Abstract
Health is gold, and good health is a matter of survival for humanity. The development of the healthcare industry aligns with the development of humans throughout history. Nowadays, along with the strong growth of science and technology, the medical domain in general and the healthcare industry have achieved many breakthroughs, such as remote medical examination and treatment applications, pandemic prediction, and remote patient health monitoring. The advent of 5th generation communication networks in the early 2020s led to the Internet of Things concept. Moreover, the 6th generation communication networks (so-called 6G) expected to launch in 2030 will be the next revolution of the IoT era, and will include autonomous IoT systems and form a series of endogenous intelligent applications that serve humanity. One of the domains that receives the most attention is smart healthcare. In this study, we conduct a comprehensive survey of IoT-based technologies and solutions in the medical field. Then, we propose an all-in-one computing architecture for real-time IoHT applications and present possible solutions to achieving the proposed architecture. Finally, we discuss challenges, open issues, and future research directions. We hope that the results of this study will serve as essential guidelines for further research in the human healthcare domain.
1. Introduction
The history of human development has proven that healthcare applications have always been the main driving force behind the development of science and technology. Since ancient times, humanity has envisioned solutions to diagnosing and treating diseases from a distance. The advent of generation network technology, also known as 5G, enables the delivery of network services with ultra-high throughput and ultra-low latency. This has led to the Internet of Things concept and shaped emerging intelligent domains. Among these areas, healthcare and medicine are becoming some of the most crucial domains.
In recent decades, electronic health information systems (e-health) have focused on developing and achieving many positive results. In the traditional architecture of e-health systems, computing, processing, and storage are located in the cloud. Its robustness, reliability, and powerful computing capacity make cloud computing (CC) the computing technology of the future [1,2]. Although cloud computing has outstanding advantages, a significant limitation of CC is its high service response time. As a result, it is impossible to use in real-time healthcare applications. In recent times, to solve this problem, the integration of IoT technology and fog computing (FC) solutions [3] with edge computing (EC) [4] has been proposed.
EC and FC technologies aim to bridge the gap between databases and end-users or bring cloud capabilities closer to users. As a result, FC and EC reduce service response times, energy consumption, and computational costs, and improve reliability.
According to Statista’s forecast, the IoT market is expected to reach USD billion by 2025 [5]. Moreover, a survey by Vodafone shows that over of people surveyed spend more on intelligent health. In addition, about of people surveyed use IoT devices to monitor vital indicators such as blood pressure, heart rate, and blood sugar [6]. These issues show that healthcare focuses on IoT technology and real-time computing solutions.
Telemedicine is one of the most significant medical applications in recent times based on IoT technology. Telemedicine can bridge the gap between rural and urban health. It provides low-cost consultation, remote examination, and diagnosis. As a result, Telemedicine can enable leading experts and doctors to reach the most remote areas and provide advanced medical services to everyone at a low cost. In other words, combining IoT technology and real-time computing solutions plays an essential role in the healthcare sector.
There are many studies on the IoT, and advanced computing technologies have been proposed in the field of smart health. To clarify this matter, we conduct a short survey of studies that have been conducted during the period 2019–2022 on the aspects of computing methods, vision, architecture, challenges, and emerging technologies.
We evaluated these aspects at three levels (High (H), Medium (M), and Low (L)), depending on the levels at which they are mentioned in each study. Thus, we searched for articles using keywords such as Intelligent Healthcare/Medicine, Smart Healthcare/Medicine, Computing Technologies, and Emerging Technologies in electronic databases such as IEEE Xplore, ACM, ScienceDirect, Springer, and MDPI. Then, we evaluated the search results using three-step processing. In the first step, the searching step, we identified 450 related works. In the second step, we removed duplicate and inappropriate papers, and the remaining number of articles was 220. In the final step, we discarded papers from low-reputation journals and conferences, resulting in 95 papers, as presented in the References section.
Based on our survey results, we evaluated the studies based on criteria such as vision, architecture, challenges, and technology solutions, and outlined the key findings of each study. The details of the survey results are presented in Table 1.

Table 1.
Statistics of typical research in the smart healthcare domain in the period 2019–2022.
The survey results show that smart healthcare systems are receiving substantial attention from academia and industry. Smart healthcare applications use one of three computing solutions (CC [7,8,10,16], FC [12,14], or EC [21]) or a combination of solutions [9,11,14,15,17,20].
Some studies also point out visions [8,16], propose improved architectures [7,8,11,12,14,15,20,21], and point out the challenges in this domain [11,19,20].
One of the most important aspects is that of technological solutions. The survey results show that many possible technologies are integrated to enhance the capabilities of smart healthcare systems, including the IoT [10,19], AI [11,21], WBAN [8], and blockchain [11,16]. [22] reported, in a recent survey, on the application of IoT solutions to monitor the COVID-19 pandemic. The author found over 155 related works in this area. The survey results indicated that IoT technology can be applied to almost all stages, such as contact tracing, health monitoring, social distancing, diagnostics, and treatment.
Although some studies have integrated one or several technologies to improve the performance, energy efficiency, or privacy and security of smart healthcare systems, the latest survey results have shown that real-time responsiveness, privacy, and security remain significant challenges for smart healthcare systems.
In this study, we conduct a comprehensive survey of IoT-based medical and healthcare applications. We propose an all-in-one computing architecture for real-time healthcare applications and indicate application directions for the proposed architecture. Finally, we discuss some challenging aspects, open issues, and future research directions. The main contributions of this study are as follows:
- We comprehensively review several key Internet of Things-based medical and healthcare applications over the past three years to highlight possible research directions.
- We investigate the core technologies and emerging technologies that enable smart healthcare applications.
- We propose an all-in-one computing architecture to reduce service response time, computation costs, and energy consumption for real-time IoHT applications.
- We indicate application scenarios for the proposed architecture.
- Finally, we discuss challenges, open issues, and future research directions.
The rest of the paper is organized as follows: In Section 2, we consider core technologies for Internet of Health Things applications. Section 3 presents emerging breakout technologies for IoHT applications. In Section 4, we describe a full picture of the applications and use cases of IoT-based healthcare systems. We propose an all-in-one computing architecture for real-time smart healthcare systems in Section 5. Section 6 indicates challenges and some open issues. Finally, our conclusions are presented in Section 7.
2. Core Technologies for Smart IoHT Applications
Some advanced technologies and solutions have been researched, developed, and deployed in the smart healthcare field, such as smart sensors, autonomous devices, robots, intelligent computing solutions, and virtual reality. In this section, we present some advanced core technologies.
2.1. Smart Sensors
A smart sensor is a device that allows users to accurately and automatically collect data on physical and chemical changes in the area where the device is mounted. Intelligent sensors collect information with high accuracy.
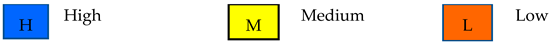
In this study, we focus on wearable sensors because of their universal applicability in IoHT applications. Wearable sensors can be embedded in clothing, implanted in the body, or worn on the wrist. In smart healthcare, devices collect patients’ vitals and transmit them to calculation servers via wired or wireless network connections. Many wearable products have been focused on development in recent years [23], such as smartwatches, wristbands, eyewear, headphones, earplugs, body straps, and devices worn on the hands and feet, as presented in Figure 1. In [24,25], the authors indicate feasible solutions to the application of wearable medical sensors by using varying smartphone sensors to detect anomaly data in healthcare areas.
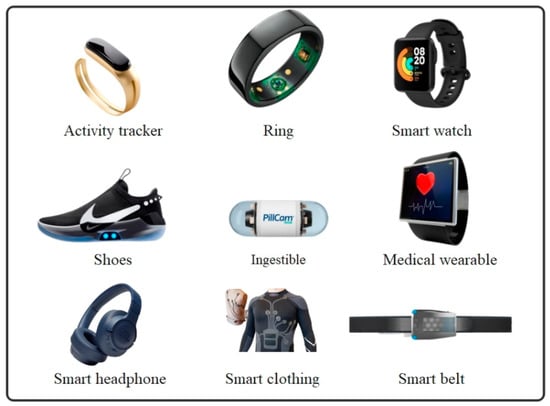
Figure 1.
An illustration of smart wearable healthcare sensors.
Sensors can be classified as wearable sensors, implantable sensors, etc. In the smart healthcare domain, wearables can be mainly used to measure and check patients’ activities and vitals to alert or provide data to healthcare systems from a distance. Some of the patient vitals that need to be monitored based on wearable sensors are as follows [26].
: A pulse sensor monitors the pulse in the human body, and can be used to monitor emergency conditions such as cardiac arrest and pulmonary embolism. The pulse signal can be installed in positions such as the wrist, earlobe, chest, fingertip, etc. Signals from the earlobe and fingertip locations are highly accurate, but placing the pulse sensors in these areas is difficult. Sensors placed in the wrist position are often more convenient and long-lasting.
