Using Wearable Sensors to Measure Goal Achievement in Older Veterans with Dementia
Abstract
1. Introduction
2. Materials and Methods
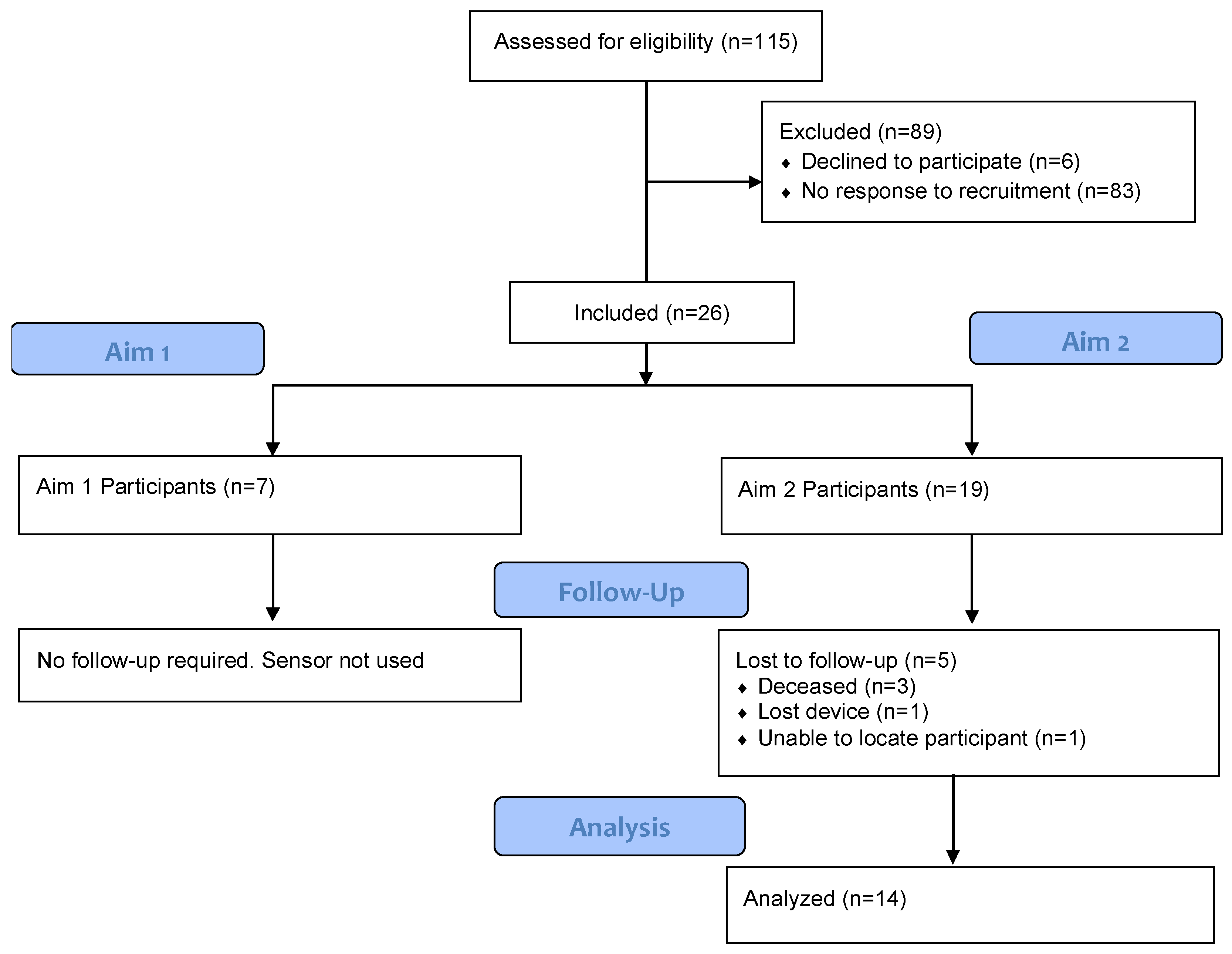
2.1. Study Population
2.2. Procedure
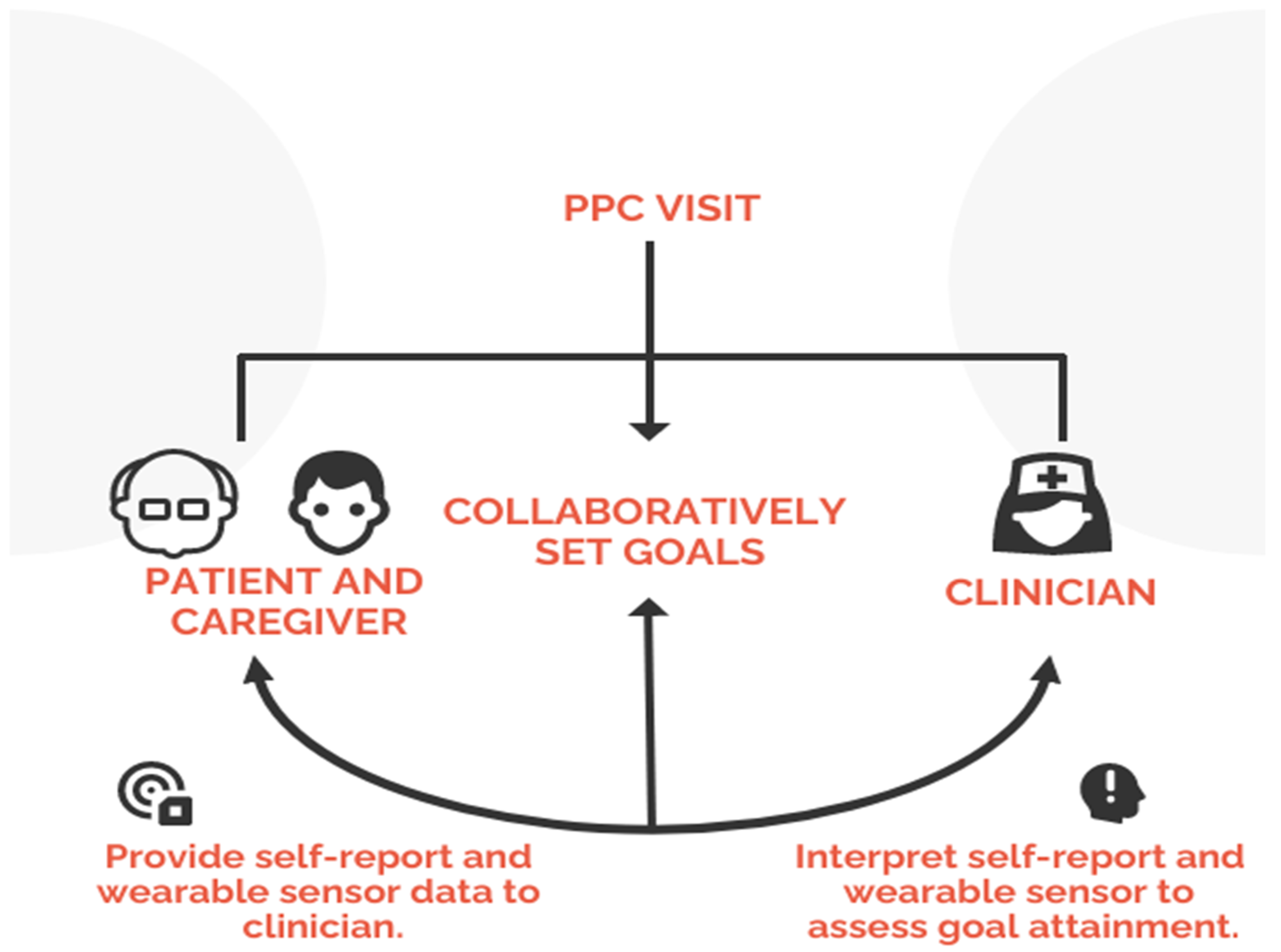
2.3. Patient Priorities Care
2.4. Wearables
2.5. Measures
2.5.1. Assessment of Dementia and Functionality
2.5.2. Survey Measures
2.5.3. Sensor-Derived Measures
2.5.4. Case Studies Describing the Utility of Wearable Devices
3. Results
3.1. Feasibility of Using Sensors
3.2. Differences in Function at Baseline and Follow-Up
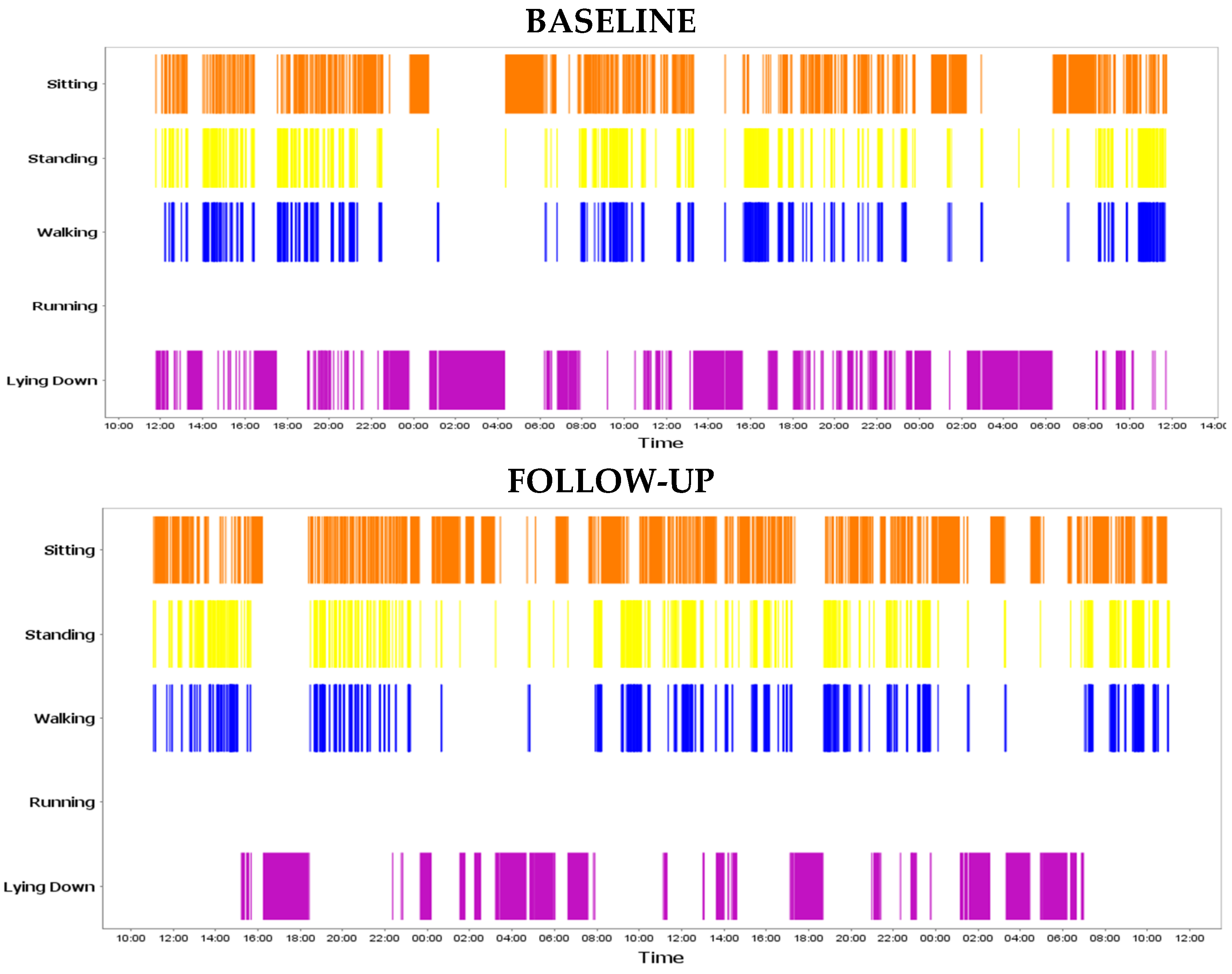
3.3. Four Case Studies Illustrating the Usefulness of Sensor Data
3.3.1. Case 1: Patient Achieved Movement Goal
3.3.2. Case 2: Patient Improved Overall
3.3.3. Case 3: Potential Barriers to Meeting Goals
3.3.4. Case 4: Sensor Shows Significant Decline
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adams, T.; Gardiner, P. Communication and interaction within dementia care triads: Developing a theory for relationship-centred care. Dementia 2005, 4, 185–205. [Google Scholar] [CrossRef]
- Lee, M.; Mishra, R.K.; Momin, A.; El-Refaei, N.; Bagheri, A.B.; York, M.K.; Kunik, M.E.; Derhammer, M.; Fatehi, B.; Lim, J. Smart-Home Concept for Remote Monitoring of Instrumental Activities of Daily Living (IADL) in Older Adults with Cognitive Impairment: A Proof of Concept and Feasibility Study. Sensors 2022, 22, 6745. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R.K.; Park, C.; Momin, A.S.; El Rafaei, N.; Kunik, M.; York, M.K.; Najafi, B. Care4AD: A Technology-Driven Platform for Care Coordination and Management: Acceptability Study in Dementia. Gerontology 2022, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Blaum, C.S.; Rosen, J.; Naik, A.D.; Smith, C.D.; Dindo, L.; Vo, L.; Hernandez-Bigos, K.; Esterson, J.; Geda, M.; Ferris, R. Feasibility of implementing patient priorities care for older adults with multiple chronic conditions. J. Am. Geriatr. Soc. 2018, 66, 2009–2016. [Google Scholar] [CrossRef]
