Technological Solutions for Social Isolation Monitoring of the Elderly: A Survey of Selected Projects from Academia and Industry
Abstract
:1. Introduction
- Physical impacts: Social isolation limits the elderly’s relationship with the outside world which leads to a decrease in physical activities that are important for their health and well-being. Consequently, it leads to a decline in physical abilities [6].
- Health impacts: Social isolation has devastating effects on the health of the elderly, particularly at the nutritional level. Indeed, the risk of malnutrition have increased among the elderly who are socially isolated [7].
2. Methods
2.1. Overview
2.2. Inclusion Criteria for Elderly Monitoring System Research
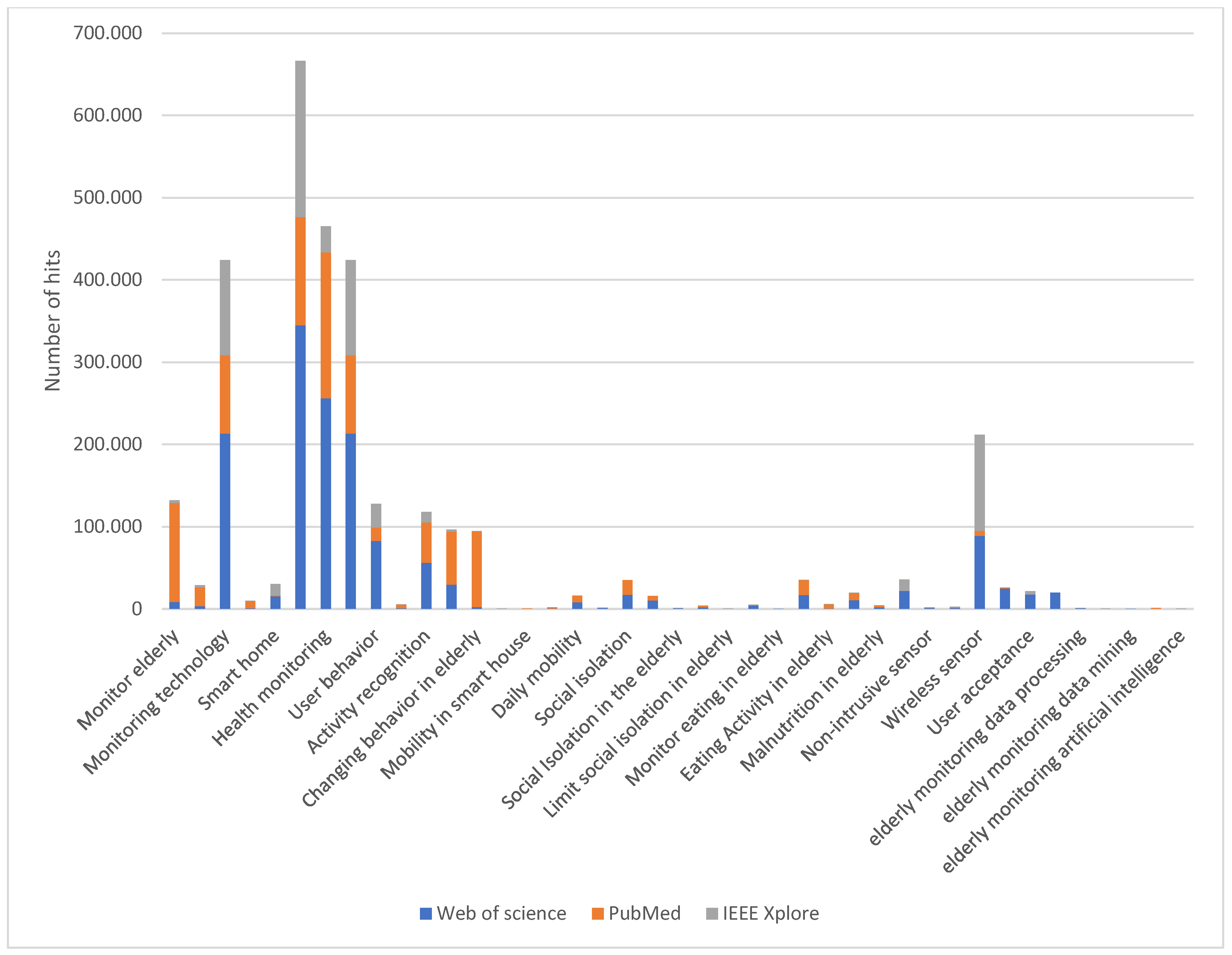
2.3. Research Methods and Strategy
2.4. Results
3. Current Issues in the Elderly Monitoring Systems
3.1. User Needs, Perception and Acceptance
3.2. Architecture Selection and Requirements
- Heterogeneity: it refers to the fact that IoT systems are composed of different components with different communication protocols, and despite this diversity, they can be integrated into a single system.
- Interoperability: it refers to the ability of the system to provide easy and understandable interfaces by all IoT components and to exchange data between them.
- Maintainability: it refers to the ability of the system to work despite the updates to its components or the addition of new components and therefore to maintain it over time.
- Scalability: it refers to the ability of the system to work as intended despite the changes in the number of users or in the hardware or software.
- Reliability: it refers to the ability of the system to consistently perform as expected and therefore be trusted.
- Efficiency: it refers to the ability of the system to perform in the best feasible way by optimizing time and resources.
- Effectiveness: it refers to the ability of the system to function as intended or to produce the expected results.
- Security: it refers to the ability of the system to ensure the security of data when it is transferred or saved as it relates to the privacy of users.
- Adaptability: it refers to the system’s ability to meet the needs of each senior, as this type of project must be personalized to the individual’s profile.
- Usability: it refers to the ability of the system to be easy to use for the elderly, regardless of their knowledge of technology. In addition, the system should consider having a function for sharing data and notifying caregivers in case of an emergency so that seniors feel safe in their homes.
- Accuracy: it refers to the ability of the system to provide the adapted services to seniors despite the different profiles and requests of each.
3.3. Hardware and Software Considerations
3.4. Ethical Considerations
4. Monitoring System Features
4.1. Meal-Taking Process
- Food shopping: This is the activity where the person goes to the market to buy different ingredients to cook or to buy already prepared meals. For the elderly, food shopping is not a simple activity, but it is considered an important social event where they can interact with others, as the risk of isolation increases. In fact, for some older people living alone, it is the only opportunity for social interaction. In [19], the authors mention that older people consider the social element and experience of food shopping as a positive factor. The social aspect of food shopping is particularly important to this age group and regular social interaction is recognized as a key element in maintaining mental and physical wellbeing.
