Influence of a Three-Month Mixed Reality Training on Gait Speed and Cognitive Functions in Adults with Intellectual Disability: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Procedure
2.2.1. Study Design
2.2.2. Cognitive Assessment
2.2.3. Gait Analysis
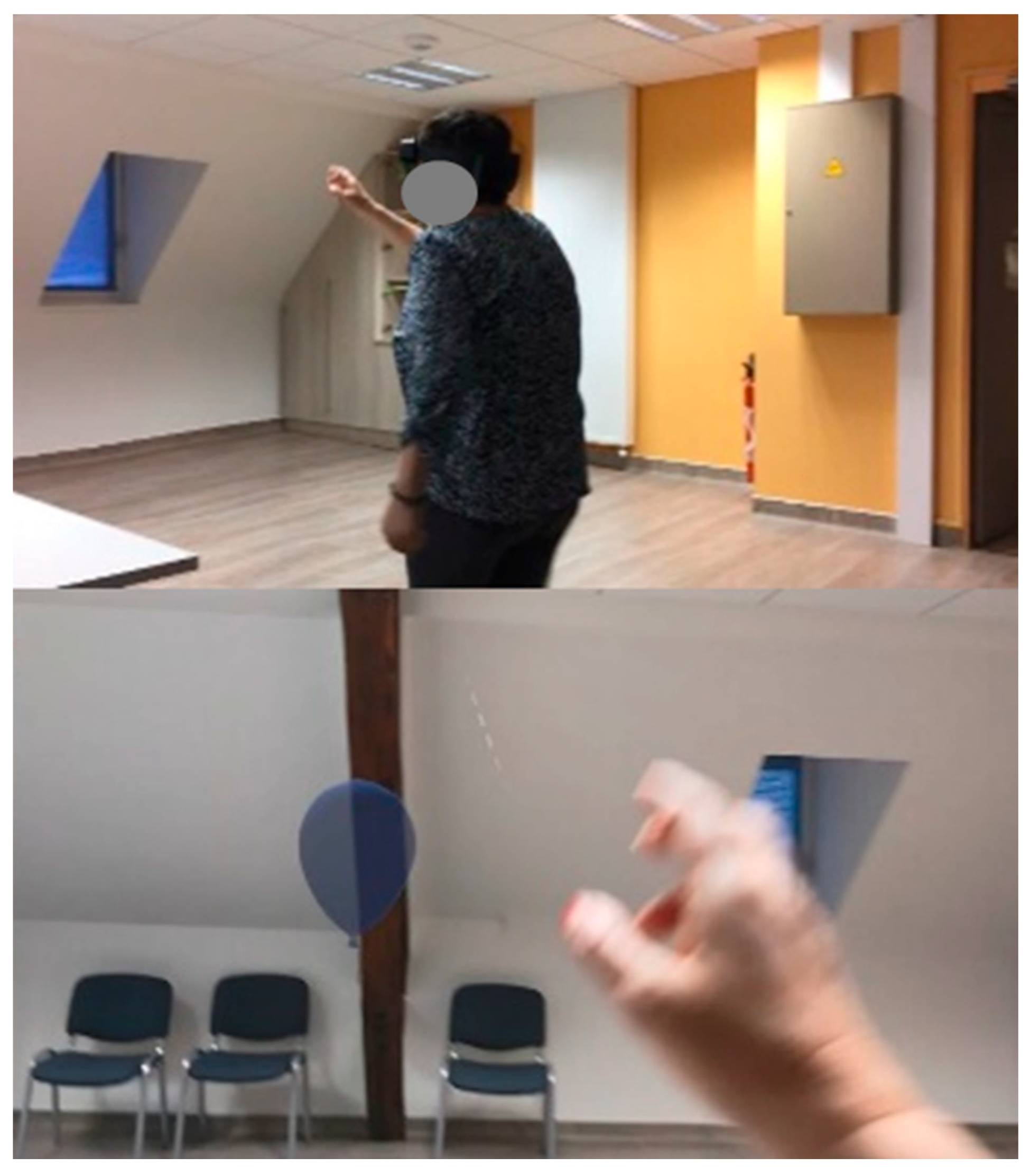
2.2.4. Mixed Reality Intervention
2.2.5. Statistical Analysis
3. Results
4. Discussion
4.1. Walking Speed
4.1.1. Initial Walking Speed
4.1.2. Increased Walking Speed after Training
4.1.3. Sensorimotor Functions Improvement
4.2. Cognitive Ability Improvement
4.3. Added Value of Mixed Reality
4.4. Limits
5. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Enkelaar, L.; Smulders, E.; van Schrojenstein Lantman-de Valk, H.; Geurts, A.C.H.; Weerdesteyn, V. A review of balance and gait capacities in relation to falls in persons with intellectual disability. Res. Dev. Disabil. 2012, 33, 291–306. [Google Scholar] [CrossRef]
- Almuhtaseb, S.; Oppewal, A.; Hilgenkamp, T.I.M. Gait characteristics in individuals with intellectual disabilities: A literature review. Res. Dev. Disabil. 2014, 35, 2858–2883. [Google Scholar] [CrossRef]
- Oppewal, A.; Festen, D.A.M.; Hilgenkamp, T.I.M. Gait Characteristics of Adults with Intellectual Disability. Am. J. Intellect. Dev. Disabil. 2018, 123, 283–299. [Google Scholar] [CrossRef]
- Carmeli, E.; Bar-Yossef, T.; Ariav, C.; Levy, R.; Liebermann, D.G. Perceptual-motor coordination in persons with mild intellectual disability. Disabil. Rehabil. 2008, 30, 323–329. [Google Scholar] [CrossRef]
- Smulders, E.; Enkelaar, L.; Weerdesteyn, V.; Geurts, A.C.H.; van Schrojenstein Lantman-de Valk, H. Falls in older persons with intellectual disabilities: Fall rate, circumstances and consequences: Falls in persons with ID. J. Intellect. Disabil. Res. 2012, 57, 1173–1182. [Google Scholar] [CrossRef]
- Diamond, A. Close Interrelation of Motor Development and Cognitive Development and of the Cerebellum and Prefrontal Cortex. Child Dev. 2000, 71, 44–56. [Google Scholar] [CrossRef]
- Azadian, E.; Torbati, H.R.T.; Kakhki, A.R.S.; Farahpour, N. The effect of dual task and executive training on pattern of gait in older adults with balance impairment: A Randomized controlled trial. Arch. Gerontol. Geriatr. 2016, 62, 83–89. [Google Scholar] [CrossRef]
- Hillman, C.H.; Erickson, K.I.; Kramer, A.F. Be smart, exercise your heart: Exercise effects on brain and cognition. Nat. Rev. Neurosci. 2008, 9, 58–65. [Google Scholar] [CrossRef]
- Bayot, M.; Dujardin, K.; Tard, C.; Defebvre, L.; Bonnet, C.T.; Allart, E.; Delval, A. The interaction between cognition and motor control: A theoretical framework for dual-task interference effects on posture, gait initiation, gait and turning. Neurophysiol. Clin. 2018, 48, 361–375. [Google Scholar] [CrossRef]
