Deep Learning Strategy for Sliding ECG Analysis during Cardiopulmonary Resuscitation: Influence of the Hands-Off Time on Accuracy
Abstract
1. Introduction
- Two-stage algorithms are implemented in the real-time AED analysis process during OHCA interventions, applying the first stage during uninterrupted CC (analysis duration 11–30 s), eventually followed by a second reconfirmation stage on clean ECG (5–9 s). A delayed shock decision with reconfirmation analysis is required in 26–100% of OHCA interventions analyzed by several commercial AED algorithms [28,29,30,31]. Such two-stage schemes demand synchronization with additional algorithms for detection of the start and stop of CC in a standard CPR protocol with compression-to-ventilation ratios of 30:2, 15:2, or 15:1 [32,33,34].
- Single-stage algorithms based on deep neural networks (DNN) are run in PC workstations with OHCA databases during CPR. The DNN input feature maps and architectures depend on study-specific processing concepts, e.g., supplying unfiltered raw ECG signals with continuous CC artefacts to the input of fully convolutional neural networks (CNNs) [35], prefiltered raw ECG signals to CNN [36,37], or a hybrid DNN architecture, including a combination of convolutional layers, residual blocks, and bidirectional long short-term memory (LSTM) layers [38].
2. Materials and Methods
2.1. ECG Databases
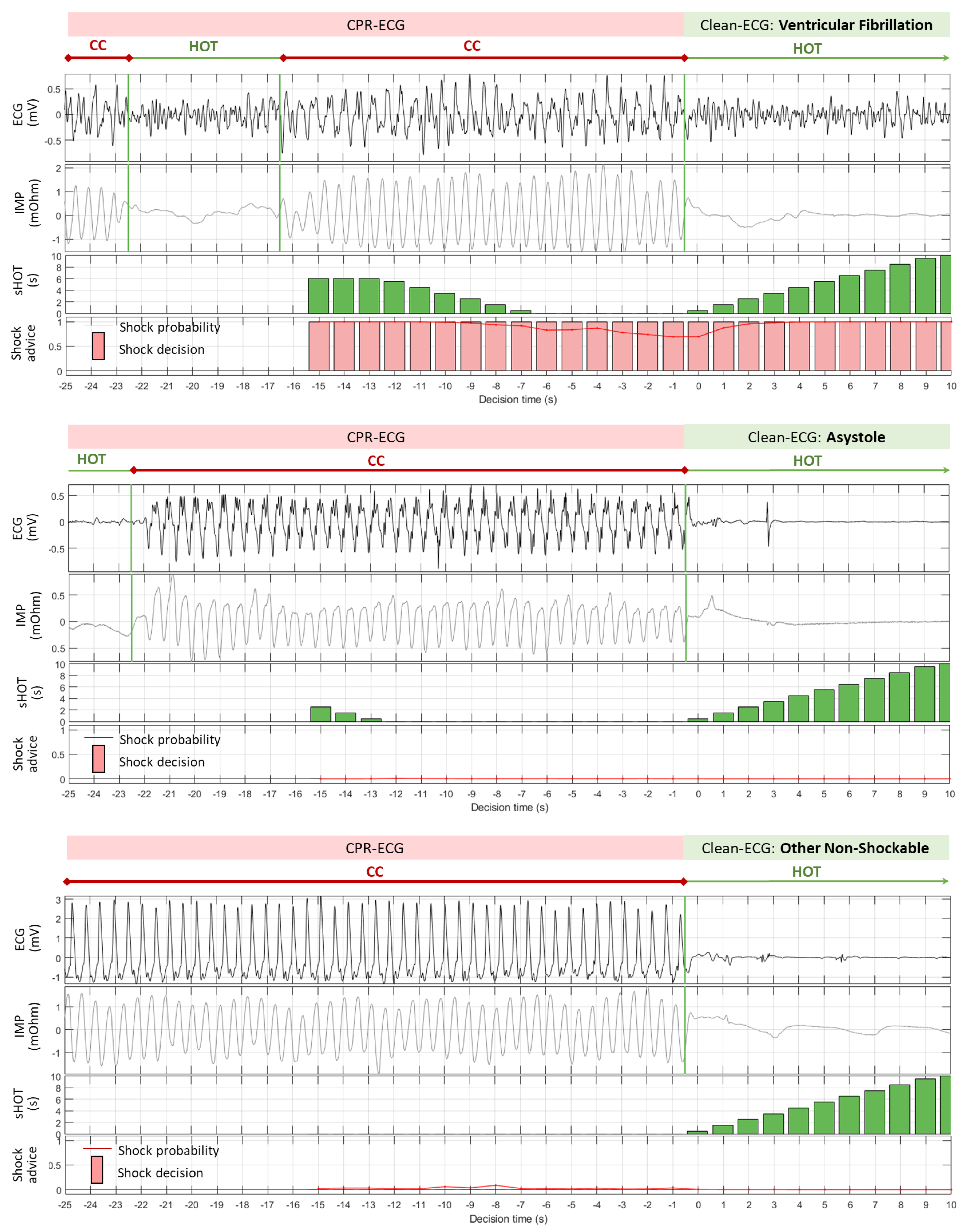
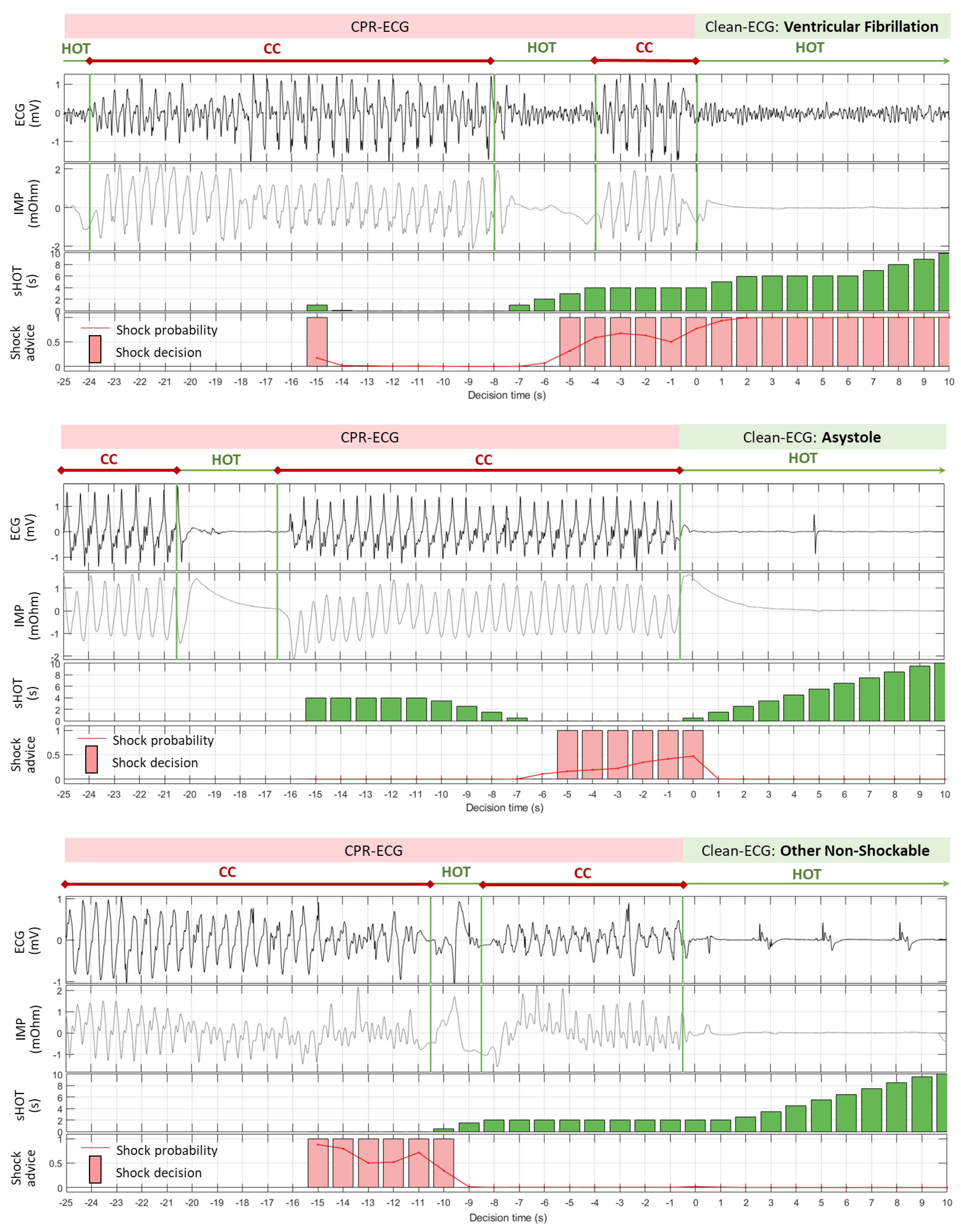
- CPR-ECG: 30 s ECG buffer (−30 s; 0 s] contaminated by CC episodes and hands-off pauses during insufflations. Notably, the instants for start and stop of CC episodes can occur randomly during the period of interest.
