Telehealth Secure Solution to Provide Childhood Obesity Monitoring
Abstract
:1. Introduction
2. Related Work
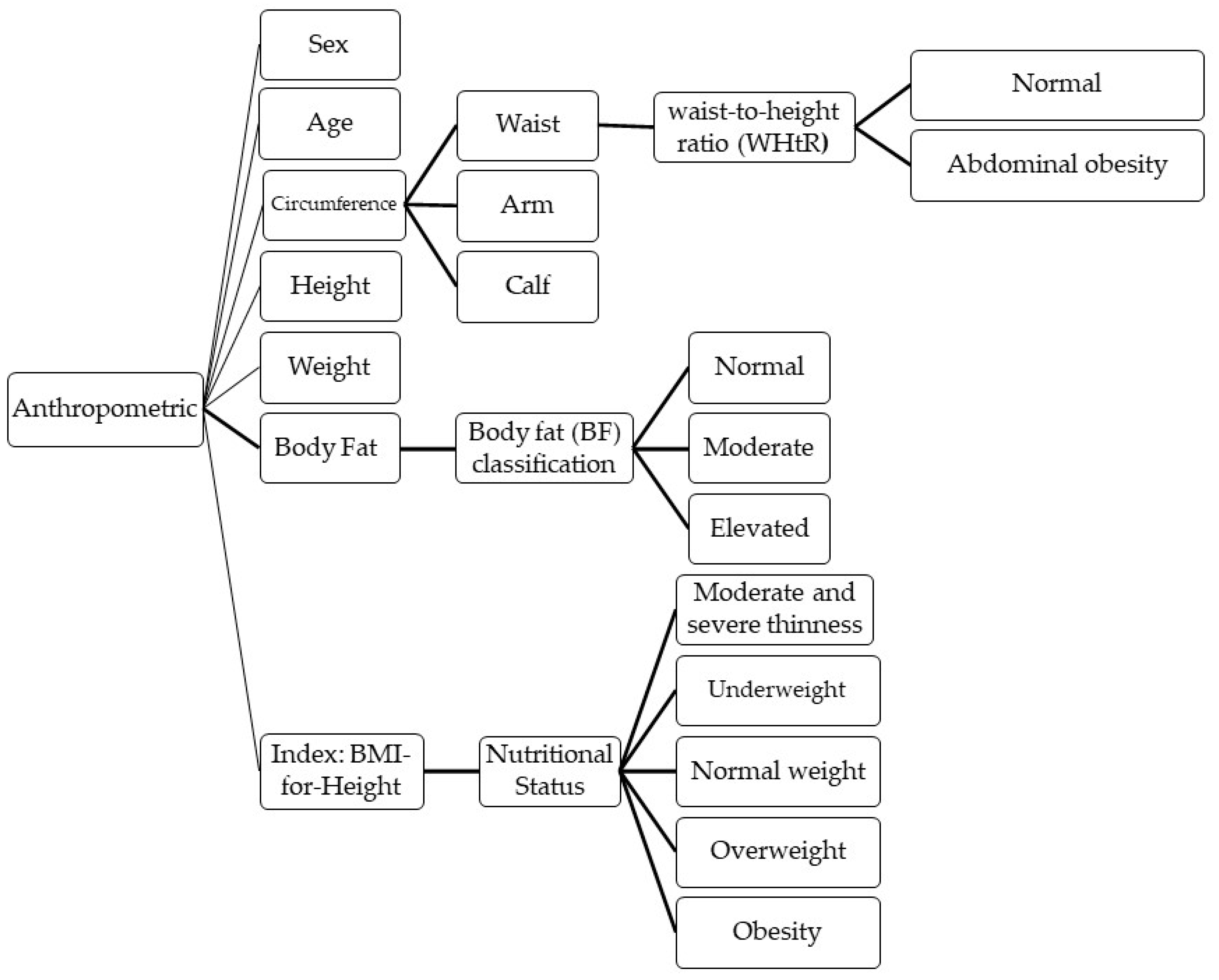
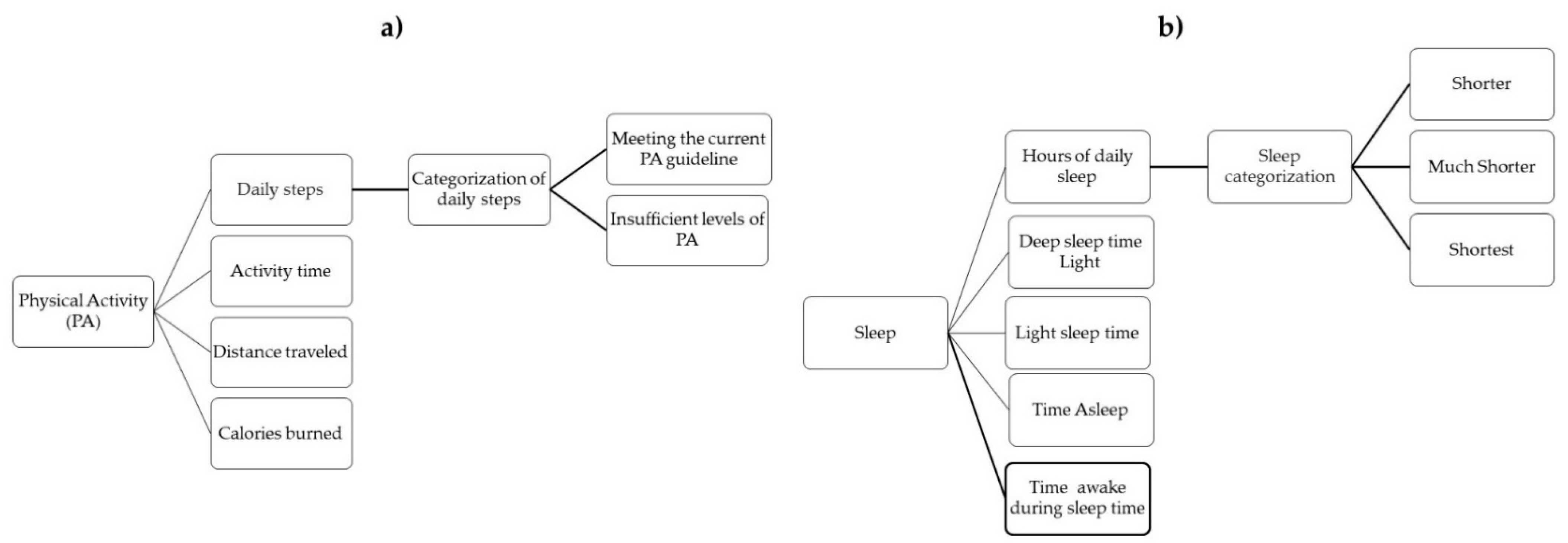
3. Family-Based Weight Management for Children
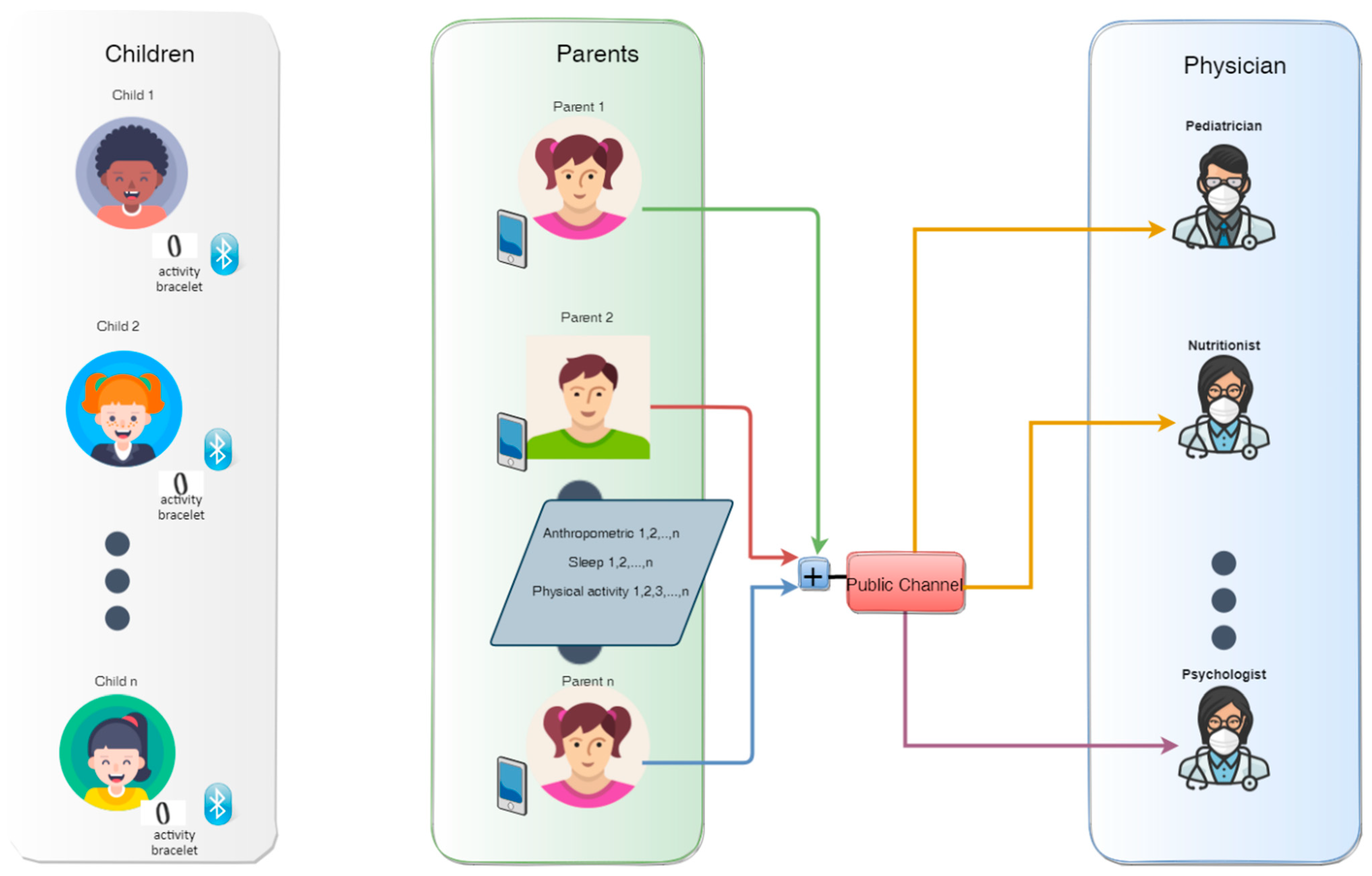
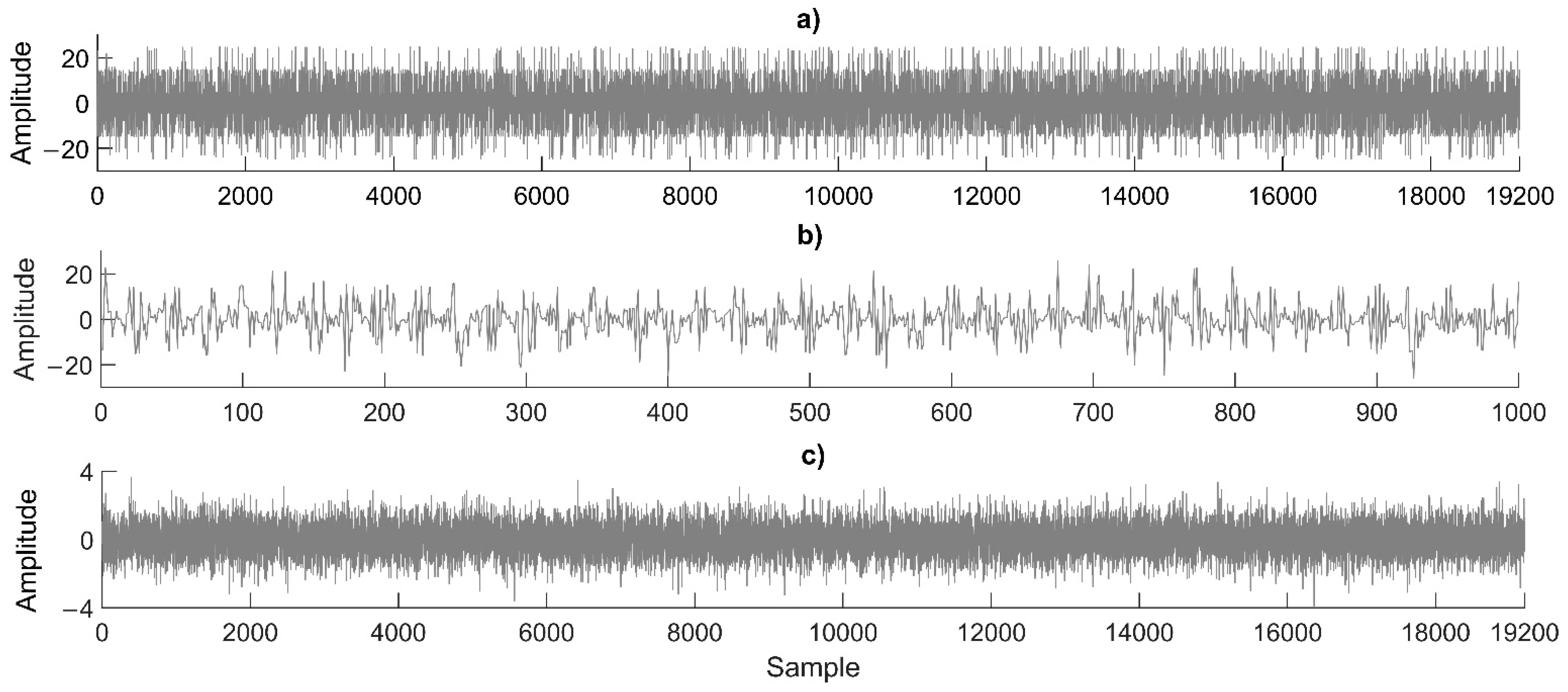
4. Proposed Multi-User Secure Monitoring Scheme
- The secret key is defined for each child-parent-specialist in a symmetric-key cryptography.
- The plain text is defined as a vector of 10 × 16-bit unsigned integer for N users. The binary plain text is coded to non-return zero (NRZ), i.e., 1 for “1” and −1 for “0”.
- The NRZ plain text of each user is modulated with binary phase shift key (BPSK) using a carried signal defined as cosine signal at 1 Hz, 1 amplitude, and 50 samples per cycle.
- The chaotic two-dimensional Hénon map is used for each user, which is defined as follows:where and are two control parameters, and and are two initial conditions, which are considered as the secret key of each user. Digital words of 64-bit floating-point are used for the Hénon map to generate 15 decimals. Chaotic data are amplified by 1,000 and the module 1 operation is used to increase chaotic uniformity. The chaotic data (CD) with values of (0,1) are coded to NRZ based on the following criteria:where CDNRZ is the chaotic data coded in NRZ.
- The plain text modulated with BPSK and the chaotic data coded in NZR are multiplied to produce the spread spectrum signal of each user. Finally, all spread spectrum signals of N users are summed to produce the cryptogram.