- Künstler, E.C.S.; Finke, K.; Günther, A.; Klingner, C.; Witte, O.; Bublak, P. Motor-cognitive dual-task performance: Effects of a concurrent motor task on distinct components of visual processing capacity. Psychol. Res. 2018, 82, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Herold, F.; Wiegel, P.; Hamacher, D.; Schega, L. Brain activity during walking: A systematic review. Neurosci. Biobehav. Rev. 2015, 57, 310–327. [Google Scholar] [CrossRef] [PubMed]
- Al-Issa, H.; Regenbrecht, H.; Hale, L. Augmented reality applications in rehabilitation to improve physical outcomes. Phys. Ther. Rev. 2012, 17, 16–28. [Google Scholar] [CrossRef]
- Bioulac, S.; de Sevin, E.; Sagaspe, P.; Claret, A.; Philip, P.; Micoulaud-Franchi, J.; Bouvard, M. Qu’apportent les outils de réalité virtuelle en psychiatrie de l’enfant et l’adolescent ? L’Encéphale 2018, 44, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Ryu, J.; Choi, Y.; Kang, Y.; Li, H.; Kim, K. Eye-Contact Game Using Mixed Reality for the Treatment of Children with Attention Deficit Hyperactivity Disorder. IEEE Access 2020, 8, 45996–46006. [Google Scholar] [CrossRef]
- Levin, M.F.; Demers, M. Motor learning in neurological rehabilitation. Disabil. Rehabil. 2021, 43, 3445–3453. [Google Scholar] [CrossRef]
- Klinger, E.; Chemin, I.; Lebreton, S.; Marié, R.-M. Virtual Action Planning in Parkinson’s Disease: A Control Study. Cyberpsychol. Behav. 2006, 9, 342–347. [Google Scholar] [CrossRef] [PubMed]
- Prasertsakul, T.; Kaimuk, P.; Chinjenpradit, W.; Limroongreungrat, W.; Charoensuk, W. The effect of virtual reality-based balance training on motor learning and postural control in healthy adults: A randomized preliminary study. Biomed. Eng. Online 2018, 17, 124. [Google Scholar] [CrossRef]
- Lopes, J.B.P.; Duarte, N.d.A.C.; Lazzari, R.D.; Oliveira, C.S. Virtual reality in the rehabilitation process for individuals with cerebral palsy and Down syndrome: A systematic review. J. Bodyw. Mov. Ther. 2020, 24, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Lotan, M.; Weiss, P.L. Improving Balance in Adults with Intellectual Developmental Disorder via Virtual Environments. Percept. Mot. Skills 2021, 128, 2638–2653. [Google Scholar] [CrossRef]
- Hughes, C.L.; Fidopiastis, C.; Stanney, K.M.; Bailey, P.S.; Ruiz, E. The Psychometrics of Cybersickness in Augmented Reality. Front. Virtual Real. 2020, 1, 602954. [Google Scholar] [CrossRef]
- Kaufeld, M.; De Coninck, K.; Schmidt, J.; Hecht, H. Chewing gum reduces visually induced motion sickness. Exp. Brain Res. 2022, 240, 651–663. [Google Scholar] [CrossRef] [PubMed]
- Vovk, A.; Wild, F.; Guest, W.; Kuula, T. Simulator Sickness in Augmented Reality Training Using the Microsoft HoloLens. In Proceedings of the 2018 Conference on Human Factors in Computing Systems, Montréal, QC, Canada, 21–26 April 2018. [Google Scholar] [CrossRef]
- Kirollos, R.; Merchant, W. Comparing Cybersickness in Virtual Reality and Mixed Reality Head-Mounted Displays. Front. Virtual Real. 2023, 4, 1130864. [Google Scholar] [CrossRef]
- Glueck, A.C.; Han, D.Y. Improvement potentials in balance and visuo-motor reaction time after mixed reality action game play: A pilot study. Virtual Real. 2020, 24, 223–229. [Google Scholar] [CrossRef]
