Real-Time Continuous Monitoring of Oral Soft Tissue Pressure with a Wireless Mouthguard Device for Assessing Tongue Thrusting Habits
Abstract
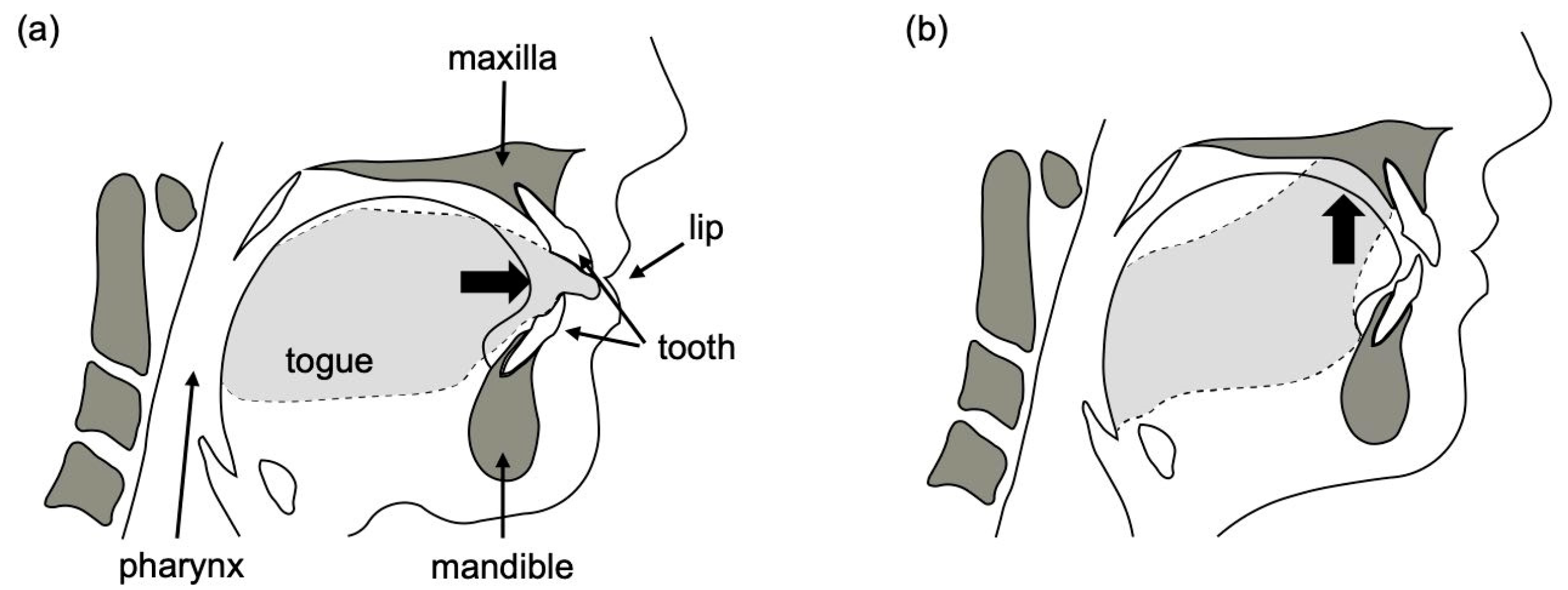
1. Introduction
2. Materials and Methods
2.1. Examination of Sensors Suitable for Measuring Oral Soft Tissue Pressure
2.1.1. Selection of a Pressure Transmission Element
2.1.2. Selection of MG Material for 2D Packaging
2.1.3. Selection of MG Materials for 3D Packaging
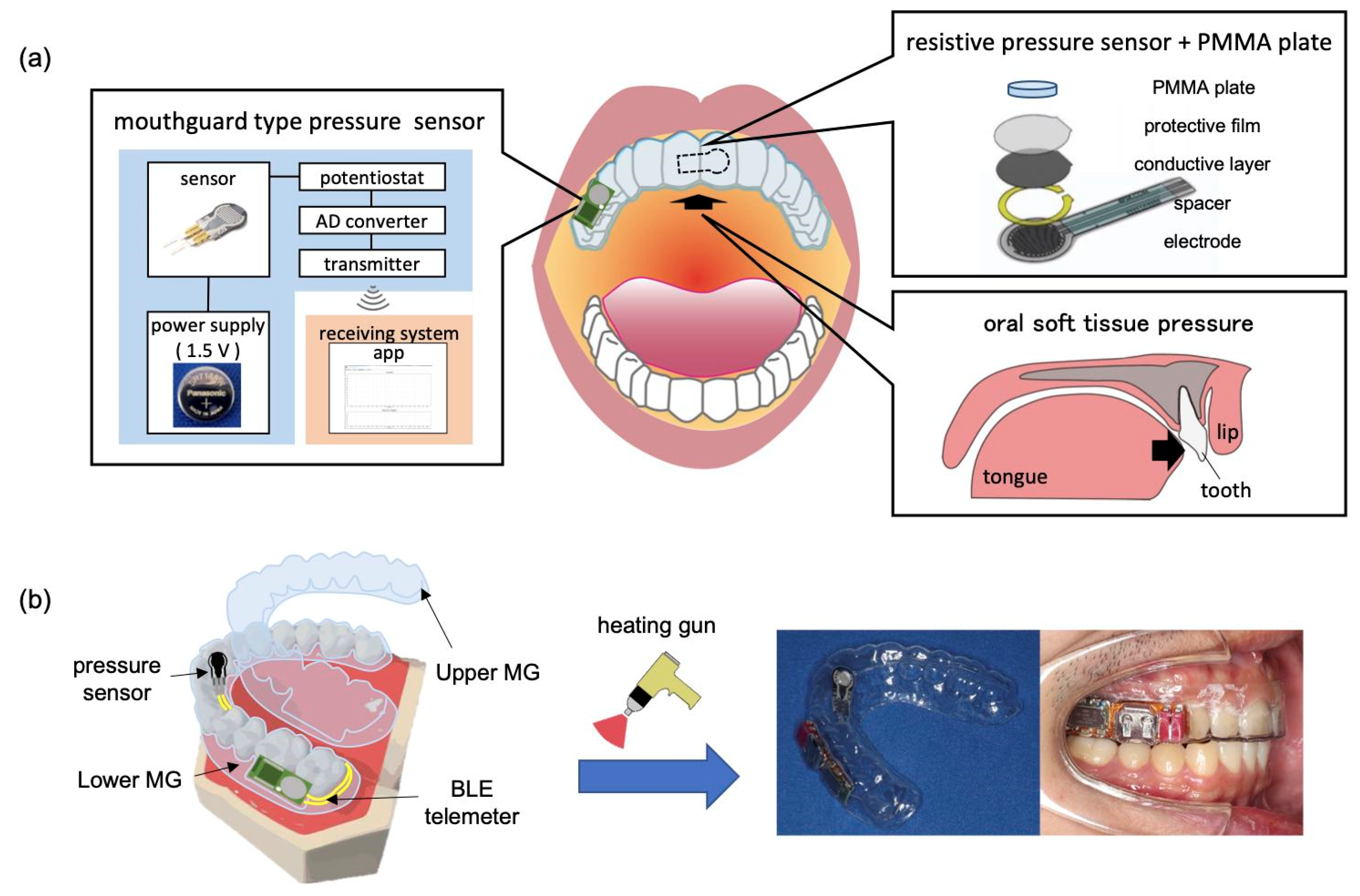
2.2. Pressure Measurement with MG-Type Sensor Device
2.2.1. Fabrication of MG-Type Sensor Device
2.2.2. Evaluation of Sensor Characteristics
2.3. Soft Tissue Pressure Measurement in the Mouth
2.3.1. Evaluation of Sensor Devices in the Mouth
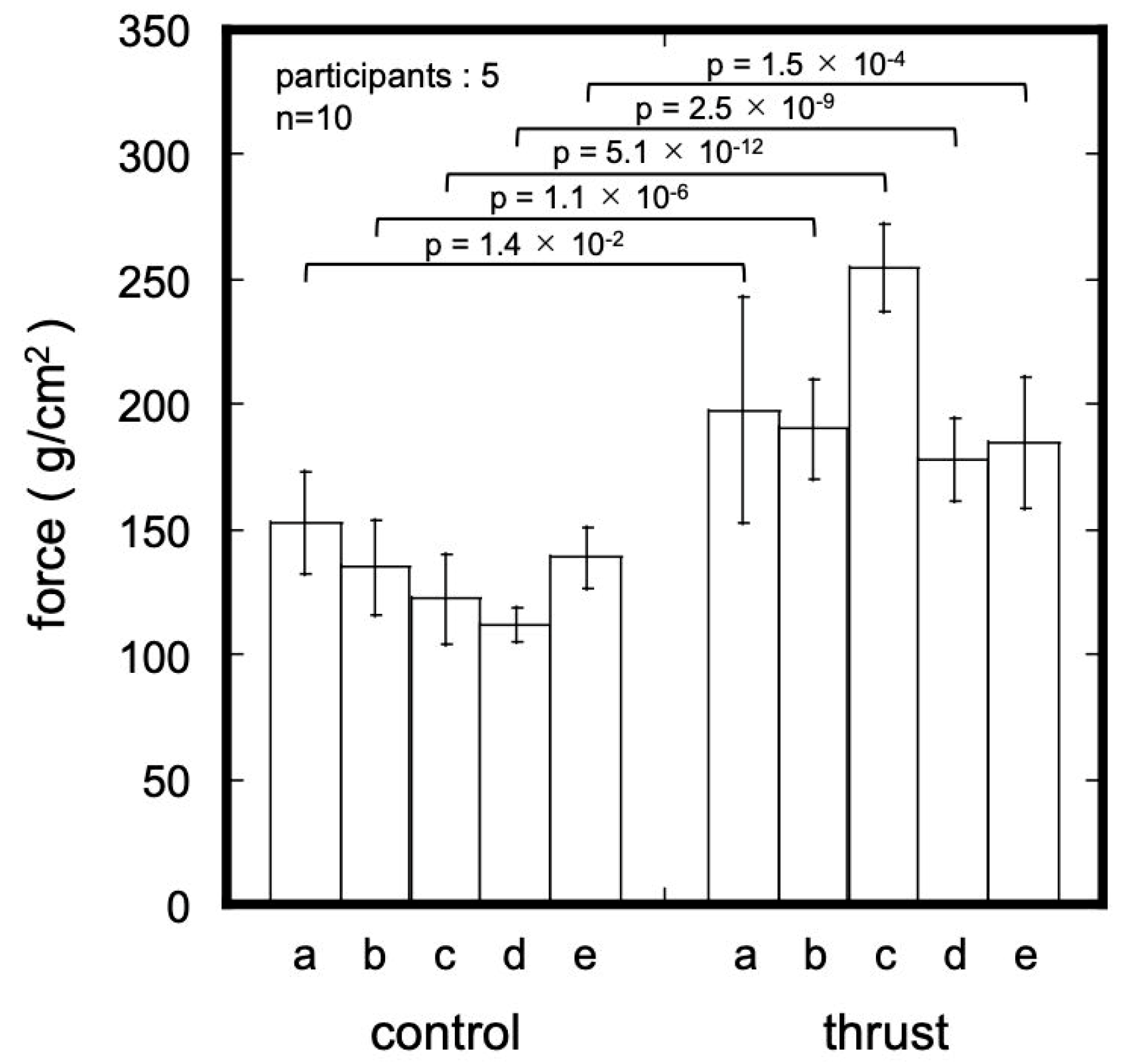
2.3.2. Tongue Pressure Measurement in the Mouth
3. Results and Discussion
3.1. Suitable Device Structure for Oral Soft Tissue Pressure Measurement
3.1.1. Effect of Diameter of Circular PMMA Plate
3.1.2. Effect of Material on the 2D Sheet-Type Sensor
3.1.3. Effect of Material on MG-Type Sensor
3.2. Wireless Measurement
3.3. Oral Soft Tissue Pressure Measurement
3.3.1. Comparison of Wired and Wireless Systems
3.3.2. Measurement of Tongue Pressure during Swallowing
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andreu-Perez, J.; Poon, C.C.Y.; Merrifield, R.D.; Wong, S.T.C.; Yang, G.Z. Big Data for Health. IEEE J. Biomed. Health Inform. 2015, 19, 1193–1208. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Dunn, J.; Salins, D.; Zhou, G.; Zhou, W.; Schüssler-Fiorenza Rose, S.M.; Perelman, D.; Colbert, E.; Runge, R.; Rego, S.; et al. Digital Health: Tracking Physiomes and Activity Using Wearable Biosensors Reveals Useful Health-Related Information. PLoS Biol. 2017, 15, e2001402. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Y.L.; Ding, X.R.; Poon, C.C.Y.; Lo, B.P.L.; Zhang, H.; Zhou, X.L.; Yang, G.Z.; Zhao, N.; Zhang, Y.T. Unobtrusive Sensing and Wearable Devices for Health Informatics. IEEE Trans. Biomed. Eng. 2014, 61, 1538–1554. [Google Scholar] [CrossRef] [PubMed]
