Adaptive Signal-to-Noise Ratio Indicator for Wearable Bioimpedance Monitoring
Abstract
:1. Introduction
- Present a custom wearable device for bioimpedance monitoring.
- Develop a SNR estimation method based on continuous wavelet transform (CWT) to identify wavelet ridges and measure their energy.
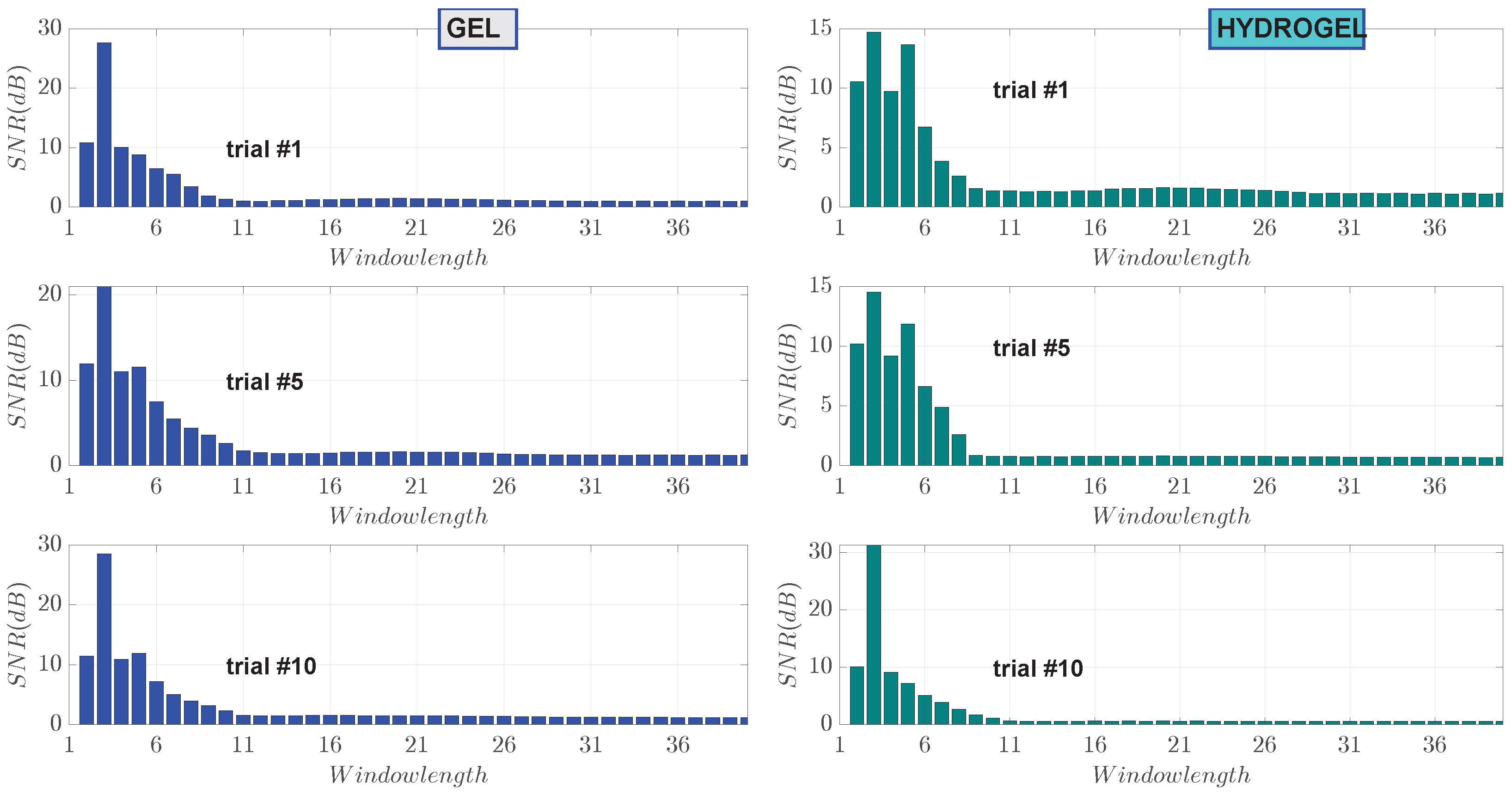
- Validate the proposed method using bioimpedance signals obtained in a small-scale experimental trial, with photoplethysmogram (PPG) signals as the reference.
- Compare the performance of the proposed adaptive method with a traditional wavelet-based signal denoising approach.
- Compare the SNR depending on different electrode-to-skin contact materials and other parameters.
2. Related Work
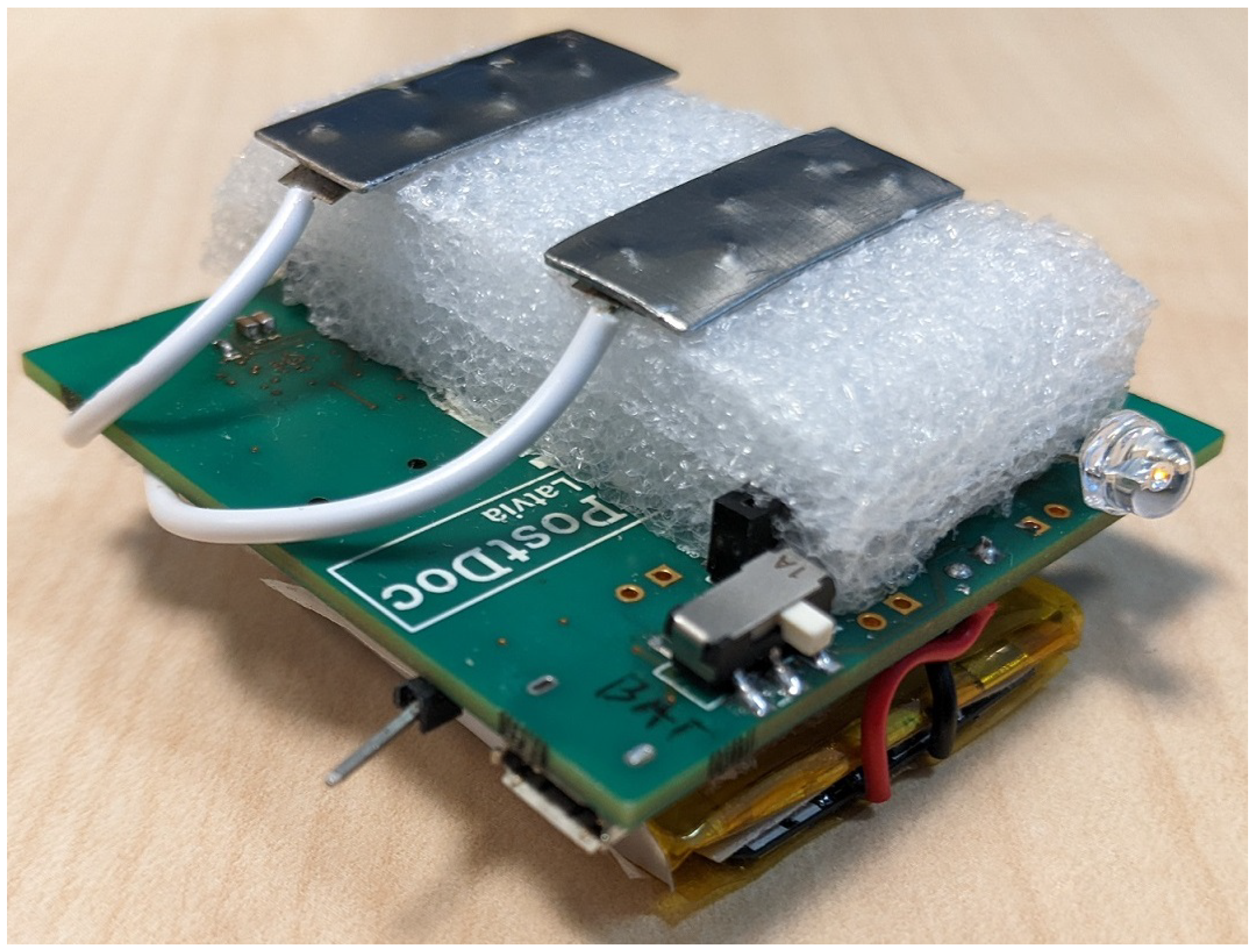
3. Experimental Platform
- nRF5340 System-on-Chip (SoC) with dual-core ARM Cortex-M33;
- MAX30001 bioimpedance chip;
- ICM-20994 nine-axial IMU chip, with accelerometer, gyroscope, and magnetometer sensors;
- Li-Ion battery;
- Power sourcing from the USB or from the battery;
- LEDs and a vibration motor for feedback to the user;
- External flash for additional on-board storage;
- User button.
