Physical Noninvasive Attacks on Photoplethysmogram by Computer Controlled Blood Pressure Cuff
Abstract
:1. Introduction
- We clarified the danger of attacks by modifying the biometric information on the device wearer and made people aware that pulse wave data can be easily manipulated.
- We implemented the proposed method in a device and showed that the proposed method can be used to attack PPG by displaying incorrect heart rate values in a smartwatch application.
- The proposed method will be used to generate specific pulse waveforms, which will involve basic research for use in interaction, communication, and other technologies.
2. Related Works
2.1. Studies on Attack Methods on Sensors and IoT
2.2. Studies on Using Pulse Waves
3. Proposed Method
3.1. Effect of Upper Arm Compression on Pulse Wave Measurement
3.2. Device Configuration
3.3. Overview of the Proposed Method
3.4. Calibration
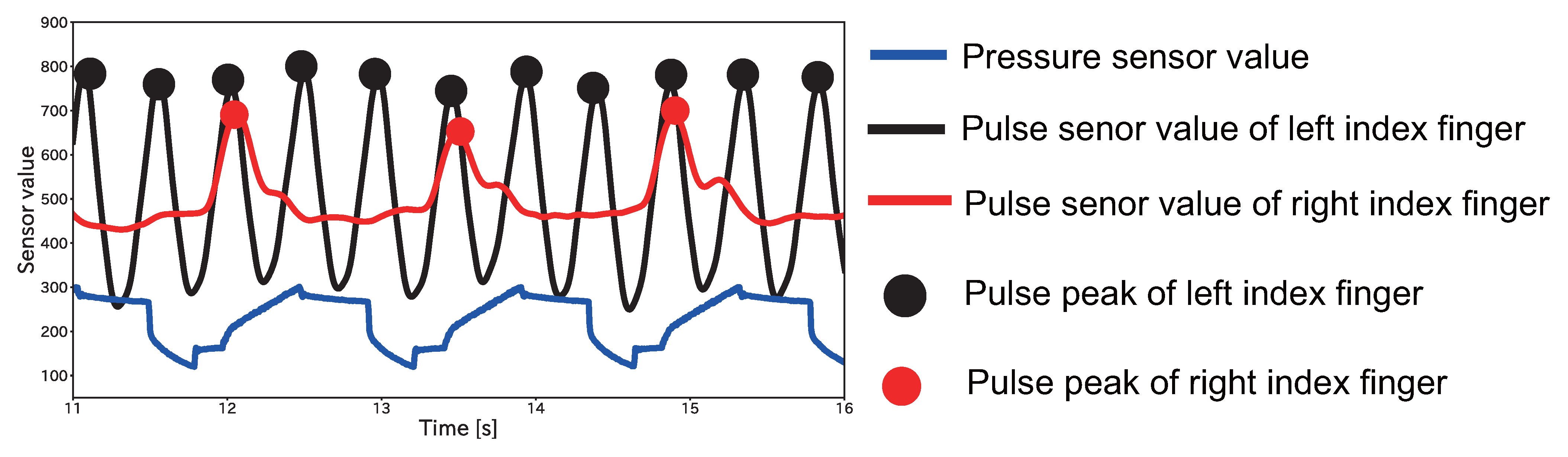
3.5. Pulse Wave Control
3.6. Implementation
4. Evaluation Experiment
4.1. Experiment Environment
4.1.1. Data Collection
4.1.2. Evaluation Index
4.2. Investigation of Limitations of Smartwatches in Displayed Heartbeat
4.2.1. Experiment Environment
4.2.2. Results
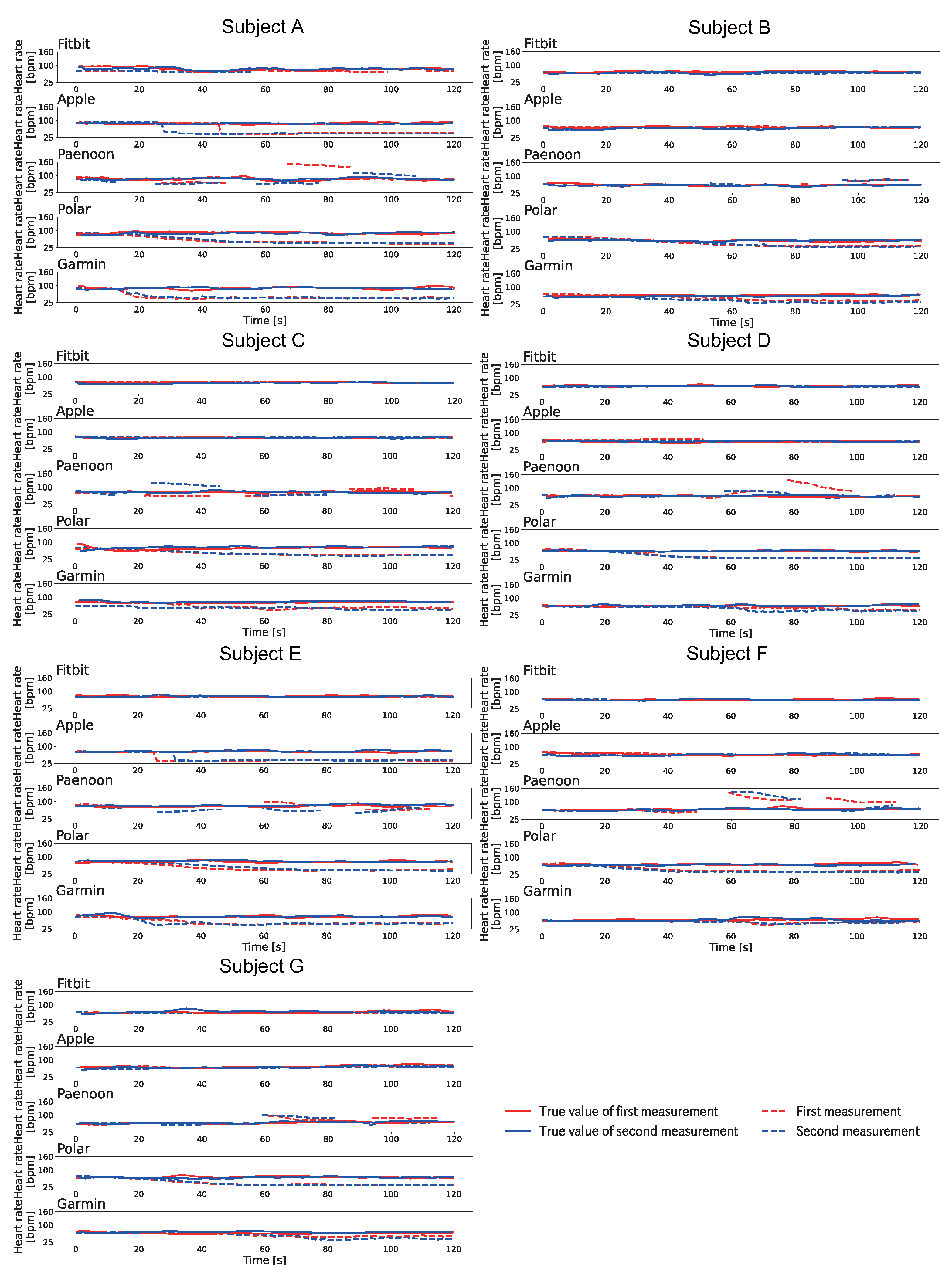
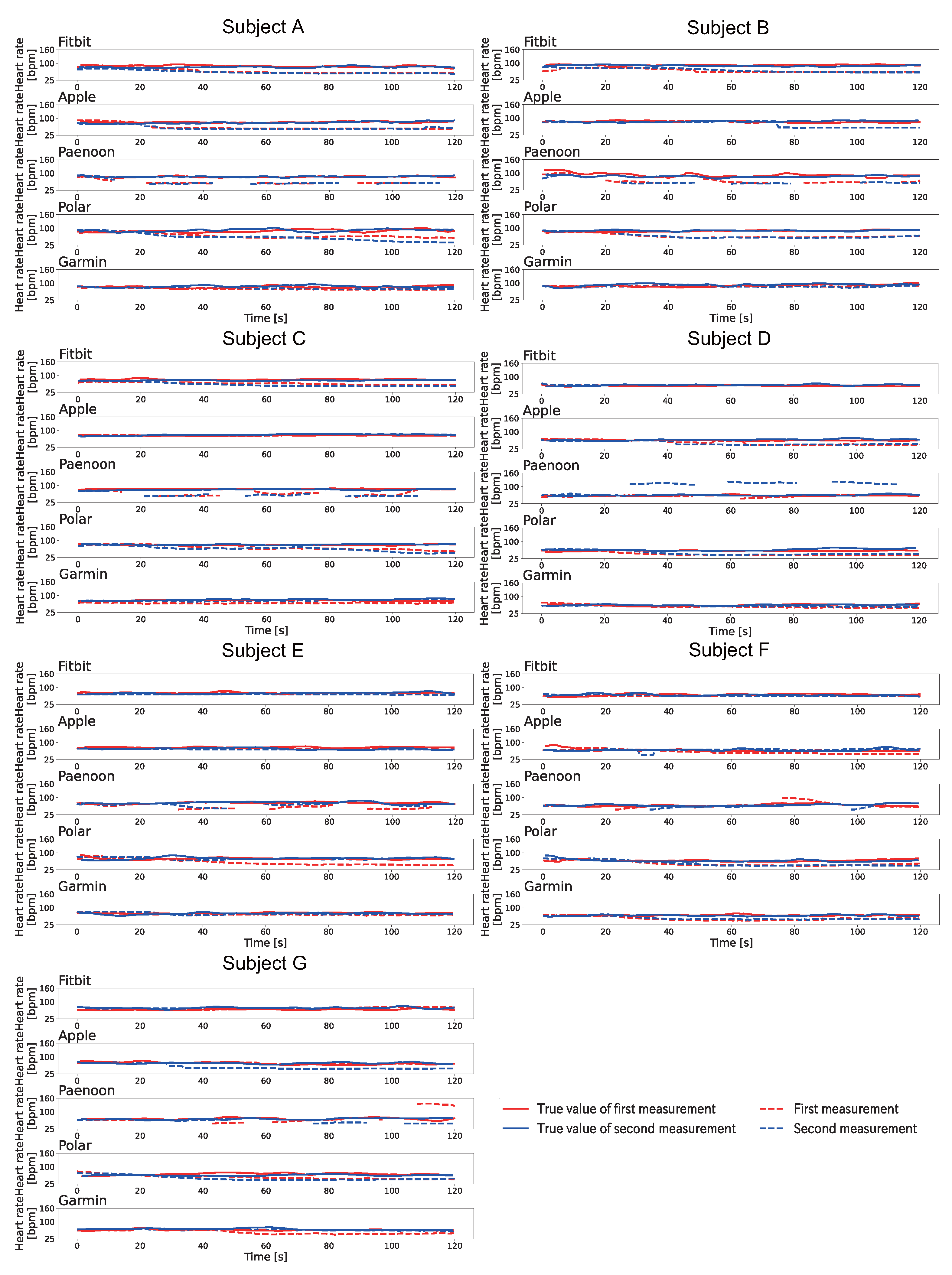
4.3. Results of Heart Rate Changes at Rest by Pulse Wave Control
4.3.1. The Results of Pattern A
4.3.2. The Results of Pattern B
4.3.3. The Results of Pattern C
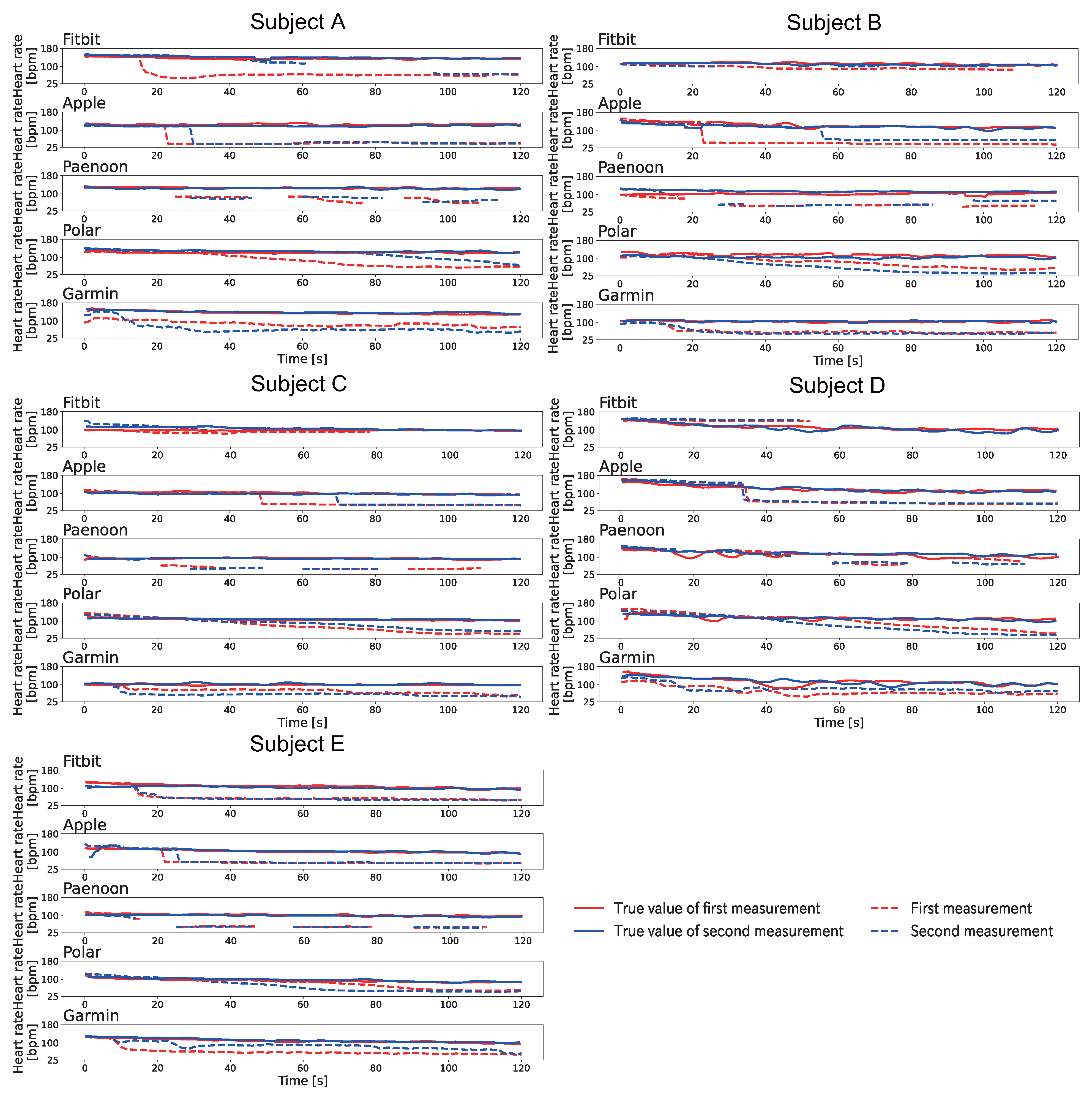
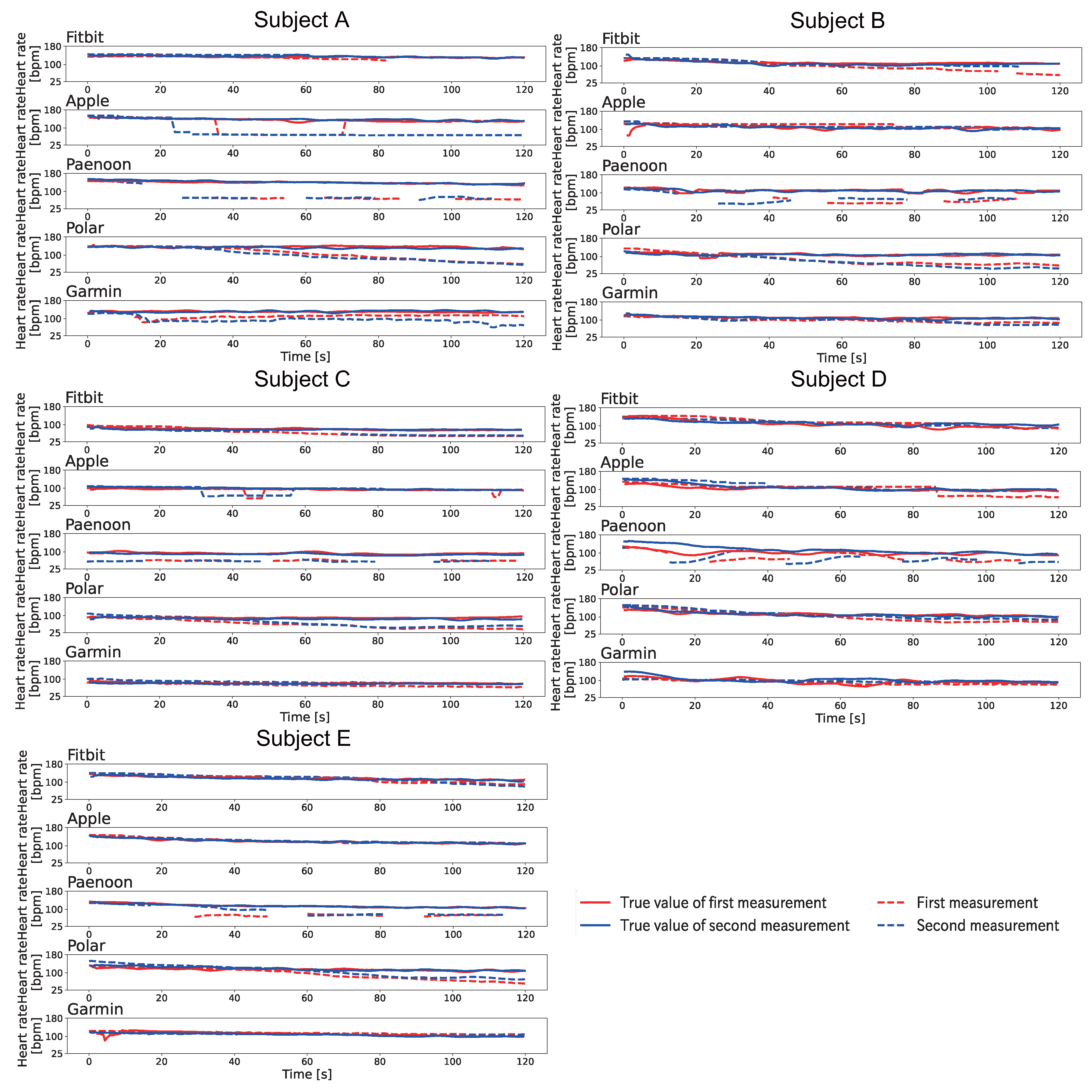
4.4. Results of Heart Rate Changes after Exercise Using Pulse Wave Control
4.4.1. The Results of Pattern A
4.4.2. The Results of Pattern B
4.4.3. The Results of Pattern C
