Real-Life Wheelchair Mobility Metrics from IMUs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Sample
2.2. Data Collection
- Distance covered;
- Linear velocity of the wheelchair;
- Number of pushes;
- Duration of pushes;
- Number of turns;
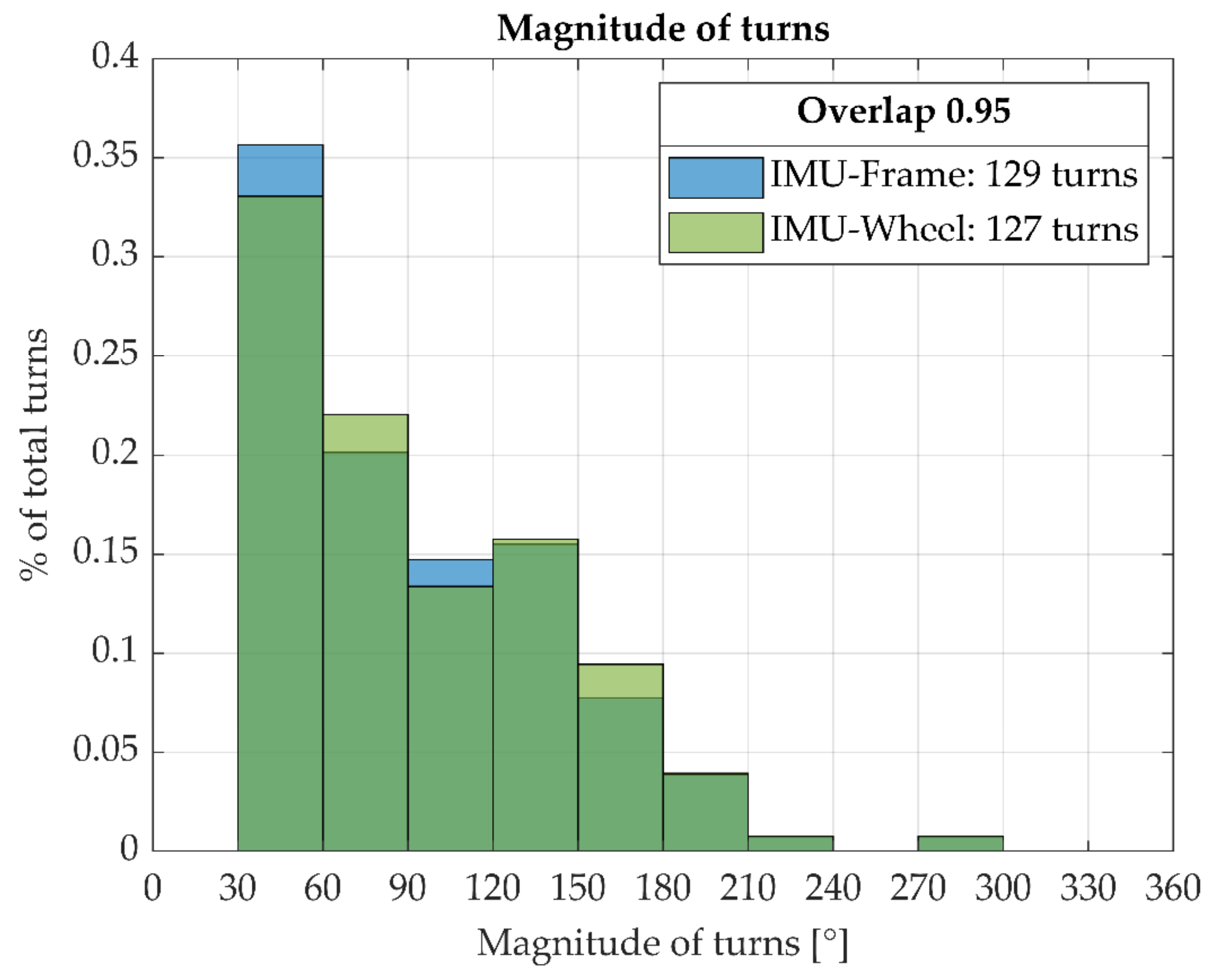
- Magnitude of turns;
- Wheelchair inclination.
