A New Wrist-Worn Tool Supporting the Diagnosis of Parkinsonian Motor Syndromes
Abstract
1. Introduction
2. Materials and Methods
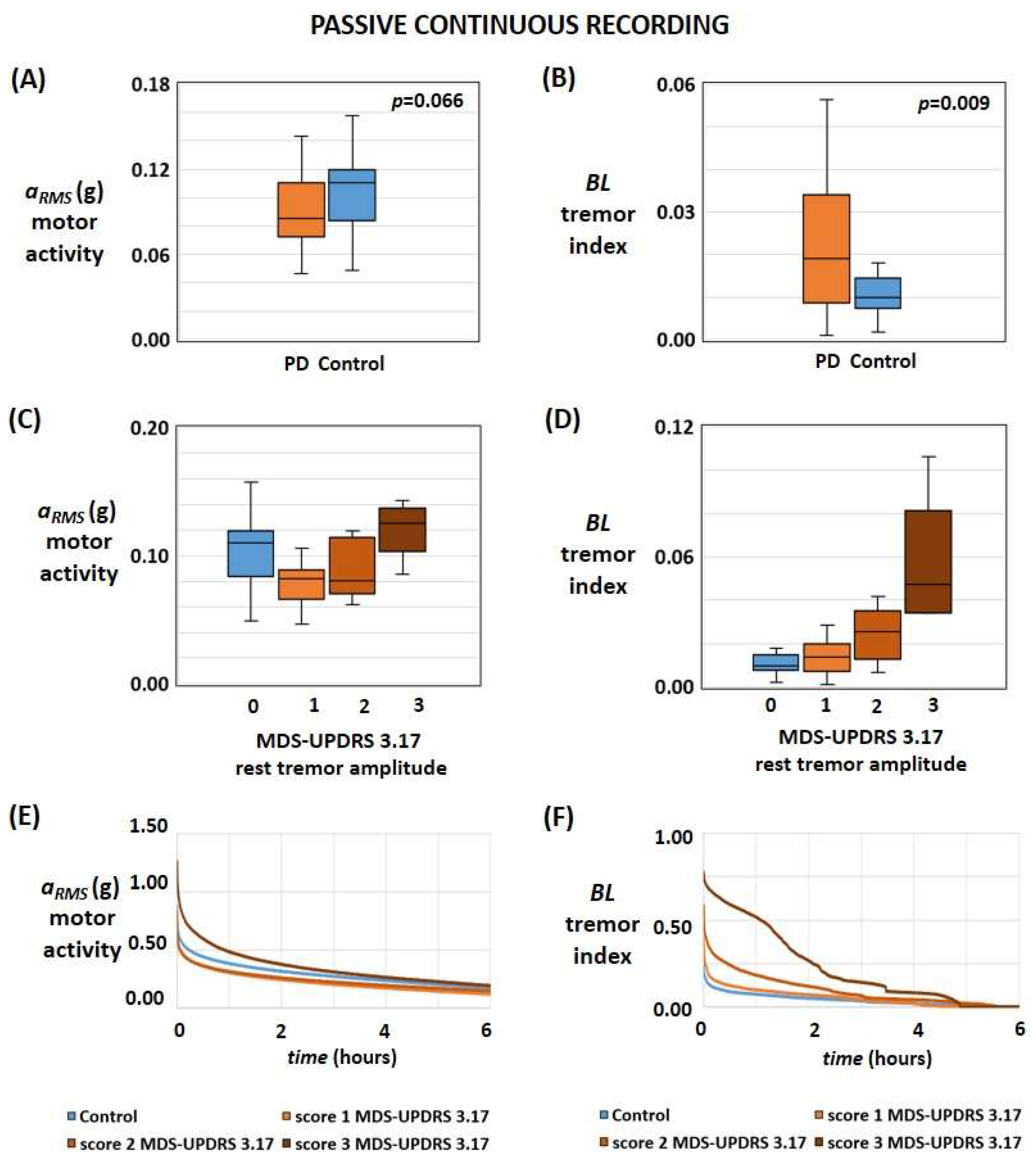
2.1. Passive Continuous Recording
- aRMS is the average value of the root mean square acceleration of the whole recording session (i.e., average daily motor activity).
- BL, also referred to as the tremor index, represents the average value of tremors for the entire 24-h recording (i.e., average daily tremor) computed by calculating the mean value of the daily pattern of said PSD ratio.