5. Discussion
5.1. Time for Upper Arm Pressure
5.2. The Pulse Waveform When the Proposed Method Was Used
5.3. Pulse Wave Measurement Position
5.4. Experiment Subjects
5.5. Impact on the Real-World Scenario
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eykholt, K.; Evtimov, I.; Fernandes, E.; Li, B.; Rahmati, A.; Xiao, C.; Prakash, A.; Kohno, T.; Song, D. Robust physical-world attacks on deep learning visual classification. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition, Salt Lake City, UT, USA, 18–23 June 2018; pp. 1625–1634. [Google Scholar]
- Trippel, T.; Weisse, O.; Xu, W.; Honeyman, P.; Fu, K. WALNUT: Waging Doubt on the Integrity of MEMS Accelerometers with Acoustic Injection Attacks. In Proceedings of the 2017 IEEE European Symposium on Security and Privacy (EuroS P), Paris, France, 26–28 April 2017; pp. 3–18. [Google Scholar] [CrossRef]
- Company, S.L.I. Vitality. 2018. Available online: https://www.sumitomolife.co.jp/english/newsrelease/pdf/nr20180719.pdf (accessed on 6 December 2023).
- Sharif, M.; Bhagavatula, S.; Bauer, L.; Reiter, M.K. Accessorize to a Crime: Real and Stealthy Attacks on State-of-the-Art Face Recognition. In Proceedings of the 2016 ACM SIGSAC Conference on Computer and Communications Security, CCS ’16, New York, NY, USA, 24–28 October 2016; pp. 1528–1540. [Google Scholar] [CrossRef]
- Yamada, T.; Gohshi, S.; Echizen, I. Privacy Visor: Method Based on Light Absorbing and Reflecting Properties for Preventing Face Image Detection. In Proceedings of the 2013 IEEE International Conference on Systems, Man, and Cybernetics, Manchester, UK, 13–16 October 2013; pp. 1572–1577. [Google Scholar] [CrossRef]
