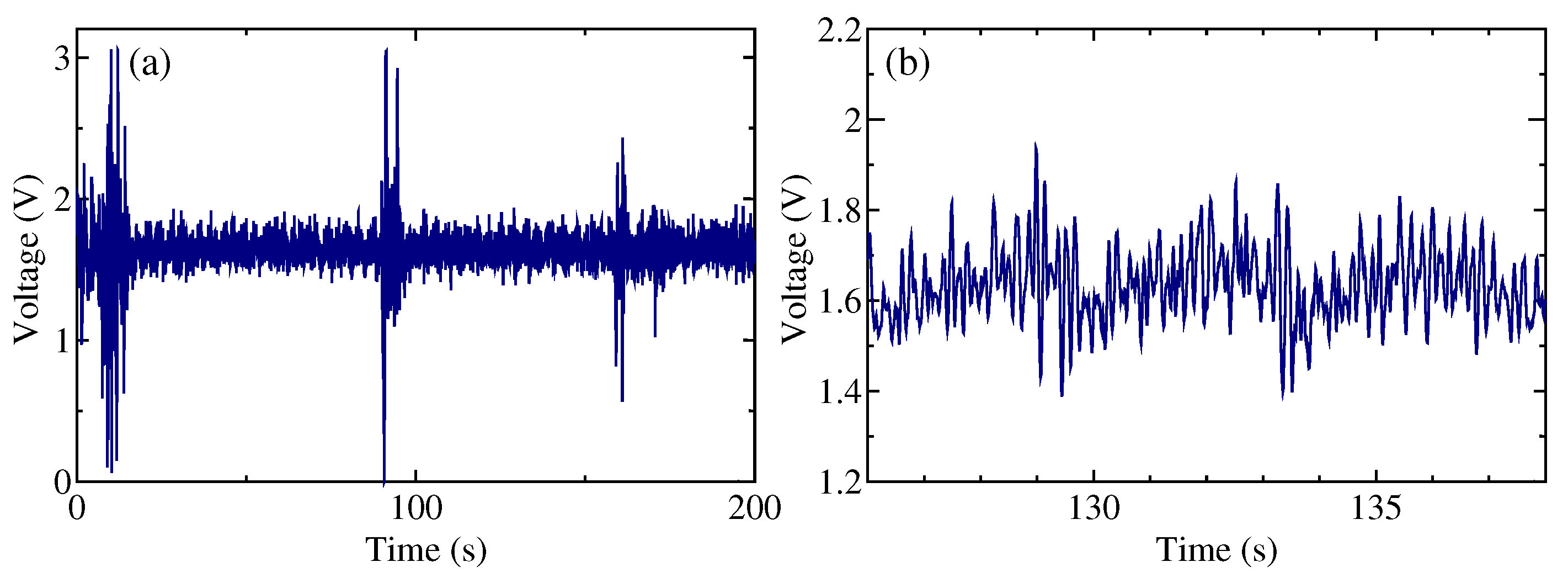
2.1. Ballistocardial Measuring Device
2.2. Measurement Procedures
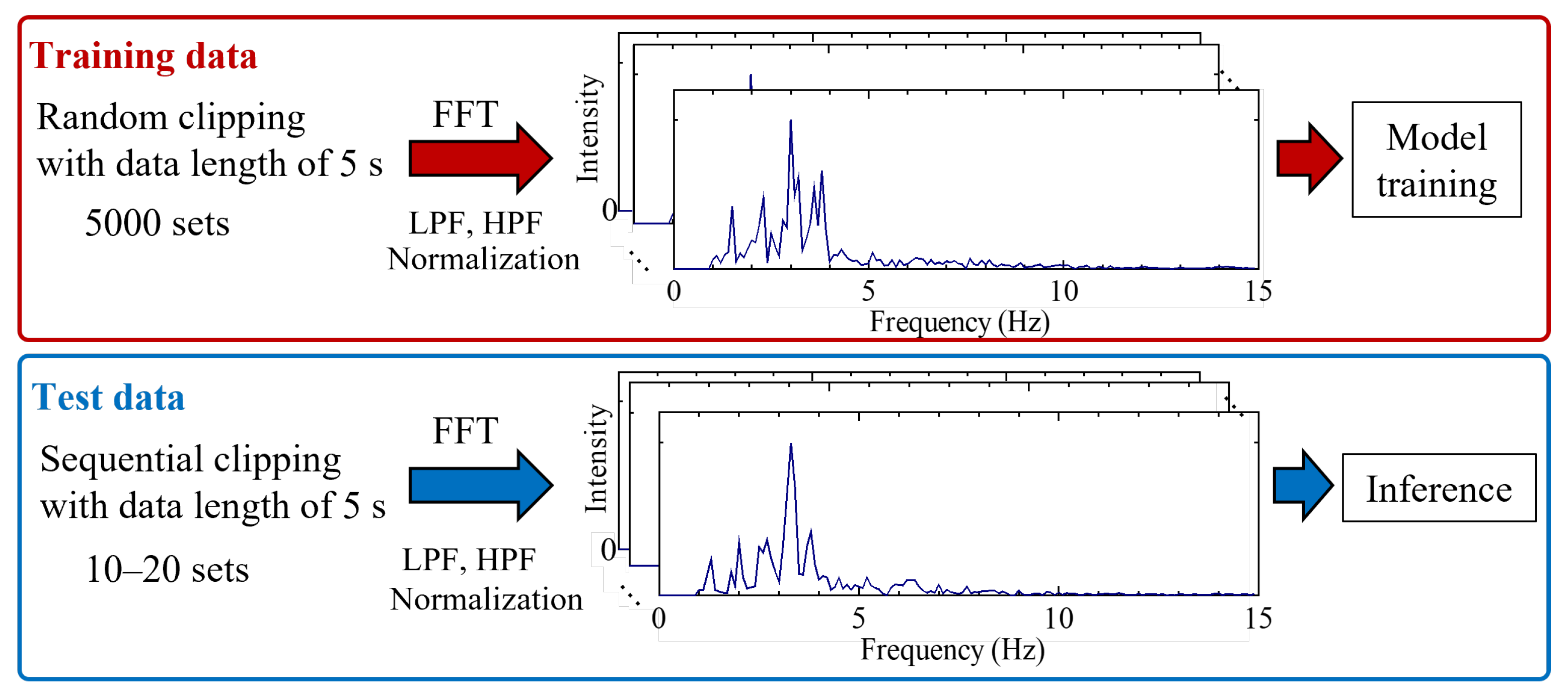
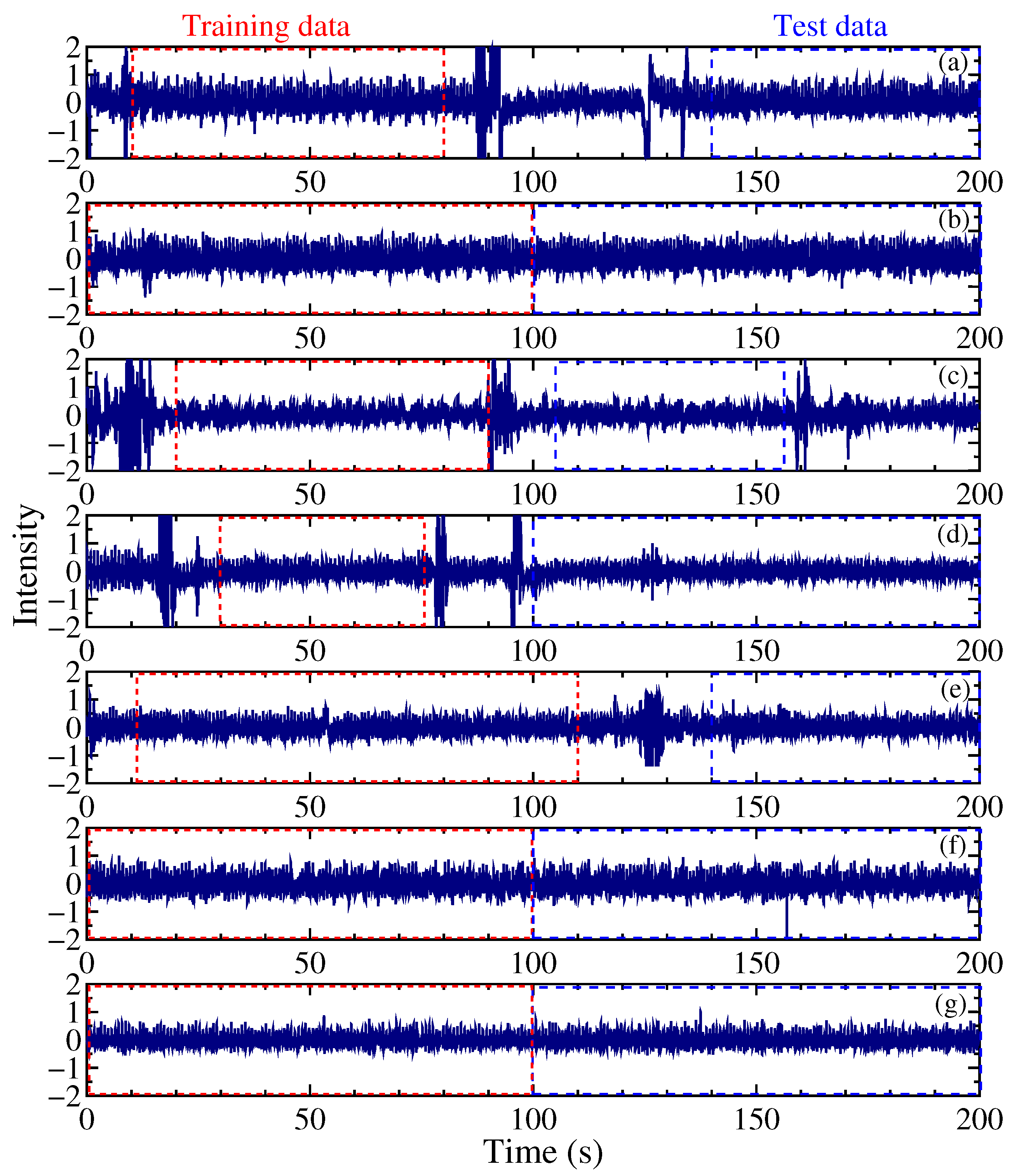
2.3. Workflow for Training Datasets
2.4. Workflow for Training Models
3. Results and Discussion
3.1. Processing Time
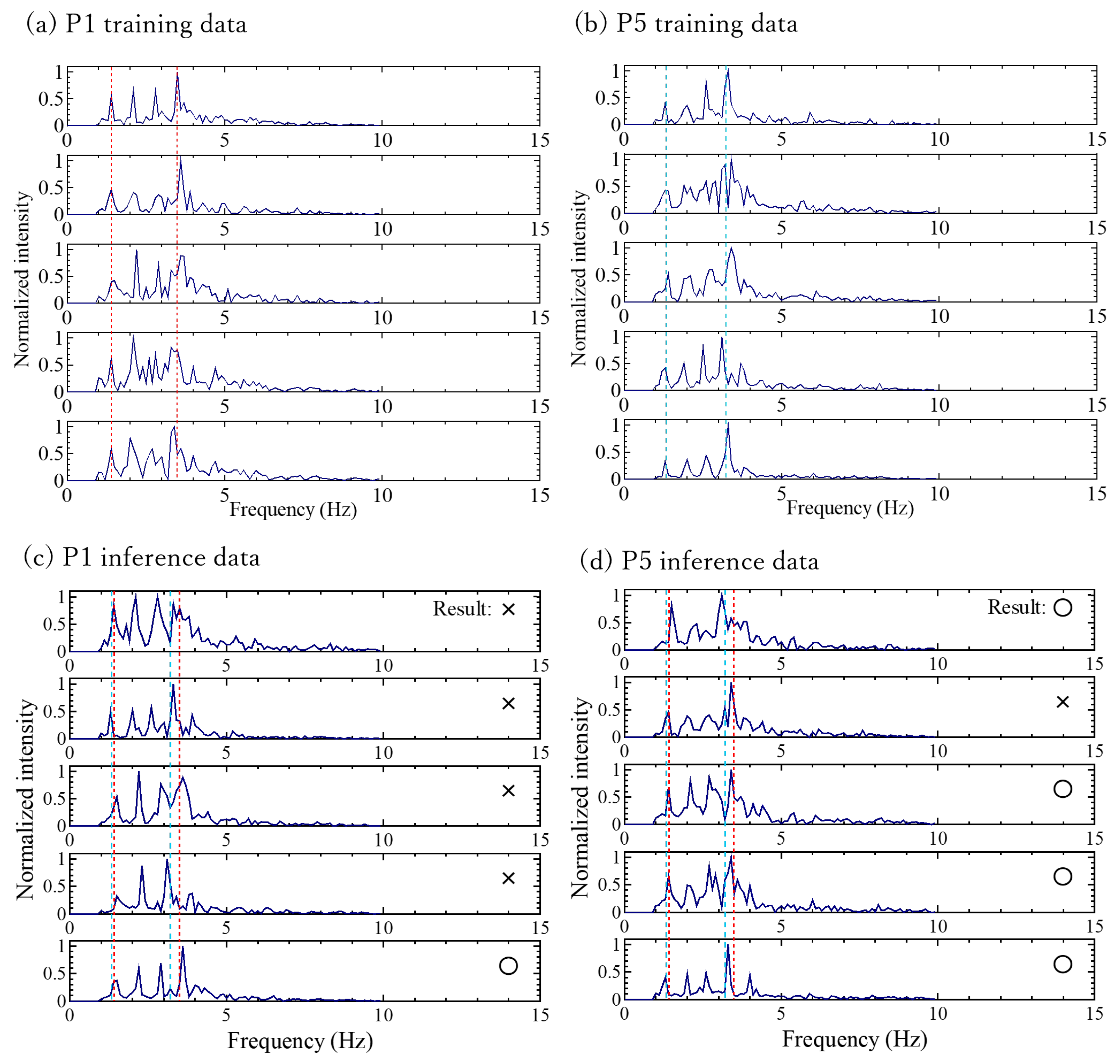
