User Perspectives of Geriatric German Patients on Smart Sensor Technology in Healthcare
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Ethics
2.2. Interviews
3. Results
3.1. Participants
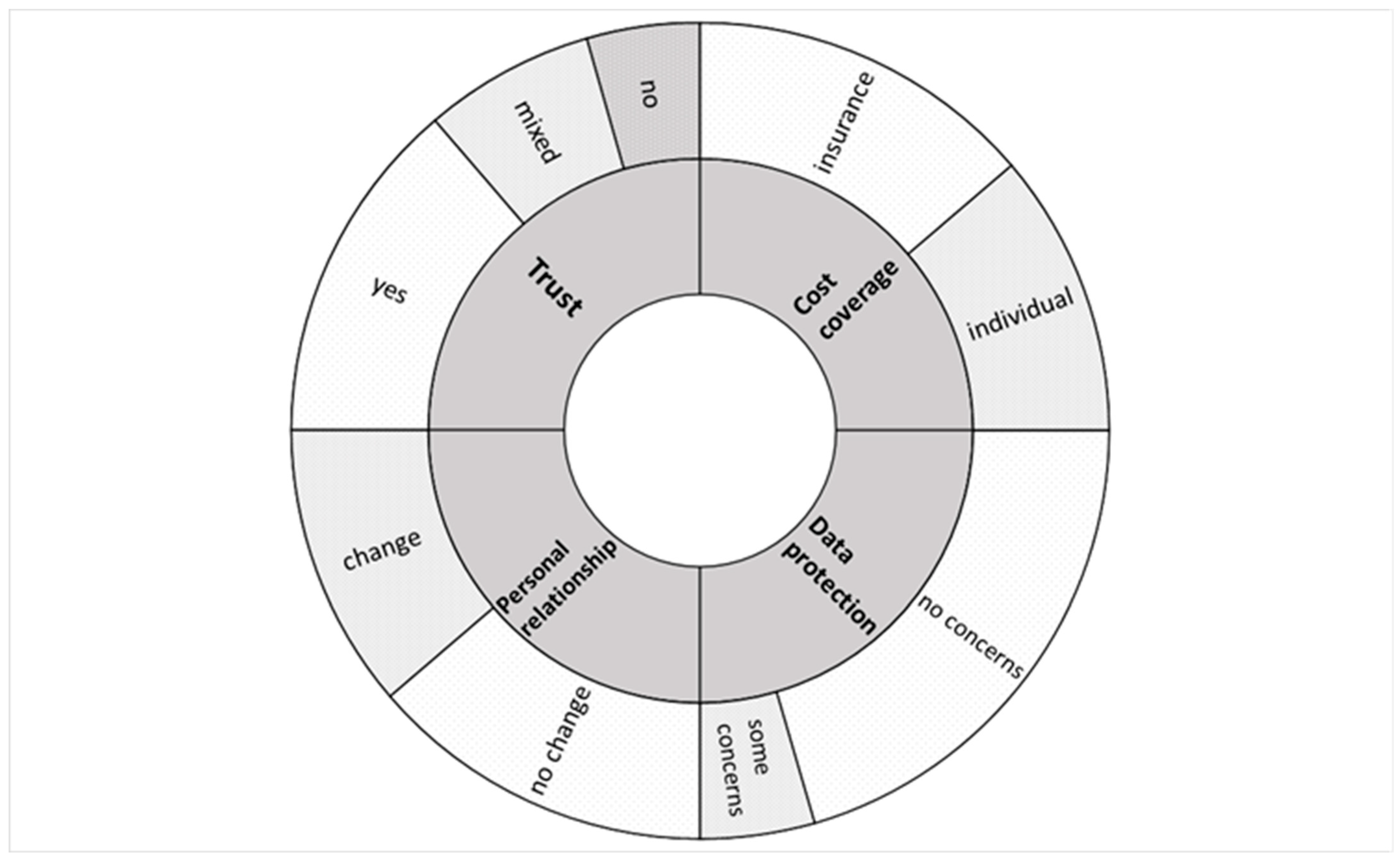
3.2. Topics
3.2.1. Trust toward Smart Sensors Technology
“Oh well, I assume that they [devices] can measure more meticulously”(iv 3)
“As a rule, people [do] always what suits them at the time. And that’s why I prefer the machine.”(iv 7)
“The treatment team needs a foundation on which to build [the recommendation]. And that is, let’s call it, objective. And the moment it’s [done] with the person [involved], it’s never objective, it’s always subjective. And that’s just the reason why I trust the machine more as an assistance.”(iv 6)
“Well, basically, the machine measurements are more objective, but I’m currently considering whether a mixture could possibly be an option. That means that machine measurements are always carried out and, in case of doubt, in certain areas they are perhaps substantiated again by people or (…) questioned.”(iv 2)
“The machine detection of movements can be very precise. The individual process (…) by the examiner can also be justified. The sensors are there and [they are] recording and, yes, I can’t influence the interpretation, but I assume that it won’t be done lightly.”(iv 5)
“[Because of] human connection.”(iv 8)
“Well, because she [healthcare professional] notices the mistakes while she is working and can correct them.”(iv 1)
3.2.2. Relationship with the Attending Healthcare Professionals
“[If] I don’t know whether I should move, how much I [should] move, what kind of movements [should] I make (…), I think, it would be good [that the sensor would] give [me] advice on (…) movements.”(iv 10)
“If questions arise here or if difficulties arise here, well, basically I would trust the smart controls (…). If problems or if different views or opinions arise, the question (…) is whether one is trying to achieve a unified opinion by simply discussing the points. So, if the person being examined has different opinions about the smart results, then maybe you should talk to [healthcare professional] who knows the system better.”(iv 2)
“Because the doctor then only has to look at this printed data and no longer has to speak to me. And then there is the danger that one [healthcare professional] generally trusts an algorithm more than perhaps a conversation with the patient. And the algorithm doesn’t always have to be right.”(iv 3)
