A Care Robot with Ethical Sensing System for Older Adults at Home
Abstract
1. Introduction
2. Related Work
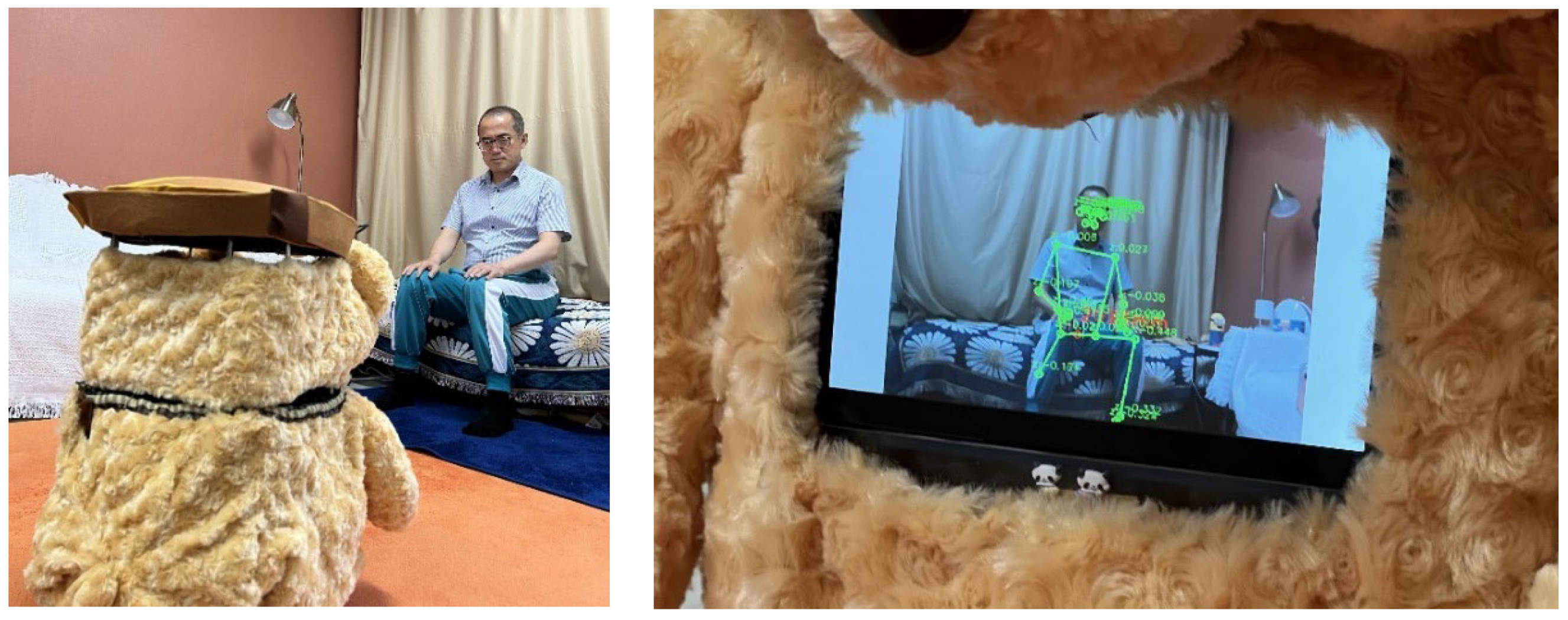
3. Designing of a Care Robot with Ethical Sensing of Human Poses
3.1. Participants and Method
3.2. Selection of Services Based on RST
- Service introduction: provide service items, basic settings, and usage guidelines
- Cognitive activities: provide quiz games based on calculation, word memory, etc., for cognitive enhancement
