“Dispatcher, Can You Help Me? A Woman Is Giving Birth”. A Pilot Study of Remote Video Assistance with Smart Glasses
Abstract
1. Introduction
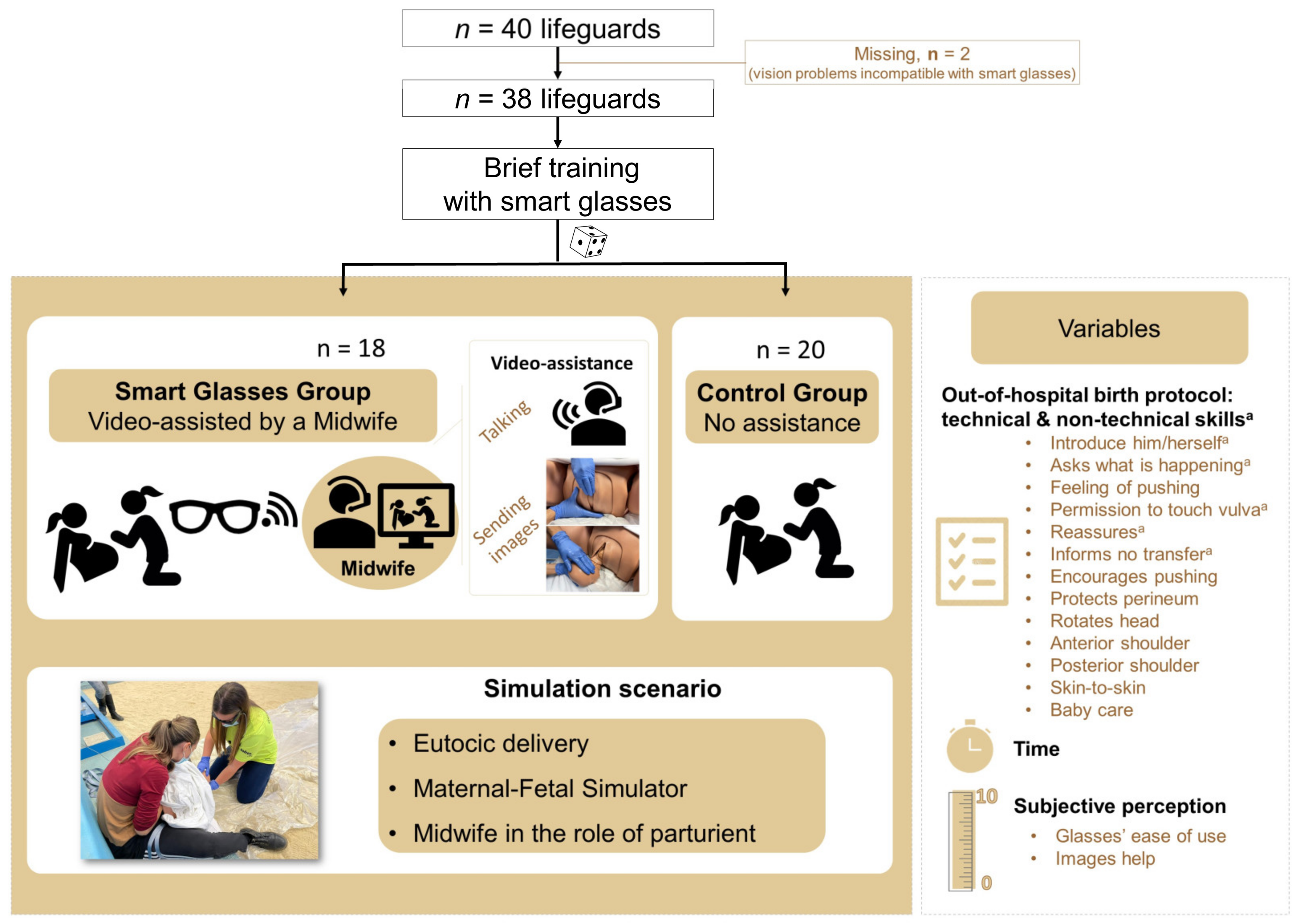
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Brief Training on Smart Glasses and Connection Details
2.4. Clinical Simulation and Variables
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Instituto Nacional de Estadística. Partos Según Residencia de la Madre por Comunidad Autónoma, Maturidad, Tamaño de los Municipios y Capital, Normalidad del Parto y Asistencia Sanitaria. 2022. Available online: https://www.ine.es/jaxi/Datos.htm?tpx=50549 (accessed on 13 January 2022).
