Measurement of Sedentary Behavior—The Outcomes of the Angle for Posture Estimation (APE) Method
Abstract
1. Introduction
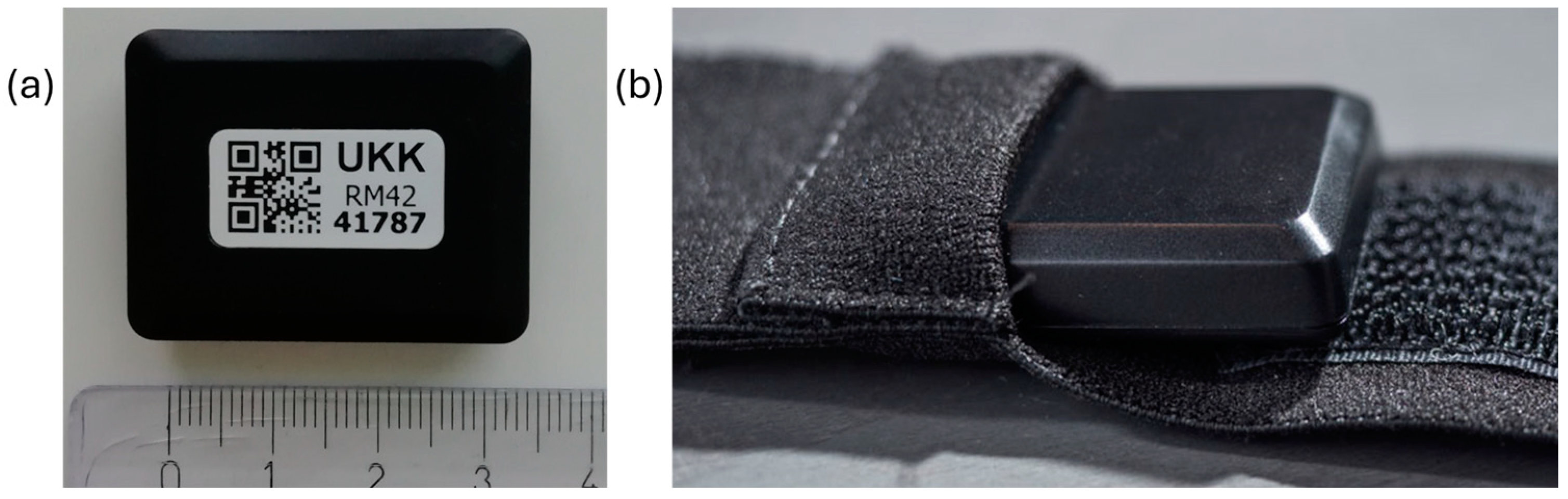
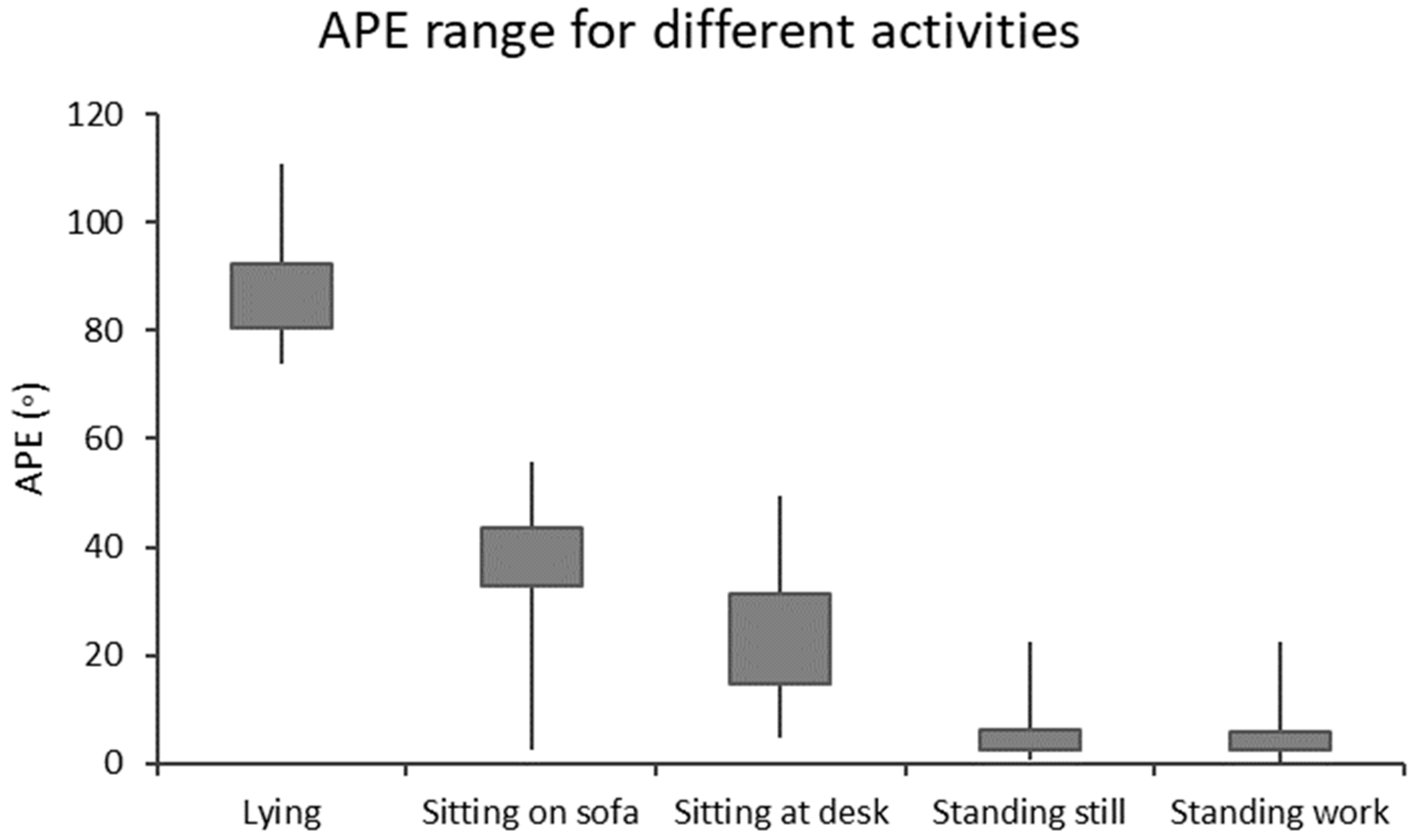
2. Materials and Methods
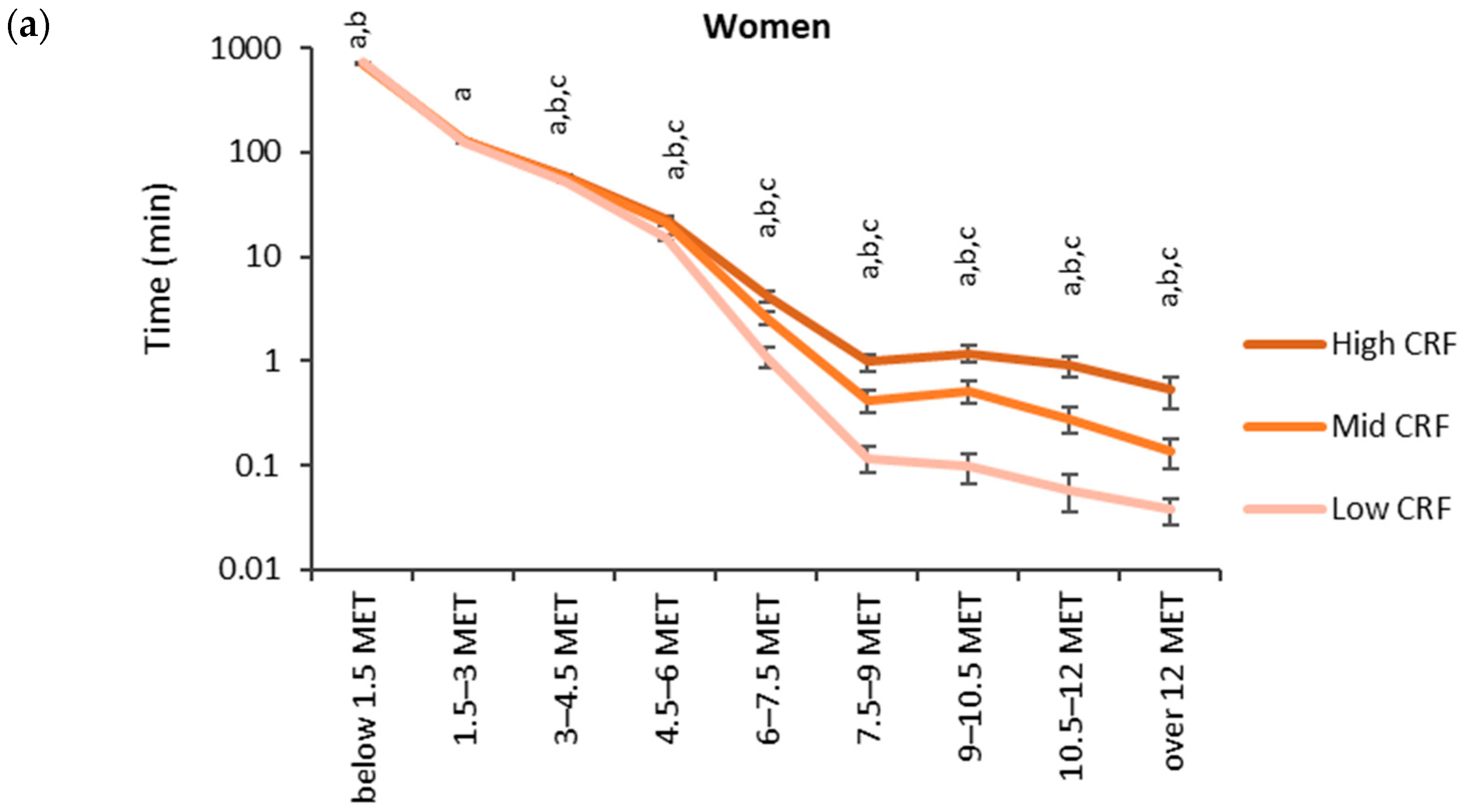
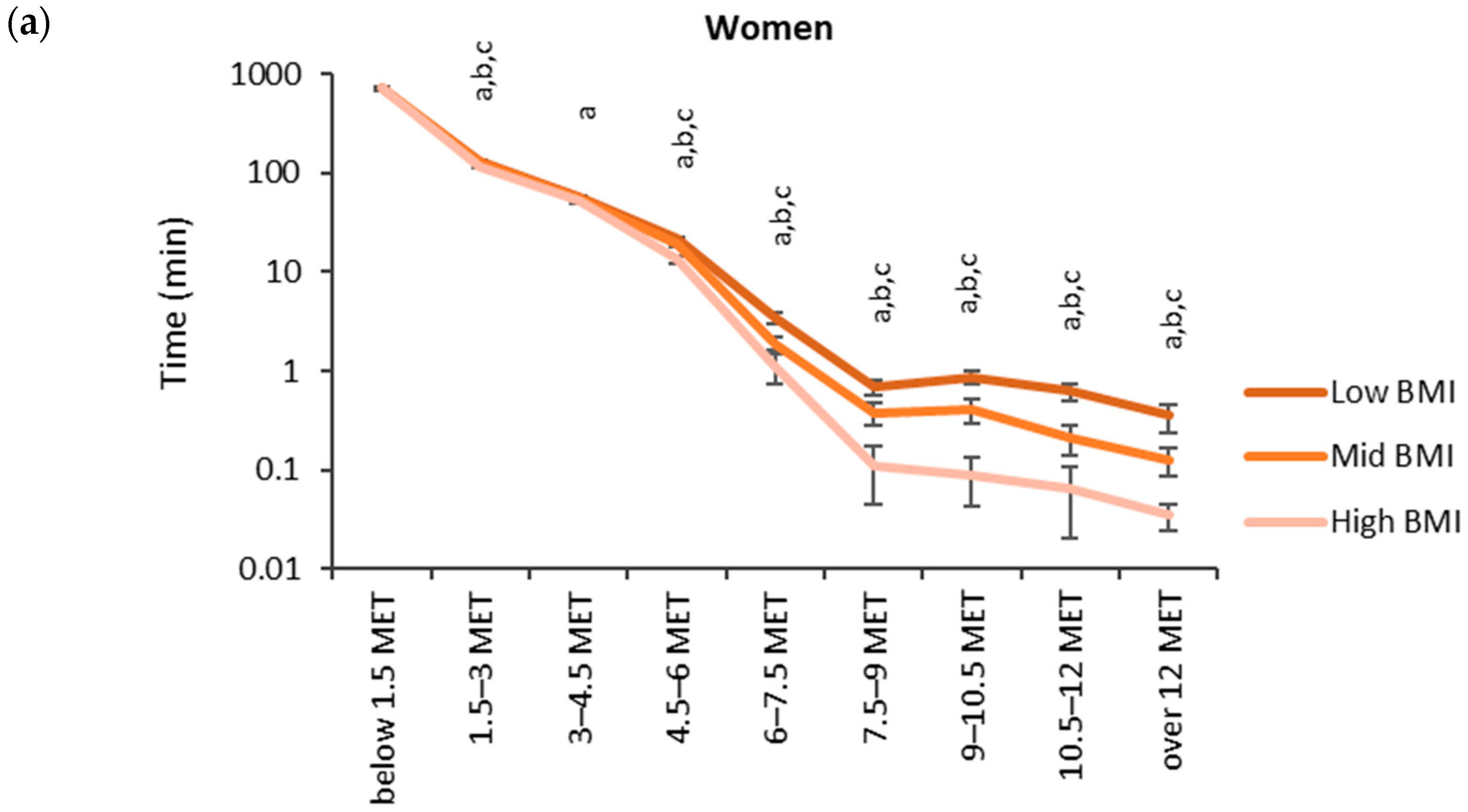
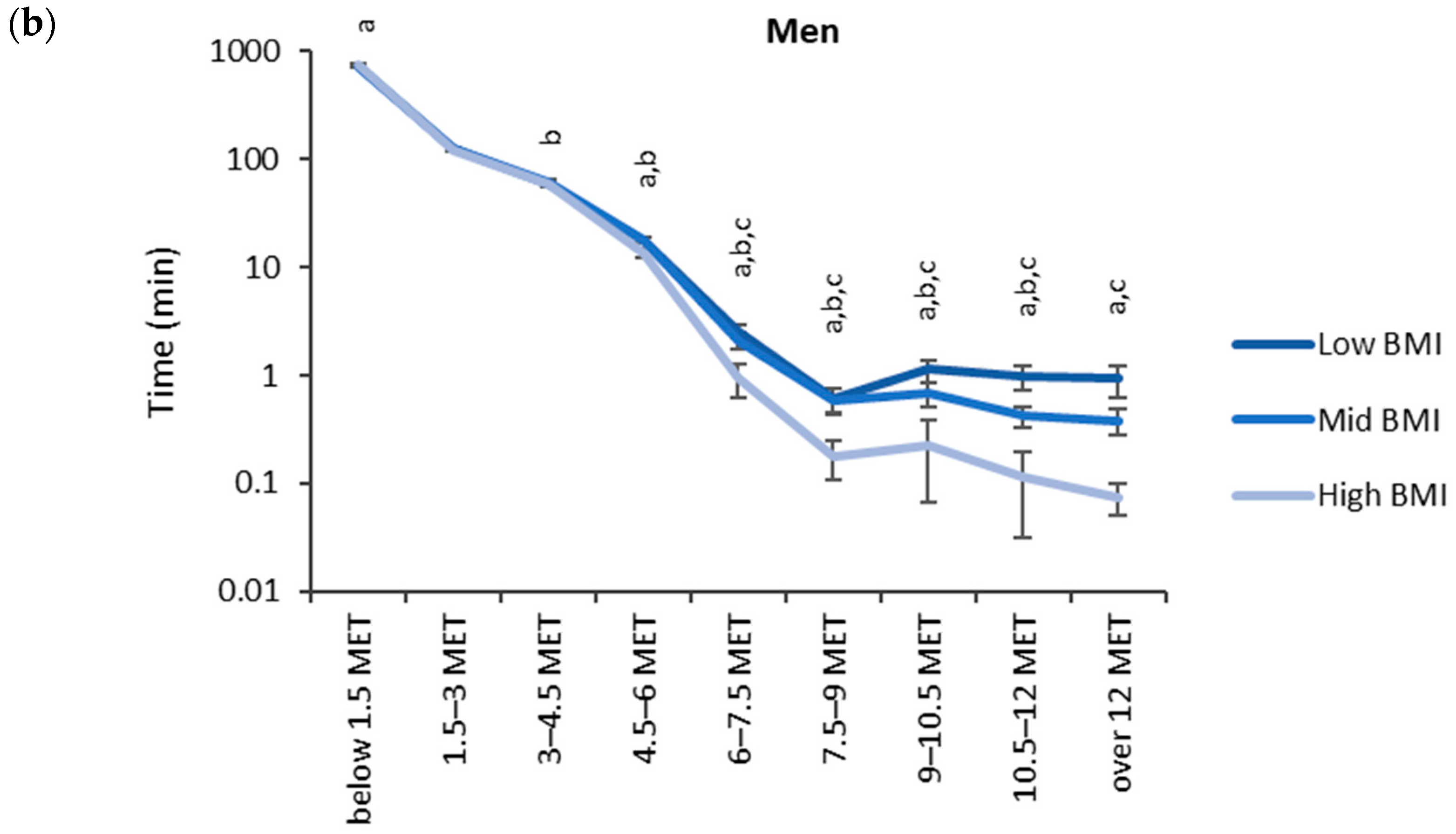
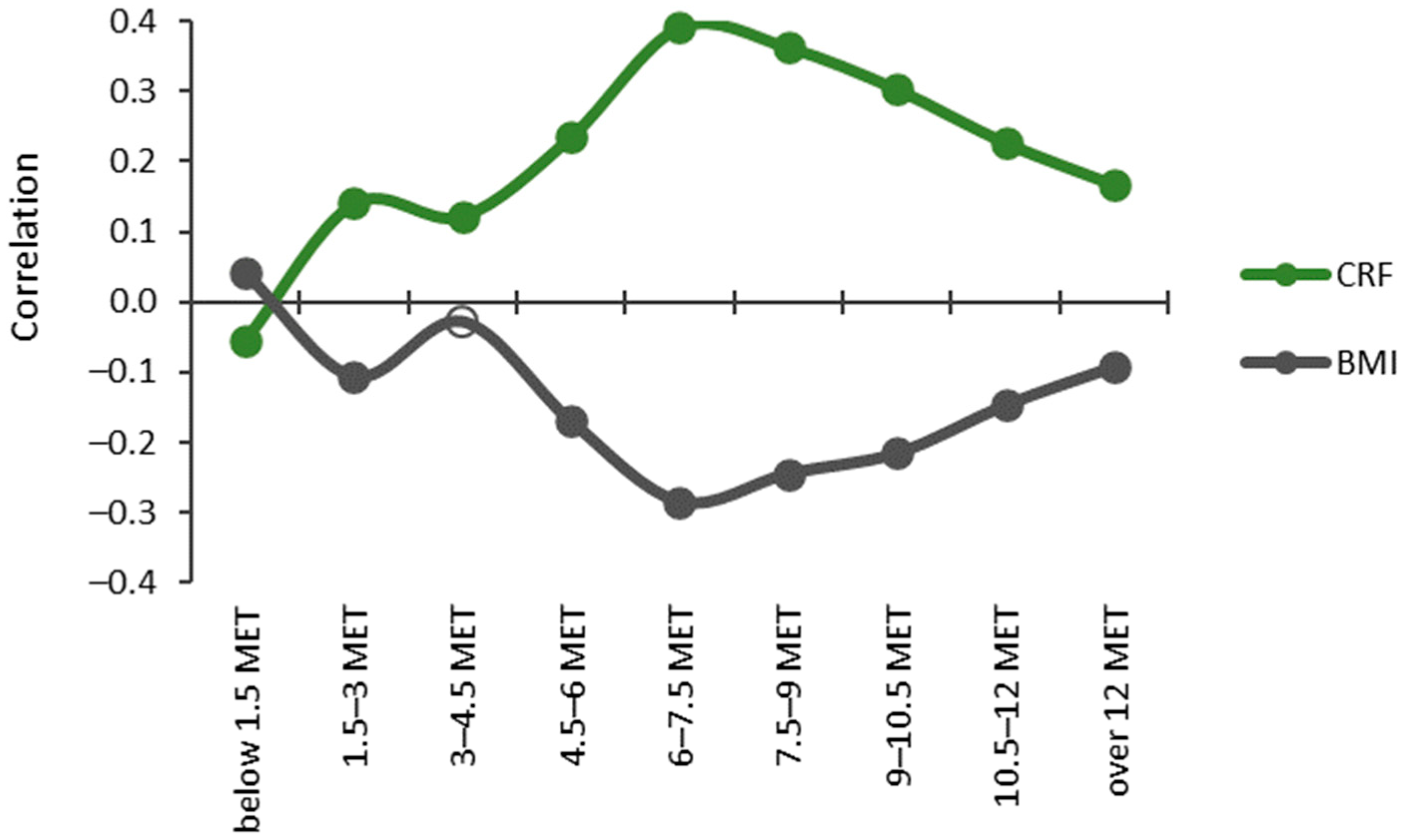
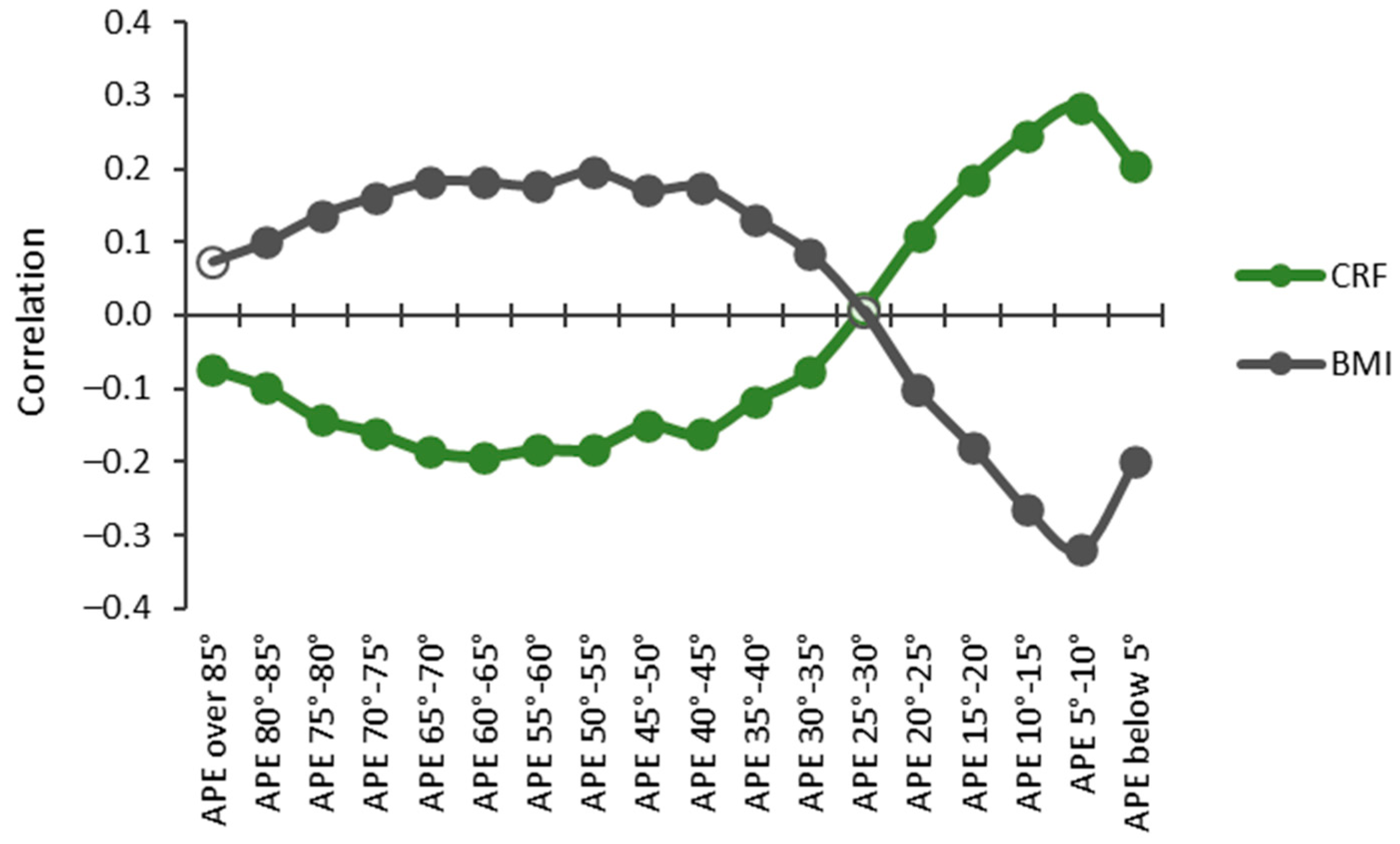
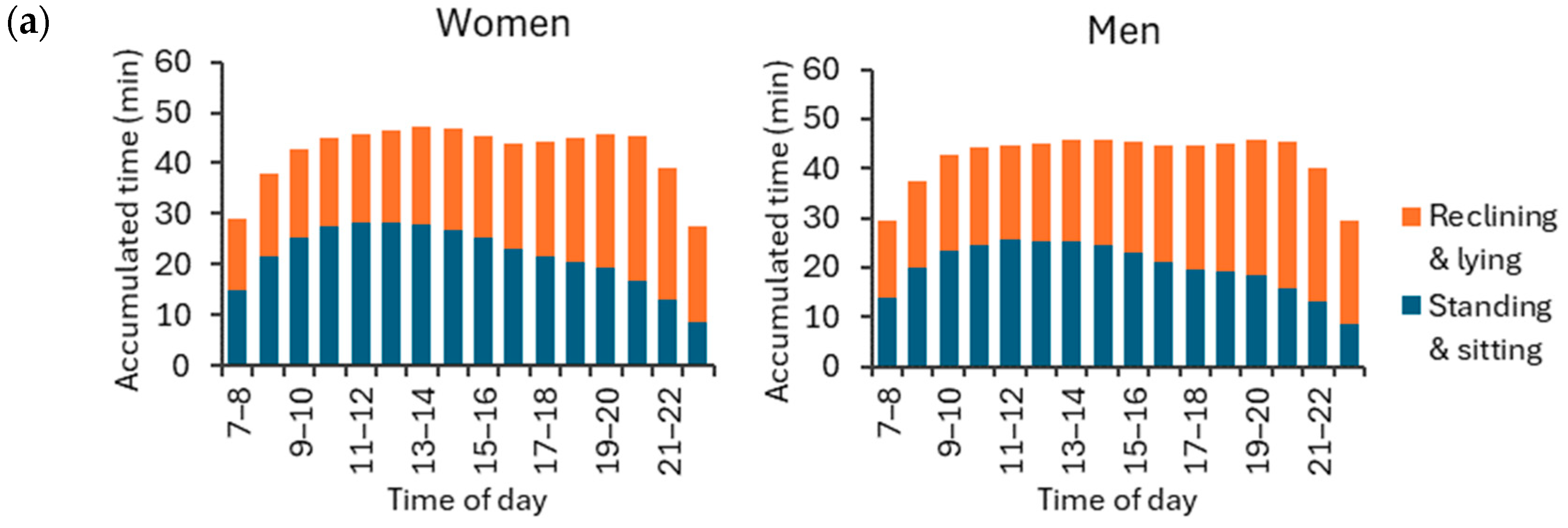
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer–Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Pinto, A.J.; Bergouignan, A.; Dempsey, P.C.; Roschel, H.; Owen, N.; Gualano, B.; Dunstan, D.W. Physiology of sedentary behavior. Physiol. Rev. 2023, 103, 2561–2622. [Google Scholar] [CrossRef]
- Chandrasekaran, B.; Pesola, A.J.; Rao, C.R.; Arumugam, A. Does breaking up prolonged sitting improve cognitive functions in sedentary adults? A mapping review and hypothesis formulation on the potential physiological mechanisms. BMC Musculoskelet. Disord. 2021, 22, 274. [Google Scholar] [CrossRef]
- Silva, F.M.; Duarte-Mendes, P.; Rusenhack, M.C.; Furmann, M.; Nobre, P.R.; Fachada, M.; Soares, C.M.; Teixeira, A.; Ferreira, J.P. Objectively measured sedentary behavior and physical fitness in adults: A systematic review and meta–analysis. Int. J. Environ. Res. Public Health 2020, 17, 8660. [Google Scholar] [CrossRef]
- Vaara, J.P.; Vasankari, T.; Wyss, T.; Pihlainen, K.; Ojanen, T.; Raitanen, J.; Vähä-Ypyä, H.; Kyröläinen, H. Device–based measures of sedentary time and physical activity are associated with physical fitness and body fat content. Front. Sports Act. Living 2020, 2, 587789. [Google Scholar] [CrossRef]
- Ekelund, U.; Brown, W.J.; Steene-Johannessen, J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.E.; Lee, I.-M. Do the associations of sedentary behaviour with cardiovascular disease mortality and cancer mortality differ by physical activity level? A systematic review and harmonised meta–analysis of data from 850,060 participants. Br. J. Sports Med. 2019, 53, 886–894. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Powell, K.E.; Jakicic, J.M.; Troiano, R.P.; Piercy, K.; Tennant, B.; 2018 Physical Activity Guidelines Advisory Committee. Sedentary behavior and health: Update from the 2018 physical activity guidelines advisory committee. Med. Sci. Sports Exerc. 2019, 51, 1227. [Google Scholar] [CrossRef]
