Passive Exoskeleton with Gait-Based Knee Joint Support for Individuals with Cerebral Palsy
Abstract
1. Introduction
2. Related Work
3. Materials and Methods
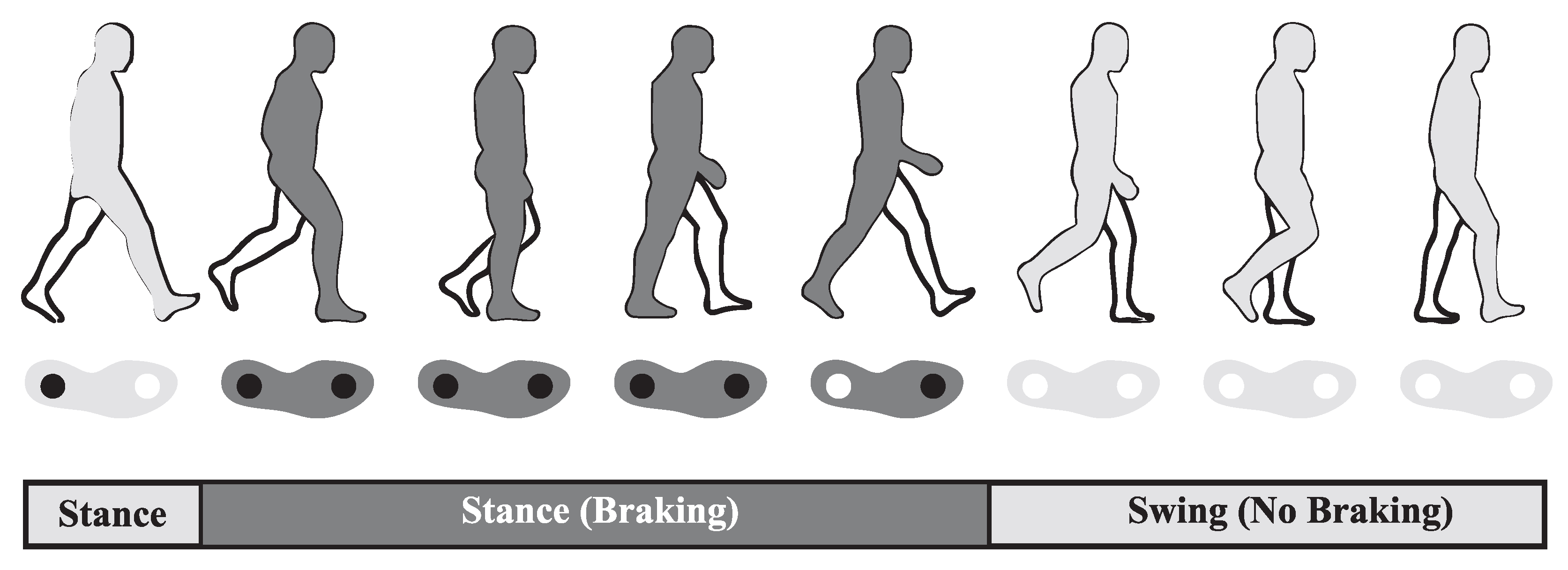
3.1. Concept
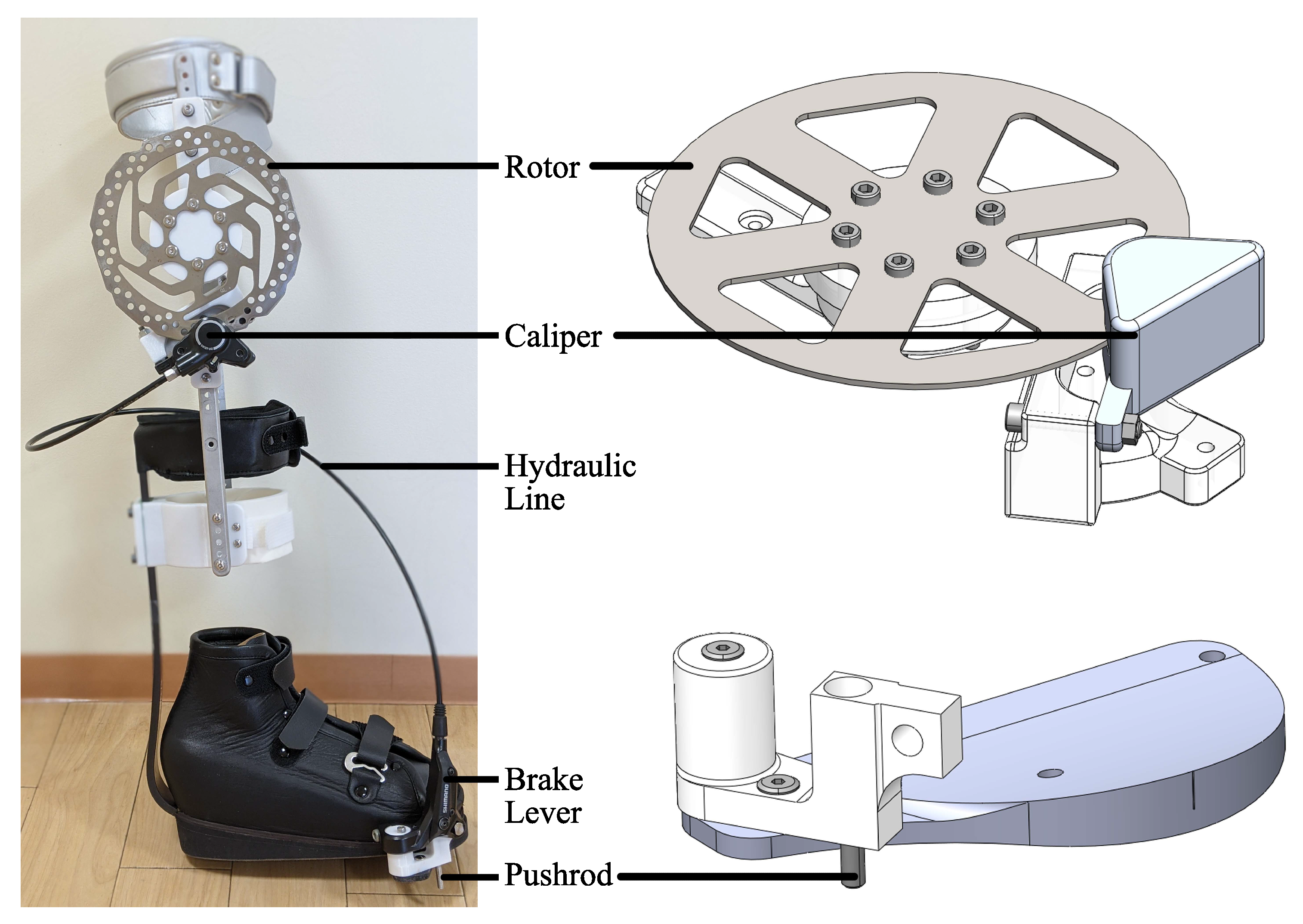
3.2. System Overview
3.3. System Modeling
4. Performance Evaluations
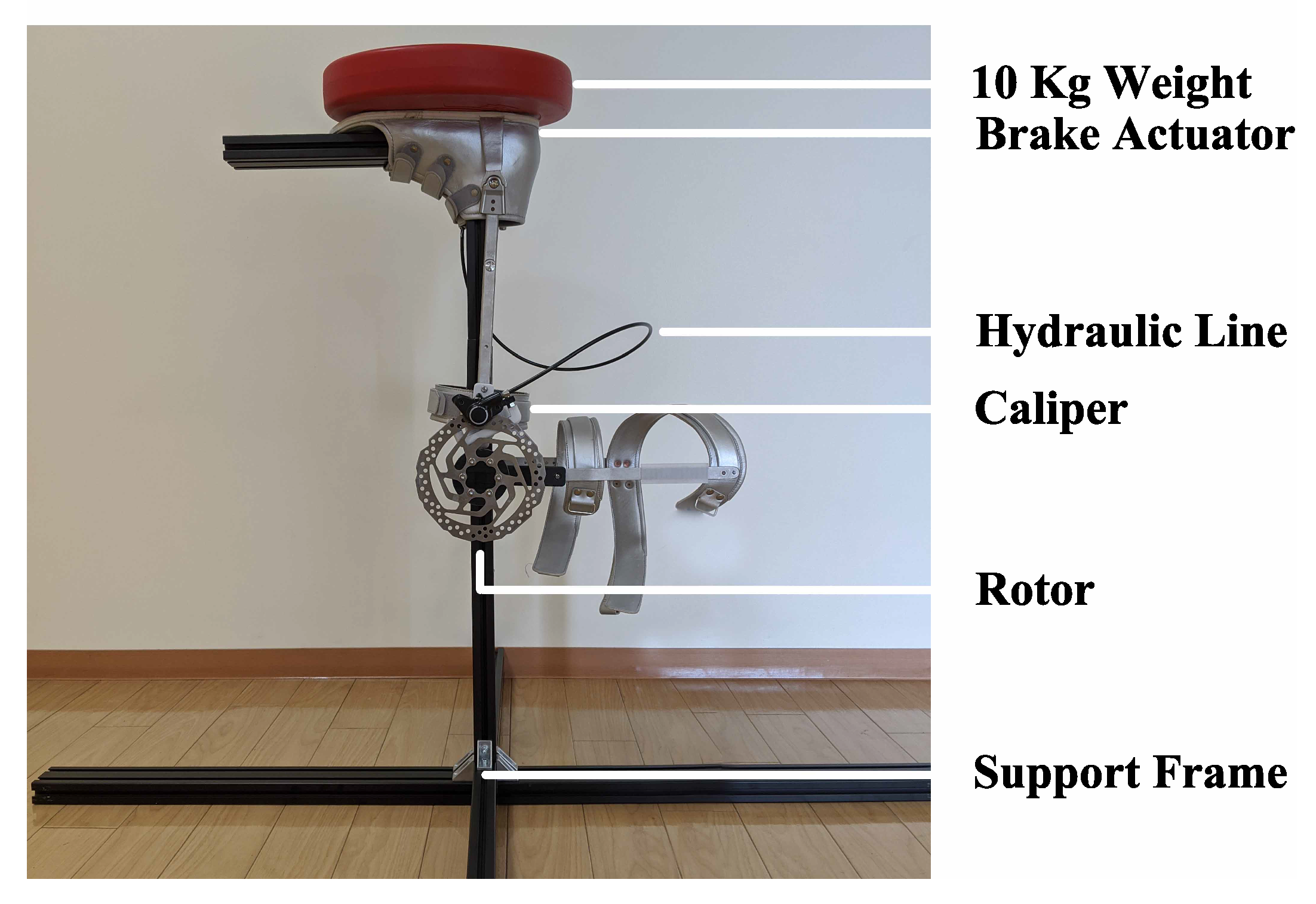
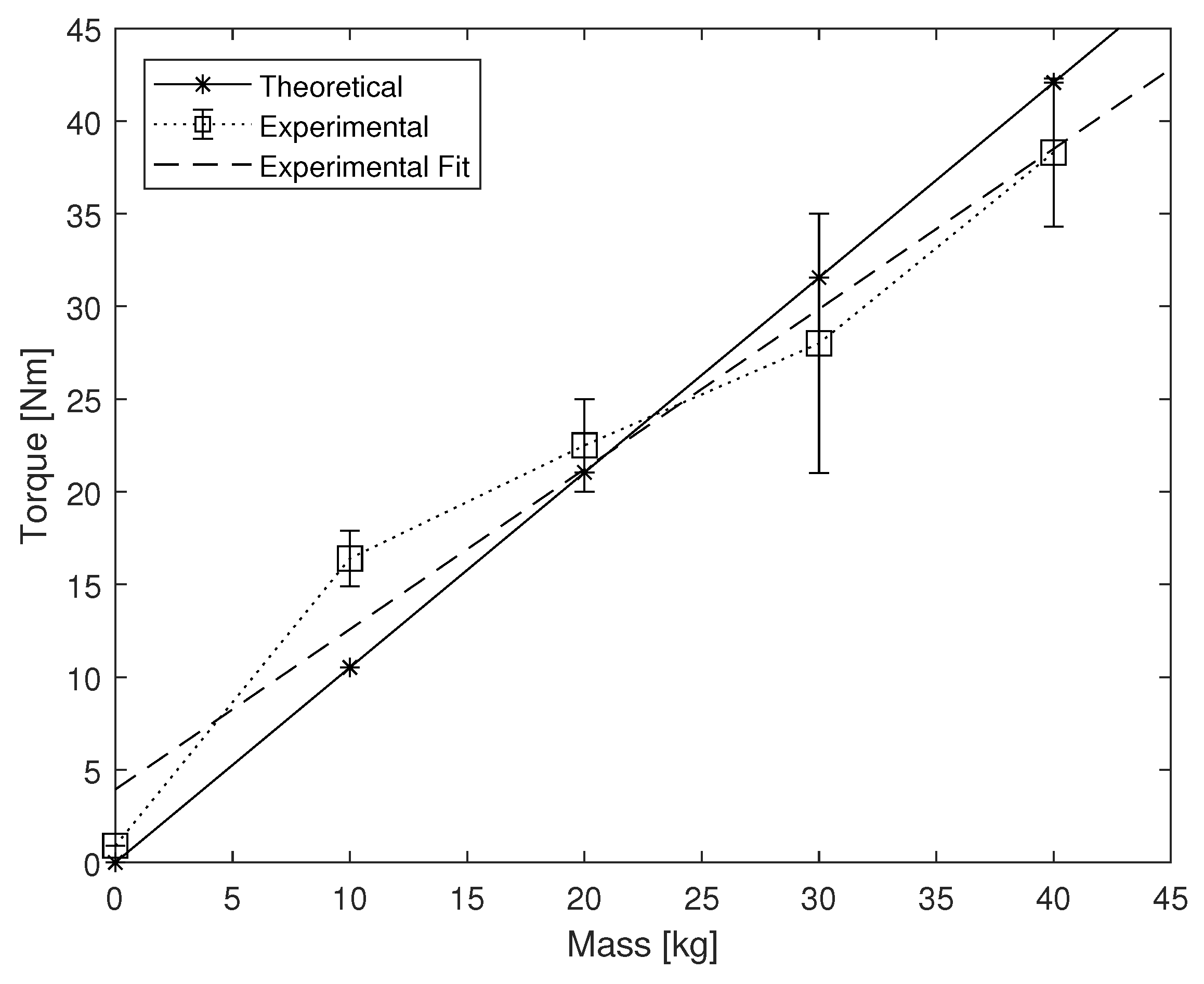
