Effects of Vibroacoustic Stimulation on Psychological, Physiological, and Cognitive Stress
Abstract
1. Introduction
State of the Art
2. Materials and Methods
2.1. Apparatus
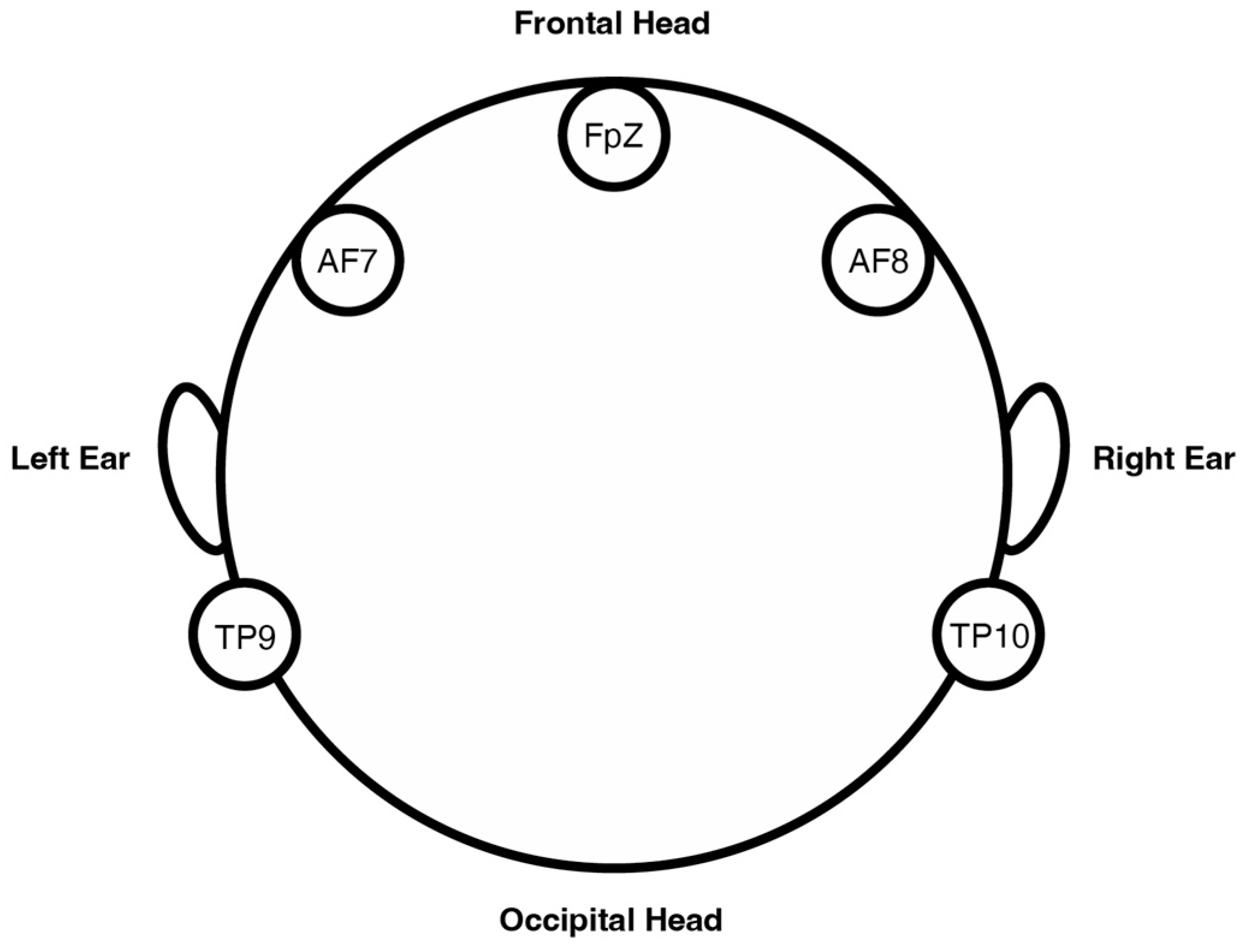
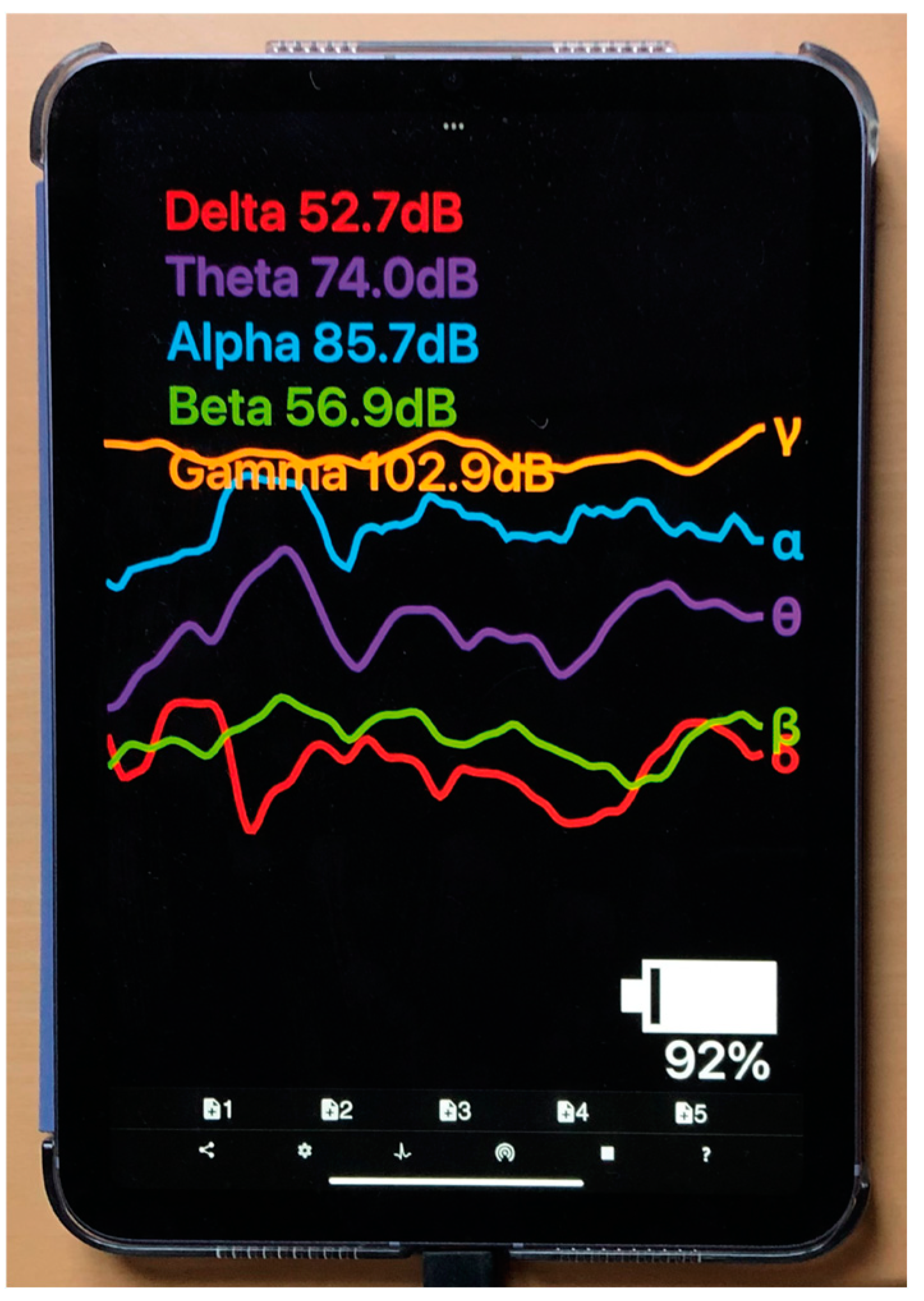
2.1.1. EEG Apparatus: Muse S (Gen 2)
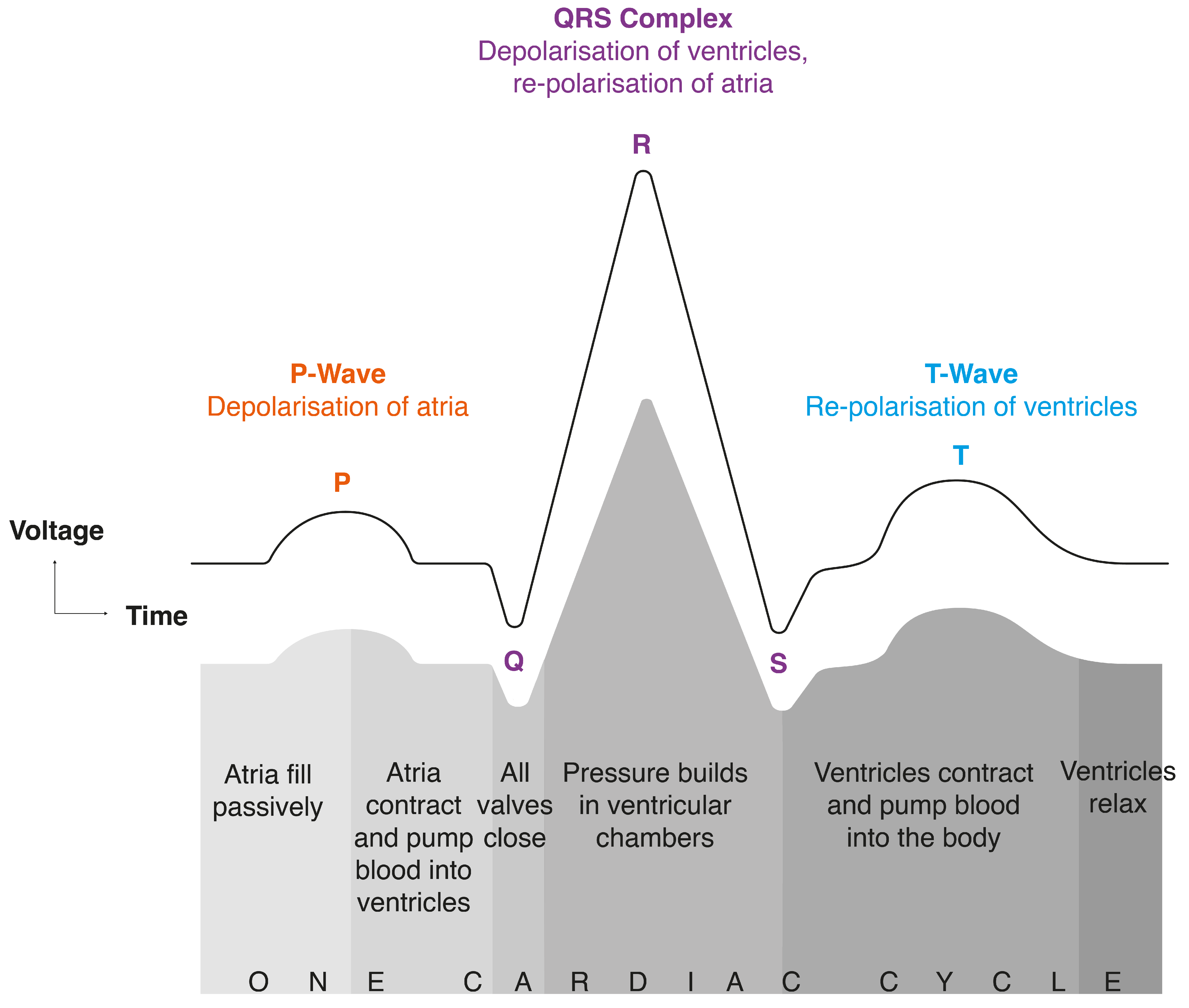
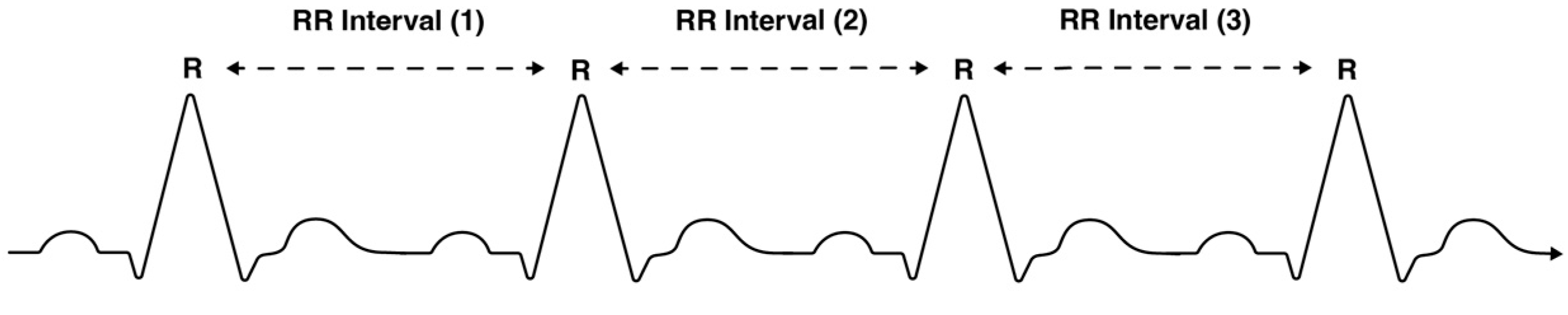
2.1.2. ECG Apparatus: Polar H10 Heart Rate Monitor
2.1.3. Questionnaire: Perceived Stress Scale PSS-10
2.1.4. Vibroacoustic Apparatus: Device and Audio
2.2. Method
2.2.1. Recruitment
2.2.2. Experimental Procedure
2.2.3. Processing of Biosignals
2.2.4. Additional Explanations of the EEG Measures
2.2.5. Statistical Analysis
3. Results
3.1. Cognitive Stress (EEG)
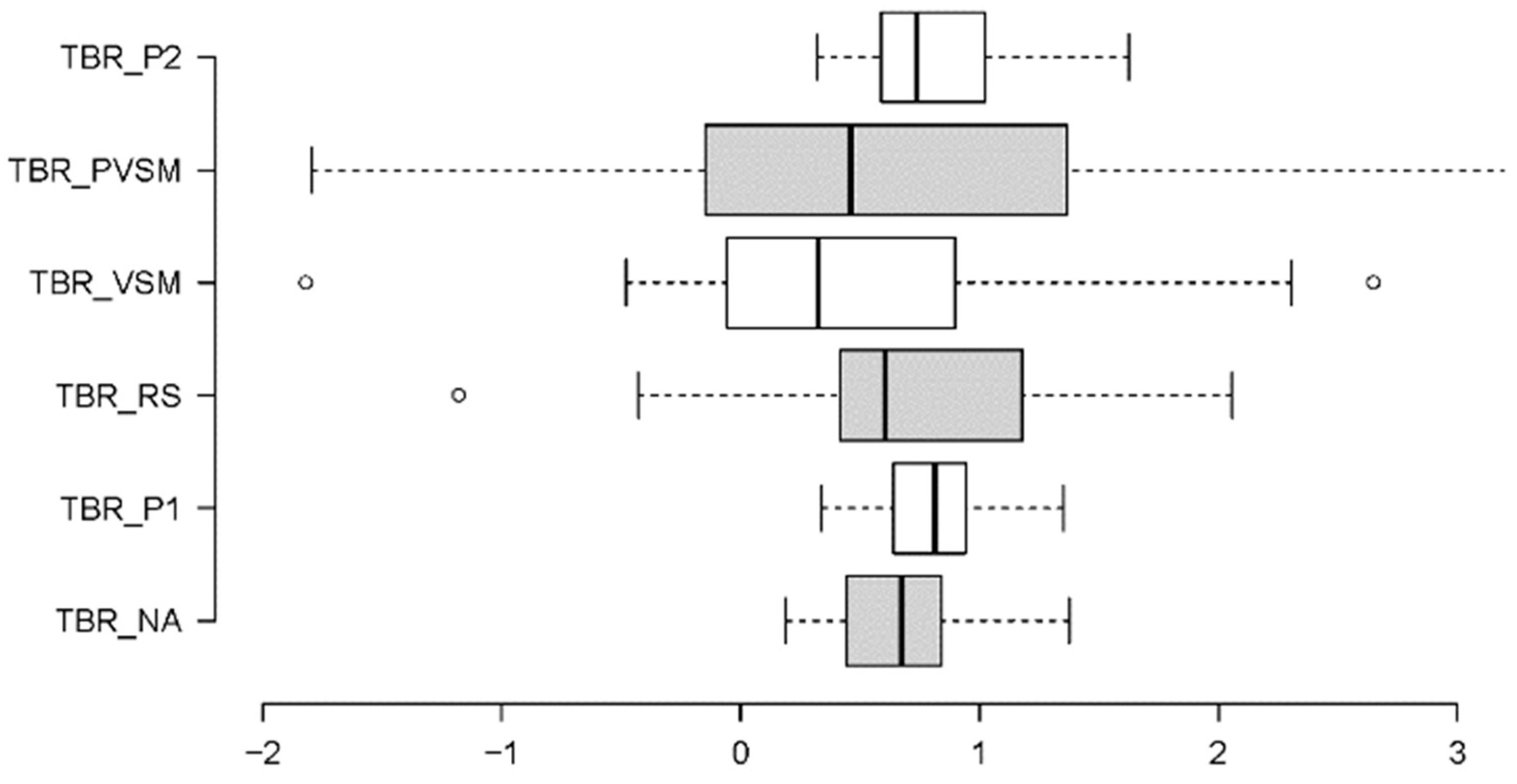
3.1.1. Theta/Beta Ratio (TBR)—Concentration and Focus
3.1.2. Beta/Alpha Ratio (BAR)—Arousal
3.1.3. Frontal/Alpha Asymmetry (FAA)—Well-Being
3.1.4. Qualitative Data: First-Person Verbal Accounts
3.2. Physiological Stress (ECG)
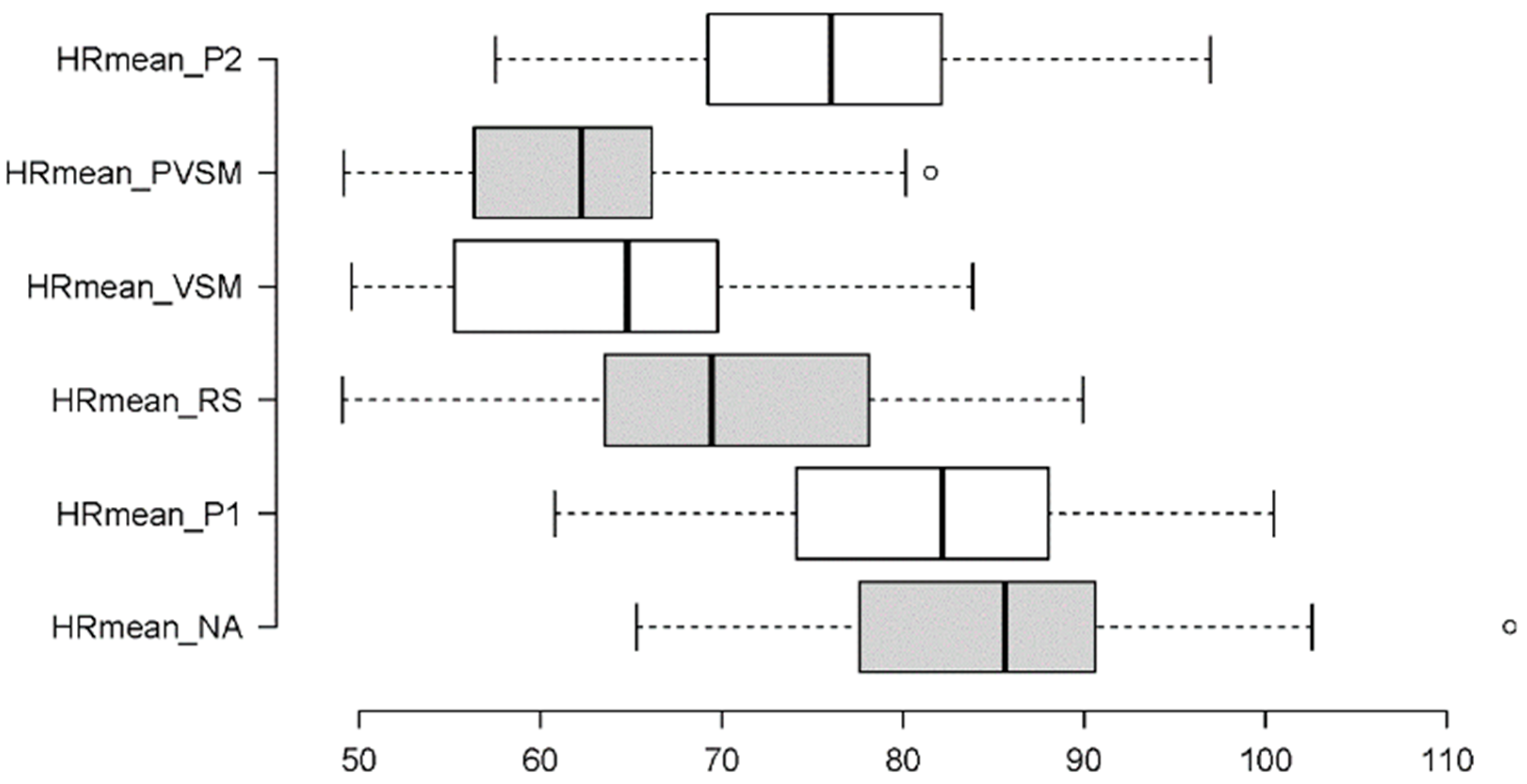
3.2.1. Mean HR
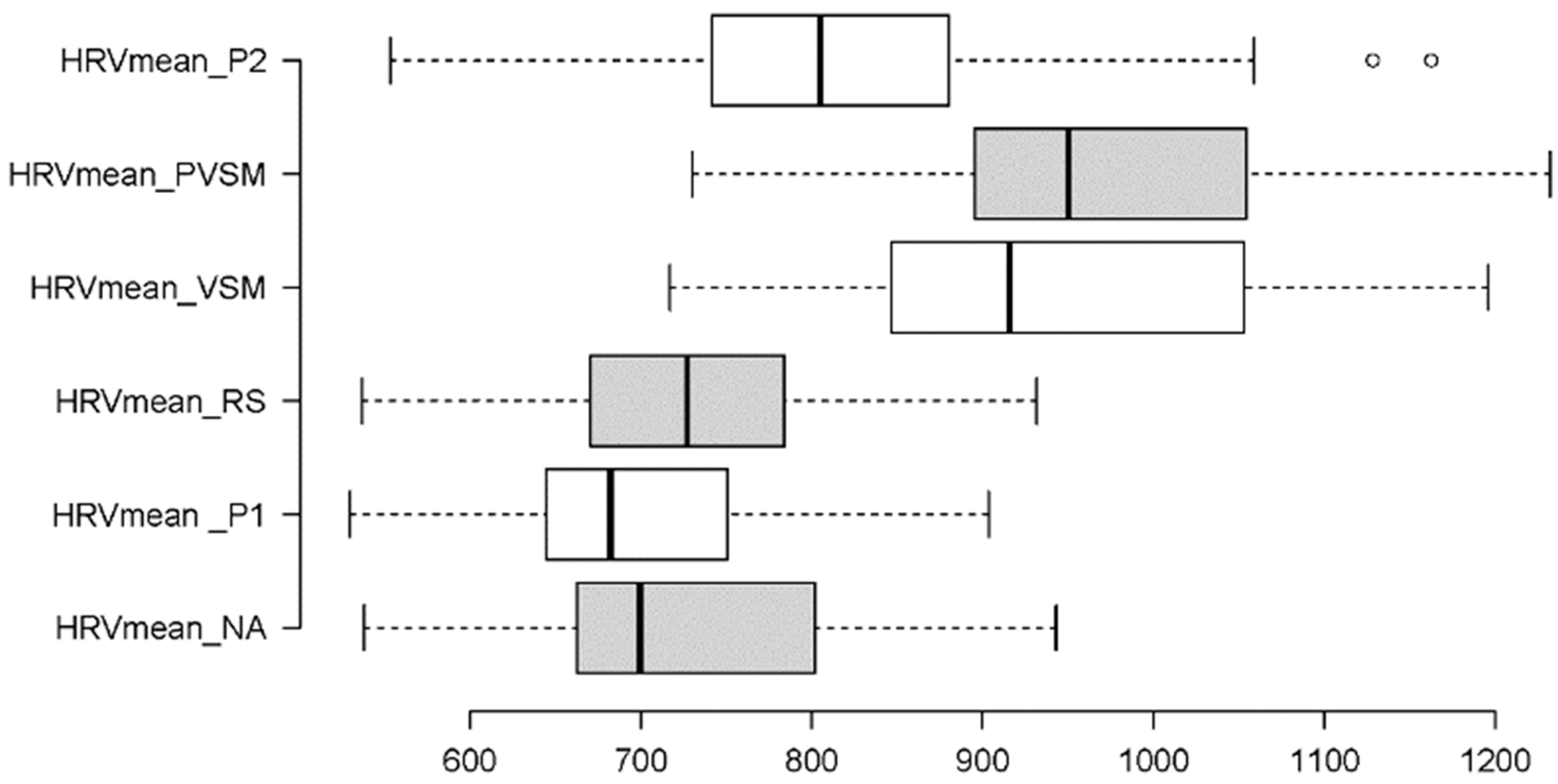
3.2.2. Mean HRV
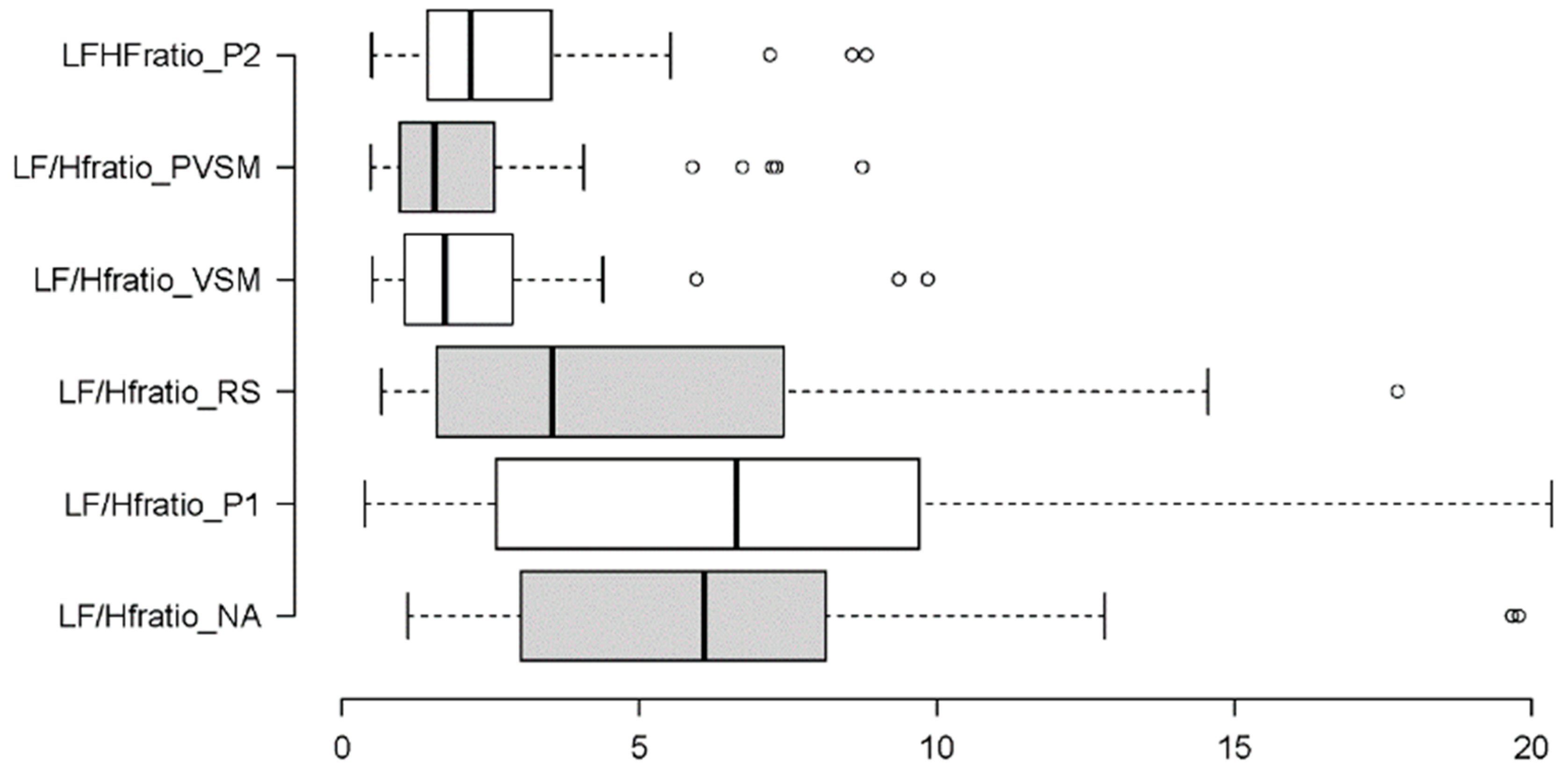
3.2.3. Sympathovagal Balance: LF/HF Ratio
3.2.4. Sympathetic Activity: SDNN and LF
3.2.5. Parasympathetic Activity: RMSSD and HF
3.3. Psychological Stress
4. Discussion