- Clean-ECG: 10 s ECG buffer (0 s; 10 s] with hands-off pause and presumably without artefacts, representing the ECG signal analyzed by the AED real-time process.
- VF: coarse ventricular fibrillation with amplitude > 200 µV;
- NSR: normal sinus rhythm with visible P-QRS-T waves and heart rate of 40–100 bpm;
- ONR: other non-shockable rhythm, including atrial fibrillation/flutter, sinus bradycardia, supraventricular tachycardia, premature ventricular contractions, heart blocks, etc.;
- ASYS: asystole with low-amplitude ECG, having peak-to-peak signal deflection ≤ 100 µV for more than 4 s.
2.2. Sliding ECG Analysis during CPR
2.3. DNN Design
- Conv1D: 1D convolution layer with kernel dimensions < Ki × Fi-1 × Fi >and biases corresponding to Fi, where the kernel sizes are K1,2,3 = {10, 20, 20}, and the number of filters is F1,2,3 = {5, 25, 50}. Consider F0 = 1, matching the input ECG dimension;
- Activation: activation layer applying rectified linear unit (ReLU) function;
- MaxPooling1D: max pooling layer with a pool size of 2;
- Dropout: dropout layer with a drop rate α = 0.3.
2.4. DNN Training
- Kernel initializer: ‘random uniform’;
- Optimizer: ‘Adam’ with learning rate of 0.001, and exponential decay rate for the first and second moment estimates β1 = 0.9 and β2 = 0.999, respectively;
- Loss function: ‘weighted binary cross-entropy’ for two target classes (Sh/NSh). Considering the unequal distribution of Sh (5.7%, 409/7172) and NSh signals (94.3%, 6763/7172) in the learning database, a penalty proportional to the class prevalence was applied in the loss (Equation (2)), where M is the size of the learning database, δm is a binary indicator function (δm = 1 if xm belongs to the shockable class; otherwise, δm = 0), and wSh = 0.943 and wNSh = 0.057 are the weights for Sh and NSh classes, complying with the condition wSh+ wNSh = 1.
- Training epochs: maximum of 750, with activated early stopping if no improvement in the validation loss was obtained for 150 epochs;
- Batch size: 128.
2.5. Performance Evaluation
3. Results
3.1. Validation Receiver Operating Characteristic Curve
3.2. Sliding CPR Analysis: Case Study
3.3. Sliding CPR Analysis: Statistical Study
- CNN-CPR (5 s): mean Se (VF) = 88–90%, Sp (ASYS) = 91.5–94%, Sp (ONR) = 96–97%, Sp (NSR) = 99–100% (Figure 8a).
- CNN-CPR (10 s): mean Se (VF) = 92–94.4%, Sp (ASYS) = 92.2–94%, Sp (ONR) = 96–97%, Sp (NSR) = 98.2–99.5% (Figure 8b).
- CNN-CPR (15 s): mean Se (VF) = 93.4–95%, Sp (ASYS) = 91.5–94%, Sp (ONR) = 95.6–96.8%, Sp (NSR) = 99–100% (Figure 8c).
- CNN-CPR (5 s): mean Se (VF) = 96–97.2%, Sp (ASYS) = 99.4–99.8%, Sp (ONR) = 99.2–99.6%, Sp (NSR) = 100% (Figure 8a).
- CNN-CPR (10 s): mean Se (VF) = 98–99%, Sp (ASYS) = 98.2–99.8%, Sp (ONR) = 98.8–99.1%, Sp (NSR) = 100% (Figure 8b).
- CNN-CPR (15 s): mean Se (VF) = 97.5–98.8%, Sp (ASYS) = 97.8–99.8%, Sp (ONR) = 98.1–99.2%, Sp (NSR) = 100% (Figure 8c).
3.4. Test Performance vs. sHOT
- Minimal sHOT = (0–1 s] was necessary for the model CNN-CPR (5 s) to improve Se (VF) to 90.1%, and CNN-CPR (10 s) to improve Sp (NSR) to 99%;
- Minimal sHOT = (1–2 s] was necessary for the models CNN-CPR (5 s) and CNN-CPR (10 s) to improve Sp (ASYS) to 96.9% and 96.4%, respectively, and CNN-CPR (15 s) to improve Sp (ONR) to 95.2%;
- Minimal sHOT = (2–3 s] was necessary for the model CNN-CPR (15 s) to improve Sp (ASYS) to 96.4%.