- Fujii, A.; Murao, K.; Matsuhisa, N. Disp2ppg: Pulse wave generation to PPG sensor using display. In 2021 International Symposium on Wearable Computers; Association for Computing Machinery: New York, NY, USA, 2021; pp. 119–123. [Google Scholar]
- Farrukh, H.; Yang, T.; Xu, H.; Yin, Y.; Wang, H.; Celik, Z.B. S3: Side-Channel Attack on Stylus Pencil through Sensors. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2021, 5, 1–25. [Google Scholar] [CrossRef]
- Gazzari, M.; Mattmann, A.; Maass, M.; Hollick, M. My(o) Armband Leaks Passwords: An EMG and IMU Based Keylogging Side-Channel Attack. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2022, 5, 1–25. [Google Scholar] [CrossRef]
- Shen, M.; Liao, Z.; Zhu, L.; Xu, K.; Du, X. VLA: A Practical Visible Light-Based Attack on Face Recognition Systems in Physical World. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2019, 3, 1–19. [Google Scholar] [CrossRef]
- Dürichen, R.; Verma, K.D.; Yee, S.Y.; Rocznik, T.; Schmidt, P.; Bödecker, J.; Peters, C. Prediction of Electrocardiography Features Points Using Seismocardiography Data: A Machine Learning Approach. In Proceedings of the 2018 ACM International Symposium on Wearable Computers, ISWC ’18, New York, NY, USA, 8–12 October 2018; pp. 96–99. [Google Scholar] [CrossRef]
- Rajala, S.; Lindholm, H.; Taipalus, T. Comparison of photoplethysmogram measured from wrist and finger and the effect of measurement location on pulse arrival time. Physiol. Meas. 2018, 39, 075010. [Google Scholar] [CrossRef] [PubMed]
