Influence of Impaired Upper Extremity Motor Function on Static Balance in People with Chronic Stroke
Abstract
1. Introduction
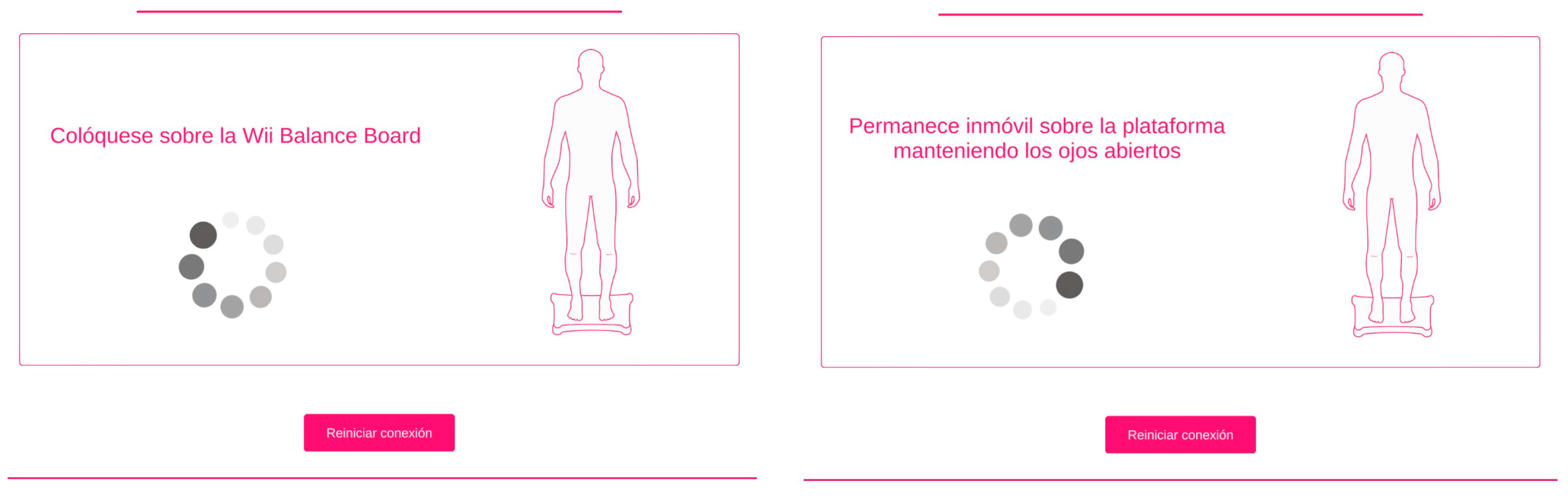
2. Materials and Methods
2.1. Study Design
2.2. Sample Size Estimation
2.3. Procedure
2.4. Statistical Analysis
3. Results
3.1. Correlation between mCTSIB and FMA-UE
3.2. Multiple Linear Regression to Assess the Influence of FMA-UE on Balance Parameters
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Quigley, P.A. Redesigned Fall and Injury Management of Patients with Stroke | Stroke Redesigned Fall and Injury Management of Patients with Stroke Emerging Evidence for Stroke Fall Prevention Strategies. Stroke 2016, 47, 92–94. [Google Scholar] [CrossRef]
- Horak, F.B. Postural orientation and equilibrium: What do we need to know about neural control of balance to prevent falls? Age Ageing 2006, 35 (Suppl. 2), 7–11. [Google Scholar] [CrossRef]
- Forbes, P.A.; Chen, A.; Blouin, J.S. Sensorimotor control of standing balance. In Handbook of Clinical Neurology; Elsevier B.V.: Amsterdam, The Netherlands, 2018; Volume 159, pp. 61–83. [Google Scholar] [CrossRef]
- Takakusaki, K. Functional neuroanatomy for posture and gait control. J. Mov. Disord. 2017, 10, 1–17. [Google Scholar] [CrossRef]
- De Oliveira, C.B.; De Medeiros, Í.R.T.; Frota, N.A.F.; Greters, M.E.; Conforto, A.B. Balance control in hemiparetic stroke patients: Main tools for evaluation. J. Rehabil. Res. Dev. 2008, 45, 1215–1226. [Google Scholar] [CrossRef]
- Paillard, T.; Noé, F. Techniques and Methods for Testing the Postural Function in Healthy and Pathological Subjects. BioMed Res. Int. 2015, 2015, 891390. [Google Scholar] [CrossRef]
- Visser, J.E.; Carpenter, M.G.; van der Kooij, H.; Bloem, B.R. The clinical utility of posturography. Clin. Neurophysiol. 2008, 119, 2424–2436. [Google Scholar] [CrossRef]
- Kuramatsu, Y.; Yamamoto, Y.; Izumi, S.I. Sensorimotor Strategies in Individuals with Poststroke Hemiparesis When Standing Up without Vision. Mot. Control 2020, 24, 150–167. [Google Scholar] [CrossRef]
- Roerdink, M.; Geurts, A.C.H.; De Haart, M.; Beek, P.J. On the relative contribution of the paretic leg to the control of posture after stroke. Neurorehabilit. Neural Repair. 2009, 23, 267–274. [Google Scholar] [CrossRef]
- Marigold, D.S.; Eng, J.J. The relationship of asymmetric weight-bearing with postural sway and visual reliance in stroke. Gait Posture 2006, 23, 249–255. [Google Scholar] [CrossRef] [PubMed]
- Rougier, P.R.; Pérennou, D. Upright standing after stroke: How loading-unloading mechanism participates to the postural stabilization. Hum. Mov. Sci. 2019, 64, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Kilby, M.C.; Molenaar, P.C.M.; Newell, K.M. Models of postural control: Shared variance in joint and COM motions. PLoS ONE 2015, 10, e0126379. [Google Scholar] [CrossRef]