3.1. Component Selection
3.1.1. Microcontroller and Radio
3.1.2. Bioimpedance Measurement Unit
3.2. Wearable Device Design
3.2.1. Design Overview
3.2.2. Energy Consumption
3.3. Software
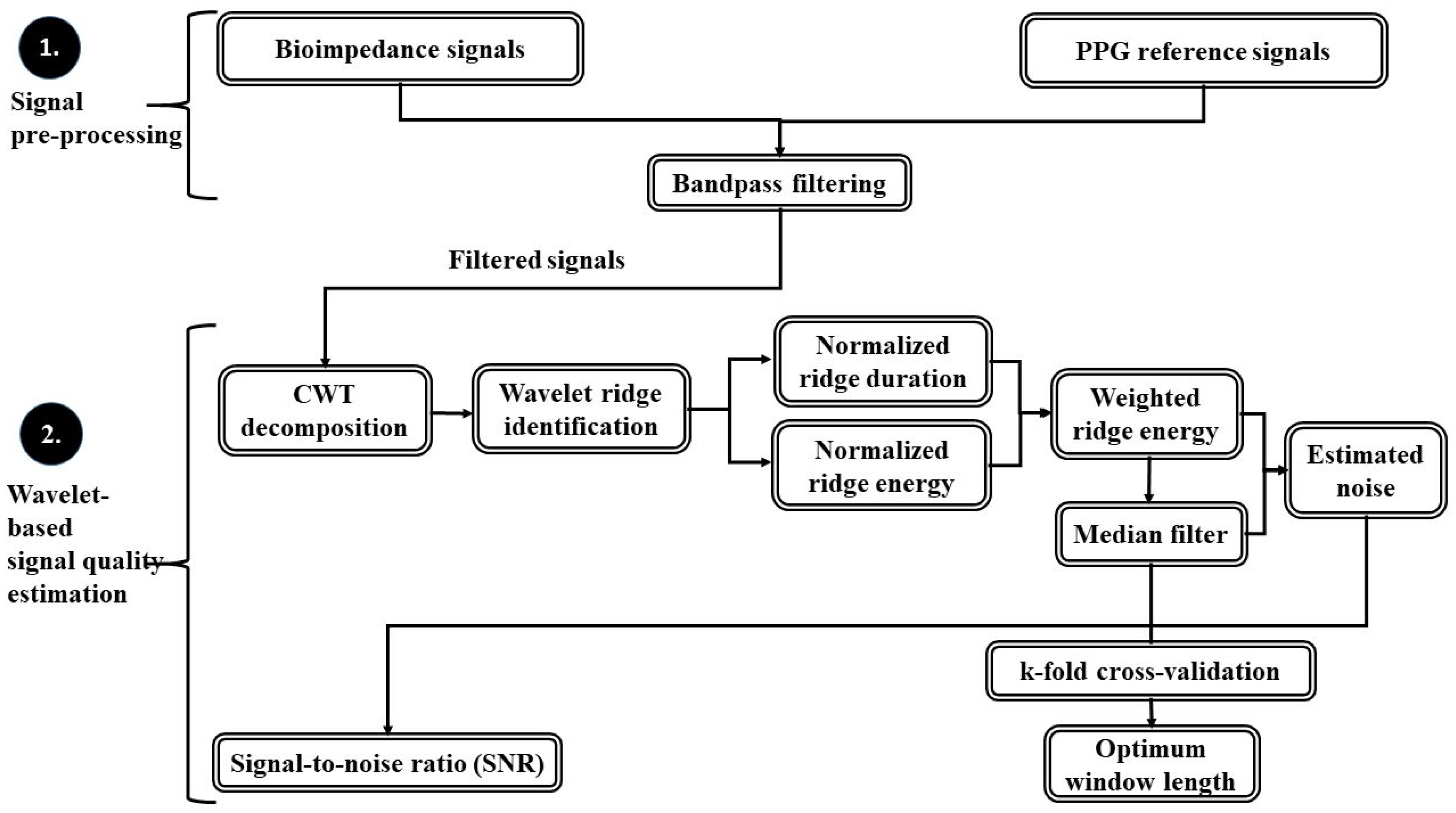
4. Methods
4.1. Band-Pass Filtering
4.2. Wavelet-Based Signal Quality Estimation
- 1.
- Derivative of absolute values of the wavelet coefficient with respect to the scale parameter s as calculated for all time instants b of the signal is zero
- 2.