- Laly, A.; Biard, J.C.; Tixier, P.A.; Ferrari, A.; Rosnet, E.; Houel, N. Influence of a Mixed Reality Training on Gait in People with Mental Disabilities. In Proceedings of the 28th Congress of the International Society of Biomechanics, ISB 2021, Stockholm, Sweden, 25–29 July 2021. [Google Scholar]
- Pellecchia, G.L. Dual-Task Training Reduces Impact of Cognitive Task on Postural Sway. J. Motor Behav. 2005, 37, 239–246. [Google Scholar] [CrossRef]
- Li, K.Z.H.; Roudaia, E.; Lussier, M.; Bherer, L.; Leroux, A.; McKinley, P.A. Benefits of Cognitive Dual-Task Training on Balance Performance in Healthy Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2010, 65A, 1344–1352. [Google Scholar] [CrossRef]
- de Andrade, L.P.; Gobbi, L.T.B.; Coelho, F.G.M.; Christofoletti, G.; Costa, J.L.R.; Stella, F. Benefits of Multimodal Exercise Intervention for Postural Control and Frontal Cognitive Functions in Individuals with Alzheimer’s Disease: A Controlled Trial. J. Am. Geriatr. Soc. 2013, 61, 1919–1926. [Google Scholar] [CrossRef] [PubMed]
- Atak, E.; Algun, Z.C. Dual-Task Balance Training for Motor Skill Development among Children with Intelligence Quotient Discrepancy. Rehabil. Res. Pract. 2022, 2022, 2822171. [Google Scholar] [CrossRef]
- Fishbein, P.; Hutzler, Y.; Ratmansky, M.; Treger, I.; Dunsky, A. A Preliminary Study of Dual-Task Training Using Virtual Reality: Influence on Walking and Balance in Chronic Poststroke Survivors. J. Stroke Cerebrovasc. Dis. 2019, 28, 104343. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool for Mild Cognitive Impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Smith, T.; Gildeh, N.; Holmes, C. The Montreal Cognitive Assessment: Validity and Utility in a Memory Clinic Setting. Can. J. Psychiatry 2007, 52, 329–332. [Google Scholar] [CrossRef]
- Pelletier, S.; Nalpas, B.; Alarcon, R.; Rigole, H.; Perney, P. Investigation of Cognitive Improvement in Alcohol-Dependent Inpatients Using the Montreal Cognitive Assessment (MoCA) Score. J. Addict. 2016, 2016, 1539096. [Google Scholar] [CrossRef]
- Bernstein, I.H.; Lacritz, L.; Barlow, C.E.; Weiner, M.F.; DeFina, L.F. Psychometric Evaluation of the Montreal Cognitive Assessment (MoCA) in Three Diverse Samples. Clin. Neuropsychol. 2011, 25, 119–126. [Google Scholar] [CrossRef]
- Vallabhajosula, S.; Humphrey, S.K.; Cook, A.J.; Freund, J.E. Concurrent Validity of the Zeno Walkway for Measuring Spatiotemporal Gait Parameters in Older Adults. J. Geriatr. Phys. Ther. 2019, 42, E42–E50. [Google Scholar] [CrossRef]
- Lynall, R.C.; Zukowski, L.A.; Plummer, P.; Mihalik, J.P. Reliability and validity of the protokinetics movement analysis software in measuring center of pressure during walking. Gait Posture 2017, 52, 308–311. [Google Scholar] [CrossRef]
- Inman, V.T.; Ralston, H.J.; Todd, F. Human Walking; Williams & Wilkins: Philadelphia, PA, USA, 1981. [Google Scholar]