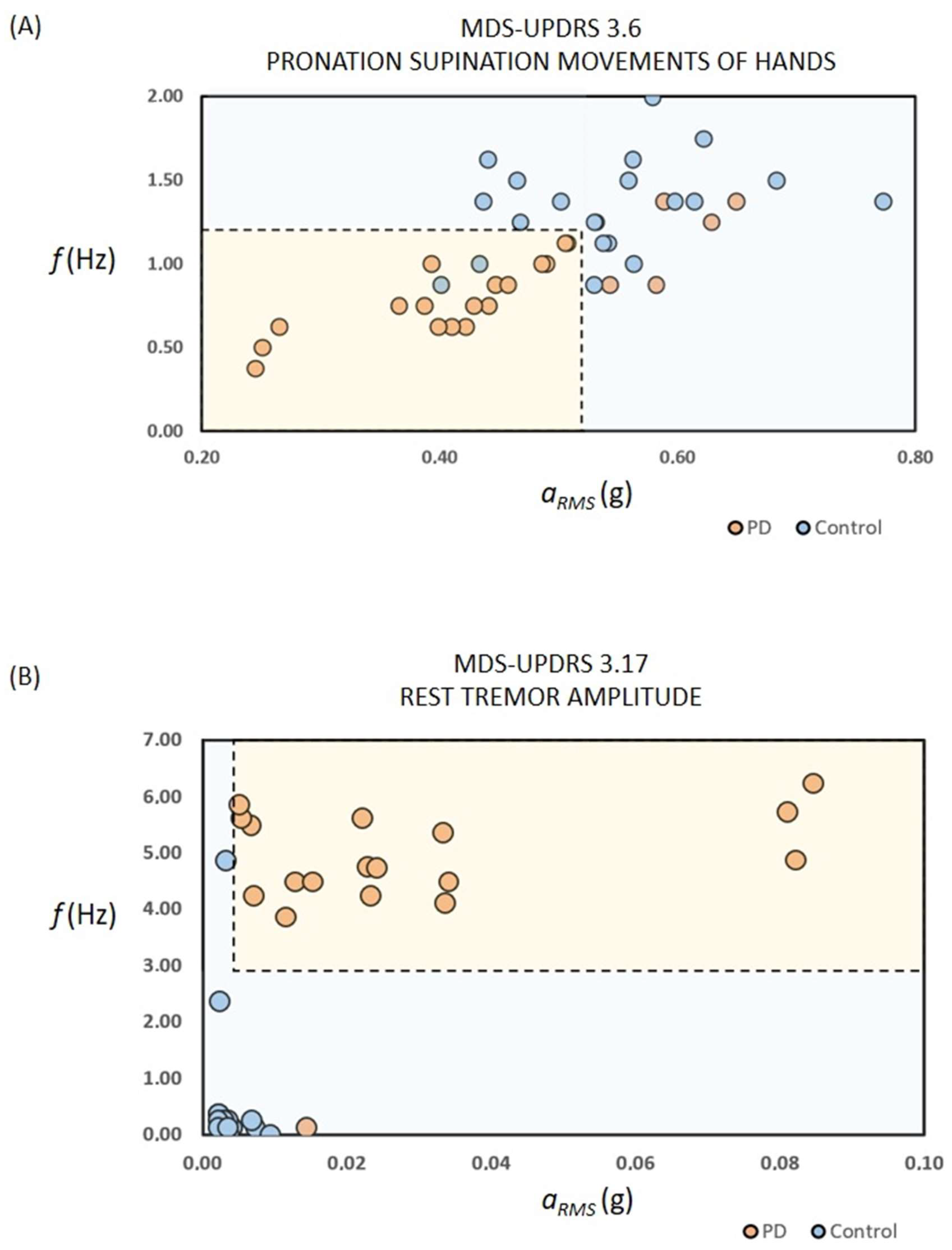
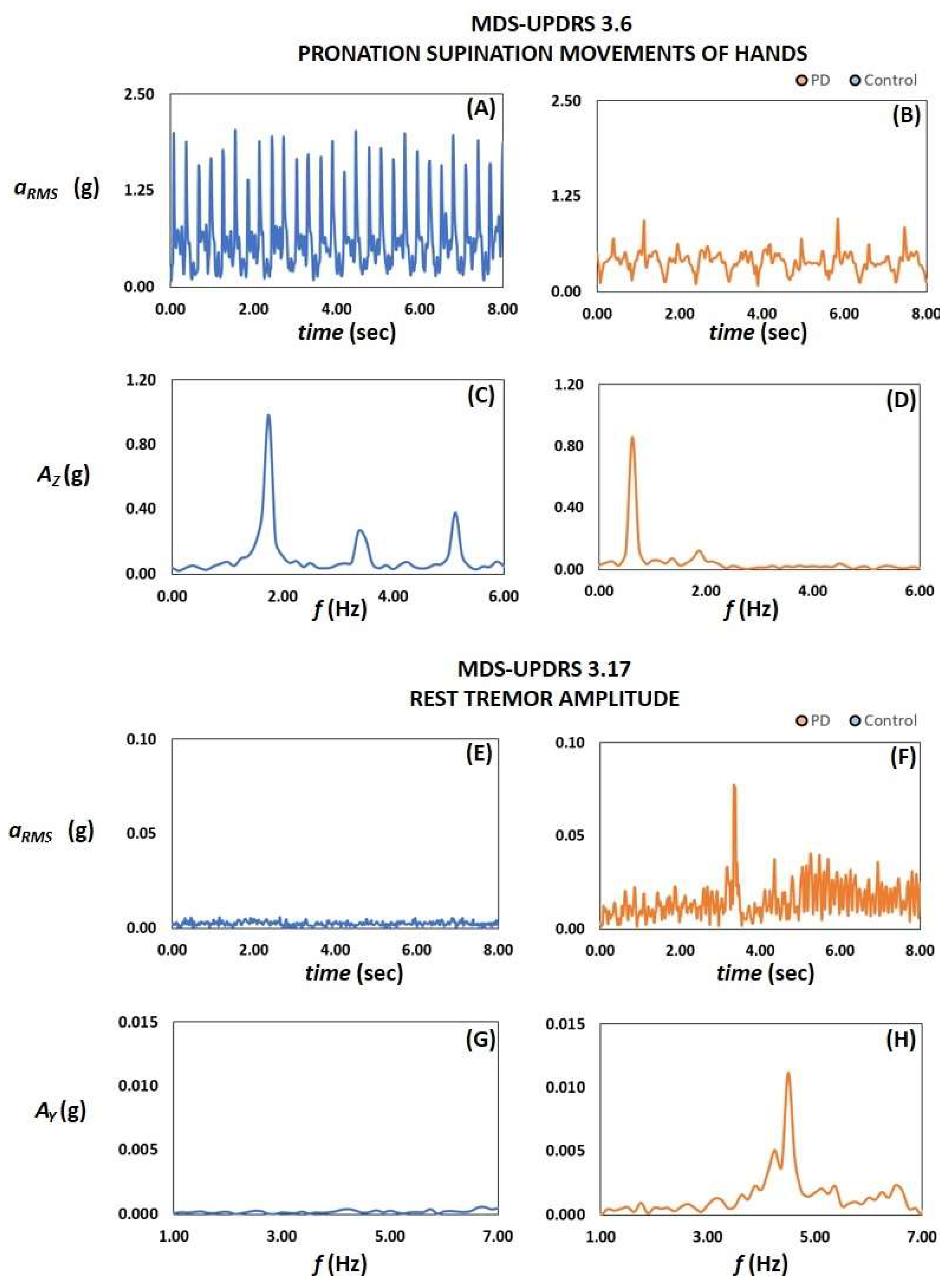
2.2. UPDRS-Based Active Tests
- aRMS is the average value of the root mean square acceleration of the whole recording session.
- AAVG, the average value of the values Ax, Ay, Az in the range between 3 Hz and 7 Hz, where Ax, Ay, Az are the Fast Fourier Transforms of the time-acceleration signals ax, ay, az for the x, y, and z axis, respectively.
- AMAX, the maximum value of Ax, Ay, Az in the range between 3 Hz and 7 Hz.
- For each axis of the tri-axial accelerometer, the frequency peaks occurring in a specific frequency range fP,x, fP,y, fP,z and the amplitude AP,x, AP,y, AP,z of each peak were computed.