- The second derivative of absolute values of the wavelet coefficient with respect to the scale parameter s as calculated for all time instants b of the signal is negative
4.3. Experimental Measurements
5. Results
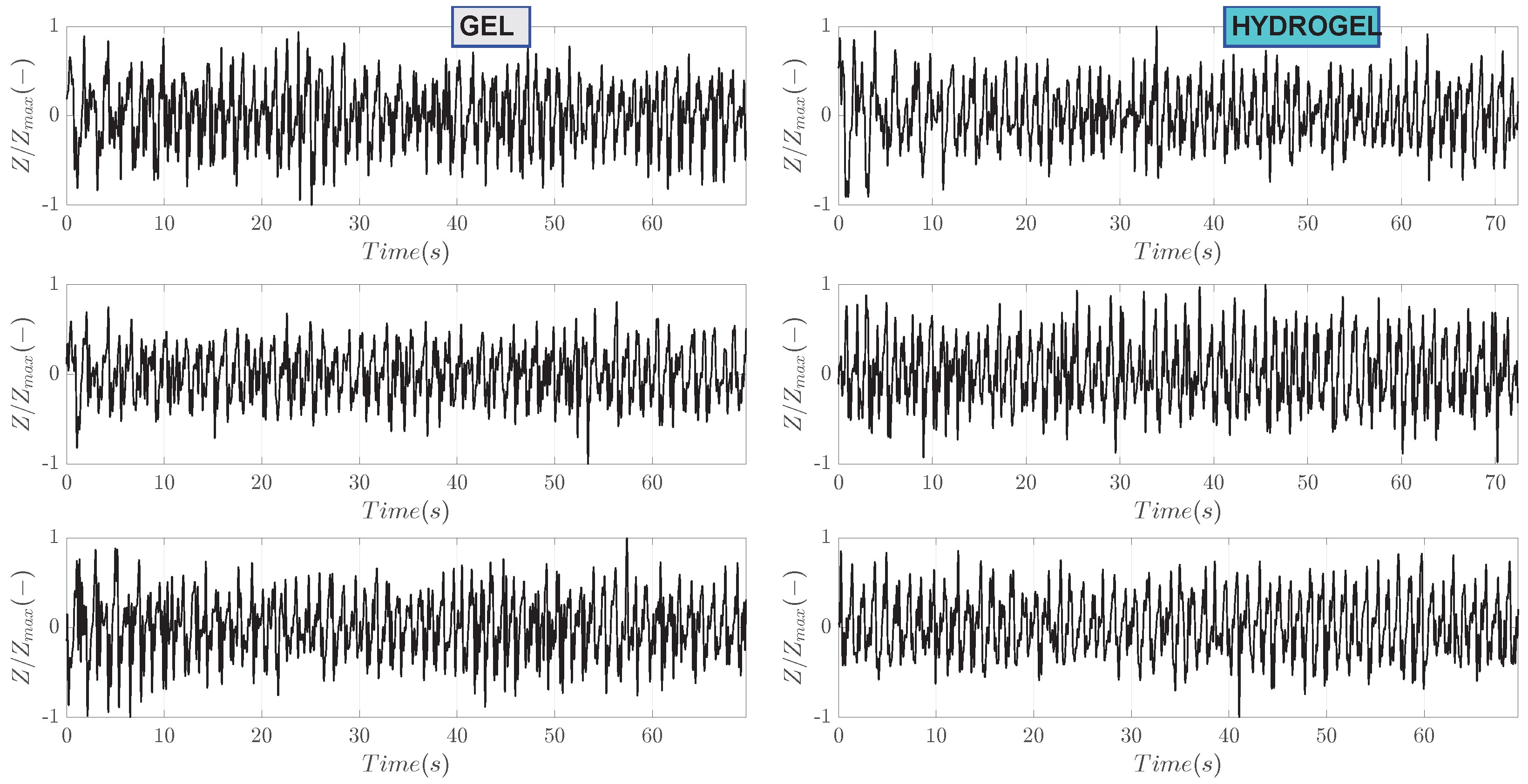
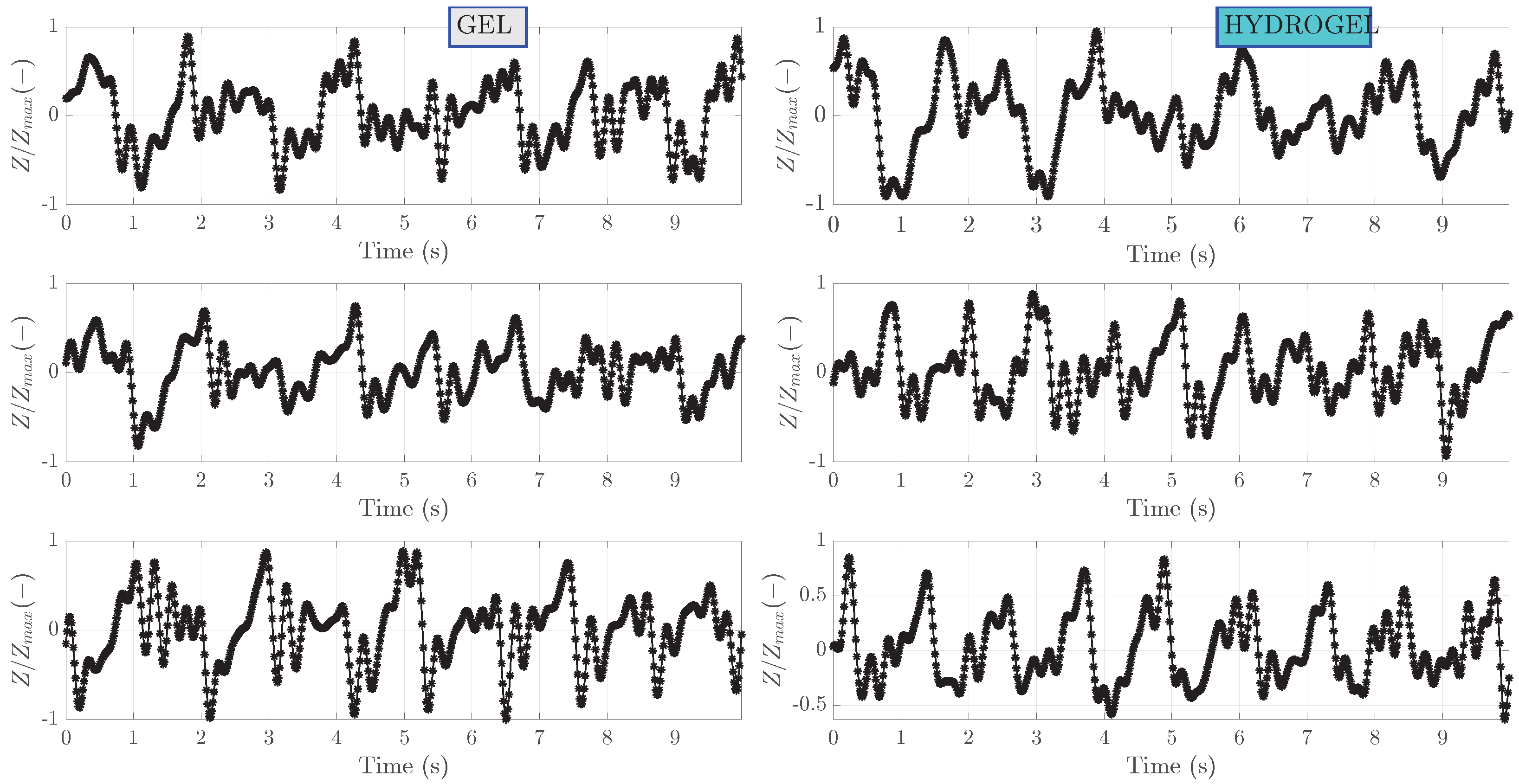
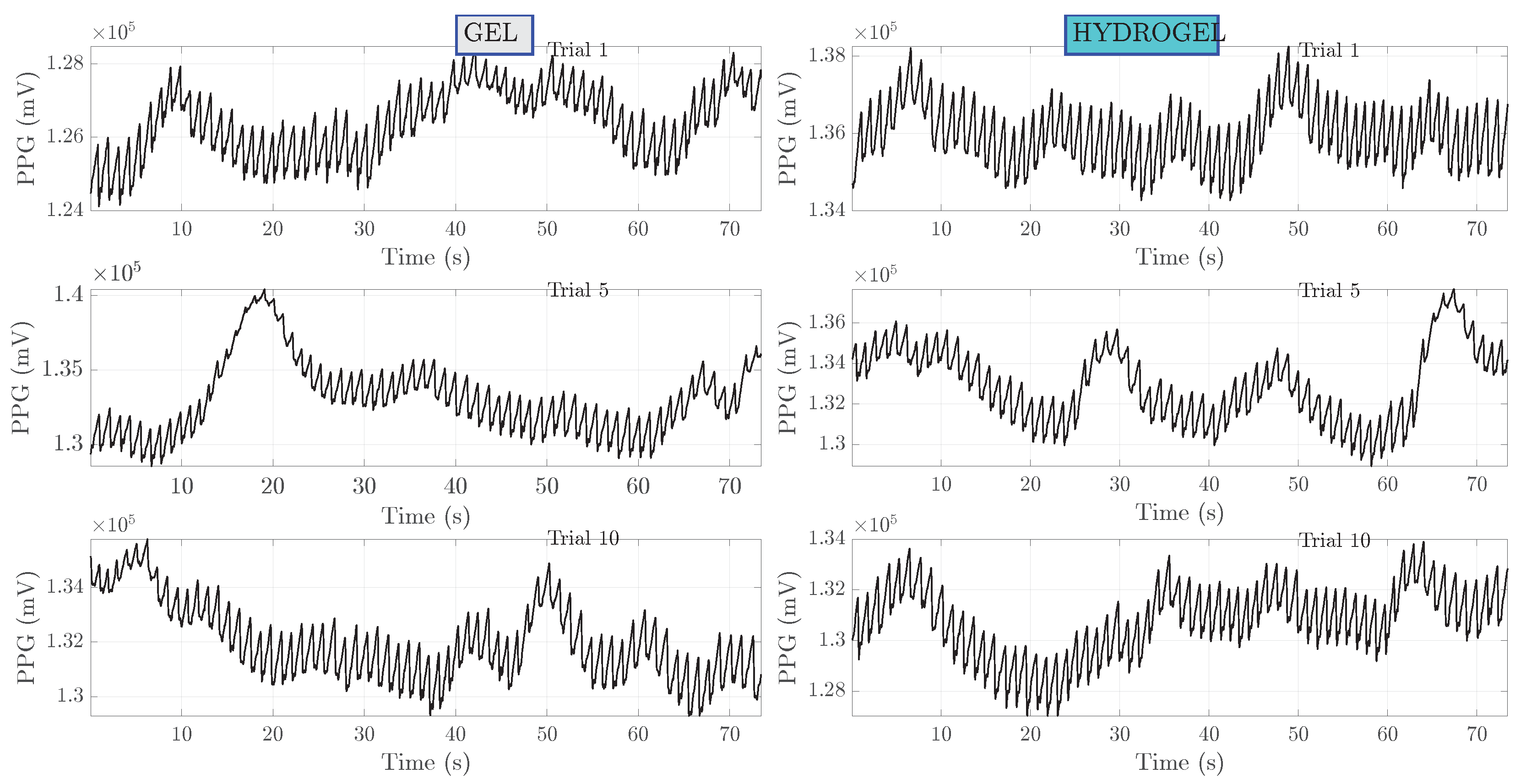
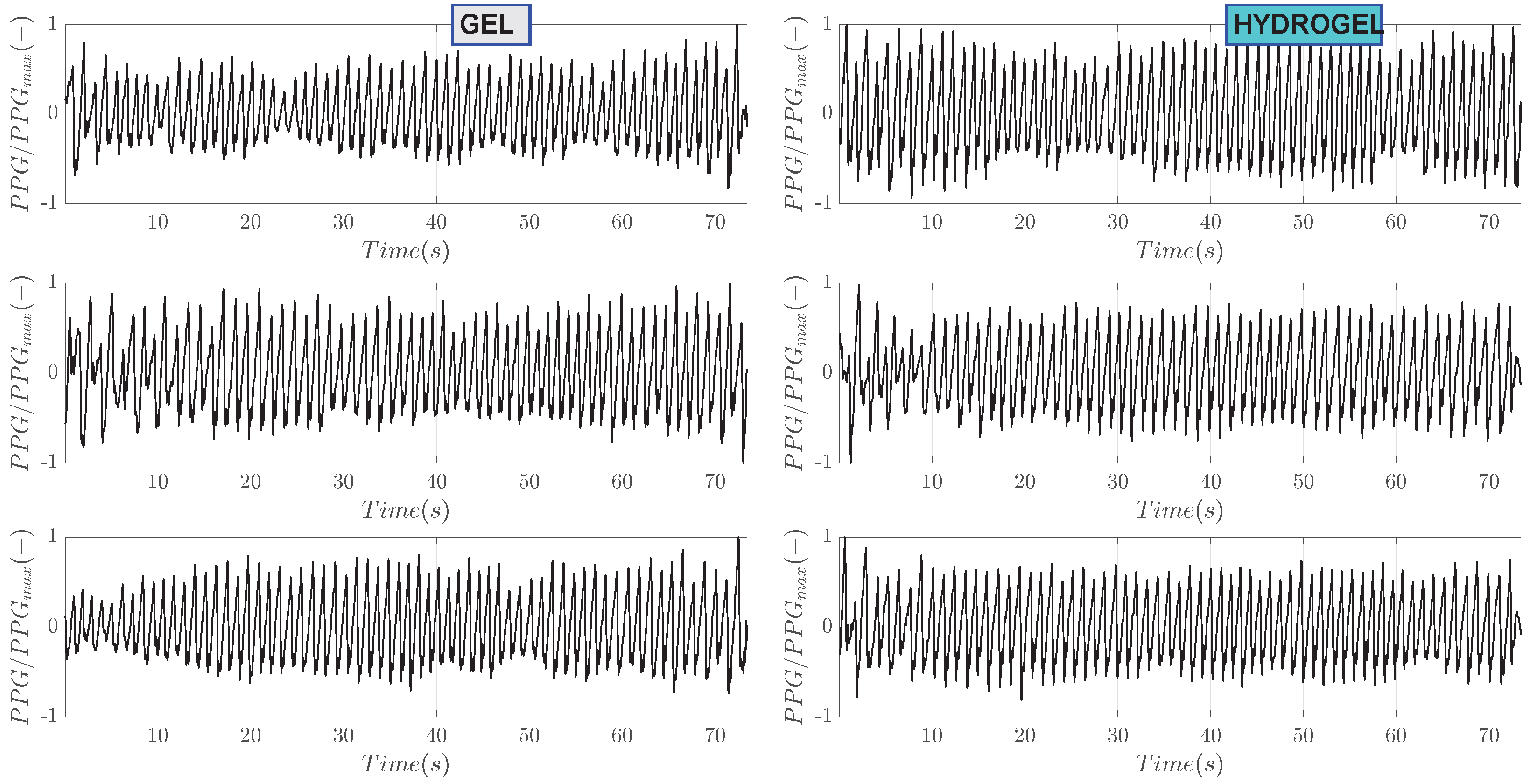
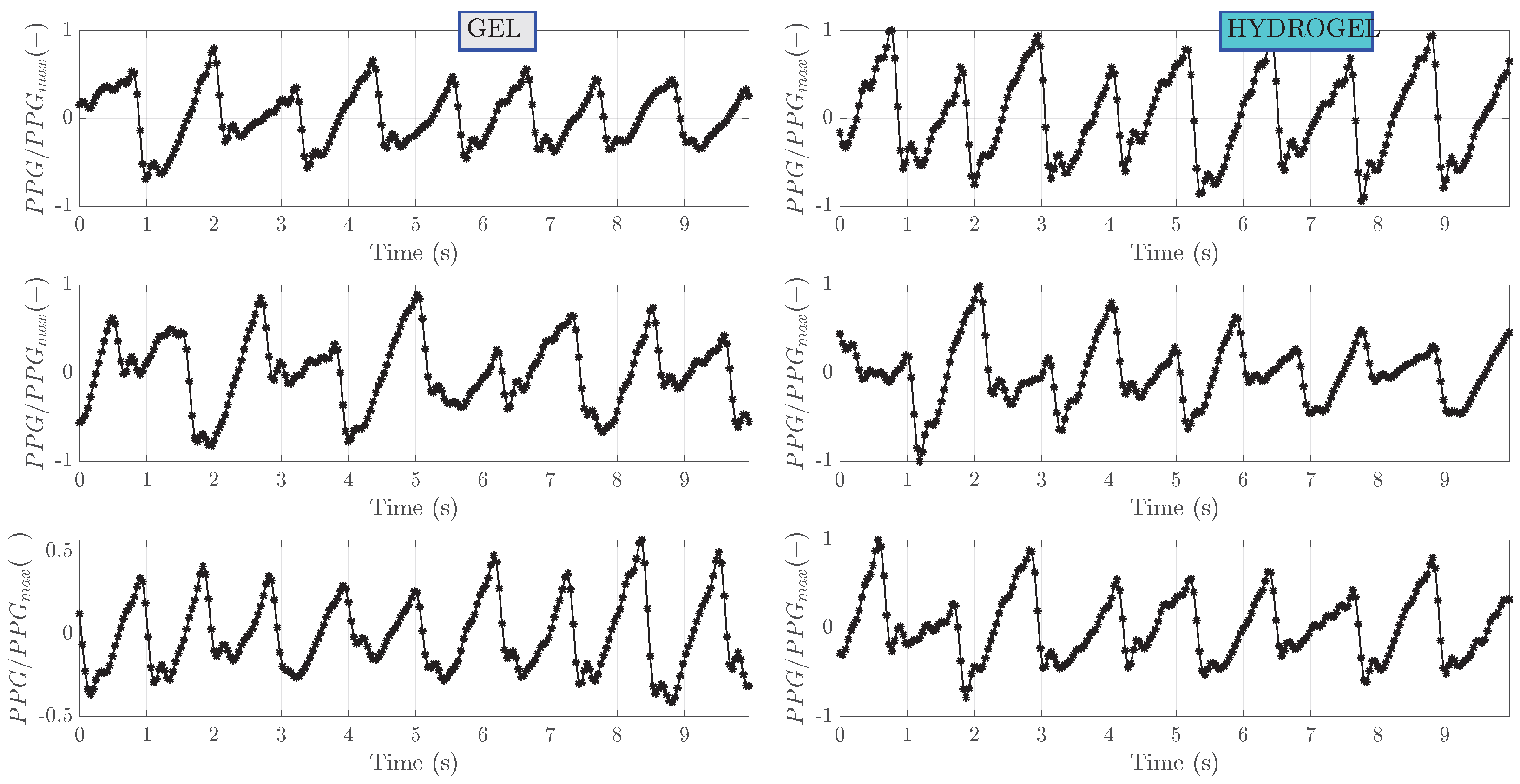
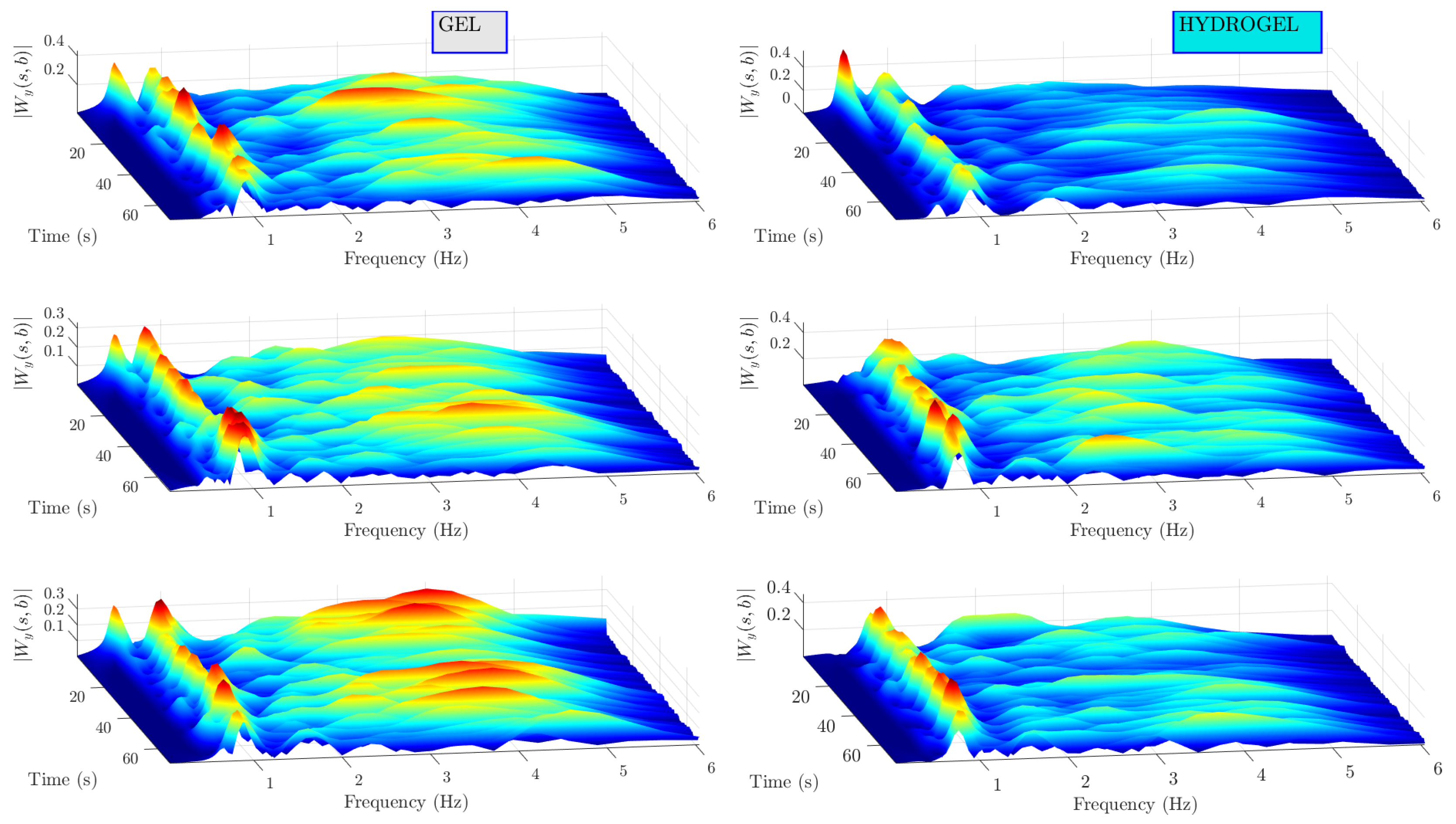
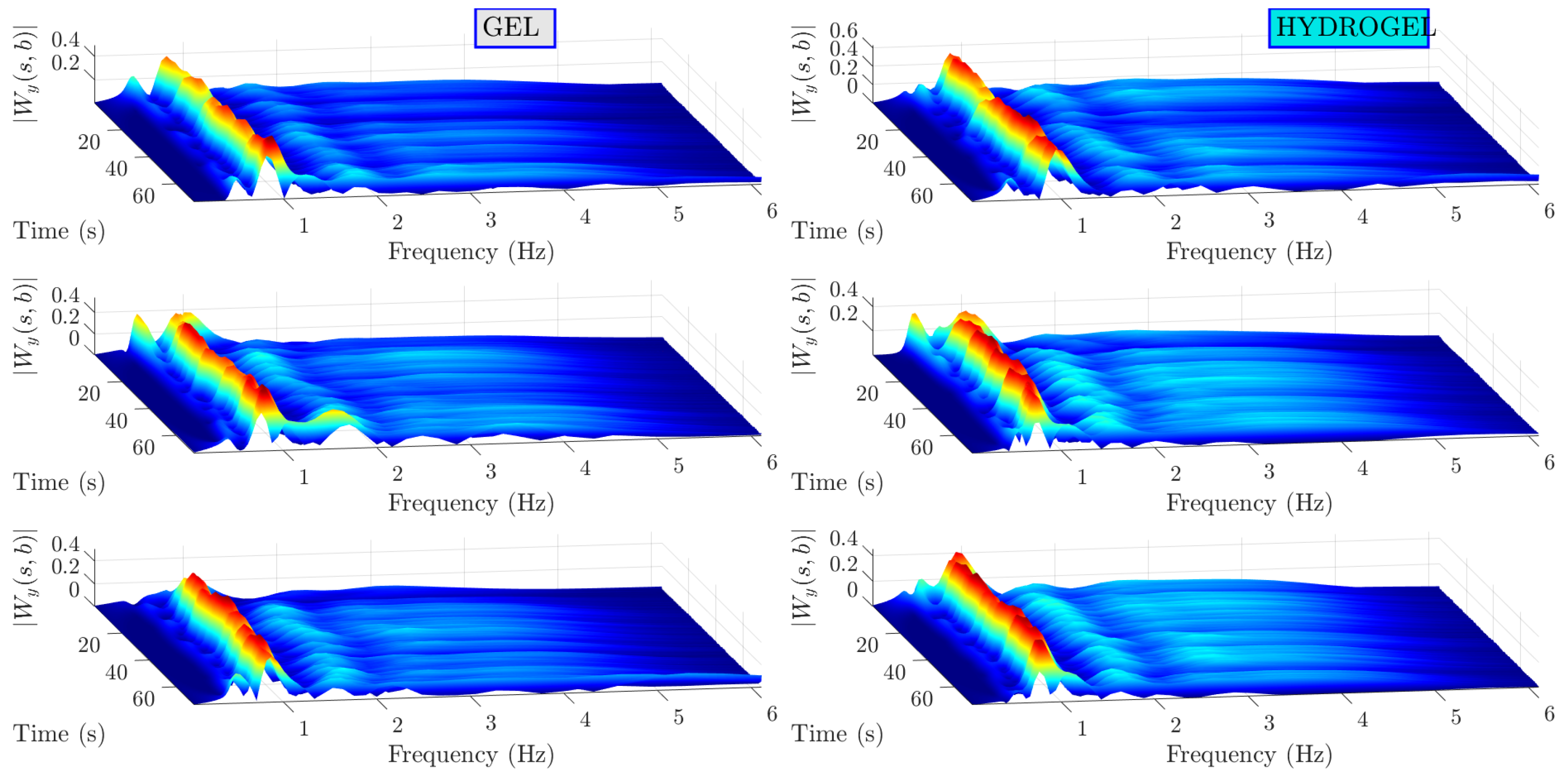
5.1. Measured Signals
5.2. Signal Stationarity and Normality
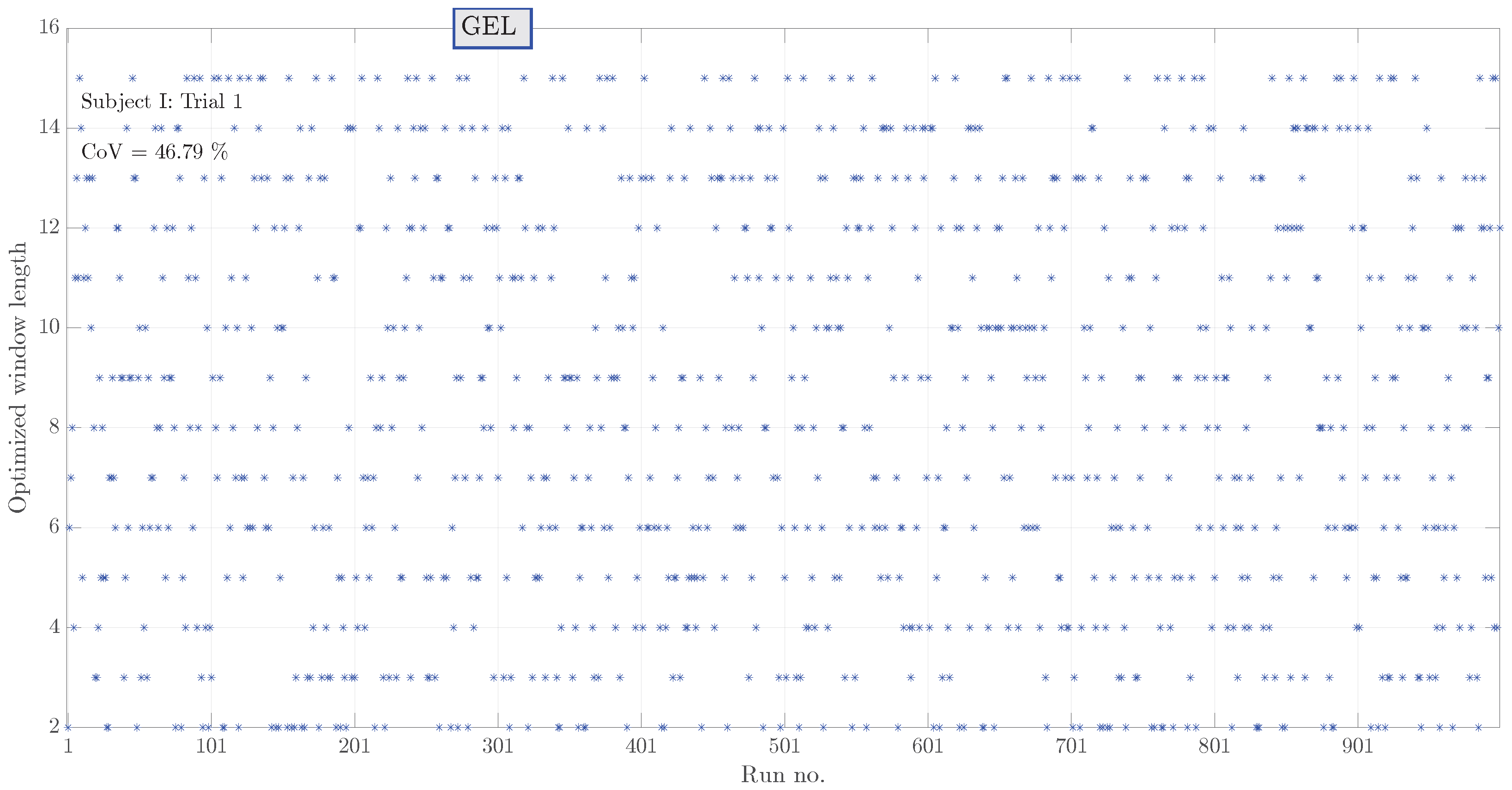
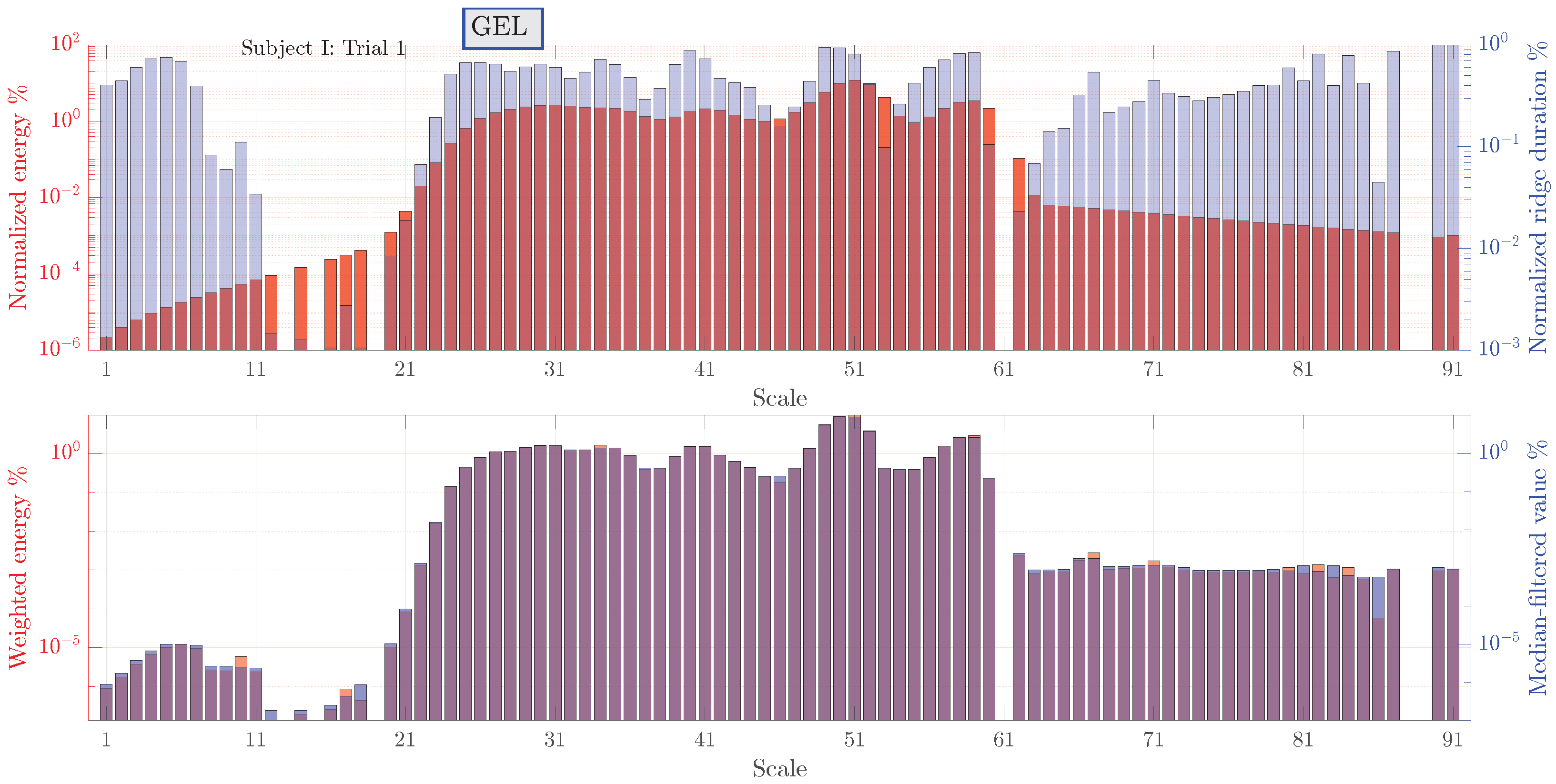