- Bariya, M.; Nyein, H.Y.Y.; Javey, A. Wearable Sweat Sensors. Nat. Electron. 2018, 1, 160–171. [Google Scholar] [CrossRef]
- Liang, T.; Yuan, Y.J. Wearable Medical Monitoring Systems Based on Wireless Networks: A Review. IEEE Sens. J. 2016, 16, 8186–8199. [Google Scholar] [CrossRef]
- Arakawa, T.; Tomoto, K.; Nitta, H.; Toma, K.; Takeuchi, S.; Sekita, T.; Minakuchi, S.; Mitsubayashi, K. A Wearable Cellulose Acetate-Coated Mouthguard Biosensor for in Vivo Salivary Glucose Measurement. Anal. Chem. 2020, 92, 12201–12207. [Google Scholar] [CrossRef]
- Kim, J.; Kim, M.; Lee, M.S.; Kim, K.; Ji, S.; Kim, Y.T.; Park, J.; Na, K.; Bae, K.H.; Kim, H.K.; et al. Wearable Smart Sensor Systems Integrated on Soft Contact Lenses for Wireless Ocular Diagnostics. Nat. Commun. 2017, 8, 14997. [Google Scholar] [CrossRef]
- Weinstein, S.; Haack, D.; Morris, L. On an Equilibrium Theory of Tooth Position. Angle Orthod. 1963, 33, 1–26. [Google Scholar]
- Proffit, W.R. Equilibrium Theory Revisited: Factors Influencing Position of the Teeth. Angle Orthod. 1978, 48, 175–186. [Google Scholar]
- Proffit, W.R. Muscle Pressures and Tooth Position: North American Whites and Australian Aborigines. Angle Orthod. 1975, 45, 1–11. [Google Scholar] [CrossRef]
- Proffit, W.R.; Mc Glone, R.E.; Barrett, M.J. Lip and Tongue Pressures Related to Dental Arch and Oral Cavity Size in Australian Aborigines. J. Dent. Res. 1975, 54, 1161–1172. [Google Scholar] [CrossRef]
- Tulley, W.J. A Critical Appraisal of Tongue-Thrusting. Am. J. Orthod. 1969, 55, 640–650. [Google Scholar] [CrossRef]
- Jalaly, T.; Ahrari, F.; Amini, F. Effect of Tongue Thrust Swallowing on Position of Anterior Teeth. J. Dent. Res. Dent. Clin. Dent. Prospect. 2009, 3, 73–77. [Google Scholar] [CrossRef]