- Thijs, L.; Voets, E.; Denissen, S.; Mehrholz, J.; Elsner, B.; Lemmens, R.; Verheyden, G.S. Trunk training following stroke. Cochrane Database Syst. Rev. 2023, 2023, CD013712. [Google Scholar] [CrossRef]
- Reddy, R.S.; Gular, K.; Dixit, S.; Kandakurti, P.K.; Tedla, J.S.; Gautam, A.P.; Sangadala, D.R. Impact of Constraint-Induced Movement Therapy (CIMT) on Functional Ambulation in Stroke Patients—A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 12809. [Google Scholar] [CrossRef]
- Ustinova, K.I.; Goussev, V.M.; Balasubramaniam, R.; Levin, M.F. Disruption of Coordination between Arm, Trunk, and Center of Pressure Displacement in Patients with Hemiparesis. Mot. Control 2004, 8, 139–159. [Google Scholar] [CrossRef]
- Chern, J.S.; Lo, C.Y.; Wu, C.Y.; Chen, C.L.; Yang, S.; Tang, F.T. Dynamic Postural Control during Trunk Bending and Reaching in Healthy Adults and Stroke Patients. Am. J. Phys. Med. Rehabil. 2010, 89, 186–197. [Google Scholar] [CrossRef]
- Lin, L.C.; Liao, C.D.; Wu, C.W.; Huang, S.W.; Hong, J.P.; Chen, H.C. Effect of arm sling application on gait and balance in patients with post-stroke hemiplegia: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 11161. [Google Scholar] [CrossRef]
- Rafsten, L.; Meirelles, C.; Danielsson, A.; Sunnerhagen, K.S. Impaired Motor Function in the Affected Arm Predicts Impaired Postural Balance after Stroke: A Cross Sectional Study. Front. Neurol. 2019, 10, 912. [Google Scholar] [CrossRef]
- Mc Combe Waller, S.; Prettyman, M.G. Arm training in standing also improves postural control in participants with chronic stroke. Gait Posture 2012, 36, 419–424. [Google Scholar] [CrossRef][Green Version]
- Holmes, N.P.; Spence, C. The body schema and multisensory representation(s) of peripersonal space. Cogn. Process. 2004, 5, 94–105. [Google Scholar] [CrossRef]
- Boström, K.J.; Dirksen, T.; Zentgraf, K.; Wagner, H. The contribution of upper body movements to dynamic balance regulation during challenged locomotion. Front. Hum. Neurosci. 2018, 12, 1–10. [Google Scholar] [CrossRef]
- Mehrholz, J.; Wagner, K.; Rutte, K.; Meißner, D.; Pohl, M. Predictive Validity and Responsiveness of the Functional Ambulation Category in Hemiparetic Patients after Stroke. Arch. Phys. Med. Rehabil. 2007, 88, 1314–1319. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, J.E. Romberg Test. In Encyclopedia of Clinical Neuropsychology; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Cumming, T.B.; Churilov, L.; Linden, T.; Bernhardt, J. Montreal cognitive assessment and mini-mental state examination are both valid cognitive tools in stroke. Acta Neurol. Scand. 2013, 128, 122–129. [Google Scholar] [CrossRef]
- Alghadir, A.H.; Al-Eisa, E.S.; Anwer, S.; Sarkar, B. Reliability, validity, and responsiveness of three scales for measuring balance in patients with chronic stroke. BMC Neurol. 2018, 18, 141. [Google Scholar] [CrossRef] [PubMed]
- Hafsteinsdóttir, T.B.; Rensink, M.; Schuurmans, M. Clinimetric properties of the timed up and go test for patients with stroke: A systematic review. Top. Stroke Rehabil. 2014, 21, 197–210. [Google Scholar] [CrossRef] [PubMed]
