Developing and Validating an Intelligent Mouth-Opening Training Device: A New Solution for Restricted Mouth Opening
Abstract
1. Introduction
2. Design of IMOTD
2.1. Design Concept
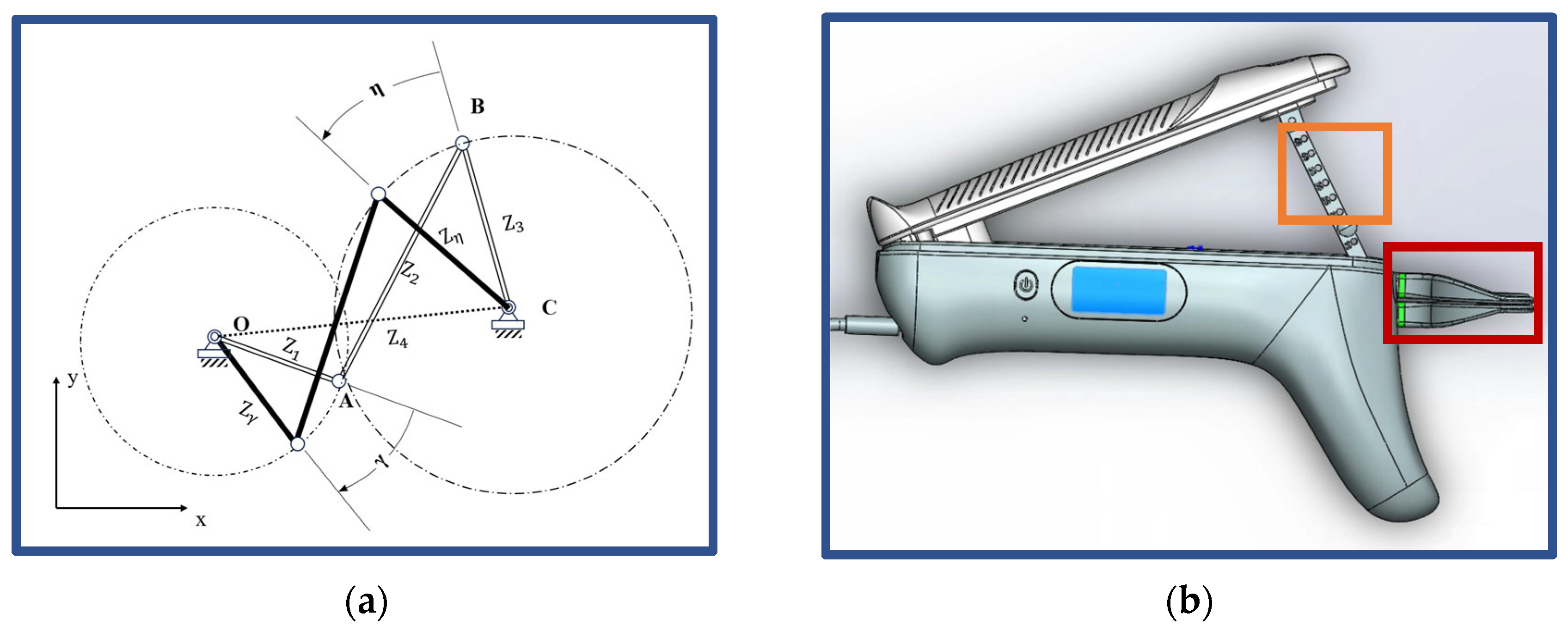
2.2. Mechanical Perspective
2.3. Intelligent Monitoring
3. Validation Methods
3.1. Piezoelectric Sensor Calibration
3.2. Finite Element Analysis
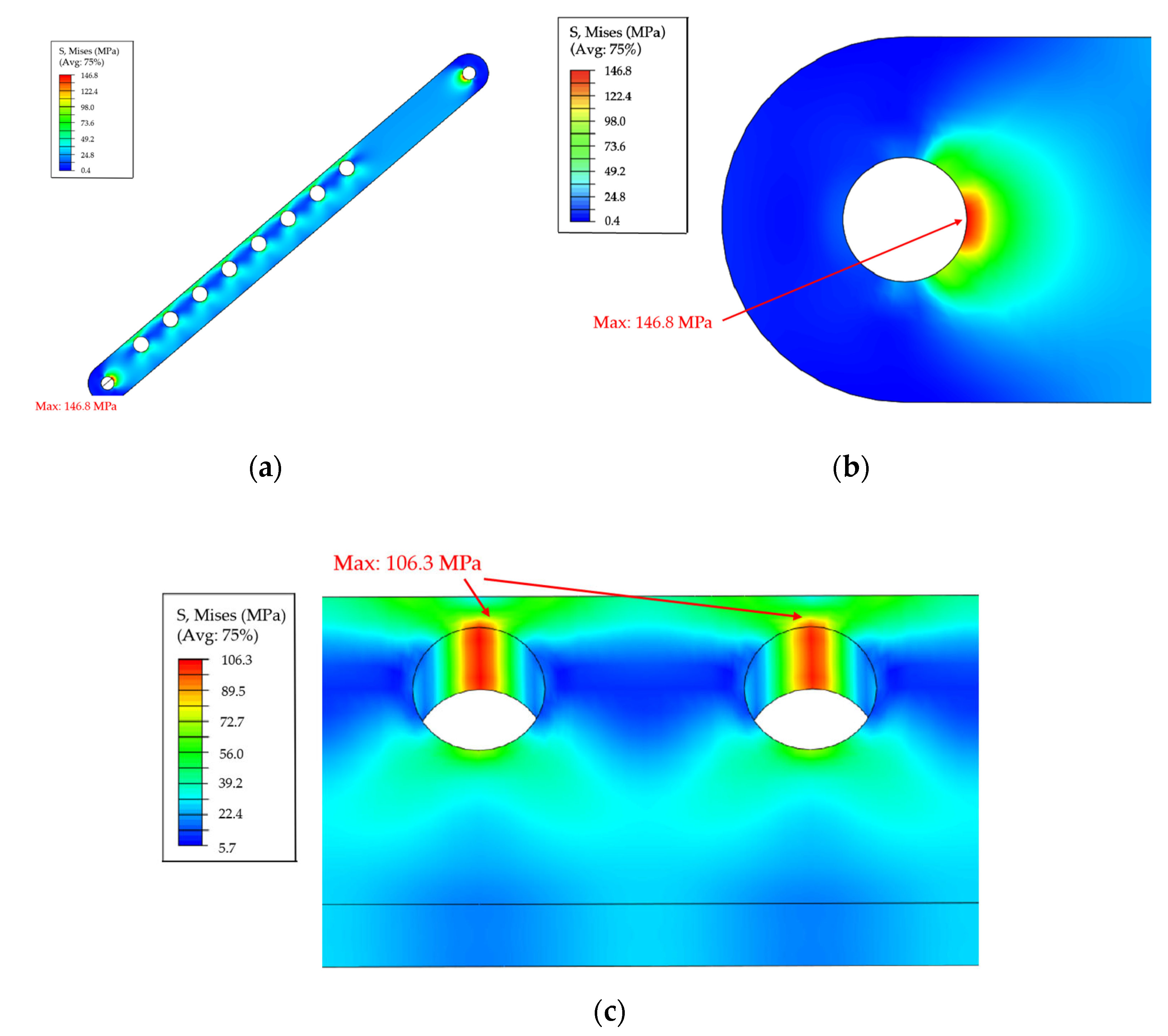
3.2.1. In Silico Safety Inspection
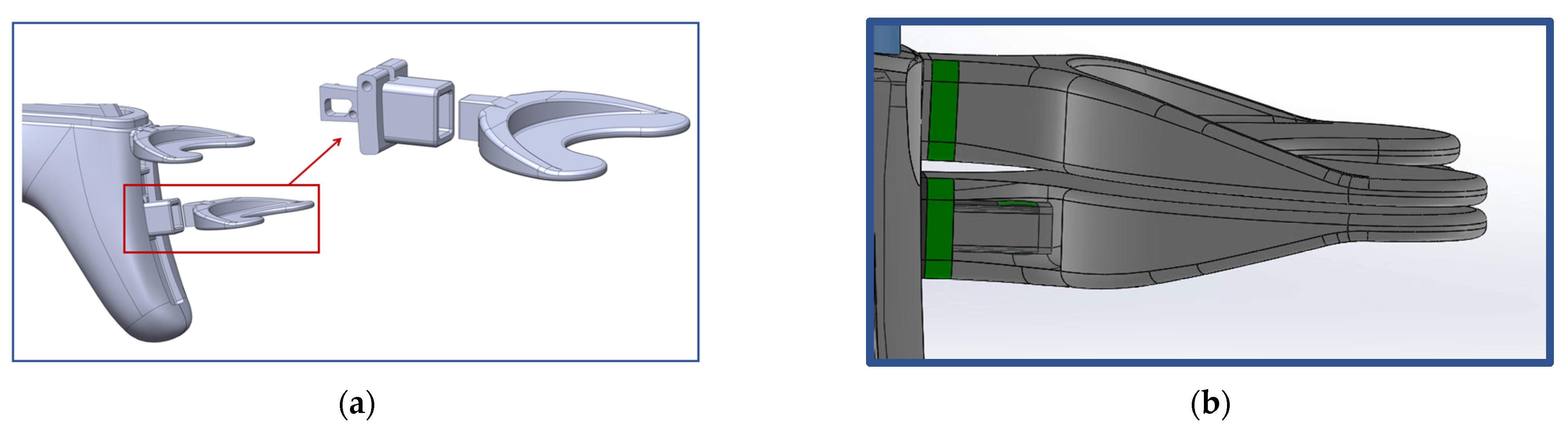
3.2.2. Occlusion Plate Insertion Method
3.3. Pilot Study
3.3.1. Patient Preparation
3.3.2. Exercise Protocol
3.3.3. Follow-Up Time
4. Validation Results
4.1. Piezoelectric Sensor Calibration
4.2. Finite Element Analysis
4.2.1. In Silico Safety Inspection
4.2.2. Optimization of Insertion Force
4.3. Pilot Study
4.3.1. The Results of IMOTD Use
4.3.2. Comparison with the Traditional Open-Mouth Training Method
5. Discussion
5.1. Comparison with Other Mouth-Opening Devices
5.1.1. Safety and Convenience
5.1.2. Improvement in Compliance
5.1.3. Quantitative Indicators
5.1.4. Hygiene
5.2. Future Work
6. Conclusions
7. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TMJ | Temporomandibular Joint |
| RMO | Restricted Mouth Opening |
| IMOTD | Intelligent Mouth-Opening Training Device |
| ABS | Acrylonitrile Butadiene Styrene |
| PC | Polycarbonate |
| MIO | Maximum Interincisal Opening |
References
- Lee, R.; Slevin, N.; Musgrove, B.; Swindell, R.; Molassiotis, A. Prediction of post-treatment trismus in head and neck cancer patients. Br. J. Oral Maxillofac. Surg. 2012, 50, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Bhrany, A.D.; Izzard, M.; Wood, A.J.; Futran, N.D. Coronoidectomy for the Treatment of Trismus in Head and Neck Cancer Patients. Laryngoscope 2009, 117, 1952–1956. [Google Scholar] [CrossRef] [PubMed]
- Mardini, S.; Chang, Y.-M.; Tsai, C.-Y.; Coskunfirat, O.K.; Wei, F.-C. Release and Free Flap Reconstruction for Trismus that Develops after Previous Intraoral Reconstruction. Plast. Reconstr. Surg. 2006, 118, 102–107. [Google Scholar] [CrossRef] [PubMed]