- Dixit, U.; Shetty, R. Comparison of Soft-Tissue, Dental, and Skeletal Characteristics in Children with and without Tongue Thrusting Habit. Contemp. Clin. Dent. 2013, 4, 2–6. [Google Scholar] [CrossRef]
- Hsu, B.S. The Nature of Arch Width Difference and Palatal Depth of the Anterior Open Bite. Am. J. Orthod. Dentofac. Orthop. 1998, 113, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Tarvade, S.M.; Ramkrishna, S. Tongue Thrusting Habit: A Review. Int. J. Contemp. Dent. Med. Rev. 2015, 2015, 1–5. [Google Scholar] [CrossRef]
- Di Fazio, D.; Lombardo, L.; Gracco, A.; D’Amico, P.; Siciliani, G. Lip Pressure at Rest and during Function in 2 Groups of Patients with Different Occlusions. Am. J. Orthod. Dentofac. Orthop. 2011, 139, e1. [Google Scholar] [CrossRef] [PubMed]
- Lapatki, B.G.; Mager, A.S.; Schulte-Moenting, J.; Jonas, I.É. The Importance of the Level of the Lip Line and Resting Lip Pressure in Class II, Division 2 Malocclusion. J. Dent. Res. 2002, 81, 323–328. [Google Scholar] [CrossRef]
- Takada, J.I.; Ono, T.; Miyamato, J.J.; Yokota, T.; Moriyama, K. Association between Intraoral Pressure and Molar Position and Inclination in Subjects with Facial Asymmetry. Eur. J. Orthod. 2011, 33, 243–249. [Google Scholar] [CrossRef] [PubMed]
- Ruan, W.; Su, J.; Ye, X. Pressure from the Lips and the Tongue in Children with Class III Malocclusion. J. Zhejiang Univ. Sci. B 2007, 8, 296–301. [Google Scholar] [CrossRef]
- Thüer, U.; Sieber, R.; Ingervall, B. Cheek and Tongue Pressures in the Molar Areas and the Atmospheric Pressure in the Palatal Vault in Young Adults. Eur. J. Orthod. 1999, 21, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Küçükkeleş, N.; Ceylanoǧlu, C. Changes in Lip, Cheek, and Tounge Pressures after Rapid: Maxillary Expansion Using a Diaphragm Pressure Transducer. Angle Orthod. 2003, 73, 662–668. [Google Scholar] [PubMed]