5.3. Noise Detection
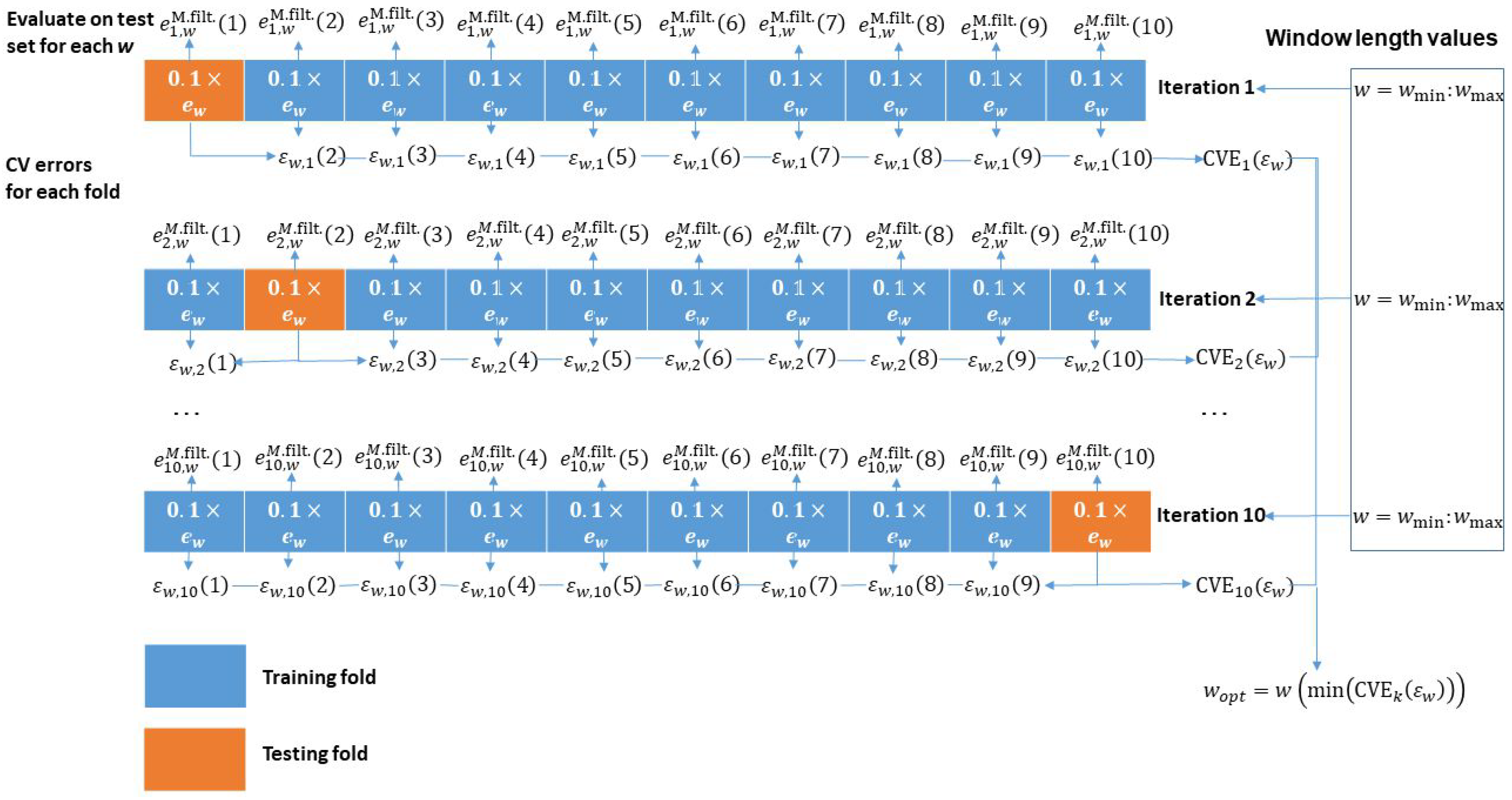
5.4. Signal Quality
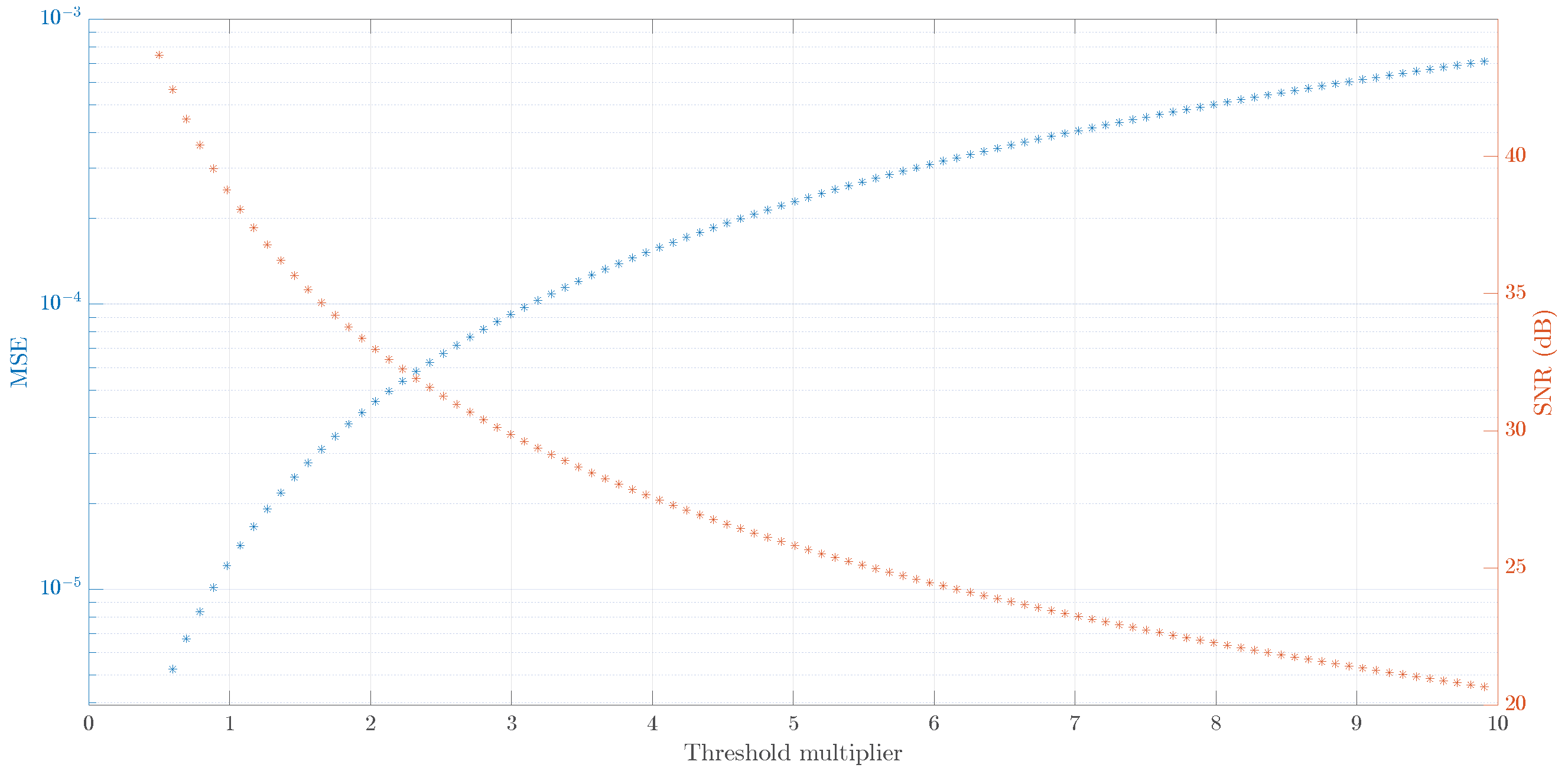
5.5. Classical Wavelet Transform Approach
6. Conclusions
- Visualization of signal components in time-frequency plane aids in signal quality estimation. The most intensive signal components corresponding to heartbeat are traced through the whole duration of the signal. Other components, including noise, can also be traced in terms of their amplitude and duration as indicated by wavelet scalograms.
- PPG signals are helpful to be correlated with bioimpedance signals to match the heartbeat component. PPG scalograms show that apart from the heartbeat component, signals are relatively clean. This means that the other components as seen in bioimpedance scalograms likely correspond to noise.
- The measured bioimpedance signals are non-stationary and are not normally distributed, meaning that many existing methods for signal quality estimation such as autocorrelation are not applicable. The proposed method, on the other hand, is based on wavelet transform of the measured signal and, hence, can handle signal non-stationarity and non-normality.
- The developed signal quality estimation method is fully adaptive. Compared to the classical wavelet-based signal denoising and signal-to-noise ratio estimation, there is no need to set fixed threshold levels or select proper threshold types. Instead, median filtering with an optimized window length is performed and noise is estimated from the available ridge information. SNR estimates obtained with the classical and the proposed methods are within error bounds.