2.3. Statistical Analysis
3. Results
3.1. Passive Continuous Recording
3.2. UPDRS-Based Active Tests
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- De Lau, L.M.L.; Breteler, M.M.B. Epidemiology of Parkinson’s disease. Lancet Neurol. 2006, 5, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Rizek, P.; Kumar, N.; Jog, M.S. An update on the diagnosis and treatment of Parkinson disease. Can. Med. Assoc. J. 2016, 188, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Janckovic, J. Parkinson’s disease: Clinical features diagnosis. J. Neurol. Neurosurg. Psychiatry 2008, 79, 368–376. [Google Scholar] [CrossRef] [PubMed]
- Postuma, R.B.; Berg, D.; Stern, M.; Poewe, W.; Olanow, C.W.; Oertel, W.; Obeso, J.; Marek, K.; Litvan, I.; Lang, A.E.; et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov. Disord. 2015, 30, 1591–1601. [Google Scholar] [CrossRef] [PubMed]
- Goetz, C.G.; Tilley, B.C.; Shaftman, S.R.; Stebbins, G.T.; Fahn, S.; Martinez-Martin, P.; Poewe, W.; Sampaio, C.; Stern, M.B.; Dodel, R.; et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating. Scale (MDS-UPDRS): Scale presentation and clinimetric testing results. Mov. Disord. 2008, 23, 2129–2170. [Google Scholar] [CrossRef] [PubMed]
- Barroso Júnior, M.C.; Esteves, G.P.; Nunes, T.P.; Silva, L.M.; Faria, A.C.D.; Melo, P.L. A telemedicine instrument for remote evaluation of tremor: Design and initial applications in fatigue and patients with Parkinson’s disease. Biomed. Eng. Online 2011, 10, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Brown, R.G.; MacCarthy, B.; Jahanshahi, M.; Marsden, C.D. Accuracy of self reported disability in patients with parkinsonism. Arch. Neurol. 1989, 46, 955–959. [Google Scholar] [CrossRef]
- Parnetti, L.; Cicognola, C.; Eusebi, P.; Chiasserini, D. Value of cerebrospinal fluid α-synuclein species as biomarker in Parkinson’s diagnosis and prognosis. Biomark. Med. 2016, 10, 35–49. [Google Scholar] [CrossRef]
- Li, T.; Le, W. Biomarkers for Parkinson’s Disease: How Good Are They? Neurosci. Bull. 2020, 36, 183–194. [Google Scholar] [CrossRef]
- He, R.; Yan, X.; Guo, J.; Xu, Q.; Tang, B.; Sun, Q. Recent Advances in Biomarkers for Parkinson’s Disease. Front. Aging Neurosci. 2018, 10, 305. [Google Scholar] [CrossRef]
- Alalayah, K.M.; Senan, E.M.; Atlam, H.F.; Ahmed, I.A.; Shatnawi, H.S.A. Automatic and Early Detection of Parkinson’s Disease by Analyzing Acoustic Signals Using Classification Algorithms Based on Recursive Feature Elimination Method. Diagnostics 2023, 13, 1924. [Google Scholar] [CrossRef] [PubMed]
- Avuçlu, E.; Elen, A. Evaluation of train and test performance of machine learning algorithms and Parkinson diagnosis with statistical measurements. Med. Biol. Eng. Comput. 2020, 58, 2775–2788. [Google Scholar] [CrossRef]
- Gupta, U.; Bansal, H.; Joshi, D. An improved sex-specific and age-dependent classification model for Parkinson’s diagnosis using handwriting measurement. Comput. Methods Programs Biomed. 2020, 189, 05305. [Google Scholar] [CrossRef]
- Mahlknecht, P.; Pechlaner, R.; Boesveldt, S.; Volc, D.; Pinter, B.; Reiter, E.; Müller, C.; Krismer, F.; Berendse, H.W.; van Hilten, J.J.; et al. Optimizing odor identification testing as quick and accurate diagnostic tool for Parkinson’s disease. Mov. Disord. 2016, 31, 1408–1413. [Google Scholar] [CrossRef]