- Verlinden, V.; van der Geest, J.; Hoogendam, Y.; Hofman, A.; Breteler, M.; Ikram, M. Gait patterns in a community-dwelling population aged 50 years and older. Gait Posture 2013, 37, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Hollman, J.H.; McDade, E.M.; Petersen, R.C. Normative spatiotemporal gait parameters in older adults. Gait Posture 2011, 34, 111–118. [Google Scholar] [CrossRef]
- Middleton, A.; Fritz, S.L.; Lusardi, M. Walking Speed: The Functional Vital Sign. J. Aging Phys. Act. 2015, 23, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.; Williams Andrews, A. Normal walking speed: A descriptive meta-analysis. Physiotherapy 2011, 97, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.E.; Ostir, G.V.; Fisher, S.R.; Ottenbacher, K.J. Assessing walking speed in clinical research: A systematic review. J. Eval. Clin. Pract. 2008, 14, 552–562. [Google Scholar] [CrossRef]
- Hilgenkamp, T.I.M.; van Wijck, R.; Evenhuis, H.M. Low physical fitness levels in older adults with ID: Results of the HA-ID study. Res. Dev. Disabil. 2012, 33, 1048–1058. [Google Scholar] [CrossRef]
- Choi, H.; Lim, J.; Lee, S. Body Fat-Related Differences in Gait Parameters and Physical Fitness Level in Weight-Matched Male Adults. Clin. Biomech. 2021, 81, 105243. [Google Scholar] [CrossRef]
- Farrell, J.W.; Merkas, J.; Pilutti, L.A. The Effect of Exercise Training on Gait, Balance, and Physical Fitness Asymmetries in Persons with Chronic Neurological Conditions: A Systematic Review of Randomized Controlled Trials. Front. Physiol. 2020, 11, 585765. [Google Scholar] [CrossRef] [PubMed]
- Okur, E.O.; Arik, M.I.; Okur, I.; Gokpinar, H.H.; Gunel, M.K. Dual-task training effect on gait parameters in children with spastic diplegic cerebral palsy: Preliminary results of a self-controlled study. Gait Posture 2022, 94, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Yogev-Seligmann, G.; Giladi, N.; Brozgol, M.; Hausdorff, J.M. A Training Program to Improve Gait While Dual Tasking in Patients with Parkinson’s Disease: A Pilot Study. Arch. Phys. Med. Rehabil. 2012, 93, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Wilkerson, G.B.; Nabhan, D.C.; Crane, R.T. Upper-Extremity Perceptual-Motor Training Improves Whole-Body Reactive Agility Among Elite Athletes with History of Sport-Related Concussion. J. Sport Rehabil. 2021, 30, 844–849. [Google Scholar] [CrossRef]
- Azar, N.R.; McKeen, P.; Carr, K.; Sutherland, C.A.; Horton, S. Impact of motor skills training in adults with autism spectrum disorder and an intellectual disability. J. Dev. Disabil. 2016, 22, 28–38. [Google Scholar]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. A structural equation model relating impaired sensorimotor function, fear of falling and gait patterns in older people. Gait Posture 2007, 25, 243–249. [Google Scholar] [CrossRef]
- Krinsky Mchale, S.; Silverman, W. Dementia and mild cognitive impairment in adults with intellectual disability: Issues of diagnosis. Dev. Disabil. Res. Rev. 2013, 18, 31–42. [Google Scholar] [CrossRef]