- Saunders, T.J.; McIsaac, T.; Douillette, K.; Gaulton, N.; Hunter, S.; Rhodes, R.E.; Prince, S.A.; Carson, V.; Chaput, J.-P.; Chastin, S.; et al. Sedentary behaviour and health in adults: An overview of systematic reviews. Appl. Physiol. Nutr. Metab. 2020, 45, S197–S217. [Google Scholar] [CrossRef]
- Meh, K.; Sember, V.; Sorić, M.; Vähä–Ypyä, H.; Rocha, P.; Jurak, G. The dilemma of physical activity questionnaires: Fitter people are less prone to over reporting. PLoS ONE 2023, 18, e0285357. [Google Scholar] [CrossRef]
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self–reported and device measured sedentary behaviour in adults: A systematic review and meta–analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 31. [Google Scholar] [CrossRef]
- Kongsvold, A.; Flaaten, M.; Logacjov, A.; Skarpsno, E.S.; Bach, K.; Nilsen TI, L.; Mork, P.J. Can the bias of self–reported sitting time be corrected? A statistical model validation study based on data from 23 993 adults in the Norwegian HUNT study. Int. J. Behav. Nutr. Phys. Act. 2023, 20, 139. [Google Scholar] [CrossRef]
- Boerema, S.T.; van Velsen, L.; Vollenbroek, M.M.; Hermens, H.J. Pattern measures of sedentary behaviour in adults: A literature review. Digit. Health 2020, 6, 2055207620905418. [Google Scholar] [CrossRef]
- O’Brien, M.W.; Daley, W.S.; Schwartz, B.D.; Shivgulam, M.E.; Wu, Y.; Kimmerly, D.S.; Frayne, R.J. Characterization of detailed sedentary postures using a tri-monitor activpal configuration in free-living conditions. Sensors 2023, 23, 587. [Google Scholar] [CrossRef]
- Hettiarachchi, P.; Aili, K.; Holtermann, A.; Stamatakis, E.; Svartengren, M.; Palm, P. Validity of a non–proprietary algorithm for identifying lying down using raw data from thigh–worn triaxial accelerometers. Sensors 2021, 21, 904. [Google Scholar] [CrossRef]