- Cooking: The skill or activity of preparing and heating food for eating. Cooking has many physical, emotional, mental and health benefits. This process begins with planning what to cook and what ingredients are needed and if there is a need to go shopping. Then, the person mixes the required ingredients according to a recipe and focuses on the meal until it is properly prepared. This is a good physical and mental exercise. A study of older women in Taiwan found that those who cooked more frequently are engaged in more health-promoting behaviors, such as socializing, and fewer health risk behaviors, such as smoking [20]. In addition, cooking is an opportunity for socialization: seniors can collaborate with each other during meal preparation and sharing food with neighbors and friends is a form of social bonding. Finally, meal preparation allows the seniors to use healthy and fresh ingredients, and thus eat delicious and nutritious meals that they prepared, which they can be proud of. A survey conducted by the University of Michigan National Poll on Healthy Aging in December 2019 shows that many adults between the ages of 50 and 80 reported enjoying cooking (71%) [21].
- Eating: It provides energy to the body. It is important for older adults to stay as active and healthy as possible. Although it is recognized that good nutrition is important for successful aging, malnutrition is one of the greatest threats to the health, autonomy, and well-being of older adults [22]. For the elderly, malnutrition is not the consequence of a lack of food, but of a deterioration in the desire to eat and is related to several factors such as serious health conditions, medication side effects, lack of exercise, difficulties in chewing, swallowing or self-eating, depression, loneliness, and social isolation [23]. Monitoring the eating activity in the elderly is essential to ensuring their well-being.
- Dishwashing: this involves cleaning the dishes of food remains on plates. This can be done manually by hand in the sink or automatically by the dishwasher. Although dishwashing is a light activity, it can be a good physical activity for the elderly that helps prolong their lives. In a U.S. study conducted by the University at Buffalo of more than 6000 white, African American and Hispanic women aged 63 to 99 years, researchers found a significantly lower risk of death for those who were active, even while performing light activity, than in those who were inactive [24].
4.2. Mobility
4.3. Social Isolation and Loneliness
4.3.1. Definitions
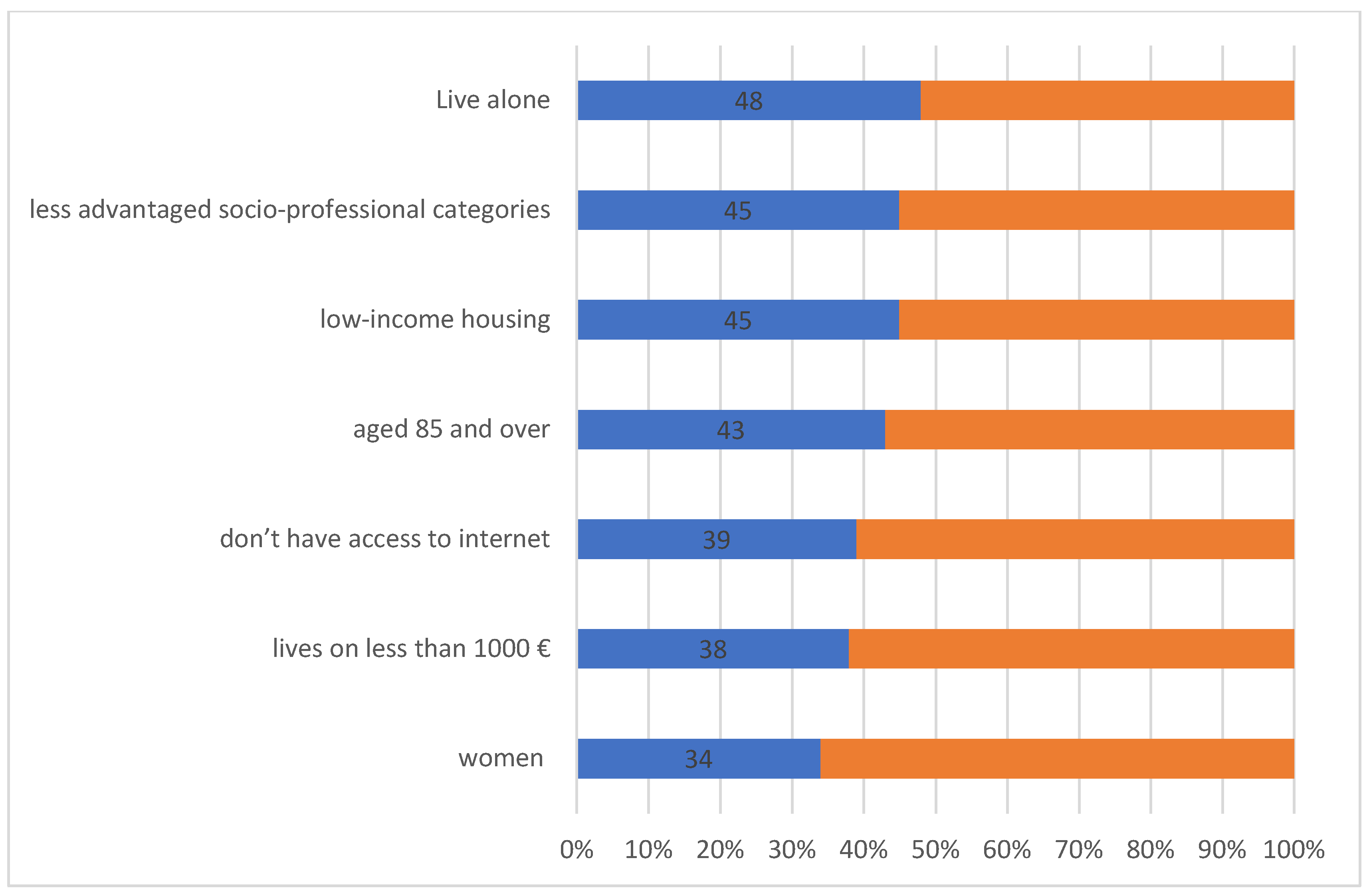
4.3.2. Risk Factors for Social Isolation/Loneliness
4.3.3. Social Isolation/Loneliness Evaluation
4.3.4. Health Impacts of Social Isolation and Loneliness
5. Overview of Systems Proposed and Data Collected
5.1. Hardware Implementation
5.1.1. Non-Wearable Sensors
5.1.2. Wearable Sensors
5.2. Software and Algorithm Processing
5.3. Participants, Duration and Location of Data Collection
6. Monitoring System Examples
6.1. Research Prototypes
6.1.1. Binary Sensor Approach
6.1.2. Binary and Non-Binary Sensor Approach
6.1.3. Video and Audio Approaches
6.1.4. Wearable Sensor Approach
6.2. Commercial Products
7. Discussion
- (1)
- Different kinds of sensors, ranging from PIR sensor to camera, were identified in the studies in order to recognize ADLs. Although there are promising results in recognizing them, it has not been possible to identify the best sensor for recognizing the meal-taking activity and mobility. A combination of different types of sensors usually provides better results in identifying the ADLs. In addition, intrusive sensors such as camera and microphone are not preferred in those types of monitoring systems due to their privacy violation.
- (2)
- Different types of algorithms have been used to identify ADLs, but the majority of the algorithms use a supervised machine learning algorithm, which gives good results in detecting them. In every system, however, there is the problem of providing annotated data because self-annotation by the user causes different problems such as omissions, errors in entering certain labels, etc. In some systems, they used the camera as a tool to label ADLs, such as in the case of the system presented in [70]. However, we face the same problem of privacy violation of the monitored person despite using the camera only for labeling and not for identifying ADLs.
