Cushioned Footwear Effect on Pain and Gait Characteristics of Individuals with Knee Osteoarthritis: A Double-Blinded 3 Month Intervention Study
Abstract
1. Introduction
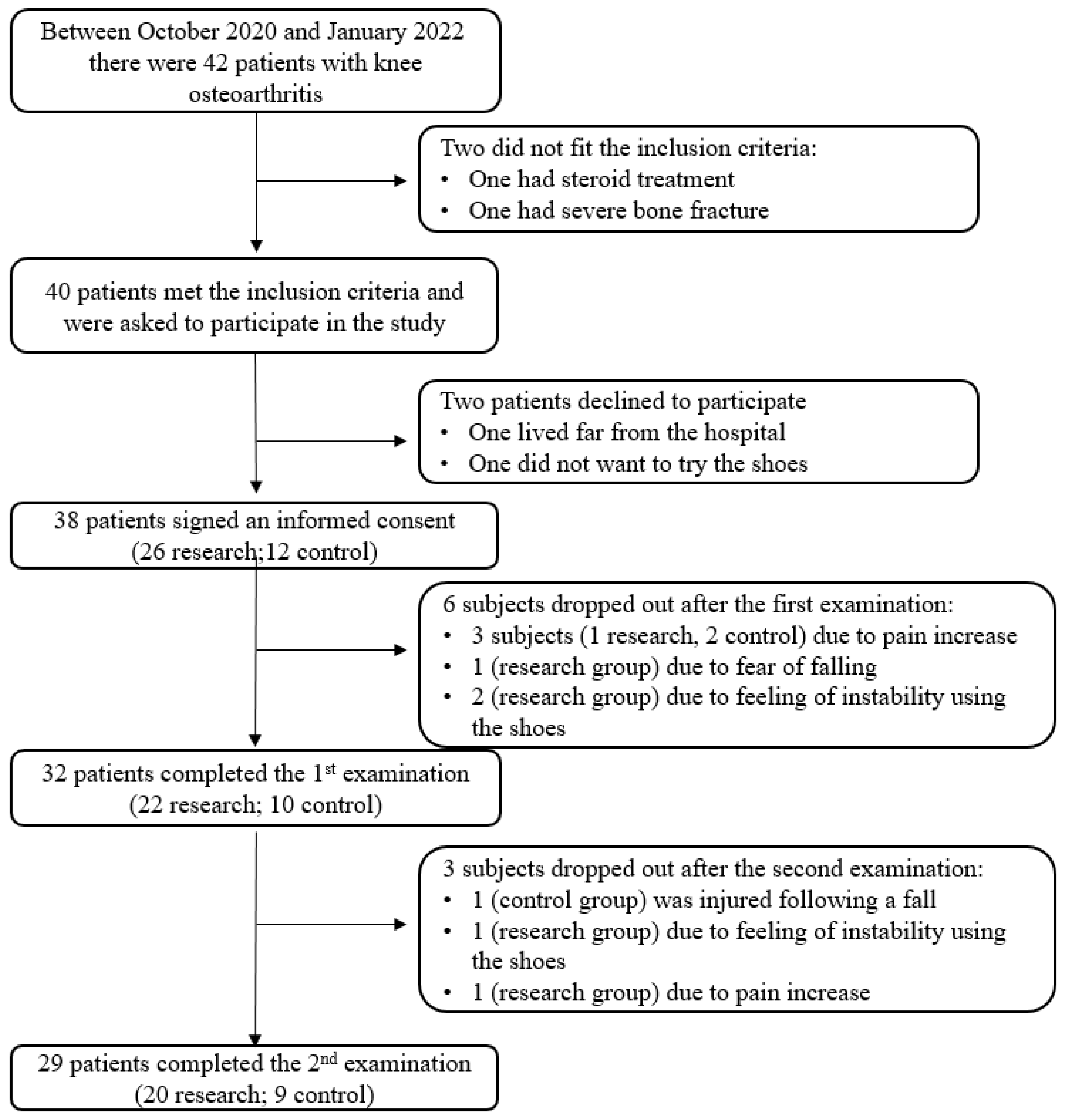
2. Materials and Methods
2.1. Population
2.2. Tools
2.3. Study Protocol
2.4. Statistical Analyses
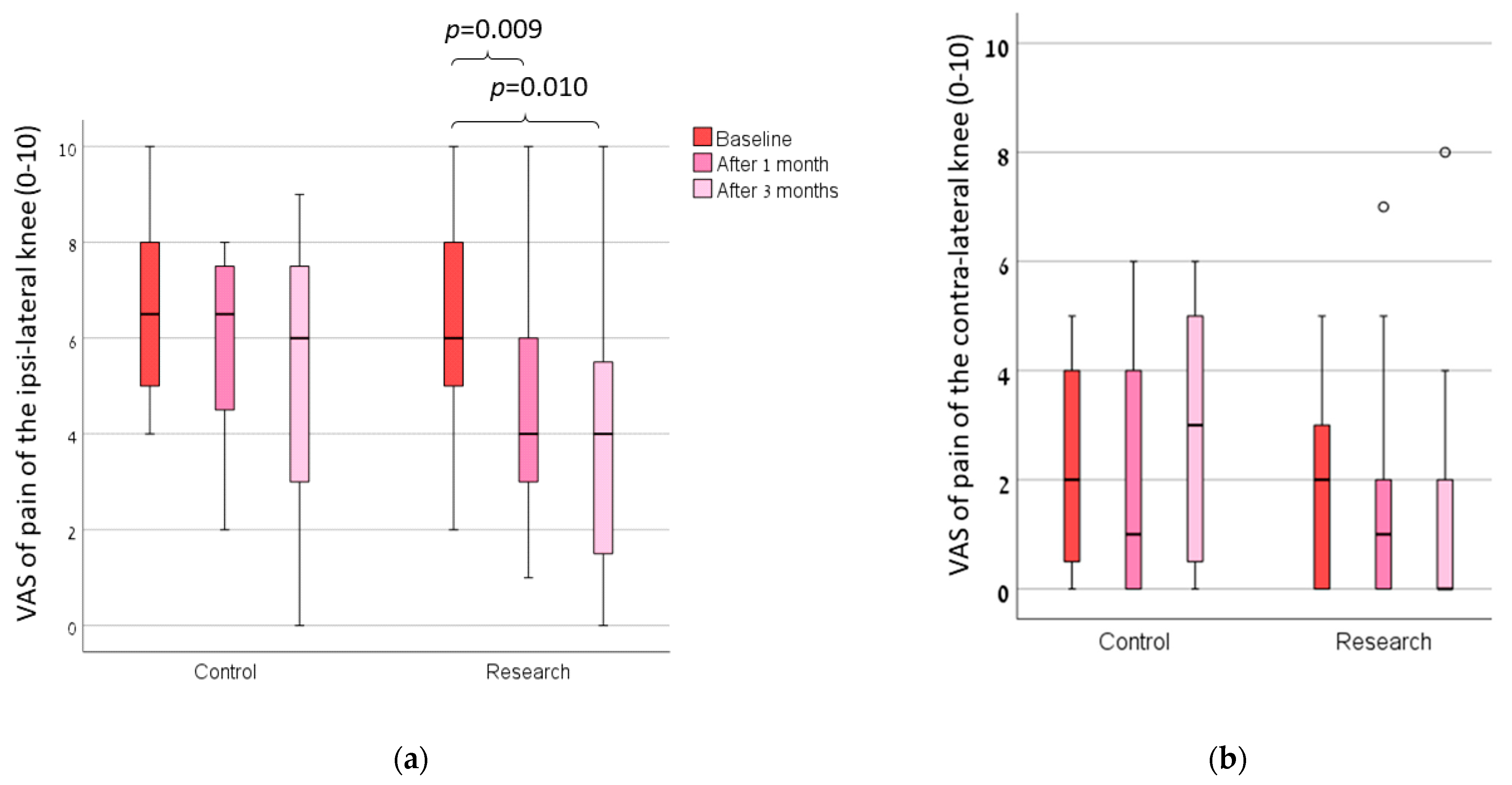
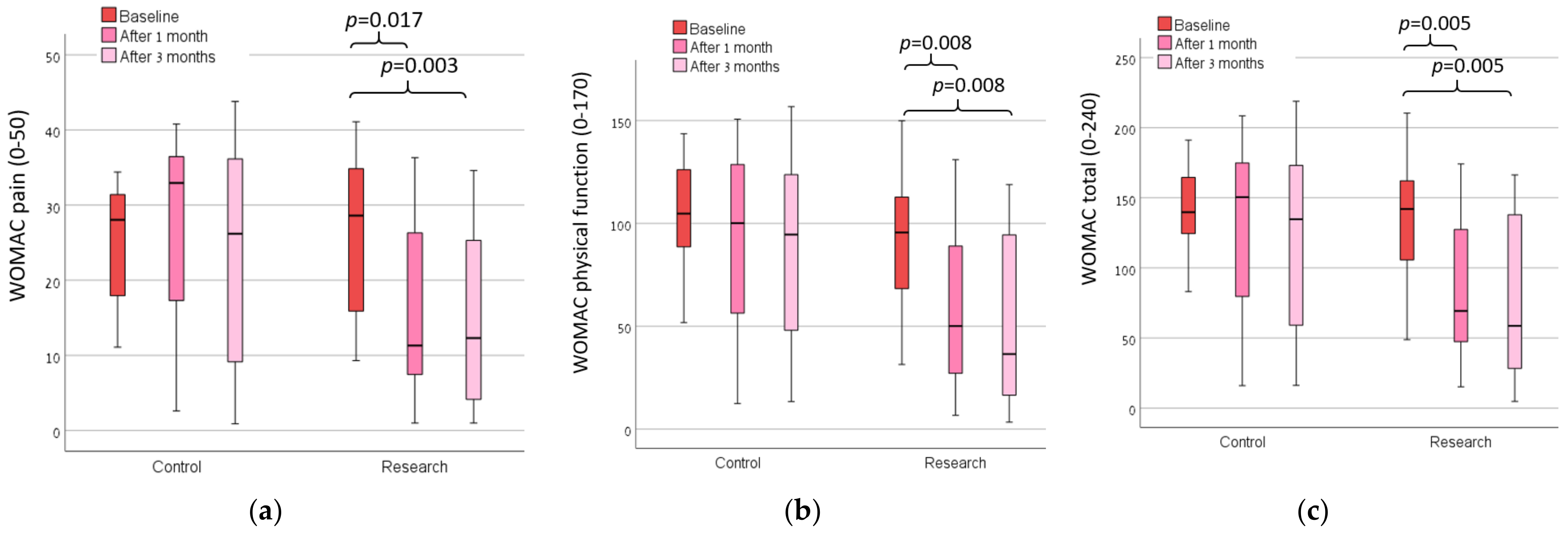
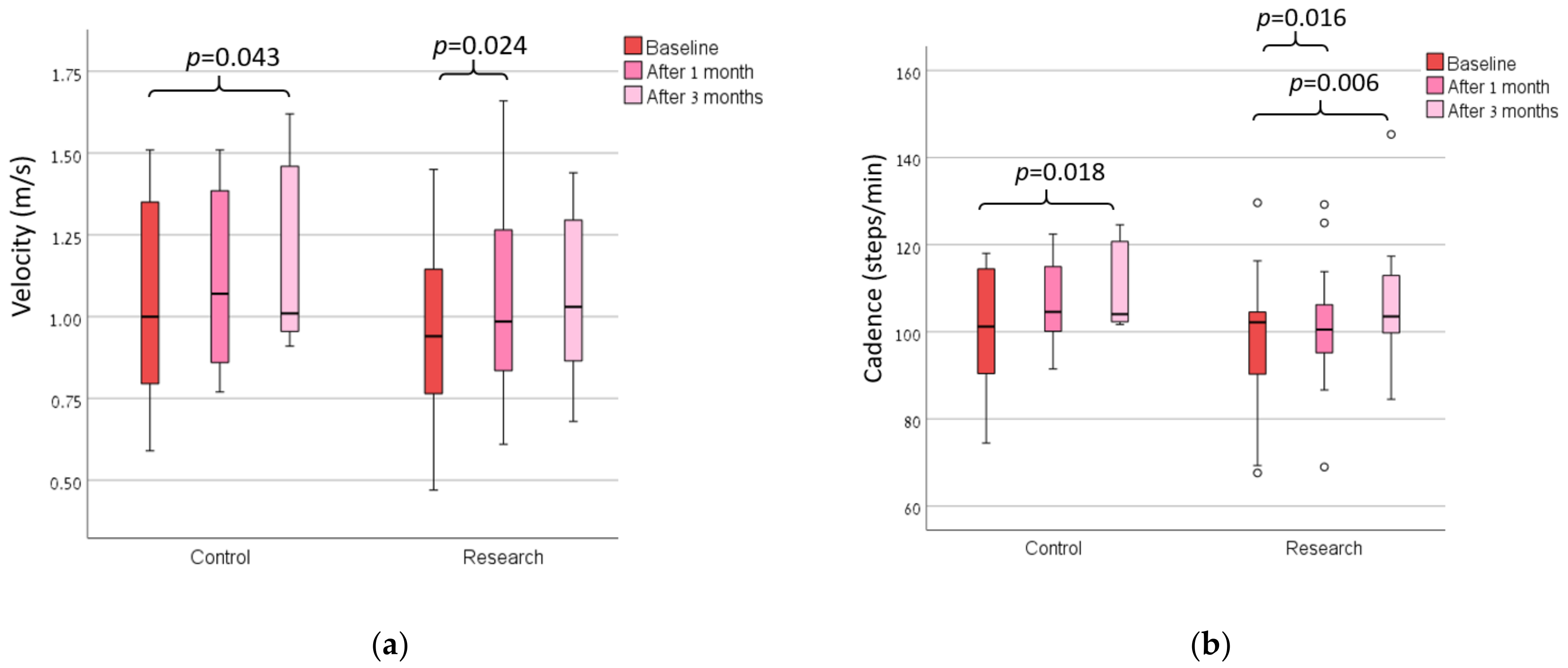
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hunter, D.J.; Lo, G.H. The Management of Osteoarthritis: An Overview and Call to Appropriate Conservative Treatment. Med. Clin. N. Am. 2009, 93, 127–143. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, R.C.; Felson, D.T.; Helmick, C.G.; Arnold, L.M.; Choi, H.; Deyo, R.A.; Gabriel, S.; Hirsch, R.; Hochberg, M.C.; Hunder, G.G.; et al. Estimates of the Prevalence of Arthritis and Other Rheumatic Conditions in the United States: Part II. Arthritis Rheum. 2008, 58, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.; Kean, W.F. Obesity and Knee Osteoarthritis. Inflammopharmacology 2012, 20, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Abbasi, J. Can Exercise Prevent Knee Osteoarthritis? JAMA 2017, 318, 2169–2171. [Google Scholar] [CrossRef] [PubMed]
- Vincent, K.R.; Vincent, H.K. Resistance Exercise for Knee Osteoarthritis. PMR 2012, 4, S45–S52. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Merchan, E.C.; De La Corte-Rodriguez, H. The Role of Orthoses in Knee Osteoarthritis. Hosp. Pract. 2019, 47, 1–5. [Google Scholar] [CrossRef]
