“Can Do” vs. “Do Do” in Older Adults: A Cross-Sectional Analysis of Sensor-Derived Physical Activity Patterns
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Inclusion and Exclusion Criteria
2.3. Measurements
2.4. PC-PA Quadrant Concept
2.5. Data Analysis
3. Results
3.1. Significance of Differences between the Four Quadrants in PA
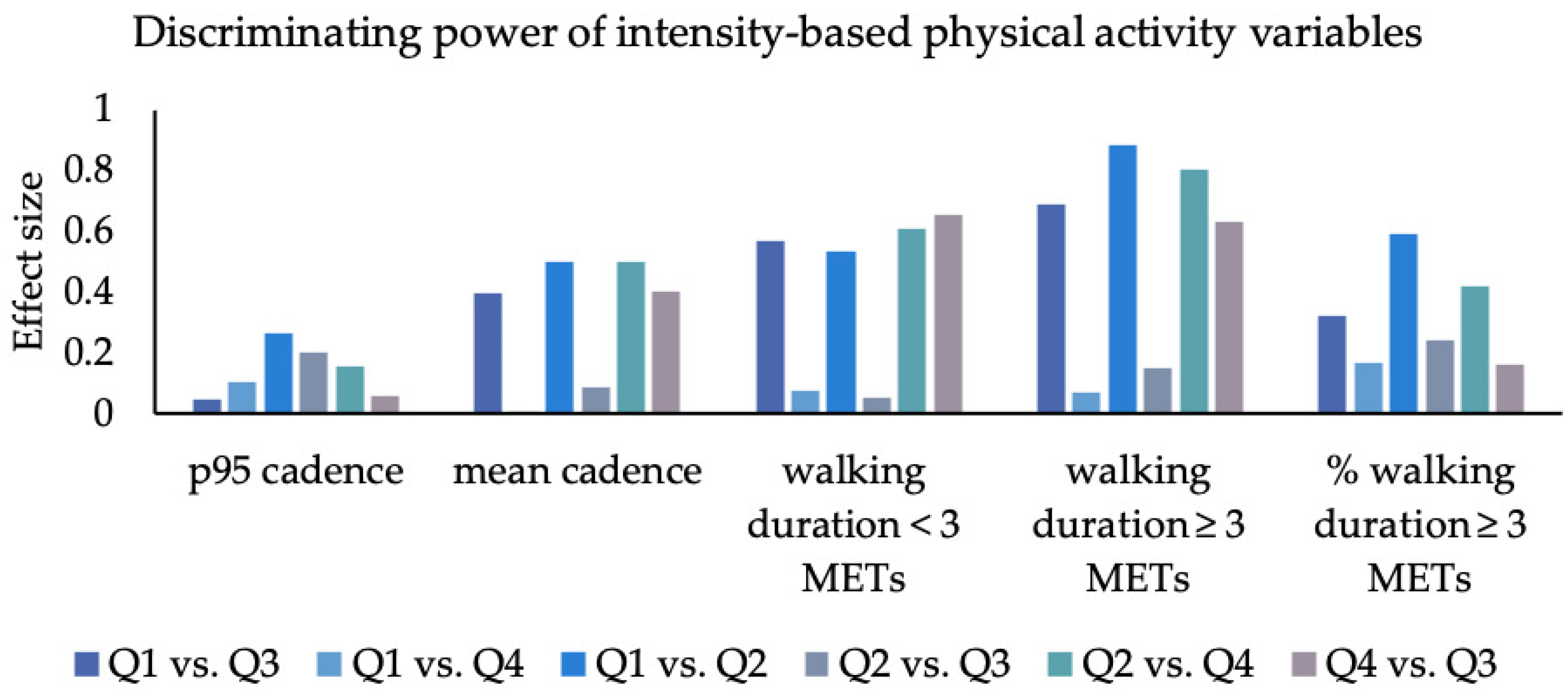
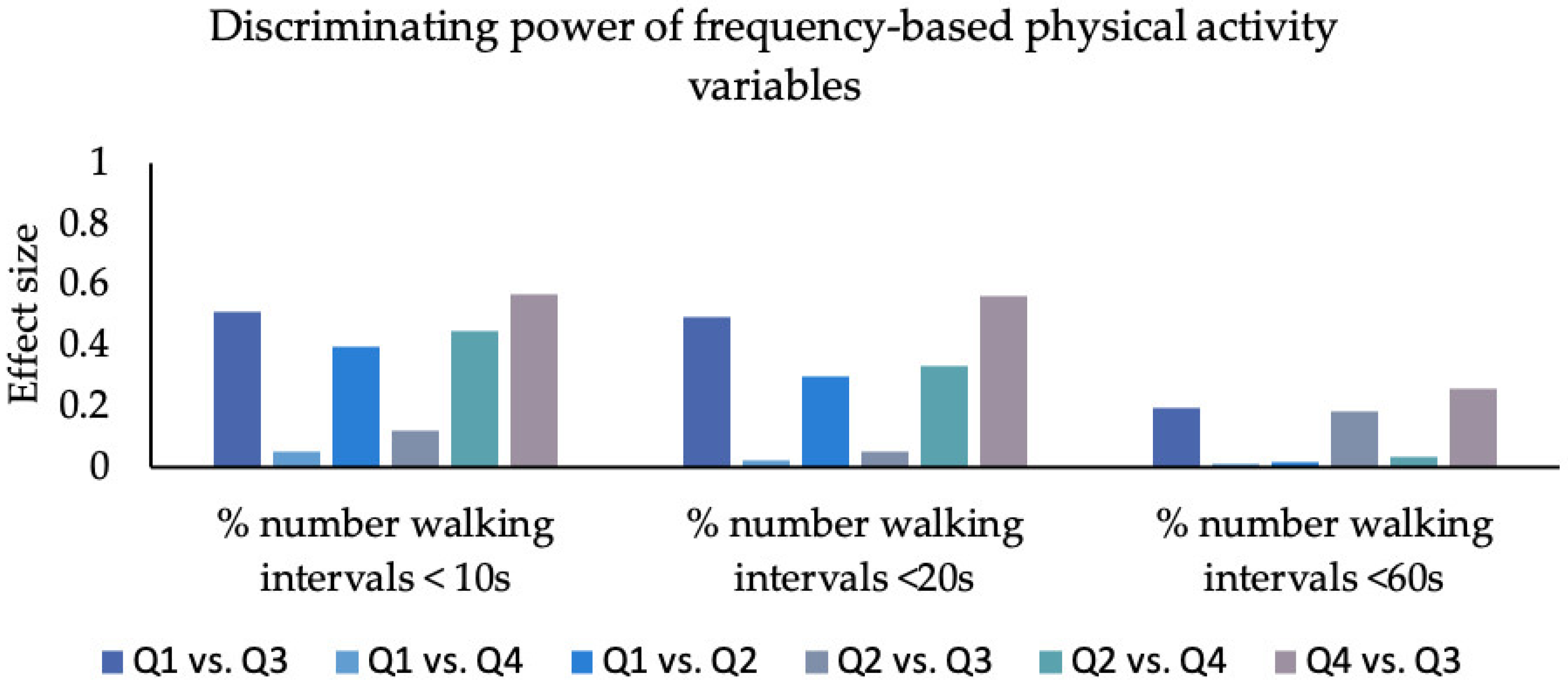
3.2. Effect Sizes
3.3. Walking Intensity
3.4. Walking Duration
3.5. Frequency
4. Discussion
4.1. Underlying Physical Activity Patterns of the Four PC-PA Groups
4.1.1. Can Do–Do Do vs. Cannot Do–Do Do
4.1.2. Can Do–Do Do vs. Can Do–Do Not Do
4.1.3. Can Do–Do Do vs. Cannot Do–Do Not Do
4.2. Most Relevant PA Variables for Discriminating the Four Groups (Largest Effect Sizes)
4.2.1. Intensity
4.2.2. Duration
4.2.3. Frequency
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Blair, S.N.; Morris, J.N. Healthy hearts—And the universal benefits of being physically active: Physical activity and health. Ann. Epidemiol. 2009, 19, 253–256. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical- (accessed on 21 December 2022).
