Development of Real-Time Cuffless Blood Pressure Measurement Systems with ECG Electrodes and a Microphone Using Pulse Transit Time (PTT)
Abstract
1. Introduction
2. Materials and Methods
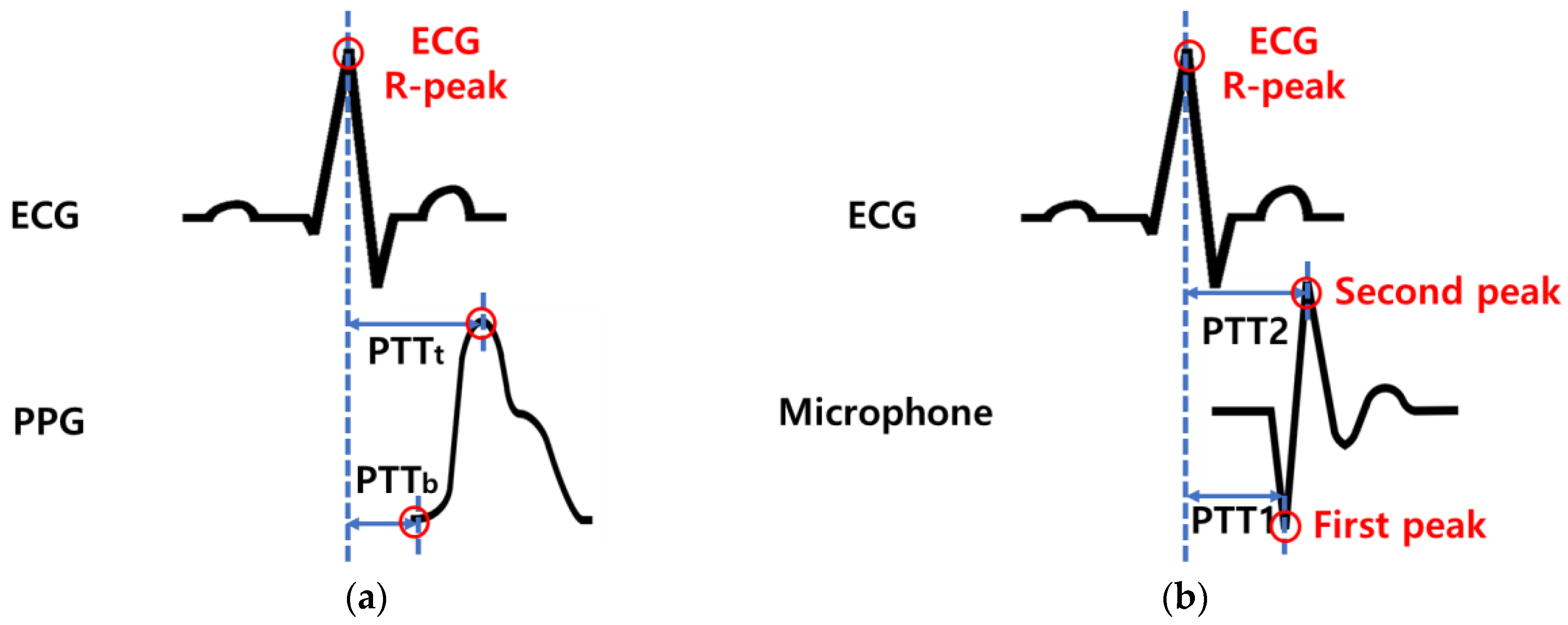
2.1. Pulse Transit Time (PTT)
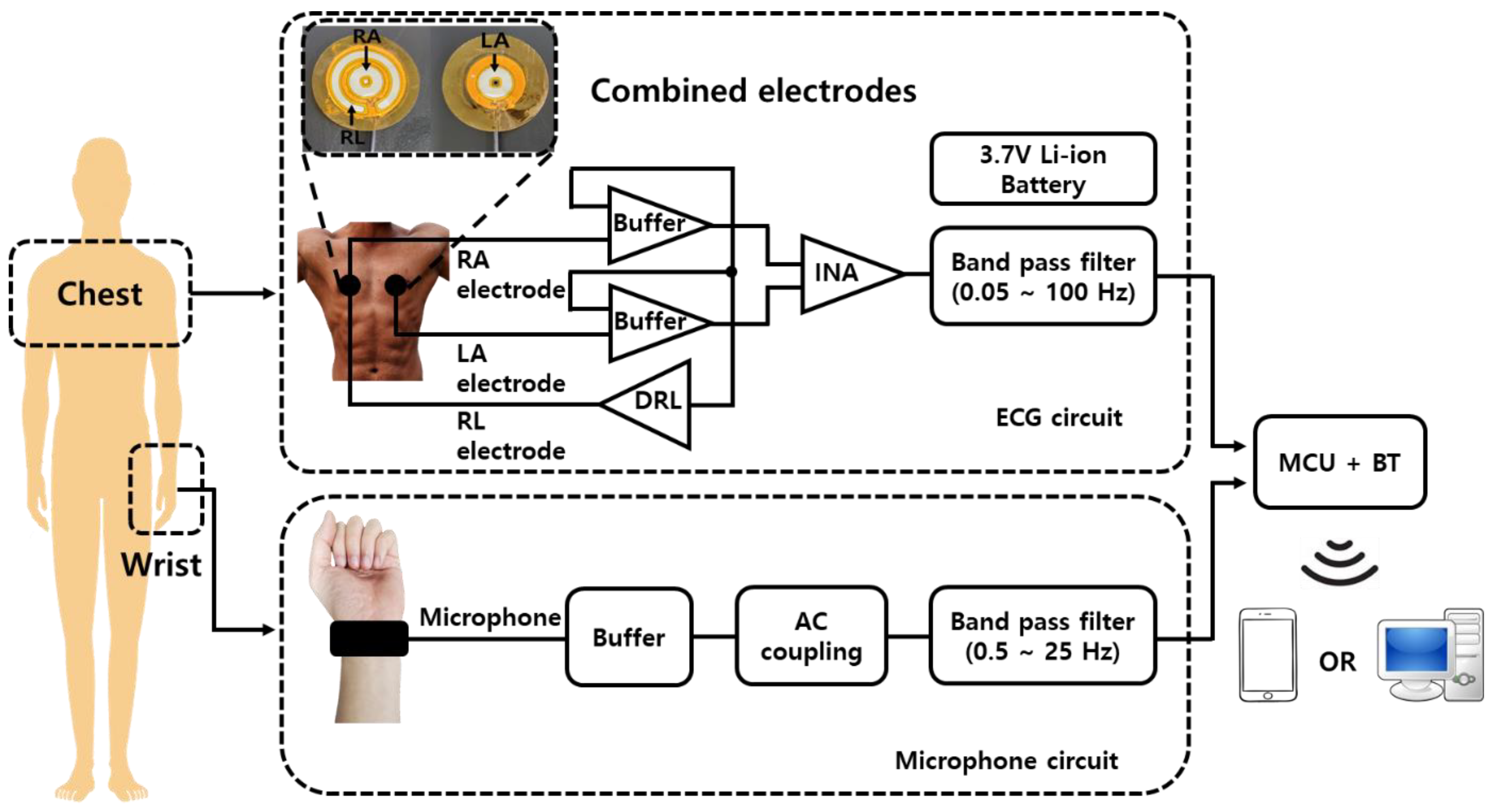
2.2. Configuration of a Blood Pressure Measurement Device Using PTT
2.2.1. ECG Measurement Device
2.2.2. Pulse Wave Measurement Device
2.3. Performance Evaluation of Blood Pressure Measurement Device
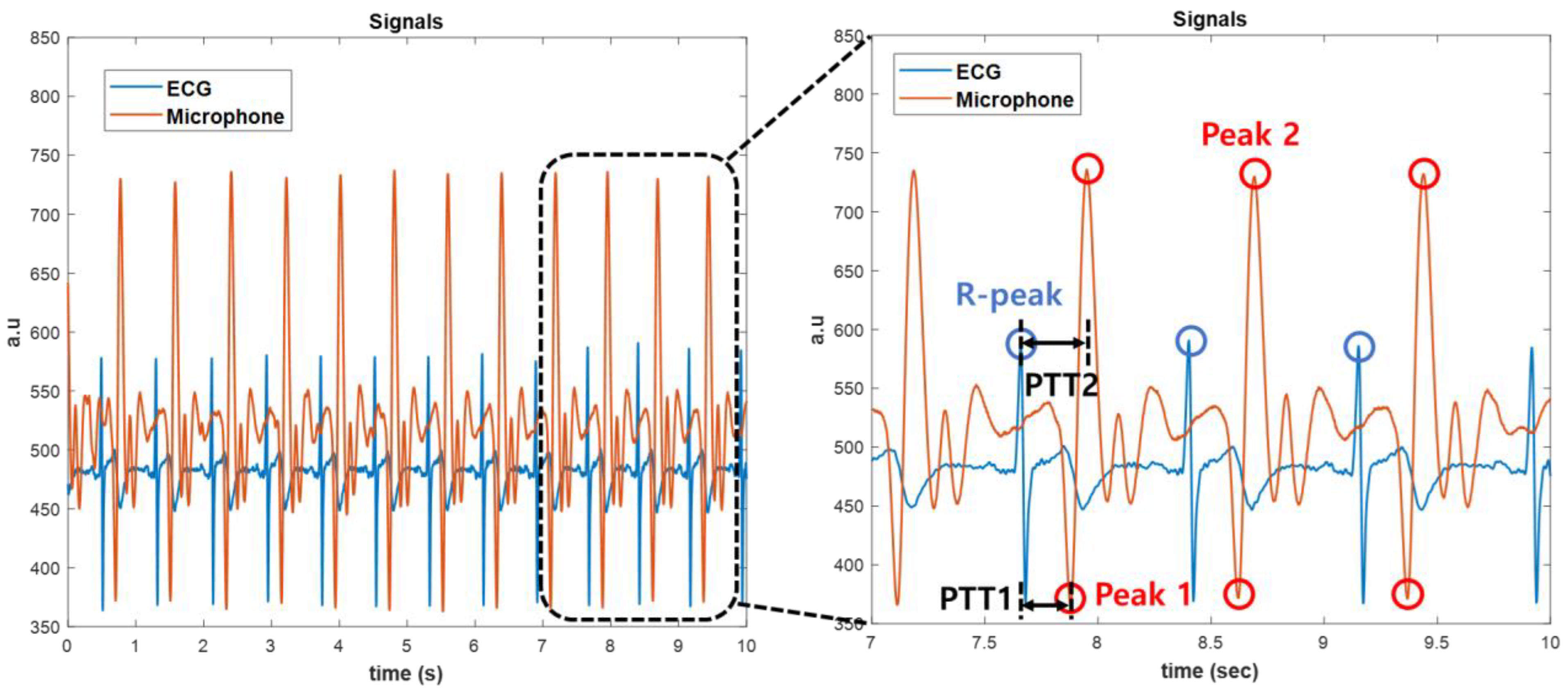
3. Results and Discussions
3.1. Fabrication Results of Blood Pressure Measurement Device
3.2. Performance Evaluation
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Drazner, M.H. The Progression of Hypertensive Heart Disease. Circulation 2011, 123, 327–334. [Google Scholar] [CrossRef]
- Gąsecki, D.; Kwarciany, M.; Nyka, W.; Narkiewicz, K. Hypertension, Brain Damage and Cognitive Decline. Curr. Hypertens Rep. 2013, 15, 547–558. [Google Scholar] [CrossRef] [PubMed]
- Eşer, I.; Khorshid, L.; Yapucu Güneş, Ü.; Demir, Y. The Effect of Different Body Positions on Blood Pressure. J. Clin. Nurs. 2007, 16, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Huang, Q.F.; Yang, W.Y.; Asayama, K.; Zhang, Z.Y.; Thijs, L.; Li, Y.; O’Brien, E.; Staessen, J.A. Ambulatory Blood Pressure Monitoring to Diagnose and Manage Hypertension. Hypertension 2021, 77, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.D.; Liu, J.K.; Wen, B.; He, Q.Y.; Li, Y.; Miao, F. Cuffless Blood Pressure Estimation Using Pressure Pulse Wave Signals. Sensors 2018, 18, 4227. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Li, X.; Hu, H.; Zhang, L.; Huang, Z.; Lin, M.; Zhang, Z.; Yin, Z.; Huang, B.; Gong, H.; et al. Monitoring of the Central Blood Pressure Waveform via a Conformal Ultrasonic Device. Nat. Biomed. Eng. 2018, 2, 687–695. [Google Scholar] [CrossRef]
- Simjanoska, M.; Gjoreski, M.; Gams, M.; Bogdanova, A.M. Non-Invasive Blood Pressure Estimation from ECG Using Machine Learning Techniques. Sensors 2018, 18, 1160. [Google Scholar] [CrossRef]
- Schroeder, E.B.; Liao, D.; Chambless, L.E.; Prineas, R.J.; Evans, G.W.; Heiss, G. Hypertension, Blood Pressure, and Heart Rate Variability: The Atherosclerosis Risk in Communities (ARIC) Study. Hypertension 2003, 42, 1106–1111. [Google Scholar] [CrossRef]
- Osman, N.A.A.; Ibrahim, F.; Abas, W.A.B.W.; Rahman, H.S.A.; Ting, H.N.; Hassan, M.K.A.; Mashor, M.Y.; Nasir, N.F.M.; Mohamed, S. Measuring of Systolic Blood Pressure Based On Heart Rate. In IFMBE Proceedings, Proceedings of the 4th Kuala Lumpur International Conference on Biomedical Engineering 2008, Kuala Lumpur, Malaysia, 25–28 June 2008; Springer: Berlin/Heidelberg, Germany, 2008; Volume 21, pp. 595–598. [Google Scholar]
- Padilla, J.M.; Berjano, E.J.; Sáiz, J.; Rodriguez, R.; Fácila, L. Pulse Wave Velocity and Digital Volume Pulse as Indirect Estimators of Blood Pressure: Pilot Study on Healthy Volunteers. Cardiovasc. Eng. 2009, 9, 104–112. [Google Scholar] [CrossRef]
- Poon, C.C.Y.; Zhang, Y.-T. Cuff-Less and Noninvasive Measurements of Arterial Blood Pressure by Pulse Transit Time. In Proceedings of the 2005 IEEE Engineering in Medicine and Biology 27th Annual Conference, Shanghai, China, 31 August—3 September 2005; pp. 5877–5880. [Google Scholar]