4.1. Discussion of Cognitive Stress Effects
4.2. Discussion of Physiological Stress Effects
4.3. Discussion of Psychological Stress Effects
4.4. Relevance and Implications
4.5. Limitations and Outlook
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nochaiwong, S.; Ruengorn, C.; Thavorn, K.; Hutton, B.; Awiphan, R.; Phosuya, C.; Ruanta, Y.; Wongpakaran, N.; Wongpakaran, T. Global Prevalence of Mental Health Issues among the General Population During the Coronavirus Disease-2019 Pandemic: A Systematic Review and Meta-analysis. Sci. Rep. 2021, 11, 10173. [Google Scholar] [CrossRef] [PubMed]
- Gale, N. The Sociology of Traditional, Complementary and Alternative Medicine. Sociol. Compass 2014, 8, 805–822. [Google Scholar] [CrossRef]
- Zou, L.; Sasaki, J.E.; Wei, G.X.; Huang, T.; Yeung, A.S.; Neto, O.B.; Chen, K.W.; Hui, S.S. Effects of Mind-Body Exercises (Tai Chi/Yoga) on Heart Rate Variability Parameters and Perceived Stress: A Systematic Review with Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2018, 7, 404. [Google Scholar] [CrossRef]
- Danylova, T.V.; Shmarhun, V.M.; Vertel, A.V.; Matyushko, B.K.; Bondarenko, A.F.; Kychkyruk, T.; Petersen, J. Effects of the eastern mind-body practices on mental health during the COVID-19 pandemic: When east meets west. Wiad. Lek. 2021, 74, 2850–2855. [Google Scholar] [CrossRef] [PubMed]