- Duivenvoorden, T.; Brouwer, R.W.; van Raaij, T.M.; Verhagen, A.P.; Verhaar, J.A.N.; Bierma-Zeinstra, S.M.A. Braces and Orthoses for Treating Osteoarthritis of the Knee. Cochrane Database Syst. Rev. 2015, 2015, 3. [Google Scholar] [CrossRef]
- Mohd Sharif, N.A.; Goh, S.L.; Usman, J.; Wan Safwani, W.K.Z. Biomechanical and Functional Efficacy of Knee Sleeves: A Literature Review. Phys. Ther. Sport 2017, 28, 44–52. [Google Scholar] [CrossRef]
- Vangsness, C.T.; Spiker, W.; Erickson, J. A Review of Evidence-Based Medicine for Glucosamine and Chondroitin Sulfate Use in Knee Osteoarthritis. Arthrosc. J. Arthrosc. Relat. Surg. 2009, 25, 86–94. [Google Scholar] [CrossRef]
- Quinn, R.H.; Murray, J.N.; Pezold, R.; Sevarino, K.S. Surgical Management of Osteoarthritis of the Knee. J. Am. Acad. Orthop. Surg. 2018, 26, e191–e193. [Google Scholar] [CrossRef]
- Bar-Ziv, Y.; Beer, Y.; Ran, Y.; Benedict, S.; Halperin, N. A Treatment Applying a Biomechanical Device to the Feet of Patients with Knee Osteoarthritis Results in Reduced Pain and Improved Function: A Prospective Controlled Study. BMC Musculoskelet. Disord. 2010, 11, 179. [Google Scholar] [CrossRef] [PubMed]
- Carlos Rodriguez-Merchan, E.; De la Corte-Rodriguez, H.; Roman-Belmonte, J.M. The Effect of Biomechanical Footwear on Pain from Knee Osteoarthritis. Arch. Bone Jt. Surg. 2022, 10, 381–384. [Google Scholar]
- Nigg, B.M.; Emery, C.; Hiemstra, L.A. Unstable Shoe Construction and Reduction of Pain in Osteoarthritis Patients. Med. Sci. Sports Exerc. 2006, 38, 1701–1708. [Google Scholar] [CrossRef] [PubMed]
- Chughtai, M.; Newman, J.M.; Akil, S.; Khlopas, A.; Sultan, A.A.; Sodhi, N.; Bhave, A.; Harwin, S.F.; Mont, M.A. Knee Pain and the Use of Various Types of Footwear—A Review. J. Knee Surg. 2018, 31, 952–964. [Google Scholar] [CrossRef] [PubMed]
