Wearables for Monitoring and Postural Feedback in the Work Context: A Scoping Review
Abstract
1. Introduction
- What variables have been considered in the identification of postural changes?
- What location, type of fixation, and number of sensors have been used to monitor and provide postural feedback in the work context?
- Which occupations or work tasks have been analysed using wearables to monitor and provide postural feedback in the work context?
- Among the identified wearables, what type and source of feedback is being used for postural correction?
- What results have been reported following the application of postural feedback in a work context?
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Source
2.3. Selection of Evidence Sources
2.4. Data Extraction
2.5. Data Presentation
3. Results
| Author, Year | Study Design | Sample | Context/ Setting | Occupation/ Work Task | Region and Anatomical Plane Under Analysis |
|---|---|---|---|---|---|
| Ribeiro et al., 2014 [43] | Randomized controlled trial | = 49.6 ± 12.4 years Eligibility: with and/or without low back pain | Healthcare institution | Healthcare and administrative professionals | Lumbopelvic region; Sagittal and frontal plane |
| Thanathornwong et al., 2014 [44] | 2 × 2 crossover randomized trial | = N/S (Min: 25 and Max: 30 years) Eligibility: dentists working at least 6 h daily. | Hospital | Dentists during molar surgery | Cervical and upper trunk; Sagittal and frontal plane |
| Thanathornwong et al., 2014 [45] | 2 × 2 crossover randomized trial | = N/S (Min: 21 and Max: 23 years) Eligibility: minimum practice of 6 h daily as a dentist and scoring over 70% on the applied questionnaire. | Real N/S | Dental students | Cervical and upper trunk; Sagittal and frontal plane |
| Thanathornwong and Suebnukarn, 2015 [46] | 2 × 2 crossover randomized trial | = N/S (Min: 21 and Max: 23 years) Eligibility: minimum practice of 6 h daily in dental work tasks. | Dental clinic | Dental students | Upper trunk; Sagittal and frontal planes |
| Zhao et al., 2015 [47] | Observational descriptive study | = N/S | Real N/S | Healthcare caregivers | Spine (++ lumbar); Sagittal plane. |
| Yan et al., 2017 [48] | Validation study | = N/S | Laboratory context and real construction context | Construction workers during brick lifting and steel rod handling tasks | Head, Cervical, and thoracic region; Sagittal plane. |
| Doss et al., 2018 [49] | Analytical cross-sectional observational study | = 26.1 ± 9.1 years Eligibility: nursing students without a history of back pain. | Clinical experience in a N/S context | Nursing students/patient transfer | Trunk; Sagittal plane. |
| Lins et al., 2018 [50] | Pilot study (experimental) | n = 11 (M = 8 e F = 3) = N/S Eligibility: N/S | Real N/S | Welders | Cervical, thoracic, lumbar, scapular waist, elbows, wrists, and knees regions. N/S Plane |
| Bootsman et al., 2019 [51] | Analytical cross-sectional observational study | = 39.77 ± 13.6 years Eligibility: healthy nurses (without low back pain) who do not engage in sedentary work tasks. | Hospital | Nurses (9 nurses from the Neonatal Intensive Care Unit and 4 home care nurses) | Lumbar spine; Sagittal plane. |
| Lind et al., 2020 [52] | Observational study | = 23.33 ± 2.9 years Eligibility: workers without discomfort and/or work-related musculoskeletal injuries that could hinder order-picking tasks. | Multinational vehicle construction company | 2 employees in logistics applications and 13 employees in order picking and assembly tasks | Dominant upper limb and trunk; Sagittal plane. |
| Ribeiro et al., 2020 [53] | Randomized controlled trial | = 45.3 ± 13.2 years Eligibility: adult healthcare professionals, with or without current presence (or history) of low back pain, currently performing their work tasks normally. | Continuing care institutions and hospitals | Healthcare professionals | Lumbopelvic region; Sagittal and frontal planes. |
| Lind et al., 2023 [54] | Analytical observational study | = 30.8 ± 11.5 years Eligibility: healthy workers without a history of pain that would hinder their W.T | Warehouse | Warehouse workers | Trunk; Sagittal plane. |
3.1. Context/Setting, Occupation/Work Task and Region and Anatomical Plane under Analysis
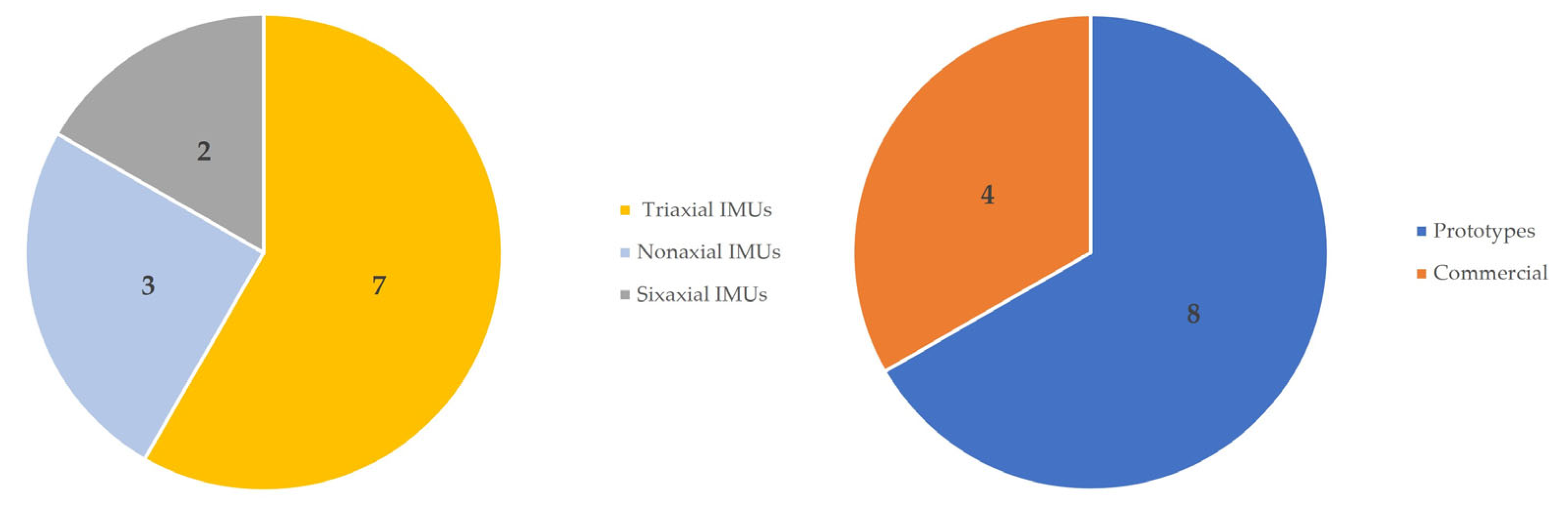
3.2. Type, Number of Sensors (Wearables), and Signal or Variable under Study