- Gangadhar, B.; Porandla, K. Yoga and Mental Health Services. Indian J. Psychiatry 2015, 57, 338–340. [Google Scholar] [CrossRef] [PubMed]
- Singphow, C.; Purohit, S.; Tekur, P.; Bista, S.; Panigrahy, S.N.; Raghuram, N.; Nagendra, H.R. Effect of Yoga on Stress, Anxiety, Depression, and Spinal Mobility in Computer Users with Chronic Low Back Pain. Int. J. Yoga 2022, 15, 114–121. [Google Scholar] [CrossRef]
- Chopra, D.; Stern, E.; Bushell, W.C.; Castle, R.D. Yoga and Pain: A Mind-Body Complex System. Front. Pain Res. 2023, 4, 1075866. [Google Scholar] [CrossRef]
- Feneberg, A.C.; Nater, U.M. An Ecological Momentary Music Intervention for the Reduction of Acute Stress in Daily Life: A Mixed Methods Feasibility Study. Front. Psychol. 2022, 13, 927705. [Google Scholar] [CrossRef]
- Feneberg, A.C.; Stijovic, A.; Forbes, P.A.G.; Lamm, C.; Piperno, G.; Pronizius, E.; Silani, G.; Nater, U.M. Perceptions of Stress and Mood Associated with Listening to Music in Daily Life during the COVID-19 Lockdown. JAMA Netw. Open 2023, 6, e2250382. [Google Scholar] [CrossRef]
- Valosek, L.; Wendt, S.; Link, J.; Abrams, A.; Hipps, J.; Grant, J.; Nidich, R.; Loiselle, M.; Nidich, S. Meditation Effective in Reducing Teacher Burnout and Improving Resilience: A Randomized Controlled Study. Front. Educ. 2021, 6, 627923. [Google Scholar] [CrossRef]