2.3. Preprocessing of IMU Data
2.4. Derivation of WCMM Variables from Reference Methods and IMU Data
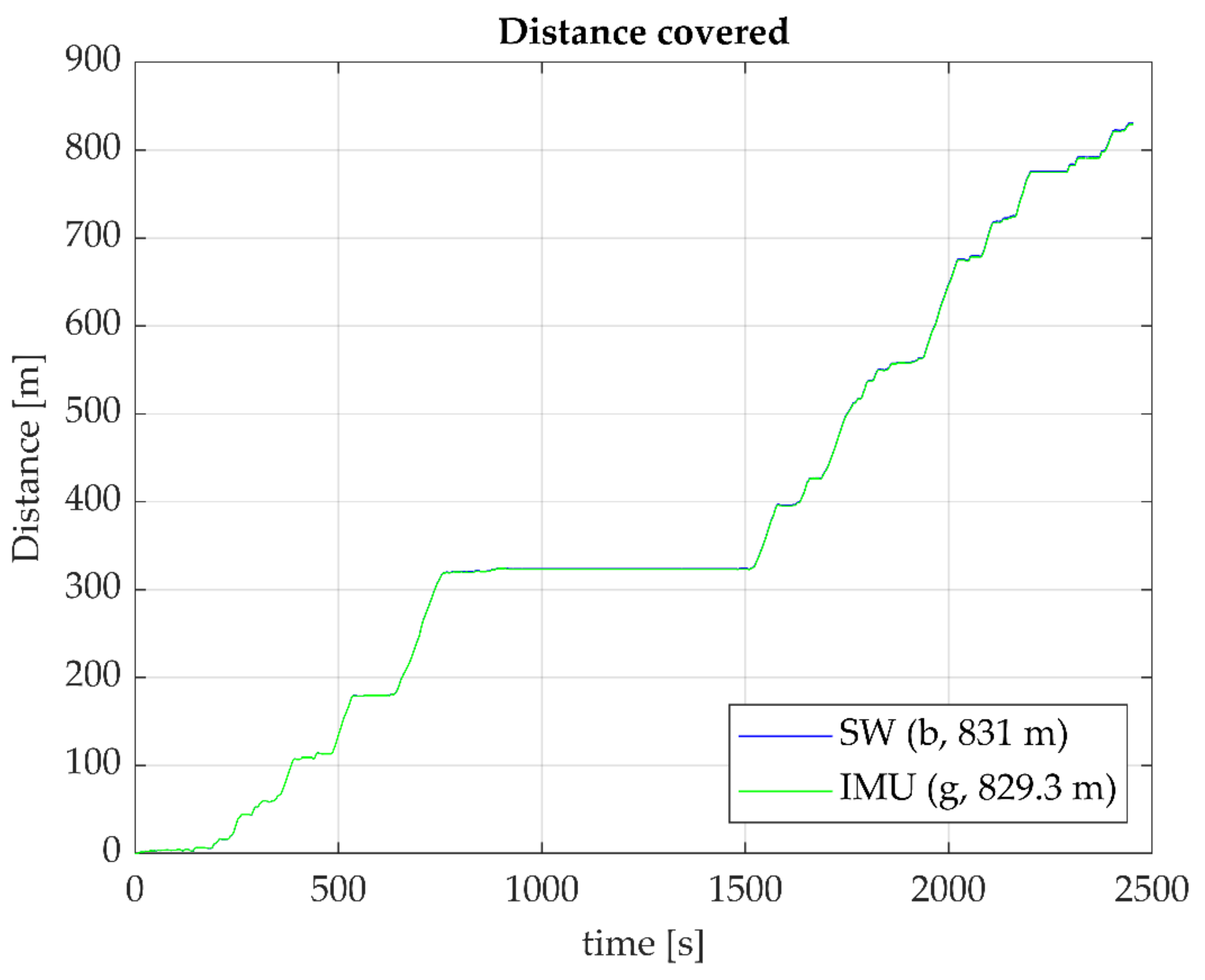
2.4.1. Distance Covered
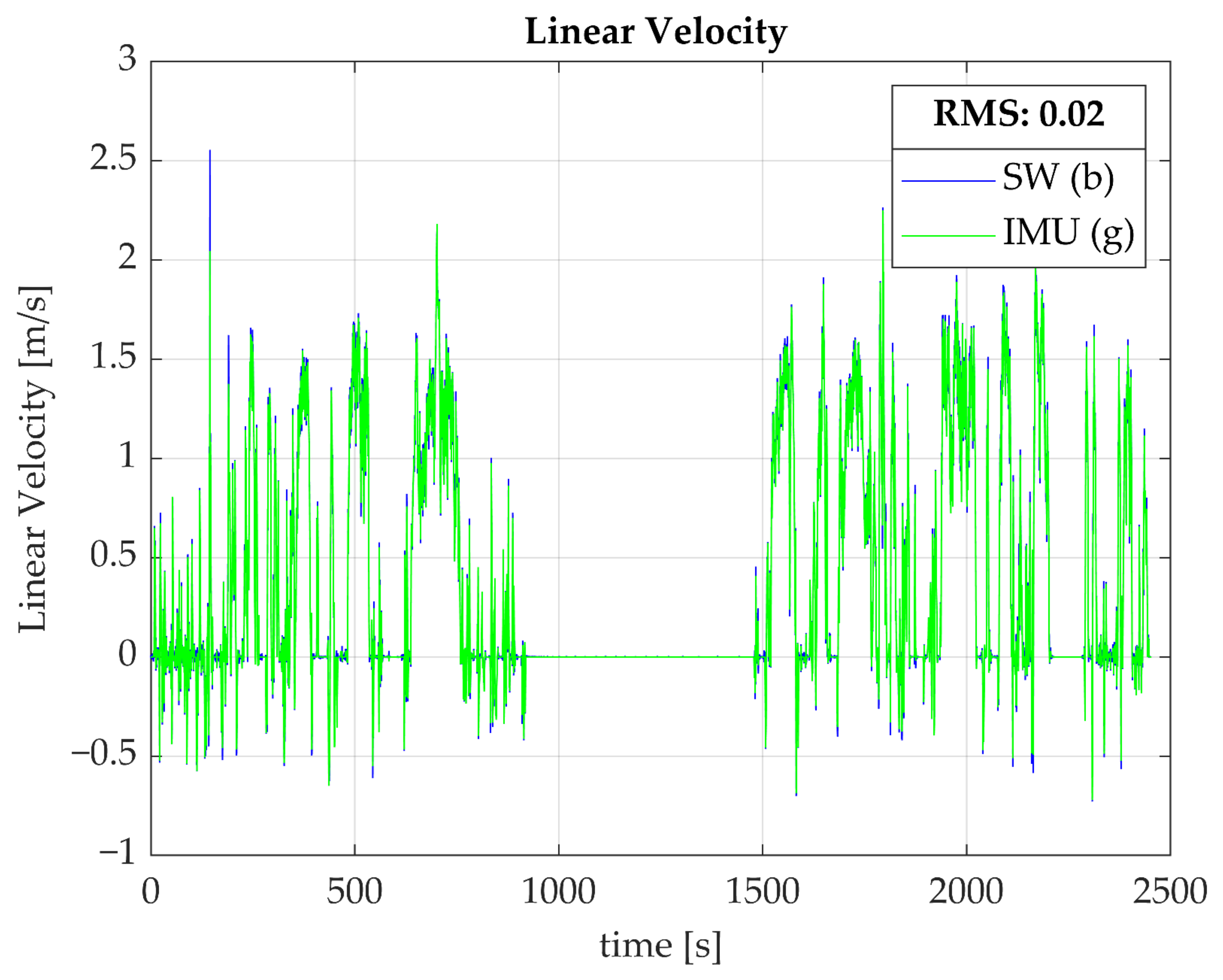
2.4.2. Linear Velocity
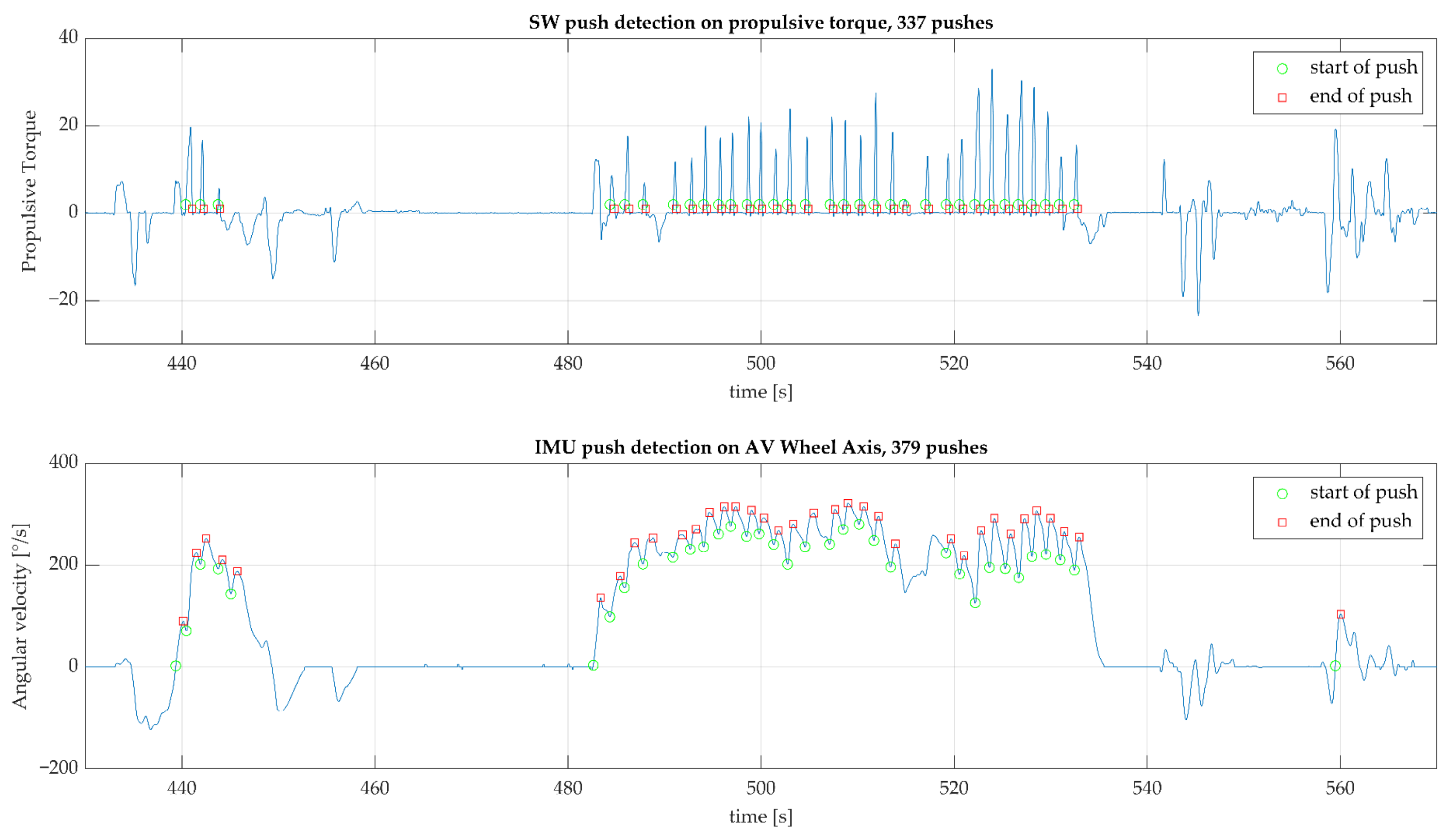
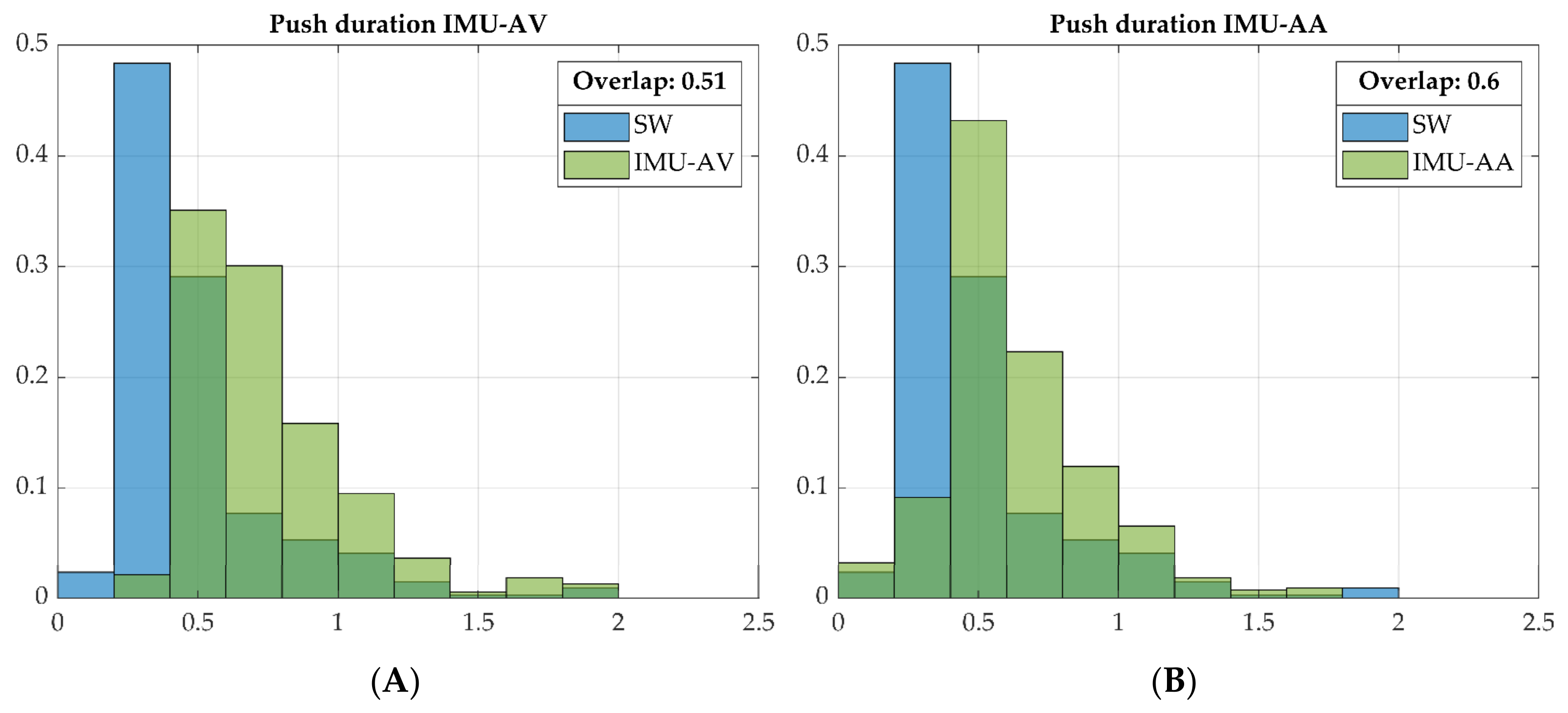
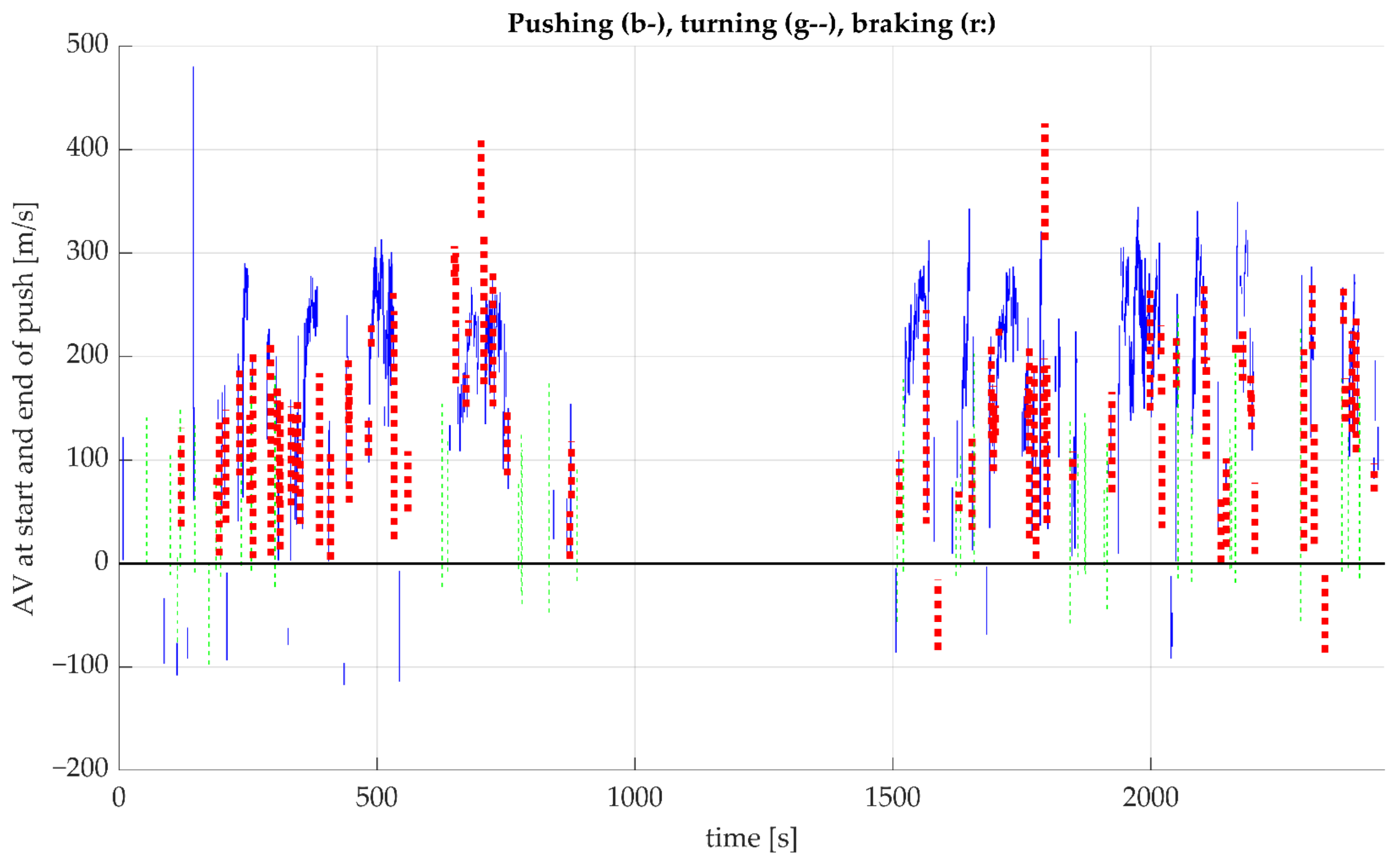
2.4.3. Number and Duration of Pushes
2.4.4. Number and Magnitude of Turns
2.4.5. Wheelchair Inclination
3. Results
3.1. Study Sample
3.2. Derivation of WCMM Variables from Smartwheel and IMU Data
3.2.1. Distance Covered
3.2.2. Linear Velocity
3.2.3. Number and Duration of Pushes
3.2.4. Number and Magnitude of Turns
3.2.5. Wheelchair Inclination
4. Discussion
4.1. Study Sample
4.2. Derivation of WCMM Variables from the Smartwheel and IMU Data
4.2.1. Distance Covered
4.2.2. Linear Velocity
4.2.3. Number and Duration of Pushes
4.2.4. Number and Magnitude of Turns
4.2.5. Wheelchair Inclination
4.3. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Liampas, A.; Neophytou, P.; Sokratous, M.; Varrassi, G.; Ioannou, C.; Hadjigeorgiou, G.M.; Zis, P. Musculoskeletal Pain Due to Wheelchair Use: A Systematic Review and Meta-Analysis. Pain Ther. 2021, 10, 973–984. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, F.M.; Arnet, U.; Brinkhof, M.W.G.; Eriks-Hoogland, I.; Lay, V.; Muller, R.; Sunnaker, M.; Hinrichs, T.; Swi, S.C.I.S.G. Shoulder pain in the Swiss spinal cord injury community: Prevalence and associated factors. Disabil. Rehabil. 2018, 40, 798–805. [Google Scholar] [CrossRef]
- Akbar, M.; Brunner, M.; Balean, G.; Grieser, T.; Bruckner, T.; Loew, M.; Raiss, P. A cross-sectional study of demographic and morphologic features of rotator cuff disease in paraplegic patients. J. Shoulder Elb. Surg./Am. Shoulder Elb. Surg. 2011, 20, 1108–1113. [Google Scholar] [CrossRef] [PubMed]
- Piatt, J.A.; Nagata, S.; Zahl, M.; Li, J.; Rosenbluth, J.P. Problematic secondary health conditions among adults with spinal cord injury and its impact on social participation and daily life. J. Spinal Cord Med. 2016, 39, 693–698. [Google Scholar] [CrossRef]