| Authors (Year) | Type, Number of Sensors (Wearables), and Signal or Variable under Study | Sensor Placement and Fixation | Feedback Source and Type |
|---|---|---|---|
| Ribeiro et al., 2014 [43] | Triaxial IMU (Accelerometer) 1 sensor (Commercial) Acceleration and linear position. | Laterally fixed on the participant’s belt at the level of the lumbopelvic region. | Integrated feedback in the sensor itself. Simultaneous intermittent auditory feedback. |
| Thanathornwong et al., 2014 [44] | Triaxial IMU (Accelerometer) 2 sensors (Prototype) Linear position. | Fixed on the PPE (visor) and posteriorly fixed on the worker’s uniform at the thoracic region (T4). | N/S Feedback. Visual feedback at the end. |
| Thanathornwong et al., 2014 [45] | Triaxial IMU (Accelerometer) 2 sensors (Prototype) Linear position. | Fixed on the PPE (visor) and posteriorly fixed on the worker’s uniform at the thoracic region. | N/S Feedback. Visual feedback at the end. |
| Thanathornwong and Suebnukarn, 2015 [46] | Triaxial IMU (Accelerometer) 1 sensor (Prototype) Trunk flexion, extension, and inclination linear position. | Fixed on the worker’s uniform, posteriorly at the thoracic region. | Integrated feedback in the sensor itself. Haptic feedback. |
| Zhao et al., 2015 [47] | Triaxial IMU (Accelerometer) 1 sensor (Commercial) Acceleration and linear position. | Smartwatch worn on the wrist (side determined by the participant). | Integrated feedback in the sensor itself. Haptic feedback. |
| Yan et al., 2017 [48] | Nonaxial IMU (triaxial Accelerometer, triaxial Gyroscope, and triaxial Magnetometer) 2 sensors (Commercial) Angular and linear acceleration. | Posteriorly fixed on the protective helmet and safety harness and vest at the thoracic region (between T1 and T2). | Smartphone-based feedback. Auditory feedback. |
| Doss et al., 2018 [49] | Triaxial IMU (Accelerometer) 2 sensors (Prototype) Trunk acceleration and linear position. | Tape-fixed at the thoracic (vest) and lumbar (belt) regions. | Smartphone-based feedback. Auditory feedback. |
| Lins et al., 2018 [50] | Sixaxial IMU (triaxial Accelerometer and triaxial Gyroscope) 15 sensors (Prototype) Linear and angular acceleration. | Tape-fixed on the worker’s uniform, specifically at the cervical, thoracic, lumbar, scapular waist, elbows, wrists, and knees regions. | Integrated feedback in the sensor itself. Haptic feedback. |
| Bootsman et al., 2019 [51] | Nonaxial IMU (triaxial Accelerometer, triaxial Gyroscope, and triaxial Magnetometer) 2 sensors (Prototype) Displacement, angular velocity, and linear acceleration. | Posteriorly fixed on the work uniform (in a built-in pocket) at the lumbar region, specifically between L1 and L5. | Smartphone-based feedback. Visual, auditory, and haptic feedback. |
| Lind et al., 2020 [52] | Nonaxial IMU (triaxial Accelerometer, triaxial Gyroscope, and triaxial Magnetometer) 3 sensors (Prototype) Angular and linear displacement of the trunk and dominant upper limb. | The IMU is bilaterally fixed on the worker’s arm (built-in pockets) at the deltoid muscle insertion. The haptic sensors are anteriorly fixed through a belt at the thoracic region (between T1–T2) and on the arm through an armband. | Smartphone-based feedback via Bluetooth. Haptic feedback. |
| Ribeiro et al., 2020 [53] | Triaxial IMU (Accelerometer) 1 sensor (Commercial). Acceleration and linear position. | Fixed on the belt at the lumbopelvic region. | Integrated feedback in the sensor itself. Auditory feedback. |
| Lind et al., 2023 [54] | Sixaxial IMU (triaxial Accelerometer and triaxial Gyroscope). 1 sensor (Prototype) Acceleration and linear position. | The IMU is fixed in a built-in pocket at the thoracic region (between T1 and T2). The haptic sensor is embedded in a pocket on the T-shirt at the sternum level. | Integrated feedback in the sensor itself. Haptic feedback. |
3.3. Sensor Placement and Fixation
3.4. Feedback Source and Type
3.5. Results after Feedback Application
| Authors (Year) | Results after Feedback Application |
|---|---|
| Ribeiro et al., 2014 [43] | In the constant feedback group, there was a reduction in lumbar flexion compared to the control and intermittent feedback groups, with constant feedback being more effective. |