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126. [Google Scholar] [CrossRef] [PubMed]
- Perkins, G.; Nolan, J. Advanced Life Support Update. Crit. Care 2022, 26, 73. [Google Scholar] [CrossRef] [PubMed]
- Wyckoff, M.H.; Greif, R.; Morley, P.T.; Ng, K.-C.; Olasveengen, T.M.; Singletary, E.M.; Soar, J.; Cheng, A.; Drennan, I.R.; Liley, H.G.; et al. 2022 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations: Summary From the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Resuscitation 2022, 181, 208–288. [Google Scholar] [CrossRef]
- Hollenbeck, R.D.; McPherson, J.A.; Mooney, M.R.; Unger, B.T.; Patel, N.C.; McMullan, P.W., Jr.; Hsu, C.H.; Seder, D.B.; Kern, K.B. Early cardiac catheterization is associated with improved survival in comatose survivors of cardiac arrest without STEMI. Resuscitation 2014, 85, 88–95. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Shah, S.M.M.; Mubashir, A.; Khan, A.R.; Fatima, K.; Schenone, A.L.; Khosa, F.; Samady, H.; Menon, V. Early coronary angiography in patients resuscitated from out of hospital cardiac arrest without ST-segment elevation: A systematic review and meta-analysis. Resuscitation 2017, 121, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Sell, R.E.; Sarno, R.; Lawrence, B.; Castillo, E.M.; Fisher, R.; Brainard, C.; Dunford, J.V.; Davis, D.P. Minimizing pre- and post-defibrillation pauses increases the likelihood of return of spontaneous circulation (ROSC). Resuscitation 2010, 81, 822–825. [Google Scholar] [CrossRef] [PubMed]
- Pierce, A.E.; Roppolo, L.P.; Owens, P.C.; Pepe, P.E.; Idris, A.H. The need to resume chest compressions immediately after defibrillation attempts: An analysis of post-shock rhythms and duration of pulselessness following out-of-hospital cardiac arrest. Resuscitation 2015, 89, 162–168. [Google Scholar] [CrossRef]
- Fitzgibbon, E.; Berger, R.; Tsitlik, J.; Halperin, H. Determination of the noise source in the electrocardiogram during cardiopulmonary resuscitation. Crit. Care Med. 2002, 30, S148–S153. [Google Scholar] [CrossRef]
- Olasveengen, T.; Semeraro, F.; Ristagno, G.; Castren, M.; Handley, A.; Kuzovlev, A.; Monsieurs, K.G.; Raffay, V.; Smyth, M.; Soar, J.; et al. European Resuscitation Council Guidelines 2021: Basic Life Support. Resuscitation 2021, 161, 98–114. [Google Scholar] [CrossRef]
- Isasi, I.; Irusta, U.; Rad, A.; Aramendi, E.; Zabihi, M.; Eftestøl, T.; Kramer-Johansen, J.; Wik, L. Automatic cardiac rhythm classification with concurrent manual chest compressions. IEEE Access 2019, 7, 115147–115159. [Google Scholar] [CrossRef]
- Isasi, I.; Irusta, U.; Elola, A.; Aramendi, E.; Eftestøl, T.; Kramer-Johansen, J.; Wik, L. A robust machine learning architecture for a reliable ECG rhythm analysis during CPR. In Proceedings of the 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, 23–27 July 2019; pp. 1903–1907. [Google Scholar] [CrossRef]
- Isasi, I.; Irusta, U.; Aramendi, E.; Idris, A.; Sörnmo, L. Restoration of the electrocardiogram during mechanical cardiopulmonary resuscitation. Physiol. Meas. 2020, 41, 105006. [Google Scholar] [CrossRef] [PubMed]
- Irusta, U.; Ruiz, J.; de Gauna, S.; Eftestøl, T.; Kramer-Johansen, J. A least mean-square filter for the estimation of the cardiopulmonary resuscitation artifact based on the frequency of the compressions. IEEE Trans. Biomed. Eng. 2009, 56, 1052–1062. [Google Scholar] [CrossRef]