- Bennell, K.L.; Kean, C.O.; Wrigley, T.V.; Hinman, R.S. Effects of a Modified Shoe on Knee Load in People with and Those without Knee Osteoarthritis. Arthritis Rheum. 2013, 65, 701–709. [Google Scholar] [CrossRef]
- Rodrigues, P.T.; Ferreira, A.F.; Pereira, R.M.R.; Bonfá, E.; Borba, E.F.; Fuller, R. Effectiveness of Medial-Wedge Insole Treatment for Valgus Knee Osteoarthritis. Arthritis Care Res. 2008, 59, 603–608. [Google Scholar] [CrossRef]
- Trombini-Souza, F.; Fuller, R.; Goldenstein-Schainberg, C.; Sacco, I.C.N. Long-Term Use of Minimal Footwear in Older Adult Women with Knee Osteoarthritis: Mechanisms of Action in the Knee Adduction Moment. J. Biomech. 2020, 108, 109885. [Google Scholar] [CrossRef]
- Shakoor, N.; Lidtke, R.H.; Wimmer, M.A.; Mikolaitis, R.A.; Foucher, K.C.; Thorp, L.E.; Fogg, L.F.; Block, J.A. Improvement in Knee Loading after Use of Specialized Footwear for Knee Osteoarthritis: Results of a Six-Month Pilot Investigation. Arthritis Rheum. 2013, 65, 1282–1289. [Google Scholar] [CrossRef]
- Hinman, R.S.; Wrigley, T.V.; Metcalf, B.R.; Campbell, P.K.; Paterson, K.L.; Hunter, D.J.; Kasza, J.; Forbes, A.; Bennell, K.L. Unloading Shoes for Self-Management of Knee Osteoarthritis a Randomized Trial. Ann. Intern. Med. 2016, 165, 381–389. [Google Scholar] [CrossRef]
- Paterson, K.L.; Wrigley, T.V.; Bennell, K.L.; Hinman, R.S. A Survey of Footwear Advice, Beliefs and Wear Habits in People with Knee Osteoarthritis. J. Foot Ankle Res. 2014, 7, 43. [Google Scholar] [CrossRef]