“The personal contact [between the patient and the attending team] will simply be missing. (…) Or it will be reduced.”(iv 8)
3.2.3. Data and Privacy Protection
“In principle no. I can’t imagine anyone having any special interest in it.”(iv 5)
“You don’t even know my private sphere. And we’re only together for a few minutes, when so many people [patients] are here, you have less contact [with individual one], right?”(iv 7)
“(…) I assume that they [insurance companies] are interested in this data.”(iv 3)
“The cost coverage by the health insurance companies means that the health insurance companies also have the right to access this data.”(iv 5)
3.2.4. Cost Coverage of the Use of Smart Sensors
“[Sensor-based activity tracking is] for health insurance and in retirement, you’re not exactly wealthy and we used to say, every penny, now every cent, is important to me. And everything that goes off the pension money is draining my wallet.”(iv 6)
“The problem is that I can’t cover the high costs. Well, I’d be willing to pay a small fee, but I can’t afford to pay a lot.”(iv 11)
“(…) it may not even be in my interest. Maybe it does not lie in my interest and still I have to use it.”(iv 3)
“Yes, if I have something out of it, I would also bear the costs.”(iv 1)
“If the matter is important to me, for my personal situation, I would participate [in the costs] because it is in my own interest.”(iv 2)
“I would participate [in the costs] if it would be beneficial to my health, so to speak, or to monitoring my health (…).”(iv 8)
“A small contribution [to the costs], I could imagine. Because I also have an advantage from it and also get information. And I also have an advantage when my doctor has information, because it can flow into the therapy or the physiotherapy. Because I’m the beneficiary.”(iv 10)
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization: Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 24 July 2023).
- The United States Census Bureau: U.S. Older Population Grew From 2010 to 2020 at Fastest Rate Since 1880 to 1890. Available online: https://www.census.gov/library/stories/2023/05/2020-census-united-states-older-population-grew.html (accessed on 22 July 2023).
- The World Bank: Population Ages 65 and above. Available online: https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS?most_recent_value_desc=true (accessed on 22 July 2023).