- Örtqvist, A.K.; Haas, J.; Ahlberg, M.; Norman, M.; Stephansson, O. Association between travel time to delivery unit and unplanned out-of-hospital birth, infant morbidity and mortality: A population-based cohort study. Acta Obstet. Gynecol. Scand. 2021, 100, 1478–1489. [Google Scholar] [CrossRef]
- Diana, L.; Glaucia, L.; Adriana, C.; Israel, F.J. Out-of-hospital deliveries: A case-control study. Turk. Arch. Pediatr. 2018, 53, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Javaudin, F.; Hamel, V.; Legrand, A.; Goddet, S.; Templier, F.; Potiron, C.; Pes, P.; Bagou, G.; Montassier, E. Unplanned out-of-hospital birth and risk factors of adverse perinatal outcome: Findings from a prospective cohort. Scand. J. Trauma Resusc. Emerg. Med. 2019, 27, 26. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.-L.; Lefèvre, P.; Dreyfus, M. Maternal and neonatal outcomes of unplanned deliveries. J. Gynecol. Obstet. Biol. Reprod. 2016, 45, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Girsen, A.I.; Mayo, J.A.; Lyell, D.J.; Blumenfeld, Y.J.; Stevenson, D.K.; El-Sayed, Y.Y.; Shaw, G.M.; Druzin, M.L. Out-of-hospital births in California 1991–2011. J. Perinatol. 2017, 38, 41–45. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, B.; Lord, B.; Reed, R.; Crimmins, G. Women’s experience of unplanned out-of-hospital birth in paramedic care. BMC Emerg. Med. 2019, 19, 54. [Google Scholar] [CrossRef]
- Ovaskainen, K.; Ojala, R.; Tihtonen, K.; Gissler, M.; Luukkaala, T.; Tammela, O. Unplanned out-of-hospital deliveries in Finland: A national register study on incidence, characteristics and maternal and infant outcomes. Acta Obstet. Gynecol. Scand. 2020, 99, 1691–1699. [Google Scholar] [CrossRef]
- He, S.; Kosatsky, T.; Smargiassi, A.; Bilodeau-Bertrand, M.; Auger, N. Heat and pregnancy-related emergencies: Risk of placental abruption during hot weather. Environ. Int. 2018, 111, 295–300. [Google Scholar] [CrossRef]
- Fernández-Méndez, F.; Otero-Agra, M.; Abelairas-Gómez, C.; Sáez-Gallego, N.M.; Rodríguez-Núñez, A.; Barcala-Furelos, R. ABCDE approach to victims by lifeguards: How do they manage a critical patient? A cross sectional simulation study. PLoS ONE 2019, 14, e0212080. [Google Scholar] [CrossRef]
- Lin, Y.-Y.; Chiang, W.-C.; Hsieh, M.-J.; Sun, J.-T.; Chang, Y.-C.; Ma, M.H.-M. Quality of audio-assisted versus video-assisted dispatcher-instructed bystander cardiopulmonary resuscitation: A systematic review and meta-analysis. Resuscitation 2018, 123, 77–85. [Google Scholar] [CrossRef]
- Chen, K.Y.; Ko, Y.C.; Hsieh, M.J.; Chiang, W.C.; Ma, M.H. Interventions to improve the quality of bystander cardiopulmonary resuscitation: A systematic review. PLoS ONE 2019, 14, e0211792. [Google Scholar] [CrossRef] [PubMed]
- Sandall, J.; Soltani, H.; Gates, S.; Shennan, A.; Devane, D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst. Rev. 2013, CD004667. [Google Scholar] [CrossRef]
- Murray-Davis, B.; Grenier, L.N.; Mattison, C.A.; Malott, A.; Cameron, C.; Hutton, E.K.; Darling, E.K. Promoting safety and role clarity among health professionals on Canada’s First Alongside Midwifery Unit (AMU): A mixed-methods evaluation. Midwifery 2022, 111, 103366. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Lara, J.M.; Gómez-Salgado, J.; Fernández-Carrasco, F.J.; Río, P.B.-D.; Vázquez-Lara, M.D.; Rodríguez-Díaz, L. Imminent out-of-hospital birth assistance. Actions during this process and care for the mother and the newborn. Rev. Esp. Salud Publica 2018, 92, e201809063. [Google Scholar]
- Alonso, N.P.; Rios, M.P.; Rodriguez, L.J.; Catalan, T.V.; Melgarejo, F.S.; Ayuso, B.L.; Martínez-Riquelme, C.; Velasco, J.L. Randomised clinical simulation designed to evaluate the effect of telemedicine using Google Glass on cardiopulmonary resuscitation (CPR). Emerg. Med. J. 2017, 34, 734–738. [Google Scholar] [CrossRef]