| Thanathornwong et al., 2014 [44] | The group that received feedback significantly decreased cervical and upper thoracic extension, as well as reduced the likelihood of WRMSDs in the post-test. |
| Thanathornwong et al., 2014 [45] | There were statistically significant differences in reducing cervical extension with posterior alignment. |
| Thanathornwong and Suebnukarn, 2015 [46] | There was a decrease in trunk flexion and inclination in the upper body in the feedback group compared to the group without feedback. |
| Zhao et al., 2015 [47] | The system developed by the authors can be used to improve safe patient handling with the use of discrete tactile feedback in real time. |
| Yan et al., 2017 [48] | After an adaptation period of nearly a day to the proposed PPE, there was an improvement in tasks, indicating the effectiveness of self-awareness and self-regulation strategy. |
| Doss et al., 2018 [49] | After using feedback, statistically significant differences were observed in the task of transferring from bed to chair, including a decrease in the average time to complete the task, a reduction in peak trunk flexion and rotation, and triaxial speed and acceleration. |
| Lins et al., 2018 [50] | The results indicate that the ideal pulse length for haptic feedback application is about 150 ms, repeated 2 or 3 times within the sequence for maximum attention. |
| Bootsman et al., 2019 [51] | Improvement in lumbar posture compared to the group that did not receive any type of feedback, with no significant differences between the different types of feedback. |
| Lind et al., 2020 [52] | Decrease in elevation of the dominant upper limb and trunk flexion immediately after haptic feedback, which was maintained after its removal. |
| Ribeiro et al., 2020 [53] | There were no statistically significant differences between the groups with the application of auditory feedback to limit the threshold of trunk flexion. |
| Lind et al., 2023 [54] | Decrease in flexion and inclination of the upper trunk in the group with feedback compared to the group that did not receive haptic feedback. |
4. Discussion
4.1. Wearables and Variables of Human Movement in the Workplace Settings
4.2. Analysis and Feedback in the Workplace: Type, Location, Attachment, and Quantity of Sensors
4.3. Occupation and Work Tasks
4.4. Feedback Source and Type
4.5. Results after Feedback Application
4.6. Limitations of the Study
4.7. Suggestions for Future Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Seeberg, K.G.V.; Andersen, L.L.; Bengtsen, E.; Sundstrup, E. Effectiveness of workplace interventions in rehabilitating musculoskeletal disorders and preventing its consequences among workers with physical and sedentary employment: Systematic review protocol. Syst. Rev. 2019, 8, 1–7. [Google Scholar] [CrossRef]
- Ciccarelli, M.; Corradini, F.; Germani, M.; Menchi, G.; Mostarda, L.; Papetti, A.; Piangerelli, M. SPECTRE: A deep learning network for posture recognition in manufacturing. J. Intell. Manuf. 2022, 34, 3469–3481. [Google Scholar] [CrossRef]
- Lorenzini, M.; Ciotti, S.; Gandarias, J.M.; Fani, S.; Bianchi, M.; Ajoudani, A. Performance Analysis of Vibrotactile and Slide-and-Squeeze Haptic Feedback Devices for Limbs Postural Adjustment. In Proceedings of the 31st IEEE International Conference on Robot and Human Interactive Communication: Social, Asocial, and Antisocial Robots (RO-MAN), Napoli, Italy, 29–31 August 2022; pp. 707–713. [Google Scholar]
- Iñigo, I.; Lorenzo, M. Work-Related Musculoskeletal Disorders: Prevalence, Costs and Demographics in the EU—Salud y Seguridad en el Trabajo—EU-OSHA; 9789294791450; EU-OSHA: Luxembourg, 2020. [Google Scholar]
- Cerqueira, S.M.; Da Silva, A.F.; Santos, C.P. Smart Vest for Real-Time Postural Biofeedback and Ergonomic Risk Assessment. IEEE Access 2020, 8, 107583–107592. [Google Scholar] [CrossRef]
- Sundstrup, E.; Seeberg, K.G.V.; Bengtsen, E.; Andersen, L.L. A Systematic Review of Workplace Interventions to Rehabilitate Musculoskeletal Disorders Among Employees with Physical Demanding Work. J. Occup. Rehabil. 2020, 30, 588–612. [Google Scholar] [CrossRef]
- Lee, R.; James, C.; Edwards, S.; Skinner, G.; Young, J.L.; Snodgrass, S.J. Evidence for the Effectiveness of Feedback from Wearable Inertial Sensors during Work-Related Activities: A Scoping Review. Sensors 2021, 21, 6377. [Google Scholar] [CrossRef]