: A respiratory rate sensor measures the respiratory rate, or the number of breaths of a patient per minute; it is used to monitor individuals with airway-related diseases such as asthma, lung cancer, respiratory failure, tuberculosis, etc.
: A body temperature sensor is used to measure a patient’s temperature. These sensors can read the appropriate temperature range to monitor the temperature of the human body. The accuracy of the body temperature sensor depends on the location of the human body.
: A blood pressure sensor is used to measure a patient’s blood pressure (BP). High blood pressure is a risk factor for cardiovascular disease. However, the accuracy of a blood pressure sensor depends on its measurement location. Since there is no precise BP measurement, several modalities have been proposed whereby two PPG optical sensors are located at different positions on the patient’s arm.
: An oxygen sensor measures the oxygen level in the blood. This is an important parameter to assist doctors in accurately diagnosing the amount of oxygen supplied to the body. However, due to the use of infrared LEDs, a major limitation of these sensors is their high power consumption. To solve this problem, measurement techniques based on the signal-to-noise ratio (SNR) and PLL [27] were proposed. The results showed that using this solution can save six times more energy than not using this solution.
Finally, the data collected from the sensors is transmitted to dedicated servers in different computing layers for processing, calculation, and storage to provide optimal intelligent medical services to patients. In the next section, we will discuss some of the advanced computing technologies in the IoHT domain.
2.2. Cloud, Fog, and Edge Computing
Cloud computing (CC) has existed for decades. One of the key unique characteristics that make CC successful is its ability to provide everything as a service, including software, infrastructure, and platforms. Over the years, power and flexibility have made CC the dominant computing technology for information and communication systems. The basic CC model consists of two layers: the cloud and end-users. The cloud layer includes servers with powerful configurations, high computing power, and large storage capacity. Cloud servers are connected to the Internet infrastructure via back bolt connections with extremely high throughput. The end-user layer includes end-users such as sensors, IoT devices, actuators, etc. These devices are connected to the cloud layer based on wired and wireless connections. Processing, computation, and storage all take place on cloud servers. One major limitation of CC is its high service response time. Therefore, it is not viable for emergency healthcare scenarios that require real-time computing power.
In recent years, to solve this problem, several computing models, such as fog computing (FC) [28] and edge computing (EC) [29], have been proposed. Figure 2 presents an all-in-one computing framework for IoT systems.
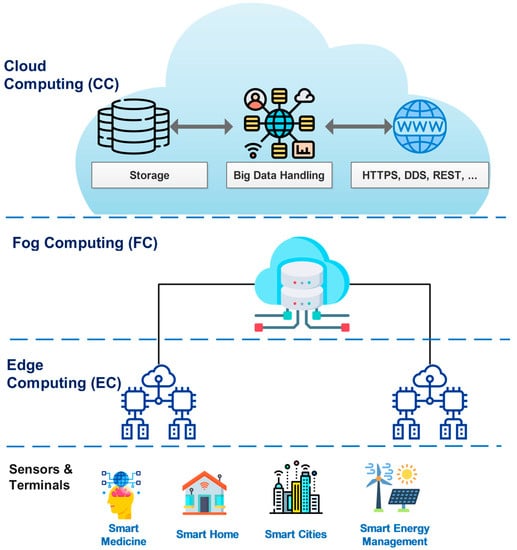
Figure 2.
An illustration of all-in-one computing architectures for IoT ecosystems [28].
Both FC and EC aim to bring database and cloud capabilities closer to the end devices. One key difference between EC and FC is their computational locations. While EC computation is integrated into devices, the edge server is set up in LAN, a few hops away from end devices; in contrast, FC computation is performed in the dedicated servers of data centers, set up from the Internet gateway to the cloud.
Each computing model has its advantages and disadvantages. CC has high computing power, but a considerable delay. EC and FC have low service response time, but inadequate computing and storage capacity. However, for each specific scenario and application, we can combine these technologies into an optimally integrated solution. To explain the capabilities of computing technologies, performance comparison studies are presented in Table 2.

Table 2.
Performance comparison between advanced computing technologies [28].
To collect patients’ vitals, each patient can carry a variety of sensors, depending on the type of disease and the indicators to be monitored. These sensors assist each other in data acquisition, communication, and the formation of Wireless Body Area Networks (WBANs). The issues with WBAN will be discussed in detail in the next section.
2.3. Wireless Body Area Networks (WBANs)
In smart healthcare, a WBAN is one of the most important core technologies. A WBAN is a set of intelligent IoT devices mounted on the human body to collect patient vitals and transmit this information to a data center for decision making. A WBAN works via wireless technology consisting of light and smart sensors attached to or implanted in the human body, measuring parameters such as heart rate, body temperature, blood glucose level, etc. These data are then visually provided to medical staff or caregivers to monitor and analyze the patient’s condition and devise appropriate treatment schemes [30].
The WBAN architecture consists of hardware, software, and communication technology. The hardware includes all devices and sensors used to collect patient data; the software consists of a man–machine interface, network protocols, and an operating system. In addition, communication technology in a WBAN plays a significant role in transmitting medical data between devices and software. Figure 3 illustrates the architecture of a typical WBAN system. Depending on the goals of each WBAN network, different communication technologies will be used. Table 3 compares the characteristics of some communication technologies of WBAN systems [31].
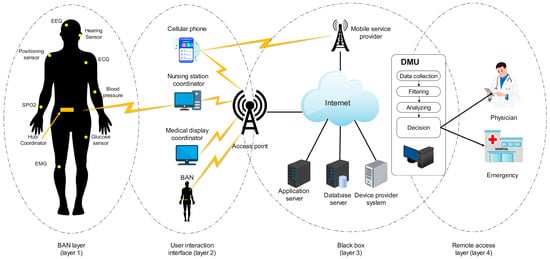
Figure 3.
An illustration of typical WBAN architecture [30].

Table 3.
A comparison of communication technologies for IoHT systems.
In recent years, to respond to more increasing requirements of humans in the smart healthcare domain. Besides existing core medical technologies, some emerging technologies are being researched and are expected to provide booming results, including the Metaverse, digital twins, and AI. In the next section, we will discuss detail these issues.
3. Emerging Technologies in Smart Healthcare
The COVID-19 pandemic has exposed the limitations of existing healthcare systems and created the concept of social distancing for the first time. These issues require a disruptive change in the smart healthcare sector. Therefore, AI, digital twins, and Metaverse technologies answer these demands. Recently, these technologies have received special attention from the research community and undergone several feasibility studies, which are summarized as follows.
3.1. Metaverse
The definition was created by writer Neal Stephenson in his science fiction novel in 1992 [32]. In this novel, Stephenson describes the Metaverse as a vast virtual environment that coexists with the physical world, in which humans interact through digital avatars. A is a shared three-dimensional space in which users can perform all actions through virtual reality technologies such as AR, MR, and VR [33], as presented in Figure 4.

Figure 4.
An illustration of Metaverse technology.
Nowadays, the Metaverse is described as the future of the Internet. In [34], the authors showed the vision of Metaverse developments in the medical domain, including telemedicine, clinical treatment, medical training, mental health, fitness, medicine, and pharmacy. Despite its advantages, a series of challenges must be addressed before the Metaverse can be widely adopted. We summarize the key challenges of Metaverse technology in Table 4.

Table 4.
Challenges facing Metaverse technology.
: The Metaverse relies on virtual reality technologies. These technologies require the processing of a huge amount of data with high computing costs and real-time service response. Hence, the hardware should be designed to be smart, flexible, and smaller at a more affordable cost. These will be significant challenges for the popular Metaverse [35].
: Several studies have shown that the collection and processing of data from users can compromise their data privacy and security [36,37]. In our opinion, the guarantee of privacy and security is one of the most crucial conditions in realizing the Metaverse, especially in the healthcare domain. If privacy and security issues are unguaranteed, they could lead to real-world disasters.
: In the Metaverse, clones can be hijacked (i.e., identity theft), and then, the hijackers can perform illegal actions, spread fake information, or steal users’ identities. Consequently, actions taken in the virtual world can have real consequences for humans in the real world [38].
: The Metaverse allows humans to interact with their friends through their avatars, and attend virtual events. Consequently, humans are becoming further and further away from real life, which can lead to health problems and neurological diseases [35,39].
: The Metaverse is more than an entertainment platform. It will be a global online marketplace with billions of users, where users can use currencies and cryptocurrencies to make payments or perform fast and smooth transactions. However, ensuring the security of e-commerce transactions will be a significant challenge [35].
: The development of the Metaverse will require the formation of new legal and policy concepts with the concepts of virtual citizens, virtual crimes, and virtual and flat worlds. Blocking a user account will not be enough to prevent illegal acts. Instead, new legal policies need to be announced to manage the Metaverse world [35].
Despite the dozens of challenges presented above, in our opinion, it is inevitable that the Metaverse will become a trend in development. Nowadays, research on the Metaverse is only at a primitive level, so we will need much breakthrough research in the future to realize the Metaverse concept in the medical domain, as well as in public life.