- Emotional activities: offer activities involving questions about user’s childhood or photos or singing along with familiar songs from their memory to counter loneliness and promote positive emotions
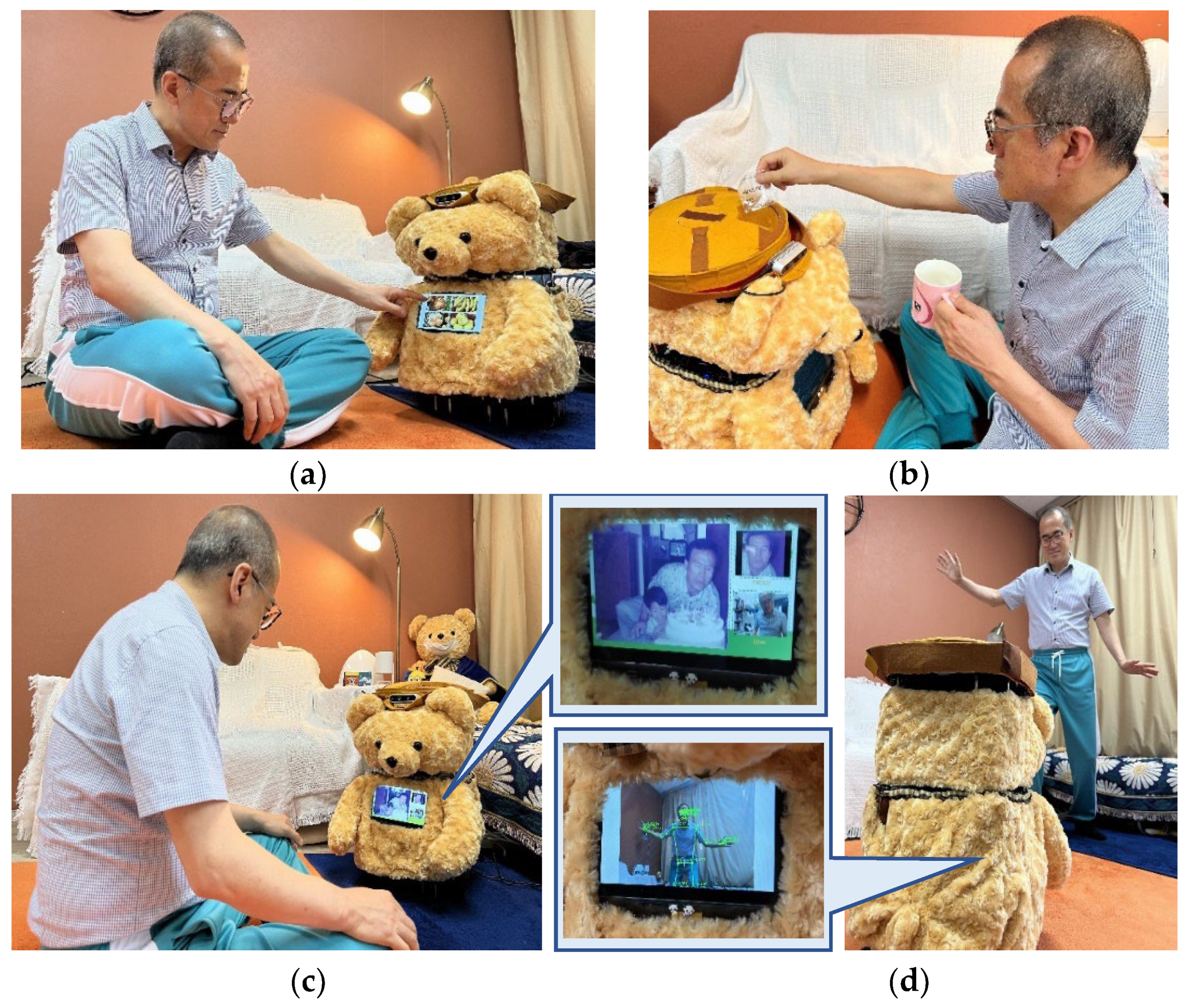
- Physical activities: offer games that detect movement of user’s body (arms and legs; e.g., the red light, green light game), or detect eating, falling, sleeping, etc.