- Lee, S.Y.; Song, K.J.; Shin, S.D.; Hong, K.J.; Kim, T.H. Comparison of the effects of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation on resuscitation outcomes after out-of-hospital cardiac arrest. Resuscitation 2020, 147, 12–20. [Google Scholar] [CrossRef]
- Mitrasinovic, S.; Camacho, E.; Trivedi, N.; Logan, J.; Campbell, C.; Zilinyi, R.; Lieber, B.; Bruce, E.; Taylor, B.; Martineau, D.; et al. Clinical and surgical applications of smart glasses. Technol. Health Care 2015, 23, 381–401. [Google Scholar] [CrossRef]
- Alonso, N.P.; Ríos, M.P.; Velasco, J.L.; Rodríguez, L.J.; Ayuso, B.L.; Solera, R.M. Randomized clinical simulation trial of a Google Glass telemedicine application to assist orotracheal intubation. Emerg. Rev. Soc. Esp. Med. Emerg. 2016, 28, 235–238. [Google Scholar]
- Currell, R.; Urquhart, C.; Wainwright, P.; Lewis, R. Telemedicine versus face to face patient care: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2000, CD002098. [Google Scholar] [CrossRef]
- Cicero, M.X.; Walsh, B.; Solad, Y.; Whitfill, T.; Paesano, G.; Kim, K.; Baum, C.R.; Cone, D.C. Do You See What I See? Insights from Using Google Glass for Disaster Telemedicine Triage. Prehospital Disaster Med. 2015, 30, 4–8. [Google Scholar] [CrossRef]
- Broach, J.; Hart, A.; Griswold, M.; Lai, J.; Boyer, E.W.; Skolnik, A.B.; Chai, P.R. Usability and Reliability of Smart Glasses for Secondary Triage During Mass Casualty Incidents. In Proceedings of the 51st Hawaii International Conference on System Sciences, HICSS 2018, Hilton Waikoloa Village, HI, USA, 3−6 January 2018; pp. 1416–1422. [Google Scholar] [CrossRef]
- Aranda-García, S.; Herrera-Pedroviejo, E.; Abelairas-Gómez, C. Basic Life-Support Learning in Undergraduate Students of Sports Sciences: Efficacy of 150 Minutes of Training and Retention after Eight Months. Int. J. Environ. Res. Public Health 2019, 16, 4771. [Google Scholar] [CrossRef] [PubMed]
- Kane-Gill, S.L.; Rincon, F. Expansion of Telemedicine Services: Telepharmacy, Telestroke, Teledialysis, Tele-Emergency Medicine. Crit. Care Clin. 2019, 35, 519–533. [Google Scholar] [CrossRef] [PubMed]
- Lapcharoensap, W.; Lund, K.; Huynh, T. Telemedicine in neonatal medicine and resuscitation. Curr. Opin. Pediatr. 2021, 33, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Andrews, V.; Thakar, R.; Sultan, A.H.; Jones, P.W. Evaluation of postpartum perineal pain and dyspareunia—A prospective study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2008, 137, 152–156. [Google Scholar] [CrossRef]
- Aasheim, V.; Nilsen, A.B.V.; Reinar, L.M.; Lukasse, M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst. Rev. 2017, 2018, CD006672. [Google Scholar] [CrossRef]
- McKinnie, V.; Swift, S.E.; Wang, W.; Woodman, P.; O’Boyle, A.; Kahn, M.; Valley, M.; Bland, D.; Schaffer, J. The effect of pregnancy and mode of delivery on the prevalence of urinary and fecal incontinence. Am. J. Obstet. Gynecol. 2005, 193, 512–517. [Google Scholar] [CrossRef]
- Mayerhofer, K.; Bodner-Adler, B.; Bodner, K.; Rabl, M.; Kaider, A.; Wagenbichler, P.; Joura, E.A.; Husslein, P. Traditional care of the perineum during birth. A prospective, randomized, multicenter study of 1076 women. J. Reprod. Med. 2002, 47, 477–482. [Google Scholar]
- Moore, B. Appropriate Technology for Birth. Lancet 1985, 326, 787–1388. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. Care in Second Stage of Labour. 2017. Available online: https://pathways.nice.org.uk/pathways/intrapartum-care#path=view%3A/pathways/intrapartum-care/care-in-second-stage-of-labour.xml&content=view-node%3Anodes-interventions-to-reduce-perineal-trauma (accessed on 13 January 2022).