3.2. Digital Twins
Digital Twin technology is a combination of virtual reality technology, big data processing, and 3D graphics to build virtual models of processes, systems, services, products, or physical objects [40]. Through digital twin technology, users can experience virtual effects, identify problems before they happen, or predict future outcomes.
In the healthcare domain, digital twin technology is considered to be revolutionary and is applied in the prediction and early diagnosis of diseases that may occur in patients by examining organs or symptoms in the body. In the case of atherosclerosis, it can be used to perform vascular surgery to restore blood flow, replace the lenses of cataract patients, transplant organs, etc. [41]. A patient’s digital twin is created as a result of transferring the physical characteristics and changes in the patient’s body to a digital environment. This technology enables accurate diagnosis and delivers tailored treatment protocols in real time to patients. Figure 5 presents an illustration of digital twins in the healthcare domain.
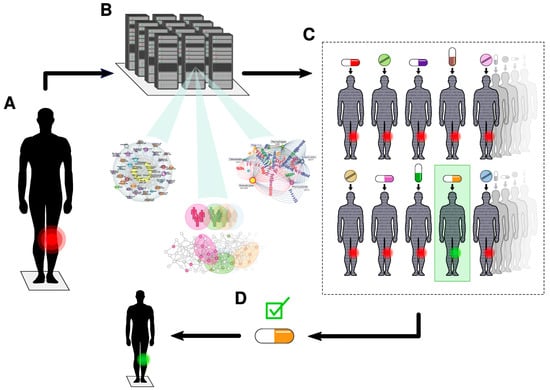
Figure 5.
An illustration of digital twin technology.
In our opinion, digital twins can be extensively applied in the smart healthcare domain in the future. For example, before physical interventions such as drug treatment, radiation therapy, or surgical operations, paramedics can perform processes on virtual digital twins to determine the optimal treatment for the patient. By creating a digital twin of the patient’s body, doctors can perform a diagnosis by examining the vital areas of the patient’s digital twin without a direct impact on the patient’s body. With the creation of digital twins of medical devices, the prediction and coordination of medical resources for medical examination and treatment have high accuracy and optimization of system resources.
3.3. Artificial Intelligence
Smart healthcare requires the use of a large number of IoT devices and smart sensors to collect data continuously from patients. Handling these huge amounts of data requires advanced data processing technologies. AI technology is the answer to these problems [42].
In reality, AI has existed for decades. AI is the ability to equip machines with human intelligence. Today, AI is applied in almost all intelligent applications that serve humans, from cleaning robots [43] to military weapons systems [44]. In the smart healthcare domain, AI contributes to all stages, including early diagnosis, disease identification, and treatment [45,46]. To suit different intelligent applications, a series of improved AI techniques have been proposed, including ML, DL [47], RL [48], and DRL [49].
It is notable that that traditional AI techniques use centralized data management, whereby data are centrally managed on servers for training. The aggregator then uses these data to train and create optimal models. However, in smart healthcare, due to the sensitivity of medical data, ensuring the privacy of patient data is one of the issues of particular concern. Therefore, it is impossible to manage patient data for AI training centrally.
In our opinion, distributed learning techniques should be considered; training should be implemented on patients’ IoT devices. This will not cause privacy issues regarding medical data; moreover, it will not put pressure on backbone links by transferring all patient data to training servers.
The purpose of AI in healthcare is to determine the relationship between patients’ information and a fitting treatment approach [50,51]. Varying AI techniques have been applied to different disease scenarios. In [52], the authors propose an AI-based recognition and image diagnostic solution. In [53], the authors propose an AI-based remote sensing image retrieval algorithm by improving the Sobel method. In [54], the authors propose an AI-based data dimension-reducing algorithm to handle big data applications that have large-scale and high-dimensional to perform criminal detection or solve smart city problems. In [55,56], the authors propose DL technique-based image diagnosis algorithms for handling fault images.
In the drug medicine domain, patient monitoring supports doctors in their decision making regarding the personalization of treatment and prescriptions [57]. Moreover, AI-based systems also support doctors in seeking related medical information from online libraries, magazines, and textbooks [58], and in the storage of medical data via cloud solutions for convenient access. In [59], the authors present a comprehensive survey of FL-based IoHT applications where patients will obtain complete medical support throughout their lives. The authors also indicate that AI can be combined with most healthcare units, including emergency medical units, medical staff, diagnostics, laboratories, and pharmacies.
Figure 6 shows that AI can be integrated with most healthcare systems to provide optimal solutions. AI can assist a patient from the moment they are admitted to the hospital through integration into emergency medical applications, process patient data, detect serious illnesses, automatically identify complex samples, and analyze complete human and patient molecular data in a clinical setting. AI can assist doctors and medical staff through highly accurate clinical reports and provide many other decision-support tools. AI effectively supports optimal treatment decision making for patients. Recent studies demonstrate that AI strongly assists in detecting cancer at an early stage.
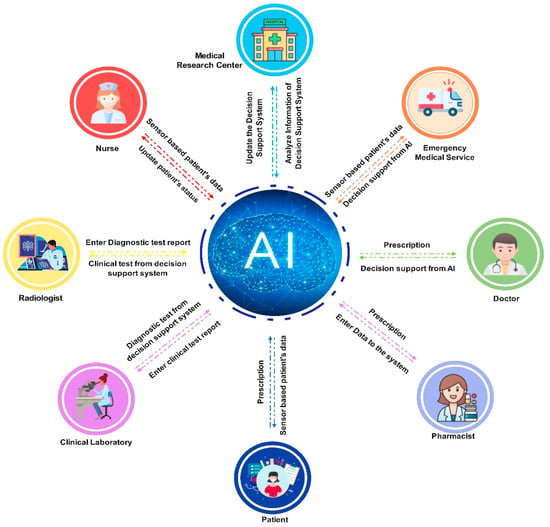
Figure 6.
An illustration of AI-based smart health systems.
3.4. Blockchain
In the Internet of Things era, smart devices, sensors, and IoT applications are connected to others based on the Internet infrastructure. This leads to real challenges regarding IoT applications in terms of privacy and security. Indeed, attackers can illegally access and hijack the system or steal data through the security vulnerabilities of IoT devices [60], operating systems [61], Internet gateways [62], remote computing servers [63], or denial of service (DDOS) attacks [64]. In the smart IoHT domain, medical data records play a particularly crucial role and are sensitive [65].
In reality, blockchain technology is an advanced database management mechanism that enables transparent information sharing across a distributed network environment. Data are stored in blocks that are linked together in a consistent chronological sequence. Hence, the user cannot delete or modify the chain without the consensus of all users. As a result, blockchain technology creates an immutable ledger that keeps track of data records [66]. In the smart IoHT domain, blockchain technology is applied to ensure privacy and security in managing patient medical records. In recent years, integrating blockchain into healthcare applications has attracted strong interest from the academic community and achieved some positive results. In [67], to enhance privacy and security, the authors integrated blockchain into MEC-based IoT applications. To solve the delay caused by blockchain, they used a lightweight block verification algorithm. To ensure a suitable edge environment, they also applied a novel DRL-based AI technique. Their results showed that the proposed scheme significantly improved performance, privacy, and security compared to existing solutions. In [68], the authors designed a novel secure mobile edge computing framework for healthcare systems, namely BEdgeHealth. Indeed, they integrated blockchain into MEC-IoHT systems to enhance privacy and security for health data record-sharing and improve QoS. The real-world evaluation results showed that compared to existing computing solutions, the BEdgeHealth framework robustly improved QoS, privacy, and security.
In our opinion, IoHT applications will be impossible if privacy and security are not guaranteed, and blockchain technology is the key to solving this problem. Figure 7 presents an illustration of Blockchain-based smart health systems.
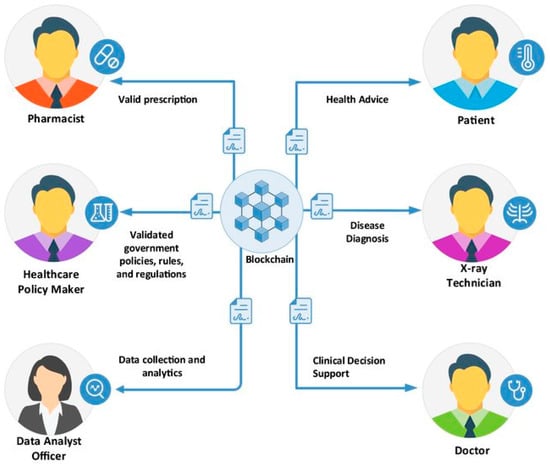
Figure 7.
An illustration of blockchain-based smart health systems.
4. IoT-Based Smart Healthcare Systems
In this section, we present IoT-based smart healthcare systems. Based on our survey results, we divided these applications into four different approaches based on the objectives of the studies, as modeled in Figure 8 and statistically in Table 5.