- Mukkamala, R.; Hahn, J.O.; Inan, O.T.; Mestha, L.K.; Kim, C.S.; Toreyin, H.; Kyal, S. Toward Ubiquitous Blood Pressure Monitoring via Pulse Transit Time: Theory and Practice. IEEE Trans. Biomed. Eng. 2015, 62, 1879–1901. [Google Scholar] [CrossRef]
- Buxi, D.; Redouté, J.M.; Yuce, M.R. A Survey on Signals and Systems in Ambulatory Blood Pressure Monitoring Using Pulse Transit Time. Physiol. Meas. 2015, 36, R1–R26. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.W.; Lin, S.F. Wearable Piezoelectric-Based System for Continuous Beat-to-Beat Blood Pressure Measurement. Sensors 2020, 20, 851. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.-T.; Poon, C.C.Y.; Chan, C.-H.; Tsang, M.W.W.; Wu, K.-F. A Health-Shirt Using e-Textile Materials for the Continuous and Cuffless Monitoring of Arterial Blood Pressure. In Proceedings of the 2006 3rd IEEE/EMBS International Summer School on Medical Devices and Biosensors, Cambridge, MA, USA, 4–6 September 2006; pp. 86–89. [Google Scholar]
- Kumar, S.; Ayub, S. Estimation of Blood Pressure by Using Electrocardiogram (ECG) and Photo-Plethysmogram (PPG). In Proceedings of the 2015 5th International Conference on Communication Systems and Network Technologies, CSNT 2015, Gwalior, India, 4–6 April 2015; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA; pp. 521–524. [Google Scholar]
- Tortora, G.J.; Derrickson, B. Principles of Anatomy and Physiology, 12th ed.; John Wiley & Sons, Inc.: New York, NY, USA, 2008. [Google Scholar]