- Schalkamp, A.K.; Peall, K.J.; Harrison, N.A.; Sandor, C. Wearable movement-tracking data identify Parkinson’s disease years before clinical diagnosis. Nat. Med. 2023. Epub ahead of print. [Google Scholar] [CrossRef]
- Chudzik, A.; Śledzianowski, A.; Przybyszewski, A.W. Machine Learning and Digital Biomarkers Can Detect Early Stages of Neurodegenerative Diseases. Sensors 2024, 24, 1572. [Google Scholar] [CrossRef] [PubMed]
- Di Cesare, M.G.; Perpetuini, D.; Cardone, D.; Merla, A. Machine Learning-Assisted Speech Analysis for Early Detection of Parkinson’s Disease: A Study on Speaker Diarization and Classification Techniques. Sensors 2024, 24, 1499. [Google Scholar] [CrossRef] [PubMed]
- Loh, H.W.; Hong, W.; Ooi, C.P.; Chakraborty, S.; Barua, P.D.; Deo, R.C.; Soar, J.; Palmer, E.E.; Acharya, U.R. Application of Deep Learning Models for Automated Identification of Parkinson’s Disease: A Review (2011–2021). Sensors 2021, 21, 7034. [Google Scholar] [CrossRef]
- Berg, D.; Postuma, R.B.; Adler, C.H.; Bloem, B.R.; Chan, P.; Dubois, B.; Gasser, T.; Goetz, C.G.; Halliday, G.; Joseph, L.; et al. MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 2015, 30, 1600–1611. [Google Scholar] [CrossRef]
- Cova, I.; Priori, A. Diagnostic biomarkers for Parkinson’s disease at a glance: Where are we? J. Neural Transm. 2018, 125, 1417–1432. [Google Scholar] [CrossRef]
- Heinzel, S.; Berg, D.; Gasser, T.; Chen, H.; Yao, C.; Postuma, R.B.; MDS Task Force on the Definition of Parkinson’s Disease. Update of the MDS research criteria for prodromal Parkinson’s disease. Mov. Disord. 2019, 34, 1464–1470. [Google Scholar] [CrossRef]
- Sica, M.; Tedesco, S.; Crowe, C.; Kenny, L.; Moore, K.; Timmons, S.; Barton, J.; O’Flynn, B.; Komaris, D.-S. Continuous home monitoring of Parkinson’s disease using inertial sensors: A systematic review. PLoS ONE 2021, 16, e0246528. [Google Scholar] [CrossRef]
- Morgan, C.; Rolinski, M.; McNaney, R.; Jones, B.; Rochester, L.; Maetzler, W.; Craddock, I.; Whone, A.L. Systematic Review Looking at the Use of Technology to Measure Free-Living Symptom and Activity Outcomes in Parkinson’s Disease in the Home or a Home-Like Environment. J. Park. Dis. 2020, 10, 429–454. [Google Scholar] [CrossRef]
- Mirelman, A.; Siderowf, A.; Chahine, L. Outcome Assessment in Parkinson Disease Prevention Trials: Utility of Clinical and Digital Measures. Neurology 2022, 99 (Suppl. 1), 52–60. [Google Scholar] [CrossRef]
- Battista, L.; Romaniello, A. A novel device for continuous monitoring of tremor and other motor symptoms. Neurol. Sci. 2018, 39, 1333–1343. [Google Scholar] [CrossRef]
- Battista, L.; Romaniello, A. A wearable tool for selective and continuous monitoring of tremor and dyskinesia in Parkinsonian patients. Park. Relat. Disord. 2020, 77, 43–47. [Google Scholar] [CrossRef] [PubMed]
- Battista, L.; Casali, M.; Brusa, L.; Radicati, F.G.; Stocchi, F. Clinical assessment of a new wearable tool for continuous and objective recording of motor fluctuations and ON/OFF states in patients with Parkinson’s disease. PLoS ONE 2023, 18, e0287139. [Google Scholar] [CrossRef] [PubMed]
- Kassavetis, P.; Saifee, T.A.; Roussos, G.; Drougkas, L.; Kojovic, M.; Rothwell, J.C.; Edwards, M.J.; Bhatia, K.P. Developing a Tool for Remote Digital Assessment of Parkinson’s Disease. Mov. Disord. Clin. Pract. 2015, 3, 59–64. [Google Scholar] [CrossRef]