- Koolen, E.H.; van Hees, H.W.; van Lummel, R.C.; Dekhuijzen, R.; Djamin, R.S.; Spruit, M.A.; van ‘t Hul, A.J. “Can do” versus “do do”: A Novel Concept to Better Understand Physical Functioning in Patients with Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2019, 8, 340. [Google Scholar] [CrossRef] [PubMed]
- Sievi, N.A.; Brack, T.; Brutsche, M.H.; Frey, M.; Irani, S.; Leuppi, J.D.; Thurnheer, R.; Kohler, M.; Clarenbach, C.F. “Can do, don’t do” are not the lazy ones: A longitudinal study on physical functioning in patients with COPD. Respir. Res. 2020, 21, 27. [Google Scholar] [CrossRef] [PubMed]
- Carl, J.; Schultz, K.; Janssens, T.; von Leupoldt, A.; Pfeifer, K.; Geidl, W. The “can do, do do” concept in individuals with chronic obstructive pulmonary disease: An exploration of psychological mechanisms. Respir. Res. 2021, 22, 260. [Google Scholar] [CrossRef]
- Vaes, A.W.; Spruit, M.A.; Koolen, E.H.; Antons, J.C.; de Man, M.; Djamin, R.S.; van Hees, H.W.H.; van ‘t Hul, A.J. “Can Do, Do Do” Quadrants and 6-Year All-Cause Mortality in Patients With COPD. Chest 2022, 161, 1494–1504. [Google Scholar] [CrossRef]
- Janssen, S.M.J.; Spruit, M.A.; Antons, J.C.; Djamin, R.S.; Abbink, J.J.; van Helvoort, H.A.C.; van ‘t Hul, A.J. “Can Do” versus “Do Do” in Patients with Asthma at First Referral to a Pulmonologist. J. Allergy Clin. Immunol. Pract. 2021, 9, 1278–1284. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Rapp, K.; Klenk, J.; Benzinger, P.; Franke, S.; Denkinger, M.D.; Peter, R. Physical performance and daily walking duration: Associations in 1271 women and men aged 65-90 years. Aging Clin. Exp. Res. 2012, 24, 455–460. [Google Scholar] [CrossRef]
- Orendurff, M.S.; Schoen, J.A.; Bernatz, G.C.; Segal, A.D.; Klute, G.K. How humans walk: Bout duration, steps per bout, and rest duration. J. Rehabil. Res. Dev. 2008, 45, 1077–1089. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Johnson, W.D.; Katzmarzyk, P.T. Accelerometer-determined steps per day in US adults. Med. Sci. Sports Exerc. 2009, 41, 1384–1391. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; de Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef]
- Gottschalk, S.; König, H.-H.; Schwenk, M.; Nerz, C.; Becker, C.; Klenk, J.; Jansen, C.-P.; Dams, J. Cost-Effectiveness of a Group vs. Individually Delivered Exercise Program in Community-Dwelling Persons Aged ≥70 Years. J. Am. Med. Dir. Assoc. 2022, 23, 736–742.e6. [Google Scholar] [CrossRef]
- Kramer, F.; Labudek, S.; Jansen, C.-P.; Nerz, C.; Fleig, L.; Clemson, L.; Becker, C.; Schwenk, M. Development of a conceptual framework for a group-based format of the Lifestyle-integrated Functional Exercise (gLiFE) programme and its initial feasibility testing. Pilot Feasibility Stud. 2020, 6, 6. [Google Scholar] [CrossRef]
- Jansen, C.-P.; Nerz, C.; Kramer, F.; Labudek, S.; Klenk, J.; Dams, J.; König, H.-H.; Clemson, L.; Becker, C.; Schwenk, M. Comparison of a group-delivered and individually delivered lifestyle-integrated functional exercise (LiFE) program in older persons: A randomized noninferiority trial. BMC Geriatr. 2018, 18, 267. [Google Scholar] [CrossRef]