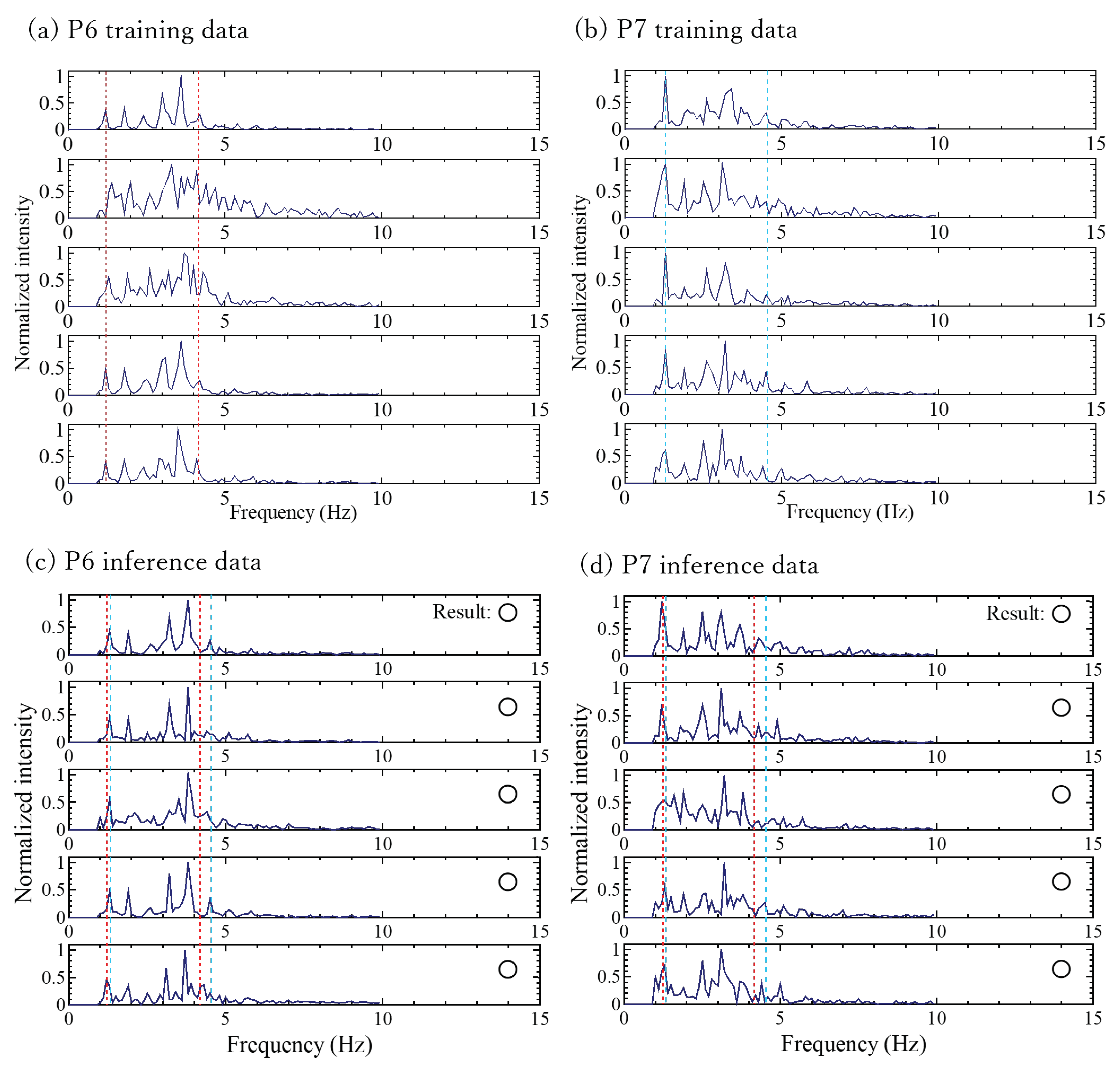
3.2. Accuracy for Personal Identification
- (1)
- Frequency spectral similarity: The variation in the dissimilarity between the frequency spectral similarities of individuals makes it difficult to distinguish individuals who exhibit similarity. To enhance the classification, it might be feasible to incorporate secondary information sources, such as the heart rate, rather than relying solely on the frequency spectra.
- (2)
- Failure to extract frequency-spectrum components (measurement instability): It is conceivable that the frequency-spectrum components cannot be reliably extracted. Occasionally, appropriate ballistrocardial signals were not obtained, such as when the subject had just repositioned themselves or in cases of a slight movement. In such cases, identification can be improved by continually scrutinizing the classification information based on the spectra of the preceding and subsequent timeframes. Persistent differences in the identifier over a certain duration could signify the presence of another person assuming the seat. However, momentary variations suggest that an appropriate BCG signal was not detected, prompting the need for identifier adjustment. This iterative approach could enhance the personal identification performance.