- Burq, M.; Rainaldi, E.; Ho, K.C.; Chen, C.; Bloem, B.R.; Evers, L.J.; Helmich, R.C.; Myers, L.; Marks, W.J., Jr.; Kapur, R. Virtual exam for Parkinson’s disease enables frequent and reliable remote measurements of motor function. Npj Digit. Med. 2022, 5, 65. [Google Scholar] [CrossRef]
- Lipsmeier, F.; Taylor, K.I.; Kilchenmann, T.; Wolf, D.; Scotland, A.; Schjodt-Eriksen, J.; Cheng, W.Y.; Fernandez-Garcia, I.; Siebourg-Polster, J.; Jin, L.; et al. Evaluation of smartphone-based testing to generate exploratory outcome measures in a phase 1 Parkinson’s disease clinical trial. Mov. Disord. 2018, 33, 1287–1297. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.L.; Kangarloo, T.; Tracey, B.; O’Donnell, P.; Volfson, D.; Latzman, R.D.; Zach, N.; Alexander, R.; Bergethon, P.; Cosman, J.; et al. Using a smartwatch and smartphone to assess early Parkinson’s disease in the WATCH-PD study. NPJ Park. Dis. 2023, 9, 64. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.W.; Hassett, L.M.; Nguy, V.; Allen, N.E. A Comparison of Activity Monitor Data from Devices Worn on the Wrist and the Waist in People with Parkinson’s Disease. Mov. Disord. Clin. Pract. 2019, 6, 693–699. [Google Scholar] [CrossRef] [PubMed]


| Subset 1 | Subset 2 | Total (Subset 1 + Subset 2) | ||||||
|---|---|---|---|---|---|---|---|---|
| Continuous Recording | Active Test | Continuous Recording | ||||||
| Characteristic | PD | Control | PD | Control | PD | Control | PD | Control |
| Number of subjects | 24 | 20 | 23 | 21 | 12 | 0 | 59 | 41 |
| Male | 15 | 9 | 13 | 12 | 6 | 0 | 34 | 21 |
| Female | 9 | 11 | 10 | 9 | 6 | 0 | 25 | 20 |
| Age | ||||||||
| Average (yr) | 65 | 61 | 70 | 60 | 65 | // | 67 | 61 |
| Standard deviation (yr) | 6 | 4 | 4 | 6 | 3 | // | 5 | 6 |
| Hoehn and Yahr Staging Scale | ||||||||
| Average | 2.3 | // | 2.0 | // | 2.9 | // | 2.3 | // |
| Standard deviation | 0.8 | // | 0.9 | // | 0.8 | // | 0.9 | // |
| MDS-UPDRS | ||||||||
| score 3.6 (pronation-supination) | 1.9 | // | 1.8 | // | 1.5 | // | // | // |
| score 3.17 (rest tremor) | 1.7 | // | 1.7 | // | 1.1 | // | // | // |
| score 4.1 (time with dyskinesia) | 0.0 | // | 0.0 | // | 1.5 | // | // | // |
| score 4.2 (impact of dyskinesia) | 0.0 | // | 0.0 | // | 1.5 | // | // | // |
| Parameter | Class #1 | Class #2 | Number of PD | Number of Controls | Statistic | Outcome |
|---|---|---|---|---|---|---|
| motor activity aRMS | Control | PD | 24 | 20 | p-value | p = 0.066—not statistically significant |
| Control | PD with MDS-UPDRS 3.17 score equal to 1 | 13 | 20 | Mann-Whitney U | U = 49 < UC—statistically significant difference | |
| Control | PD with MDS-UPDRS 3.17 score equal to 2 | 6 | 20 | Mann-Whitney U | U = 39 > UC—not statistically significant | |
| Control | PD with MDS-UPDRS 3.17 score equal to 2 and 3 | 11 | 20 | Mann-Whitney U | U = 107 < UC—statistically significant difference | |
| Control | PD with mild-to-moderate dyskinesia | 10 | 20 | Mann-Whitney U | U = 80 > UC—not statistically significant | |
| tremor index BL | Control | PD | 24 | 20 | p-value | p = 0.009—statistically significant difference |
| Control | PD with MDS-UPDRS 3.17 score equal to 1 | 13 | 20 | Mann-Whitney U | U = 109 > UC—not statistically significant | |