- Gibbs, B.B.; Hergenroeder, A.L.; Katzmarzyk, P.T.; Lee, I.M.; Jakicic, J.M. Definition, measurement, and health risks associated with sedentary behavior. Med. Sci. Sports Exerc. 2015, 47, 1295. [Google Scholar] [CrossRef]
- Chastin, S.; McGregor, D.; Palarea–Albaladejo, J.; Diaz, K.M.; Hagströmer, M.; Hallal, P.C.; van Hees, V.T.; Hooker, S.; Howard, V.J.; Lee, I.-M.; et al. Joint association between accelerometry–measured daily combination of time spent in physical activity, sedentary behaviour and sleep and all–cause mortality: A pooled analysis of six prospective cohorts using compositional analysis. Br. J. Sports Med. 2021, 55, 1277–1285. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Rowlands, A.V.; Bunnewell, S.; Sanders, J.; Esliger, D.W.; Gorely, T.; O’connell, S.; Davies, M.J.; Khunti, K.; Yates, T. Accuracy of Posture Allocation Algorithms for Thigh-and Waist-Worn Accelerometers. Med. Sci. Sports Exerc. 2016, 48, 1085–1090. [Google Scholar] [CrossRef]
- Kalisch, T.; Theil, C.; Gosheger, G.; Ackmann, T.; Schoenhals, I.; Moellenbeck, B. Measuring sedentary behavior using waist-and thigh-worn accelerometers and inclinometers—Are the results comparable? Ther. Adv. Musculoskelet. Dis. 2022, 14, 1759720X221079256. [Google Scholar] [CrossRef]
- Júdice, P.B.; Teixeira, L.; Silva, A.M.; Sardinha, L.B. Accuracy of Actigraph inclinometer to classify free-living postures and motion in adults with overweight and obesity. J. Sports Sci. 2019, 37, 1708–1716. [Google Scholar] [CrossRef]
- Vähä-Ypyä, H.; Husu, P.; Suni, J.; Vasankari, T.; Sievänen, H. Reliable recognition of lying, sitting, and standing with a hip-worn accelerometer. Scand. J. Med. Sci. Sports 2018, 28, 1092–1102. [Google Scholar] [CrossRef]
- Greenwood-Hickman, M.A.; Nakandala, S.; Jankowska, M.M.; Rosenberg, D.E.; Tuz-Zahra, F.; Bellettiere, J.; Carlson, J.; Hibbing, P.R.; Zou, J.; Lacroix, A.Z.; et al. The CNN Hip Accelerometer Posture (CHAP) method for classifying sitting patterns from hip accelerometers: A validation study. Med. Sci. Sports Exerc. 2021, 53, 2445. [Google Scholar] [CrossRef]