- Antwi-Afari, M.F.; Li, H.; Yu, Y.; Kong, L. Wearable insole pressure system for automated detection and classification of awkward working postures in construction workers. Autom. Constr. 2018, 96, 433–441. [Google Scholar] [CrossRef]
- Cordella, F.; Di Luzio, F.S.; Lauretti, C.; Draicchio, F.; Zollo, L. A biofeedback-based posture correction system for working environments. In Proceedings of the 2019 IEEE International Workshop on Metrology for Industry 4.0 and IoT, MetroInd 4.0 and IoT 2019, Naples, Italy, 4–6 June 2019; pp. 405–409. [Google Scholar]
- Eklund, J.; Forsman, M. Smart work clothes give better health—Through improved work technique, work organization and production technology. Adv. Comput. 2019, 820, 515–519. [Google Scholar] [CrossRef]
- Tlili, F.; Haddad, R.; Bouallegue, R.; Shubair, R. Design and architecture of smart belt for real time posture monitoring. Internet Things 2022, 17, 100472. [Google Scholar] [CrossRef]
- Poscia, A.; Moscato, U.; La Milia, D.I.; Milovanovic, S.; Stojanovic, J.; Borghini, A.; Collamati, A.; Ricciardi, W.; Magnavita, N. Workplace health promotion for older workers: A systematic literature review. BMC Health Serv. Res. 2016, 16, 415–428. [Google Scholar] [CrossRef] [PubMed]
- Simpson, L.; Maharaj, M.M.; Mobbs, R.J. The role of wearables in spinal posture analysis: A systematic review. BMC Musculoskelet. Disord. 2019, 20, 55. [Google Scholar] [CrossRef] [PubMed]
- Conforti, I.; Ilaria, M.; Zaccaria, D.P.; Eduardo, P. Measuring Biomechanical Risk in Lifting Load Tasks Machine-Learning Approach. Sensors 2020, 20, 1557. [Google Scholar] [CrossRef] [PubMed]
- Wilczyński, J.; Lipińska-Stańczak, M.; Wilczyński, I. Body Posture Defects and Body Composition in School-Age Children. Children 2020, 7, 204. [Google Scholar] [CrossRef] [PubMed]
- Adesida, Y.; Papi, E.; McGregor, A.H. Exploring the role of wearable technology in sport kinematics and kinetics: A systematic review. Sensors 2019, 19, 1597. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wei, Y.; Qiu, Y. Advanced Flexible Skin-Like Pressure and Strain Sensors for Human Health Monitoring. Micromachines 2021, 12, 695. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Pavic, A.; Goodwin, V.A. Wearable inertial sensors to measure gait and posture characteristic differences in older adult fallers and non-fallers: A scoping review. Gait Posture 2020, 76, 110–121. [Google Scholar] [CrossRef]
- de-la-Fuente-Robles, Y.-M.; Ricoy-Cano, A.-J.; Albin-Rodriguez, A.-P.; Luis Lopez-Ruiz, J.; Espinilla-Estevez, M. Past, Present and Future of Research on Wearable Technologies for Healthcare: A Bibliometric Analysis Using Scopus. Sensors 2022, 22, 8559. [Google Scholar] [CrossRef] [PubMed]
- Stefana, E.; Marciano, F.; Rossi, D.; Cocca, P.; Tomasoni, G. Wearable Devices for Ergonomics: A Systematic Literature Review. Sensors 2021, 21, 777. [Google Scholar] [CrossRef]
- Paloschi, D.; Bravi, M.; Schena, E.; Miccinilli, S.; Morrone, M.; Sterzi, S.; Saccomandi, P.; Massaroni, C. Validation and Assessment of a Posture Measurement System with Magneto-Inertial Measurement Units. Sensors 2021, 21, 6610. [Google Scholar] [CrossRef]
- Yoong, N.K.; Perring, J.; Mobbs, R.J. Commercial Postural Devices: A Review. Sensors 2019, 19, 5128. [Google Scholar] [CrossRef]
- Aryal, A.; Ghahramani, A.; Becerik-Gerber, B. Monitoring fatigue in construction workers using physiological measurements. Autom. Constr. 2017, 82, 154–165. [Google Scholar] [CrossRef]
- Schall, M.C.; Sesek, R.F.; Cavuoto, L.A. Barriers to the Adoption of Wearable Sensors in the Workplace: A Survey of Occupational Safety and Health Professionals. Hum. Factors 2018, 60, 351–362. [Google Scholar] [CrossRef]
- Buisseret, F.; Dierick, F.; Van der Perre, L. Wearable Sensors Applied in Movement Analysis. Sensors 2022, 22, 8239. [Google Scholar] [CrossRef]
- Clark, B.K.; Brakenridge, C.L.; Healy, G.N. The Importance of Research on Occupational Sedentary Behaviour and Activity Right Now. Int. J. Environ. Res. Public Health 2022, 19, 15816. [Google Scholar] [CrossRef]
- Chander, H.; Burch, R.F.; Talegaonkar, P.; Saucier, D.; Luczak, T.; Ball, J.E.; Turner, A.; Arachchige, S.N.K.K.; Carroll, W.; Smith, B.K.; et al. Wearable Stretch Sensors for Human Movement Monitoring and Fall Detection in Ergonomics. Int. J. Environ. Res. Public Health 2020, 17, 3554. [Google Scholar] [CrossRef]