- Martin, A.; Voix, J. In-Ear Audio Wearable: Measurement of Heart and Breathing Rates for Health and Safety Monitoring. IEEE Trans. Biomed. Eng. 2018, 65, 1256–1263. [Google Scholar] [CrossRef]
- Lazareck, L.J.; Moussavi, Z.M.K. Classification of Normal and Dysphagic Swallows by Acoustical Means. IEEE Trans. Biomed. Eng. 2004, 51, 2103–2112. [Google Scholar] [CrossRef]
- Lanatà, A.; Pasquale Scilingo, E.; de Rossi, D. A Multimodal Transducer for Cardiopulmonary Activity Monitoring in Emergency. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 817–825. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Imtiaz, S.A.; Rodriguez-Villegas, E. Acoustic Sensing as a Novel Wearable Approach for Cardiac Monitoring at the Wrist. Sci. Rep. 2019, 9, 20079. [Google Scholar] [CrossRef] [PubMed]
- de Pinho Ferreira, N.; Gehin, C.; Massot, B. A Review of Methods for Non-Invasive Heart Rate Measurement on Wrist. IRBM 2021, 42, 4–18. [Google Scholar] [CrossRef]
- Fung, P.; Dumont, G.; Ries, C.; Mott, C.; Ansermino, M. Continuous Noninvasive Blood Pressure Measurement by Pulse Transit Time. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; pp. 738–741. [Google Scholar]
- Searle, A.; Kirkup, L. A Direct Comparison of Wet, Dry and Insulating Bioelectric Recording Electrodes. Physiol. Meas. 2000, 21, 271–283. [Google Scholar] [CrossRef]
- Kang, Y.; Choi, S.; Koo, C.; Joung, Y. Development and Optimization of Silicon−Dioxide−Coated Capacitive Electrode for Ambulatory ECG Measurement System. Sensors 2022, 22, 8388. [Google Scholar] [CrossRef]