- (3)
- The majority of data used in different systems are collected in smart home laboratory conditions during several days with participation of young adults. This first step is appreciable but it is not efficient. In fact, collecting real data in the homes of the persons is quite different compared to collecting the data in the laboratory because each person has its own rhythm when performing ADLs. They are not real enough, they do not allow enough variety and complexity and the observed person is more comfortable when performing tasks in their home. In addition, to ameliorate the results of identification of ADLs, systems need to collect data during several weeks and not for a few days because the rhythm of performing the activities can change. Furthermore, the purpose of the monitoring systems is to be installed in homes of seniors. Therefore, collecting and analyzing data of young adults is not adequate because the rhythm of realizing ADLs of the elderly is different from their rhythm. That is why collecting real data in homes of seniors for long period of time is the best way to obtaining better results in identifying ADLs.
- (4)
- Despite much research in the field of ADL monitoring in the elderly, few researchers, such as [55], have used ADL identification as a first step to identifying potential risk of loneliness and depression in the elderly. We did not find any article, based on our research, which uses identification of ADLs (mobility and meal-taking activity) to identify seniors with risk of social isolation.
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gilmour, H.; Ramage-Morin, P. Social Isolation and Mortality among Canadian Seniors; Health Reports/Statistics Canada; Canadian Centre for Health Information: Ottawa, ON, Canada, 2020; pp. 27–38. [Google Scholar]
- Higgs, P.; Robert, L.B.; Joseph, S.C. Social Isolation among Older Individuals: The Relationship to Mortality and Morbidity; National Academy Press: Washington, DC, USA, 1992. [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; Assessment of Social Isolation and Loneliness in Research; National Academies Press: Washington, DC, USA, 2020. [Google Scholar]
- Rapport Petits Frères des Pauvres: Isolement des Personnes Âgées: Les Impacts de la Crise Sanitaire #5; Petits Frères des Pauvre: Paris, France, 2021.
- Wiktorsson, S.; Runeson, B.; Skoog, I.; Ostling, S.; Waern, M. Attempted Suicide in the Elderly: Characteristics of Suicide Attempters 70 Years and Older and a General Population Comparison Group. Am. J. Geriatr. Psychiatry Off. J. Am. Assoc. Geriatr. Psychiatry 2010, 18, 57–67. [Google Scholar] [CrossRef]
- del Pozo Cruz, B.; Perales, F.; Alfonso-Rosa, R.; Del Pozo-Cruz, J. Impact of Social Isolation on Physical Functioning among Older Adults: A 9-Year Longitudinal Study of a U.S.-Representative Sample. Am. J. Prev. Med. 2021, 61, 158–164. [Google Scholar] [CrossRef]
- Boulos, C.; Salameh, P.; Barberger-Gateau, P. Social isolation and risk for malnutrition among older people. Geriatr. Gerontol. Int. 2017, 17, 286–294. [Google Scholar] [CrossRef]
- Rapport Petits Frères des Pauvres: Solitude et Isolement Quand on a plus de 60 ans en France en 2017; Petits Frères des Pauvre: Paris, France, 2017.
- 2020 Generational Real Estate Trends Report: Aging in Place. Available online: https://sothebysrealty.ca/insightblog/en/2020/03/04/2020-generational-real-estate-trends-report-aging-in-place (accessed on 28 September 2021).
- Minister of Loneliness in United Kingdom. Available online: https://www.gov.uk/government/publications/loneliness-annual-report-the-first-year/loneliness-annual-report-january-2020--2 (accessed on 28 September 2021).
- Minister of Social Isolation in Japan. Available online: https://bigthink.com/the-present/japan-loneliness-minister/#rebelltitem2 (accessed on 28 September 2021).
- Pol, M.; van Nes, F.; Van Hartingsveldt, M.; Buurman, B.; de Rooij, S.; Krose, B. Older People’s Perspectives Regarding the Use of Sensor Monitoring in Their Home. Gerontologist 2014, 56, 485–493. [Google Scholar] [CrossRef] [Green Version]
- Tsertsidis, A.; Kolkowska, E.; Hedström, K. Factors influencing seniors’ acceptance of technology for ageing in place in the post-implementation stage: A literature review. Int. J. Med. Inform. 2019, 129, 324–333. [Google Scholar] [CrossRef] [PubMed]
- Ngankam, H.; Pigot, H.; Parenteau, M.; Lussier, M.; Aboujaoudé, A.; Laliberté, C.; Couture, M.; Bier, N.; Giroux, S. An IoT Architecture of Microservices for Ambient Assisted Living Environments to Promote Aging in Smart Cities. In International Conference on Smart Homes and Health Telematics; Springer: Cham, Switzerland, 2019. [Google Scholar]
- Steele, R.; Lo, A.; Secombe, C.; Wong, Y. Elderly persons’ perception and acceptance of using wireless sensor networks to assist healthcare. Int. J. Med. Inform. 2009, 78, 788–801. [Google Scholar] [CrossRef] [PubMed]
- Ulrich, C.; Demiris, G.; Kennedy, R.; Rothwell, E. The Ethics of Sensor Technology Use in Clinical Research. Nurs. Outlook 2020, 68, 720–726. [Google Scholar] [CrossRef]
- Eating Well as You Age. Available online: https://www.helpguide.org/articles/healthy-eating/eating-well-as-you-age.htm (accessed on 28 September 2021).
- Diagnosis of Malnutrition in People Aged 70 and over. Available online: https://www.has-sante.fr/upload/docs/application/pdf/2021-11/argumentaire_denutrition_pa_10_nov_2021_v2.pdf (accessed on 28 September 2021).
- Lesakova, D. Seniors and Their Food Shopping Behavior: An Empirical Analysis. Procedia-Soc. Behav. Sci. 2016, 220, 243–250. [Google Scholar] [CrossRef] [Green Version]
- Farmer, N.; Touchton-Leonard, K.; Ross, A. Psychosocial Benefits of Cooking Interventions: A Systematic Review. Health Educ. Behav. 2017, 45, 167–180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Joy of Cooking and Its Benefits for Older Adults. Available online: https://www.healthyagingpoll.org/report/joy-cooking-and-its-benefits-older-adults (accessed on 28 September 2021).
- Sulmont-Rossé, C. Eating in the Elderly. In Handbook of Eating and Drinking: Interdisciplinary Perspectives; Meiselman, H.L., Ed.; Springer International Publishing: Cham, 2020; pp. 433–457. ISBN 978-3-030-14504-0. [Google Scholar]
- Reasons Why Seniors Lose Their Appetite. Available online: https://dailycaring.com/why-do-seniors-lose-their-appetites/ (accessed on 28 September 2021).