- Westgren, N.; Levi, R. Quality of life and traumatic spinal cord injury. Arch. Phys. Med. Rehabil. 1998, 79, 1433–1439. [Google Scholar] [CrossRef] [PubMed]
- Dalyan, M.; Cardenas, D.D.; Gerard, B. Upper extremity pain after spinal cord injury. Spinal Cord 1999, 37, 191–195. [Google Scholar] [CrossRef] [PubMed]
- Mercer, J.L.; Boninger, M.; Koontz, A.; Ren, D.; Dyson-Hudson, T.; Cooper, R. Shoulder joint kinetics and pathology in manual wheelchair users. Clin. Biomech. 2006, 21, 781–789. [Google Scholar] [CrossRef] [PubMed]
- Van Drongelen, S.; Van der Woude, L.H.; Janssen, T.W.; Angenot, E.L.; Chadwick, E.K.; Veeger, D.H. Mechanical load on the upper extremity during wheelchair activities. Arch. Phys. Med. Rehabil. 2005, 86, 1214–1220. [Google Scholar] [CrossRef] [PubMed]
- Hogaboom, N.S.; Worobey, L.A.; Boninger, M.L. Transfer Technique Is Associated With Shoulder Pain and Pathology in People With Spinal Cord Injury: A Cross-Sectional Investigation. Arch. Phys. Med. Rehabil. 2016, 97, 1770–1776. [Google Scholar] [CrossRef]
- Akbar, M.; Balean, G.; Brunner, M.; Seyler, T.M.; Bruckner, T.; Munzinger, J.; Grieser, T.; Gerner, H.J.; Loew, M. Prevalence of rotator cuff tear in paraplegic patients compared with controls. J Bone Jt. Surg Am.. 2010, 92, 23–30. [Google Scholar] [CrossRef]
- Arnet, U.; van Drongelen, S.; Scheel-Sailer, A.; van der Woude, L.H.; Veeger, D.H. Shoulder load during synchronous handcycling and handrim wheelchair propulsion in persons with paraplegia. J. Rehabil. Med. 2012, 44, 222–228. [Google Scholar] [CrossRef][Green Version]
- Veeger, H.E.; Rozendaal, L.A.; van der Helm, F.C. Load on the shoulder in low intensity wheelchair propulsion. Clin. Biomech. 2002, 17, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, F.M.; Boninger, M.L.; Cools, A.; Hogaboom, N.; Eriks-Hoogland, I.; Arnet, U.; Swi, S.C.I.S.G. Changes in supraspinatus and biceps tendon thickness: Influence of fatiguing propulsion in wheelchair users with spinal cord injury. Spinal Cord 2020, 58, 324–333. [Google Scholar] [CrossRef]