- Breit, S.; Kupferberg, A.; Rogler, G.; Hasler, G. Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Front. Psychiatry 2018, 9, 44. [Google Scholar] [CrossRef] [PubMed]
- Gerritsen, R.J.S.; Band, G.P.H. Breath of Life: The Respiratory Vagal Stimulation Model of Contemplative Activity. Front. Hum. Neurosci. 2018, 12, 397. [Google Scholar] [CrossRef] [PubMed]
- Kromenacker, B.W.; Sanova, A.A.; Marcus, F.I.; Allen, J.J.B.; Lane, R.D. Vagal Mediation of Low-Frequency Heart Rate Variability during Slow Yogic Breathing. Psychosom. Med. 2018, 80, 581–587. [Google Scholar] [CrossRef]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Front. Psychol. 2017, 8, 213. [Google Scholar] [CrossRef]
- Akinrodoye, M.A.; Lui, F. Neuroanatomy, Somatic Nervous System. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK556027/ (accessed on 2 May 2024).
- Waxenbaum, J.A.; Reddy, V.; Varacallo, M. Anatomy, Autonomic Nervous System. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. Available online: https://www.ncbi.nlm.nih.gov/books/NBK539845/ (accessed on 2 May 2024).
- Mitchell, L.B. Premature Atrial Beats. Available online: https://www.msdmanuals.com/pt-br/casa/dist%C3%BArbios-do-cora%C3%A7%C3%A3o-e-dos-vasos-sangu%C3%ADneos/arritmias-card%C3%ADacas/batimentos-atriais-prematuros (accessed on 25 June 2024).