- Buchner, D.; Rillamas-Sun, E.; Di, C.; Evenson, K.; Bellettiere, J.; Lewis, C.; Lee, I.-M.; Tinker, L.; Seguin-Fowler, R.; Zaslavsky, O.; et al. Accelerometer-Measured Physical Activity and Mortality in Women Aged 63 to 99. J. Am. Geriatr. Soc. 2017, 66, 886–894. [Google Scholar]
- Eating Well as You Age. Available online: https://www.insee.fr/fr/statistiques/2118039?sommaire=2118074 (accessed on 28 September 2021).
- Amini, D.A.; Kannenberg, K.; Bodison, S.; Chang, P.; Colaianni, D.; Goodrich, B.; Mahaffey, L.; Painter, M.; Urban, M.; Handley-More, D.; et al. Occupational therapy practice framework: Domain.; process 3rd edition. Am. J. Occup. Ther. 2014, 68 (Suppl. S1), S1–S48. [Google Scholar]
- Remarkable Reasons to Encourage and Promote Senior Mobility. Available online: https://www.sunshineretirementliving.com/sunshine-stories/7-remarkable-reasons-encourage-promote-senior-mobility/ (accessed on 28 September 2021).
- Zunzunegui, M.V.; Alvarado, B.E.; Guerra, R.; Gómez, J.F.; Ylli, A.; Guralnik, J.M. Imias Research Group the Mobility Gap between Older Men and Women: The Embodiment of Gender. Arch. Gerontol. Geriatr. 2015, 61, 140–148. [Google Scholar] [CrossRef]
- Spalt, E.; Curl, C.; Allen, R.; Cohen, M.; Adar, S.; Stukovsky, K.; Avol, E.; Castro-Diehl, C.; Nunn, C.; Mancera-Cuevas, K.; et al. Time-location patterns of a diverse population of older adults: The Multi-Ethnic Study of Atherosclerosis and Air Pollution (MESA Air). J. Expo. Sci. Environ. Epidemiol. 2016, 26, 349–355. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singer, C. Health Effects of Social Isolation and Loneliness. J. Aging Life Care 2018, 28, 4–8. [Google Scholar]
- Interventions for Loneliness and Social Isolation. Available online: https://www.york.ac.uk/media/crd/Loneliness%20and%20social%20isolation.pdf/ (accessed on 28 September 2021).
- Cudjoe, T.; Roth, D.; Szanton, S.; Wolff, J.; Boyd, C.; Thorpe, R., Jr. The Epidemiology of Social Isolation: National Health & Aging Trends Study. J. Gerontology. Ser. B Psychol. Sci. Soc. Sci. 2018, 75, 107–113. [Google Scholar]
- Beach, B.; Bamford, S.M. Isolation: The Emerging Crisis for Older Men; A Report Exploring Experiences of Social Isolation and Loneliness among Older Men in England; Independent Age: London, UK, 2014. [Google Scholar]
- Older Adults and Technology Use. Available online: https://www.pewresearch.org/internet/2014/04/03/older-adults-and-technology-use/ (accessed on 28 September 2021).
- Rapport Petits Frères des Pauvres: Solitude et Isolement des Personnes âgées en France quels Liens avec les Territoires? Petits Frères des Pauvre: Paris, France, 2019.
- PhenX Toolkit Supplemental Information, Social Support. Available online: https://www.phenxtoolkit.org/toolkit_content/supplemental_info/social/measures/Social_Support_Berkman_Syme.doc (accessed on 28 September 2021).
- Berkman, L.; Syme, L. Social networks, host resistance, and mortality: A nine-year follow-up study of Alameda County residents. Am. J. Epidemiol. 1979, 109, 186–204. [Google Scholar] [CrossRef]
- Lubben, J. Assessing Social Networks Among Elderly Populations. Fam. Community Health 1988, 11, 42–52. [Google Scholar] [CrossRef]
- Lubben, J.; Gironda, M. Centrality of social ties to the health and well-being of older adults. In Social Work and Health Care in an Aging World; Springer Press: New York, USA, 2003; pp. 319–350. [Google Scholar]
- Lubben, J.; Blozik, E.; Gillmann, G.; Iliffe, S.; Kruse, W.; Beck, J.; Stuck, A. Performance of an Abbreviated Version of the Lubben Social Network Scale Among Three European Community-Dwelling Older Adult Populations. Gerontologist 2006, 46, 503–513. [Google Scholar] [CrossRef] [Green Version]
- Lubben Social Network Scale. Available online: https://www.bc.edu/content/bc-web/schools/ssw/sites/lubben/description.html (accessed on 28 September 2021).
- Steptoe, A.; Shankar, A.; Demakakos, P.; Wardle, J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc. Natl. Acad. Sci. USA 2013, 110, 5797–5801. [Google Scholar] [CrossRef] [Green Version]
- Russell, D.; Peplau, L.; Cutrona, C. The Revised UCLA Loneliness Scale: Concurrent and discriminate validity evidence. J. Personal. Soc. Psychol. 1980, 39, 472–480. [Google Scholar] [CrossRef]
- Hughes, M.; Waite, L.; Hawkley, L.; Cacioppo, J. A Short Scale for Measuring Loneliness in Large Surveys: Results from Two Population-Based Studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef]
- Weiss, R.S. Loneliness: The Experience of Emotional and Social Isolation; The MIT Press: Cambridge, MA, USA, 1973; Volume 22. [Google Scholar]
- Gierveld, J.; Kamphuis, F.H. The development of a Rasch-type loneliness scale. Appl. Psychol. Meas. 1985, 9, 289–299. [Google Scholar] [CrossRef]
- Gierveld, J.; van Tilburg, T. A 6-Item Scale for Overall, Emotional, and Social Loneliness Confirmatory Tests on Survey Data. Res. Aging 2006, 28, 582–598. [Google Scholar] [CrossRef] [Green Version]
- Zhu, V.; Lenert, L.; Bunnell, B.; Obeid, J.; Jefferson, M.; Hughes-Halbert, C. Automatically identifying social isolation from clinical narratives for patients with prostate Cancer. BMC Med. Inform. Decis. Mak. 2019, 19, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Domènech-Abella, J.; Mundó, J.; Haro, J.M.; Rubio-Valera, M. Anxiety, depression, loneliness and social network in the elderly: Longitudinal associations from The Irish Longitudinal Study on Ageing (TILDA). J. Affect. Disord. 2018, 246, 82–88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holt-Lunstad, J.; Smith, T.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rapport Petits Frères des Pauvres: Isolement des Personnes âgées: Les Effets du Confinement l’Isolement de nos Aînés est une Vraie Distanciation Sociale; Petits Frères des Pauvre: Paris, France, 2020.
- Gale, C.; Westbury, L.; Cooper, C. Social isolation and loneliness as risk factors for the progression of frailty. Age Ageing 2017, 47, 392–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medicare Spends More on Socially Isolated Older Adults. Available online: https://www.aarp.org/ppi/info-2017/medicare-spends-more-on-socially-isolated-older-adults.html (accessed on 28 September 2021).