- Christopher, A.; Kraft, E.; Olenick, H.; Kiesling, R.; Doty, A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: A systematic review. Disabil. Rehabil. 2021, 43, 1799–1813. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Rosenthal, R. Parametric Measures of Effect Size. In The Handbook of Research Synthesis; Cooper, H., Hedges, L.V., Valentine, J.C., Eds.; Russell Sage Foundation: New York, NY, USA, 1994; pp. 231–244. [Google Scholar]
- White, S.M.; Wójcicki, T.R.; McAuley, E. Physical activity and quality of life in community dwelling older adults. Health Qual. Life Outcomes 2009, 7, 10. [Google Scholar] [CrossRef]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar] [CrossRef]
- Marques, E.A.; Baptista, F.; Santos, D.A.; Silva, A.M.; Mota, J.; Sardinha, L.B. Risk for losing physical independence in older adults: The role of sedentary time, light, and moderate to vigorous physical activity. Maturitas 2014, 79, 91–95. [Google Scholar] [CrossRef]
- Giannouli, E.; Bock, O.; Mellone, S.; Zijlstra, W. Mobility in Old Age: Capacity Is Not Performance. Biomed. Res. Int. 2016, 2016, 3261567. [Google Scholar] [CrossRef]
- Rantanen, T. Promoting mobility in older people. J. Prev. Med. Public Health 2013, 46 (Suppl. 1), S50–S54. [Google Scholar] [CrossRef] [PubMed]
- Newman, A.B.; Simonsick, E.M.; Naydeck, B.L.; Boudreau, R.M.; Kritchevsky, S.B.; Nevitt, M.C.; Pahor, M.; Satterfield, S.; Brach, J.S.; Studenski, S.A.; et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA 2006, 295, 2018–2026. [Google Scholar] [CrossRef]
- Schnohr, P.; Scharling, H.; Jensen, J.S. Intensity versus duration of walking, impact on mortality: The Copenhagen City Heart Study. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 72–78. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Kim, J.; Kim, J. A Study of Leisure Walking Intensity Levels on Mental Health and Health Perception of Older Adults. Gerontol. Geriatr. Med. 2021, 7, 2333721421999316. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, D.B.; Slentz, C.A.; Willis, L.H.; Hoselton, A.; Huebner, J.L.; Kraus, V.B.; Moss, J.; Muehlbauer, M.J.; Spielmann, G.; Muoio, D.M.; et al. Rejuvenation of Neutrophil Functions in Association with Reduced Diabetes Risk Following Ten Weeks of Low-Volume High Intensity Interval Walking in Older Adults with Prediabetes—A Pilot Study. Front. Immunol. 2020, 11, 729. [Google Scholar] [CrossRef]
- De Melo, L.L.; Menec, V.H.; Ready, A.E. Relationship of functional fitness with daily steps in community-dwelling older adults. J. Geriatr. Phys. Ther. 2014, 37, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Boulton, E.R.; Horne, M.; Todd, C. Multiple influences on participating in physical activity in older age: Developing a social ecological approach. Health Expect. 2018, 21, 239–248. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Mora-Gonzalez, J.; Ducharme, S.W.; Aguiar, E.J.; Schuna, J.M.; Barreira, T.V.; Moore, C.C.; Chase, C.J.; Gould, Z.R.; Amalbert-Birriel, M.A.; et al. Walking cadence (steps/min) and intensity in 61–85-year-old adults: The CADENCE-Adults study. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 129. [Google Scholar] [CrossRef]