- Tang, B.; Li, Z.; Hu, S.; Xiong, J. Economic Implications of Health Care Burden for Elderly Population. Inquiry 2022, 59. [Google Scholar] [CrossRef]
- Macinko, J.; Andrade, F.C.D.; Bof de Andrade, F.; Lima-Costa, M.F. Universal health coverage: Are older adults being left behind? Evidence from aging cohorts in twenty-three countries. Health Aff. 2020, 39, 1951–1960. [Google Scholar] [CrossRef]
- Van der Schaar, M.; Alaa, A.M.; Floto, A.; Gimson, A.; Scholtes, S.; Wood, A.; McKinney, E.; Jarett, D.; Lio, P.; Ercole, A. How artificial intelligence and machine learning can help healthcare systems respond to COVID-19. Mach. Learn. 2021, 110, 1–14. [Google Scholar] [CrossRef]
- Rajpurkar, P.; Chen, E.; Banerjee, O.; Topol, E.J. AI in health and medicine. Nat. Med. 2022, 28, 31–38. [Google Scholar] [CrossRef]
- Chan, M.; Estève, D.; Fourniols, J.-Y.; Escriba, C.; Campo, E. Smart wearable systems: Current status and future challenges. Artif. Intell. Med. 2012, 56, 137–156. [Google Scholar] [CrossRef]
- Mendes, J.J.A., Jr.; Vieira, M.E.M.; Pires, M.B.; Stevan, S.L., Jr. Sensor Fusion and Smart Sensor in Sports and Biomedical Applications. Sensors 2016, 16, 1569. [Google Scholar] [CrossRef] [PubMed]
- Maric, B.; Kaan, A.; Ignaszewski, A.; Lear, S.A. systematic review of telemonitoring technologies in heart failure. Eur. J. Heart Fail. 2009, 11, 506–507. [Google Scholar] [CrossRef] [PubMed]
- Batista, M.; Moncusi, A.M.; López-Aguilar, P.; Martínez-Ballesté, A.; Solanas, A. Sensors for Context-Aware Smart Healthcare: A Security Perspective. Sensors 2021, 21, 6886. [Google Scholar] [CrossRef]
- Penteridis, L.; D’Onofrio, G.; Sancarlo, D.; Giuliani, F.; Ricciardi, F.; Cavallo, F.; Greco, A.; Trochidis, I.; Gkiokas, A. Robotic and sensor technologies for mobility in older people. Rejuvenation Res. 2017, 20, 401–410. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Su, C.; He, C. Rehabilitation Exercise Recognition and Evaluation Based on Smart Sensors With Deep Learning Framework. IEEE Access 2020, 8, 77561–77571. [Google Scholar] [CrossRef]
- Klenk, J.; Wekenmann, S.; Schwickert, L.; Lindemann, U.; Becker, C.; Rapp, K. Change of objectively-measured physical activity during geriatric rehabilitation. Sensors 2019, 19, 5451. [Google Scholar] [CrossRef]
- Lukowicz, P.; Kirstein, T.; Tröster, G. Wearable systems for health care applications. Methods Inf. Med. 2004, 43, 232–238. [Google Scholar] [CrossRef]
- Belsi, A.; Papi, E.; McGregor, A.H. Impact of wearable technology on psychosocial factors of osteoarthritis management: A qualitative study. BMJ Open 2016, 6, e010064. [Google Scholar] [CrossRef][Green Version]
- Barlow, J.; Wright, C.; Sheasby, J.; Turner, A.; Hainsworth, J. Self-management approaches for people with chronic conditions: A review. Patient Educ. Couns. 2002, 48, 177–187. [Google Scholar] [CrossRef]
- Bonato, P. Wearable sensors and systems. From enabling technology to clinical applications. IEEE Eng. Med. Biol. Mag. 2010, 29, 25–36. [Google Scholar] [CrossRef] [PubMed]
- Timmermann, C.; Ursin, F.; Predel, C.; Steger, F. Aligning Patient’s Ideas of a Good Life with Medically Indicated Therapies in Geriatric Rehabilitation Using Smart Sensors. Sensors 2021, 21, 8479. [Google Scholar] [CrossRef]
- Predel, C.; Timmermann, C.; Ursin, F.; Orzechowski, M.; Ropinski, T.; Steger, F. Conflicting Aims and Values in the Application of Smart Sensors in Geriatric Rehabilitation: Ethical Analysis. JMIR Mhealth Uhealth 2022, 10, e32910. [Google Scholar] [CrossRef] [PubMed]
- Hopf, C. Qualitative Interviews. In Qualitative Forschung, 6th ed.; Flick, U., von Kardoff, E., Steinke, I., Eds.; Rohwolt: Reinbek bei Hamburg, Germany, 2008; pp. 349–360. [Google Scholar]
- Baumann, A.; Salloch, S.; Schildmann, J.; Vollmann, J. Empirische Methoden in der Medizinethik. In Empirische Medizinethik: Konzepte, Methoden, Ergebnisse; Vollmann, J., Schildmann, J., Eds.; LIT: Münster, Germany, 2011; pp. 25–44. [Google Scholar]