- Pan, J.; Tompkins, W.J. A Real-Time QRS Detection Algorithm. IEEE Trans. Biomed. Eng. 1985, BME-32, 230–236. [Google Scholar] [CrossRef]
- White, W.B.; Berson, A.S.; Robbins, C.; Jamieson, M.J.; Prisant, L.M.; Roccella, E.; Sheps, S.G. National Standard for Measurement of Resting and Ambulatory Blood Pressures With Automated Sphygmomanometers. Hypertension 1993, 21, 504–509. [Google Scholar] [CrossRef] [PubMed]
- Lazazzera, R.; Belhaj, Y.; Carrault, G. A New Wearable Device for Blood Pressure Estimation Using Photoplethysmogram. Sensors 2019, 19, 2557. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.J.; Chen, C.H.; Sue, C.Y.; Lu, W.H.; Chiou, Y.H. Estimation of Blood Pressure in the Radial Artery Using Strain-Based Pulse Wave and Photoplethysmography Sensors. Micromachines 2018, 9, 556. [Google Scholar] [CrossRef] [PubMed]






| Day | Time | DBP Error (MAE ± SD mmHg) | SBP Error (MAE ± SD mmHg) |
|---|---|---|---|
| Day 1 | 09:00 | 2.23 ± 3.17 | 2.12 ± 2.42 |
| 15:00 | 3.10 ± 0.71 | 2.55 ± 3.54 | |
| 21:00 | 2.95 ± 1.85 | 1.92 ± 5.90 | |
| Day 2 | 09:00 | 3.60 ± 0.084 | 1.67 ± 7.38 |
| 15:00 | 2.17 ± 0.78 | 2.16 ± 2.93 | |
| 21:00 | 2.98 ± 2.35 | 1.75 ± 2.20 | |
| Day 3 | 09:00 | 2.89 ± 6.04 | 2.98 ± 2.25 |
| 15:00 | 3.25 ± 6.23 | 3.18 ± 5.61 | |
| 21:00 | 2.65 ± 3.88 | 2.20 ± 5.32 | |
| Day 4 | 09:00 | 2.81 ± 5.65 | 3.05 ± 2.42 |
| 15:00 | 2.16 ± 3.76 | 1.98 ± 3.40 | |
| 21:00 | 2.05 ± 4.95 | 2.57 ± 2.82 | |
| Day 5 | 09:00 | 2.87 ± 1.76 | 1.39 ± 1.72 |
| 15:00 | 2.90 ± 3.80 | 2.17 ± 2.07 | |
| 21:00 | 2.22 ± 5.48 | 2.71 ± 3.04 | |
| Average | 2.72 ± 3.42 | 2.29 ± 3.53 | |