- Hollman, J.H.; McDade, E.M.; Petersen, R.C. Normative spatiotemporal gait parameters in older adults. Gait Posture 2011, 34, 111–118. [Google Scholar] [CrossRef]
- Kojima, G.; Masud, T.; Kendrick, D.; Morris, R.; Gawler, S.; Treml, J.; Iliffe, S. Does the timed up and go test predict future falls among British community-dwelling older people? Prospective cohort study nested within a randomised controlled trial. BMC Geriatr. 2015, 15, 38. [Google Scholar] [CrossRef]
- Shumway-Cook, A.; Brauer, S.; Woollacott, M. Predicting the Probability for Falls in Community-Dwelling Older Adults Using the Timed Up & Go Test. Physical Therapy 2000, 80, 896–903. [Google Scholar] [CrossRef]
- Bischoff, H.A.; Stähelin, H.B.; Monsch, A.U.; Iversen, M.D.; Weyh, A.; von Dechend, M.; Akos, R.; Conzelmann, M.; Dick, W.; Theiler, R. Identifying a cut-off point for normal mobility: A comparison of the timed ‘up and go’ test in community-dwelling and institutionalised elderly women. Age Ageing 2003, 32, 315–320. [Google Scholar] [CrossRef]
- Thorpe, O.; Johnston, K.; Kumar, S. Barriers and enablers to physical activity participation in patients with COPD: A systematic review. J. Cardiopulm. Rehabil. Prev. 2012, 32, 359–369. [Google Scholar] [CrossRef]
- Dawe, R.J.; Leurgans, S.E.; Yang, J.; Bennett, J.M.; Hausdorff, J.M.; Lim, A.S.; Gaiteri, C.; Bennett, D.A.; Buchman, A.S. Association between Quantitative Gait and Balance Measures and Total Daily Physical Activity in Community-Dwelling Older Adults. J. Gerontol. A Biol. Sci. Med. Sci. 2018, 73, 636–642. [Google Scholar] [CrossRef]
- Jansen, C.-P.; Gordt-Oesterwind, K.; Schwenk, M. Wearable Motion Sensors in Older Adults: On the Cutting Edge of Health and Mobility Research. Sensors 2022, 22, 973. [Google Scholar] [CrossRef]


| PA Property | PA Variable |
|---|---|
| Intensity |
|
| Duration |
|
| Frequency |
|
| Can Do–Do Do | Can Do–Do Not Do | Cannot Do–Do Do | Cannot Do–Do Not Do | p * | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Subjects | 81 | - | 45 | - | 71 | - | 97 | - | - |
| % female | 71.6 | - | 62.2 | - | 78.9 | - | 74.2 | - | 0.26 ** |
| Age, years | 77.3 | 4.7 | 76.1 | 4.7 | 79.9 | 5.4 | 80.5 | 5.3 | <0.001 |
| BMI, kg/m2 | 26.1 | 4.0 | 27.6 | 4.9 | 25.8 | 4.0 | 28.9 | 5.6 | <0.001 |
| TUG, s | 10.6 | 1.0 | 10.5 | 1.1 | 14.7 | 3.2 | 15.8 | 4.3 | <0.001 |
| Steps per day, steps | 8047 | 2338 | 3583 | 1161 | 7767 | 1976 | 3077 | 1107 | <0.001 |
| Number of walking intervals < 10 s | 279.2 | 82.2 | 184.7 | 57.7 | 290.2 | 101.6 | 178.2 | 60.6 | <0.001 |