- Laine, K.; Pirhonen, T.; Rolland, R.; Pirhonen, J. Decreasing the Incidence of Anal Sphincter Tears During Delivery. Obstet. Gynecol. 2008, 111, 1053–1057. [Google Scholar] [CrossRef]
- Scott, T.; Esen, U.I. Unplanned out of hospital births—Who delivers the babies? Ir. Med. J. 2005, 98, 70–72. [Google Scholar]
- World Health Organization, Maternal and Newborn Health/Safe Motherhood Unit. Thermal Protection of the Newborn: A Practical Guide [internet]; World Health Organization: Geneva, Switzerland, 1999; Available online: https://apps.who.int/iris/handle/10665/63986 (accessed on 13 January 2022).
- Srivastava, S.; Gupta, A.; Bhatnagar, A.; Dutta, S. Effect of very early skin to skin contact on success at breastfeeding and preventing early hypothermia in neonates. Indian J. Public Health 2014, 58, 22. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.R.; Bergman, N.; Anderson, G.C.; Medley, N. Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane Database Syst. Rev. 2016, 2016, CD003519. [Google Scholar] [CrossRef] [PubMed]
- Erlandsson, K.; Lustig, H.; Lindgren, H. Women’s experience of unplanned out-of-hospital birth in Sweden—A phenomenological description. Sex. Reprod. Healthc. 2015, 6, 226–229. [Google Scholar] [CrossRef]
- National Collaborating Centre for Women’s and Children’s Health. Summary of Recommendations and Care Pathway; National Collaborating Centre for Women’s and Children’s Health: London, UK, 2011. [Google Scholar]
- World Health Organization. Recomendaciones de la OMS Para Los Cuidados Durante El Parto, Para Una Experiencia De Parto Positiva. 2019. Available online: http://www.who.int/reproductivehealth/publications/intrapartum-care-guidelines/es/ (accessed on 13 January 2022).
- Aune, I.; Torvik, H.M.; Selboe, S.-T.; Skogås, A.-K.; Persen, J.; Dahlberg, U. Promoting a normal birth and a positive birth experience—Norwegian women’s perspectives. Midwifery 2015, 31, 721–727. [Google Scholar] [CrossRef] [PubMed]
- Elmir, R.; Schmied, V.; Wilkes, L.; Jackson, D. Women’s perceptions and experiences of a traumatic birth: A meta-ethnography. J. Adv. Nurs. 2010, 66, 2142–2153. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, B.; Haustein, D.; Landeweerd, L. Smart-Glasses: Exposing and Elucidating the Ethical Issues. Sci. Eng. Ethic. 2016, 23, 701–721. [Google Scholar] [CrossRef]
| Unplanned Out-of-Hospital Birth Sequence | Technical Skill | Non-Technical Skill | Skills Description |
|---|---|---|---|
| (1) Introduce him/herself | x | The lifeguard (L) introduces him/herself to the pregnant woman (P) | |
| (2) Asks what is happening | x | L asks what is happening and how the P is | |
| (3) Feeling of pushing | x | L asks the P if she has a feeling of pushing | |
| (4) Permission to touch vulva | x | L asks the P for permission to examine her vulva | |
| (5) Reassures | x | L reassures the P | |
| (6) Informs no transfer | x | L informs P that childbirth is imminent and she cannot be transferred to a health center | |
| (7) Encourages pushing | x | Expulsive phase (EP): L encourages the P woman to push | |
| (8) Protects perineum | x | EP: L protects the P’s perineum with his hands | |
| (9) Rotates head | x | EP: L enables the baby’s head to turn | |
| (10) Anterior shoulder | x | EP: L holds the baby to enable the baby’s anterior shoulder to come out | |
| (11) Posterior shoulder | x | EP: L holds the baby to enable the baby’s posterior shoulder to come out | |
| (12) Skin-to-skin | x | L places the baby skin-to-skin in contact with its mother | |
| (13) Baby care | x | L dries, wraps up, and warms the baby’s head and body |