- Kydd, W.L.; Akamine, J.S.; Mendel, R.A.; Kraus, B.S. Tongue and Lip Forces Exerted during Deglutition in Subjects with and without an Anterior Open Bite. J. Dent. Res. 1963, 42, 858–866. [Google Scholar] [CrossRef]
- Lambrechts, H.; De Baets, E.; Fieuws, S.; Willems, G. Lip and Tongue Pressure in Orthodontic Patients. Eur. J. Orthod. 2010, 32, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Kato, Y. Intraoral Pressure Measurement with Telemetry System. Kokubyo Gakkai Zasshi. 1987, 54, 175–189. [Google Scholar] [CrossRef]
- Takahashi, S.; Ono, T.; Ishiwata, Y.; Kuroda, T. Effect of Changes in the Breathing Mode and Body Position on Tongue Pressure with Respiratory-Related Oscillations. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 239–246. [Google Scholar] [CrossRef]
- Hellsing, E.; L’Estrange, P. Changes in Lip Pressure Following Extension and Flexion of the Head and at Changed Mode of Breathing. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Tsuiki, S.; Handa, S.; Ohyama, K. A Simple Method for Evaluation of Tongue Position. J. Oral Rehabil. 2007, 34, 304–310. [Google Scholar] [CrossRef]
- Zeng, J.; Xu, K.; Gao, X.; Xu, T. Tongue Resting Pressure of the Tongue Anchorage Pad in Different Body Positions: A Pilot Study. J. Oral Rehabil. 2015, 42, 414–419. [Google Scholar] [CrossRef]
- Takahashi, S.; Ono, T.; Ishiwata, Y.; Kuroda, T. Breathing Modes, Body Positions and Suprahyoid Muscle Activity. J. Orthod. 2002, 29, 279. [Google Scholar] [CrossRef]
- Douglas, N.J.; White, D.P.; Pickett, C.K.; Weil, J.V.; Clifford, W. Respiration during Sleep. Thorax 1982, 37, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Qazi, H.S.; Kucukkeles, N.O. Buccal and Lingual Soft Tissue Pressures In Different Malocclusions. POJ 2016, 8, 7–16. [Google Scholar]
- Taslana, S.; Birenb, S.; Ceylanogluc, C. Tongue Pressure Changes before, during and after Crib Appliance Therapy. Angle Orthod. 2010, 80, 533–539. [Google Scholar] [CrossRef] [PubMed]