- Tiwari, R.; Kumar, R.; Malik, S.; Raj, T.; Kumar, P. Analysis of Heart Rate Variability and Implication of Different Factors on Heart Rate Variability. Curr. Cardiol. Rev. 2021, 17, e160721189770. [Google Scholar] [CrossRef] [PubMed]
- Chesky, K.S.; Michel, D.E. The Music Vibration Table (MVT): Developing a Technology and Conceptual Model for Pain Relief. Music Ther. Perspect. 1991, 9, 32–38. [Google Scholar] [CrossRef]
- Naghdi, L.; Ahonen, H.; Macario, P.; Bartel, L. The Effect of Low-Frequency Sound Stimulation on Patients with Fibromyalgia: A Clinical Study. Pain Res. Manag. 2015, 20, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Rüütel, E.; Vinkel, I.; Eelmäe, P. The Effects of Short-Term Vibroacoustic Treatment on Spasticity and Perceived Health Conditions of Patients with Spinal Cord and Brain Injuries. Music Med. 2017, 9, 202–208. [Google Scholar] [CrossRef]
- Campbell, E.; Burger, B.; Ala-Ruona, E. A Single-Case, Mixed Methods Study Exploring the Role of Music Listening in Vibroacoustic Treatment. Voices World Forum Music Ther. 2019, 19, 27. [Google Scholar] [CrossRef][Green Version]
- Campbell, E.A.; Hynynen, J.; Burger, B.; Vainionpää, A.; Ala-Ruona, E. Vibroacoustic treatment to improve functioning and ability to work: A multidisciplinary approach to chronic pain rehabilitation. Disabil. Rehabil. 2021, 43, 2055–2070. [Google Scholar] [CrossRef]
- Hallihan, C.; Siegle, G.J. Effect of Vibroacoustic Stimulation on Athletes Recovering from Exercise. Eur. J. Appl. Physiol. 2022, 122, 2427–2435. [Google Scholar] [CrossRef] [PubMed]
- Rüütel, E.; Ratnik, M.; Tamm, E.; Zilensk, H. The Experience of Vibroacoustic Therapy in the Therapeutic Intervention of Adolescent Girls. Nord. J. Music Ther. 2004, 13, 33–46. [Google Scholar] [CrossRef]
- Braun Janzen, T.; Al Shirawi, M.I.; Rotzinger, S.; Kennedy, S.H.; Bartel, L. A Pilot Study Investigating the Effect of Music-Based Intervention on Depression and Anhedonia. Front. Psychol. 2019, 10, 1038. [Google Scholar] [CrossRef]
- Karkkainen, M.; Mitsui, J. The Effects of Sound Based Vibration Treatment on the Human Mind and Body the Physioacoustic Method. J. Int. Soc. Life Inf. Sci. 2006, 24, 155–164. [Google Scholar] [CrossRef]
- Kantor, J.; Campbell, E.A.; Kantorová, L.; Marečková, J.; Regec, V.; Karasová, K.; Sedláčková, D.; Klugar, M. Exploring Vibroacoustic Therapy in Adults Experiencing Pain: A Scoping Review. BMJ Open 2022, 12, e046591. [Google Scholar] [CrossRef]
- Campbell, E.; Hynynen, J.; Ala-Ruona, E. Vibroacoustic Treatment for Chronic Pain and Mood Disorders in a Specialised Healthcare Setting. Music Med. 2017, 9, 187–197. [Google Scholar] [CrossRef]
- Campbell, E.A.; Hynynen, J.; Burger, B.; Ala-Ruona, E. Exploring the Use of Vibroacoustic Treatment for Managing Chronic Pain and Comorbid Mood Disorders: A Mixed Methods Study. Nord. J. Music Ther. 2019, 28, 291–314. [Google Scholar] [CrossRef]
- Lehikoinen, P. The physioacoustic method. In Music Vibration and Health; Wigram, T., Dileo, C., Eds.; Jeffrey Books: Cherry Hill, NJ, USA, 1997; pp. 206–216. [Google Scholar]
- Mosabbir, A.; Almeida, Q.J.; Ahonen, H. The Effects of Long-Term 40-Hz Physioacoustic Vibrations on Motor Impairments in Parkinson’s Disease: A Double-Blinded Randomized Control Trial. Healthcare 2020, 8, 113. [Google Scholar] [CrossRef]
- Patrick, G. The Effects of Vibroacoustic Music on Symptom Reduction. IEEE Eng. Med. Biol. Mag. 1999, 18, 97–100. [Google Scholar] [CrossRef]
- Skille, O. VibroAcoustic Therapy. Music Ther. 1989, 8, 61–77. [Google Scholar] [CrossRef][Green Version]
- Kantor, J.; Vilímek, Z.; Vítězník, M.; Smrčka, P.; Campbell, E.A.; Bucharová, M.; Grohmannová, J.; Špinarová, G.; Janíčková, K.; Du, J.; et al. Effect of Low Frequency Sound Vibration on Acute Stress Response in University Students-Pilot Randomized Controlled Trial. Front. Psychol. 2022, 13, 980756. [Google Scholar] [CrossRef]
- Vilímek, Z.; Kantor, J.; Krejčí, J.; Janečka, Z.; Jedličková, Z.; Nekardová, A.; Botek, M.; Bucharová, M.; Campbell, E.A. The Effect of Low Frequency Sound on Heart Rate Variability and Subjective Perception: A Randomized Crossover Study. Healthcare 2022, 10, 1024. [Google Scholar] [CrossRef] [PubMed]
- Delmastro, F.; Martino, F.D.; Dolciotti, C. Physiological Impact of Vibro-Acoustic Therapy on Stress and Emotions through Wearable Sensors. In Proceedings of the 2018 IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops), Athens, Greece, 19–23 March 2018; pp. 621–626. [Google Scholar]
- Brodsky, W. Post-Exposure Effects of Music-Generated Vibration and Whole-Body Acoustic Stimulation among Symphony Orchestra Musicians. Psychol. Music 2000, 28, 98–115. [Google Scholar] [CrossRef]
- Rüütel, E. The Psychophysiological Effects of Music and Vibroacoustic Stimulation. Nord. J. Music Ther. 2002, 11, 16–26. [Google Scholar] [CrossRef]
- Koike, Y.; Hoshitani, M.; Tabata, Y.; Seki, K.; Nishimura, R.; Kano, Y. Effects of Vibroacoustic Therapy on Elderly Nursing Home Residents with Depression. J. Phys. Ther. Sci. 2012, 24, 291–294. [Google Scholar] [CrossRef]
- Cavallo, F.; Rovini, E.; Dolciotti, C.; Radi, L.; Ragione, R.D.; Bongioanni, P.; Fiorini, L. Physiological response to Vibro-Acoustic stimulation in healthy subjects: A preliminary study. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 5921–5924. [Google Scholar]
- Kantor, J.; Vilímek, Z.; Du, J.; Campbell, E. Effects of Vibroacoustic Therapy on Physiological Responses Related to Stress and its Measurements in Adults a Scoping Review Protocol. Zdr. Listy 2022, 10, 77. [Google Scholar]
- VibroAcoustics Bass Module. Available online: https://vibroacoustics.dk/product (accessed on 1 May 2024).
- Fernandez, M. Acoustics and Universal Movement. In Music Vibration and Health; Wigram, T., Dileo, C., Eds.; Jeffrey Books: Cherry Hill, NJ, USA, 1997; pp. 11–26. [Google Scholar]
- Ala-Ruona, E.; Punkanen, M.; Campbell, E. Vibroacoustic Therapy: Conception, Development, and Future Directions. Musiikkiterapia 2015, 30, 48–71. [Google Scholar]
- Attar, E.T. Review of electroencephalography signals approaches for mental stress assessment. Neurosciences 2022, 27, 209–215. [Google Scholar] [CrossRef]
- Balzarotti, S.; Biassoni, F.; Colombo, B.; Ciceri, M.R. Cardiac vagal control as a marker of emotion regulation in healthy adults: A review. Biol. Psychol. 2017, 130, 54–66. [Google Scholar] [CrossRef]
- Pavlov, V.A.; Tracey, K.J. The Vagus Nerve and the Inflammatory Reflex—Linking Immunity and Metabolism. Nat. Rev. Endocrinol. 2012, 8, 743–754. [Google Scholar] [CrossRef]
- Schaffarczyk, M.; Rogers, B.; Reer, R.; Gronwald, T. Validity of the Polar H10 Sensor for Heart Rate Variability Analysis during Resting State and Incremental Exercise in Recreational Men and Women. Sensors 2022, 22, 6536. [Google Scholar] [CrossRef]
- Gilgen-Ammann, R.; Schweizer, T.; Wyss, T. RR interval signal quality of a heart rate monitor and an ECG Holter at rest and during exercise. Eur. J. Appl. Physiol. 2019, 119, 1525–1532. [Google Scholar] [CrossRef] [PubMed]
- Speer, K.E.; Semple, S.; Naumovski, N.; McKune, A.J. Measuring Heart Rate Variability Using Commercially Available Devices in Healthy Children: A Validity and Reliability Study. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 390–404. [Google Scholar] [CrossRef]
- Wilfong, A.; Schultz, R.J. Vagus Nerve Stimulation for Treatment of Epilepsy in Rett Syndrome. Dev. Med. Child. Neurol. 2006, 48, 683–686. [Google Scholar] [CrossRef]
- Panebianco, M.; Rigby, A.; Marson, A.G. Vagus Nerve Stimulation for Focal Seizures. Cochrane Database Syst. Rev. 2022, 7, Cd002896. [Google Scholar] [CrossRef]
- Elger, G.; Hoppe, C.; Falkai, P.; Rush, A.J.; Elger, C.E. Vagus Nerve Stimulation is Associated with Mood Improvements in Epilepsy Patients. Epilepsy Res. 2000, 42, 203–210. [Google Scholar] [CrossRef]
- Rush, A.J.; George, M.S.; Sackeim, H.A.; Marangell, L.B.; Husain, M.M.; Giller, C.; Nahas, Z.; Haines, S.; Simpson, R.K., Jr.; Goodman, R. Vagus Nerve Stimulation (VNS) for Treatment-Resistant Depressions: A Multicenter Study. Biol. Psychiatry 2000, 47, 276–286. [Google Scholar] [CrossRef]
- Sobocki, J.; Fourtanier, G.; Estany, J.; Otal, P. Does Vagal Nerve Stimulation Affect Body Composition and Metabolism? Experimental Study of a New Potential Technique in Bariatric Surgery. Surgery 2006, 139, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Silberstein, S.D.; Yuan, H.; Najib, U.; Ailani, J.; de Morais, A.L.; Mathew, P.G.; Liebler, E.; Tassorelli, C.; Diener, H.C. Non-Invasive Vagus Nerve Stimulation for Primary Headache: A Clinical Update. Cephalalgia 2020, 40, 1370–1384. [Google Scholar] [CrossRef] [PubMed]
- Sigurdardóttir, G.A.; Nielsen, P.M.; Rønager, J.; Wang, A.G. A Pilot Study on High Amplitude Low Frequency—Music Impulse Stimulation as an Add-On Treatment for Depression. Brain Behav. 2019, 9, e01399. [Google Scholar] [CrossRef]
- Peng, D.; Tong, W.; Collins, D.J.; Ibbotson, M.R.; Prawer, S.; Stamp, M. Mechanisms and Applications of Neuromodulation Using Surface Acoustic Waves—A Mini-Review. Front. Neurosci. 2021, 15, 629056. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Herman, K.; Ciechanowski, L.; Przegalińska, A. Emotional well-being in urban wilderness: Assessing states of calmness and alertness in informal green spaces (IGSs) with muse—Portable EEG headband. Sustainability 2021, 13, 2212. [Google Scholar] [CrossRef]
- Mind Monitor Technical Manual. Available online: https://mind-monitor.com/Technical_Manual.php (accessed on 5 April 2023).