- Bellettiere, J.; Nakandala, S.; Tuz-Zahra, F.; Winkler, E.A.; Hibbing, P.R.; Healy, G.N.; Dunstan, D.W.; Owen, N.; Greenwood-Hickman, M.A.; Rosenberg, D.E.; et al. CHAP–Adult: A Reliable and Valid Algorithm to Classify Sitting and Measure Sitting Patterns Using Data From Hip–Worn Accelerometers in Adults Aged 35+. J. Meas. Phys. Behav. 2022, 5, 215–223. [Google Scholar] [CrossRef]
- Farrahi, V.; Kangas, M.; Walmsley, R.; Niemelä, M.; Kiviniemi, A.; Puukka, K.; Collings, P.J.; Korpelainen, R.; Jämsä, T. Compositional associations of sleep and activities within the 24-h cycle with cardiometabolic health markers in adults. Med. Sci. Sports Exerc. 2021, 53, 324. [Google Scholar] [CrossRef]
- Hibbing, P.R.; Carlson, J.A.; Steel, C.; Greenwood-Hickman, M.A.; Nakandala, S.; Jankowska, M.M.; Bellettiere, J.; Zou, J.; LaCroix, A.Z.; Kumar, A.; et al. Low movement, deep-learned sitting patterns, and sedentary behavior in the International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE). Int. J. Obes. 2023, 47, 1100–1107. [Google Scholar] [CrossRef]
- Husu, P.; Tokola, K.; Vähä-Ypyä, H.; Sievänen, H.; Suni, J.; Heinonen, O.J.; Heiskanen, J.; Kaikkonen, K.M.; Savonen, K.; Kokko, S.; et al. Physical activity, sedentary behavior, and time in bed among finnish adults measured 24/7 by triaxial accelerometry. J. Meas. Phys. Behav. 2021, 4, 163–173. [Google Scholar] [CrossRef]
- Husu, P.; Vähä-Ypyä, H.; Tokola, K.; Sievänen, H.; Mänttäri, A.; Kokko, S.; Kaikkonen, K.M.; Savonen, K.; Vasankari, T. Measurement of physical fitness and 24/7 physical activity, standing, sedentary behavior, and time in bed in working-age Finns: Study protocol for FINFIT 2021. Methods Protoc. 2022, 5, 7. [Google Scholar] [CrossRef]
- Mänttäri, A.; Suni, J.; Sievänen, H.; Husu, P.; Vähä-Ypyä, H.; Valkeinen, H.; Tokola, K.; Vasankari, T. Six-minute walk test: A tool for predicting maximal aerobic power (VO2 max) in healthy adults. Clin. Physiol. Funct. Imaging 2018, 38, 1038–1045. [Google Scholar] [CrossRef]
- Caramaliu, R.V.; Vasile, A.; Bacis, I. Wearable vital parameters monitoring system. Advanced Topics in Optoelectronics. Microelectron. Nanotechnol. 2015, 9258, 187–192. [Google Scholar] [CrossRef]
- Jaeschke, L.; Luzak, A.; Steinbrecher, A.; Jeran, S.; Ferland, M.; Linkohr, B.; Schulz, H.; Pischon, T. 24 h-accelerometry in epidemiological studies: Automated detection of non-wear time in comparison to diary information. Sci. Rep. 2017, 7, 2227. [Google Scholar] [CrossRef]