- Freytag, J.; Dindo, L.; Catic, A.; Johnson, A.L.; Bush Amspoker, A.; Gravier, A.; Dawson, D.B.; Tinetti, M.E.; Naik, A.D. Feasibility of clinicians aligning health care with patient priorities in geriatrics ambulatory care. J. Am. Geriatr. Soc. 2020, 68, 2112–2116. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Naik, A.D.; Dindo, L.; Costello, D.M.; Esterson, J.; Geda, M.; Rosen, J.; Hernandez-Bigos, K.; Smith, C.D.; Ouellet, G.M. Association of patient priorities–aligned decision-making with patient outcomes and ambulatory health care burden among older adults with multiple chronic conditions: A nonrandomized clinical trial. JAMA Intern. Med. 2019, 179, 1688–1697. [Google Scholar] [CrossRef]
- Mishra, R.; Park, C.; York, M.K.; Kunik, M.E.; Wung, S.-F.; Naik, A.D.; Najafi, B. Decrease in mobility during the COVID-19 pandemic and its association with increase in depression among older adults: A longitudinal remote mobility monitoring using a wearable sensor. Sensors 2021, 21, 3090. [Google Scholar] [CrossRef]
- Najafi, B.; Mishra, R. Harnessing Digital Health Technologies to Remotely Manage Diabetic Foot Syndrome: A Narrative Review. Medicina 2021, 57, 377. [Google Scholar] [CrossRef]
- Park, C.; Mishra, R.; Sharafkhaneh, A.; Bryant, M.S.; Nguyen, C.; Torres, I.; Naik, A.D.; Najafi, B. Digital biomarker representing frailty phenotypes: The use of machine learning and sensor-based sit-to-stand test. Sensors 2021, 21, 3258. [Google Scholar] [CrossRef]
- Park, C.; Mishra, R.; Golledge, J.; Najafi, B. Digital Biomarkers of Physical Frailty and Frailty Phenotypes Using Sensor-Based Physical Activity and Machine Learning. Sensors 2021, 21, 5289. [Google Scholar] [CrossRef]
- Kinker Mishra, R.; Park, C.; Zhou, H.; Najafi, B.; Thrasher, T.A. Evaluation of Motor and Cognitive Performance in People with Parkinson’s Disease Using Instrumented Trail-Making Test. Gerontology 2022, 68, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Mishra, R.K.; Bara, R.O.; Zulbaran-Rojas, A.; Park, C.; Fernando, M.E.; Ross, J.; Lepow, B.; Najafi, B. The Application of Digital Frailty Screening to Triage Nonhealing and Complex Wounds. J. Diabetes Sci. Technol. 2022, 19322968221111194. [Google Scholar] [CrossRef]