- Papi, E.; Koh, W.S.; McGregor, A.H. Wearable technology for spine movement assessment: A systematic review. J. Biomech. 2017, 64, 186–197. [Google Scholar] [CrossRef]
- Carey, S.; Ross, J.M.; Balasubramaniam, R. Auditory, tactile, and multimodal noise reduce balance variability. Exp. Brain Res. 2023, 241, 1241–1249. [Google Scholar] [CrossRef]
- Lind, C.M.; Abtahi, F.; Forsman, M. Wearable Motion Capture Devices for the Prevention of Work-Related Musculoskeletal Disorders in Ergonomics-An Overview of Current Applications, Challenges, and Future Opportunities. Sensors 2023, 23, 4259. [Google Scholar] [CrossRef]
- Fani, S.; Ciotti, S.; Bianchi, M. Multi-Cue Haptic Guidance Through Wearables for Enhancing Human Ergonomics. IEEE Trans. Haptics 2022, 15, 115–120. [Google Scholar] [CrossRef]
- Wang, Q.; Markopoulos, P.; Yu, B.; Chen, W.; Timmermans, A. Interactive wearable systems for upper body rehabilitation: A systematic review. J. Neuroeng. Rehabil. 2017, 14, 17. [Google Scholar] [CrossRef]
- Lim, S.; Yang, X. Real-time vibrotactile feedback system for reducing trunk flexion exposure during construction tasks. Appl. Ergon. 2023, 110, 104019. [Google Scholar] [CrossRef]
- Svertoka, E.; Saafi, S.; Rusu-Casandra, A.; Burget, R.; Marghescu, I.; Hosek, J.; Ometov, A. Wearables for Industrial Work Safety: A Survey. Sensors 2021, 21, 3844. [Google Scholar] [CrossRef]
- Huang, X.; Xue, Y.; Ren, S.; Wang, F. Sensor-Based Wearable Systems for Monitoring Human Motion and Posture: A Review. Sensors 2023, 23, 9047. [Google Scholar] [CrossRef]
- Yang, M.; Liu, Y.; Yang, W.; Liu, J. Thread-Embedded-in-PDMS Wearable Strain Sensor for Real-Time Monitoring of Human Joint Motion. Micromachines 2023, 14, 2250. [Google Scholar] [CrossRef]
- Norasi, H.; Tetteh, E.; Money, S.R.; Davila, V.J.; Meltzer, A.J.; Morrow, M.M.; Fortune, E.; Mendes, B.C.; Hallbeck, M.S. Intraoperative posture and workload assessment in vascular surgery. Appl. Ergon. 2021, 92, 103344. [Google Scholar] [CrossRef]
- Owlia, M.; Kamachi, M.; Dutta, T. Reducing lumbar spine flexion using real-time biofeedback during patient handling tasks. Work 2020, 66, 41–51. [Google Scholar] [CrossRef]
- Kamachi, M.; Owlia, M.; Dutta, T. Evaluating a wearable biofeedback device for reducing end-range sagittal lumbar spine flexion among home caregivers. Appl. Ergon. 2021, 97, 103547. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Sole, G.; Abbott, J.H.; Milosavljevic, S. The effectiveness of a lumbopelvic monitor and feedback device to change postural behavior: A feasibility randomized controlled trial. J. Orthop. Sports Phys. Ther. 2014, 44, 702–711. [Google Scholar] [CrossRef]
- Thanathornwong, B.; Suebnukarn, S.; Songpaisan, Y.; Ouivirach, K. A system for predicting and preventing work-related musculoskeletal disorders among dentists. Comput. Methods Biomech. Biomed. Engin. 2014, 17, 177–185. [Google Scholar] [CrossRef]
- Thanathornwong, B.; Suebnukarn, S.; Ouivirach, K. A system for predicting musculoskeletal disorders among dental students. Int. J. Occup. Saf. Ergon. 2014, 20, 463–475. [Google Scholar] [CrossRef]
- Thanathornwong, B.; Suebnukarn, S. The Improvement of Dental Posture Using Personalized Biofeedback. Stud. Health Technol. Inform. 2015, 216, 756–760. [Google Scholar] [CrossRef]
- Zhao, W. Privacy-Aware Human Motion Tracking with Realtime Haptic Feedback. In Proceedings of the 2015 IEEE International Conference on Mobile Services, New York, NY, USA, 27 June–2 July 2015; pp. 446–453. [Google Scholar]
- Yan, X.; Li, H.; Li, A.R.; Zhang, H. Wearable IMU-based real-time motion warning system for construction workers’ musculoskeletal disorders prevention. Autom. Constr. 2017, 74, 2–11. [Google Scholar] [CrossRef]
- Doss, R.; Robathan, J.; Abdelmalek, D.; Holmes, M.W.R. Posture Coaching and Feedback during Patient Handling in a Student Nurse Population. IISE Trans. 2018, 6, 116–127. [Google Scholar] [CrossRef]
- Lins, C.; Fudickar, S.; Gerka, A.; Hein, A. A Wearable Vibrotactile Interface for Unfavorable Posture Awareness Warning. In Proceedings of the 4th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2018), Funchal, Portugal, 22–23 March 2018; pp. 178–183. [Google Scholar]
- Bootsman, R.; Markopoulos, P.; Qi, Q.; Wang, Q.; Timmermans, A.A.A. Wearable technology for posture monitoring at the workplace. Int. J. Hum. Comput. 2019, 132, 99–111. [Google Scholar] [CrossRef]