- Morrow, M.M.; Van Straaten, M.G.; Murthy, N.S.; Braman, J.P.; Zanella, E.; Zhao, K.D. Detailed shoulder MRI findings in manual wheelchair users with shoulder pain. Biomed. Res. Int. 2014, 2014, 769649. [Google Scholar] [CrossRef] [PubMed]
- Beirens, B.J.H.; Bossuyt, F.M.; Arnet, U.; van der Woude, L.H.V.; de Vries, W.H.K. Shoulder Pain Is Associated with Rate of Rise and Jerk of the Applied Forces during Wheelchair Propulsion in Individuals with Paraplegic Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2021, 102, 856–864. [Google Scholar] [CrossRef]
- Li, Y.; Li, F.M.; Carrington, P. Breaking the “Inescapable” Cycle of Pain: Supporting Wheelchair Users’ Upper Extremity Health Awareness and Management with Tracking Technologies. In Proceedings of the 2023 CHI Conference on Human Factors in Computing Systems, Hamburg, Germany, 23–28 April 2023; pp. 1–17. [Google Scholar]
- Jayaraman, C.; Moon, Y.; Sosnoff, J.J. Shoulder pain and time dependent structure in wheelchair propulsion variability. Med. Eng. Phys. 2016, 38, 648–655. [Google Scholar] [CrossRef] [PubMed]
- Arnet, U.; van Drongelen, S.; Veeger, D.H.; van der Woude, L.H. Force application during handcycling and handrim wheelchair propulsion: An initial comparison. J. Appl. Biomech. 2013, 29, 687–695. [Google Scholar] [CrossRef]
- Rice, I.; Impink, B.; Niyonkuru, C.; Boninger, M. Manual wheelchair stroke characteristics during an extended period of propulsion. Spinal Cord 2009, 47, 413–417. [Google Scholar] [CrossRef]
- Benning, N.H.; Knaup, P.; Rupp, R. Measurement Performance of Activity Measurements with Newer Generation of Apple Watch in Wheelchair Users with Spinal Cord Injury. Methods Inf. Med. 2021, 60, e103–e110. [Google Scholar] [CrossRef]
- Chen, P.B.; Morgan, K. Toward community-based wheelchair evaluation with machine learning methods. J. Rehabil. Assist. Technol. Eng. 2018, 5, 2055668318808409. [Google Scholar] [CrossRef]