- The authorized specialist receives the cryptogram.
- With the corresponding secret key of the user N, the authorized specialist uses the same chaotic Hénon map and generates the CDNRZ as in encryption process.
- The same carried signal defined in the encryption process is generated.
- The cryptogram is multiplied with CDNRZ to generate the inverse spread spectrum signal.
- The sign function with a length of 50 samples is applied to the inverse spread spectrum to retrieve the plain text in binary format according to the following criteria:where PTB is the recover plain text in binary format.
- Finally, groups of 16-bit data are converted to decimal format to retrieve the original plain text of the N user.
5. Experimental Results
6. Security Analysis
6.1. Key Space Analysis
6.2. Key Sensitivity Analysis
6.3. Bit Error Rate
6.4. Encryption Time and Throughput
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- World Health Organization. Prioritizing Areas for Action in the Field of Population-Based Prevention of Childhood Obesity: A Set of Tools for Member States to Determine and Identify Priority Areas for Action; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- Anderson, P.M.; Butcher, K.F.; Schanzenbach, D.W. Understanding recent trends in childhood obesity in the United States. Econ. Hum. Biol. 2019, 34, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [Green Version]
- The Organisation for Economic Co-operation and Development. The Organisation for Economic Co-operation and Development. The Heavy Burden of Obesity: The Economics of Prevention. In The Organisation for Economic Co-Operation and Development (OECD) Health Polici Studies; OECD Publishing: Paris, France, 2019. [Google Scholar]
- Bhattacharjee, R.; Kim, J.; Kheirandish-Gozal, L.; Gozal, D. Obesity and Obstructive Sleep Apnea Syndrome in Children: A Tale of Inflammatory Cascades. Pediatr. Pulmonol. 2011, 46, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Trasande, L.; Elbel, B. The economic burden placed on healthcare systems by childhood obesity. Expert Rev. Pharmacoecon. Outcomes Res. 2012, 12, 39–45. [Google Scholar] [CrossRef]
- Taheri, S. The link between short sleep duration and obesity. Arch. Dis. Child. 2006, 91, 881–884. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Consideration of the Evidence on Childhood Obesity for the Commission on Ending Childhood Obesity: Report of the Ad Hoc Working Group on Science and Evidence for Ending Childhood Obesity, Geneva, Switzerland; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Karnik, S.; Kanekar, A. Childhood obesity: A global public health crisis. Int. J. Prev. Med. 2012, 3, 1–7. [Google Scholar]
- Popkin, B.M.; Du, S.; Grenn, W.D.; Beck, M.A.; Algaith, T.; Herbst, C.H.; Alsukait, R.F.; Alluhidan, M.; Alazemi, N.; Shekar, M. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 2020, 21, 1–17. [Google Scholar] [CrossRef]
- Nogueira-de-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.; Contini, A.A.; Ued, F.D.V. COVID-19 and obesity in childhood and adolescence: A clinical review. J. Pediatr. 2020, 96, 546–558. [Google Scholar] [CrossRef]
- Dietz, W.; Santos-Burgoa, C. Obesity and its Implications for COVID-19 Mortality. Obesity 2020, 28, 1005. [Google Scholar] [CrossRef] [Green Version]