- Huynh, S.; Tan, H.P.; Lee, Y. Towards Unobtrusive Mental Well-Being Monitoring for Independent-Living Elderly. In Proceedings of the 4th International on Workshop on Physical Analytics, Niagara Falls, NY, USA, 19–23 June 2017; pp. 1–6. [Google Scholar]
- Barsocchi, P.; Cesta, A.; Cortellessa, G.; Palumbo, F. Monitoring User Position in the GiraffPlus AAL Environment. In Proceedings of the IEEE International Instrumentation and Measurement Technology Conference (I2MTC), Pisa, Italy, 11–14 May 2015. [Google Scholar]
- Lussier, M.; Couture, M.; Moreau, M.; Laliberté, C.; Giroux, S.; Pigot, H.; Gaboury, S.; Bouchard, K.; Belchior, P.; Bottari, C.; et al. Integrating an Ambient Assisted Living monitoring system into clinical decision-making in home care: An embedded case study. Gerontechnology 2020, 19, 77–92. [Google Scholar] [CrossRef]
- Gochoo, M.; Tan, T.H.; Yeh, W.C.; Liu, S.H.; Alnajjar, F. DCNN-based elderly activity recognition using binary sensors. In Proceedings of the International Conference on Electrical and Computing Technologies and Applications (ICECTA), Ras Al Khaimah, United Arab Emirates, 21–23 November 2017; pp. 1–5. [Google Scholar]
- Dawadi, P.; Cook, D.; Schmitter-Edgecombe, M. Automated Cognitive Health Assessment from Smart Home-Based Behavior Data. IEEE J. Biomed. Health Inform. 2015, 20, 1188–1194. [Google Scholar] [CrossRef] [Green Version]
- Ngankam, H.; Pigot, H.; Lorrain, D.; Viens, I.; Giroux, S. Context awareness architecture for ambient-assisted living applications: Case study of nighttime wandering. J. Rehabil. Assist. Technol. Eng. 2020, 7, 2055668319887864. [Google Scholar]
- Pinard, S.; Bottari, C.; Laliberté, C.; Pigot, H.; Olivares, M.; Couture, M.; Giroux, S.; Bier, N. Design and usability evaluation of COOK, an assistive technology for meal preparation for persons with severe TBI. Disabil. Rehabil. Assist. Technol. 2019, 16, 687–701. [Google Scholar] [CrossRef] [PubMed]
- Pirzada, P.; White, N.; Wilde, A. Sensors in Smart Homes for Independent Living of the Elderly. In Proceedings of the 5th International Multi-Topic ICT Conference (IMTIC), Jamshoro, Pakistan, 25–27 April 2018; pp. 1–8. [Google Scholar]
- Ghosh, A.; Sanyal, A.; Chakraborty, A.; Sharma, P.; Saha, M.; Nandi, S.; Saha, S. On automatizing recognition of multiple human activities using ultrasonic sensor grid. In Proceedings of the 9th International Conference on Communication Systems and Networks (COMSNETS), Bengaluru, India, 4–8 January 2017; pp. 488–491. [Google Scholar]
- Seint, P.; Zin, T.; Yokota, M. Medication and Meal Intake Monitoring using Human-Object Interaction. In Proceedings of the IEEE 7th Global Conference on Consumer Electronics (GCCE), Nara, Japan, 9–12 October 2018; pp. 399–400. [Google Scholar]
- Park, S.; Kautz, H. Hierarchical recognition of activities of daily living using multi-scale, multi-perspective vision and RFID. 2008 IET 4th International Conference on Intelligent Environments, Seattle, WA, USA, 21–22 July2008; pp. 1–4. [Google Scholar] [CrossRef] [Green Version]
- Cippitelli, E.; Gasparrini, S.; Gambi, E.; Spinsante, S. Unobtrusive intake actions monitoring through RGB and depth information fusion. In Proceedings of the IEEE 12th International Conference on Intelligent Computer Communication and Processing (ICCP), Cluj-Napoca, Romania, 8–10 September 2016; pp. 19–26. [Google Scholar]
- Computer Vision-Based Descriptive Analytics of Seniors’ Daily Activities for Long-Term Health Monitoring. Available online: https://static1.squarespace.com/static/59d5ac1780bd5ef9c396eda6/t/5b7373254ae23704e284bdf4/1534292778467/18.pdf (accessed on 28 September 2021).
- Vuegen, L.; Van Den Broeck, B.; Karsmakers, P.; Van Hamme, H.; Vanrumste, B. Monitoring activities of daily living using Wireless Acoustic Sensor Networks in clean and noisy conditions. In Proceedings of the 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4966–4969. [Google Scholar]
- Hamad, R.; Salguero, A.; Bouguelia, M.R.; Espinilla, M.; Medina, J. Efficient Activity Recognition in Smart Homes Using Delayed Fuzzy Temporal Windows on Binary Sensors. IEEE J. Biomed. Health Inform. 2019, 24, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Ueda, K.; Tamai, M.; Yasumoto, K. A method for recognizing living activities in homes using positioning sensor and power meters. In Proceedings of the IEEE International Conference on Pervasive Computing and Communication Workshops (PerCom Workshops), St. Louis, MO, USA, 23–27 March 2015; pp. 354–359. [Google Scholar]
- Belley, C.; Gaboury, S.; Bouchard, B.; Bouzouane, A. Nonintrusive System for Assistance and Guidance in Smart Homes Based on Electrical Devices Identification. Expert Syst. Appl. 2015, 42, 6552–6577. [Google Scholar] [CrossRef]
- Fortin-Simard, D.; Bilodeau, J.S.; Gaboury, S.; Bouchard, B.; Bouzouane, A. Method of Recognition and Assistance Combining Passive RFID and Electrical Load Analysis That Handles Cognitive Errors. Int. J. Distrib. Sens. Netw. 2015, 11, 18. [Google Scholar] [CrossRef]
- Fortin-Simard, D.; Bilodeau, J.S.; Bouchard, K.; Gaboury, S.; Bouchard, B.; Bouzouane, A. Exploiting Passive RFID Technology for Activity Recognition in Smart Homes. IEEE Intell. Syst. 2015, 30, 7–15. [Google Scholar] [CrossRef]
- Tsang, W.H.; Qureshi, U.; Lam, K.Y.; Ng, K.Y.; Han, S.; Papavasileiou, I. Tracking Indoor Activities of Patients with Mild Cognitive Impairment Using Motion Sensors. In Proceedings of the IEEE 31st International Conference on Advanced Information Networking and Applications (AINA), Taipei, Taiwan, 27–29 March 2017. [Google Scholar]
- Charlon, Y.; Piau, A.; Brulin, D.; Campo, E. Design and Evaluation of a Connected Insole to Support Healthy Aging of Frail Patients at Home. Wirel. Sens. Netw. 2019, 11, 67–80. [Google Scholar] [CrossRef]
- Feng, Y.; Chang, C.K.; Chang, H. An ADL Recognition System on Smart Phone. In International Conference on Smart Homes and Health Telematics; Springer: Wuhan, China, 2016; pp. 148–158. [Google Scholar]
- Wearables Have a Dirty Little Secret: 50% of Users Lose Interest-TechRepublic. Available online: http://www.techrepublic.com/article/wearables-have-a-dirty-little-secret-most-people-lose-interest/ (accessed on 28 September 2021).