- Huang, I.Y.; Wu, C.F.; Shen, Y.S.; Yang, C.F.; Shieh, T.Y.; Hsu, H.J.; Chen, C.H.; Chen, C.M. Importance of patient’s cooperation in surgical treatment for oral submucous fibrosis. J. Oral Maxillofac. Surg. 2008, 66, 699–703. [Google Scholar] [CrossRef] [PubMed]
- Mehrotra, D.; Pradhan, R.; Gupta, S. Retrospective comparison of surgical treatment modalities in 100 patients with oral submucous fibrosis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 107, e1–e10. [Google Scholar] [CrossRef] [PubMed]
- Bensadoun, R.-J.; Riesenbeck, D.; Lockhart, P.B.; Elting, L.S.; Spijkervet, F.K.L.; Brennan, M.T. A systematic review of trismus induced by cancer therapies in head and neck cancer patients. Support. Care Cancer 2010, 18, 1033. [Google Scholar] [CrossRef]
- Scherpenhuizen, A.; van Waes, A.M.A.; Janssen, L.M.; Van Cann, E.M.; Stegeman, I. The effect of exercise therapy in head and neck cancer patients in the treatment of radiotherapy-induced trismus: A systematic review. Oral Oncol. 2015, 51, 745. [Google Scholar] [CrossRef]
- Tveterås, K.; Kristensen, S. The aetiology and pathogenesis of trismus. Clin. Otolaryngol. Allied Sci. 1986, 11, 383–387. [Google Scholar] [CrossRef]
- Eipe, N. The chewing of betel quid and oral submucous fibrosis and anesthesia. Anesth Analg. 2005, 100, 1210–1213. [Google Scholar] [CrossRef]
- Johnson, N.W.; Warnakulasuriya, S.; Gupta, P.C.; Dimba, E.; Chindia, M.; Otoh, E.C.; Sankaranarayanan, R.; Califano, J.; Kowalski, L. Global oral health inequalities in incidence and outcomes for oral cancer: Causes and solutions. Adv. Dent. Res. 2011, 23, 237–246. [Google Scholar] [CrossRef]
- Bengtson, B.P.; Schusterman, M.A.; Baldwin, B.J.; Miller, M.J.; Reece, G.P.; Kroll, S.S.; Robb, G.L.; Goepfert, H. Influence of prior radiotherapy on the development of postoperative complications and success of free tissue transfers in head and neck cancer reconstruction. Am. J. Surg. 1993, 166, 326–330. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, P.U.; Kalk, W.W.I.; Roodenburg, J.L.N. Trismus in head and neck oncology: A systematic review. Oral Oncol. 2004, 40, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Weber, C.; Dommerich, S.; Pau, H.W.; Kramp, B. Limited mouth opening after primary therapy of head and neck cancer. Oral Maxillofac. Surg. 2010, 14, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Louise Kent, M.; Brennan, M.T.; Noll, J.L.; Fox, P.C.; Burri, S.H.; Hunter, J.C.; Lockhart, P.B. Radiation-induced trismus in head and neck cancer patients. Support. Care Cancer. 2008, 16, 305–309. [Google Scholar] [CrossRef]
- Johnson, J.; van As-Brooks, C.J.; Fagerberg-Mohlin, B.; Finizia, C. Trismus in head and neck cancer patients in Sweden: Incidence and risk factors. Med. Sci. Monit. 2010, 16, 278–282. [Google Scholar]
- Watters, A.L.; Cope, S.; Keller, M.N.; Padilla, M.; Enciso, R. Prevalence of trismus in patients with head and neck cancer: A systematic review with meta-analysis. Head Neck 2019, 41, 3408–3421. [Google Scholar] [CrossRef]
- Wu, H.; Zhou, Z.; Zhang, C.; Shen, S.; Liu, J.; Zhang, C. The progress of post-treatment restricted mouth opening in oral and maxillofacial malignant tumor patients. Front. Oral Maxillofac. Med. 2021, 3, 7. [Google Scholar] [CrossRef]
- Epstein, J.B.; Thariat, J.; Bensadoun, R.J.; Barasch, A.; Murphy, B.A.; Kolnick, L.; Popplewell, L.; Maghami, E. Oral complications of cancer and cancer therapy. CA Cancer J. Clin. 2012, 62, 400–422. [Google Scholar] [CrossRef]
- Li, Y.H.; Liu, C.C.; Chiang, T.E.; Chen, Y.W. EZBite open-mouth device: A new treatment option for oral submucous fibrosis-related trismus. J. Dent. Sci. 2018, 13, 80–81. [Google Scholar] [CrossRef] [PubMed]