- Gladstone, D.J.; Danells, C.J.; Black, S.E. The Fugl-Meyer Assessment of Motor Recovery after Stroke: A Critical Review of Its Measurement Properties. Neurorehabilit. Neural Repair. 2002, 16, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W.S.M. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef] [PubMed]
- Llorens, R.; Latorre, J.; Noé, E.; Keshner, E.A. Posturography using the Wii Balance BoardTM. A feasibility study with healthy adults and adults post-stroke. Gait Posture 2016, 43, 228–232. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA; Elsevier: Amsterdam, The Netherlands, 1977. [Google Scholar] [CrossRef]
- Baldi, B.; Moore, D.S. The Practice of Statistics in the Life Sciences, 3rd ed.; W.H. Freeman and Company: New York, NY, USA, 2014. [Google Scholar]
- Kuramatsu, Y.; Suzukamo, Y.; Izumi, S.I. Two types of sensorimotor strategies for whole-body movement in individuals with stroke: A pilot study. Physiother. Theory Pract. 2022, 38, 2580–2591. [Google Scholar] [CrossRef]
- Qin, W.; Yang, M.; Li, F.; Chen, C.; Zhen, L.; Tian, S. Influence of positional changes on spasticity of the upper extremity in poststroke hemiplegic patients. Neurosci. Lett. 2019, 712, 134479. [Google Scholar] [CrossRef]
- Baldan, A.M.S.; Alouche, S.R.; Araujo, I.M.G.; Freitas, S.M.S.F. Effect of light touch on postural sway in individuals with balance problems: A systematic review. Gait Posture 2014, 40, 1–10. [Google Scholar] [CrossRef]
- Bolton, D.A.E.; McIlroy, W.E.; Staines, W.R. The impact of light fingertip touch on haptic cortical processing during a standing balance task. Exp. Brain Res. 2011, 212, 279–291. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A.; Prince, F.; Frank, J.S.; Powell, C.; Zabjek, K.F. Unified theory regarding A/P and M/L balance in quiet stance. J. Neurophysiol. 1996, 75, 2334–2343. [Google Scholar] [CrossRef]
- Roelofs, J.M.B.; van Heugten, K.; de Kam, D.; Weerdesteyn, V.; Geurts, A.C.H. Relationships between Affected-Leg Motor Impairment, Postural Asymmetry, and Impaired Body Sway Control after Unilateral Supratentorial Stroke. Neurorehabilit. Neural Repair. 2018, 32, 953–960. [Google Scholar] [CrossRef]
- Objero, C.N.; Wdowski, M.M.; Hill, M.W. Can arm movements improve postural stability during challenging standing balance tasks? Gait Posture 2019, 74, 71–75. [Google Scholar] [CrossRef]
- Johnson, E.; Ellmers, T.J.; Muehlbauer, T.; Lord, S.R.; Hill, M.W. Effects of free versus restricted arm movements on postural control in normal and modified sensory conditions in young and older adults. Exp. Gerontol. 2023, 184, 112338. [Google Scholar] [CrossRef]