- Park, C.; Mishra, R.; Vigano, D.; Macagno, M.; Rossotti, S.; D’Huyvetter, K.; Garcia, J.; Armstrong, D.G.; Najafi, B. Smart offloading boot system for remote patient monitoring: Toward adherence reinforcement and proper physical activity prescription for diabetic foot ulcer patients. J. Diabetes Sci. Technol. 2022, 19322968211070850. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Atique, M.M.U.; Mishra, R.; Najafi, B. Association between fall history and gait, balance, physical activity, depression, fear of falling, and motor capacity: A 6-month follow-up study. Int. J. Environ. Res. Public Health 2022, 19, 10785. [Google Scholar] [CrossRef] [PubMed]
- Vaiyapuri, T.; Lydia, E.L.; Sikkandar, M.Y.; Diaz, V.G.; Pustokhina, I.V.; Pustokhin, D.A. Internet of Things and Deep Learning Enabled Elderly Fall Detection Model for Smart Homecare. IEEE Access 2021, 9, 113879–113888. [Google Scholar] [CrossRef]
- Krichen, M. Anomalies Detection Through Smartphone Sensors: A Review. IEEE Sens. J. 2021, 21, 7207–7217. [Google Scholar] [CrossRef]
- Muangprathub, J.; Sriwichian, A.; Wanichsombat, A.; Kajornkasirat, S.; Nillaor, P.; Boonjing, V. A Novel Elderly Tracking System Using Machine Learning to Classify Signals from Mobile and Wearable Sensors. Int. J. Environ. Res. Public Health 2021, 18, 12652. [Google Scholar] [CrossRef]
- Qaisar, S.; Mihoub, A.; Krichen, M.; Nisar, H. Multirate Processing with Selective Subbands and Machine Learning for Efficient Arrhythmia Classification. Sensors 2021, 21, 1511. [Google Scholar] [CrossRef]
- Qaisar, S.M.; Khan, S.I.; Dallet, D.; Tadeusiewicz, R.; Pławiak, P. Signal-piloted processing metaheuristic optimization and wavelet decomposition based elucidation of arrhythmia for mobile healthcare. Biocybern. Biomed. Eng. 2022, 42, 681–694. [Google Scholar] [CrossRef]
- Takahashi, S.; Nakazawa, E.; Ichinohe, S.; Akabayashi, A.; Akabayashi, A. Wearable Technology for Monitoring Respiratory Rate and SpO2 of COVID-19 Patients: A Systematic Review. Diagnostics 2022, 12, 2563. [Google Scholar] [CrossRef]
- Javed, A.R.; Fahad, L.G.; Farhan, A.A.; Abbas, S.; Srivastava, G.; Parizi, R.M.; Khan, M.S. Automated cognitive health assessment in smart homes using machine learning. Sustain. Cities Soc. 2021, 65, 102572. [Google Scholar] [CrossRef]
- Javed, A.R.; Sarwar, M.U.; ur Rehman, S.; Khan, H.U.; Al-Otaibi, Y.D.; Alnumay, W.S. PP-SPA: Privacy Preserved Smartphone-Based Personal Assistant to Improve Routine Life Functioning of Cognitive Impaired Individuals. Neural Process. Lett. 2021. [Google Scholar] [CrossRef]