- Lind, C.M.; Yang, L.; Abtahi, F.; Hanson, L.; Lindecrantz, K.; Lu, K.; Forsman, M.; Eklund, J. Reducing postural load in order picking through a smart workwear system using real-time vibrotactile feedback. Appl. Ergon. 2020, 89, 103188. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Milosavljevic, S.; Terry, J.; Abbott, J.H. Effectiveness of a lumbopelvic monitor and feedback device to change postural behaviour: The ELF cluster randomised controlled trial. Occup. Environ. Med. 2020, 77, 462–469. [Google Scholar] [CrossRef]
- Lind, C.M.; De Clercq, B.; Forsman, M.; Grootaers, A.; Verbrugghe, M.; Van Dyck, L.; Yang, L. Effectiveness and usability of real-time vibrotactile feedback training to reduce postural exposure in real manual sorting work. Ergonomics 2023, 66, 198–216. [Google Scholar] [CrossRef]
- Nygaard, N.P.B.; Thomsen, G.F.; Rasmussen, J.; Skadhauge, L.R.; Gram, B. Workability in the Ageing Workforce-A Population-Based Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 12656. [Google Scholar] [CrossRef]
- Chan, L.Y.T.; Chua, C.S.; Chou, S.M.; Seah, R.Y.B.; Huang, Y.; Luo, Y.; Dacy, L.; Bin Abd Razak, H.R. Assessment of shoulder range of motion using a commercially available wearable sensor—A validation study. mHealth 2022, 8, 1–12. [Google Scholar] [CrossRef]
- Fan, X.; Lind, C.M.; Rhen, I.M.; Forsman, M. Effects of Sensor Types and Angular Velocity Computational Methods in Field Measurements of Occupational Upper Arm and Trunk Postures and Movements. Sensors 2021, 21, 5527. [Google Scholar] [CrossRef]
- Choi, B.; Hwang, S.; Lee, S.H. What drives construction workers’ acceptance of wearable technologies in the workplace?: Indoor localization and wearable health devices for occupational safety and health. Autom. Constr. 2017, 84, 31–41. [Google Scholar] [CrossRef]
- Donisi, L.; Cesarelli, G.; Pisani, N.; Ponsiglione, A.M.; Ricciardi, C.; Capodaglio, E. Wearable Sensors and Artificial Intelligence for Physical Ergonomics: A Systematic Review of Literature. Diagnostics 2022, 12, 3048. [Google Scholar] [CrossRef]
- Alberto, R.; Draicchio, F.; Varrecchia, T.; Silvetti, A.; Iavicoli, S. Wearable monitoring devices for biomechanical risk assessment at work: Current status and future challenges—A systematic review. Int. J. Environ. Res. Public Health 2018, 15, 2001. [Google Scholar] [CrossRef]
- Dufaug, A.; Barthod, C.; Goujon, L.; Marechal, L. New joint analysis of electromyography spectrum and amplitude-based methods towards real-time muscular fatigue evaluation during a simulated surgical procedure: A pilot analysis on the statistical significance. Med. Eng. Phys. 2020, 79, 1–9. [Google Scholar] [CrossRef]
- Chan, V.C.H.; Beaudette, S.M.; Smale, K.B.; Beange, K.H.E.; Graham, R.B. A subject-specific approach to detect fatigue-related changes in spine motion using wearable sensors. Sensors 2020, 20, 2646. [Google Scholar] [CrossRef]
- Brambilla, C.; Lavit Nicora, M.; Storm, F.; Reni, G.; Malosio, M.; Scano, A. Biomechanical Assessments of the Upper Limb for Determining Fatigue, Strain and Effort from the Laboratory to the Industrial Working Place: A Systematic Review. Bioengineering 2023, 10, 445. [Google Scholar] [CrossRef]
- Poitras, I.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.J.; Roy, J.S. Validity of wearable sensors at the shoulder joint: Combining wireless electromyography sensors and inertial measurement units to perform physical workplace assessments. Sensors 2019, 19, 1885. [Google Scholar] [CrossRef]
- Yang, L.; Grooten, W.J.A.; Forsman, M. An iPhone application for upper arm posture and movement measurements. Appl. Ergon. 2017, 65, 492–500. [Google Scholar] [CrossRef]
- Chen, L.; Fan, S.; Kumar, V.; Jia, Y. A Method of Human Activity Recognition in Transitional Period. Information 2020, 11, 416. [Google Scholar] [CrossRef]
- Wong, W.Y.; Wong, M.S. Trunk posture monitoring with inertial sensors. Eur. Spine J. 2008, 17, 743–753. [Google Scholar] [CrossRef]
- Rusek, W.; Baran, J.; Leszczak, J.; Adamczyk, M.; Weres, A.; Baran, R.; Inglot, G.; Pop, T. The Influence of Body Mass Composition on the Postural Characterization of School-Age Children and Adolescents. Biomed. Res. Int. 2018, 2018, 9459014. [Google Scholar] [CrossRef]