- Medication instruction: detect, recognize, and approach user, tell them it is time to take their medication, and present the medication
- Caregiver management: keep nurse’s notes for regular caregiver to review health care information, check living environment, provide summary of health information check, and alert guardians if necessary
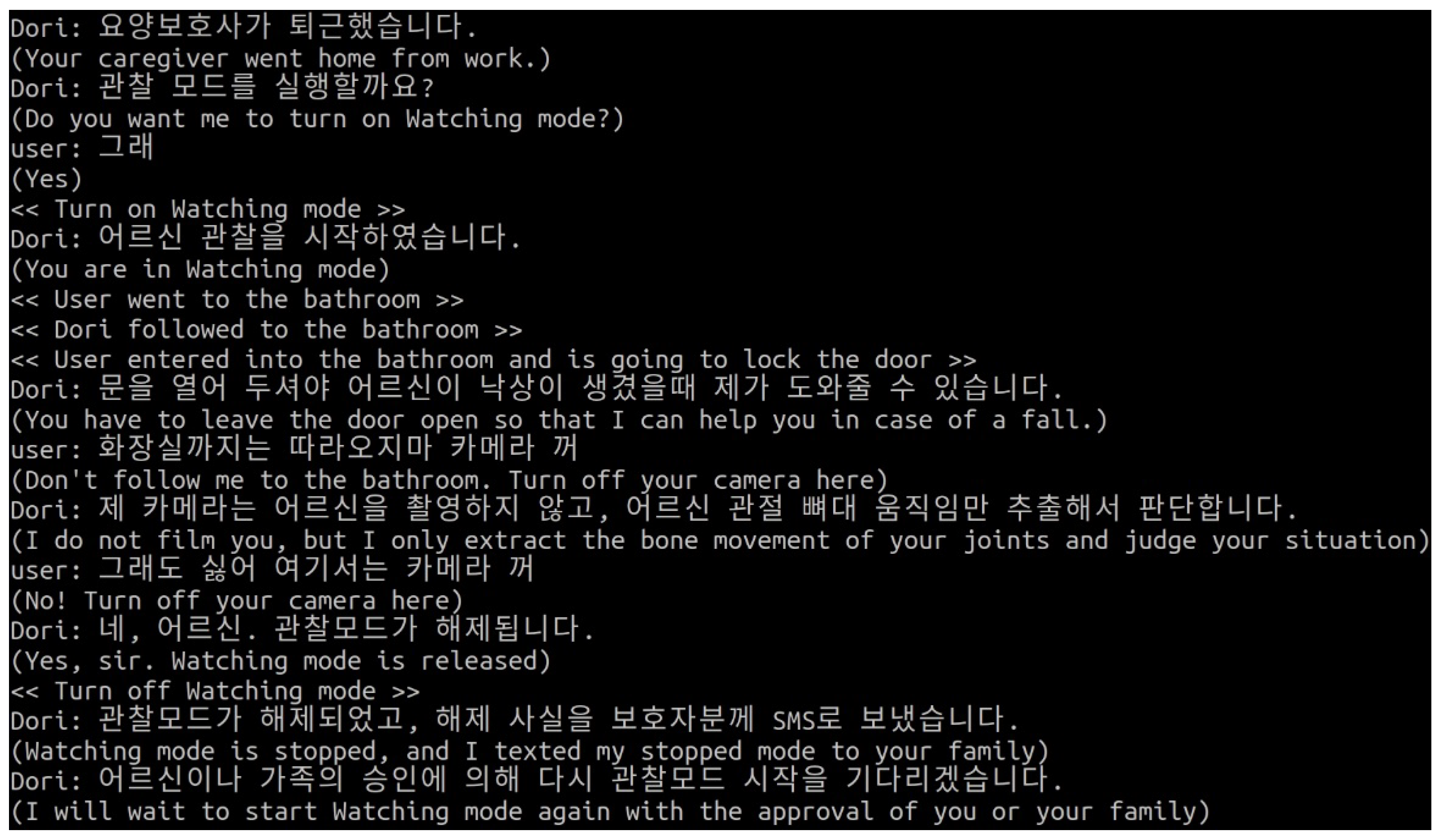
3.3. Service Design of Ethical Sensing
- Dilemma 1—Physical activities: Mr. A has nearly fallen twice recently. Therefore, he leaves the bathroom door open and allows the care robot to monitor him. However, Mr. A does not want to let the care robot monitor him while he takes off his clothes in the bathroom. Should he stop or continue the care robot’s body image sensing when he is in the bathroom?