- Giorgino, F.; Bhana, S.; Czupryniak, L.; Dagdelen, S.; Galstyan, G.R.; Janež, A.; Lalić, N.; Nouri, N.; Rahelić, D.; Stoian, A.P.; et al. Management of patients with diabetes and obesity in the COVID-19 era: Experiences and learnings from South and East Europe, the Middle East, and Africa. Diabetes Res. Clin. Pract. 2021, 172, 1–10. [Google Scholar] [CrossRef]
- World Health Organization. Report of the Commission on Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2021, 2, 1–12. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Vandoni, M.; Rossi, V.; Di Profio, E.; Carnevale Pellino, V.; Tranfaglia, V.; Pascuzzi, M.C.; Borsani, B.; Bosetti, A.; et al. Telehealth: A Useful Tool for the Management of Nutrition and Exercise Programs in Pediatric Obesity in the COVID-19 Era. Nutrients 2021, 13, 3689. [Google Scholar] [CrossRef]
- de Oliveira Andrade, A.; Soares, A.B.; de Andrade Palis, A.; Cabral, A.M.; Barreto, C.G.L.; de Souza, D.B.; de Paula Silva, F.; Santos, F.P.; Silva, G.L.; Guimarães, J.F.V.; et al. On the use of telemedicine in the context of COVID-19: Legal aspects and a systematic review of technology. Res. Biomed. Eng. 2021, 2–29. [Google Scholar] [CrossRef]
- Arguello, F.; Bugallo, M.; Amor, M. Multi-user receivers for spread spectrum communications based on chaotic sequences. Int. J. Bifurcat. Chaos 2002, 12, 847–853. [Google Scholar] [CrossRef]
- Aledhari, M.; Marhoon, A.; Hamad, A.; Saeed, F. A new cryptography algorithm to protect cloud-based healthcare services. In Proceedings of the IEEE/ACM International Conference on Connected Health: Applications, Systems and Engineering Technologies, Philadelphia, PA, USA, 17–19 July 2017. [Google Scholar]
- Murillo-Escobar, M.A.; Cardoza-Avendaño, L.; López-Gutiérrez, R.M.; Cruz-Hernández, C. A double chaotic layer encryption algorithm for clinical signals in telemedicine. J. Med. Syst. 2017, 41, 1–17. [Google Scholar] [CrossRef]
- Rammyaa, B.; Vishvaksenan, K.S.; Poobal, S. Performance of spectrum sharing cognitive radio network based on MIMO MC-CDMA system for medical image transmission. Cluster Comput. 2019, 22, 7705–7712. [Google Scholar] [CrossRef]
- Michel-Macarty, J.A.; Murillo-Escobar, M.A.; López-Gutiérrez, R.M.; Cruz-Hernández, C.; Cardoza-Avendaño, L. Multiuser communication scheme based on binary phase-shift keying and chaos for telemedicine. Comput. Methods Programs Biomed. 2018, 162, 165–175. [Google Scholar] [CrossRef]
- Ebbeling, C.B.; Pawlak, D.B.; Ludwig, D.S. Childhood obesity: Public-health crisis, common sense cure. Lancet 2002, 360, 473–482. [Google Scholar] [CrossRef]
- Schröder, H.; Ribas, L.; Koebnick, C.; Funtikova, A.; Gómez, S.F.; Fito, M.; Perez-Rodrigo, C.; Serra-Majem, L. Prevalence of Abdominal Obesity in Spanish Children and Adolescents. Do We Need Waist Circumference Measurements in Pediatric Practice? PLoS ONE 2014, 9, e87549. [Google Scholar] [CrossRef] [PubMed]
- Browning, L.M.; Hsieh, S.D.; Ashwell, M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0.5 could be a suitable global boundary value. Nutr. Res. Rev. 2010, 23, 247–269. [Google Scholar] [CrossRef] [Green Version]