- Razjouyan, J.; Najafi, B.; Horstman, M.; Sharafkhaneh, A.; Amirmazaheri, M.; Zhou, H.; Kunik, M.E.; Naik, A. Toward using wearables to remotely monitor cognitive frailty in community-living older adults: An observational study. Sensors 2020, 20, 2218. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Naik, A.D.; Dodson, J.A. Moving from disease-centered to patient goals–directed care for patients with multiple chronic conditions: Patient value-based care. JAMA Cardiol. 2016, 1, 9–10. [Google Scholar] [CrossRef] [PubMed]
- Naik, A.D.; Dindo, L.N.; Van Liew, J.R.; Hundt, N.E.; Vo, L.; Hernandez-Bigos, K.; Esterson, J.; Geda, M.; Rosen, J.; Blaum, C.S. Development of a clinically feasible process for identifying individual health priorities. J. Am. Geriatr. Soc. 2018, 66, 1872–1879. [Google Scholar] [CrossRef]
- Najafi, B.; Aminian, K.; Loew, F.; Blanc, Y.; Robert, P.A. Measurement of stand-sit and sit-stand transitions using a miniature gyroscope and its application in fall risk evaluation in the elderly. IEEE Trans. Biomed. Eng. 2002, 49, 843–851. [Google Scholar] [CrossRef]
- Najafi, B.; Aminian, K.; Paraschiv-Ionescu, A.; Loew, F.; Bula, C.J.; Robert, P. Ambulatory system for human motion analysis using a kinematic sensor: Monitoring of daily physical activity in the elderly. IEEE Trans. Biomed. Eng. 2003, 50, 711–723. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef]
- Mitchell, A.J. The Mini-Mental State Examination (MMSE): An update on its diagnostic validity for cognitive disorders. In Cognitive Screening Instruments; Springer: Berlin/Heidelberg, Germany, 2013; pp. 15–46. [Google Scholar]
- Wallace, M.; Shelkey, M. Katz index of independence in activities of daily living (ADL). Urol Nurs 2007, 27, 93–94. [Google Scholar]
- Group, W. The development of the World Health Organization quality of life assessment instrument (the WHOQOL). In Quality of Life Assessment: International Perspectives; Springer: Berlin/Heidelberg, Germany, 1994; pp. 41–57. [Google Scholar]
- Willer, B.; Ottenbacher, K.J.; Coad, M.L. The community integration questionnaire. A comparative examination. Am. J. Phys. Med. Rehabil. 1994, 73, 103–111. [Google Scholar] [CrossRef]