- Gläser, J.; Laudel, G. Experteninterviews und Qualitative Inhaltsanalyse; Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2009. [Google Scholar]
- Mayring, P. Einführung in die Qualitative Sozialforschung; Beltz: Basel, Switzerland, 2016. [Google Scholar]
- Ritchie, J.; Spencer, L.; O’Connor, W. Carrying out Qualitative Analysis. In Qualtitative Research Practice: A Guide for Social Science Students and Researchers; Ritchie, J., Lewis, J., Eds.; SAGE: London, UK, 2003; pp. 219–262. [Google Scholar]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Ghorayeb, A.; Comber, R.; Gooberman-Hill, R. Older adults’ perspektives of smart home technology: Are we developing the technology that older people want? Int. J. Hum. Comput. 2021, 147, 102571. [Google Scholar] [CrossRef]
- Pol, M.; van Nes, F.; van Hartingsveldt, M.; Buurman, B.; de Rooij, S.; Kröse, B. Older People’s Perspectives Regarding the Use of Sensor Monitoring in Their Home. Gerontologist 2016, 56, 485–493. [Google Scholar] [CrossRef] [PubMed]
- Demiris, G.; Hensel, B.K.; Skubic, M.; Rantz, M. Senior residents’ perceived need of and preferences for „smart home“ sensor technologies. Int. J. Technol. Assess. Health Care 2008, 24, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Galambos, C.; Rantz, M.; Craver, A.; Bongiorno, M.; Pelts, M.; Holik, A.J.; Jun, J.S. Living with Intelligent Sensors. Older Adult and Family Member Perceptions. Comput. Inform. Nurs. 2019, 37, 615–627. [Google Scholar] [CrossRef] [PubMed]
- Skuban-Eiseler, T.; Orzechowski, M.; Denkinger, M.; Derya Kocar, T.; Leinert, C.; Steger, F. Artificial Intelligence-based Clinical Decision Support Systems in Geriatrics: An Ethical Analysis. J. Am. Med. Dir. Assoc. 2023, 24, 1271–1276.e4. [Google Scholar] [CrossRef] [PubMed]
- Lagerin, A.; Törnkvist, L.; Fastbom, J.; Lundh, L. District nurses’ experiences of using a clinical decision support system and an assessment tool at elderly care units in primary health care: A qualitative study. Prim. Health Care Res. Dev. 2021, 22, e45. [Google Scholar] [CrossRef] [PubMed]
- Lukkien, D.R.M.; Nap, H.H.; Buimer, H.P.; Peine, A.; Boon, W.P.C.; Ket, J.C.F.; Minkman, M.M.N.; Moors, E.H.M. Toward Responsible Artificial Intelligence in Long-Term Care: A Scoping Review on Practical Approaches. Gerontologist 2023, 63, 155–168. [Google Scholar] [CrossRef]
- Heponiemi, T.; Kaihlanen, A.M.; Kouvonen, A.; Leemann, L.; Taipale, S.; Gluschkoff, K. The role of age and digital competence on the use of online health and social care services: A cross-sectional population-based survey. Digit. Health 2022, 8, 20552076221074485. [Google Scholar] [CrossRef]
- Molnar, C.; Casalicchio, G.; Bischl, B. Interpretable machine learning—A brief history, state-of-the-art and challenges. In ECML PKDD 2020 Workshops, Workshops of the European Conference on Machine Learning and Knowledge Discovery in Databases (ECML PKDD 2020): SoGood 2020, PDFL 2020, MLCS 2020, NFMCP 2020, DINA 2020, EDML 2020, XKDD 2020 and INRA 2020, Ghent, Belgium, 14–18 September 2020; Communications in Computer and Information Science; Springer: Cham, Switzerland, 2020; p. 1323. [Google Scholar]
- Alrassi, J.; Katsufrakis, P.J.; Chandran, L. Technology Can Augment, but Not Replace, Critical Human Skills Needed for Patient Care. Acad. Med. 2021, 96, 37–43. [Google Scholar] [CrossRef]
- Williams, S.L.; Haskard, K.B.; DiMatteo, M.R. The therapeutic effects of the physician-older patient relationship: Effective communication with vulnerable older patients. Clin. Interv. Aging 2007, 2, 453–467. [Google Scholar]
- Robeyns, I.; Byskov, M.F. The capability approach. In The Stanford Encyclopedia of Philosophy; Zalta, E.N., Ed.; The Metaphysics Research Lab - Stanford University: Stanford, CA, USA, 2021; Available online: https://plato.stanford.edu/entries/capability-approach/ (accessed on 27 July 2023).