4.1. Brake Torque Measurement
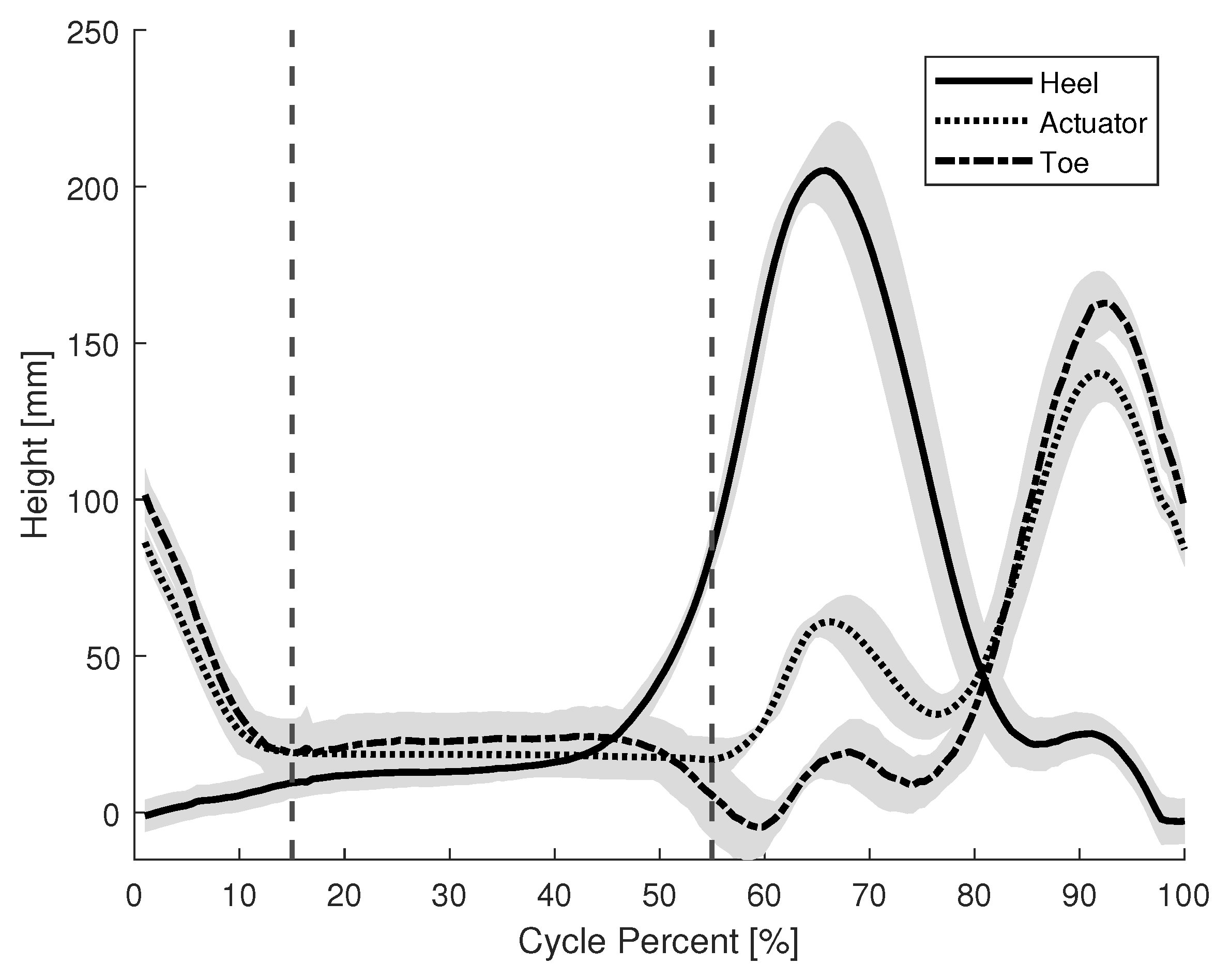
4.2. Brake Activation Timing
5. Experimental Evaluations
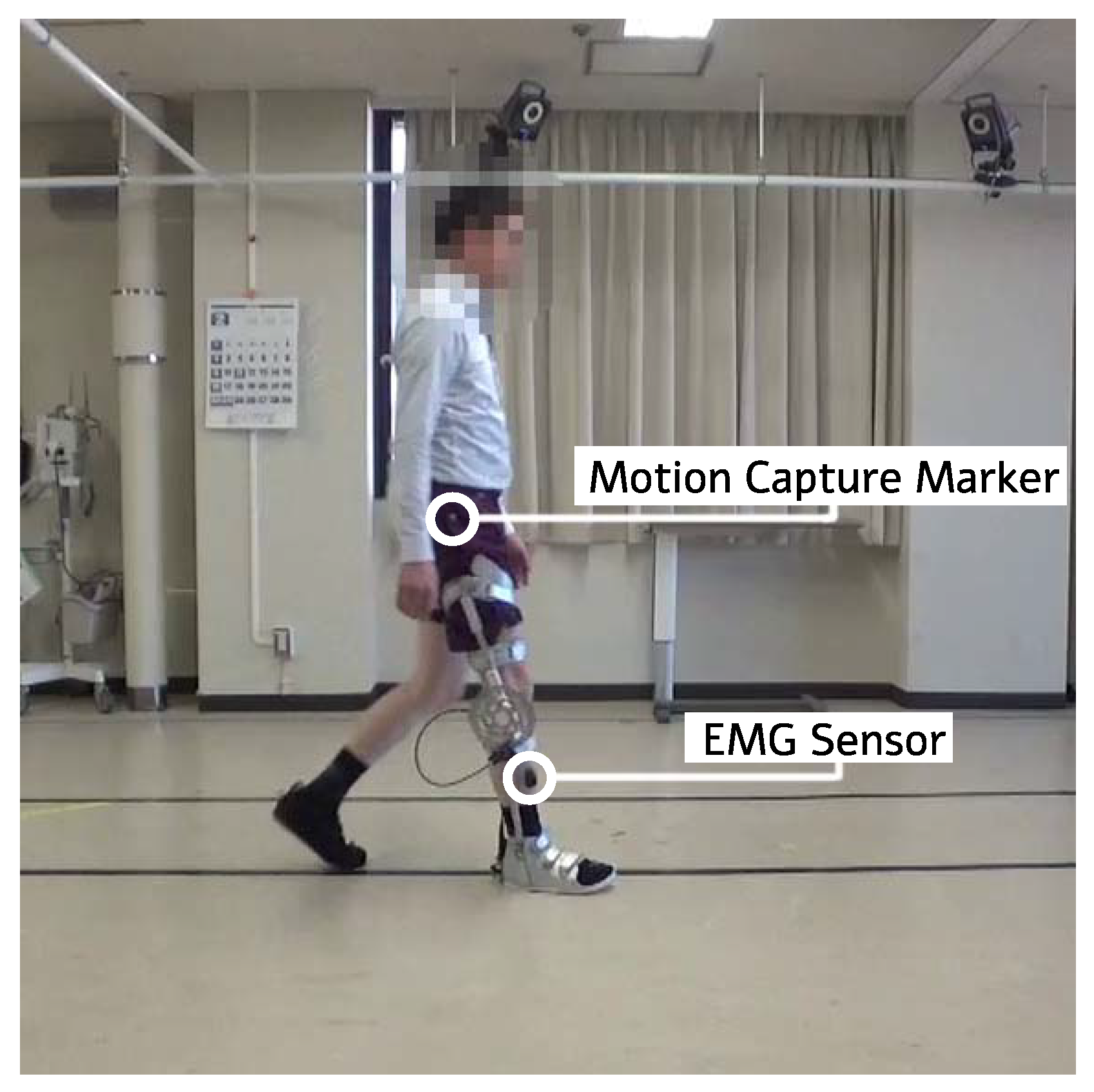
5.1. Gait Support Experiment: Healthy Participants
5.2. Gait Support Experiment: Individual with Cerebral Palsy
6. Results
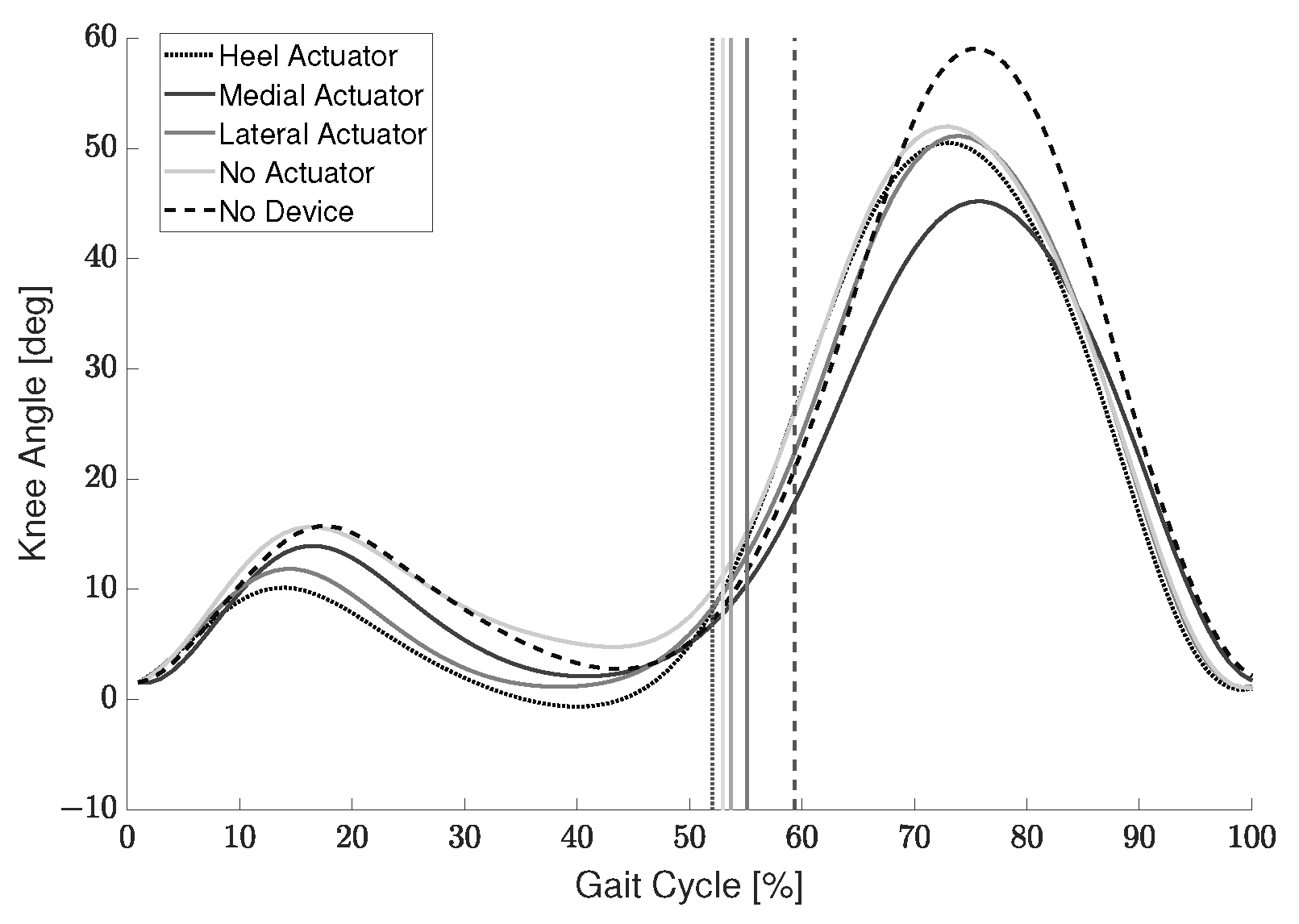
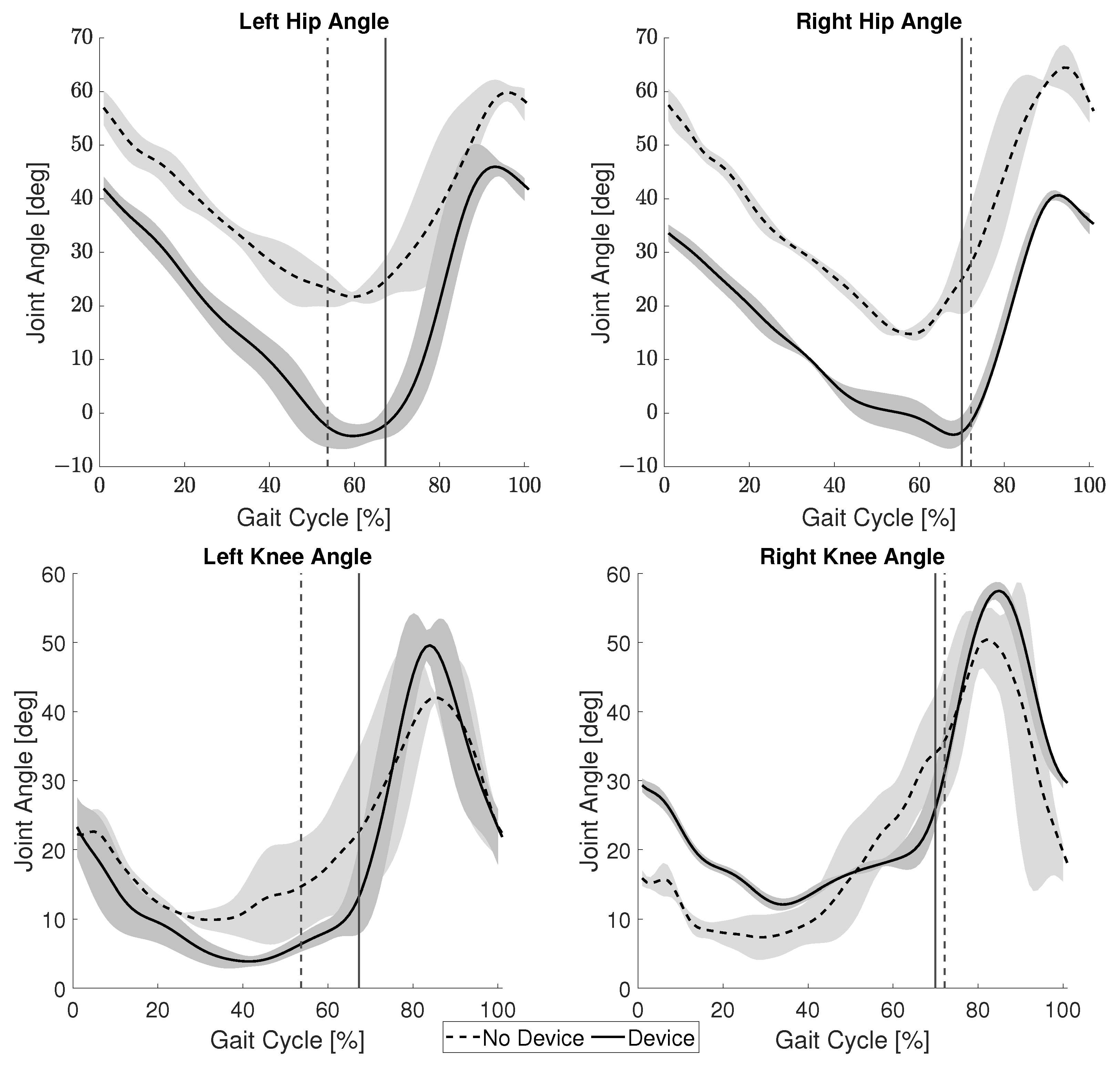
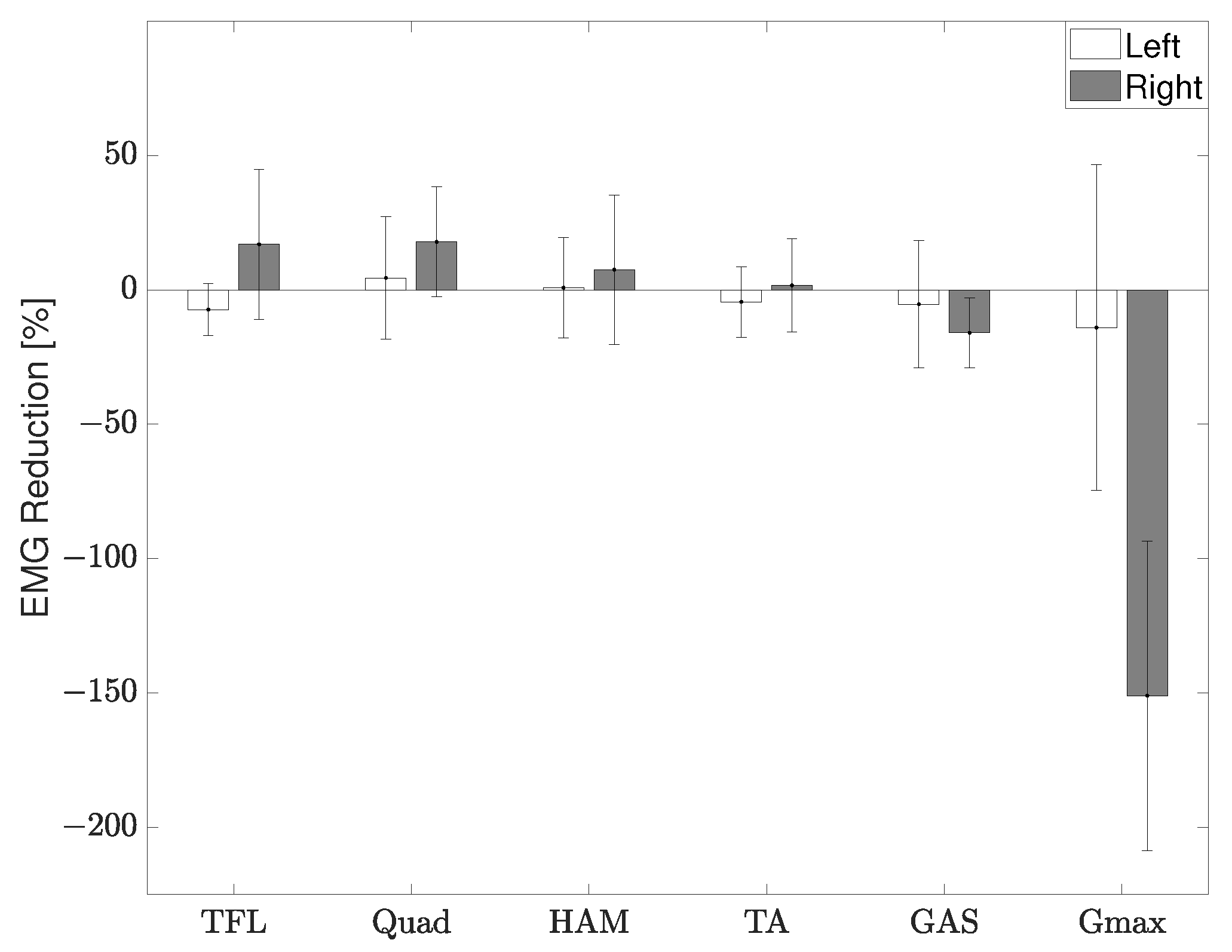