- Vähä-Ypyä, H.; Sievänen, H.; Husu, P.; Tokola, K.; Vasankari, T. Intensity paradox—Low-fit people are physically most active in terms of their fitness. Sensors 2021, 21, 2063. [Google Scholar] [CrossRef]
- Vähä-Ypyä, H.; Bretterhofer, J.; Husu, P.; Windhaber, J.; Vasankari, T.; Titze, S.; Sievänen, H. Performance of Different Accelerometry-Based Metrics to Estimate Oxygen Consumption during Track and Treadmill Locomotion over a Wide Intensity Range. Sensors 2023, 23, 5073. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Donaldson, S.C.; Montoye, A.H.; Imboden, M.T.; Kaminsky, L.A. Variability of objectively measured sedentary behavior. Med. Sci. Sports Exerc. 2016, 48, 755. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Ketels, M.; Rasmussen, C.L.; Korshøj, M.; Gupta, N.; De Bacquer, D.; Holtermann, A.; Clays, E. The relation between domain–specific physical behaviour and cardiorespiratory fitness: A cross–sectional compositional data analysis on the physical activity health paradox using accelerometer–assessed data. Int. J. Environ. Res. Public Health 2020, 17, 7929. [Google Scholar] [CrossRef]
- Kitano, N.; Kai, Y.; Jindo, T.; Fujii, Y.; Tsunoda, K.; Arao, T. Association of domain-specific physical activity and sedentary behavior with cardiometabolic health among office workers. Scand. J. Med. Sci. Sports 2022, 32, 1224–1235. [Google Scholar] [CrossRef]
- Aunger, J.; Wagnild, J. Objective and subjective measurement of sedentary behavior in human adults: A toolkit. Am. J. Hum. Biol. 2022, 34, e23546. [Google Scholar] [CrossRef]
- Raichlen, D.A.; Pontzer, H.; Zderic, T.W.; Harris, J.A.; Mabulla, A.Z.; Hamilton, M.T.; Wood, B.M. Sitting, squatting, and the evolutionary biology of human inactivity. Proc. Natl. Acad. Sci. USA 2020, 117, 7115–7121. [Google Scholar] [CrossRef]
- Norha, J.; Sjöros, T.; Garthwaite, T.; Laine, S.; Saarenhovi, M.; Kallio, P.; Laitinen, K.; Houttu, N.; Vähä-Ypyä, H.; Sievänen, H.; et al. Effects of reducing sedentary behavior on cardiorespiratory fitness in adults with metabolic syndrome: A 6-month RCT. Scand. J. Med. Sci. Sports 2023, 33, 1452–1461. [Google Scholar] [CrossRef]