| Control | PD with MDS-UPDRS 3.17 score equal to 2 | 6 | 20 | Mann-Whitney U | U = 21 < UC—statistically significant difference | |
| Control | PD with MDS-UPDRS 3.17 score equal to 2 and 3 | 11 | 20 | Mann-Whitney U | U = 21 < UC—statistically significant difference |
| Test | Parameter(s) | Condition(s) | AUC | TP | TN | FP | FN | Sensitivity | Specificity | Accuracy | F1-Score | Kappa |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Continuous passive recording | aRMS | aRMS < aT | 0.626 | 17 | 15 | 5 | 7 | 0.71 | 0.75 | 0.73 | 0.74 | 0.45 |
| BL | BL > BLT | 0.701 | 12 | 20 | 0 | 12 | 0.50 | 1.00 | 0.73 | 0.67 | 0.48 | |
| BL, aRMS | (aRMS < aT) AND (BL > BLT) | // | 22 | 15 | 5 | 2 | 0.92 | 0.75 | 0.84 | 0.86 | 0.68 | |
| Active test 3.6 Pronation-supination movements of hands | aRMS | aRMS < aT,3.6 | 0.670 | 17 | 14 | 7 | 6 | 0.74 | 0.67 | 0.70 | 0.72 | 0.41 |
| f | f < fT1,3.6 | 0.764 | 17 | 17 | 4 | 6 | 0.74 | 0.81 | 0.77 | 0.77 | 0.55 | |
| f | f < fT2,3.6 | 0.764 | 19 | 15 | 6 | 4 | 0.83 | 0.71 | 0.77 | 0.79 | 0.54 | |
| f, aRMS | (aRMS < aT,3.6) AND (f < fT1,3.6) | // | 17 | 19 | 2 | 6 | 0.74 | 0.90 | 0.82 | 0.81 | 0.64 | |
| Active test 3.17 Rest tremor amplitude | aRMS | aRMS > aT,3.17 | 0.870 | 19 | 18 | 3 | 0 | 1.00 | 0.86 | 0.93 | 0.93 | 0.85 |
| f | 3 Hz < f < 7 Hz | // | 18 | 20 | 1 | 1 | 0.95 | 0.95 | 0.95 | 0.95 | 0.90 | |
| f, aRMS | (aRMS > aT,3.17) AND (3 Hz < f < 7 Hz) | // | 18 | 21 | 0 | 1 | 0.95 | 1.00 | 0.98 | 0.97 | 0.95 | |
| AAVG | AAVG > AT1,3.17 | 0.919 | 19 | 19 | 2 | 0 | 1.00 | 0.90 | 0.95 | 0.95 | 0.90 | |
| AAVG | AAVG > AT2,3.17 | 0.919 | 18 | 20 | 1 | 1 | 0.95 | 0.95 | 0.95 | 0.95 | 0.90 | |
| AMAX | AMAX > AT,3.17 | 1.000 | 19 | 21 | 0 | 0 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |
| Active test 3.15 Postural tremor of hands | aRMS | aRMS > aT1,3.15 | 0.803 | 17 | 17 | 4 | 2 | 0.89 | 0.81 | 0.85 | 0.85 | 0.70 |
| aRMS | aRMS > aT2,3.15 | 0.803 | 16 | 18 | 3 | 3 | 0.84 | 0.86 | 0.85 | 0.84 | 0.70 | |
| f | 3 Hz < f < 7 Hz | // | 12 | 20 | 1 | 7 | 0.63 | 0.95 | 0.80 | 0.75 | 0.59 | |
| f, aRMS | (aRMS > aT1,3.17) AND (3 Hz < f < 7 Hz) | // | 11 | 21 | 0 | 8 | 0.58 | 1.00 | 0.80 | 0.73 | 0.59 | |
| f, aRMS | (aRMS > aT2,3.17) AND (3 Hz < f < 7 Hz) | // | 11 | 21 | 0 | 8 | 0.58 | 1.00 | 0.80 | 0.73 | 0.59 | |
| AAVG | AAVG > AT,3.15 | 0.905 | 18 | 20 | 1 | 1 | 0.95 | 0.95 | 0.95 | 0.95 | 0.90 | |
| AMAX | AMAX > ATM,3.15 | 0.852 | 15 | 21 | 0 | 4 | 0.79 | 1.00 | 0.90 | 0.88 | 0.80 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Battista, L.; Romaniello, A. A New Wrist-Worn Tool Supporting the Diagnosis of Parkinsonian Motor Syndromes. Sensors 2024, 24, 1965. https://doi.org/10.3390/s24061965
Battista L, Romaniello A. A New Wrist-Worn Tool Supporting the Diagnosis of Parkinsonian Motor Syndromes. Sensors. 2024; 24(6):1965. https://doi.org/10.3390/s24061965
Chicago/Turabian StyleBattista, Luigi, and Antonietta Romaniello. 2024. "A New Wrist-Worn Tool Supporting the Diagnosis of Parkinsonian Motor Syndromes" Sensors 24, no. 6: 1965. https://doi.org/10.3390/s24061965
APA StyleBattista, L., & Romaniello, A. (2024). A New Wrist-Worn Tool Supporting the Diagnosis of Parkinsonian Motor Syndromes. Sensors, 24(6), 1965. https://doi.org/10.3390/s24061965