- Yoon, Y.Z.; Kang, J.M.; Kwon, Y.; Park, S.; Noh, S.; Kim, Y.; Park, J.; Hwang, S.W. Cuff-Less Blood Pressure Estimation Using Pulse Waveform Analysis and Pulse Arrival Time. IEEE J. Biomed. Health Inform. 2018, 22, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.D.; Liu, J.K.; Wen, B.; He, Q.Y.; Li, Y.; Miao, F. Cuffless Blood Pressure Estimation Using Pressure Pulse Wave Signals. Sensors 2018, 18, 4227. [Google Scholar] [CrossRef] [PubMed]
- Sun, S.; Bezemer, R.; Long, X.; Muehlsteff, J.; Aarts, R.M. Systolic blood pressure estimation using PPG and ECG during physical exercise. Physiol. Meas. 2016, 37, 2154–2169. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, K.; Murao, K. Load Position Estimation Method for Wearable Devices Based on Difference in Pulse Wave Arrival Time. Sensors 2022, 22, 1090. [Google Scholar] [CrossRef] [PubMed]
- Geddes, L.; Voelz, M.; Combs, C.; Reiner, D.; Babbs, C.F. Characterization of the oscillometric method for measuring indirect blood pressure. Ann. Biomed. Eng. 1982, 10, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Geddes, L.; Moore, A.G. The efficient detection of Korotkoff sounds. Med. Biol. Eng. 1968, 6, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Geddes, L.; Spencer, W.; Hoff, H. Graphic recording of the korotkoff sounds. Am. Heart J. 1959, 57, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Akimoto, Y.; Murao, K. Design and Implementation of an Input Interface for Wearable Devices Using Pulse Wave Control by Compressing the Upper Arm. In Proceedings of the Augmented Humans International Conference 2021, New York, NY, USA, 22–24 February 2021; pp. 280–282. [Google Scholar] [CrossRef]
- Murphy, J.; Gitman, Y. Works with Everything. 2018. Available online: https://pulsesensor.com/ (accessed on 6 December 2023).