| Number of walking intervals < 20 s | 371.3 | 108.1 | 229.9 | 72.3 | 390.3 | 128.9 | 226.7 | 74.9 | <0.001 |
| Number of walking intervals < 60 s | 424.5 | 125.8 | 252.0 | 78.7 | 445.4 | 141.9 | 248.2 | 80.6 | <0.001 |
| Can Do–Do Do (Q1) | Can Do–Do Not Do (Q2) | Cannot Do–Do Do (Q3) | Cannot Do–Do Not Do (Q4) | p-Value * | |||||
|---|---|---|---|---|---|---|---|---|---|
| PA Variable | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| P95 cadence (in steps per min) | 108.67 | 7.84 | 107.64 | 8.23 | 107.24 | 8.44 | 104.31 | 8.62 | 0.003 |
| Mean cadence (in steps per min) | 67.68 | 4.81 | 63.06 | 4.91 | 68.03 | 5.39 | 61.73 | 5.68 | <0.001 |
| Mean walking duration per day (in min) | 105.61 | 28.13 | 51.55 | 15.42 | 105.9 | 25.43 | 47.54 | 14.92 | <0.001 |
| Walking duration lower 3 METs (in min) | 48.95 | 17.50 | 28.43 | 10.00 | 53.82 | 21.21 | 30.32 | 10.77 | <0.001 |
| Walking duration greater equal 3 METs (in min) | 56.66 | 19.96 | 23.13 | 9.97 | 52.12 | 18.14 | 17.23 | 10.06 | <0.001 |
| Percentage walking duration greater equal 3 METs (%) | 53.66 | 11.63 | 44.13 | 13.08 | 49.51 | 13.80 | 34.30 | 16.50 | <0.001 |
| Maximum continuous number of steps | 1585.3 | 1009.6 | 868.36 | 816.6 | 1209.5 | 674.8 | 606.6 | 400.8 | <0.001 |
| Maximum walking interval length (in s) | 15.16 | 9.86 | 8.50 | 5.95 | 12.19 | 6.27 | 7.09 | 4.58 | <0.001 |
| Average walking interval length (in s) | 15.04 | 3.58 | 12.03 | 2.55 | 14.70 | 4.31 | 11.59 | 3.58 | <0.001 |
| Number of walking intervals | 437.01 | 126.47 | 259.13 | 79.10 | 457.83 | 140.87 | 254.25 | 80.61 | <0.001 |
| Percentage of walking intervals < 10 s (%) | 64.08 | 5.69 | 71.69 | 6.13 | 62.80 | 6.56 | 69.83 | 7.98 | <0.001 |
| Percentage of walking intervals < 20 s (%) | 84.96 | 3.95 | 88.65 | 3.27 | 84.70 | 4.90 | 88.74 | 5.29 | <0.001 |
| Percentage of walking intervals < 60 s (%) | 96.91 | 1.71 | 97.02 | 1.42 | 96.91 | 2.00 | 97.38 | 1.98 | 0.021 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adams, M.; Carrascosa, L.; Jansen, C.-P.; Ritter, Y.; Schwenk, M. “Can Do” vs. “Do Do” in Older Adults: A Cross-Sectional Analysis of Sensor-Derived Physical Activity Patterns. Sensors 2023, 23, 1879. https://doi.org/10.3390/s23041879
Adams M, Carrascosa L, Jansen C-P, Ritter Y, Schwenk M. “Can Do” vs. “Do Do” in Older Adults: A Cross-Sectional Analysis of Sensor-Derived Physical Activity Patterns. Sensors. 2023; 23(4):1879. https://doi.org/10.3390/s23041879
Chicago/Turabian StyleAdams, Michael, Lara Carrascosa, Carl-Philipp Jansen, Yvonne Ritter, and Michael Schwenk. 2023. "“Can Do” vs. “Do Do” in Older Adults: A Cross-Sectional Analysis of Sensor-Derived Physical Activity Patterns" Sensors 23, no. 4: 1879. https://doi.org/10.3390/s23041879
APA StyleAdams, M., Carrascosa, L., Jansen, C.-P., Ritter, Y., & Schwenk, M. (2023). “Can Do” vs. “Do Do” in Older Adults: A Cross-Sectional Analysis of Sensor-Derived Physical Activity Patterns. Sensors, 23(4), 1879. https://doi.org/10.3390/s23041879