- Valle-Leal, J.; Abundis-Castro, L.; Hernández-Escareño, J.; Flores-Rubio, S. Índice Cintura-Estatura Como Indicador De Riesgo Metabólico En Niños. Rev. Chil. Pediatr. 2016, 8, 180–185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reed, G.M.; McLaughlin, C.J.; Milholland, K. Ten interdisciplinary principles for professional practice in telehealth: Implications for psychology. Prof. Psychol. Res. Pract. 2000, 31, 170–178. [Google Scholar] [CrossRef]
- Frija-Masson, J.; Mullaert, J.; Vidal-Petiot, E.; Pons-Kerjean, N.; Flamant, M.; d’Ortho, M.P. Accuracy of Smart Scales on Weight and Body Composition: Observational Study. JMIR mHealth uHealth 2021, 9, e22487. [Google Scholar] [CrossRef]
- Freedman, D.S.; Wang, J.; Thornton, J.C.; Mei, Z.; Sopher, A.B.; Pierson, R.N.; Dietz, W.H.; Horlick, M. Classification of body fatness by body mass index-for-age categories among children. Arch. Pediatr. Adolesc. Med. 2009, 163, 805–811. [Google Scholar] [CrossRef] [Green Version]
- Lobstein, T.; Baur, L.; Uauy, R. Obesity in children and young people: A crisis in public health. Obes. Rev. Suppl. 2004, 5, 4–104. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Da Silva, M.P.; Fontana, F.E.; Callahan, E.; Mazzardo, O.; De Campos, W. Step-count guidelines for children and adolescents: A systematic review. J. Phys. Act. Health 2015, 12, 1184–1191. [Google Scholar] [CrossRef] [PubMed]
- Morrissey, B.; Taveras, E.; Allender, S.; Strugnell, C. Sleep and obesity among children: A systematic review of multiple sleep dimensions. Pediatr. Obes. 2020, 15, e12619. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cao, M.; Zhu, Y.; Sun, F.; Luo, J.; Jing, J. Short sleep duration is associated with specific food intake increase among school-aged children in China: A national cross-sectional study. BMC Public Health 2019, 19, 558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, X.; Beydoun, M.A.; Wang, Y. Is sleep duration associated with childhood obesity? A systematic review and meta-analysis. Obesity 2008, 16, 265–274. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.A.; Kruisbrink, M.; Wallace, J.; Ji, C.; Cappuccio, F.P. Sleep duration and incidence of obesity in infants, children, and adolescents: A systematic review and meta-analysis of prospective studies. Sleep 2018, 41, zsy018. [Google Scholar] [CrossRef] [PubMed]
- The MathWorks, Inc. MATLAB R2015a; The MathWorks, Inc.: Natick, MA, USA, 2015. [Google Scholar]
- Kaggle. Kaggle Datasets. Available online: https://www.kaggle.com/datasets (accessed on 17 September 2021).
- IEEE Std 754-2019; IEEE Standard for Floating-Point Arithmetic. (Revision of IEEE 754–2008). Institute of Electrical and Electronics Engineers (IEEE): Piscataway, NJ, USA, 2019; pp. 1–84.
| Age Group (years) | Recommended Sleep (hours) |
|---|---|
| <5 | >11 |
| 5–10 | >10 |
| >10 | >9 |
| User 1 | User 2 | User 3 | User 4 | User 5 | |
|---|---|---|---|---|---|
| Weekly steps (mean) | 12,891 | 10,616 | 12,221 | 10,829 | 14,504 |
| Weekly activity (mean min) | 160 | 134 | 154 | 144 | 184 |
| Weekly distance (km) | 47 | 30 | 38 | 31 | 44 |
| Calories burned (cal) | 1208 | 700 | 1039 | 745 | 1023 |
| Sleep (mean min) | 533 | 480 | 562 | 511 | 546 |
| Deep sleep (mean min) | 136 | 217 | 220 | 149 | 146 |