- miMonitor. Available online: https://www.mimonitor.co.uk/dementia (accessed on 28 September 2021).
- Just Checking. Available online: https://justchecking.co.uk (accessed on 28 September 2021).
- Canary Care. Available online: https://www.canarycare.co.uk/ (accessed on 28 September 2021).
- Kiwatch. Available online: https://www.kiwatch.com/offre-videosurveillance/maintien-domicile/surveillance (accessed on 28 September 2021).
- Teleassistance-Allovie. Available online: https://teleassistance-allovie.com/teleassistance/ (accessed on 28 September 2021).
- Reminder Rosie. Available online: https://smpltec.com/reminder-rosie (accessed on 28 September 2021).
- Mytrusense. Available online: https://mytrusense.com/ (accessed on 28 September 2021).
- Bouaziz, G.; Brulin, D.; Pigot, H.; Campo, E. Detection of Social Isolation Based on Meal-Taking Activity and Mobility of Elderly People Living Alone. In JETSAN 2021-Colloque en Télésanté et Dispositifs Biomédicaux, 8th ed.; Université Toulouse III-Paul Sabatier: Toulouse, France, 2021. [Google Scholar]
| Keywords | |
|---|---|
| Elderly people | Social isolation |
| Elderly monitoring | Loneliness |
| Smart home | Social Isolation in the elderly |
| Monitoring system | Limit social isolation |
| Health monitoring | Taking meals |
| User behavior | Monitor eating in elderly |
| Elderly People Living Alone | Eating Activity |
| Activity recognition | Non-intrusive sensor |
| Activity daily living | Unobtrusive sensors |
| Changing behavior in elderly | Wireless sensor |
| Monitor mobility in elderly | User privacy |
| Daily mobility | Smart sensing |
| Nutrition | Malnutrition |
| Keywords | Web of Science | PubMed | IEEE Xplore |
|---|---|---|---|
| Monitor elderly | 8700 | 120,291 | 2998 |
| Elderly monitoring system | 3545 | 22,742 | 2421 |
| Monitoring technology | 213,286 | 95,162 | 116,056 |
| Long term elderly monitor | 891 | 8858 | 205 |
| Smart home | 15,545 | 1101 | 13,497 |
| Monitoring system | 345,087 | 131,532 | 189,744 |
| Health monitoring | 256,174 | 177,388 | 31,965 |
| Monitoring technology | 213,286 | 95,162 | 116,056 |
| User behavior | 82,881 | 16,103 | 28,829 |
| Elderly People Living Alone | 877 | 4449 | 229 |
| Activity recognition | 56,194 | 49,094 | 12,687 |
| Activity daily living | 29,382 | 64,711 | 2589 |
| Changing behavior in elderly | 2333 | 91,998 | 117 |
| Unobtrusive Activity Recognition | 202 | 54 | 133 |
| Mobility in smart house | 140 | 12 | 62 |
| Monitor mobility in elderly | 372 | 1377 | 156 |
| Daily mobility | 8180 | 7926 | 1018 |
| Daily mobility in elderly | 1073 | 5135 | 86 |
| Social isolation | 17,026 | 17,947 | 538 |
| Loneliness | 10,501 | 5321 | 125 |
| Social Isolation in the elderly | 741 | 6711 | 42 |
| Limit social isolation | 1661 | 2144 | 39 |
| Limit social isolation in elderly | 71 | 850 | 1 |
| Taking meals | 4227 | 514 | 194 |
| Monitor eating in elderly | 66 | 1027 | 20 |
| Eating Activity | 16,859 | 18,186 | 346 |
| Eating Activity in elderly | 321 | 5266 | 21 |
| Nutrition in elderly | 10,593 | 9044 | 33 |
| Malnutrition in elderly | 2314 | 1893 | 6 |
| Smart sensing | 21,915 | 2694 | 13,830 |
| Non-intrusive sensor | 1186 | 173 | 898 |
| Unobtrusive sensors | 1296 | 529 | 1112 |
| Wireless sensor | 89,018 | 6251 | 116,392 |
| User privacy | 24,957 | 1109 | 18,278 |
| User acceptance | 17,489 | 4621 | 4199 |
| User satisfaction | 19,825 | 3240 | 6434 |
| Elderly monitoring data processing | 623 | 3860 | 576 |
| Elderly monitoring big data | 119 | 203 | 79 |
| Elderly monitoring data mining | 91 | 227 | 95 |
| Elderly monitoring machine learning | 252 | 747 | 273 |
| Elderly monitoring artificial intelligence | 177 | 1065 | 414 |
| Metropolitan France | Rural Communities | Small Cities * | Medium Cities * | Large Provincial Cities * | Parisian Agglomeration | |
|---|---|---|---|---|---|---|
| Occasional loneliness | 27% | 25% | 31% | 24% | 28% | 27% |
| Frequent loneliness | 9% | 7% | 12% | 8% | 7% | 10% |
| Leave home daily | 60% | 50% | 57% | 58% | 64% | 73% |
| Use public transport every week | 18% | 5% | 5% | 10% | 28% | 48% |
| Spend whole days without talking to anyone | 19% | 21% | 20% | 19% | 18% | 18% |
| Regularly invite each other to their homes | 52% | 56% | 50% | 53% | 50% | 49% |
| Lack of solidarity where they live | 31% | 27% | 32% | 30% | 32% | 37% |
| Sensor | Source | Position | Parameter Obtained | Advantages | Drawbacks |
|---|---|---|---|---|---|
| PIR | Huynh et al. [55] | PIR in every room | Detection of movement in each room | Low cost system Preserve privacy | Not able to distinguish who is moving if there is more than one person living in the same house |
| Barsocchi et al. [56] | PIR in every room | Detection of movement in each room | |||
| Lussier et al. [57] | Two PIR sensors in the bedroom (one directed at the bed and another one towards the space between the exit and the bed) and one in the rest of each room | Detection of movement in different positions inside the house and the act of going out | |||
| Gochoo et al. [58] | 31 PIR sensors in different locations around the house 4 Reed switch | Detection of movement in different positions inside the house | |||
| Dawadi et al. [59] | 23 PIR sensors in different locations in the house | Detection of movement in different positions inside the house and the act of going out | |||
| Kenfack Ngankam et al. [60] | 11 PIR sensors | Detection of movement in each room | |||
| Pinard et al. [61] | PIR sensors in each room and some around the stove | Detection of movement around the oven | |||
| Reed switch | Huynh et al. [55] | Reed switch in outer door | Detection of the act of going out | Low cost system, preserve privacy | Not able to determine who is using the items if there is more than one person living in the same house |
| Barsocchi et al. [56] | Reed switch in outer door, refrigerator and the door of the bedroom | Detection of the act of going out and the use of the refrigerator | |||
| Lussier et al. [57] | Reed switch in outer door, drawer, wardrobe, refrigerator, utensil drawer, kitchen cabinet, and food storage cabinet | Detection of the act of going out and the use of the drawer, wardrobe, the refrigerator, the utensil drawer, the kitchen cabinet, and the food storage cabinet | |||
| Gochoo et al. [58] | 4 door sensors (back door, garage door, front door and pantry) | Detection of the act of going out and the use of the pantry | |||
| Dawadi et al. [59] | 6 reed switches in different locations in the house | Detection of the act of going out and the use of different items in the kitchen | |||
| Kenfack Ngankam et al. [60] | 13 Reed switch sensors in different locations in the house | Detection of the act of going out and the use of different items in the house | |||