- Pauli, N.; Johnson, J.; Finizia, C.; Andréll, P. The incidence of trismus and long-term impact on health-related quality of life in patients with head and neck cancer. Acta Oncol. 2012, 52, 1137–1145. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, P.U.; Huisman, P.M.; Roodenburg, J.L.N. Criteria for trismus in head and neck oncology. Int. J. Oral Maxillofac. Surg. 2006, 35, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Stubblefield, M.D.; Manfield, L.; Riedel, E.R. A preliminary report on the efficacy of a dynamic jaw opening device (dynasplint trismus system) as part of the multimodal treatment of trismus in patients with head and neck cancer. Arch. Phys. Med. Rehabil. 2010, 91, 1278–1282. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.-H.; Chang, W.-C.; Chiang, T.-E.; Lin, C.-S.; Chen, Y.-W. Mouth-opening device as a treatment modality in trismus patients with head and neck cancer and oral submucous fibrosis: A prospective study. Clin. Oral Investig. 2018, 23, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Van der Geer, S.J.; van Rijn, P.V.; Kamstra, J.I.; Roodenburg, J.L.N.; Dijkstra, P.U. Criterion for trismus in head and neck cancer patients: A verification study. Support. Care Cancer 2018, 27, 1129–1137. [Google Scholar] [CrossRef]
- Lee, Y.-C.; Wong, T.-Y.; Shieh, S.-J.; Lee, J.-W. Trismus Release in Oral Cancer Patients. Ann. Plast. Surg. 2012, 69, 598–601. [Google Scholar] [CrossRef]
- LENT SOMA tables. Radiother Oncol. 1995, 35, 17–60. [CrossRef]
- Grandi, G.; Silva, M.L.; Streit, C.; Wagner, J.C.B. A mobilization regimen to prevent mandibular hypomobility in irradiated patients: An analysis and comparison of two techniques. Med. Oral Patol. Oral Cir. Bucal 2007, 12, E105–E109. [Google Scholar] [PubMed]







| Patient No. | Gender | Age | Tumor Location | Treatment Regimens | Pre-Operative MIO * (mm) | Post-Operative MIO * (Mm) at 2 Weeks | Post-Operative MIO * (mm) at 3 Weeks | Post-Operative MIO * (mm) at 4 Weeks |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 38 | Left buccal | S + R | 40 | 20 | 20 | 30 |
| 2 | M | 70 | Left buccal | S + R | 35 | 15 | 15 | 25 |
| 3 | F | 68 | Right buccal | S + R | 42 | 35 | 35 | 35 |
| 4 | M | 71 | Left buccal | S + R | 27 | 20 | 20 | 20 |
| 5 | M | 68 | Right buccal | S + R | 35 | 25 | 25 | 25 |