- Chung, S.; Lee, K.; Kim, Y. Effects of shoulder reaching exercise on the balance of patients with hemiplegia after stroke. J. Phys. Ther. Sci. 2016, 28, 2151–2153. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schwab, S.M.; Mayr, R.; Davis, T.J.; Silva, P.L.; Riley, M.A. Precision aiming performance with the paretic upper limb is associated with center of pressure patterns in individuals with chronic stroke. Gait Posture 2023, 103, 133–139. [Google Scholar] [CrossRef] [PubMed]
- Leech, K.A.; Roemmich, R.T.; Gordon, J.; Reisman, D.S.; Cherry-Allen, K.M. Updates in Motor Learning: Implications for Physical Therapist Practice and Education. Phys. Ther. 2022, 102, pzab250. [Google Scholar] [CrossRef]
- Garbus, R.B.S.C.; Prado-Rico, J.M.; Nardini, A.G.; Freitas, S.M.S.F. Immediate Effects of Arm Reaching Training in Standing on Postural Control Differ between Right and Left Stroke Individuals. J. Stroke Cerebrovasc. Dis. 2021, 30, 105984. [Google Scholar] [CrossRef]
- Major, M.J.; Stine, R.; Shirvaikar, T.; Gard, S.A. Effects of Upper Limb Loss or Absence and Prosthesis Use on Postural Control of Standing Balance. Am. J. Phys. Med. Rehabil. 2020, 99, 366–371. [Google Scholar] [CrossRef]
- Barra, J.; Marquer, A.; Joassin, R.; Reymond, C.; Metge, L.; Chauvineau, V.; Pérennou, D. Humans use internal models to construct and update a sense of verticality. Brain 2010, 133, 3552–3563. [Google Scholar] [CrossRef] [PubMed]
- Maravita, A.; Spence, C.; Driver, J. Multisensory integration and the body schema: Close to hand and within reach. Curr. Biol. 2003, 13, 531–539. [Google Scholar] [CrossRef]
- Morasso, P.; Casadio, M.; Mohan, V.; Rea, F.; Zenzeri, J. Revisiting the body-schema concept in the context of whole-body postural-focal dynamics. Front. Hum. Neurosci. 2015, 9, 83. [Google Scholar] [CrossRef]
- Lüdemann-Podubecká, J.; Nowak, D.A. Mapping cortical hand motor representation using TMS: A method to assess brain plasticity and a surrogate marker for recovery of function after stroke? Neurosci. Biobehav. Rev. 2016, 69, 239–251. [Google Scholar] [CrossRef]
- Bassolino, M.; Franza, M.; Guanziroli, E.; Sorrentino, G.; Canzoneri, E.; Colombo, M.; Crema, A.; Bertoni, T.; Mastria, G.; Vissani, M.; et al. Body and peripersonal space representations in chronic stroke patients with upper limb motor deficits. Brain Commun. 2022, 4, fcac179. [Google Scholar] [CrossRef]
- Romano, D.; Marini, F.; Maravita, A. Standard body-space relationships: Fingers hold spatial information. Cognition 2017, 165, 105–112. [Google Scholar] [CrossRef]
- Williamson, J.N.; Sikora, W.A.; James, S.A.; Parmar, N.J.; Lepak, L.V.; Cheema, C.F.; Refai, H.H.; Wu, D.H.; Sidorov, E.V.; Dewald, J.P.A.; et al. Cortical Reorganization of Early Somatosensory Processing in Hemiparetic Stroke. J. Clin. Med. 2022, 11, 6449. [Google Scholar] [CrossRef] [PubMed]
- Murnaghan, C.D.; Horslen, B.C.; Inglis, J.T.; Carpenter, M.G. Exploratory behavior during stance persists with visual feedback. Neuroscience 2011, 195, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, M.G.; Murnaghan, C.D.; Inglis, J.T. Shifting the balance: Evidence of an exploratory role for postural sway. Neuroscience 2010, 171, 196–204. [Google Scholar] [CrossRef]