- Garcia-Moreno, F.M.; Bermudez-Edo, M.; Garrido, J.L.; Rodríguez-Fórtiz, M.J. Reducing Response Time in Motor Imagery Using A Headband and Deep Learning. Sensors 2020, 20, 6730. [Google Scholar] [CrossRef]
- Van Son, D.; de Rover, M.; De Blasio, F.M.; van der Does, W.; Barry, R.J.; Putman, P. Electroencephalography theta/beta ratio covaries with mind wandering and functional connectivity in the executive control network. Ann. N. Y. Acad. Sci. 2019, 1452, 52–64. [Google Scholar] [CrossRef]
- McMahan, T.; Parberry, I.; Parsons, T.D. Evaluating Player Task Engagement and Arousal Using Electroencephalography. Procedia Manuf. 2015, 3, 2303–2310. [Google Scholar] [CrossRef]
- Wutzl, B.; Leibnitz, K.; Kominami, D.; Ohsita, Y.; Kaihotsu, M.; Murata, M. Analysis of the Correlation between Frontal Alpha Asymmetry of Electroencephalography and Short-Term Subjective Well-Being Changes. Sensors 2023, 23, 7006. [Google Scholar] [CrossRef]
- Heart Rate Monitor. Available online: https://play.google.com/store/apps/details?id=com.bmi.hr_monitor&hl=en&gl=US (accessed on 20 May 2024).
- Lee, E.H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Baik, S.H.; Fox, R.S.; Mills, S.D.; Roesch, S.C.; Sadler, G.R.; Klonoff, E.A.; Malcarne, V.L. Reliability and validity of the Perceived Stress Scale-10 in Hispanic Americans with English or Spanish language preference. J. Health Psychol. 2019, 24, 628–639. [Google Scholar] [CrossRef]
- Klein, E.M.; Brähler, E.; Dreier, M.; Reinecke, L.; Müller, K.W.; Schmutzer, G.; Wölfling, K.; Beutel, M.E. The German version of the Perceived Stress Scale—Psychometric characteristics in a representative German community sample. BMC Psychiatry 2016, 16, 159. [Google Scholar] [CrossRef]
- Nordin, M.; Nordin, S. Psychometric evaluation and normative data of the Swedish version of the 10-item perceived stress scale. Scand. J. Psychol. 2013, 54, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Eskildsen, A.; Dalgaard, V.L.; Nielsen, K.J.; Andersen, J.H.; Zachariae, R.; Olsen, L.R.; Jørgensen, A.; Christiansen, D.H. Cross-cultural adaptation and validation of the Danish consensus version of the 10-item Perceived Stress Scale. Scand. J. Work. Environ. Health 2015, 41, 486–490. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, R.S.; Simons, R.F.; Losito, B.D.; Fiorito, E.; Miles, M.A.; Zelson, M. Stress recovery during exposure to natural and urban environments. J. Environ. Psychol. 1991, 11, 201–230. [Google Scholar] [CrossRef]
- Ratcliffe, E.; Gatersleben, B.; Sowden, P.T. Bird Sounds and their Contributions to Perceived Attention Restoration and Stress Recovery. J. Environ. Psychol. 2013, 36, 221–228. [Google Scholar] [CrossRef]
- Buxton, R.T.; Pearson, A.L.; Allou, C.; Fristrup, K.; Wittemyer, G. A Synthesis of Health Benefits of Natural Sounds and their Distribution in National Parks. Proc. Natl. Acad. Sci. USA 2021, 118, e2013097118. [Google Scholar] [CrossRef]
- Ratcliffe, E. Sound and Soundscape in Restorative Natural Environments: A Narrative Literature Review. Front. Psychol. 2021, 12, 570563. [Google Scholar] [CrossRef]
- Van Praag, C.D.G.; Garfinkel, S.N.; Sparasci, O.; Mees, A.; Philippides, A.O.; Ware, M.; Ottaviani, C.; Critchley, H.D. Mind-Wandering and Alterations to Default Mode Network Connectivity when Listening to Naturalistic Versus Artificial Sounds. Sci. Rep. 2017, 7, 45273. [Google Scholar] [CrossRef]
- Nozaradan, S. Exploring how musical rhythm entrains brain activity with electroencephalogram frequency-tagging. Philos. Trans. R. Soc. B Biol. Sci. 2014, 369, 20130393. [Google Scholar] [CrossRef]
- Thaut, M.H.; McIntosh, G.C.; Hoemberg, V. Neurobiological Foundations of Neurologic Music Therapy: Rhythmic Entrainment and the Motor System. Front. Psychol. 2014, 5, 1185. [Google Scholar] [CrossRef]
- Engel, A.; Hoefle, S.; Monteiro, M.C.; Moll, J.; Keller, P.E. Neural Correlates of Listening to Varying Synchrony between Beats in Samba Percussion and Relations to Feeling the Groove. Front. Neurosci. 2022, 16, 779964. [Google Scholar] [CrossRef]
- Stupacher, J.; Matthews, T.E.; Pando-Naude, V.; Foster Vander Elst, O.; Vuust, P. The Sweet Spot between Predictability and Surprise: Musical Groove in Brain, Body, and Social Interactions. Front. Psychol. 2022, 13, 906190. [Google Scholar] [CrossRef] [PubMed]
- Bartel, L.R.; Chen, R.; Alain, C.; Ross, B. Vibroacoustic Stimulation and Brain Oscillation: From Basic Research to Clinical Application. Music Med. 2017, 9, 153. [Google Scholar] [CrossRef]
- Fries, P. Neuronal Gamma-Band Synchronization as a Fundamental Process in Cortical Computation. Annu. Rev. Neurosci. 2009, 32, 209–224. [Google Scholar] [CrossRef] [PubMed]
- Jirakittayakorn, N.; Wongsawat, Y. Brain Responses to 40-Hz Binaural Beat and Effects on Emotion and Memory. Int. J. Psychophysiol. 2017, 120, 96–107. [Google Scholar] [CrossRef]
- Fooks, C.; Niebuhr, O. Assessing Vibroacoustic Sound Massage Through The Biosignal of Human Speech: Evidence of Improved Wellbeing. In Proceedings of the IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP), Seoul, Republic of Korea, 14–19 April 2024; pp. 11401–11405. [Google Scholar]
- Davidson, R.J.; Schaffer, C.E.; Saron, C. Effects of lateralized presentations of faces on self-reports of emotion and EEG asymmetry in depressed and non-depressed subjects. Psychophysiology 1985, 22, 353–364. [Google Scholar] [CrossRef]
- Stewart, J.L.; Bismark, A.W.; Towers, D.N.; Coan, J.A.; Allen, J.J.B. Resting frontal EEG asymmetry as an endophenotype for depression risk: Sex-specific patterns of frontal brain asymmetry. J. Abnorm. Psychol. 2010, 119, 502–512. [Google Scholar] [CrossRef]
- Alyan, E.; Saad, N.M.; Kamel, N.; Yusoff, M.Z.; Zakariya, M.A.; Rahman, M.A.; Guillet, C.; Merienne, F. Frontal Electroencephalogram Alpha Asymmetry during Mental Stress Related to Workplace Noise. Sensors 2021, 21, 1968. [Google Scholar] [CrossRef]
- Pivik, R.T.; Harman, K. A comparison of slow and fast EEG components in the assessment of mental workload. Int. J. Psychophysiol. 1995, 20, 135–146. [Google Scholar]
- Kislov, A.; Gorin, A.; Konstantinovsky, N.; Klyuchnikov, V.; Bazanov, B.; Klucharev, V. Central EEG beta/alpha ratio predicts the population-wide efficiency of advertisements. Brain Sci. 2022, 13, 57. [Google Scholar] [CrossRef]
- Swartwood, J.N.; Swartwood, M.O.; Lubar, J.F.; Timmermann, D.L. EEG differences in ADHD-combined type during baseline and cognitive tasks. Pediatr. Neurol. 2003, 28, 199–204. [Google Scholar] [CrossRef]
- Köpruner, V.; Pfurtscheller, G.; Auer, L.M. Quantitative EEG in normals and in patients with cerebral ischemia. Progress. Brain Res. 1984, 62, 29–50. [Google Scholar]
- van Son, D.; De Blasio, F.M.; Fogarty, J.S.; Angelidis, A.; Barry, R.J.; Putman, P. Frontal EEG theta/beta ratio during mind wandering episodes. Biol. Psychol. 2019, 140, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Van Der Vinne, N.; Vollebregt, M.A.; Van Putten, M.J.; Arns, M. Frontal alpha asymmetry as a diagnostic marker in depression: Fact or fiction? A meta-analysis. Neuroimage Clin. 2017, 16, 79–87. [Google Scholar] [CrossRef]