- Gitman, Y.; Murphy, J.; Murphy, J.; Yury, G. PulseSensor_Amped_Arduino. 2018. Available online: https://github.com/WorldFamousElectronics/ (accessed on 6 December 2023).
- Metrodyne Microsystem Corp. MIS-2500 Series Pressure Sensor. 2011. Available online: https://www.metrodynemems.com/product-MIS-2500-Series-Pressure-Sensor-MIS-2500.html (accessed on 6 December 2023).
- Cosland. Tact Switches DTS Series. 2003. Available online: https://www.cosland.com/pro_detail.php?classmaster=26&productsid=375 (accessed on 6 December 2023).
- Fitbit Inc. Fitbit Versa 2. 2019. Available online: https://www.fitbit.com/global/us/products/smartwatches/versa (accessed on 6 December 2023).
- Apple Inc. Apple Watch Series 6. 2020. Available online: https://support.apple.com/kb/SP826?viewlocale=en_US&locale=ja_JP (accessed on 6 December 2023).
- Polar Electro Ignite. Polar Ignite. 2020. Available online: https://www.polar.com/en/ignite/ (accessed on 6 December 2023).
- Garmin Ltd. Garmin Swim 2. 2020. Available online: https://www.garmin.com/en-US/p/665374 (accessed on 6 December 2023).
- Virtanen, P.; Gommers, R.; Oliphant, T.E.; Haberland, M.; Reddy, T.; Cournapeau, D.; Burovski, E.; Peterson, P.; Weckesser, W.; Bright, J.; et al. SciPy 1.0: Fundamental Algorithms for Scientific Computing in Python. Nat. Methods 2020, 17, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Machado, F.A.; Denadai, B.S. Validity of maximum heart rate prediction equations for children and adolescents. Arq. Bras. Cardiol. 2011, 97, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Ostchega, Y. Resting Pulse Rate Reference Data for Children, Adolescents, and Adults: United States, 1999–2008; Number 41; US Department of Health and Human Services, Centers for Disease Control and Prevention: Atlanta, GA, USA, 2012. [Google Scholar]