- Chen, P.W.; Klaesner, J.; Zwir, I.; Morgan, K.A. Detecting clinical practice guideline-recommended wheelchair propulsion patterns with wearable devices following a wheelchair propulsion intervention. Assist. Technol. 2023, 35, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Coulter, E.H.; Dall, P.M.; Rochester, L.; Hasler, J.P.; Granat, M.H. Development and validation of a physical activity monitor for use on a wheelchair. Spinal Cord 2011, 49, 445–450. [Google Scholar] [CrossRef]
- Dowling, A.V.; Eberly, V.; Maneekobkunwong, S.; Mulroy, S.J.; Requejo, P.S.; Gwin, J.T. Telehealth monitor to measure physical activity and pressure relief maneuver performance in wheelchair users. Assist. Technol. 2017, 29, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Glasheen, E.; Domingo, A.; Kressler, J. Accuracy of Apple Watch fitness tracker for wheelchair use varies according to movement frequency and task. Ann. Phys. Rehabil. Med. 2021, 64, 101382. [Google Scholar] [CrossRef]
- Hiremath, S.V.; Ding, D.; Cooper, R.A. Development and evaluation of a gyroscope-based wheel rotation monitor for manual wheelchair users. J. Spinal Cord Med. 2013, 36, 347–356. [Google Scholar] [CrossRef]
- Hiremath, S.V.; Ding, D.; Farringdon, J.; Cooper, R.A. Predicting energy expenditure of manual wheelchair users with spinal cord injury using a multisensor-based activity monitor. Arch. Phys. Med. Rehabil. 2012, 93, 1937–1943. [Google Scholar] [CrossRef]
- Karinharju, K.S.; Boughey, A.M.; Tweedy, S.M.; Clanchy, K.M.; Trost, S.G.; Gomersall, S.R. Validity of the Apple Watch((R)) for monitoring push counts in people using manual wheelchairs. J. Spinal Cord Med. 2021, 44, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Karinharju, K.S.; Gomersall, S.R.; Clanchy, K.M.; Trost, S.G.; Yeo, L.T.; Tweedy, S.M. Validity of Two Wheelchair-Mounted Devices for Estimating Wheelchair Speed and Distance Traveled. Adapt. Phys. Act. Q. 2021, 38, 435–451. [Google Scholar] [CrossRef]
- Learmonth, Y.C.; Kinnett-Hopkins, D.; Rice, I.M.; Dysterheft, J.L.; Motl, R.W. Accelerometer output and its association with energy expenditure during manual wheelchair propulsion. Spinal Cord 2016, 54, 110–114. [Google Scholar] [CrossRef]