- Duncan, P.; Murphy, M.; Man, M.-S.; Chaplin, K.; Gaunt, D.; Salisbury, C. Development and validation of the multimorbidity treatment burden questionnaire (MTBQ). BMJ Open 2020, 8, e019413. [Google Scholar]
- Ullrich, P.; Werner, C.; Bongartz, M.; Kiss, R.; Bauer, J.; Hauer, K. Validation of a Modified Life-Space Assessment in Multimorbid Older Persons With Cognitive Impairment. Gerontol. 2019, 59, e66–e75. [Google Scholar] [CrossRef]
- Najafi, B.; Armstrong, D.G.; Mohler, J. Novel Wearable Technology for Assessing Spontaneous Daily Physical Activity and Risk of Falling in Older Adults with Diabetes; SAGE Publications Sage CA: Los Angeles, CA, USA, 2013. [Google Scholar]
- Razjouyan, J.; Lee, H.; Parthasarathy, S.; Mohler, J.; Sharafkhaneh, A.; Najafi, B. Improving Sleep Quality Assessment Using Wearable Sensors by Including Information From Postural/Sleep Position Changes and Body Acceleration: A Comparison of Chest-Worn Sensors, Wrist Actigraphy, and Polysomnography. J. Clin. Sleep Med. 2017, 13, 1301–1310. [Google Scholar] [CrossRef]
- Schulman-Green, D.J.; Naik, A.D.; Bradley, E.H.; McCorkle, R.; Bogardus, S.T. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Educ. Couns. 2006, 63, 145–151. [Google Scholar] [CrossRef]
- Sanders, J.J.; Curtis, J.R.; Tulsky, J.A. Achieving goal-concordant care: A conceptual model and approach to measuring serious illness communication and its impact. J. Palliat. Med. 2018, 21, S-17–S-27. [Google Scholar] [CrossRef]
- Bhattacherjee, A.; Hikmet, N. Physicians’ resistance toward healthcare information technology: A theoretical model and empirical test. Eur. J. Inf. Syst. 2007, 16, 725–737. [Google Scholar] [CrossRef]
- Piau, A.; Wild, K.; Mattek, N.; Kaye, J. Current state of digital biomarker technologies for real-life, home-based monitoring of cognitive function for mild cognitive impairment to mild Alzheimer disease and implications for clinical care: Systematic review. J. Med. Internet Res. 2019, 21, e12785. [Google Scholar] [CrossRef]
- Taylor, J.K.; Buchan, I.E.; van der Veer, S.N. Assessing life-space mobility for a more holistic view on wellbeing in geriatric research and clinical practice. Aging Clin. Exp. Res. 2019, 31, 439–445. [Google Scholar] [CrossRef]

| Participant Characteristics | |