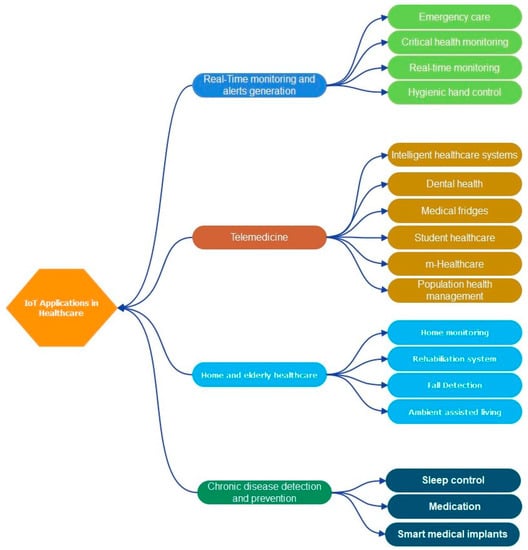
Figure 8.
IoT-based smart healthcare systems.

Table 5.
Summary of typical research results of recent IoHT Applications.
4.1. Real-Time Monitoring and Alarm Generation
Monitoring health metrics such as temperature, heart rate, and blood oxygen is critical to delivering real-time healthcare services. Through the IoT, sensors are attached to the human body and measure various indicators, which are then analyzed to recommend drugs for the emergency treatment of patients. [69] developed an electronic medical system that monitors electrocardiograms, temperature, foot pressure, and heart rate. This system determines the patient’s GPS location to provide urgent care, and uses to identify each patient, the mainboard as the microcontroller, and as the middleware for medical signal handling. [70] proposed a real-time IoHT system that relies on the platform and some sensor types, such as and sensors, to monitor blood pressure or heart rate. [71] designed a real-time IoHT application that relies on and the platforms to handle big data and aims to reduce response time. Their experimental results demonstrated the effectiveness of the proposed solution in handling the big data of smart cities or countries.
4.2. Telemedicine
Telemedicine allows for the provision of remote medical services and relies upon Internet infrastructure and communication technologies. Overall, these enhance the response capacities of medical services and staff, improve patients’ health, and reduce treatment costs. In [72], Zouka et al. introduced an AI-based IoHT system to analyze collected data from medical devices mounted on patients’ bodies. The information collected from medical sensors is transferred through the GSM system to the Azure data center for data handling and decision making. In [73], Rohokale et al. designed a novel IoHT system for rural residents by monitoring their main survival indicators. The patients wore an RFID tag for identification.
When patients’ vital indicators, such as blood pressure and heart rate, have abnormal changes, the IoHT system will generate alarms, and then, send them to doctors, hospitals, or caregivers. Mohammed et al. [74] designed an IoHT system for remote patient monitoring by combining web services and cloud computing-based solutions. Indeed, the authors developed an ECG Android App to monitor the electrocardiogram indicators of patients. The obtained signals are transferred to Microsoft’s Azure platform for handling. Moreover, they also used a hybrid cloud, where patients’ sensitive medical records are pushed into private clouds, and general medical information is pushed into public clouds.
4.3. Chronic Disease Detection and Prevention
A massive number of patients face serious diseases such as heart disease, diabetes, cancer, etc., which then cause depression in patients. To solve this problem, Sundhara Kumar et al. [75] designed an IoHT system to monitor autistic patients. The application measures and collects EEG waveform signals through neural sensors, and then, alerts are sent to caregivers in case any abnormal results are detected. [76] have proposed different architectures and frameworks that support IoT-based healthcare solutions for cancer patients. The focus is on cloud services, which use big data technology to analyze data over the air. Sood et al. [77] designed an IoHT system to monitor the chikungunya virus pandemic. The system uses medical sensors to collect medical information, and then, the system transfers this information to a private cloud. From there, fog computing methods combine fuzzy logic systems and aim to detect the possibility of infection in patients and immediately alert hospitals and caregivers. Sensitive medical records related to the patients’ information is pushed into the private cloud for privacy and security.
4.4. Home Healthcare and Healthcare for the Elderly
IoT and reality technologies can be deployed at home to continuously monitor elderly people who move slowly and take longer to arrive at the hospital for routine or urgent health care services. [78] proposed a life support health monitoring system. Indeed, the authors used varying sensor types to collect medical signals, and then, the information was transferred to the cloud infrastructure for handling and big data analyses. Additionally, they also designed a prototype to prove the effectiveness of the proposed solution. This system consists of six medical sensor types: a Bluetooth-based communication module, a Raspberry Pi-based microprocessor, and a Wi-Fi-based communication module. All the medical signals are stored in cloud infrastructure.
[79] proposed a system of individualized health care for people who live alone and use wheelchairs. The system combines IoT technology and WBAN technology to provide efficient medical solutions for wheelchair patients by monitoring real-time heart rate, ECGs, blood pressure, and environmental indicators. Cerina et al. [80] presented a new method for patient health monitoring using IoT technologies. Patients are fitted with medical sensors to monitor ECGs and survival indicators, and then, this medical signal is transferred to cloud servers that rely upon wireless links.
The IoHT systems analyzed above have varying requirements. Some IoHT systems have no service response time. Contrarily, others have strict requirements for service response time. The computing architectures directly affect the system performance. In the next section, we will discuss several recent existing computing architectures for IoHT systems.
5. Proposed Architecture for IoT Healthcare Application
Some conditions are significant and need to be treated promptly, such as cardiovascular diseases or conditions that occur in patients following dangerous accidents that affect their lives. Such situations require fast real-time action with minimal delay. In a general cloud environment, data are transmitted to the cloud, processed in the cloud, and receive a response, which takes a long time and involves considerable delays. To overcome or limit latency issues, we can use fog computing, which brings computing devices and storage resources closer to the edge of the network. Most current healthcare solutions use the cloud’s decision-making environment. In recent years, many other proposed solutions have considered fog computing for healthcare applications where the time factor is of interest. Some architectures for existing solutions are shown in Table 6.

Table 6.
A comparison of the existing IoHT architectures.
According to our survey results, traditional three-layer architectures are presented for IoHT applications in [20,83,85,86,87,88,89,90], including the sensor, fog, and cloud layers. The use of techniques to increase the security of identity management, user authentication [86,88,90,91], or the application of emerging technologies in healthcare, such as AI, WBAN, big data, and blockchain [86], is recommended by the authors.
The authors of [81,91] use a four-layer architecture based on FC to support healthcare, namely the physical, boundary, fog, and cloud layers.
[82] proposed a five-layer FC architecture for remote patient health monitoring that includes data acquisition, event classification, information mining, decision making, and cloud storage layers. Another study also proposed a five-layer computing architecture that includes sensing, transport, processing, application, and business layers [14]. Our survey results show that integrating various computing solutions with CC reduces service response time and realizes real-time smart healthcare applications. However, one limitation of the existing proposals is that there needs to be a fully integrated architecture framework for all existing solutions in the smart healthcare domain.
In this study, we propose a fully integrated architectural framework for computing solutions for IoT-based healthcare applications to optimize service response time, compute costs, and realize real-time smart healthcare applications, as shown in Figure 9.
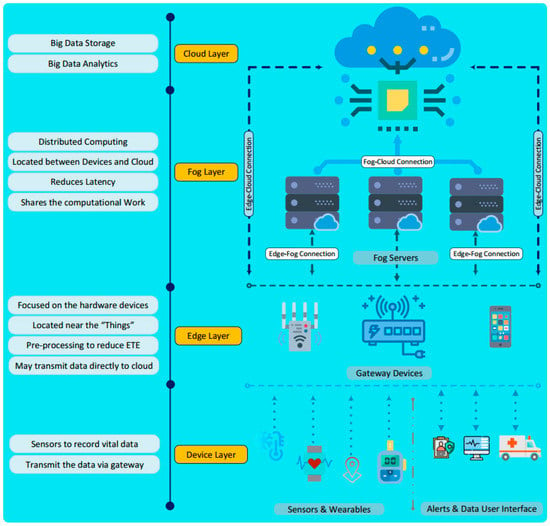
Figure 9.
The all-in-one computing architecture for IoT-based smart healthcare applications.
The proposed architecture includes four layers (the things layer, edge computing, fog computing, and cloud computing), where the things layer includes smart IoT devices, health sensors, actors, ambulances, etc. The main task of this class is to collect medical data and patient vitals in real time. The collected data are sent to local server nodes based on wired or wireless connections and communication technologies for EC.
The edge nodes are deployed in the LANs of hospitals or patient treatment places. As a result, computation is performed closest to the end-users, minimizing transmission delays, reducing data load on backbone connections, and improving computing performance. Depending on the processing results, the results can be sent directly to doctors, families, and emergency services (notification module) or sent to higher calculation layers for further processing.