- Nightingale, T.E.; Walhin, J.P.; Thompson, D.; Bilzon, J.L. Influence of accelerometer type and placement on physical activity energy expenditure prediction in manual wheelchair users. PLoS ONE 2015, 10, e0126086. [Google Scholar] [CrossRef]
- Ojeda, M.; Ding, D. Temporal parameters estimation for wheelchair propulsion using wearable sensors. Biomed. Res. Int. 2014, 2014, 645284. [Google Scholar] [CrossRef]
- Popp, W.L.; Brogioli, M.; Leuenberger, K.; Albisser, U.; Frotzler, A.; Curt, A.; Gassert, R.; Starkey, M.L. A novel algorithm for detecting active propulsion in wheelchair users following spinal cord injury. Med. Eng. Phys. 2016, 38, 267–274. [Google Scholar] [CrossRef]
- Satizabal, H.F.; Grillon, A.; Upegui, A.; Millet, G.; Picasso, G.; Perez-Uribe, A. ActiDote—A wireless sensor-based system for self-tracking activity levels among manual wheelchair users. EAI Endorsed Trans. Pervasive Health Technol. 2017, 3, e5. [Google Scholar] [CrossRef]
- Sonenblum, S.E.; Sprigle, S.; Caspall, J.; Lopez, R. Validation of an accelerometer-based method to measure the use of manual wheelchairs. Med. Eng. Phys. 2012, 34, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.K.; Hasler, J.P.; Dall, P.M.; Granat, M.H. Objective assessment of mobility of the spinal cord injured in a free-living environment. Spinal Cord 2008, 46, 352–357. [Google Scholar] [CrossRef]
- van der Slikke, R.; Berger, M.; Bregman, D.; Veeger, D. Push Characteristics in Wheelchair Court Sport Sprinting. Procedia Eng. 2016, 147, 730–734. [Google Scholar] [CrossRef]
- van der Slikke, R.M.; Berger, M.A.; Bregman, D.J.; Lagerberg, A.H.; Veeger, H.E. Opportunities for measuring wheelchair kinematics in match settings; reliability of a three inertial sensor configuration. J. Biomech. 2015, 48, 3398–3405. [Google Scholar] [CrossRef] [PubMed]
- Mason, B.S.; Rhodes, J.M.; Goosey-Tolfrey, V.L. Validity and reliability of an inertial sensor for wheelchair court sports performance. J. Appl. Biomech. 2014, 30, 326–331. [Google Scholar] [CrossRef]