- Souza, F.H.N.; Lisboa, A.K.P.; Maia, M.D.F.T.; Dos Santos, M.R.D.; Silva Filho, E.M.; Cezarino, L.G.; Cacho, R.O.; Cacho, Ê.W.A. Effects of dual task training on gait temporal-spatial parameters of children with autism. Man. Ther. Posturol. Rehabil. J. 2017, 15, 527. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef]


| Study Sample (18 Subjects) | ||
|---|---|---|
| Age | ||
| years, m ± sd, range | 44 ± 14, 23–69 | |
| Women | ||
| n (%) | 6 (33.3%) | |
| Height (m), m ± sd | 1.57 ± 0.10 | |
| Mass (kg) m ± sd | 60.67 ± 14.9 | |
| Men | ||
| n (%) | 12 (66.7%) | |
| Height (m) m ± sd | 1.73 ± 0.04 | |
| Mass (kg) m ± sd | 85.4 ± 31.0 | |
| Known co-disorders | ||
| ASD, n (%) | 4 men (22.2%) | |
| Pre | Post | p-Value (Statistic Test) | ||
|---|---|---|---|---|
| m ± sd | m ± sd | |||
| Gait spatiotemporal parameters | ||||
| Speed, | cm/s | 78.13 ± 22.03 | 89.10 ± 29.85 | 0.028 * |
| cadence, | step/min | 101.40 ± 13.59 | 104.55 ± 19.38 | 0.382 |
| Walk Ratio, | cm/step/min | 0.45 ± 0.11 | 0.46 ± 0.08 | 0.314 |
| Step length, | cm | 44.78 ± 10.33 | 48.12 ± 11.20 | 0.048 * |
| Stride length, | cm | 89.58 ± 20.87 | 97.40 ± 22.77 | 0.039 * |
| Stride width, | cm | 12.96 ± 4.33 | 12.76 ± 4.27 | 0.700 |
| Step time, | s | 0.59 ± 0.08 | 0.57 ± 0.11 | 0.132 |
| Sride time, | s | 1.18 ± 0.17 | 1.16 ± 0.23 | 0.215 |
| Stance phase, | s | 0.77 ± 0.14 | 0.75 ± 0.17 | 0.372 |
| Stance phase, | %GC | 65.85 ± 3.31 | 65.79 ± 3.26 | 0.472 |
| Single support time, | %GC | 33.86 ± 3.02 | 34.21 ± 4.22 | 0.777 |
| Double support time, | %GC | 31.41 ± 6.81 | 32.44 ± 6.52 | 0.306 |
| Initial double support time, | %GC | 16.30 ± 3.09 | 16.19 ± 3.32 | 0.744 |
| Swing phase, | %GC | 34.12 ± 3.28 | 34.21 ± 3.26 | 0.472 |
| Feet angle asymetry, | 6.66 ± 5.40 | 7.39 ± 5.79 | 0.602 | |
| Montréal Cognitive Assement | ||||
| MoCA, | score/30 | 9.76 ± 6.20 | 11.18 ± 7.50 | 0.011 † |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Laly, A.; Rosnet, E.; Houel, N. Influence of a Three-Month Mixed Reality Training on Gait Speed and Cognitive Functions in Adults with Intellectual Disability: A Pilot Study. Sensors 2024, 24, 1821. https://doi.org/10.3390/s24061821
Laly A, Rosnet E, Houel N. Influence of a Three-Month Mixed Reality Training on Gait Speed and Cognitive Functions in Adults with Intellectual Disability: A Pilot Study. Sensors. 2024; 24(6):1821. https://doi.org/10.3390/s24061821
Chicago/Turabian StyleLaly, Alexis, Elisabeth Rosnet, and Nicolas Houel. 2024. "Influence of a Three-Month Mixed Reality Training on Gait Speed and Cognitive Functions in Adults with Intellectual Disability: A Pilot Study" Sensors 24, no. 6: 1821. https://doi.org/10.3390/s24061821
APA StyleLaly, A., Rosnet, E., & Houel, N. (2024). Influence of a Three-Month Mixed Reality Training on Gait Speed and Cognitive Functions in Adults with Intellectual Disability: A Pilot Study. Sensors, 24(6), 1821. https://doi.org/10.3390/s24061821