The FC layer is operated by computing servers that are deployed at cloud gateways or computing service centers, also known as cloudlets. The data sent up from the lower layers are analyzed, processed, and aggregated via FC. Although FC’s transmission delay is higher than EC’s, FC’s storage and computing capacity are better than EC’s. As a result, FC can handle more complex problems than EC. Like EC, FC’s results can be sent directly to the message module or sent to the CC for further processing.
Instead of performing computations like traditional solutions, the CC layer in this architecture will receive the results from the FC layer and analyze and store the data to perform big data computation tasks, such as statistics and disease diagnosis, in the medical domain.
A comparison with existing computing architectures is presented in Table 6. Our architecture has many outstanding advantages. The parameters were considered to compare the different architectures of the layers, the architectures’ complexity, the data’s reliability in the fog layer, the real-time application support, and the security. The values for the selected parameters can be any of the following: low, moderate, or high. The value for complexity was chosen based on the classes and the function or module implemented in each class. The value for the reliability of the data in the fog layer was chosen based on the availability of clusters or distributed computers in the fog layer. No existing architecture emphasizes data reliability in the fog layer, which is a major concern for urgent care applications. The value for the real-time support application was selected based on the existence of the fog layer and the amount of work performed in this layer. Finally, security issues in the layers were taken care of. Most of the previous jobs should have emphasized the security of the architecture.
The use of the IoT as a technology in healthcare is still in its infancy. Therefore, there are still many challenges that need to be addressed by the research community and industry. Some of the existing challenges and solutions are discussed in the next section.
6. Challenges and Open Issues
Nowadays, smart healthcare systems are growing explosively, in both number and scale, due to increasing human needs. Despite the the positively achieved results, smart healthcare systems face several challenges [92]. In this section, we discuss some important challenges, such as issues with fault tolerance, latency, power efficiency, interoperability, and availability, as presented in Figure 10.
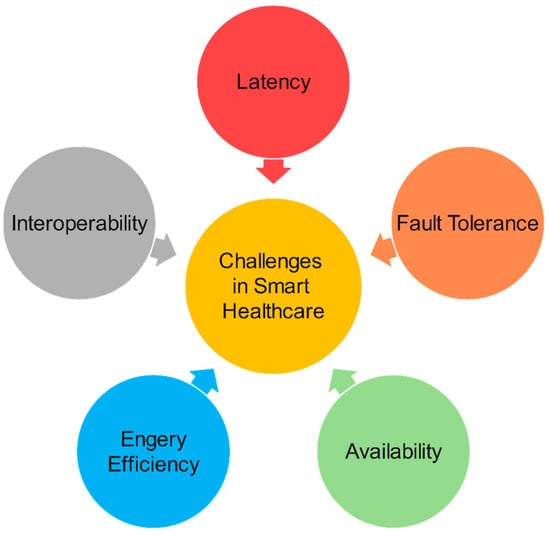
Figure 10.
Challenges in smart healthcare.
: The reliability of an IoT-based healthcare system is affected by the operation of the sensors and communication nodes that pass data onto the computational layers above. Reliability is one of the most important elements of a smart healthcare system, especially in emergency scenarios. In [93], the authors proposed a method of using redundant IoT nodes to improve the fault tolerance of the system.
: The lag time of smart healthcare applications directly affects the quality of medical services. The main factors affecting delay time are transmission delay in the network layer and delay due to the computation and processing of services. Each type of smart healthcare application has different latency QA requirements. In [93], the authors proposed a computational architecture framework based on FC to reduce the delay time.
: The health IoT sensors or devices in health apps use batteries, so energy-efficient solutions should be considered. Moreover, extending the lifetime of these devices also directly affects the reliability and fault tolerance of the system, especially in emergency medical scenarios [88]. To solve this problem, in [94], the authors proposed using renewable energy sources such as solar energy to power IoT devices and smart sensors.
: The rapid growth, in both scale and number, of smart healthcare systems requires devices to interact and communicate with others in a flexible and customizable manner. This requires policymakers to quickly develop standards for connectivity, communication, and security. Currently, several standards have been proposed to standardize the healthcare domain, such as the 6LoWPAN communication protocol [95]. In our opinion, the interoperability of health devices should further focus on tackling the many threats and security vulnerabilities of the IoT era.
: Another important challenge facing the IoT in general and the IoT in healthcare is security and privacy. Due to the limited resources of IoT devices, it is not feasible to implement robust security algorithms on IoT devices. In addition, health IoT devices collect large amounts of medical data that require security and privacy. If security and privacy are not ensured, the dissemination of smart healthcare systems is not feasible. Therefore, the study of lightweight security algorithms could represent a solution to these problems.
Moreover, integrating AI into the edge of networks is a possible direction for diagnosis and treatment. However, the AI training process requires powerful servers, while edge devices have limited resources; hence, approaches using lightweight AI techniques and federated learning models need to be studied. Additionally, the Metaverse and digital twins are expected to be breakthrough technologies in smart healthcare; however, due to the potential dangers to security and privacy, IoHT systems face a series of real challenges. We think that the integration of cryptographic algorithms of blockchain technology could be the key to this problem.
In our opinion, despite the dozens of challenges that still need to be addressed, smart healthcare will be an inevitable development trend in the era of the Internet of Things, and will serve to fulfil the increasing needs of people in the healthcare domain.
7. Conclusions
The field of IoT-based smart healthcare systems is rapidly expanding, but there are still several challenges that need to be addressed. This study presented a comprehensive survey of core technologies for smart healthcare and various computing technologies, including CC, FC, and EC. Recent studies have shown that powerful advances and integrated solutions to realizing real-time smart healthcare applications are gradually being developed. We proposed an all-in-one computing architecture framework for real-time smart healthcare applications, highlighting the advantages and challenges of the proposed architecture. A limitation of this study is that the effectiveness of the proposed computing framework is still fully evaluating yet. This aspect will be assessed by our research group in a future study. Despite these challenges, the future of medicine lies in real-time smart healthcare systems. Emerging technologies, such as the Metaverse, digital twins, and AI, will be key drivers in revolutionizing smart healthcare to serve humanity’s healthcare needs. We hope that this study will serve as an important guide and promote further research into smart healthcare in the Internet of Things era.
Author Contributions
Conceptualization, V.A.D., Q.V.K. and D.C.N.; methodology, V.A.D., Q.V.K., V.-H.N., T.N. and D.C.N.; software, V.A.D. and T.N.; validation, V.A.D., Q.V.K., V.-H.N. and D.C.N.; formal analysis, V.A.D., Q.V.K., V.-H.N., T.N. and D.C.N.; investigation, Q.V.K., V.-H.N. and D.C.N.; resources, V.A.D. and Q.V.K.; data curation, Q.V.K., V.-H.N., T.N. and D.C.N.; writing—original draft, V.A.D. and Q.V.K.; writing—review and editing, Q.V.K., V.-H.N. and D.C.N.; visualization, V.A.D., Q.V.K., V.-H.N. and D.C.N.; supervision, Q.V.K. and D.C.N.; project administration, Q.V.K. and D.C.N.; funding acquisition, Q.V.K. and D.C.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not Applicable.
Data Availability Statement
Not Applicable.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Abbreviations
| Abbr. | Definition | Abbr. | Definition |
| 6LoWPAN | IPv6 over Low-Power Wireless Personal Area Networks | GUI | Graphical user interface |
| AI | Artificial intelligence | IoHT | Internet of Healthcare Things |
| AR | Augmented reality | IoMT | Internet of Medical Things |
| BLE | Bluetooth Low Energy | IoT | Internet of Things |
| BP | Blood pressure | LAN | Local area network |
| CC | Cloud computing | M2M | Machine-to-machine |
| DL | Deep learning | ML | Machine learning |
| DRL | Deep reinforcement learning | MEC | Mobile edge computing |
| EC | Edge computing | Pi2 | Portrait innovations photo |
| ECG | Electrocardiogram | PLL | Phase-locked loops |
| EEG | Electroencephalogram | QA | Quality assurance |
| e-Health | Electronic health | RFID | Radio frequency identification |
| EMS | Emergency Medical Service | RL | Reinforcement learning |
| FBIS | Foreign Broadcast Information Service | SNR | Signal-to-noise ratio |
| FC | Fog computing | VR | Virtual reality |
| FL | Federated learning | WBAN | Wireless Body Area Network |
| GPS | Global Positioning System | WBSN | Wireless Body Sensor Network |
| GSM | Global System for Mobile Communication | WSN | Wireless Sensor Network |
References
- Nguyen, D.C.; Pathirana, P.N.; Seneviratne, A.; Zomaya, A.Y. Federated Learning for COVID-19 Detection with Generative Adversarial Networks in Edge Cloud Computing. IEEE Internet Things J. 2022, 9, 10257–10271. [Google Scholar] [CrossRef]
- Quy, V.K.; Van-Hau, N.; Quy, N.M.; Anh, D.V.; Ngoc, L.A.; Chehri, A. An Efficient Edge Computing Management Mechanism for Sustainable Smart Cities. Sustain. Comput. Inform. Syst. 2023, 37, 100867. [Google Scholar] [CrossRef]
- Mukherjee, M.; Shu, L.; Wang, D. Survey of Fog Computing: Fundamental, Network Applications, and Research Challenges. IEEE Commun. Surv. Tutor. 2018, 20, 1826–1857. [Google Scholar] [CrossRef]
- Abbas, N.; Zhang, Y.; Taherkordi, A.; Skeie, T. Mobile Edge Computing: A Survey. IEEE Internet Things J. 2018, 5, 450–465. [Google Scholar] [CrossRef]
- Statista. Available online: https://www.statista.com/statistics/471264/iot-number-of-connected-devices-worldwide (accessed on 1 February 2023).