- Binder, E.; Leimbach, M.; Pool, E.; Volz, L.J.; Eickhoff, S.B.; Fink, G.R.; Grefkes, C. Cortical reorganization after motor stroke: A pilot study on differences between the upper and lower limbs. Hum. Brain Mapp. 2021, 42, 1013–1033. [Google Scholar] [CrossRef]
- Anson, E.; Bigelow, R.T.; Swenor, B.; Deshpande, N.; Studenski, S.; Jeka, J.J.; Agrawal, Y. Loss of peripheral sensory function explains much of the increase in postural sway in healthy older adults. Front. Aging Neurosci. 2017, 9, 202. [Google Scholar] [CrossRef] [PubMed]


| Parameters | ||
|---|---|---|
| * Age (years) | 56.77 (±12.860) | |
| † Sex (frequencies and percentages) | M: 37 (56.92%); F: 28 (43.08%) | |
| * Injury time (years) | 4.469 (±4.8169) | |
| † Affected side | R: 27 (41.54%); L: 38 (58.46%) | |
| † Stroke type | Ischemic: 45 (69.23%); Haemorrhagic: 20 (30.77%) | |
| * TUG | 12.4035 (±7.23) | |
| * BBS | 50.34 (±4.819) | |
| † FAC | 5: 36 (55.38%); 4: 23 (35.39%); 3: 6 (9.23%) | |
| † Individual treatment | 32 (49.23%) | |
| † Groupal treatement | 11 (16.92%) | |
| † Absence of treatment | 22 (33.85%) | |
| * Teatment intensity (hours/week) | 0.6769 (±0.57405) | |
| † MAS | Shoulder flexors | 1+: 3 (4.62%); 1: 19 (29.23%); 0: 43 (66.15%) |
| Elbow flexors | 4: 2 (3.08%); 3: 6 (9.23%); 2: 10 (15.38%); 1+: 11 (16.92%); 1: 9 (13.85%); 0: 27 (41.54%) | |
| Wrist flexors | 4: 1 (1.54%); 3: 10 (15.38%); 2: 27 (10.78%); 1+: 2 (3.08%); 1: 11 (16.92%); 0: 34 (52.30%) | |
| Balance Parameters | FMA-Motor (A–D) | |||
|---|---|---|---|---|
| r | CI 95% | p Value | ||
| UL | LL | |||
| mCTSIB oscillation AP OEs (cm) | 0.073 | 0.82 | 0.59 | 0.566 |
| mCTSIB oscillation AP CEs (cm) | 0.021 | 0.43 | −0.03 | 0.867 |
| mCTSIB oscillation AP OEs foam (cm) | −0.070 | −0.55 | −0.80 | 0.582 |
| mCTSIB oscillation AP CEs foam (cm) | −0.24 | 0.00 | −0.46 | 0.058 |
| mCTSIB oscillation ML OEs (cm) | −0.44 | −0.23 | −0.62 | <0.001 * |
| mCTSIB oscillation ML CEs (cm) | −0.53 | −0.33 | −0.68 | <0.001 * |
| mCTSIB oscillation ML OEs foam (cm) | −0.39 | −0.16 | −0.58 | 0.001 * |
| mCTSIB oscillation ML CEs foam (cm) | −0.49 | −0.28 | −0.66 | <0.001 * |
| mCTSIB mean speed OEs (cm/s) | −0.22 | 0.02 | −0.44 | 0.076 |
| mCTSIB mean speed CEs (cm/s) | −0.28 | −0.03 | −0.49 | 0.023 |
| mCTSIB mean speed OEs foam (cm/s) | −0.07 | 0.17 | −0.30 | 0.582 |
| mCTSIB mean speed CEs foam (cm/s) | −0.39 | −0.16 | −0.58 | 0.001 * |
| Balance Parameters | FMA-A | FMA-B | FMA-C | FMA-D | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | CI 95% | p Value | r | CI 95% | p Value | r | CI 95% | p Value | r | CI 95% | p Value | |||||
| UL | LL | UL | LL | UL | LL | UL | LL | |||||||||
| mCTSIB oscillation AP OEs (cm) | 0.05 | 0.29 | −0.19 | 0.647 | 0.049 | 0.65 | 0.27 | 0.697 | 0.10 | 0.33 | −0.14 | 0.430 | 0.02 | 0.26 | −0.22 | 0.849 |