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| BCG | Ballistocardiogram |
| BBI | Beat-to-beat intervals |
| FFT | Fast Fourier transformed |
| ReLU | Rectified liner unit |
References
- Bharucha, A.J.; London, A.J.; Barnard, D.; Wactlar, H.; Dew, M.A.; Reynolds, C.F., III. Ethical Considerations in the Conduct of Electronic Surveillance Research. J. Law Med. Ethics 2006, 34, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Kaye, J.A.; Maxwell, S.A.; Mattek, N.; Hayes, T.L.; Dodge, H.; Pavel, M.; Jimison, H.B.; Wild, K.; Boise, L.; Zitzelberger, T.A. Intelligent Systems for Assessing Aging Changes: Home-Based, Unobtrusive, and Continuous Assessment of Aging. J. Gerontol. B Psychol. Sci. Soc. Sci. 2011, 66B, i180–i190. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-C.; Hsu, Y.-L. Remote monitoring and assessment of daily activities in the home environment. J. Clin. Gerontol. Geriatr. 2012, 3, 97–104. [Google Scholar] [CrossRef]
- Mahoney, D.M.F.; Mutschler, P.H.; Tarlow, B.; Liss, E. Real world implementation lessons and outcomes from the Worker Interactive Networking (WIN) project: Workplace-based online caregiver support and remote monitoring of elders at home. Telemed. e-Health 2008, 14, 224–234. [Google Scholar] [CrossRef] [PubMed]
- Koketsu, T.; Ohno, Y.; Ishihara, T.; Nishimoto, Y.; Kobayashi, K. Monitoring Living Activities of the Elderly Living Alone Using a Lifeline. Jpn. J. Appl. IT Healthc. 2018, 13, 12–19. [Google Scholar]
- Tsukiyama, T. In-home Health Monitoring System for Solitary Elderly. Procedia Comput. Sci. 2015, 63, 229–235. [Google Scholar] [CrossRef]
- Kim, H.; Jang, S.J.; Lee, H.D.; Ko, J.H.; Lim, J.Y. Smart Floor Mats for a Health Monitoring System Based on Textile Pressure Sensing:Development and Usability Study. JMIR Publ. 2023, 7, e47325. [Google Scholar]
- Muheidat, F.; Tawalbeh, L. In-Home Floor Based Sensor System-Smart Carpet- to Facilitate Healthy Aging in Place (AIP). IEEE Access 2020, 8, 178627–178638. [Google Scholar] [CrossRef]
- Hong, Y.J.; Kim, I.J.; Ahn, S.C.; Kim, H.G. Mobile health monitoring system based on activity recognition using accelerometer. Simul. Model. Pract. Theory 2010, 18, 446–455. [Google Scholar] [CrossRef]
- Anto Arockia Rosaline, R.; Ponnuviji, N.P.; Subbu Lakshmi, T.C.; Manisha, G. Enhancing lifestyle and health monitoring of elderly populations using CSA-TkELM classifier. Knowl.-Based Syst. 2023, 276, 110758. [Google Scholar] [CrossRef]
- Al-khafajiy, M.; Baker, T.; Chalmers, C.; Asim, M.; Kolivand, H.; Fahim, M.; Waraich, A. Remote health monitoring of elderly through wearable sensors. Multimed. Tools Appl. 2019, 78, 24681–24706. [Google Scholar] [CrossRef]
- Patel, S.; Park, H.; Bonato, P.; Chan, L.; Rodgers, M. A review of wearable sensors and systems with application in rehabilitation. J. Neuro Eng. Rehabil. 2012, 9, 21. [Google Scholar] [CrossRef] [PubMed]
- Kumari, P.; Mathew, L.; Syal, P. Increasing trend of wearables and multimodal interface for human activity monitoring: A review. Biosens. Bioelectron. 2017, 90, 298–307. [Google Scholar] [CrossRef]