- Vodafone. Available online: https://www.vodafone.com/business/news-and-insights/white-paper/global-trends-barometer-2019 (accessed on 1 February 2023).
- Mahmoud, M.M.E.; Rodrigues, J.J.P.C.; Saleem, K. Cloud of Things for Healthcare: A Survey from Energy Efficiency Perspective. In Proceedings of the International Conference on Computer and Information Sciences (ICCIS), Sakaka, Saudi Arabia, 3–4 April 2019; pp. 1–7. [Google Scholar] [CrossRef]
- Habibzadeh, H.; Dinesh, K.; Rajabi Shishvan, O.; Boggio-Dandry, A.; Sharma, G.; Soyata, T. A Survey of Healthcare Internet of Things (HIoT): A Clinical Perspective. IEEE Internet Things J. 2020, 7, 53–71. [Google Scholar] [CrossRef] [PubMed]
- Alshehri, F.; Muhammad, G. A Comprehensive Survey of the Internet of Things (IoT) and AI-Based Smart Healthcare. IEEE Access 2021, 9, 3660–3678. [Google Scholar] [CrossRef]
- John Dian, F.; Vahidnia, R.; Rahmati, A. Wearables and the Internet of Things (IoT), Applications, Opportunities, and Challenges: A Survey. IEEE Access 2020, 8, 69200–69211. [Google Scholar] [CrossRef]
- Qadri, Y.A.; Nauman, A.; Zikria, Y.B.; Vasilakos, A.V.; Kim, S.W. The Future of Healthcare Internet of Things: A Survey of Emerging Technologies. IEEE Commun. Surv. Tutor. 2020, 22, 1121–1167. [Google Scholar] [CrossRef]
- Ullah, A.; Azeem, M.; Ashraf, H.; Alaboudi, A.A.; Humayun, M.; Jhanjhi, N. Secure Healthcare Data Aggregation and Transmission in IoT- A Survey. IEEE Access 2021, 9, 16849–16865. [Google Scholar] [CrossRef]
- Malamas, V.; Chantzis, F.; Dasaklis, T.K.; Stergiopoulos, G.; Kotzanikolaou, P.; Douligeris, C. Risk Assessment Methodologies for the Internet of Medical Things: A Survey and Comparative Appraisal. IEEE Access 2021, 9, 40049–40075. [Google Scholar] [CrossRef]
- Bhatia, H.; Panda, S.N.; Nagpal, D. Internet of Things and its Applications in Healthcare-A Survey. In Proceedings of the International Conference on Reliability, Infocom Technologies and Optimization (Trends and Future Directions) (ICRITO), Noida, India, 4–5 June 2020; pp. 305–310. [Google Scholar] [CrossRef]
- Amin, S.U.; Hossain, M.S. Edge Intelligence and Internet of Things in Healthcare: A Survey. IEEE Access 2021, 9, 45–59. [Google Scholar] [CrossRef]
- Adavoudi Jolfaei, A.; Aghili, S.F.; Singelee, D. A Survey on Blockchain-Based IoMT Systems: Towards Scalability. IEEE Access 2021, 9, 148948–148975. [Google Scholar] [CrossRef]
- Dong, Y.; Yao, Y.D. IoT Platform for COVID-19 Prevention and Control: A Survey. IEEE Access 2021, 9, 49929–49941. [Google Scholar] [CrossRef] [PubMed]
- Taimoor, N.; Rehman, S. Reliable and Resilient AI and IoT-Based Personalised Healthcare Services: A Survey. IEEE Access 2022, 10, 535–563. [Google Scholar] [CrossRef]
- Barua, A.; A1 Alamin, M.A.; Hossain, M.S.; Hossain, E. Security and Privacy Threats for Bluetooth Low Energy in IoT and Wearable Devices: A Comprehensive Survey. IEEE Open J. Commun. Soc. 2022, 3, 251–281. [Google Scholar] [CrossRef]
- Aledhari, M.; Razzak, R.; Qolomany, B.; A1-Fuqaha, A.; Saees, F. Biomedical IoT: Enabling Technologies, Architectural Elements, Challenges, and Future Directions. IEEE Access 2022, 10, 31306–31339. [Google Scholar] [CrossRef]
- Ali, M.; Naeem, F.; Tariq, M.; Kaddoum, G. Federated Learning for Privacy Preservation in Smart Healthcare Systems: A Comprehensive Survey. IEEE J. Biomed. Health Inform. 2023, 27, 778–789. [Google Scholar] [CrossRef]
- Andročec, D. Using Internet of Things to Tackle Covid-19: A Systematic Review. In Proceedings of the 2021 IEEE 3rd Eurasia Conference on Biomedical Engineering, Healthcare and Sustainability (ECBIOS), Tainan, Taiwan, 28–30 May 2021; pp. 230–233. [Google Scholar] [CrossRef]
- Seneviratne, S.; Hu, Y.; Nguyen, T.; Lan, G.; Khalifa, S.; Thilakarathna, K.; Hassan, M.; Seneviratne, A. A Survey of Wearable Devices and Challenges. IEEE Commun. Surv. Tutor. 2017, 19, 2573–2620. [Google Scholar] [CrossRef]
- Krichen, M. Anomalies Detection Through Smartphone Sensors: A Review. IEEE Sens. J. 2021, 21, 7207–7217. [Google Scholar] [CrossRef]
- Majumder, S.; Deen, M.J. Smartph 25one Sensors for Health Monitoring and Diagnosis. Sensors 2019, 19, 2164. [Google Scholar] [CrossRef]
- Baker, S.B.; Xiang, W.; Atkinson, I. Internet of Things for Smart Healthcare: Technologies, Challenges, and Opportunities. IEEE Access 2017, 5, 26521–26544. [Google Scholar] [CrossRef]
- Gubbi, S.V.; Amrutur, B. Adaptive Pulse Width Control and Sampling for Low Power Pulse Oximetry. IEEE Trans. Biomed. Circuits Syst. 2015, 9, 272–283. [Google Scholar] [CrossRef] [PubMed]
- Quy, V.K.; Hau, N.V.; Anh, D.V.; Ngoc, L.A. Smart Healthcare IoT Applications Based on Fog Computing: Architecture, Applications and Challenges. Complex Intell. Syst. 2022, 8, 3805–3815. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Chen, C.; Khosravi, M.R.; Pei, Q.; Wan, S. UAV-Assisted Vehicular Edge Computing for the 6G Internet of Vehicles: Architecture, Intelligence, and Challenges. IEEE Commun. Stand. Mag. 2021, 5, 12–18. [Google Scholar] [CrossRef]
- Al_Barazanchi, I.; Shibghatullah, A.S.; Selamat, S.R. A New Routing Protocols for Reducing Path Loss in Wireless Body Area Network (WBAN). J. Telecommun. Electron. Comput. Eng. 2017, 9, 93–97. [Google Scholar]
- Khan, M.; Jilani, M.T.; Khan, M.K.; Bin Ahmed, M. A security framework for wireless body area network based smart healthcare system. Ceur. Workshop Proc. 2017, 1852, 80–85. [Google Scholar]
- Abbate, S.; Centobelli, P.; Cerchione, R.; Oropallo, E.; Riccio, E. A first bibliometric literature review on Metaverse. In Proceedings of the IEEE Technology and Engineering Management Conference (TEMSCON EUROPE), Izmir, Turkey, 25–29 April 2022; pp. 254–260. [Google Scholar] [CrossRef]
- Ning, H.; Wang, H.; Lin, Y.; Wang, W.; Dhelim, S.; Farha, E.; Ding, J.; Daneshmand, M. A survey on metaverse: The state-of-the-art, technologies, applications, and challenges. arXiv 2021, arXiv:2111.09673. [Google Scholar] [CrossRef]
- Bansal, G.; Rajgopal, K.; Chamola, V.; Xiong, Z.; Niyato, D. Healthcare in Metaverse: A Survey on Current Metaverse Applications in Healthcare. IEEE Access 2022, 10, 119914–119946. [Google Scholar] [CrossRef]
- Xi, N.; Chen, J.; Gama, F.; Riar, M.; Hamari, J. The challenges of entering the metaverse: An experiment on the effect of extended reality on workload. Inf. Syst. Front. 2022, 25, 659–680. [Google Scholar] [CrossRef]
- Chen, D.; Zhang, R. Exploring research trends of emerging technologies in health metaverse: A bibliometric analysis. SSRN Electron. J. 2022, 5, 1–32. [Google Scholar] [CrossRef]
- Zhao, R.; Zhang, Y.; Zhu, Y.; Lan, R.; Hua, Z. Metaverse: Security and Privacy Concerns. arXiv 2022, arXiv:2203.03854. [Google Scholar] [CrossRef]
- Slater, M.; Gonzalez-Liencres, C.; Haggard, P.; Vinkers, C.; Gregory-Clarke, R.; Jelley, S.; Watson, Z.; Breen, G.; Schwarz, R.; Steptoe, W.; et al. The Ethics of Realism in Virtual and Augmented Reality. Front. Virtual Real. 2020, 1, 1. [Google Scholar] [CrossRef]