| Authors | Technique | Statistical Method | SBP Error (mmHg) | DBP Error (mmHg) | Ref |
|---|---|---|---|---|---|
| Lazazzera et al. | PTT (ECG, PPG) | MAE ± SD | 1.52 ± 9.45 | 0.39 ± 4.93 | [28] |
| Simjanoska et al. | PTT (ECG) | MAE ± SD | 7.72 ± 10.22 | 9.45 ± 10.03 | [7] |
| Wang et al. | PTT (Strain-based pulse wave sensor, PPG) | MAE ± SD | 3.71 ± 3.06 | 5.44 ± 5.10 | [29] |
| Present Work | PTT (ECG, Microphone) | MAE ± SD | 2.72 ± 3.42 | 2.29 ±3.53 | This work |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, J.; Kang, Y.; Park, J.; Joung, Y.; Koo, C. Development of Real-Time Cuffless Blood Pressure Measurement Systems with ECG Electrodes and a Microphone Using Pulse Transit Time (PTT). Sensors 2023, 23, 1684. https://doi.org/10.3390/s23031684
Choi J, Kang Y, Park J, Joung Y, Koo C. Development of Real-Time Cuffless Blood Pressure Measurement Systems with ECG Electrodes and a Microphone Using Pulse Transit Time (PTT). Sensors. 2023; 23(3):1684. https://doi.org/10.3390/s23031684
Chicago/Turabian StyleChoi, Jingyu, Younghwan Kang, Jaesoon Park, Yeunho Joung, and Chiwan Koo. 2023. "Development of Real-Time Cuffless Blood Pressure Measurement Systems with ECG Electrodes and a Microphone Using Pulse Transit Time (PTT)" Sensors 23, no. 3: 1684. https://doi.org/10.3390/s23031684
APA StyleChoi, J., Kang, Y., Park, J., Joung, Y., & Koo, C. (2023). Development of Real-Time Cuffless Blood Pressure Measurement Systems with ECG Electrodes and a Microphone Using Pulse Transit Time (PTT). Sensors, 23(3), 1684. https://doi.org/10.3390/s23031684