|---|---|
| Number of Participants, n | 19 |
| Gender, Male Age, Years | 100% 85.6 ± 6.0 |
| MoCA, Score | 15.3 ± 6.3 |
| Cognitive Ability | |
| Severe Impairment | 7 |
| Moderate Impairment | 6 |
| Mild Impairment | 6 |
| Activity of Daily Life | |
| Lowest Ability | 8 |
| Mid-Range | 5 |
| Highest Ability | 6 |
| Sensor Parameter | Mean Difference | 95% CI | p |
|---|---|---|---|
| Walking duration (min.) | 8.08 | −18.45, 34.60 | 0.536 |
| Step count | 823.45 | −753.35, 2400 | 0.292 |
| Average steps per walking bout 1 | 4.61 | −1.42, 10.64 | 0.131 |
| Number of long walking bouts 2 | 5.53 | −15.29, 26.37 | 0.588 |
| Percent walking relative to sedentary behavior 3 | 4.08 | −11.96, 3.82 | 0.297 |
| Sleep duration (min) | 0.13 | −0.56, 0.81 | 0.702 |
| Sleep onset latency (min) 4 | 10.42 | −4.35, 25.20 | 0.158 |
| Wakefulness after sleep onset (min) 5 | 11.73 | −59.44, 35.98 | 0.617 |
| Sit-to-stand transition (seconds) | 0.02 | −0.37, 0.41 | 0.916 |
| Survey Measure | |||
| World Health Organization Quality of Life OLD (WHOQOL-OLD) | 0.02 | −1.88, 2.28 | 0.845 |
| Multimorbid Treatment Burden Questionnaire (MTBQ) | 0.67 | −3.51, 3.65 | 0.970 |
| Community Integration Questionnaire (CIQ) | 0.73 | 0.98, −1.27 | 0.459 |
| Life space function | −0.07 | −4.61, 4.48 | 0.976 |
| Case 1: Mr. J | Case 2: Mr. K | Case 3: Mr. L | Case 4: Mr. M | |
|---|---|---|---|---|
| Cognitive Ability | Moderate Impairment | Moderate Impairment | Low Impairment | Severe Impairment |
| ADL/IADL Function | Highest Ability | Lowest Ability | Highest Ability | Mid-range Ability |
| Values and Goals | He enjoys his hobbies and engaging in physical activity. He was walking his dogs regularly, he but stopped. His goal is to walk his dogs every day. He is to continue treatment, and there are no issues or barriers to achieving goals. | He wants to remain as independent as possible. He would like to play with his dogs and do light housework. To maintain his strength, he will continue physical therapy weekly. He will also continue to manage his diabetes. | He enjoys spending time with his family and wants to visit his sister in Florida. He will continue treatment for memory loss. His caregiver should tell his sister that a change in environment might upset his