| No. | Occlusal Plate (Outer Dimension) | Slider (Inner Dimension) | Insertion Force (N) | |||||
|---|---|---|---|---|---|---|---|---|
| Width (mm) | Height (mm) | Depth (mm) | Taper (degree) | Width (mm) | Height (mm) | Depth (mm) | ||
Type I The occlusal plate tapered from the base to the end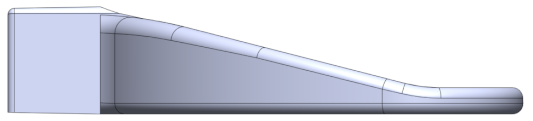 | ||||||||
| 1 | 5.8 | 8.2 | 7 | 1 | 5.7 | 8.1 | 8 | 1007.7 |
| 2 | 5.8 | 8.2 | 7 | 1 | 5.75 | 8.15 | 8 | 294.24 |
| 3 | 5.8 | 8.2 | 7 | 1 | 5.72 | 8.12 | 8 | 616.98 |
| 4 | 5.8 | 8.2 | 7 | 1 | 5.73 | 8.13 | 8 | 458.96 |
| 5 | 5.8 | 8.2 | 7 | 1 | 5.74 | 8.14 | 8 | 325.02 |
Type II straight cross-section followed by tapered to the end | ||||||||
| 6 | 5.8 | 8.2 | 3 (7) | 1 | 5.74 | 8.14 | 8 | 1204.2 |
| 7 | 5.8 | 8.2 | 3 (7) | 1 | 5.78 | 8.18 | 8 | 320.92 |
Type III straight cross-section 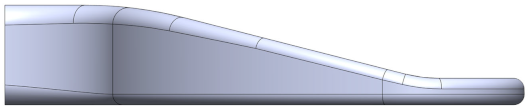  | ||||||||
| 8 | 5.5 | 3.5 | 7 | 0 | 5.5 | 3.5 | 8 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, H.; Wang, Z.; Han, J.; Wu, T.; Zhai, G.; Zhang, C.; Liu, J. Developing and Validating an Intelligent Mouth-Opening Training Device: A New Solution for Restricted Mouth Opening. Sensors 2024, 24, 1988. https://doi.org/10.3390/s24061988
Wu H, Wang Z, Han J, Wu T, Zhai G, Zhang C, Liu J. Developing and Validating an Intelligent Mouth-Opening Training Device: A New Solution for Restricted Mouth Opening. Sensors. 2024; 24(6):1988. https://doi.org/10.3390/s24061988
Chicago/Turabian StyleWu, Hao, Zilin Wang, Jing Han, Tianchi Wu, Guangtao Zhai, Chenping Zhang, and Jiannan Liu. 2024. "Developing and Validating an Intelligent Mouth-Opening Training Device: A New Solution for Restricted Mouth Opening" Sensors 24, no. 6: 1988. https://doi.org/10.3390/s24061988
APA StyleWu, H., Wang, Z., Han, J., Wu, T., Zhai, G., Zhang, C., & Liu, J. (2024). Developing and Validating an Intelligent Mouth-Opening Training Device: A New Solution for Restricted Mouth Opening. Sensors, 24(6), 1988. https://doi.org/10.3390/s24061988