- Fuller, D.; Colwell, E.; Low, J.; Orychock, K.; Tobin, M.A.; Simango, B.; Buote, R.; Van Heerden, D.; Luan, H.; Cullen, K.; et al. Reliability and Validity of Commercially Available Wearable Devices for Measuring Steps, Energy Expenditure, and Heart Rate: Systematic Review. JMIR Mhealth Uhealth 2020, 8, e18694. [Google Scholar] [CrossRef] [PubMed]
- Tochikubo, O.; Miyazaki, N.; Kaneko, Y. Relationship between 24-hour Arterial Pressure and Heart Rate Variation in Normotensives, Hypertensives and Patients with Shy-Drager Syndrome. Jpn. Circ. J. 1987, 51, 485–494. [Google Scholar] [CrossRef] [PubMed]


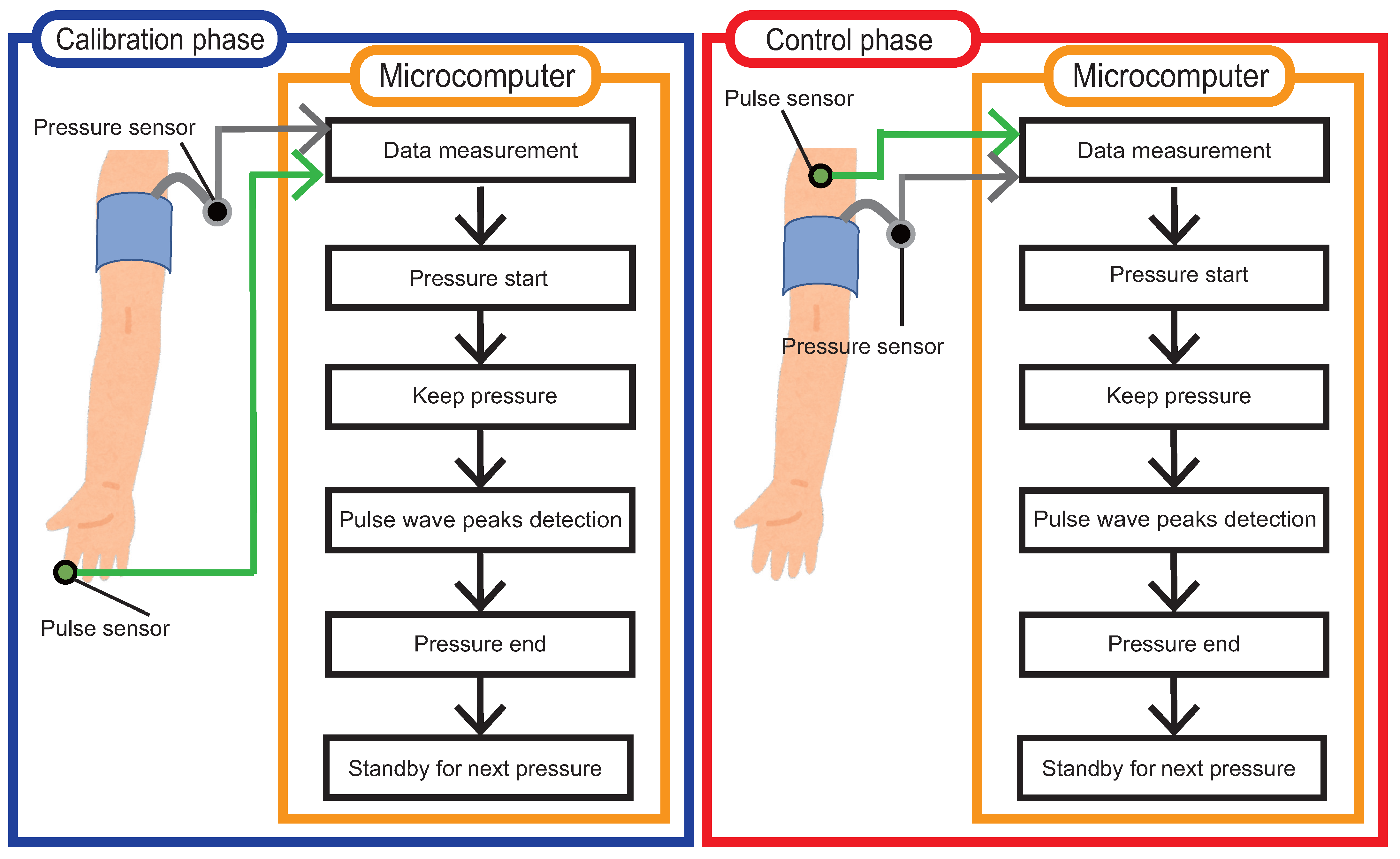





| Order | Name of the Procedure | Description |
|---|---|---|
| 1 | Data measurement |
|
| 2 | Pressure start |
|
| 3 | Keep pressure |
|
| 4 | Pulse wave peaks detection |
|
| 5 | Pressure end |
|
| 6 | Standby for next pressure |
|
| Order | Name of the Procedure | Description |
|---|---|---|
| 1 | Data measurement |
|
| 2 | Pressure start |
|
| 3 | Pressure keeping |
|
| 4 | Pulse wave peaks detection |
|
| 5 | Pressure end |
|
| 6 | Standby for next pressure |
|
| Smartwatch | Maximum | Minimum | ||
|---|---|---|---|---|
| Input | Output | Input | Output | |
| Fitbit | 210 | 201 | 55 | 54 |
| Apple | 220 | 210 | 45 | 44 |
| Polar | Nan | Nan | Nan | Nan |
| Garmin | 240 | 189 | 30 | 45 |
| Paenoon | 190 | 180 | 48 | 48 |
| Pattern | Subject | Session | Smartwatch | ||||
|---|---|---|---|---|---|---|---|
| Fitbit | Apple | Paenoon | Polar | Garmin | |||
| A | A | 1st | ↘ | ↗ | ↘ | ↘ | |
| 2nd | ↘ | ↗ | ↘ | ↘ | |||
| B | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↗ | ↘ | ↘ | ||||