- Fuss, F.K.; Subic, A.; Chua, J.J.C. Analysis of wheelchair rugby accelerations with fractal dimensions. Procedia Eng. 2012, 34, 439–442. [Google Scholar] [CrossRef]
- Pansiot, J.; Zhang, Z.; Lo, B.; Yang, G.Z. WISDOM: Wheelchair inertial sensors for displacement and orientation monitoring. Meas. Sci. Technol. 2011, 22, 105801. [Google Scholar] [CrossRef]
- van Dijk, M.P.; van der Slikke, R.M.A.; Rupf, R.; Hoozemans, M.J.M.; Berger, M.A.M.; Veeger, D. Obtaining wheelchair kinematics with one sensor only? The trade-off between number of inertial sensors and accuracy for measuring wheelchair mobility performance in sports. J. Biomech. 2022, 130, 110879. [Google Scholar] [CrossRef] [PubMed]
- Gaspar, R.; Padula, N.; Freitas, T.B.; de Oliveira, J.P.J.; Torriani-Pasin, C. Physical Exercise for Individuals With Spinal Cord Injury: Systematic Review Based on the International Classification of Functioning, Disability, and Health. J. Sport Rehabil. 2019, 28, 505–516. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Functioning, Disability and Health: ICF; WHO Publishing: Geneva, Switzerland, 2001. [Google Scholar]
- Vegter, R.J.; Hartog, J.; de Groot, S.; Lamoth, C.J.; Bekker, M.J.; van der Scheer, J.W.; van der Woude, L.H.; Veeger, D.H. Early motor learning changes in upper-limb dynamics and shoulder complex loading during handrim wheelchair propulsion. J. Neuroeng. Rehabil. 2015, 12, 26. [Google Scholar] [CrossRef]
- Cooper, R.A.; DiGiovine, C.P.; Boninger, M.L.; Shimada, S.D.; Koontz, A.M.; Baldwin, M.A. Filter frequency selection for manual wheelchair biomechanics. J. Rehabil. Res. Dev. 2002, 39, 323–336. [Google Scholar] [PubMed]
- Giannouli, E.; Kim, E.K.; Fu, C.; Weibel, R.; Sofios, A.; Infanger, D.; Portegijs, E.; Rantanen, T.; Huang, H.; Schmidt-Trucksass, A.; et al. Psychometric properties of the MOBITEC-GP mobile application for real-life mobility assessment in older adults. Geriatr. Nurs. 2022, 48, 280–286. [Google Scholar] [CrossRef]