- Melander, C.; Sävenstedt, S.; Wälivaara, B.M.; Olsson, M. Human capabilities in advanced dementia: Nussbaum’s approach. Int. J. Older People Nurs. 2018, 13, e12178. [Google Scholar] [CrossRef]
- Soofi, H. What moral work can Nussbaum’s account of human dignity do in the context of dementia care? J. Med. Ethics 2022, 48, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Sen, A. Equality of What? In Tanner Lectures on Human Values; McMurrin, S.M., Ed.; Cambridge University Press: Cambridge, UK, 1979; pp. 197–220. [Google Scholar]
- Dzeng, E. Habermasian communication pathologies in do-not-resuscitate discussions at the end of life: Manipulation as an unintended consequence of an ideology of patient autonomy. Sociol. Health Illn. 2019, 41, 325–342. [Google Scholar] [CrossRef]
- Mendelson, D.; Rees, A.; Wolf, G. Medical Confidentiality and Patient Privacy. In Health Law in Australia, 3rd ed.; White, B., McDonald, F., Willmott, L., Eds.; Thomson Reuters: Sydney, Australia, 2018; pp. 396–433. [Google Scholar]
- Cartwright, A.J. The elephant in the room: Cybersecurity in healthcare. J. Clin. Monit. Comput. 2023, 37, 1123–1132. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, T.; Childress, J. Principles of Biomedical Ethics, 8th ed.; Oxford University Press: Oxford, UK, 2019. [Google Scholar]
- Tabassum, A.; Jabir, A. Factors affecting the consumers’ willingness to pay for health and wellness food products. J. Agric. Food Res. 2020, 2, 100076. [Google Scholar] [CrossRef]
- Petrovsky, D.V.; Ðoàn, L.N.; Loizos, M.; O’Conor, R.; Prochaska, M.; Tsang, M.; Hopman-Droste, R.; Klinedinst, T.C.; Mathur, A.; Mandeen-Roche, K.; et al. Key recommendations from the 2021 “inclusion of older adults in clinical research” workshop. J. Clin. Transl. Sci. 2022, 5, e55. [Google Scholar] [CrossRef] [PubMed]
- Bird, M.; Ouellette, C.; Whitmore, C.; Li, L.; Nair, K.; McGillion, M.H.; Yost, J.; Banfield, L.; Campbell, E.; Carroll, S.L. Preparing for patient partnership: A scoping review of patient partner engagement and evaluation in research. Health Expect. 2020, 23, 523–539. [Google Scholar] [CrossRef]
- Guest, G.; Bunce, A.; Johnson, L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Guest, G.; Namey, E.; McKenna, K. How many focus groups are enough? Building an evidence base for nonprobability sample sizes. Field Methods 2017, 29, 3–22. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orzechowski, M.; Skuban-Eiseler, T.; Ajlani, A.; Lindemann, U.; Klenk, J.; Steger, F. User Perspectives of Geriatric German Patients on Smart Sensor Technology in Healthcare. Sensors 2023, 23, 9124. https://doi.org/10.3390/s23229124
Orzechowski M, Skuban-Eiseler T, Ajlani A, Lindemann U, Klenk J, Steger F. User Perspectives of Geriatric German Patients on Smart Sensor Technology in Healthcare. Sensors. 2023; 23(22):9124. https://doi.org/10.3390/s23229124
Chicago/Turabian StyleOrzechowski, Marcin, Tobias Skuban-Eiseler, Anna Ajlani, Ulrich Lindemann, Jochen Klenk, and Florian Steger. 2023. "User Perspectives of Geriatric German Patients on Smart Sensor Technology in Healthcare" Sensors 23, no. 22: 9124. https://doi.org/10.3390/s23229124
APA StyleOrzechowski, M., Skuban-Eiseler, T., Ajlani, A., Lindemann, U., Klenk, J., & Steger, F. (2023). User Perspectives of Geriatric German Patients on Smart Sensor Technology in Healthcare. Sensors, 23(22), 9124. https://doi.org/10.3390/s23229124