- Ayala, U.; Irusta, U.; Ruiz, J.; Eftestøl, T.; Kramer-Johansen, J.; Alonso-Atienza, F.; Alonso, E.; González-Otero, D. A reliable method for rhythm analysis during cardiopulmonary resuscitation. Biomed. Res. Int. 2014, 2014, 872470. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.; Irusta, U.; De Gauna, S.; Eftestøl, T. Cardiopulmonary resuscitation artefact suppression using a Kalman filter and the frequency of chest compressions as the reference signal. Resuscitation 2010, 81, 1087–1094. [Google Scholar] [CrossRef]
- Aramendi, E.; Ayala, U.; Irusta, U.; Alonso, E.; Eftestøl, T.; Kramer-Johansen, J. Suppression of the cardiopulmonary resuscitation artefacts using the instantaneous chest compression rate extracted from the thoracic impedance. Resuscitation 2012, 83, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Babaeizadeh, S.; Firoozabadi, R.; Han, C.; Helfenbein, E. Analyzing cardiac rhythm in the presence of chest compression artifact for automated shock advisory. J. Electrocardiol. 2014, 47, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Gao, P.; Wei, L.; Dai, C.; Zhang, L.; Li, Y. An enhanced adaptive filtering method for suppressing cardiopulmonary resuscitation artifact. IEEE Trans. Biomed. Eng. 2016, 64, 471–478. [Google Scholar] [CrossRef]
- Berger, R.; Palazzolo, J.; Halperin, H. Rhythm discrimination during uninterrupted CPR using motion artifact reduction system. Resuscitation 2007, 75, 145–152. [Google Scholar] [CrossRef]
- Tan, Q.; Freeman, G.; Geheb, F.; Bisera, J. Electrocardiographic analysis during uninterrupted cardiopulmonary resuscitation. Crit. Care Med. 2008, 36, S409–S412. [Google Scholar] [CrossRef]
- Rheinberger, K.; Steinberger, T.; Unterkofler, K.; Baubin, M.; Klotz, A.; Amann, A. Removal of CPR artifacts from the ventricular fibrillation ECG by adaptive regression on lagged reference signals. IEEE Trans. Biomed. Eng. 2007, 55, 130–137. [Google Scholar] [CrossRef]
- Krasteva, V.; Jekova, I.; Dotsinsky, I.; Didon, J.P. Shock advisory system for heart rhythm analysis during cardiopulmonary resuscitation using a single ECG input of automated external defibrillators. Ann. Biomed. Eng. 2010, 38, 1326–1336. [Google Scholar] [CrossRef] [PubMed]
- Amann, A.; Klotz, A.; Niederklapfer, T.; Kupferthaler, A.; Werther, T.; Granegger, M.; Lederer, W.; Baubin, M.; Lingnau, W. Reduction of CPR artifacts in the ventricular fibrillation ECG by coherent line removal. Biomed. Eng. Online 2010, 9, 2. [Google Scholar] [CrossRef]
- De Gauna, S.; Ruiz, J.; Irusta, U.; Aramendi, E.; Eftestøl, T.; Kramer-Johansen, J. A method to remove CPR artefacts from human ECG using only the recorded ECG. Resuscitation 2008, 76, 271–278. [Google Scholar] [CrossRef]
- Hajeb, M.S.; Cascella, A.; Valentine, M.; Chon, K.H. Automated Condition-Based Suppression of the CPR Artifact in ECG Data to Make a Reliable Shock Decision for AEDs during CPR. Sensors 2021, 21, 8210. [Google Scholar] [CrossRef] [PubMed]
- Hajeb, M.S.; Cascella, A.; Valentine, M.; Chon, K.H. Enhancing the accuracy of shock advisory algorithms in automated external defibrillators during ongoing cardiopulmonary resuscitation using a deep convolutional Encoder-Decoder filtering model. Expert Syst. Appl. 2022, 203, 117499. [Google Scholar] [CrossRef]
- Li, Y.; Bisera, J.; Geheb, F.; Tang, W.; Weil, M. Identifying potentially shockable rhythms without interrupting cardiopulmonary resuscitation. Crit. Care Med. 2008, 36, 198–203. [Google Scholar] [CrossRef]