- van Dijk, M.P.; van der Slikke, R.M.A.; Berger, M.A.M.; Hoozemans, M.J.M.; Veeger, H.E.J. Look mummy, no hands! The effect of trunk motion on forward wheelchair propulsion. In Proceedings of the 39th International Society of Biomechanics in Sport Conference (Online), Canberra, Australia, 3–6 September 2021. [Google Scholar]
- Chaikhot, D.; Taylor, M.J.D.; de Vries, W.H.K.; Hettinga, F.J. Biomechanics of wheelchair turning manoeuvres: Novel insights into wheelchair propulsion. Front. Sports Act. Living 2023, 5, 1127514. [Google Scholar] [CrossRef]

| Variable | Reference Value | IMUs Value | Error | Error Measure 1 | ICC | p-Value |
|---|---|---|---|---|---|---|
| Distance covered (m) | 647.6 | 646.1 | −0.2% | MAND | 1.000 | <0.001 |
| Linear velocity (m/s) | - | - | 0.02 | RMS | - | |
| Number of pushes AV | 429.6 | 428.6 | 4.1% | MAND | 0.989 | <0.001 |
| Number of pushes AA | 429.6 | 510.9 | 19.1% | MAND | 0.869 | <0.001 |
| Push duration AV (s) | 0.41 | 0.65 | 59.5% | MAND | 0.030 | 0.159 |
| Push duration AA (s) | 0.41 | 0.54 | 33.1% | MAND | 0.129 | 0.048 |
| Cumulated WC turn (figure-8) (°) | 1604 | 1600 | 0.65% | MAND | 1.000 | <0.001 |
| Number of WC turns | 86 | 88 | 3.4% | MAND | 0.977 | <0.001 |
| Magnitude of turns | 95.9% | % overlap | - | |||
| Inclination long slopes 2 | 1.6, 1.8, 2.2 | 1.65, 1.9, 1.8 | 0.3 | MAND | 0.975 3 | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Vries, W.H.K.; van der Slikke, R.M.A.; van Dijk, M.P.; Arnet, U. Real-Life Wheelchair Mobility Metrics from IMUs. Sensors 2023, 23, 7174. https://doi.org/10.3390/s23167174
de Vries WHK, van der Slikke RMA, van Dijk MP, Arnet U. Real-Life Wheelchair Mobility Metrics from IMUs. Sensors. 2023; 23(16):7174. https://doi.org/10.3390/s23167174
Chicago/Turabian Stylede Vries, Wiebe H. K., Rienk M. A. van der Slikke, Marit P. van Dijk, and Ursina Arnet. 2023. "Real-Life Wheelchair Mobility Metrics from IMUs" Sensors 23, no. 16: 7174. https://doi.org/10.3390/s23167174
APA Stylede Vries, W. H. K., van der Slikke, R. M. A., van Dijk, M. P., & Arnet, U. (2023). Real-Life Wheelchair Mobility Metrics from IMUs. Sensors, 23(16), 7174. https://doi.org/10.3390/s23167174