- Nikolaidis, P.T.; Knechtle, B. Sedentarism in Recreational Marathon Runners. Open Access J. Sports Med. 2023, 14, 103–109. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Thyfault, J.P. Physiological Responses to Sedentary Behaviour. In Sedentary Behaviour Epidemiology; Leitzmann, M.F., Jochem, C., Schmid, D., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 109–153. [Google Scholar]
- Sjöros, T.; Laine, S.; Garthwaite, T.; Vähä-Ypyä, H.; Löyttyniemi, E.; Koivumäki, M.; Houttu, N.; Laitinen, K.; Kalliokoski, K.K.; Sievänen, H.; et al. Reducing sedentary time and whole-body insulin sensitivity in metabolic syndrome: A 6-month randomized controlled trial. Med. Sci. Sports Exerc. 2023, 55, 342. [Google Scholar] [CrossRef]
- Garthwaite, T.; Sjöros, T.; Laine, S.; Vähä-Ypyä, H.; Löyttyniemi, E.; Sievänen, H.; Houttu, N.; Laitinen, K.; Kalliokoski, K.; Vasankari, T.; et al. Effects of reduced sedentary time on cardiometabolic health in adults with metabolic syndrome: A three–month randomized controlled trial. J. Sci. Med. Sport 2022, 25, 579–585. [Google Scholar] [CrossRef]
- O’Brien, M.W.; Wu, Y.; Petterson, J.L.; Frayne, R.J.; Kimmerly, D.S. Ecological validity of prolonged sitting studies: How well do they represent real–life sedentary patterns? A pilot study. Transl. J. Am. Coll. Sports Med. 2022, 7, e000182. [Google Scholar] [CrossRef]
- Vasankari, V.; Husu, P.; Vähä-Ypyä, H.; Suni, J.H.; Tokola, K.; Borodulin, K.; Wennman, H.; Halonen, J.; Hartikainen, J.; Sievänen, H.; et al. Subjects with cardiovascular disease or high disease risk are more sedentary and less active than their healthy peers. BMJ Open Sport—Exerc. Med. 2018, 4, e000363. [Google Scholar] [CrossRef]
- Husu, P.; Suni, J.; Tokola, K.; Vähä-Ypyä, H.; Valkeinen, H.; Mäki-Opas, T.; Sievänen, H.; Vasankari, T. Frequent sit–to–stand transitions and several short standing periods measured by hip–worn accelerometer are associated with smaller waist circumference among adults. J. Sports Sci. 2019, 37, 1840–1848. [Google Scholar] [CrossRef]