- Fumagalli, F.; Silver, A.; Tan, Q.; Zaidi, N.; Ristagno, G. Cardiac rhythm analysis during ongoing cardiopulmonary resuscitation using the Analysis During Compressions with Fast Reconfirmation technology. Heart Rhythm 2018, 15, 248–255. [Google Scholar] [CrossRef]
- Hu, Y.; Tang, H.; Liu, C.; Jing, D.; Zhu, H.; Zhang, Y.; Yu, X.; Zhang, G.; Xu, J. The performance of a new shock advisory algorithm to reduce interruptions during CPR. Resuscitation 2019, 143, 1–9. [Google Scholar] [CrossRef]
- De Graaf, C.; Beesems, S.; Oud, S.; Stickney, R.E.; Piraino, D.W.; Chapman, F.W.; Koster, R.W. Analyzing the heart rhythm during chest compressions: Performance and clinical value of a new AED algorithm. Resuscitation 2021, 162, 320–328. [Google Scholar] [CrossRef]
- Didon, J.P.; Menetre, S.; Jekova, I.; Stoyanov, T.; Krasteva, V. Analyze whilst compressing algorithm for detection of ventricular fibrillation during CPR: A comparative performance evaluation for automated external defibrillators. Resuscitation 2021, 160, 94–102. [Google Scholar] [CrossRef]
- Ayala, U.; Irusta, U.; Kramer-Johansen, J.; González-Otero, D.; Ruiz de Gauna, S.; Ruiz, J.; Alonso, E.; Eftestøl, T. Automatic detection of chest compression pauses for rhythm analysis during 30:2 CPR in an ALS scenario. Resuscitation 2014, 85S, S9. [Google Scholar] [CrossRef]
- González-Otero, D.; Ruiz de Gauna, S.; Ruiz, J.; Ayala, U.; Alonso, E. Automatic detection of chest compression pauses using the transthoracic impedance signal. Comput. Cardiol. 2012, 39, 21–24. [Google Scholar]
- Didon, J.P.; Krasteva, V.; Ménétré, S.; Stoyanov, T.; Jekova, I. Shock advisory system with minimal delay triggering after end of chest compressions: Accuracy and gained hands-off time. Resuscitation 2011, 82S, S8–S15. [Google Scholar] [CrossRef] [PubMed]
- Jekova, I.; Krasteva, V. Optimization of end-to-end convolutional neural networks for analysis of out-of-hospital cardiac arrest rhythms during cardiopulmonary resuscitation. Sensors 2021, 21, 4105. [Google Scholar] [CrossRef]
- Isasi, I.; Irusta, U.; Aramendi, E.; Eftestøl, T.; Kramer-Johansen, J.; Wik, L. Rhythm analysis during cardiopulmonary resuscitation using convolutional neural networks. Entropy 2020, 22, 595. [Google Scholar] [CrossRef]
- Isasi, I.; Irusta, U.; Aramendi, E.; Olsen, J.-Å.; Wik, L. Detection of shockable rhythms using convolutional neural networks during chest compressions provided by a load distributing band. Comput. Cardiol. 2020, 47, 1–4. [Google Scholar] [CrossRef]
- Hajeb, M.; Cascella, A.; Valentine, M.; Chon, K. Deep neural network approach for continuous ECG-based automated external defibrillator shock advisory system during cardiopulmonary resuscitation. J. Am. Heart Assoc. 2021, 10, e019065. [Google Scholar] [CrossRef]
- Ayala, U.; Irusta, U.; Ruiz, J.; Ruiz de Gauna, S.; González-Otero, D.; Alonso, E.; Kramer-Johansen, J.; Naas, H.; Eftestøl, T. Fully automatic rhythm analysis during chest compression pauses. Resus 2015, 89, 25–30. [Google Scholar] [CrossRef]
- Ruiz, J.; Ayala, U.; Ruiz de Gauna, S.; Irusta, U.; González-Otero, D.; Alonso, E.; Kramer-Johansen, J.; Eftestøl, T. Feasibility of automated rhythm assessment in chest compression pauses during cardiopulmonary resuscitation. Resuscitation 2013, 84, 1223–1228. [Google Scholar] [CrossRef]
- Krasteva, V.; Ménétré, S.; Didon, J.P.; Jekova, I. Fully convolutional deep neural networks with optimized hyperparameters for detection of shockable and non-shockable rhythms. Sensors 2020, 20, 2875. [Google Scholar] [CrossRef]