| mCTSIB oscillation AP CEs (cm) | 0.01 | 0.25 | −0.23 | 0.923 | 0.00 | 0.24 | −0.24 | 0.986 | 0.06 | 0.29 | −0.18 | 0.602 | −0.02 | 0.22 | −0.26 | 0.827 |
| mCTSIB oscillation AP OEs, foam (cm) | −0.13 | 0.11 | −0.36 | 0.288 | 0.00 | 0.24 | −0.24 | 0.997 | 0.04 | 0.28 | −0.20 | 0.751 | −0.15 | 0.09 | −0.37 | 0.208 |
| mCTSIB oscillation AP CEs foam (cm) | −0.28 | −0.03 | −0.49 | 0.022 | −0.21 | 0.03 | −0.43 | 0.085 | −0.08 | 0.16 | −0.31 | 0.491 | −0.23 | 0.01 | −0.44 | 0.070 |
| mCTSIB oscillation ML OEs (cm) | −0.50 | −0.29 | −0.66 | <0.001 * | −0.36 | −0.12 | −0.55 | 0.003 * | −0.29 | −0.04 | −0.49 | 0.016 | −0.38 | −0.15 | −0.57 | 0.002 * |
| mCTSIB oscillation ML CEs (cm) | −0.54 | −0.34 | −0.69 | <0.001 * | −0.43 | −0.20 | −0.60 | <0.001 * | −0.44 | −0.21 | −0.61 | <0.001 * | −0.48 | −0.26 | −0.64 | <0.001 * |
| mCTSIB oscillation ML OEs, foam (cm) | −0.43 | −0.20 | −0.60 | <0.001 * | −0.29 | −0.04 | 0.49 | 0.018 | −0.25 | 0.00 | −0.46 | 0.041 | −0.40 | −0.17 | −0.58 | 0.001 * |
| mCTSIB oscillation ML CEs, foam (cm) | −0.53 | −0.32 | −0.68 | <0.001 * | −0.42 | −0.19 | −0.60 | 0.001 * | −0.32 | −0.08 | −0.52 | 0.008 | −0.49 | −0.27 | −0.65 | <0.001 * |
| mCTSIB mean speed OEs (cm/s) | −0.26 | −0.01 | −0.47 | 0.035 | −0.15 | 0.09 | −0.37 | 0.210 | −0.12 | 0.12 | −0.35 | 0.33 | −0.25 | 0.00 | −0.46 | 0.041 |
| mCTSIB mean speed CEs (cm/s) | −0.32 | −0.08 | −0.52 | 0.007 | −0.21 | 0.03 | −0.43 | 0.091 | −0.15 | 0.09 | −0.37 | 0.211 | −0.32 | −0.08 | −0.52 | 0.008 |
| mCTSIB mean speed OEs, foam (cm/s) | −0.38 | −0.15 | −0.57 | 0.002 * | −0.25 | 0.00 | −0.46 | 0.044 | −0.22 | 0.02 | −0.44 | 0.078 | −0.35 | −0.11 | −0.54 | 0.004 * |
| mCTSIB mean speed CEs, foam (cm/s) | −0.32 | −0.08 | −0.52 | 0.009 | −0.27 | −0.02 | −0.48 | 0.032 | −0.18 | 0.06 | −0.40 | 0.146 | −0.31 | −0.07 | −0.51 | 0.013 |
| Balance Parameters | FMA-H | FMA-I | FMA-J | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r | CI 95% | p Value | r | CI 95% | p Value | r | CI 95% | p Value | ||||
| UL | LL | UL | LL | UL | LL | |||||||
| mCTSIB oscillation AP OEs (cm) | −0.11 | 0.13 | −0.34 | 0.364 | 0.12 | 0.35 | −0.12 | 0.320 | −0.06 | 0.18 | −0.29 | 0.635 |
| mCTSIB oscillation AP CEs (cm) | −0.19 | 0.05 | −0.41 | 0.127 | 0.05 | 0.29 | −0.19 | 0.676 | −0.10 | 0.14 | −0.33 | 0.409 |
| mCTSIB oscillation AP OEs foam (cm) | −0.17 | 0.07 | −0.39 | 0.154 | 0.07 | 0.30 | −0.17 | 0.558 | −0.08 | 0.16 | −0.31 | 0.498 |
| mCTSIB oscillation AP CEs foam (cm) | −0.15 | 0.09 | −0.37 | 0.226 | −0.13 | 0.11 | −0.36 | 0.308 | −0.20 | 0.04 | −0.42 | 0.101 |
| mCTSIB oscillation ML OEs (cm) | −0.35 | −0.11 | −0.54 | 0.003 * | −0.24 | 0.00 | −0.45 | 0.046 | −0.06 | 0.18 | −0.29 | 0.612 |
| mCTSIB oscillation ML CEs (cm) | −0.41 | −0.18 | −0.59 | 0.001 * | −0.25 | 0.00 | −0.46 | 0.040 | 0.10 | 0.33 | −0.14 | 0.426 |
| mCTSIB oscillation ML OEs foam (cm) | −0.40 | −0.17 | −0.58 | 0.001 * | −0.22 | 0.02 | −0.44 | 0.066 | −0.02 | 0.22 | −0.26 | 0.842 |