- Agelink, M.W.; Malessa, R.; Baumann, B.; Majewski, T.; Akila, F.; Zeit, T.; Ziegler, D. Standardized tests of heart rate variability: Normal ranges obtained from 309 healthy humans, and effects of age, gender, and heart rate. Clin. Auton. Res. 2001, 11, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Wen, T.Y.; Aris, S.M. Electroencephalogram (EEG) stress analysis on alpha/beta ratio and theta/beta ratio. Indones. J. Electr. Eng. Comput. Sci. 2020, 17, 175–182. [Google Scholar] [CrossRef]
- Wang, H.-M.; Huang, S.-C. SDNN/RMSSD as a Surrogate for LF/HF: A Revised Investigation. Model. Simul. Eng. 2012, 2012, 931943. [Google Scholar] [CrossRef]
- Shaffer, F.; Ginsberg, J.P. An Overview of Heart Rate Variability Metrics and Norms. Front. Public Health 2017, 5, 258. [Google Scholar] [CrossRef]
- Emanuel, R.; Adams, J.; Baker, K.; Daufin, E.K.; Ellington, C.; Fitts, E.; Himsel, J.; Holladay, L.; Okeowo, D. How College Students Spend Their Time Communicating. Int. J. List. 2008, 22, 13–28. [Google Scholar] [CrossRef]
- Sandler, H.; Tamm, S.; Fendel, U.; Rose, M.; Klapp, B.F.; Bösel, R. Positive Emotional Experience: Induced by Vibroacoustic Stimulation Using a Body Monochord in Patients with Psychosomatic Disorders: Is Associated with an Increase in EEG-Theta and a Decrease in EEG-Alpha Power. Brain Topogr. 2016, 29, 524–538. [Google Scholar] [CrossRef]
- Bourdillon, N.; Yazdani, S.; Vesin, J.M.; Schmitt, L.; Millet, G.P. RMSSD Is More Sensitive to Artifacts Than Frequency-Domain Parameters: Implication in Athletes’ Monitoring. J. Sports Sci. Med. 2022, 21, 260–266. [Google Scholar] [CrossRef]
- Massaro, S.; Pecchia, L. Heart Rate Variability (HRV) Analysis: A Methodology for Organizational Neuroscience. Organ. Res. Methods 2019, 22, 354–393. [Google Scholar] [CrossRef]
- Fooks, C.; Niebuhr, O. Assessing Effects of Vibroacoustic Stimulation Compared to a Guided Mindfulness Meditation Using the Biosignal of Human Speech. 2025; manuscript in preparation; to be submitted. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Sauer, S.; Walach, H.; Offenbächer, M.; Lynch, S.; Kohls, N. Measuring Mindfulness: A Rasch Analysis of the Freiburg Mindfulness Inventory. Religions 2011, 2, 693–706. [Google Scholar] [CrossRef]
- Kaske, E.A.; Chen, C.S.; Meyer, C.; Yang, F.; Ebitz, B.; Grissom, N.; Kapoor, A.; Darrow, D.P.; Herman, A.B. Prolonged Physiological Stress Is Associated with a Lower Rate of Exploratory Learning That Is Compounded by Depression. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2023, 8, 703–711. [Google Scholar] [CrossRef]
- Whiston, A.; Igou, E.R.; Fortune, D.G.; Semkovska, M. Longitudinal interactions between residual symptoms and physiological stress in the remitted symptom network structure of depression. Acta Psychol. 2023, 241, 104078. [Google Scholar] [CrossRef] [PubMed]
- Pate, B.S.; Smiley, C.E.; Harrington, E.N.; Bielicki, B.H.; Davis, J.M.; Reagan, L.P.; Grillo, C.A.; Wood, S.K. Voluntary wheel running as a promising strategy to promote autonomic resilience to social stress in females: Vagal tone lies at the heart of the matter. Auton. Neurosci. 2024, 253, 103175. [Google Scholar] [CrossRef]
- Satyjeet, F.; Naz, S.; Kumar, V.; Aung, N.H.; Bansari, K.; Irfan, S.; Rizwan, A. Psychological Stress as a Risk Factor for Cardiovascular Disease: A Case-Control Study. Cureus 2020, 12, e10757. [Google Scholar] [CrossRef]
- Kumar, R.; Rizvi, M.R.; Saraswat, S. Obesity and Stress: A Contingent Paralysis. Int. J. Prev. Med. 2022, 13, 95. [Google Scholar] [CrossRef] [PubMed]
- Dakanalis, A.; Mentzelou, M.; Papadopoulou, S.K.; Papandreou, D.; Spanoudaki, M.; Vasios, G.K.; Pavlidou, E.; Mantzorou, M.; Giaginis, C. The Association of Emotional Eating with Overweight/Obesity, Depression, Anxiety/Stress, and Dietary Patterns: A Review of the Current Clinical Evidence. Nutrients 2023, 15, 1173. [Google Scholar] [CrossRef]
- Moore, J.P. Interoceptive signals from the heart and coronary circulation in health and disease. Auton. Neurosci. 2024, 253, 103180. [Google Scholar] [CrossRef]
- Zhao, W.; Van Someren, E.J.W.; Xu, Z.; Ren, Z.; Tang, L.; Li, C.; Lei, X. Identifying the insomnia-related psychological issues associated with hyperarousal: A network perspective. Int. J. Psychophysiol. 2024, 195, 112276. [Google Scholar] [CrossRef]
- Beffara, B.; Bret, A.G.; Vermeulen, N.; Mermillod, M. Resting high frequency heart rate variability selectively predicts cooperative behavior. Physiol. Behav. 2016, 164, 417–428. [Google Scholar] [CrossRef]
- Pinna, T.; Edwards, D.J. A Systematic Review of Associations between Interoception, Vagal Tone, and Emotional Regulation: Potential Applications for Mental Health, Wellbeing, Psychological Flexibility, and Chronic Conditions. Front. Psychol. 2020, 11, 1792. [Google Scholar] [CrossRef]
- Lemay, V.; Hoolahan, J.; Buchanan, A. Impact of a Yoga and Meditation Intervention on Students’ Stress and Anxiety Levels. Am. J. Pharm. Educ. 2019, 83, 7001. [Google Scholar] [CrossRef]
- Kirk, U.; Axelsen, J.L. Heart rate variability is enhanced during mindfulness practice: A randomized controlled trial involving a 10-day online-based mindfulness intervention. PLoS ONE 2020, 15, e0243488. [Google Scholar] [CrossRef]
- Panchal, S.; Irani, F.; Trivedi, G.Y. Impact of Himalayan Singing Bowls Meditation Session on Mood and Heart Rate Variability. Int. J. Psychother. Pract. Res. 2020, 1, 20–29. [Google Scholar] [CrossRef]
- Goldsby, T.L.; Goldsby, M.E.; McWalters, M.; Mills, P.J. Effects of Singing Bowl Sound Meditation on Mood, Tension, and Well-being: An Observational Study. J. Evid.-Based Complement. Altern. Med. 2017, 22, 401–406. [Google Scholar] [CrossRef]
- Trivedi, G.Y.; Saboo, B. A Comparative Study of the Impact of Himalayan Singing Bowls and Supine Silence on Stress Index and Heart Rate Variability. J. Behav. Ther. Ment. Health 2019, 2, 40–50. [Google Scholar] [CrossRef]
- Brewer, J.A.; Worhunsky, P.D.; Gray, J.R.; Tang, Y.Y.; Weber, J.; Kober, H. Meditation experience is associated with differences in default mode network activity and connectivity. Proc. Natl. Acad. Sci. USA 2011, 108, 20254–20259. [Google Scholar] [CrossRef]
- Matko, K.; Sedlmeier, P.; Bringmann, H.C. Differential Effects of Ethical Education, Physical Hatha Yoga, and Mantra Meditation on Well-Being and Stress in Healthy Participants—An Experimental Single-Case Study. Front. Psychol. 2021, 12, 672301. [Google Scholar] [CrossRef]
- Goldsby, T.L.; Goldsby, M.E. Eastern Integrative Medicine and Ancient Sound Healing Treatments for Stress: Recent Research Advances. Integr. Med. 2020, 19, 24–30. [Google Scholar]
- Touch the Sound. Available online: https://vibroacoustics.dk/ (accessed on 31 July 2024).