- Luna-Perejón, F.; Muñoz-Saavedra, L.; Civit-Masot, J.; Civit, A.; Domínguez-Morales, M. AnkFall—Falls, falling risks and daily-life activities dataset with an ankle-placed accelerometer and training using recurrent neural networks. Sensors 2021, 21, 1889. [Google Scholar] [CrossRef]
- Yang, J.; Lee, J.; Choi, J. Activity recognition based on RFID object usage for smart mobile devices. J. Comput. Sci. Technol. 2011, 26, 239–246. [Google Scholar] [CrossRef]
- Ueno, H. An Analysis for Characteristics of Biosignal Abstracted from Piezoelectric Sensor. In Proceedings of the TENCON 2018-2018 IEEE Region 10 Conference, Jeju, Republic of Korea, 28–31 October 2018; Volume 28–31, pp. 436–440. [Google Scholar]
- Nakagawa, A.; Kim, J.; Nakajima, K. Personal Identifcation Using a Ballistocardiogram during Urination Obtained from a Toilet Seat. Adv. Biomed. Eng. 2020, 9, 233–240. [Google Scholar] [CrossRef]
- Ueno, H. A Piezoelectric Sensor Signal Analysis Method for Identifying Persons Groups. Sensors 2019, 19, 733. [Google Scholar] [CrossRef] [PubMed]
- Bu, N.; Ueno, N.; Fukuda, O. Monitoring of Respiration and Heartbeat during Sleep using a Flexible Piezoelectric Film Sensor and Empirical Mode Decomposition. In Proceedings of the 2007 29th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Lyon, France, 22–26 August 2007; pp. 1362–1366. [Google Scholar]
- Ahmad, M.A. Piezoelectric extraction of ECG signal. Sci. Rep. 2016, 6, 37093. [Google Scholar] [CrossRef] [PubMed]
- Rajala, S.; Lekkala, J. Film-Type Sensor Materials PVDF and EMFi in Measurement of Cardiorespiratory Signals—A Review. IEEE Sens. J. 2012, 12, 439–446. [Google Scholar] [CrossRef]



| Train A, Train B | Inference A | Inference B |
|---|---|---|
| P1, P2 | 67% | 100% |
| P1, P3 | 67% | 100% |
| P1, P4 | 83% | 90% |
| P1, P5 | 25% | 80% |
| P1, P6 | 100% | 100% |
| P1, P7 | 83% | 100% |
| P2, P3 | 100% | 100% |
| P2, P4 | 100% | 40% |
| P2, P5 | 100% | 70% |
| P2, P6 | 100% | 100% |
| P2, P7 | 100% | 100% |
| P3, P4 | 100% | 90% |
| P3, P5 | 100% | 80% |
| P3, P6 | 100% | 100% |
| P3, P7 | 100% | 95% |
| P4, P5 | 55% | 80% |
| P4, P6 | 85% | 100% |
| P4, P7 | 85% | 100% |
| P5, P6 | 100% | 100% |
| P5, P7 | 100% | 100% |
| P6, P7 | 100% | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takahashi, K.; Ueno, H. Ballistocardial Signal-Based Personal Identification Using Deep Learning for the Non-Invasive and Non-Restrictive Monitoring of Vital Signs. Sensors 2024, 24, 2527. https://doi.org/10.3390/s24082527
Takahashi K, Ueno H. Ballistocardial Signal-Based Personal Identification Using Deep Learning for the Non-Invasive and Non-Restrictive Monitoring of Vital Signs. Sensors. 2024; 24(8):2527. https://doi.org/10.3390/s24082527
Chicago/Turabian StyleTakahashi, Karin, and Hitoshi Ueno. 2024. "Ballistocardial Signal-Based Personal Identification Using Deep Learning for the Non-Invasive and Non-Restrictive Monitoring of Vital Signs" Sensors 24, no. 8: 2527. https://doi.org/10.3390/s24082527
APA StyleTakahashi, K., & Ueno, H. (2024). Ballistocardial Signal-Based Personal Identification Using Deep Learning for the Non-Invasive and Non-Restrictive Monitoring of Vital Signs. Sensors, 24(8), 2527. https://doi.org/10.3390/s24082527