| Pinard et al. [61] | 2 reed switch sensors for oven door aperture and the outer door | Detection of the act of going out and the use of the oven | |||
| Pirzada et al. [62] | 40 to 50 reed switch sensors in different locations in the house | Detection of the act of going out and the use of different items in the house | |||
| Ultrasonic | Ghosh et al. [63] | The board fitted with 5 ultrasonic sensors has been suspended from the ceiling | Detection of body movements | Highly accurate sensing distance | |
| Video camera | Seint et al. [64] | Camera in front of the monitored person (tests realized in the laboratory) | Video of the monitored person | Provide rich information | Sensitive to light Do not preserve privacy |
| Park et al. [65] | Two wide field-of-view (FOV) cameras and two narrow FOV cameras | ||||
| Kinect sensor | Cippitelli et al. [66] | Kinect sensor (RGB and depth camera) has been suspended from the ceiling | Color and depth streams | Provide rich information Robust to light variation | Do not preserve privacy |
| Depth sensor and thermal sensor | Zelun et al. [67] | Depth sensor and thermal sensor has been suspended from the ceiling | Depth and thermal streams | Robust to light variation | Expensive system |
| Pressure | Barsocchi et al. [56] | Pressure-sensitive mats in the bed and the chair | Presence of the person in the bed and chair | Easy to install Provide accurate information | Not able to determine who is moving if there is more than one person living in the same house |
| Kenfack Ngankam et al. [60] | 3 Pressure sensors: bed, sofa and chair | Presence of the person in the bed, sofa and chair | |||
| Pinard et al. [61] | 4 Pressure sensors for 4 burners of the stove (to detect objects placed on burners) | Presence of objects placed on burners | |||
| Microphone | Vuegen et al. [68] | 7 nodes (each node composed of 3 microphones) in bedroom, bathroom, toilet, oven, table of the kitchen and 2 in the living room | Audio recording | Provide rich information | Do not preserve privacy |
| Flowmeters | Pinard et al. [61] | Flowmeters on the tap of the kitchen | The use of the kitchen faucet | Provide accurate information | Not able to determine who is moving if there is more than one person living in the same house Expensive |
| Float switch | Rebeen et al. [69] | Float switch in the toilet | Measure the toilet being flushed | ||
| Wattmeter | Barsocchi et al. [56] | Wattmeter in the water boiler or oven | Using the water boiler or oven | Provide accurate information | Not able to determine who is moving if there is more than one person living in the same house |
| Kenfack Ngankam et al. [60] | Wattmeter for the TV | The use of the TV | |||
| Pinard et al. [61] | 4 Wattmeter for 4 burners of the stove | The use of the 4 burners of the stove | |||
| Ueda et al. [70] | Two Wattmeters for the TV and the cooking heaters | The use of the TV and the cooking heaters | |||
| Power analyzer | Belley et al. [71] | Single power analyzer placed in the electric panel | The use of the TV and different electrical gadgets in the house (the 4 burners of the stove, the electric kettle, the oven, the toaster, the extractor hood, the coffee maker, the microwave oven, the hair dryer, the blender, the electric mixer, the stereo and the refrigerator) | Not able to determine who is moving if there is more than one person living in the same house Expensive sensor | |
| Fortin-Simard et al. [72] | Single power analyzer placed in the electric panel | The use of different electrical gadgets in the kitchen | |||
| Passive RFID | Fortin-Simard et al. [73] | Antennas Tags in different items of the kitchen (each object has a specific size, a type so it is associated with one or many RFID tags) | The use of different items of the kitchen | Provide accurate information | Expensive Difficult to install due to the number of tags that need to be installed on different items |
| Ultrasonic positioning sensor | Ueda et al. [70] | 19 receivers of the ultrasonic positioning sensor in different place in the house Ultrasonic positioning sensor attached to the body of the person | Location of the position of the person inside the house | Provide accurate information | Must be attached to the body Problem of battery duration |
| Active RFID | Park et al. [65] | Multiple RFID tags are attached to various objects including furniture, appliances, and utensils around the smart homes. Bracelet that contains the RFID reader | The use of different items of the kitchen | Provide accurate information | Must be attached to the body Problem of battery duration |
| Smartphone | Yunfei et al. [73] | Smartphone | Orientation of the phone head, light level around the phone, GPS and other functions such as step detector, accelerator and time stamp | Provide accurate information Easy to use Widespread between persons | Must be attached to the body Problem of battery duration Do not preserve privacy |
| Accelerometer | Tsang et al. [74] | Accelerometers | Body movement and posture | Low cost sensor | Must be attached to the body |
| Charlon et al. [75] | Smart insole (contain accelerometer) |
| Source | PIR | Reed Switch | Ultrasonic Sensor | Camera | Pressure Sensor | Microphone | Electrical Power Sensors | Flowmeter | Float Switch | RFID | Smartphone | Accelerometer |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Huynh et al. [55] | ✓ | ✓ | ||||||||||
| Barsocchi et al. [56] | ✓ | ✓ | ✓ | ✓ | ||||||||
| Lussier et al. [57] | ✓ | ✓ | ✓ | |||||||||
| Gochoo et al. [58] | ✓ | ✓ | ||||||||||
| Dawadi et al. [59] | ✓ | ✓ | ||||||||||
| Kenfack Ngankam et al. [60] | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Pinard et al. [61] | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||
| Pirzada et al. [62] | ✓ | |||||||||||
| Ghosh et al. [63] | ✓ | |||||||||||
| Seint et al. [64] | ✓ | |||||||||||
| Park et al. [65] | ✓ | ✓ | ||||||||||
| Cippitelli et al. [66] | ✓ | |||||||||||
| Zelun et al. [67] | ✓ | |||||||||||
| Vuegen et al. [68] | ✓ | |||||||||||
| Rebeen et al. [69] | ✓ | ✓ | ✓ | |||||||||
| Ueda et al. [70] | ✓ | ✓ | ||||||||||
| Belley et al. [71] | ✓ | |||||||||||
| Fortin-Simard et al. [72] | ✓ | ✓ | ||||||||||
| Fortin-Simard et al. [73] | ✓ | |||||||||||
| Yunfei et al. [76] | ✓ | |||||||||||
| Tsang et al. [74] | ✓ | |||||||||||
| Charlon et al. [75] | ✓ |
| Source | Algorithms or Software Involved | Outputs | Evaluation Metrics (%) | Labelled Data |
|---|---|---|---|---|
| Barsocchi et al. [56] |
| Detection of ADLs such as lunch/dinner, resting/pc/tv, sleeping and hygiene. | 81% sensitivity | Yes |
| Lussier et al. [57] |