- Laijawala, V.; Aachaliya, A.; Jatta, H.; Pinjarkar, V. Classification Algorithms based Mental Health Prediction using Data Mining. In Proceedings of the International Conference on Communication and Electronics Systems (ICCES), Coimbatore, India, 21–22 October 2020; pp. 1174–1178. [Google Scholar] [CrossRef]
- Erol, T.; Mendi, A.F.; Doğan, D. The Digital Twin Revolution in Healthcare. In Proceedings of the International Symposium on Multidisciplinary Studies and Innovative Technologies (ISMSIT), Istanbul, Turkey, 22–24 October 2020; pp. 1–7. [Google Scholar] [CrossRef]
- Greenbaum, D.; Lavazza, A.; Beier, K.; Bruynseels, K.; Santoni De Sio, F.; Van Den Hoven, J. Digital Twins in Health Care: Ethical Implications of an Emerging Engineering Paradigm. Front. Genet. 2018, 9, 31. [Google Scholar] [CrossRef]
- Lu, M. AI-based tank truck cleaning robot. In Proceedings of the IEEE International Conference on Advances in Electrical Engineering and Computer Applications (AEECA), Dalian, China, 20–21 August 2022; pp. 1197–1202. [Google Scholar] [CrossRef]
- Zhang, Y.; Dai, Z.; Zhang, L.; Wang, Z.; Chen, L.; Zhou, Y. Application of Artificial Intelligence in Military: From Projects View. In Proceedings of the International Conference on Big Data and Information Analytics (BigDIA), Shenzhen, China, 4–6 December 2020; pp. 113–116. [Google Scholar] [CrossRef]
- Lin, C.-H.; Chan, S.-B.; Lai, Y.-C.; Liang, W.-L.; Huang, M.-S.; Chen, Y.-Y. AI in eHealth: Diagnosis of Parkinson’s Disease with Augmented Reality. In Proceedings of the IEEE International Conference on Consumer Electronics-Taiwan (ICCE-TW), Penghu, Taiwan, 15–17 September 2021; pp. 1–2. [Google Scholar] [CrossRef]
- Lin, K.; Liu, J.; Goa, J. AI-Driven Decision Making for Auxiliary Diagnosis of Epidemic Diseases. IEEE Trans. Mol. Biol. Multi-Scale Commun. 2022, 8, 9–16. [Google Scholar] [CrossRef]
- Lanubile, F.; Calefato, F.; Quaranta, L.; Amoruso, M.; Fumarola, F.; Filannino, M. Towards Productizing AI/ML Models: An Industry Perspective from Data Scientists. In Proceedings of the IEEE/ACM 1st Workshop on AI Engineering—Software Engineering for AI (WAIN), Madrid, Spain, 30–31 May 2021; pp. 129–132. [Google Scholar] [CrossRef]
- Dalvi, C.; Rathod, M.; Patil, S.; Gite, S.; Kotecha, K. A Survey of AI-Based Facial Emotion Recognition: Features, ML & DL Techniques, Age-Wise Datasets and Future Directions. IEEE Access 2021, 9, 165806–165840. [Google Scholar] [CrossRef]
- Dahlin, N.; Chang, K.; Kalagarla, K.C.; Jain, R.; Nuzzo, P. Practical Control Design for the Deep Learning Age: Distillation of Deep RL-Based Controllers. In Proceedings of the Annual Allerton Conference on Communication, Control, and Computing (Allerton), Monticello, IL, USA, 1–27 September 2022; pp. 1–8. [Google Scholar] [CrossRef]
- Joo, H.-T.; Kim, H.-J. Visualization of Deep Reinforcement Learning using Grad-CAM: How AI Plays Atari Games? In Proceedings of the IEEE Conference on Games (CoG), London, UK, 20–23 August 2019; pp. 1–2. [Google Scholar] [CrossRef]
- Yu, K.H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.S.; Muhammad, G.; Alamri, A. Smart healthcare monitoring: A voice pathology detection paradigm for smart cities. Multimed. Syst. 2019, 25, 565–575. [Google Scholar] [CrossRef]
- Chen, G.; Wang, L.; Kamruzzaman, M.M. Spectral classification of ecological spatial polarization SAR image based on target decomposition algorithm and machine learning. Neural Comput. Appl. 2020, 32, 5449–5460. [Google Scholar] [CrossRef]
- Chen, G.; Jiang, Z.; Kamruzzaman, M.M. Radar remote sensing image retrieval algorithm based on improved Sobel operator. J. Vis. Commun. Image Represent. 2020, 71, 102720. [Google Scholar] [CrossRef]
- Kim, H.; Ben-Othman, J. Toward Integrated Virtual Emotion System with AI Applicability for Secure CPS-Enabled Smart Cities: AI-Based Research Challenges and Security Issues. IEEE Netw. 2020, 34, 30–36. [Google Scholar] [CrossRef]
- Chen, X.; Zhang, L.; Liu, T.; Kamruzzaman, M.M. Research on deep learning in the field of mechanical equipment fault diagnosis image quality. J. Vis. Commun. Image Represent. 2019, 62, 402–409. [Google Scholar] [CrossRef]
- Noorbakhsh-Sabet, N.; Zand, R.; Zhang, Y.; Abedi, V. Artificial Intelligence Transforms the Future of Health Care. Am. J. Med. 2019, 132, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.; Fox, J.; Purohit, M.P. Artificial intelligence-enabled healthcare delivery. J. R. Soc. Med. 2019, 112, 22–28. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Pham, Q.V.; Pathirana, P.N.; Ding, M.; Seneviratne, A.; Lin, Z.; Dobre, O.; Hwang, W.J. Federated Learning for Smart Healthcare: A Survey. ACM Comput. Surv. 2023, 55, 60. [Google Scholar] [CrossRef]
- Iqbal, W.; Abbas, H.; Daneshmand, M.; Rauf, B.; Bangash, Y.A. An In-Depth Analysis of IoT Security Requirements, Challenges, and Their Countermeasures via Software-Defined Security. IEEE Internet Things J. 2020, 7, 10250–10276. [Google Scholar] [CrossRef]
- Zhou, W.; Jia, Y.; Peng, A.; Zhang, Y.; Liu, P. The Effect of IoT New Features on Security and Privacy: New Threats, Existing Solutions, and Challenges Yet to Be Solved. IEEE Internet Things J. 2019, 6, 1606–1616. [Google Scholar] [CrossRef]
- Lins, F.A.; Vieira, M. Security Requirements and Solutions for IoT Gateways: A Comprehensive Study. IEEE Internet Things J. 2021, 8, 8667–8679. [Google Scholar] [CrossRef]
- Xiao, Y.; Jia, Y.; Liu, C.; Cheng, X.; Yu, J.; Lv, W. Edge Computing Security: State of the Art and Challenges. Proc. IEEE 2019, 107, 1608–1631. [Google Scholar] [CrossRef]
- Jia, Y.; Zhong, F.; Alrawais, A.; Gong, B.; Cheng, X. FlowGuard. An Intelligent Edge Defense Mechanism Against IoT DDoS Attacks. IEEE Internet Things J. 2020, 7, 9552–9562. [Google Scholar] [CrossRef]
- Yaqoob, I.; Salah, K.; Jayaraman, R.; Al-Hammadi, Y. Blockchain for healthcare data management: Opportunities, challenges, and future recommendations. Neural Comput. Appl. 2022, 34, 11475–11490. [Google Scholar] [CrossRef]
- Deepa, N.; Pham, Q.V.; Nguyen, D.C.; Bhattacharya, S.; Prabadevi, B.; Gadekallu, T.R.; Maddikunta, P.K.; Fang, F.; Pathirana, P.N. A survey on blockchain for big data: Approaches, Opportunities, and Future Directions. Future Gener. Comput. Syst. 2022, 131, 209–226. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Nguyen, V.D.; Ding, M.; Chatzinotas, S.; Pathirana, P.N.; Seneviratne, A.; Dobre, O.; Zomaya, A.Y. Intelligent Blockchain-Based Edge Computing via Deep Reinforcement Learning: Solutions and Challenges. IEEE Netw. 2022, 36, 12–19. [Google Scholar] [CrossRef]
- Nguyen, D.C.; Pathirana, P.N.; Ding, M.; Seneviratne, A. BEdgeHealth: A Decentralized Architecture for Edge-Based IoMT Networks Using Blockchain. IEEE Internet Things J. 2021, 8, 11743–11757. [Google Scholar] [CrossRef]