- Jacobs, J.V.; Hettinger, L.J.; Huang, Y.H.; Jeffries, S.; Lesch, M.F.; Simmons, L.A.; Verma, S.K.; Willetts, J.L. Employee acceptance of wearable technology in the workplace. Appl. Ergon. 2019, 78, 148–156. [Google Scholar] [CrossRef]
- Jacquier-Bret, J.; Gorce, P. Prevalence of Body Area Work-Related Musculoskeletal Disorders among Healthcare Professionals: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 841. [Google Scholar] [CrossRef]
- Lee, Y.C.; Hong, X.; Man, S.S. Prevalence and Associated Factors of Work-Related Musculoskeletal Disorders Symptoms among Construction Workers: A Cross-Sectional Study in South China. Int. J. Environ. Res. Public Health 2023, 20, 4653. [Google Scholar] [CrossRef]
- Lorenzini, M.; Kim, W.; De Momi, E.; Ajoudani, A. An Online Method to Detect and Locate an External Load on the Human Body with Applications in Ergonomics Assessment. Sensors 2020, 20, 4471. [Google Scholar] [CrossRef]
- Knight, J.F.; Baber, C. A tool to assess the comfort of wearable computers. Hum. Factors 2005, 47, 77–91. [Google Scholar] [CrossRef]
- Gioberto, G.; Dunne, L. Theory and characterization of a top-thread coverstitched stretch sensor. In Proceedings of the IEEE International Conference on Systems, Man and Cybernetics, Seoul, Republic of Korea, 14–17 October 2012; pp. 3275–3280. [Google Scholar]
- Sharma, A.K.; Vigdorchik, J.M.; Kolin, D.A.; Elbuluk, A.M.; Windsor, E.N.; Jerabek, S.A. Assessing Pelvic Tilt in Patients Undergoing Total Hip Arthroplasty Using Sensor Technology. Arthroplast. Today 2022, 13, 98–103. [Google Scholar] [CrossRef]
- Park, S.Y.; Yoo, W.G. Effect of EMG-based feedback on posture correction during computer operation. J. Occup. Health 2012, 54, 271–277. [Google Scholar] [CrossRef]
- Barone, V.J.; Yuen, M.C.; Kramer-Boniglio, R.; Sienko, K.H. Sensory garments with vibrotactile feedback for monitoring and informing seated posture. In Proceedings of the RoboSoft 2019—2019 IEEE International Conference on Soft Robotics, Seoul, Republic of Korea, 14–18 April 2019; pp. 391–397. [Google Scholar]
- Lind, C.M.; Diaz-Olivares, J.A.; Lindecrantz, K.; Eklund, J. A Wearable Sensor System for Physical Ergonomics Interventions Using Haptic Feedback. Sensors 2020, 20, 6010. [Google Scholar] [CrossRef]
- Alnaser, M.Z.; Almaqsied, A.M.; Alshatti, S.A. Risk factors for work-related musculoskeletal disorders of dentists in Kuwait and the impact on health and economic status. Work 2021, 68, 213–221. [Google Scholar] [CrossRef]
- Holzgreve, F.; Fraeulin, L.; Betz, W.; Erbe, C.; Wanke, E.M.; Brüggmann, D.; Nienhaus, A.; Groneberg, D.A.; Maurer-grubinger, C.; Ohlendorf, D. A RULA-Based Comparison of the Ergonomic Risk of Typical Working Procedures for Dentists and Dental Assistants of General Dentistry, Endodontology, Oral and Maxillofacial Surgery, and Orthodontics. Sensors 2022, 22, 805. [Google Scholar] [CrossRef]
- Kawtharani, A.A.; Chemeisani, A.; Salman, F.; Haj Younes, A.; Msheik, A. Neck and Musculoskeletal Pain Among Dentists: A Review of the Literature. Cureus 2023, 15, 1–11. [Google Scholar] [CrossRef]
- Blume, K.S.; Holzgreve, F.; Fraeulin, L.; Erbe, C.; Betz, W.; Wanke, E.M.; Brueggmann, D.; Nienhaus, A.; Maurer-Grubinger, C.; Groneberg, D.A.; et al. Ergonomic Risk Assessment of Dental Students-RULA Applied to Objective Kinematic Data. Int. J. Environ. Res. Public Health 2021, 18, 10550. [Google Scholar] [CrossRef]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Risi, A.; Prati, C. Musculoskeletal Disorders among Italian Dentists and Dental Hygienists. Int. J. Environ. Res. Public Health 2021, 18, 2705. [Google Scholar] [CrossRef]
- Sezer, B.; Kartal, S.; Sıddıkoğlu, D.; Kargül, B. Association between work-related musculoskeletal symptoms and quality of life among dental students: A cross-sectional study. BMC Musculoskelet. Disord. 2022, 23, 41. [Google Scholar] [CrossRef]
- Antwi-Afari, M.F.; Li, H.; Chan, A.H.S.; Seo, J.; Anwer, S.; Mi, H.-Y.; Wu, Z.; Wong, A.Y.L. A science mapping-based review of work-related musculoskeletal disorders among construction workers. J. Safety Res. 2023, 85, 114–128. [Google Scholar] [CrossRef]
- Oppici, L.; Grütters, K.; Garofolini, A.; Rosenkranz, R.; Narciss, S. Deliberate Practice and Motor Learning Principles to Underpin the Design of Training Interventions for Improving Lifting Movement in the Occupational Sector: A Perspective and a Pilot Study on the Role of Augmented Feedback. Front. Sports Act Living 2021, 3, 746142. [Google Scholar] [CrossRef] [PubMed]