- Skjeflo, G.W.; Nordseth, T.; Loennechen, J.P.; Bergum, D.; Skogvoll, E. ECG changes during resuscitation of patients with initial pulseless electrical activity are associated with return of spontaneous circulation. Resuscitation 2018, 127, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, S.; Doan, J.; Blackwood, J.; Coult, J.; Kudenchuk, P.; Sherman, L.; Rea, T.; Kwok, H. Rhythm profiles and survival after out-of-hospital ventricular fibrillation cardiac arrest. Resuscitation 2018, 125, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Soar, J.; Böttiger, B.; Carli, P.; Couper, K.; Deakin, C.; Djärv, T.; Lott, C.; Olasveengen, T.; Paal, P.; Pellis, T.; et al. European Resuscitation Council Guidelines 2021: Adult advanced life support. Resus 2021, 161, 115–151. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.; Ayala, U.; Ruiz de Gauna, S.; Irusta, U.; Gonzalez-Otero, D.; Aramendi, E.; Alonso, E.; Eftestøl, T. Direct evaluation of the effect of filtering the chest compression artifacts on the uninterrupted cardiopulmonary resuscitation time. Am. J. Emerg. Med. 2013, 31, 910–915. [Google Scholar] [CrossRef]
- Kwok, H.; Coult, J.; Blackwood, J.; Sotoodehnia, N.; Kudenchuk, P.; Rea, T. A method for continuous rhythm classification and early detection of ventricular fibrillation during CPR. Resuscitation 2022, 176, 90–97. [Google Scholar] [CrossRef]
- Kerber, R.E.; Becker, L.B.; Bourland, J.D.; Cummins, R.O.; Hallstrom, A.P.; Michos, M.B.; Nichol, G.; Ornato, J.P.; Thies, W.H.; White, R.D.; et al. Automatic external defibrillation: Recommendations for specifying and reporting arrhythmia analysis algorithm performance, incorporating new waveforms, and enhancing safety. Circulation 1997, 95, 1677–1682. [Google Scholar] [CrossRef]
- Koster, R.; Baubin, M.; Bossaert, L.; Caballero, A.; Cassan, P.; Castrén, M.; Granja, C.; Handley, A.J.; Monsieurs, K.G.; Perkins, G.D.; et al. European Resuscitation Council Guidelines for Resuscitation 2010 Section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 2010, 81, 1277–1292. [Google Scholar] [CrossRef]
- Shen, C.P.; Freed, B.C.; Walter, D.P.; Perry, J.C.; Barakat, A.F.; Elashery, A.R.A.; Shah, K.S.; Kutty, S.; McGillion, M.; Siong Ng, F.; et al. Convolution neural network algorithm for shockable arrhythmia classification within a digitally connected automated external defibrillator. J. Am. Heart Assoc. 2023, 2023, e026974. [Google Scholar] [CrossRef]
- Roeder, L. Netron, Visualizer for neural network, deep learning, and machine learning models. Comput. Softw. 2017. [Google Scholar] [CrossRef]
- Eilevstjønn, J.; Eftestøl, T.; Aase, S.O.; Myklebust, H.; Husøya, J.H.; Steen, P.A. Feasibility of shock advice analysis during CPR through removal of CPR artefacts from the human ECG. Resuscitation 2004, 61, 131–141. [Google Scholar] [CrossRef]
- Gong, Y.; Wei, L.; Yan, S.; Zuo, F.; Zhang, H.; Li, Y. Transfer learning based deep network for signal restoration and rhythm analysis during cardiopulmonary resuscitation using only the ECG waveform. Inf. Sci. 2023, 626, 754–772. [Google Scholar] [CrossRef]
- Irusta, U.; Aramendi, E.; Chicote, B.; Alonso, D.; Corcuera, C.; Veintemillas, J.; Larrea, A.; Olabarria, M. Deep learning approach for a shock advise algorithm using short electrocardiogram analysis intervals. Resuscitation 2019, 42, e85. [Google Scholar] [CrossRef]
- Picon, A.; Irusta, U.; lvarez-Gila, A.; Aramendi, E.; Alonso-Atienza, F.; Figuera, C.; Ayala, U.; Garrote, E.; Wik, L.; Kramer-Johansen, J.; et al. Mixed convolutional and long short-term memory network for the detection of lethal ventricular arrhythmia. PLoS ONE 2019, 14, e0216756. [Google Scholar] [CrossRef] [PubMed]