| Light sleep (mean min) | 396 | 262 | 342 | 181 | 400 |
| Fell asleep at | 675 | 326 | 630 | 657 | 651 |
| Woke up at | 488 | 447 | 472 | 465 | 481 |
| Awake time (mean min) | 0 | 0 | 0 | 16 | 2 |
| User 1 | 1.400112233445566 | 0.300112233445566 | 0.556677889900112 | 0.667788990011223 |
| User 2 | 1.400223344556677 | 0.300223344556677 | 0.667788990011223 | 0.778899001122334 |
| User 3 | 1.400334455667788 | 0.300223344556677 | 0.778899001122334 | 0.889900112233445 |
| User 4 | 1.400445566778899 | 0.300334455667788 | 0.889900112233445 | 0.990011223344556 |
| User 5 | 1.400556677889900 | 0.300445566778899 | 0.990011223344556 | 0.001122334455667 |
| User 1 | 1.400112233445566 | 0.300112233445566 | 0.556677889900118 | 0.667788990011223 |
| User 2 | 1.400223344556677 | 0.300223344556677 | 0.667788990011223 | 0.778899001122334 |
| User 3 | 1.400334455667788 | 0.300223344556677 | 0.778899001122334 | 0.889900112233445 |
| User 4 | 1.400445566778899 | 0.300334455667788 | 0.889900112233445 | 0.990011223344557 |
| User 5 | 1.400556677889900 | 0.300445566778899 | 0.990011223344556 | 0.001122334455667 |
| User 1 | User 2 | User 3 | User 4 | User 5 | |
|---|---|---|---|---|---|
| Weekly steps (mean) | 4801 | 10,616 | 12,221 | 5416 | 14,504 |
| Weekly activity (mean min) | 11,734 | 134 | 154 | 44,277 | 184 |
| Distance week (km) | 818 | 30 | 38 | 33,968 | 44 |
| Calories burned (cal) | 32,953 | 700 | 1039 | 482 | 1023 |
| Sleep (mean min) | 56,196 | 480 | 562 | 19,737 | 546 |
| Deep sleep (mean min) | 36,955 | 217 | 220 | 61,087 | 146 |
| Light sleep (mean min) | 44,513 | 262 | 342 | 15,880 | 400 |
| Fell asleep at | 6900 | 326 | 630 | 56,226 | 651 |
| Woke up at | 22,135 | 447 | 472 | 12,731 | 481 |
| Awake time (mean min) | 23,445 | 0 | 0 | 58,027 | 2 |
| SNR (dB) | 0.001 | 0.01 | 0.1 | 1 | 3 | 0 |
|---|---|---|---|---|---|---|
| User 1 BER (%) | 45.05 | 53.12 | 47.91 | 48.95 | 48.95 | 48.69 |
| User 2 BER (%) | 0.89 | 0.59 | 0. 59 | 0.59 | 0 | 0 |
| User 3 BER (%) | 0.89 | 0.29 | 0.19 | 0.29 | 0.29 | 0 |
| User 4 BER (%) | 50.52 | 48.17 | 50.00 | 51.56 | 49.47 | 50.78 |
| User 5 BER (%) | 0.59 | 0.52 | 0.59 | 0.27 | 0.26 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiménez-García, E.; Murillo-Escobar, M.Á.; Fontecha-Diezma, J.; López-Gutiérrez, R.M.; Cardoza-Avendaño, L. Telehealth Secure Solution to Provide Childhood Obesity Monitoring. Sensors 2022, 22, 1213. https://doi.org/10.3390/s22031213
Jiménez-García E, Murillo-Escobar MÁ, Fontecha-Diezma J, López-Gutiérrez RM, Cardoza-Avendaño L. Telehealth Secure Solution to Provide Childhood Obesity Monitoring. Sensors. 2022; 22(3):1213. https://doi.org/10.3390/s22031213
Chicago/Turabian StyleJiménez-García, Elitania, Miguel Ángel Murillo-Escobar, Jesús Fontecha-Diezma, Rosa Martha López-Gutiérrez, and Liliana Cardoza-Avendaño. 2022. "Telehealth Secure Solution to Provide Childhood Obesity Monitoring" Sensors 22, no. 3: 1213. https://doi.org/10.3390/s22031213
APA StyleJiménez-García, E., Murillo-Escobar, M. Á., Fontecha-Diezma, J., López-Gutiérrez, R. M., & Cardoza-Avendaño, L. (2022). Telehealth Secure Solution to Provide Childhood Obesity Monitoring. Sensors, 22(3), 1213. https://doi.org/10.3390/s22031213