- Hannigan, J.J.; Pollard, C.D. Comparing Walking Biomechanics of Older Females in Maximal, Minimal, and Traditional Shoes. Gait Posture 2021, 83, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Cueva, J.H.; Castillo, D.; Espinós-Morató, H.; Durán, D.; Díaz, P.; Lakshminarayanan, V. Detection and Classification of Knee Osteoarthritis. Diagnostics 2022, 12, 2362. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test-Retest Reliability, Validity, and Minimum Detectable Change of Visual Analog, Numerical Rating, and Verbal Rating Scales for Measurement of Osteoarthritic Knee Pain. J. Pain Res. 2018, 11, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological Assessment of Osteo-Arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef] [PubMed]
- Akizuki, K.; Yamaguchi, K.; Morita, Y.; Ohashi, Y. The Effect of Proficiency Level on Measurement Error of Range of Motion. J. Phys. Ther. Sci. 2016, 28, 2644–2651. [Google Scholar] [CrossRef] [PubMed]
- Tubach, F.; Ravaud, P.; Baron, G.; Falissard, B.; Logeart, I.; Bellamy, N.; Bombardier, C.; Felson, D.; Hochberg, M.; Van Der Heijde, D.; et al. Evaluation of Clinically Relevant Changes in Patient Reported Outcomes in Knee and Hip Osteoarthritis: The Minimal Clinically Important Improvement. Ann. Rheum. Dis. 2005, 64, 29–33. [Google Scholar] [CrossRef]
- Bellamy, N.; Buchanan, W.W.; Goldsmith, C.H.; Campbell, J.; Stitt, L.W. Validation Study of WOMAC: A Health Status Instrument for Measuring Clinically Important Patient Relevant Outcomes to Antirheumatic Drug Therapy in Patients with Osteoarthritis of the Hip or Knee. J. Rheumatol. 1988, 15, 1833–1840. [Google Scholar]