| C | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↗ | ↘ | ↘ | ||||
| D | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↗ | ↘ | ↘ | ||||
| E | 1st | ↘ | ↗ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| F | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↗ | ↘ | ↘ | ||||
| G | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↗ | ↘ | ↘ | ||||
| B | A | 1st | ↘ | ↘ | ↘ | ↘ | |
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| B | 1st | ↘ | ↘ | ↘ | |||
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| C | 1st | ↘ | ↘ | ↘ | |||
| 2nd | ↘ | ↘ | ↘ | ||||
| D | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↗ | ↘ | ↘ | |||
| E | 1st | ↘ | ↘ | ||||
| 2nd | ↘ | ||||||
| F | 1st | ↘ | ↗ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ||||
| G | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↘ | ↘ | ↘ | ||||
| C | A | 1st | ↘ | ↗ | ↘ | ↘ | |
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| B | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| C | 1st | ↘ | ↘ | ↘ | |||
| 2nd | ↘ | ↗ | ↘ | ||||
| D | 1st | ↗ | ↘ | ||||
| 2nd | ↗ | ↘ | ↘ | ||||
| E | 1st | ↘ | ↘ | ||||
| 2nd | ↘ | ↘ | |||||
| F | 1st | ↗ | |||||
| 2nd | ↗ | ||||||
| G | 1st | ↘ | ↘ | ||||
| 2nd | ↗ | ↘ | ↘ | ||||
| Pattern | Subject | Session | Smartwatch | ||||
|---|---|---|---|---|---|---|---|
| Fitbit | Apple | Paenoon | Polar | Garmin | |||
| A | A | 1st | ↘ | ↘ | ↘ | ↘ | ↘ |
| 2nd | ↘ | ↘ | ↘ | ↘ | ↘ | ||
| B | 1st | ↘ | ↘ | ↘ | ↘ | ↘ | |
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| C | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| D | 1st | ↗ | ↘ | ↘ | ↘ | ↘ | |
| 2nd | ↗ | ↘ | ↘ | ↘ | ↘ | ||
| E | 1st | ↘ | ↘ | ↘ | ↘ | ↘ | |