| Detection of ADLs. Results showed that AAL monitoring technologies provide health professionals with information about seniors related to self-neglect such as malnutrition, deficient hygiene, lack of household chores, oversleeping, and social isolation. | No data available | No data available |
| Gochoo et al. [58] |
| Detection of four ADLs: bed to toilet movement, eating, preparation meals, and relaxing. DCNN classifier gives an average accuracy of 99.36%. | 99.36% accuracy | Yes |
| Dawadi et al. [59] |
| Detection of seven ADLs: sleep, bed to toilet movement, cooking, eating, relaxation, personal hygiene, and the mobility of the resident inside the home. There is a correlation between the predicted clinical assessment using activity behavior and the mobility scores provided by the clinician. | 95% accuracy | Yes |
| Pirzada et al. [60] |
| Detection of anomalies in patterns. | No data available | No data available |
| Ghosh et al. [63] |
| Detection of standing, sitting and falling. | 90% accuracy | Yes |
| Rebeen et al. [69] |
| Better results in recognition activities (eating, grooming, going out, showering, sleeping, saving time and going to the bathroom) when the recognition of the activity is delayed, preceding 1-min sensor activations with 5-min delays (20-min delay, 1-h delay, etc.) compared to considering only the 1-min delay sensor data. | CNN LSTM: 96.97% and 96.72% f1-score for the first and second database, respectively | Yes |
| Seint et al. [64] |
| Detection of medication and meal intake. | 90% accuracy for taking medication and 95% accuracy for taking meals | Yes |
| Cippitelli et al. [66] |
| Detection of eating and drinking actions. | 98.3% accuracy | Yes |
| Vuegen et al. [68] |
| Detection of brushing teeth, washing dishes, dressing, eating, preparing food, setting table, showering, sleeping, toileting and washing hands. | 78.6 ± 1.4% accuracy | Yes |
| Yunfei et al. [72] |
| Detection of 6 ADLs: working on a desktop PC in the bedroom, wandering walk, hygiene activities, cooking, washing dishes, and eating. | Between 92.35% and 99.17% accuracy for each of the four databases | Yes |
| Tsang et al. [74] |
| Recognition of five indoor activities: sleeping, watching TV, toileting, cooking and eating. All other activities including outdoor activities are assigned to “others”. | 99.8% accuracy | Yes |
| Park et al. [65] |
| Recognition of six activities: walking around, sitting and watching TV, preparing a utensil, storing utensil, preparing cereal and drinking water. | 83% mean accuracy for all activities | Yes |
| Ueda et al. [70] |
| Recognition of six different activities: watching TV, taking a meal, cooking, reading a book, washing dishes, and others. | 85% accuracy | Yes |
| Source | Number of Participants | Duration of Data Collection | Gender | Age | Health Status of the Participants | Type of Home Where Test Was Done |
|---|---|---|---|---|---|---|
| Huynh et al. [55] | 43 | 6 months | 19 males, 24 females | Mean age 77.59 and standard deviation 7.65 | No data available | Apartment |
| Barsocchi et al. [56] | 1 | 10 days | One female | No data available | No data available | GIRAFFPLUS test site |
| Lussier et al. [57] | 3 | 1 month | One female, two males |
| Numerous health issues for each person |
|
| Gochoo et al. [58] | 1 | 21 months | One female | No data available | Healthy person, | Laboratory Smart home |
| Dawadi et al. [59] | 18 | 2 years | 5 females, 13 males | (M = 84.71, SD = 5.24, range 73−92) | cognitively healthy (N = 7), at risk for cognitive difficulties (N = 6), and experiencing cognitive difficulties (N = 5) | Laboratory Smart home |
| Kenfack Ngankam et al. [60] | 1 | 6 weeks | One female | 78-year-old | Moderate cognitive impairment | Apartment |
| Pinard et al. [61] | 3 | 6 months | Three males | Ages range from 39 to 57 | Sustained severe traumatic brain injury | Individual apartment in the supported-living residence |
| Pirzada et al. [62] | 2 | 14 days | No data available | No data available | No data available | Apartment |
| Ghosh et al. [63] | 10 | 100 samples for each | No data available | No data available | No data available | Laboratory Smart home |
| Seint et al. [64] | Different persons | 10 sequences | No data available | No data available | No data available | Laboratory Smart home |
| Park et al. [65] | 5 | Each person does five repetitions per activity in two sessions | No data available | No data available | No data available | Laboratory Smart home |
| Cippitelli et al. [66] | 35 | 48 sequences | No data available | 22 − 38 years | No data available | Laboratory Smart home |
| Vuegen et al. [68] | 2 | Multiple samples of 10 different activities | No data available | No data available | No data available | Apartment |
| Rebeen et al. [69] | 2 | (1) 14 days (2) 22 days | No data available | No data available | No data available | Apartment |
| Ueda et al. [70] | 2 | 3 days | One male | In their twenties | No data available | Laboratory Smart home |
| Belley et al. [71] | 1 | 10 consecutive tests for different selected sequences of tasks | No data available | No data available | No data available | Laboratory Smart home |
| Fortin-Simard et al. [72] | 1 | Five different ADLs performed 25 times | No data available | No data available | No data available | Laboratory Smart home |
| Fortin-Simard et al. [73] | 1 | Five different ADLs performed 25 times | No data available | No data available | No data available | Laboratory Smart home |
| Yunfei et al. [76] | 4 | No data available | No data available | No data available | No data available | Apartment |
| Tsang et al. [74] | 1 | Different samples | No data available | No data available | No data available | Apartment |
| Charlon et al. [75] | 9 | Use of smart insole for half hour for each participant | Six males, three females | Mean age was 70.1 years (65 to 75) | healthy | Laboratory Smart home |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouaziz, G.; Brulin, D.; Campo, E. Technological Solutions for Social Isolation Monitoring of the Elderly: A Survey of Selected Projects from Academia and Industry. Sensors 2022, 22, 8802. https://doi.org/10.3390/s22228802
Bouaziz G, Brulin D, Campo E. Technological Solutions for Social Isolation Monitoring of the Elderly: A Survey of Selected Projects from Academia and Industry. Sensors. 2022; 22(22):8802. https://doi.org/10.3390/s22228802
Chicago/Turabian StyleBouaziz, Ghazi, Damien Brulin, and Eric Campo. 2022. "Technological Solutions for Social Isolation Monitoring of the Elderly: A Survey of Selected Projects from Academia and Industry" Sensors 22, no. 22: 8802. https://doi.org/10.3390/s22228802