- Williams, V.J.; Piva, S.R.; Irrgang, J.J.; Crossley, C.; Fitzgerald, G.K. Comparison of Reliability and Responsiveness of Patient-Reported Clinical Outcome Measures in Knee Osteoarthritis Rehabilitation. J. Orthop. Sports Phys. Ther. 2012, 42, 716–723. [Google Scholar] [CrossRef]
- Kennedy, D.M.; Stratford, P.W.; Wessel, J.; Gollish, J.D.; Penney, D. Assessing Stability and Change of Four Performance Measures: A Longitudinal Study Evaluating Outcome Following Total Hip and Knee Arthroplasty. BMC Musculoskelet. Disord. 2005, 6, 3. [Google Scholar] [CrossRef]
- Kim, C.M.; Eng, J.J. Symmetry in Vertical Ground Reaction Force Is Accompanied by Symmetry in Temporal but Not Distance Variables of Gait in Persons with Stroke. Gait Posture 2003, 18, 23–28. [Google Scholar] [CrossRef]
- Gilbert, A.L.; Song, J.; Cella, D.; Chang, R.W.; Dunlop, D.D. What Is an Important Difference in Gait Speed in Adults With Knee Osteoarthritis? Arthritis Care Res. 2021, 73, 559–565. [Google Scholar] [CrossRef] [PubMed]
- Arnold, J.B.; Wong, D.X.; Jones, R.K.; Hill, C.L.; Thewlis, D. Lateral Wedge Insoles for Reducing Biomechanical Risk Factors for Medial Knee Osteoarthritis Progression: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2016, 68, 936–951. [Google Scholar] [CrossRef] [PubMed]
- Faber, J.; Fonseca, L.M. How Sample Size Influences Research Outcomes. Dental Press J. Orthod. 2014, 19, 27–29. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: Abingdon, UK, 1988. [Google Scholar]