- Sagelv, E.H.; Hopstock, L.A.; Morseth, B.; Hansen, B.H.; Steene-Johannessen, J.; Johansson, J.; Nordström, A.; Saint-Maurice, P.F.; Løvsletten, O.; Wilsgaard, T.; et al. Device-measured physical activity, sedentary time, and risk of all-cause mortality: An individual participant data analysis of four prospective cohort studies. Br. J. Sports Med. 2023, 57, 1457–1463. [Google Scholar] [CrossRef]
- Giurgiu, M.; Bussmann, J.B.; Hill, H.; Anedda, B.; Kronenwett, M.; Koch, E.D.; Ebner-Priemer, U.W.; Reichert, M. Validating accelerometers for the assessment of body position and sedentary behavior. J. Meas. Phys. Behav. 2020, 3, 253–263. [Google Scholar] [CrossRef]
- Blodgett, J.M.; Ahmadi, M.N.; Atkin, A.J.; Chastin, S.; Chan, H.W.; Suorsa, K.; Bakker, E.A.; Hettiarcachchi, P.; Johansson, P.J.; Sherar, L.B.; et al. Device-measured physical activity and cardiometabolic health: The Prospective Physical Activity, Sitting, and Sleep (ProPASS) consortium. Eur. Heart J. 2024, 45, 458–471. [Google Scholar] [CrossRef]
- Straczkiewicz, M.; Huang, E.J.; Onnela, J.P. A “one-size-fits-most” walking recognition method for smartphones, smartwatches, and wearable accelerometers. npj Digit. Med. 2023, 6, 29. [Google Scholar] [CrossRef]
- Neugebauer, J.M.; Collins, K.H.; Hawkins, D.A. Ground reaction force estimates from ActiGraph GT3X+ hip accelerations. PLoS ONE 2014, 9, e99023. [Google Scholar] [CrossRef]
- Ancillao, A.; Tedesco, S.; Barton, J.; O’Flynn, B. Indirect measurement of ground reaction forces and moments by means of wearable inertial sensors: A systematic review. Sensors 2018, 18, 2564. [Google Scholar] [CrossRef]




| Age Group (Years) | CRF Third | Women | Men | BMI Category | Women | Men |
|---|---|---|---|---|---|---|
| 20–29 | high | 114 | 56 | low | 133 | 41 |
| mid | 58 | 14 | mid | 46 | 32 | |
| low | 14 | 10 | high | 7 | 7 | |
| 30–39 | high | 154 | 92 | low | 196 | 84 |
| mid | 103 | 90 | mid | 88 | 83 | |
| low | 67 | 19 | high | 40 | 34 | |
| 40–49 | high | 165 | 99 | low | 238 | 100 |
| mid | 149 | 108 | mid | 125 | 134 | |
| low | 131 | 76 | high | 82 | 49 | |
| 50–59 | high | 66 | 44 | low | 202 | 93 |
| mid | 197 | 143 | mid | 200 | 185 | |
| low | 243 | 163 | high | 104 | 72 | |