- Didon, J.P.; Dotsinsky, I.; Jekova, I.; Krasteva, V. Detection of shockable and non-shockable rhythms in presence of CPR artifacts by time-frequency ECG analysis. Comput. Cardiol. 2009, 36, 817–820. [Google Scholar]
- Jekova, I.; Krasteva, V.; Dotsinsky, I. Filtering of chest compression artefacts in the electrocardiogram. Bioautomation 2009, 13, 19–28. [Google Scholar]
- Li, Y.; Tang, W. Techniques for artefact filtering from chest compression corrupted ECG signals: Good, but not enough. Resuscitation 2009, 80, 1219–1220. [Google Scholar] [CrossRef] [PubMed]








| Database | Total Number of Episodes (Patients *) | Number of Episodes (Patients) per Rhythm | |||
|---|---|---|---|---|---|
| VF | NSR | ONR | ASYS | ||
| Learning | 7173 (1504) | 409 (172) | 175 (82) | 1976 (611) | 4613 (1092) |
| Test | 6397 (1334) | 393 (145) | 177 (83) | 1848 (544) | 3979 (916) |
| Total | 13570 (2838) | 802 (317) | 352 (165) | 3824 (1155) | 8592 (2008) |
| CNN-CPR (5 s) | CNN-CPR (10 s) | CNN-CPR (15 s) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| sHOT | Se | Sp | Sp | Sp | Se | Sp | Sp | Sp | Se | Sp | Sp | Sp |
| (VF) | (NSR) | (ONR) | (ASYS) | (VF) | (NSR) | (ONR) | (ASYS) | (VF) | (NSR) | (ONR) | (ASYS) | |
| (s) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) |
| 0 | 87.8 * | 99.3 | 95.4 | 90.6 * | 91.4 | 97.8 * | 95.1 | 88.5 * | 92.3 | 99.2 | 94.2 * | 85.7 * |
| (0–1] | 90.1 | 99.7 | 97.7 | 94.6 * | 92.3 | 99.0 | 95.9 | 93.0 * | 93.2 | 100 | 94.2 * | 91.1 * |
| (1–2] | 93.0 | 99.6 | 98.5 | 96.9 | 94.0 | 99.4 | 97.7 | 96.4 | 94.8 | 100 | 95.2 | 94.8 * |
| (2–3] | 95.8 | 99.6 | 99.3 | 97.8 | 96.2 | 99.6 | 98.5 | 97.5 | 96.0 | 100 | 97.6 | 96.4 |
| (3–4] | 95.8 | 100 | 99.6 | 99.0 | 96.7 | 100 | 99.2 | 98.5 | 97.1 | 100 | 99.1 | 98.0 |
| (4–5] | 96.6 | 99.9 | 99.2 | 99.6 | 97.8 | 100 | 99.1 | 99.3 | 97.2 | 100 | 99.1 | 98.8 |
| (5–6] | 99.0 | 100 | 99.3 | 99.2 | 97.7 | 100 | 99.0 | 99.2 | ||||
| (6–7] | 98.8 | 100 | 99.2 | 99.4 | 98.0 | 100 | 98.9 | 99.3 | ||||
| (7–8] | 98.8 | 100 | 98.8 | 99.7 | 98.5 | 100 | 99.0 | 99.7 | ||||
| (8–9] | 98.7 | 100 | 98.5 | 99.7 | 98.7 | 100 | 99.1 | 99.8 | ||||
| (9–10] | 98.9 | 100 | 97.7 | 99.6 | 98.9 | 100 | 99.0 | 99.8 | ||||
| >10 | 98.9 | 100 | 98.7 | 99.5 | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krasteva, V.; Didon, J.-P.; Ménétré, S.; Jekova, I. Deep Learning Strategy for Sliding ECG Analysis during Cardiopulmonary Resuscitation: Influence of the Hands-Off Time on Accuracy. Sensors 2023, 23, 4500. https://doi.org/10.3390/s23094500
Krasteva V, Didon J-P, Ménétré S, Jekova I. Deep Learning Strategy for Sliding ECG Analysis during Cardiopulmonary Resuscitation: Influence of the Hands-Off Time on Accuracy. Sensors. 2023; 23(9):4500. https://doi.org/10.3390/s23094500
Chicago/Turabian StyleKrasteva, Vessela, Jean-Philippe Didon, Sarah Ménétré, and Irena Jekova. 2023. "Deep Learning Strategy for Sliding ECG Analysis during Cardiopulmonary Resuscitation: Influence of the Hands-Off Time on Accuracy" Sensors 23, no. 9: 4500. https://doi.org/10.3390/s23094500
APA StyleKrasteva, V., Didon, J.-P., Ménétré, S., & Jekova, I. (2023). Deep Learning Strategy for Sliding ECG Analysis during Cardiopulmonary Resuscitation: Influence of the Hands-Off Time on Accuracy. Sensors, 23(9), 4500. https://doi.org/10.3390/s23094500