- De Rooij, M.; Van Der Leeden, M.; Heymans, M.W.; Holla, J.F.M.; Häkkinen, A.; Lems, W.F.; Roorda, L.D.; Veenhof, C.; Sanchez-Ramirez, D.C.; De Vet, H.C.W.; et al. Prognosis of Pain and Physical Functioning in Patients with Knee Osteoarthritis: A Systematic Review and Meta-Analysis. Arthritis Care Res. 2016, 68, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Teichtahl, A.J.; Abram, F.; Hussain, S.M.; Pelletier, J.P.; Cicuttini, F.M.; Martel-Pelletier, J. Knee Pain as a Predictor of Structural Progression over 4 Years: Data from the Osteoarthritis Initiative, a Prospective Cohort Study. Arthritis Res. Ther. 2018, 20, 250. [Google Scholar] [CrossRef]
- Covinsky, K.E.; Lindquist, K.; Dunlop, D.D.; Gill, T.M.; Yelin, E. Effect of Arthritis in Middle Age on Older-Age Functioning. J. Am. Geriatr. Soc. 2008, 56, 23–28. [Google Scholar] [CrossRef]
- Elkarif, V.; Kandel, L.; Rand, D.; Schwartz, I.; Greenberg, A.; Portnoy, S. Kinematics Following Gait Perturbation in Adults with Knee Osteoarthritis: Scheduled versus Not Scheduled for Knee Arthroplasty. Gait Posture 2020, 81, 144–152. [Google Scholar] [CrossRef]
- Elkarif, V.; Kandel, L.; Rand, D.; Schwartz, I.; Greenberg, A.; Portnoy, S. Muscle Activity While Ambulating on Stairs and Slopes: A Comparison between Individuals Scheduled and Not Scheduled for Knee Arthroplasty and Healthy Controls. Musculoskelet. Sci. Pract. 2021, 52, 102346. [Google Scholar] [CrossRef]
| Research Group (N = 26) | Control Group (N = 12) | p | |
|---|---|---|---|
| Age (years) | 67.5 ± 8.8 | 64.6 ± 8.0 | 0.171 |
| Sex | 9 males, 17 females | 8 males, 4 females | 0.516 |
| Height (m) | 164.4 ± 9.6 | 167.6 ± 7.6 | 0.271 |
| Weight (kg) | 84.7 ± 15.5 | 86.5 ± 11.3 | 0.765 |
| Shoe size (EU) | 40.3 ± 2.6 | 40.8 ± 2.1 | 0.412 |
| Ipsi-lateral knee | 15 right, 11 left | 7 right, 5 left | 0.330 |