- Shanin, F.; Das, H.A.; Krishnan, G.A.; Neha, L.S.; Thaha, N.; Aneesh, R.P.; Embrandiri, S.; Jayakrishan, S. Portable and Centralised E-Health Record System for Patient Monitoring Using Internet of Things(IoT). In Proceedings of the International CET Conference on Control, Communication, and Computing (IC4), Thiruvananthapuram, India, 5–7 July 2018; pp. 165–170. [Google Scholar] [CrossRef]
- Swaroop, K.N.; Chandu, K.; Gorrepotu, R.; Deb, S. A health monitoring system for vital signs using IoT. Internet Things 2019, 5, 116–129. [Google Scholar] [CrossRef]
- Rathore, M.M.; Ahmad, A.; Paul, A.; Wan, J.; Zhang, D. Real-time Medical Emergency Response System: Exploiting IoT and Big Data for Public Health. J. Med. Syst. 2016, 40, 283. [Google Scholar] [CrossRef] [PubMed]
- El Zouka, H.A.; Hosni, M.M. Secure IoT communications for smart healthcare monitoring system. Internet Things 2019, 13, 100036. [Google Scholar] [CrossRef]
- Rohokale, V.M.; Prasad, N.R.; Prasad, R. A cooperative Internet of Things (IoT) for rural healthcare monitoring and control. In Proceedings of the International Conference on Wireless Communication, Vehicular Technology, Information Theory and Aerospace & Electronic Systems Technology (Wireless VITAE), Chennai, India, 28 February–3 March 2011; pp. 1–6. [Google Scholar] [CrossRef]
- Mohammed, J.; Lung, C.H.; Ocneanu, A.; Thakral, A.; Jones, C.; Adler, A. Internet of Things: Remote Patient Monitoring Using Web Services and Cloud Computing. In Proceedings of the IEEE International Conference on Internet of Things (iThings), and IEEE Green Computing and Communications (GreenCom) and IEEE Cyber, Physical and Social Computing (CPSCom), Taipei, Taiwan, 1–3 September 2014; pp. 256–263. [Google Scholar] [CrossRef]
- Sundhara Kumar, K.B.; Bairavi, K. IoT Based Health Monitoring System for Autistic Patients. In Proceedings of the International Symposium on Big Data and Cloud Computing Challenges (ISBCC-16′), Vellore, India, 10–11 March 2016; pp. 371–376. [Google Scholar] [CrossRef]
- Onasanya, A.; Elshakankiri, M. Smart integrated IoT healthcare system for cancer care. Wirel. Netw. 2021, 27, 4297–4312. [Google Scholar] [CrossRef]
- Sood, S.K.; Mahajan, I. Wearable IoT sensor based healthcare system for identifying and controlling chikungunya virus. Comput. Ind. 2017, 91, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Abdelgawad, A.; Yelamarthi, K.; Khattab, A. IoT-Based Health Monitoring System for Active and Assisted Livin. In Smart Objects and Technologies for Social Good, Proceedings of the Lecture Notes of the Institute for Computer Sciences, Social Informatics and Telecommunications Engineering, Venice, Italy, 30 November–1 December 2016; Gaggi, O., Manzoni, P., Palazzi, C., Bujari, A., Marquez-Barja, J., Eds.; Springer: Cham, Switzerland, 2016; Volume 195. [Google Scholar] [CrossRef]
- Yang, L.; Ge, Y.; Li, W.; Rao, W.; Shen, W. A home mobile healthcare system for wheelchair users. In Proceedings of the 2014 IEEE 18th International Conference on Computer Supported Cooperative Work in Design (CSCWD), Hsinchu, Taiwan, 21–23 May 2014; pp. 609–614. [Google Scholar] [CrossRef]
- Yang, Z.; Zhou, Q.; Lei, L.; Zheng, K.; Xiang, W. An IoT-cloud Based Wearable ECG Monitoring System for Smart Healthcare. J. Med. Syst. 2016, 40, 286. [Google Scholar] [CrossRef]
- Cerina, L.; Notargiacomo, S.; Paccanit, M.G.; Santambrogio, M.D. A fog-computing architecture for preventive healthcare and assisted living in smart ambients. In Proceedings of the IEEE 3rd International Forum on Research and Technologies for Society and Industry (RTSI), Modena, Italy, 11–13 September 2017; pp. 1–6. [Google Scholar] [CrossRef]
- Verma, P.; Sood, S.K. Fog Assisted-IoT Enabled Patient Health Monitoring in Smart Homes. IEEE Internet Things J. 2018, 5, 1789–1796. [Google Scholar] [CrossRef]
- Azimi, I.; Anzanpour, A.; Rahmani, A.M.; Pahikkala, T.; Levorato, M.; Liljeberg, P.; Dutt, N. HiCH: Hierarchical fog-assisted computing architecture for healthcare IoT. ACM Trans. Embed. Comput. Syst. 2017, 16, 174. [Google Scholar] [CrossRef]
- Kumar, N. IoT architecture and system design for healthcare systems. In Proceedings of the International Conference on Smart Technologies for Smart Nation (SmartTechCon), Bengaluru, India, 17–19 August 2017; pp. 1118–1123. [Google Scholar] [CrossRef]
- Balakrishnan, L. An Internet of Things(IoT) Based Intelligent Framework for Healthcare—A Survey. In Proceedings of the International Conference on Signal Processing and Communication (ICPSC), Coimbatore, India, 13–14 May 2021; pp. 243–251. [Google Scholar] [CrossRef]
- Krishnamoorthy, S.; Dua, A.; Gupta, S. Role of emerging technologies in future IoT-driven Healthcare 4.0 technologies: A survey, current challenges and future directions. J. Ambient Intell. Humaniz. Comput. 2023, 14, 361–407. [Google Scholar] [CrossRef]
- Mahmud, R.; Koch, F.L.; Buyya, R. Cloud-fog interoperability in IoT-enabled healthcare solutions. In Proceedings of the 19th International Conference on Distributed Computing and Networking, Varanasi, India, 4–7 January 2018; pp. 1–10. [Google Scholar] [CrossRef]
- Debauche, O.; Mahmoudi, S.; Manneback, P.; Assila, A. Fog IoT for Health: A new Architecture for Patients and Elderly Monitoring. Procedia Comput. Sci. 2019, 160, 289–297. [Google Scholar] [CrossRef]
- Paul, A.; Pinjari, H.; Hong, W.H.; Seo, H.C.; Rho, S. Fog Computing-Based IoT for Health Monitoring System. J. Sens. 2018, 2018, 1386470. [Google Scholar] [CrossRef]
- Awaisi, K.S.; Hussain, S.; Ahmed, M.; Khan, A.A.; Ahmed, G. Leveraging IoT and Fog Computing in Healthcare Systems. IEEE Internet Things Mag. 2020, 3, 52–56. [Google Scholar] [CrossRef]
- Abdelmoneem, R.M.; Benslimane, A.; Shaaban, E.; Abdelhamid, S.; Ghoneim, S. A Cloud-Fog Based Architecture for IoT Applications Dedicated to Healthcare. In Proceedings of the ICC 2019—2019 IEEE International Conference on Communications (ICC), Shanghai, China, 20–24 May 2019. [Google Scholar] [CrossRef]
- Islam, S.R.; Kwak, D.; Kabir, M.H.; Hossain, M.; Kwak, K.S. The Internet of Things for Health Care: A Comprehensive Survey. IEEE Access 2015, 3, 678–708. [Google Scholar] [CrossRef]
- Farahani, B.; Firouzi, F.; Chang, V.; Badaroglu, M.; Constant, N.; Mankodiya, K. Towards fog-driven IoT eHealth: Promises and challenges of IoT in medicine and healthcare. Future Gener. Comput. Syst. 2018, 78, 659–676. [Google Scholar] [CrossRef]
- Wu, T.; Wu, F.; Redoute, J.M.; Yuce, M.R. An Autonomous Wireless Body Area Network Implementation Towards IoT Connected Healthcare Applications. IEEE Access 2017, 5, 11413–11422. [Google Scholar] [CrossRef]
- Verma, A.; Ranga, V. Security of RPL Based 6LoWPAN Networks in the Internet of Things: A Review. IEEE Sens. J. 2020, 20, 5666–5690. [Google Scholar] [CrossRef]
- Ghamari, M.; Janko, B.; Sherratt, R.S.; Harwin, W.; Piechockic, R.; Soltanpur, C. A Survey on Wireless Body Area Networks for eHealthcare Systems in Residential Environments. Sensors 2016, 16, 831. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).