- Harvey, R.H.; Peper, E.; Mason, L.; Joy, M. Effect of Posture Feedback Training on Health. Appl. Psychophysiol. Biofeedback 2020, 45, 59–65. [Google Scholar] [CrossRef]
- Wang, Q.; Chen, W.; Timmermans, A.A.A.; Karachristos, C.; Martens, J.B.; Markopoulos, P. Smart Rehabilitation Garment for posture monitoring. In Proceedings of the 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 5736–5739. [Google Scholar]
- Kuo, Y.L.; Huang, K.Y.; Kao, C.Y.; Tsai, Y.J. Sitting posture during prolonged computer typing with and without a wearable biofeedback sensor. Int. J. Environ. Res. Public Health 2021, 18, 5430. [Google Scholar] [CrossRef]
- Boocock, M.; Naudé, Y.; Taylor, S.; Kilby, J.; Mawston, G. Influencing lumbar posture through real-time biofeedback and its effects on the kinematics and kinetics of a repetitive lifting task. Gait Posture 2019, 73, 93–100. [Google Scholar] [CrossRef]





| Criteria | |
|---|---|
| Population | Active adults assessed in the context of work tasks |
| Concept | Use of wearables to monitor and correct work-related postural changes through sensory biofeedback |
| Context | Workstation |
| Database | Search Strategies |
|---|---|
| PubMed® | (posture OR “postural assessment” OR “body posture” OR “Postural Analysis” OR “posture monitoring” OR “postural correction”) AND (“Wearable Devices” OR Wearables OR “wearable systems” OR “commercial wearable” OR textiles OR sensor* OR “inertial sensor” OR “sensor system” OR “sensor network” OR “smart sensor” OR “pressure sensor” OR “plantar sensor” OR IMU OR gyroscope OR magnetometer OR electromyography OR *feedback) AND (Workplace OR “work-related musculoskeletal disorder” OR “real-time measurement” OR Industry OR “work-station” OR “real-context”) NOT (stress OR exoskeleton OR “Physical activity” OR Physiological) |
| Web of Science® (WOS) | AK = ((wearable OR postural wearable OR commercial wearable OR textiles OR sensor*) AND (workplace OR workstation OR office WORK OR work-related musculoskeletal disorder) AND postur*) OR AB = ((wearable OR postural wearable OR commercial wearable OR textiles OR sensor*) AND (workplace OR workstation OR office WORK OR work-related musculoskeletal disorder) AND postur*) OR AB = (Wearable AND sensor* AND workplace) OR TI = (Wearable AND sensor* AND workplace) AB= ((posture OR “postural assessment” OR “body posture” OR “Postural Analysis” OR “posture monitoring” OR “postural correction”) AND (‘Wearable Electronic Devices’ OR ‘Wearables’ OR “wearable systems” OR “postural wearable” OR “ commercial wearable” OR textiles OR sensors OR sensor OR “inertial sensor” OR “ sensor system” OR “sensor network” OR “smart sensor” OR “pressure sensor” OR “plantar sensor” OR IMU OR gyroscope OR magnetometer OR electromyography OR feedback) AND (Workplace OR “work-related musculoskeletal disorder” OR “real-time measurement” OR Industry OR “work-station” OR “real- context”)) |
| Scopus® | Posture AND Wearable AND Workplace |
| Google Scholar® | (“Postural Analysis” OR “Postural Correction”) AND (Wearable* OR *feedback) AND Workplace |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Figueira, V.; Silva, S.; Costa, I.; Campos, B.; Salgado, J.; Pinho, L.; Freitas, M.; Carvalho, P.; Marques, J.; Pinho, F. Wearables for Monitoring and Postural Feedback in the Work Context: A Scoping Review. Sensors 2024, 24, 1341. https://doi.org/10.3390/s24041341
Figueira V, Silva S, Costa I, Campos B, Salgado J, Pinho L, Freitas M, Carvalho P, Marques J, Pinho F. Wearables for Monitoring and Postural Feedback in the Work Context: A Scoping Review. Sensors. 2024; 24(4):1341. https://doi.org/10.3390/s24041341
Chicago/Turabian StyleFigueira, Vânia, Sandra Silva, Inês Costa, Bruna Campos, João Salgado, Liliana Pinho, Marta Freitas, Paulo Carvalho, João Marques, and Francisco Pinho. 2024. "Wearables for Monitoring and Postural Feedback in the Work Context: A Scoping Review" Sensors 24, no. 4: 1341. https://doi.org/10.3390/s24041341
APA StyleFigueira, V., Silva, S., Costa, I., Campos, B., Salgado, J., Pinho, L., Freitas, M., Carvalho, P., Marques, J., & Pinho, F. (2024). Wearables for Monitoring and Postural Feedback in the Work Context: A Scoping Review. Sensors, 24(4), 1341. https://doi.org/10.3390/s24041341