| 60–70 | high | 48 | 14 | low | 267 | 150 |
| mid | 194 | 125 | mid | 227 | 243 | |
| low | 375 | 344 | high | 123 | 90 |
| Group | Age (Years) | VO2max (mL/kg/min) | BMI (kg/m2) | ||
|---|---|---|---|---|---|
| CRF thirds | women | high | 36.1 (11.5, 20–69) | 39.5 (2.4, 36.3–48.6) | 22.0 (2.2, 16.5–32.5) |
| mid | 45.2 (13.7, 20–69) | 33.8 (1.4, 31.2–36.3) | 24.6 (2.6, 17.3–39.6) | ||
| low | 53.0 (11.9, 20–70) | 26.3 (3.7, 9.9–31.2) | 29.7 (4.4, 19.2–47.3) | ||
| men | high | 34.7 (10.4, 20–69) | 44.0 (2.8, 40.4–53.4) | 24.4 (2.8, 16.7–33.3) | |
| mid | 45.6 (12.1, 20–69) | 37.4 (1.6, 34.4–40.4) | 26.4 (3.1, 14.9–35.8) | ||
| low | 54.4 (12.7, 20–70) | 29.6 (4.0, 12.5–34.4) | 29.0 (4.5, 19.0–48.7) | ||
| BMI categories | women | low | 41.8 (14.3, 20–69) | 36.8 (4.0, 19.4–48.6) | 22.2 (1.8, 16.5–25.0) |
| mid | 47.2 (14.1, 20–70) | 31.1 (3.9, 18.2–41.8) | 27.1 (1.4, 25.0–30.0) | ||
| high | 50.2 (11.6, 26–70) | 24.5 (4.4, 9.9–40.2) | 33.7 (3.2, 30.0–47.3) | ||
| men | low | 41.7 (14.5, 20–70) | 40.6 (5.4, 22.9–53.4) | 23.0 (1.6, 14.9–25.0) | |
| mid | 46.4 (13.9, 20–70) | 36.3 (5.6, 16.2–51.1) | 27.2 (1.4, 25.0–30.0) | ||
| high | 47.9 (13.4, 22–69) | 30.9 (6.5, 12.5–46.9) | 33.2 (3.4, 30.0–48.7) | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vähä-Ypyä, H.; Husu, P.; Sievänen, H.; Vasankari, T. Measurement of Sedentary Behavior—The Outcomes of the Angle for Posture Estimation (APE) Method. Sensors 2024, 24, 2241. https://doi.org/10.3390/s24072241
Vähä-Ypyä H, Husu P, Sievänen H, Vasankari T. Measurement of Sedentary Behavior—The Outcomes of the Angle for Posture Estimation (APE) Method. Sensors. 2024; 24(7):2241. https://doi.org/10.3390/s24072241
Chicago/Turabian StyleVähä-Ypyä, Henri, Pauliina Husu, Harri Sievänen, and Tommi Vasankari. 2024. "Measurement of Sedentary Behavior—The Outcomes of the Angle for Posture Estimation (APE) Method" Sensors 24, no. 7: 2241. https://doi.org/10.3390/s24072241
APA StyleVähä-Ypyä, H., Husu, P., Sievänen, H., & Vasankari, T. (2024). Measurement of Sedentary Behavior—The Outcomes of the Angle for Posture Estimation (APE) Method. Sensors, 24(7), 2241. https://doi.org/10.3390/s24072241