| Kellgren and Lawrence classification (0–4) | 2.7 ± 0.7 | 3.3 ± 0.9 | 0.078 |
| Flexion ROM of the ipsi-lateral knee (°) | 117.1 ± 9.3 | 118.3 ± 9.4 | 0.610 |
| VAS ipsi-lateral knee (1–10) | 6.5 ±2.1 | 7.2 ± 2.0 | 0.381 |
| VAS contra-lateral knee (1–10) | 2.4 ± 2.3 | 2.6 ± 2.5 | 0.797 |
| TUG (s) | 14.1 ± 4.2 | 13.3 ± 5.2 | 0.335 |
| WOMAC pain (0–50) | 28.4 ± 10.5 | 23.5 ± 10.4 | 0.172 |
| WOMAC stiffness (0–20) | 12.0 ± 5.7 | 11.1 ± 5.0 | 0.649 |
| WOMAC physical function (0–170) | 98.8 ± 34.3 | 95.0 ± 40.3 | 0.733 |
| WOMAC total (0–240) | 141.0 ± 48.2 | 129.6 ± 52.4 | 0.451 |
| Time Effects | Group Effects | Group by Time Interaction | ||||
|---|---|---|---|---|---|---|
| p | η2 | p | η2 | p | η2 | |
| Flexion ROM of the ipsi-lateral knee (°) | 0.065 | 0.103 | 0.659 | 0.008 | 0.132 | 0.078 |
| VAS ipsi-lateral knee (1–10) | 0.003 | 0.206 | 0.295 | 0.044 | 0.586 | 0.021 |
| VAS contra-lateral knee (1–10) | 0.783 | 0.010 | 0.324 | 0.039 | 0.261 | 0.052 |
| TUG (s) | 0.238 | 0.058 | 0.493 | 0.020 | 0.698 | 0.015 |
| WOMAC pain (0–50) | 0.044 | 0.117 | 0.165 | 0.076 | 0.040 | 0.121 |
| WOMAC stiffness (0–20) | 0.080 | 0.096 | 0.124 | 0.092 | 0.795 | 0.009 |
| WOMAC physical function (0–170) | 0.003 | 0.213 | 0.070 | 0.131 | 0.379 | 0.040 |
| WOMAC total (0–240) | 0.003 | 0.203 | 0.107 | 0.101 | 0.234 | 0.056 |
| Velocity (m/s) | 0.005 | 0.223 | 0.386 | 0.036 | 0.750 | 0.014 |
| Cadence (steps/min) | <0.001 | 0.302 | 0.504 | 0.022 | 0.704 | 0.017 |
| Stance duration of the ipsi-lateral limb (%GC) | 0.067 | 0.121 | 0.532 | 0.019 | 0.298 | 0.056 |
| Step length of the ipsi-lateral limb (cm) | 0.036 | 0.153 | 0.291 | 0.056 | 0.088 | 0.114 |