- Zimmerman, D.W. Two separate effects of variance heterogeneity on the validity and power of significance tests of location. Stat. Methodol. 2006, 3, 351–374. [Google Scholar] [CrossRef]
- Pashler, H. Dual-task interference in simple tasks: Data and theory. Psychol. Bull. 1994, 116, 220–244. [Google Scholar] [CrossRef] [PubMed]
















| Stage | Duration (Minutes) | Eyes | Posture | Activity | Purpose |
|---|---|---|---|---|---|
| Stage 1 Normal activity (NA) | 5 | Open | Sat, chair. | Study introduction. | Neutralise elevated heart rate. |
| Stage 2 Prosody 1 (P1) | 5 | Open | Sat, VSM module. | Reading speech passage. | Speech prosody analysis. (not discussed). |
| Stage 3 Rest State (RS) | 2 | Closed | Supine position, VSM module. | No activity required. | Control for basal heart rate, physiological stress, and cognitive stress. |
| Stage 4 VSM stimulation (VSM) | 45 | Closed | Supine position, VSM module. | Vibroacoustic Sound Massage and vibrotactile soundscape. | Independent variable. |
| Stage 5 Post-VSM (PVSM) | 5 | Closed | Supine position, VSM module. | No activity required. | Durational measure for VSM effects. |
| Stage 6 Prosody 2 (P2) | 5 | Open | Sat, VSM module. | Reading speech passage. | Speech prosody analysis. (not discussed). |
| Theta/Beta Ratio (TBR)—Concentration and Focus | Beta/Alpha Ratio (BAR)—Arousal and Relaxation | Frontal Alpha Asymmetry (FAA)—Well-Being |
|---|---|---|
| “I craved rhythm, interesting how rhythm doesn’t come through aurally, but physically through vibrations, body craves it, then gets it” | “Not awake but not sleeping, in-between” | “Cathartic” |
| “Could really match my breath work” | “Hyperactive in my head, rested in my body” | “Really relaxing” |
| “Not thinking about anything, zone into how much my bodies feeling” | “Disconnected from my body” | “Extremely empowering” |
| “Zoning into sounds themselves” | ”Felt like flying translated into your body” | “Very pleasant” |
| “Sometimes my thoughts were somewhere else, going in and out of zones” | “After the vibrations it feels numb in a good way, you can’t feel the borders of your body” | “Felt familiar, reminded me of home” |
| “Mind wondering but still aware of a lot of things” | “It felt liberating” | “I feel super calm and open” |
| “Pulled down again by thought” | “Complete serenity” | “Clear mind-body connection” |
| “Distracted me from (ADHD) medication, thinking ‘what is happening with my body?’” | “Body felt super relaxed and calm” | “100% enjoyable” |
| “There were phases when I was really relaxed, couldn’t think about anything, then all of a sudden really aware” | “Feeling of wanting to transcend, feeling my whole—a unity between my mind and body” | “My tension and stress feels released” |
| “Once in a while came back to focusing on what’s going on, the music, vibrations” | “Takes away the racing mind” | “Sounds were very calming, especially the birds” |
| “Totally immersive” | “Feel like you’re floating” | “Nice waves sounds, all ambient relaxing sounds” |
| “Felt super creative” | “No idea what kind of state I was in” | “Felt like a weighted blanket—safe and comfortable” |
| “Saw shapes, forms and colours that followed the vibrations in music” | “Vibrations going through the body” | “The vibration resonated with my body deeply” |
| “I saw colours that made sense with the sounds” | “The stronger the vibration the more relaxed I was, I couldn’t think” | “Feel physically something in my body taken out of me—I feel very light” |
| “Don’t know where my head went, felt I was tripping” | “The more vibration, the less aware I was” | “A yummy space—feels like a good place—like you’re being mothered somehow” |
| “Felt like a psychedelic trip” | “Lost track of time” | “Felt like being in my mother’s womb—very safe” |
| “I felt medicated or drugged in some way” | “Seeing the sound waves going through my body in dancing waves” | “Delightful—reminded me of being a child” |
| “Blurred lines between otherness and myself” | ||
| “Felt I was letting go of thoughts, allowing the experience and sound to come over me lead to deep relaxation” | ||
| “Stimulated—really relaxing but intense at the same time” |
| Main Effect of | Test Statistics | p | Effect Size | Sig. Multiple Comp. Tests | Test Statistics | p | Effect Size |
|---|---|---|---|---|---|---|---|
| SDNN | F [5,160] = 7.267 | <0.001 | ηp2 = 0.164 | VSM vs. NA | t[37] = 2.062 | 0.046 | d = 36.78 |
| VSM vs. P1 | t[37] = 2.075 | 0.046 | d = 42.04 | ||||
| VSM vs. P2 | t[37] = −2.266 | 0.030 | d = 51.84 | ||||
| NA vs. PVSM | t[37] = 3.746 | 0.001 | d = 8.26 | ||||
| NA vs. P2 | t[37] = 3.463 | 0.001 | d = 7.81 | ||||
| P1 vs. RS | t[37] = 1.987 | 0.050 | d = 7.50 | ||||
| P1 vs. PVSM | t[37] = 4.459 | <0.001 | d = 7.09 | ||||
| P1 vs. P2 | t[37] = 3.855 | <0.001 | d = 7.18 | ||||
| RS vs. P2 | t[37] = 2.777 | 0.009 | d = 4.61 | ||||
| LF | χ2[5] = 21.038 | <0.001 | W = 0.11 | VSM vs. NA | W = 4.108 | <0.001 | r = 0.67 |
| VSM vs. P1 | W = 2.269 | 0.023 | r = 0.39 | ||||
| VSM vs. RS | W = 2.453 | 0.014 | r = 0.40 | ||||
| VSM vs. P2 | W = −3.004 | 0.003 | r = 0.49 | ||||
| PVSM vs. NA | W = 3.066 | 0.002 | r = 0.50 | ||||
| PVSM vs. P2 | W = −1.962 | 0.050 | r = 0.32 | ||||
| Main Effect | Test Statistics | p | Effect Size | Sig. Multiple Comp. Tests | Test Statistics | p | Effect Size |
|---|---|---|---|---|---|---|---|
| RMSSD | χ2[5] = 44.180 | <0.001 | W = 0.24 | VSM vs. NA | W = 3.250 | <0.001 | r = 0.53 |
| VSM vs. P1 | W = 3.740 | 0.023 | r = 0.61 | ||||
| VSM vs. RS | W = 2.453 | 0.014 | r = 0.40 | ||||
| NA vs. PVSM | W = 4.108 | <0.001 | r = 0.67 | ||||
| NA vs. P2 | W = 4.599 | <0.001 | r = 0.67 | ||||
| P1 vs. PVSM | W = 4.599 | <0.001 | r = 0.75 | ||||
| P1 vs. P2 | W = 4.108 | <0.001 | r = 0.75 | ||||
| RS vs. PVSM | W = −3.311 | <0.001 | r = 0.54 | ||||
| RS vs. P2 | W = −3.311 | <0.001 | r = 0.54 | ||||
| HF | χ2[5] = 37.263 | <0.001 | W = 0.20 | VSM vs. P1 | W = 3.740 | <0.001 | r = 0.61 |
| VSM vs. RS | W = 2.207 | 0.027 | r = 0.36 | ||||
| NA vs. PVSM | W = −2.942 | 0.003 | r = 0.48 | ||||
| NA vs. P2 | W = −2.820 | 0.005 | r = 0.46 | ||||
| P1 vs. PVSM | W = −4.660 | <0.001 | r = 0.76 | ||||
| P1 vs. P2 | W = −4.782 | <0.001 | r = 0.78 | ||||
| RS vs. PVSM | W = −3.250 | 0.002 | r = 0.53 | ||||
| RS vs. P2 | W = −3.127 | 0.001 | r = 0.51 | ||||
| Measure | TBR | BAR | FAA | HR Mean | HRV Mean | LF/HF Ratio | SDNN | LF | RMSSD | HF |
|---|---|---|---|---|---|---|---|---|---|---|
| Rho [36] | 0.02 | 0.13 | −0.19 | 0.07 | −0.04 | −0.07 | −0.34 * | −0.32 * | −0.17 | −0.20 |
| p | 0.89 | 0.44 | 0.24 | 0.65 | 0.79 | 0.66 | 0.03 | 0.05 | 0.31 | 0.23 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fooks, C.; Niebuhr, O. Effects of Vibroacoustic Stimulation on Psychological, Physiological, and Cognitive Stress. Sensors 2024, 24, 5924. https://doi.org/10.3390/s24185924
Fooks C, Niebuhr O. Effects of Vibroacoustic Stimulation on Psychological, Physiological, and Cognitive Stress. Sensors. 2024; 24(18):5924. https://doi.org/10.3390/s24185924
Chicago/Turabian StyleFooks, Charlotte, and Oliver Niebuhr. 2024. "Effects of Vibroacoustic Stimulation on Psychological, Physiological, and Cognitive Stress" Sensors 24, no. 18: 5924. https://doi.org/10.3390/s24185924
APA StyleFooks, C., & Niebuhr, O. (2024). Effects of Vibroacoustic Stimulation on Psychological, Physiological, and Cognitive Stress. Sensors, 24(18), 5924. https://doi.org/10.3390/s24185924