| mCTSIB oscillation ML CEs foam (cm) | −0.49 | −0.27 | −0.65 | <0.001 * | −0.28 | −0.03 | −0.49 | 0.024 | −0.14 | 0.10 | −0.37 | 0.275 |
| mCTSIB mean speed OEs (cm/s) | −0.18 | 0.06 | −0.40 | 0.147 | 0.00 | 0.24 | −0.24 | 0.950 | 0.00 | 0.24 | −0.24 | 0.978 |
| mCTSIB mean speed CEs (cm/s) | −0.20 | 0.04 | −0.42 | 0.103 | 0.29 | 0.49 | 0.04 | 0.819 | −0.07 | 0.17 | −0.30 | 0.551 |
| mCTSIB mean speed OEs, foam (cm/s) | −0.31 | −0.07 | −0.51 | 0.011 | 0.00 | 0.24 | −0.24 | 0.958 | 0.01 | 0.25 | −0.23 | 0.918 |
| mCTSIB mean speed CEs, foam (cm/s) | −0.16 | 0.08 | −0.38 | 0.209 | −0.04 | 0.20 | −0.28 | 0.746 | 0.00 | 0.24 | −0.24 | 0.979 |
| mCTSIB Oscillation ML OEs (cm) | mCTSIB Oscillation ML CEs (cm) | mCTSIB Oscillation ML OEs, Foam (cm) | mCTSIB Oscillation ML CEs, Foam (cm) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R2 | B | SE | p Value | R2 | B | SE | p Value | R2 | B | SE | p Value | R2 | B | SE | p Value | |
| FMA A-D | 0.203 | −0.441 | 0.009 | <0.001 * | 0.312 | −0.560 | 0.01 | <0.001 * | 0.165 | −0.415 | 0.011 | 0.001 * | 0.267 | −0.524 | 0.012 | <0.001 * |
| FMA-A | 0.258 | −0.497 | 0.017 | <0.001 * | 0.325 | −0.564 | 0.019 | <0.001 * | 0.197 | −0.450 | 0.021 | <0.001 * | 0.302 | −0.552 | 0.022 | <0.001 * |
| FMA-B | 0.135 | −0.354 | 0.047 | 0.006 * | 0.218 | −0.468 | 0.052 | <0.001 * | 0.093 | −0.314 | 0.059 | 0.017 | 0.197 | −0.453 | 0.063 | <0.001 * |
| FMA-C | 0.096 | −0.282 | 0.034 | 0.028 | 0.174 | −0.453 | 0.037 | <0.001 * | 0.073 | −0.271 | 0.042 | 0.037 | 0.128 | −0.354 | 0.046 | 0.006 * |
| FMA-D | 0.150 | −0.371 | 0.097 | 0.004 * | 0.258 | −0506 | 0.105 | <0.001 * | 0.178 | −0.433 | 0.116 | 0.001 * | 0.275 | −0.535 | 0.123 | <0.001 * |
| FMA-H | 0.135 | −0.343 | 0.057 | 0.006 * | 0.184 | −0.412 | 0.064 | 0.001 * | 0.173 | −0.418 | 0.067 | 0.001 * | 0.269 | −0.518 | 0.071 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mallo-López, A.; Cuesta-Gómez, A.; Fernández-Pardo, T.E.; Aguilera-Rubio, Á.; Molina-Rueda, F. Influence of Impaired Upper Extremity Motor Function on Static Balance in People with Chronic Stroke. Sensors 2024, 24, 4311. https://doi.org/10.3390/s24134311
Mallo-López A, Cuesta-Gómez A, Fernández-Pardo TE, Aguilera-Rubio Á, Molina-Rueda F. Influence of Impaired Upper Extremity Motor Function on Static Balance in People with Chronic Stroke. Sensors. 2024; 24(13):4311. https://doi.org/10.3390/s24134311
Chicago/Turabian StyleMallo-López, Ana, Alicia Cuesta-Gómez, Teresa E. Fernández-Pardo, Ángela Aguilera-Rubio, and Francisco Molina-Rueda. 2024. "Influence of Impaired Upper Extremity Motor Function on Static Balance in People with Chronic Stroke" Sensors 24, no. 13: 4311. https://doi.org/10.3390/s24134311
APA StyleMallo-López, A., Cuesta-Gómez, A., Fernández-Pardo, T. E., Aguilera-Rubio, Á., & Molina-Rueda, F. (2024). Influence of Impaired Upper Extremity Motor Function on Static Balance in People with Chronic Stroke. Sensors, 24(13), 4311. https://doi.org/10.3390/s24134311