- The effect of coupling agent does not have a significant impact on signal quality as assessed by the SNR. All the differences are within the error bounds. Also, there is no evidence that physical activity levels, age and BMI of test subjects have a role in signal quality of the bioimpedance signals. Again, all differences are within error bounds.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mansouri, S.; Chabchoub, S.; Alharbi, Y.; Alshrouf, A.; Nebhen, J. A Real-Time Heart Rate Detection Algorithm Based on Peripheral Electrical Bioimpedance. IEEJ Trans. Electr. Electron. Eng. 2022, 17, 1054–1060. [Google Scholar] [CrossRef]
- Lapsa, D.; Janeliukštis, R.; Elsts, A. Electrode Comparison for Heart Rate Detection via Bioimpedance Measurements. In Proceedings of the 2022 Workshop on Microwave Theory and Techniques in Wireless Communications (MTTW), Riga, Latvia, 5–7 October 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 41–46. [Google Scholar]
- Lenis, G.; Pilia, N.; Loewe, A.; Schulze, W.H.; Dössel, O. Comparison of baseline wander removal techniques considering the preservation of ST changes in the ischemic ECG: A simulation study. Comput. Math. Methods Med. 2017, 2017, 9295029. [Google Scholar] [CrossRef] [PubMed]
- Asgari, S.; Mehrnia, A. A novel low-complexity digital filter design for wearable ECG devices. PLoS ONE 2017, 12, e0175139. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Dong, A.; Shu, M.; Wang, Y. Sparse ECG denoising with generalized minimax concave penalty. Sensors 2019, 19, 1718. [Google Scholar] [CrossRef]
- Chen, B.; Li, Y.; Cao, X.; Sun, W.; He, W. Removal of power line interference from ECG signals using adaptive notch filters of sharp resolution. IEEE Access 2019, 7, 150667–150676. [Google Scholar] [CrossRef]
- Appathurai, A.; Carol, J.J.; Raja, C.; Kumar, S.; Daniel, A.V.; Malar, A.J.G.; Fred, A.L.; Krishnamoorthy, S. A study on ECG signal characterization and practical implementation of some ECG characterization techniques. Measurement 2019, 147, 106384. [Google Scholar] [CrossRef]
- Poungponsri, S.; Yu, X. An adaptive filtering approach for electrocardiogram (ECG) signal noise reduction using neural networks. Neurocomputing 2013, 117, 206–213. [Google Scholar] [CrossRef]
- Mohebbian, M.R.; Alam, M.W.; Wahid, K.A.; Dinh, A. Single channel high noise level ECG deconvolution using optimized blind adaptive filtering and fixed-point convolution kernel compensation. Biomed. Signal Process. Control 2020, 57, 101673. [Google Scholar] [CrossRef]
- Rakshit, M.; Das, S. An efficient ECG denoising methodology using empirical mode decomposition and adaptive switching mean filter. Biomed. Signal Process. Control 2018, 40, 140–148. [Google Scholar] [CrossRef]
- Kumar, S.; Panigrahy, D.; Sahu, P. Denoising of electrocardiogram (ECG) signal by using empirical mode decomposition (EMD) with non-local mean (NLM) technique. Biocybern. Biomed. Eng. 2018, 38, 297–312. [Google Scholar] [CrossRef]
- Vázquez, R.; Velez-Perez, H.; Ranta, R.; Dorr, V.; Maquin, D.; Maillard, L. Blind source separation wavelet denoising and discriminant analysis for EEG artefacts and noise cancelling. Biomed. Signal Process. Control 2012, 7, 389–400. [Google Scholar] [CrossRef]
- Singhal, A.; Singh, P.; Fatimah, B.; Pachori, R. An efficient removal of power-line interference and baseline wander from ECG signals by employing Fourier decomposition technique. Biomed. Signal Process. Control 2020, 57, 101741. [Google Scholar] [CrossRef]
- Kumar, A.; Tomar, H.; Mehla, V.K.; Komaragiri, R.; Kumar, M. Stationary wavelet transform based ECG signal denoising method. ISA Trans. 2021, 114, 251–262. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Komaragiri, R.; Kumar, M. Heart rate monitoring and therapeutic devices: A wavelet transform based approach for the modeling and classification of congestive heart failure. ISA Trans. 2018, 79, 239–250. [Google Scholar] [CrossRef]
- Kumar, A.; Kumar, M.; Komaragiri, R. Design of a biorthogonal wavelet transform based R-peak detection and data compression scheme for implantable cardiac pacemaker systems. J. Med. Syst. 2018, 42, 102. [Google Scholar] [CrossRef]
- Berwal, D.; Vandana, C.; Dewan, S.; Jiji, C.; Baghini, M.S. Motion artifact removal in ambulatory ECG signal for heart rate variability analysis. IEEE Sens. J. 2019, 19, 12432–12442. [Google Scholar] [CrossRef]
- Li, C.; Deng, H.; Yin, S.; Wang, C.; Zhu, Y. sEMG signal filtering study using synchrosqueezing wavelet transform with differential evolution optimized threshold. Results Eng. 2023, 18, 101150. [Google Scholar] [CrossRef]
- Donoho, D.; Johnstone, I. Adapting to unknown smoothness via wavelet shrinkage. J. Am. Stat. Assoc. 1995, 90, 1200–1224. [Google Scholar] [CrossRef]
- Sai, C.Y.; Mokhtar, N.; Arof, H.; Cumming, P.; Iwahashi, M. Automated classification and removal of EEG artifacts with SVM and wavelet-ICA. IEEE J. Biomed. Health Inform. 2018, 22, 664–670. [Google Scholar] [CrossRef]
- Singh, P.; Pradhan, G.; Shahnawazuddin, S. Denoising of ECG signal by non-local estimation of approximation coefficients in DWT. Biocybern. Biomed. Eng. 2017, 37, 599–610. [Google Scholar] [CrossRef]
- Storn, R.; Price, K. Differential evolution—A simple and efficient heuristic for global optimization over continuous spaces. J. Glob. Optim. 1997, 11, 341–359. [Google Scholar] [CrossRef]
- Elsts, A.; McConville, R. Are microcontrollers ready for deep learning-based human activity recognition? Electronics 2021, 10, 2640. [Google Scholar] [CrossRef]
- Critcher, S.; Freeborn, T.J. Localized bioimpedance measurements with the max3000x integrated circuit: Characterization and demonstration. Sensors 2021, 21, 3013. [Google Scholar] [CrossRef] [PubMed]
- Grimnes, S.; Martinsen, Ø.G. Sources of error in tetrapolar impedance measurements on biomaterials and other ionic conductors. J. Phys. Appl. Phys. 2006, 40, 9. [Google Scholar] [CrossRef]
- Yılmaz, K.; Adeyemi, A.; Antink, C.H.; Vehkaoja, A. Comparison of Electrode Configurations for Impedance Plethysmography Based Heart Rate Estimation at the Forearm. In Proceedings of the 2022 IEEE Sensors, Dallas, TX, USA, 30 October–2 November 2022; IEEE: Piscataway, NJ, USA, 2022; pp. 1–4. [Google Scholar]
- TENS GEL. Available online: https://en.morettispa.com/prodotto/gel-per-e-c-g-e-tens-260-g/ (accessed on 1 October 2023).
- Hydrogel Pads. Available online: https://www.amazon.com/UYGHHK-Trainer-Replacement-Stimulator-Training/dp/B07MK6K8HK (accessed on 1 October 2023).