| Variable | Description | Smart Glasses | Control | pb |
|---|---|---|---|---|
| n (%) | n (%) | |||
| (1) Introduce him/herself a | The lifeguard (L) introduces him/herself to the pregnant woman (P) | 15 (75) | 0 (0) | <0.001 |
| (2) Asks what is happening a | L asks what is happening and how the P is | 19 (95) | 2 (11) | <0.001 |
| (3) Feeling of pushing | L asks the P if she has a feeling of pushing | 19 (95) | 1 (6) | <0.001 |
| (4) Permission to touch vulva a | L asks the P for permission to examine her vulva | 18 (90) | 1 (6) | <0.001 |
| (5) Reassures a | L reassures the P | 18 (90) | 9 (50) | 0.007 |
| (6) Informs no transfer a | L informs P that childbirth is imminent and she cannot be transferred to a health center | 18 (90) | 0 (0) | <0.001 |
| (7) Encourages pushing | Expulsive phase (EP): L encourages the P woman to push | 19 (95) | 11 (61) | 0.011 |
| (8) Protects perineum | EP: L protects the P’s perineum with his hands | 18 (90) | 0 (0) | <0.001 |
| (9) Rotates head | EP: L enables the baby’s head to turn | 20 (100) | 8 (44) | <0.001 |
| (10) Anterior shoulder | EP: L holds the baby to enable the baby’s anterior shoulder to come out | 19 (95) | 12 (67) | 0.024 |
| (11) Posterior shoulder | EP: L holds the baby to enable the baby’s posterior shoulder to come out | 20 (100) | 11 (65) | 0.004 |
| (12) Skin-to-skin | L places the baby skin-to-skin in contact with its mother | 16 (80) | 0 (0) | <0.001 |
| (13) Baby care | L dries, wraps up, and warms the baby’s head and body | 19 (95) | 2 (11) | <0.001 |
| Complete sequence | 7 (35) | 0 (0) | 0.005 | |
| All technical skills | 12 (60) | 0 (0) | <0.001 | |
| All non-technical skills a | 11 (55) | 1 (6) | <0.001 |
| Smart Glasses | Control | p | |
|---|---|---|---|
| n (%) | n (%) | ||
| Self-reported level of competence | 6.8 ± 1.5 | 3.8 ± 1.8 | <0.001 |
| Self-reported level of confidence | 7.0 ± 1.4 | 3.3 ± 2.9 | <0.001 |
| Difficulty using smart glasses | 1.2 ± 2.0 | - | - |
| Images facilitate the help | 8.6 ± 2.1 | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aranda-García, S.; Santos-Folgar, M.; Fernández-Méndez, F.; Barcala-Furelos, R.; Pardo Ríos, M.; Hernández Sánchez, E.; Varela-Varela, L.; San Román-Mata, S.; Rodríguez-Núñez, A. “Dispatcher, Can You Help Me? A Woman Is Giving Birth”. A Pilot Study of Remote Video Assistance with Smart Glasses. Sensors 2023, 23, 409. https://doi.org/10.3390/s23010409
Aranda-García S, Santos-Folgar M, Fernández-Méndez F, Barcala-Furelos R, Pardo Ríos M, Hernández Sánchez E, Varela-Varela L, San Román-Mata S, Rodríguez-Núñez A. “Dispatcher, Can You Help Me? A Woman Is Giving Birth”. A Pilot Study of Remote Video Assistance with Smart Glasses. Sensors. 2023; 23(1):409. https://doi.org/10.3390/s23010409
Chicago/Turabian StyleAranda-García, Silvia, Myriam Santos-Folgar, Felipe Fernández-Méndez, Roberto Barcala-Furelos, Manuel Pardo Ríos, Encarna Hernández Sánchez, Lucía Varela-Varela, Silvia San Román-Mata, and Antonio Rodríguez-Núñez. 2023. "“Dispatcher, Can You Help Me? A Woman Is Giving Birth”. A Pilot Study of Remote Video Assistance with Smart Glasses" Sensors 23, no. 1: 409. https://doi.org/10.3390/s23010409
APA StyleAranda-García, S., Santos-Folgar, M., Fernández-Méndez, F., Barcala-Furelos, R., Pardo Ríos, M., Hernández Sánchez, E., Varela-Varela, L., San Román-Mata, S., & Rodríguez-Núñez, A. (2023). “Dispatcher, Can You Help Me? A Woman Is Giving Birth”. A Pilot Study of Remote Video Assistance with Smart Glasses. Sensors, 23(1), 409. https://doi.org/10.3390/s23010409