6.1. Gait Support Experiment: Healthy Participants
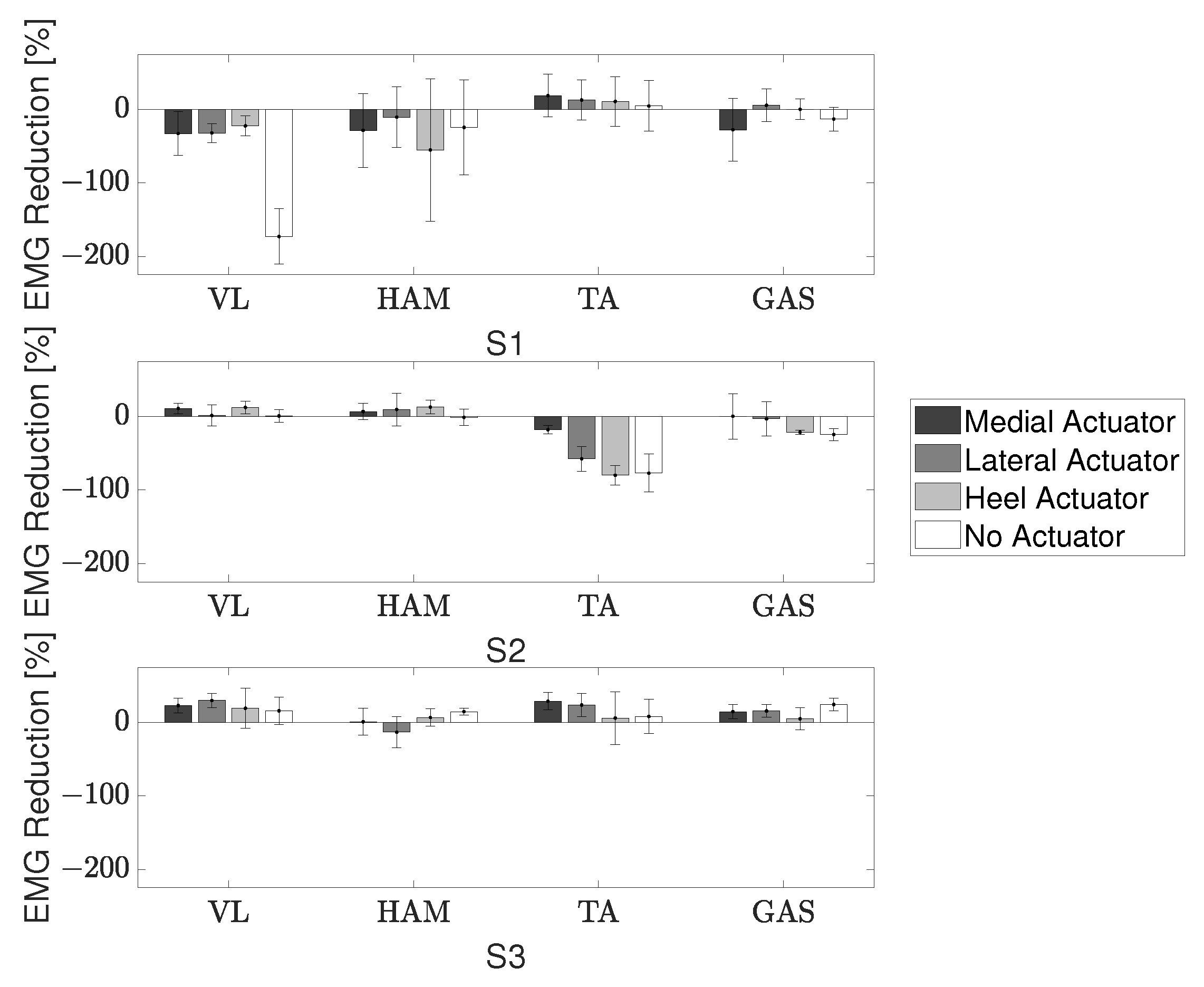
6.2. Gait Support Experiment: Individual with Cerebral Palsy
7. Discussion
7.1. Device Evaluation: Healthy Participants
7.2. Device Evaluation: Individual with Cerebral Palsy
7.3. Gait Support
7.4. Comparison to Related Work
7.5. Future Improvements
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CP | cerebral palsy |