- Gajewski, P.; Żyła, W.; Kazimierczak, K.; Marcinkowska, A. Hydrogel Polymer Electrolytes: Synthesis, Physicochemical Characterization and Application in Electrochemical Capacitors. Gels 2023, 9, 527. [Google Scholar] [CrossRef]
- Ishai, P.B.; Talary, M.S.; Caduff, A.; Levy, E.; Feldman, Y. Electrode polarization in dielectric measurements: A review. Meas. Sci. Technol. 2013, 24, 102001. [Google Scholar] [CrossRef]
- Shin, H.S.; Lee, C.; Lee, M. Adaptive threshold method for the peak detection of photoplethysmographic waveform. Comput. Biol. Med. 2009, 39, 1145–1152. [Google Scholar] [CrossRef]
- Jia, Y.; Pengfei, X. Noise cancellation in vibration signals using an oversampling and two-stage autocorrelation model. Results Eng. 2020, 6, 100136. [Google Scholar] [CrossRef]



| Family | Name | Max Clock Frequency | Architecture | Radio |
|---|---|---|---|---|
| nRF52 | nRF52840 | 64-MHz | Cortex M4F | BLE 5, IEEE 802.15.4, Propr. 2.4 GHz |
| nRF52 | nRF52832 | 64-MHz | Cortex M4F | BLE 5.1, Propr. 2.4 GHz |
| nRF53 | nRF5340 | 128-MHz | Cortex M33 | BLE 5.2, IEEE 802.15.4, Propr. 2.4 GHz |
| TI SimpleLink | CC2652R | 48-MHz | Cortex M4F | BLE 5.1, IEEE 802.15.4 |
| MSP432 | msp432p401r | 48-MHz | Cortex M4F | No Built-in |
| STM32L | STM32L475 | 48-MHz | Cortex M4F | No Built-in |
| ESP32 | ESP32 | 240-MHz | Xtensa LX6 | BLE 5.0, WIFI, IEEE 802.11 b/g/n, |
| ESP32-C3 | ESP32-C3 | 160-MHz | RISC-V | BLE 5.0, WIFI, IEEE 802.11 b/g/n, |
| EFR32 | EFR32BG22 | 76.8-MHz | Cortex M33 | BLE 5.2, 802.15.4 g |
| SAM3X | ATSAM3X8E | 84-MHz | Cortex M3 | No Built-in |
| Name | Active Current/Radio Current @0 dB | Avg. mA | RAM | FLASH | ||||
|---|---|---|---|---|---|---|---|---|
| mA | µA/MHz | Rx (mA) | Tx (mA) | RAM ret. (µA) | @ 48 MHz | kB | kB | |
| nRF52840 | 3.328 | 52 | 4.6 | 4.8 | 3.16 | 53.1 | 256 | 1024 |
| nRF52832 | 3.7 | 58 | 5.4 | 5.3 | 1.9 | 57.6 | 64/32 | 512/256 |
| nRF5340 | 7.3 | 57 | 3.8 | 4.2 | 2.3 | 57 | 512 + 64 | 1024 + 256 |
| CC2652R | 3.4 | 70.8 | 6.9 | 7.3 | 0.94 | 69 | 80 | 352 |
| msp432p401r | 3.84 | 80 | - | - | 0.35 | - | 64 | 256 |
| STM32L475 | 8 | 166.7 | - | - | 0.236 | - | 128 | 1000 |
| ESP32 | 68 | 283.3 | 100 | 130 | 10 | 282.9 | 400 | 384 |
| ESP32-C3 | 20 | 125 | - | - | 5 | - | 400 | 384 |
| EFR32BG22 | 2.07 | 27 | 3.6 | 4.1 | 1.4 | 27.3 | 32 | 512 |
| ATSAM3X8E | 70.89 | 923 | - | - | 2.5 | - | 96 | 512 |
| Subject | Gender | Age (Years) | Mass (kg) | Height (m) | BMI | Activity Level |
|---|---|---|---|---|---|---|
| I | male | 34 | 76 | 1.80 | 23.46 | high |
| II | male | 54 | 94 | 1.84 | 27.76 | low |
| III | male | 22 | 57 | 1.78 | 17.99 | medium |
| IV | male | 30 | 75 | 1.95 | 19.72 | medium |
| V | male | 39 | 70 | 1.83 | 20.90 | medium |
| VI | male | 26 | 83 | 1.83 | 24.78 | medium |
| VII | female | 23 | 70 | 1.75 | 22.86 | low |
| VIII | male | 30 | 88 | 1.75 | 28.73 | high |
| IX | male | 24 | 105 | 2.03 | 25.48 | low |
| Kolmogorov–Smirnov Test | Anderson–Darling Test | Jarque–Bera Test | |||||||
|---|---|---|---|---|---|---|---|---|---|
| p-Value | KS | KS Crit. | p-Value | AD | AD Crit. | p-Value | JB | JB Crit. | |
| Gel #1 | 0 | 0.27 | 0.0197 | 0.0005 | 3.59 | 0.75 | 0.001 | 28.26 | 5.98 |
| Gel #2 | 0 | 0.32 | 0.0195 | 0.0005 | 6.37 | 0.75 | 0.001 | 31.09 | 5.98 |
| Gel #3 | 0 | 0.28 | 0.0197 | 0.0005 | 5.97 | 0.75 | 0.001 | 37.29 | 5.98 |
| Gel #4 | 0 | 0.25 | 0.0196 | 0.0005 | 6.10 | 0.75 | 0.001 | 55.09 | 5.98 |
| Gel #5 | 0 | 0.29 | 0.0197 | 0.0005 | 2.31 | 0.75 | 0.001 | 20.11 | 5.98 |
| Gel #6 | 0 | 0.26 | 0.0196 | 0.0005 | 3.90 | 0.75 | 0.001 | 20.00 | 5.98 |
| Gel #7 | 0 | 0.30 | 0.0193 | 0.0005 | 1.80 | 0.75 | 0.001 | 15.05 | 5.98 |
| Gel #8 | 0 | 0.30 | 0.0203 | 0.0005 | 5.21 | 0.75 | 0.001 | 68.05 | 5.98 |
| Gel #9 | 0 | 0.27 | 0.0198 | 0.0005 | 2.70 | 0.75 | 0.001 | 21.72 | 5.98 |
| Gel #10 | 0 | 0.26 | 0.0198 | 0.0044 | 1.18 | 0.75 | 0.006 | 10.71 | 5.98 |
| H.gel #1 | 0 | 0.36 | 0.0168 | 0.0005 | 2.29 | 0.75 | 0.001 | 240.36 | 5.98 |
| H.gel #2 | 0 | 0.31 | 0.0191 | 0.0005 | 1.87 | 0.75 | 0.006 | 10.41 | 5.98 |
| H.gel #3 | 0 | 0.27 | 0.0193 | 0.0005 | 5.52 | 0.75 | 0.003 | 12.57 | 5.98 |
| H.gel #4 | 0 | 0.31 | 0.0196 | 0.0005 | 6.43 | 0.75 | 0.001 | 28.12 | 5.98 |
| H.gel #5 | 0 | 0.26 | 0.0195 | 0.0005 | 4.17 | 0.75 | 0.001 | 37.50 | 5.98 |
| H.gel #6 | 0 | 0.25 | 0.0196 | 0.0005 | 7.05 | 0.75 | 0.001 | 55.15 | 5.98 |
| H.gel #7 | 0 | 0.26 | 0.0195 | 0.0005 | 15.19 | 0.75 | 0.001 | 89.20 | 5.98 |
| H.gel #8 | 0 | 0.27 | 0.0194 | 0.0005 | 4.72 | 0.75 | 0.001 | 31.16 | 5.98 |
| H.gel #9 | 0 | 0.26 | 0.0199 | 0.0005 | 7.07 | 0.75 | 0.001 | 41.09 | 5.98 |
| H.gel #10 | 0 | 0.27 | 0.0195 | 0.0005 | 12.84 | 0.75 | 0.001 | 81.95 | 5.98 |
| Augmented Dickey–Fuller Test | Variance Ratio Test | |||||
|---|---|---|---|---|---|---|
| p-Value | ADF | ADF Crit. | p-Value | VR | VR Crit. | |
| Gel #1 | 0.001 | −6.79 | −1.94 | 0 | 35.14 | 1.96 |
| Gel #2 | 0.001 | −7.51 | −1.94 | 0 | 34.97 | 1.96 |
| Gel #3 | 0.001 | −6.88 | −1.94 | 0 | 35.26 | 1.96 |
| Gel #4 | 0.001 | −7.43 | −1.94 | 0 | 36.39 | 1.96 |
| Gel #5 | 0.001 | −7.06 | −1.94 | 0 | 33.30 | 1.96 |
| Gel #6 | 0.001 | −7.26 | −1.94 | 0 | 34.65 | 1.96 |
| Gel #7 | 0.001 | −7.53 | −1.94 | 0 | 36.12 | 1.96 |
| Gel #8 | 0.001 | −7.43 | −1.94 | 0 | 34.97 | 1.96 |
| Gel #9 | 0.001 | −7.23 | −1.94 | 0 | 33.79 | 1.96 |
| Gel #10 | 0.001 | −7.68 | −1.94 | 0 | 34.22 | 1.96 |
| Hydrogel #1 | 0.001 | −7.76 | −1.94 | 0 | 40.81 | 1.96 |
| Hydrogel #2 | 0.001 | −6.55 | −1.94 | 0 | 35.91 | 1.96 |
| Hydrogel #3 | 0.001 | −6.44 | −1.94 | 0 | 33.95 | 1.96 |
| Hydrogel #4 | 0.001 | −6.11 | −1.94 | 0 | 34.35 | 1.96 |
| Hydrogel #5 | 0.001 | −6.92 | −1.94 | 0 | 34.74 | 1.96 |
| Hydrogel #6 | 0.001 | −6.18 | −1.94 | 0 | 35.13 | 1.96 |
| Hydrogel #7 | 0.001 | −6.86 | −1.94 | 0 | 36.19 | 1.96 |
| Hydrogel #8 | 0.001 | −6.76 | −1.94 | 0 | 33.42 | 1.96 |
| Hydrogel #9 | 0.001 | −5.97 | −1.94 | 0 | 34.17 | 1.96 |
| Hydrogel #10 | 0.001 | −6.34 | −1.94 | 0 | 34.92 | 1.96 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lapsa, D.; Janeliukstis, R.; Elsts, A. Adaptive Signal-to-Noise Ratio Indicator for Wearable Bioimpedance Monitoring. Sensors 2023, 23, 8532. https://doi.org/10.3390/s23208532
Lapsa D, Janeliukstis R, Elsts A. Adaptive Signal-to-Noise Ratio Indicator for Wearable Bioimpedance Monitoring. Sensors. 2023; 23(20):8532. https://doi.org/10.3390/s23208532
Chicago/Turabian StyleLapsa, Didzis, Rims Janeliukstis, and Atis Elsts. 2023. "Adaptive Signal-to-Noise Ratio Indicator for Wearable Bioimpedance Monitoring" Sensors 23, no. 20: 8532. https://doi.org/10.3390/s23208532
APA StyleLapsa, D., Janeliukstis, R., & Elsts, A. (2023). Adaptive Signal-to-Noise Ratio Indicator for Wearable Bioimpedance Monitoring. Sensors, 23(20), 8532. https://doi.org/10.3390/s23208532