- Hori, K.; Ono, T.; Tamine, K.i.; Kondo, J.; Hamanaka, S.; Maeda, Y.; Dong, J.; Hatsuda, M. Newly Developed Sensor Sheet for Measuring Tongue Pressure during Swallowing. J. Prosthodont. Res. 2009, 53, 28–32. [Google Scholar] [CrossRef] [PubMed]
- Ichida, T.; Takiguchi, R.; Yamada, K. Relationship between the Lingual-Palatal Contact Duration Associated with Swallowing and Maxillofacial Morphology with the Use of Electropalatography. Am. J. Orthod. Dentofacial Orthop. 1999, 116, 146–151. [Google Scholar] [CrossRef]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Matsumoto, H.; Tomoto, K.; Kawase, G.; Iitani, K.; Toma, K.; Arakawa, T.; Mitsubayashi, K.; Moriyama, K. Real-Time Continuous Monitoring of Oral Soft Tissue Pressure with a Wireless Mouthguard Device for Assessing Tongue Thrusting Habits. Sensors 2023, 23, 5027. https://doi.org/10.3390/s23115027
Matsumoto H, Tomoto K, Kawase G, Iitani K, Toma K, Arakawa T, Mitsubayashi K, Moriyama K. Real-Time Continuous Monitoring of Oral Soft Tissue Pressure with a Wireless Mouthguard Device for Assessing Tongue Thrusting Habits. Sensors. 2023; 23(11):5027. https://doi.org/10.3390/s23115027
Chicago/Turabian StyleMatsumoto, Hidekazu, Keisuke Tomoto, Gentaro Kawase, Kenta Iitani, Koji Toma, Takahiro Arakawa, Kohji Mitsubayashi, and Keiji Moriyama. 2023. "Real-Time Continuous Monitoring of Oral Soft Tissue Pressure with a Wireless Mouthguard Device for Assessing Tongue Thrusting Habits" Sensors 23, no. 11: 5027. https://doi.org/10.3390/s23115027
APA StyleMatsumoto, H., Tomoto, K., Kawase, G., Iitani, K., Toma, K., Arakawa, T., Mitsubayashi, K., & Moriyama, K. (2023). Real-Time Continuous Monitoring of Oral Soft Tissue Pressure with a Wireless Mouthguard Device for Assessing Tongue Thrusting Habits. Sensors, 23(11), 5027. https://doi.org/10.3390/s23115027