| Base width of the ipsi-lateral limb (cm) | 0.901 | 0.005 | 0.964 | <0.001 | 0.529 | 0.030 |
| Stance duration SI (0–200) | 0.442 | 0.038 | 0.192 | 0.080 | 0.927 | 0.004 |
| Double support duration SI (0–200) | 0.193 | 0.075 | 0.972 | <0.001 | 0.899 | 0.005 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwartz, I.; Ofran, Y.; Bernovsky, S.; Kandel, L.; Rivkin, G.; Karniel, N.; Seyres, M.; Portnoy, S. Cushioned Footwear Effect on Pain and Gait Characteristics of Individuals with Knee Osteoarthritis: A Double-Blinded 3 Month Intervention Study. Sensors 2023, 23, 1375. https://doi.org/10.3390/s23031375
Schwartz I, Ofran Y, Bernovsky S, Kandel L, Rivkin G, Karniel N, Seyres M, Portnoy S. Cushioned Footwear Effect on Pain and Gait Characteristics of Individuals with Knee Osteoarthritis: A Double-Blinded 3 Month Intervention Study. Sensors. 2023; 23(3):1375. https://doi.org/10.3390/s23031375
Chicago/Turabian StyleSchwartz, Isabella, Yonah Ofran, Svetlana Bernovsky, Leonid Kandel, Gurion Rivkin, Naama Karniel, Martin Seyres, and Sigal Portnoy. 2023. "Cushioned Footwear Effect on Pain and Gait Characteristics of Individuals with Knee Osteoarthritis: A Double-Blinded 3 Month Intervention Study" Sensors 23, no. 3: 1375. https://doi.org/10.3390/s23031375
APA StyleSchwartz, I., Ofran, Y., Bernovsky, S., Kandel, L., Rivkin, G., Karniel, N., Seyres, M., & Portnoy, S. (2023). Cushioned Footwear Effect on Pain and Gait Characteristics of Individuals with Knee Osteoarthritis: A Double-Blinded 3 Month Intervention Study. Sensors, 23(3), 1375. https://doi.org/10.3390/s23031375