| 2nd | ↘ | ↘ | ↘ | ↘ | ↘ | ||
| B | A | 1st | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ↘ | |||
| B | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ||||
| C | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↘ | ↘ | ||||
| D | 1st | ↘ | ↘ | ↘ | |||
| 2nd | ↘ | ↘ | ↘ | ||||
| E | 1st | ↘ | ↘ | ↘ | |||
| 2nd | ↘ | ↘ | ↘ | ||||
| C | A | 1st | ↘ | ↘ | ↘ | ↘ | ↘ |
| 2nd | ↘ | ↘ | ↘ | ↘ | ↘ | ||
| B | 1st | ↘ | ↘ | ↘ | |||
| 2nd | ↘ | ↘ | ↘ | ||||
| C | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↘ | ↗ | ↘ | ↘ | |||
| D | 1st | ↗ | ↘ | ↘ | |||
| 2nd | ↗ | ↗ | ↘ | ||||
| E | 1st | ↘ | ↘ | ↘ | ↘ | ||
| 2nd | ↗ | ↘ | ↘ | ↘ | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoshida, K.; Sawano, R.; Okamoto, M.; Murao, K.; Tsuchida, S.; Terada, T. Physical Noninvasive Attacks on Photoplethysmogram by Computer Controlled Blood Pressure Cuff. Sensors 2023, 23, 9764. https://doi.org/10.3390/s23249764
Yoshida K, Sawano R, Okamoto M, Murao K, Tsuchida S, Terada T. Physical Noninvasive Attacks on Photoplethysmogram by Computer Controlled Blood Pressure Cuff. Sensors. 2023; 23(24):9764. https://doi.org/10.3390/s23249764
Chicago/Turabian StyleYoshida, Kazuki, Ryota Sawano, Masahiro Okamoto, Kazuya Murao, Shuhei Tsuchida, and Tsutomu Terada. 2023. "Physical Noninvasive Attacks on Photoplethysmogram by Computer Controlled Blood Pressure Cuff" Sensors 23, no. 24: 9764. https://doi.org/10.3390/s23249764
APA StyleYoshida, K., Sawano, R., Okamoto, M., Murao, K., Tsuchida, S., & Terada, T. (2023). Physical Noninvasive Attacks on Photoplethysmogram by Computer Controlled Blood Pressure Cuff. Sensors, 23(24), 9764. https://doi.org/10.3390/s23249764