| CSV | comma-separated values |
| EMG | electromyography |
| GAS | gastrocnemius |
| Gmax | gluteus maximus |
| HAM | hamstring |
| KAFO | knee ankle foot orthosis |
| NMES | neuromuscular electrical stimulation |
| QUAD | quadriceps |
| RR | reduction ratio |
| TA | tibialis anterior |
| TFL | tensor fascia latae |
| VL | vastus lateralis |
References
- NINDS. Cerebral Palsy: Hope Through Research; NIH Publication: Bethesda, MA, USA, 2013; pp. 13–159. [Google Scholar]
- Van Naarden Braun, K.; Doernberg, N.; Schieve, L.; Christensen, D.; Goodman, A.; Yeargin-Allsopp, M. Birth Prevalence of Cerebral Palsy: A Population-Based Study. Pediatrics 2016, 137, e20152872. [Google Scholar] [CrossRef] [PubMed]
- Pakula, A.T.; Braun, K.V.N.; Yeargin-Allsopp, M. Cerebral Palsy: Classification and Epidemiology. Phys. Med. Rehabil. Clin. N. Am. 2009, 20, 425–452. [Google Scholar] [CrossRef] [PubMed]
- Das, S.P.; Ganesh, G.S. Evidence-based Approach to Physical Therapy in Cerebral Palsy. Indian J. Orthop. 2019, 53, 20–34. [Google Scholar] [CrossRef] [PubMed]
- Dreher, T.; Vegvari, D.; Wolf, S.I.; Geisbüsch, A.; Gantz, S.; Wenz, W.; Braatz, F. Development of knee function after hamstring lengthening as a part of multilevel surgery in children with spastic diplegia: A long-term outcome study. J. Bone Jt. Surg. Am. 2012, 94, 121–130. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Economic Costs Associated with Mental Retardation, Cerebral Palsy, Hearing Loss, and Vision Impairment—United States, 2003; MMWR Morbidity and Mortality Weekly Report; CDC (Centers for Disease Control and Prevention): Atlanta, GA, USA, 2004; Volume 53, pp. 57–59.