routines. His physician also recommended alarm system because he wandered at night. | He values remaining independent and living at home. His caregiver does not live with him but visits him every morning with food. However, he sometimes does not eat lunch. His physician recommended homemaking services to prepare his lunch and ensure he eats it. |
| Sensor Parameter | Percent change from baseline to follow-up for each sensor parameter | |||
| Walking duration (min.) | 28 | 143 | −19 | −76 |
| Step count | 18 | 60 | −145 | −466 |
| Average steps per walking bout 1 | 14 | 28 | −42 | −39 |
| Number of long walking bouts 2 | 50 | 0 t | −53 | −100 |
| Percent walking relative to sedentary behavior 3 | 144 | 171 | −160 | −264 |
| Sleep duration (min) | 1 | 10 | 0 | 33 |
| Sleep onset latency (min) 4 | 8 | −721 | −52 | −35 |
| wakefulness after sleep onset (min) 5 | 6 | 56 | 13 | 54 |
| Survey Measure | Baseline Survey score, Follow-Up Survey score | |||
| WHO-QOL-OLD | 20, 20 | 20, 18 | 16, 16 | 17, 16 |
| MTBQ | 2, 2 | 2, 4 | 6, 6 | 10, 6 |
| CIQ | 15, 15 | 8, 12 | 12, 12 | 13, 13 |
| Life Space Function | 30, 30 | 21.5, 24.5 | 34, 34 | 21, 18 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freytag, J.; Mishra, R.K.; Street, R.L., Jr.; Catic, A.; Dindo, L.; Kiefer, L.; Najafi, B.; Naik, A.D. Using Wearable Sensors to Measure Goal Achievement in Older Veterans with Dementia. Sensors 2022, 22, 9923. https://doi.org/10.3390/s22249923
Freytag J, Mishra RK, Street RL Jr., Catic A, Dindo L, Kiefer L, Najafi B, Naik AD. Using Wearable Sensors to Measure Goal Achievement in Older Veterans with Dementia. Sensors. 2022; 22(24):9923. https://doi.org/10.3390/s22249923
Chicago/Turabian StyleFreytag, Jennifer, Ram Kinker Mishra, Richard L. Street, Jr., Angela Catic, Lilian Dindo, Lea Kiefer, Bijan Najafi, and Aanand D. Naik. 2022. "Using Wearable Sensors to Measure Goal Achievement in Older Veterans with Dementia" Sensors 22, no. 24: 9923. https://doi.org/10.3390/s22249923
APA StyleFreytag, J., Mishra, R. K., Street, R. L., Jr., Catic, A., Dindo, L., Kiefer, L., Najafi, B., & Naik, A. D. (2022). Using Wearable Sensors to Measure Goal Achievement in Older Veterans with Dementia. Sensors, 22(24), 9923. https://doi.org/10.3390/s22249923