- Abbasi, L.; Rojhani-Shirazi, Z.; Razeghi, M.; Raeisi Shahraki, H. Trunk Kinematic Analysis during Gait in Cerebral Palsy Children with Crouch Gait Pattern. J. Biomed. Phys. Eng. 2018, 8, 281–288. [Google Scholar] [PubMed]
- Cecarelli, M.; Carbone, G. Design and Operation of Human Locomotion Systems; Elsevier: Amsterdam, The Netherlands, 2020. [Google Scholar]
- Hicks, J.L.; Schwartz, M.H.; Arnold, A.S.; Delp, S.L. Crouched postures reduce the capacity of muscles to extend the hip and knee during the single-limb stance phase of gait. J. Biomech. 2008, 41, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Rose, J.; Gamble, J.G.; Burgos, A.; Medeiros, J.; Haskell, W.L. Energy expenditure index of walking for normal children and for children with cerebral palsy. Dev. Med. Child Neurol. 1990, 32, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Kennard, M.; Kadone, H.; Suzuki, K. Passive Knee Exoskeleton with Variable Stiffness Control for Assisting Crouch Gait. In Proceedings of the JSME Annual Conference on Robotics and Mechatronics (Robomec), Kanazawa, Japan, 27–30 May 2020; Volume 2020, p. 2P2-E13. [Google Scholar] [CrossRef]
- Lerner, Z.F.; Damiano, D.L.; Park, H.; Gravunder, A.J.; Bulea, T.C. A Robotic Exoskeleton for Treatment of Crouch Gait in Children With Cerebral Palsy: Design and Initial Application. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 650–659. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Kadone, H.; Shimizu, Y.; Suzuki, K. An Exoskeleton Brake Unit for Children with Crouch Gait Supporting the Knee Joint During Stance. In Proceedings of the 2018 International Symposium on Micro-NanoMechatronics and Human Science (MHS), Nagoya, Japan, 9–12 December 2018; pp. 1–7. [Google Scholar] [CrossRef]
- Shideler, B.L.; Bulea, T.C.; Chen, J.; Stanley, C.J.; Gravunder, A.J.; Damiano, D.L. Toward a hybrid exoskeleton for crouch gait in children with cerebral palsy: Neuromuscular electrical stimulation for improved knee extension. J. Neuroeng. Rehabil. 2020, 17, 121. [Google Scholar] [CrossRef] [PubMed]
- Pröbsting, E.; Kannenberg, A.; Zacharias, B. Safety and walking ability of KAFO users with the C-Brace® Orthotronic Mobility System, a new microprocessor stance and swing control orthosis. Prosthetics Orthot. Int. 2017, 41, 65–77. [Google Scholar] [CrossRef] [PubMed]
- Mataki, Y.; Kamada, H.; Mutsuzaki, H.; Shimizu, Y.; Takeuchi, R.; Mizukami, M.; Yoshikawa, K.; Takahashi, K.; Matsuda, M.; Iwasaki, N.; et al. Use of Hybrid Assistive Limb (HAL®) for a postoperative patient with cerebral palsy: A case report. BMC Res. Notes 2018, 11, 201. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Lee, K.; Ji, J. A Passive Gait-Based Weight-Support Lower Extremity Exoskeleton with Compliant Joints. IEEE Trans. Robot. 2016, 32, 933–942. [Google Scholar] [CrossRef]
- van Dijk, W.; van der Kooij, H.; Hekman, E. A passive exoskeleton with artificial tendons: Design and experimental evaluation. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–6. [Google Scholar] [CrossRef]
- Kirkwood, G.L.; Otmar, C.D.; Hansia, M. Who’s Leading This Dance?: Theorizing Automatic and Strategic Synchrony in Human-Exoskeleton Interactions. Front Psychol. 2021, 12, 624108. [Google Scholar] [CrossRef] [PubMed]
- MathWorks. Longitudinal Wheel with Disc, Drum, or Mapped Brake. Available online: https://www.mathworks.com/help/autoblks/ref/longitudinalwheel.html (accessed on 21 January 2022).
- Armand, S.; Decoulon, G.; Bonnefoy-Mazure, A. Gait analysis in children with cerebral palsy. EFORT Open Rev. 2016, 1, 448–460. [Google Scholar] [CrossRef]
- Skaaret, I.; Steen, H.; Niratisairak, S.; Swanson, D.; Holm, I. Postoperative changes in vertical ground reaction forces, walking barefoot and with ankle-foot orthoses in children with Cerebral Palsy. Clin. Biomech. 2021, 84, 105336. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.; Martelli, D.; Vashista, V.; Martinez-Hernandez, I.; Kim, H.; Agrawal, S.K. Robot-driven downward pelvic pull to improve crouch gait in children with cerebral palsy. Sci. Robot. 2017, 2, eaan2634. [Google Scholar] [CrossRef] [PubMed]
- Hussain, I.; Park, S.J. Prediction of Myoelectric Biomarkers in Post-Stroke Gait. Sensors 2021, 21, 5334. [Google Scholar] [CrossRef] [PubMed]




| Exoskeleton | Actuator | Support Mechanism | Power | Weight (kg) |
|---|---|---|---|---|
| Lerner [12] | Active | DC Motor | Battery/External | 3.2 |
| Yamada [13] | Active | DC Motor | Battery | 1.76 |
| Shideler [14] | Semi-Active | NMES | Battery | 3.2 |
| C-Brace * [15] | Active | Hydraulic | Battery | 1.39 |
| HAL * [16] | Active | DC Motor | Battery | 14 |
| Wang [17] | Passive | Spring | - | 1.95 |
| Van Dijk [18] | Passive | Spring | - | 12 |
| Component | Weight (kg) |
|---|---|
| Commercial KAFO | 0.50 |
| Carbon Fiber Shoe | 0.95 |
| Caliper/Actuator | 0.25 |
| Rotor | 0.14 |
| Polycarbonate Mounts | 0.28 |
| Total * | 2.2 |
| S1 | S2 | S3 | |
|---|---|---|---|
| Medial | 0.13 | 2.11 | 2.64 |
| Lateral | 0.51 | 5.67 | 5.43 |
| Heel | 2.93 | 8.95 | 4.82 |
| No Actuator | −10.21 | 2.89 | 5.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kennard, M.; Kadone, H.; Shimizu, Y.; Suzuki, K. Passive Exoskeleton with Gait-Based Knee Joint Support for Individuals with Cerebral Palsy. Sensors 2022, 22, 8935. https://doi.org/10.3390/s22228935
Kennard M, Kadone H, Shimizu Y, Suzuki K. Passive Exoskeleton with Gait-Based Knee Joint Support for Individuals with Cerebral Palsy. Sensors. 2022; 22(22):8935. https://doi.org/10.3390/s22228935
Chicago/Turabian StyleKennard, Maxwell, Hideki Kadone, Yukiyo Shimizu, and Kenji Suzuki. 2022. "Passive Exoskeleton with Gait-Based Knee Joint Support for Individuals with Cerebral Palsy" Sensors 22, no. 22: 8935. https://doi.org/10.3390/s22228935
APA StyleKennard, M., Kadone, H., Shimizu, Y., & Suzuki, K. (2022). Passive Exoskeleton with Gait-Based Knee Joint Support for Individuals with Cerebral Palsy. Sensors, 22(22), 8935. https://doi.org/10.3390/s22228935