- Dilemma 2—Medication management: Mr. K has been suffering from excessive sleepiness whenever he takes his lunchtime medication. Due to this, he does not want to take his lunchtime medication today and ignores the instructions of the care robot. The care robot continues to hover around Mr. K when he does not take the medicine and to instruct him to take it. Should he stop or continue the care robot’s medication management?
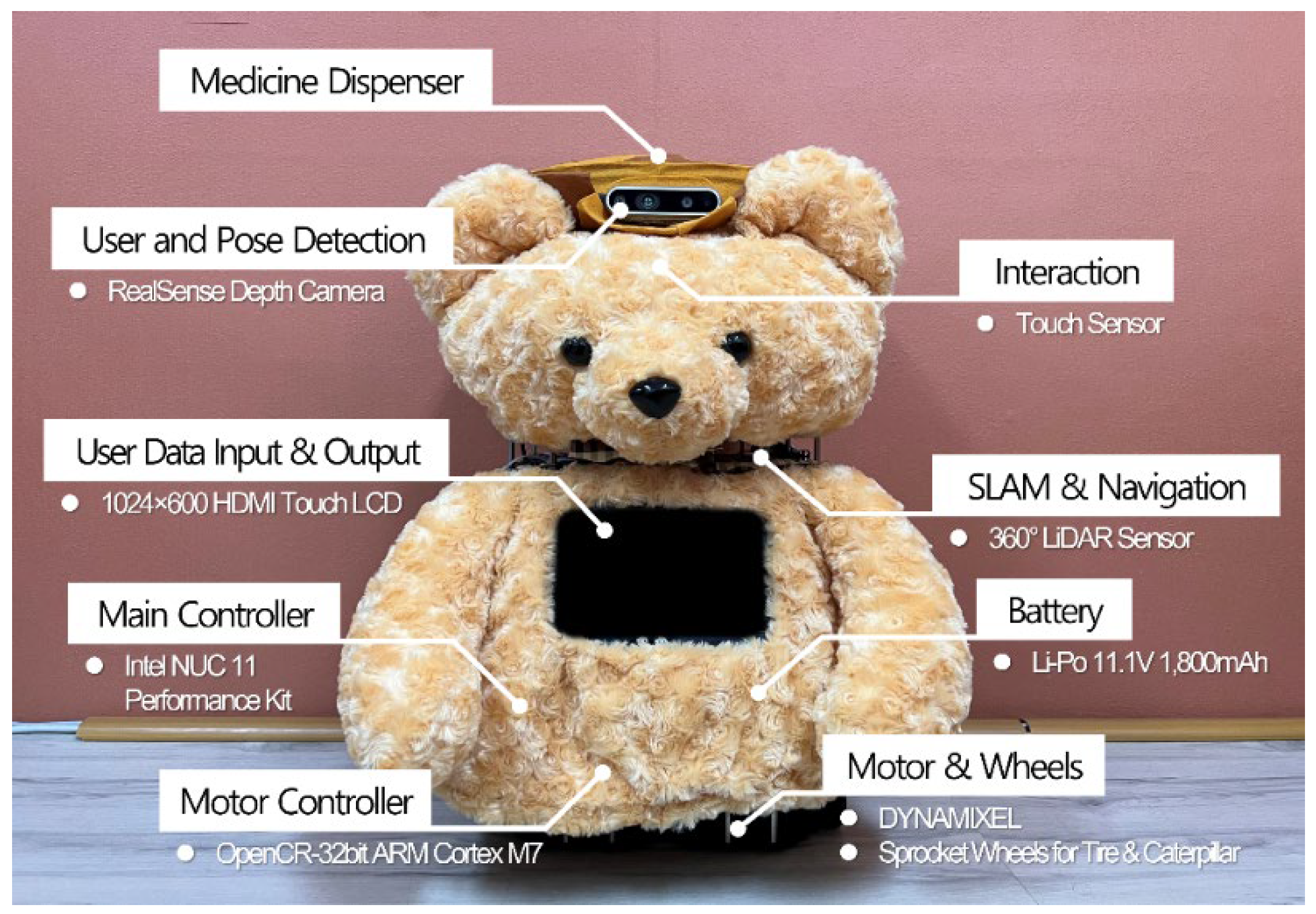
4. Development
4.1. Robot Development Environment
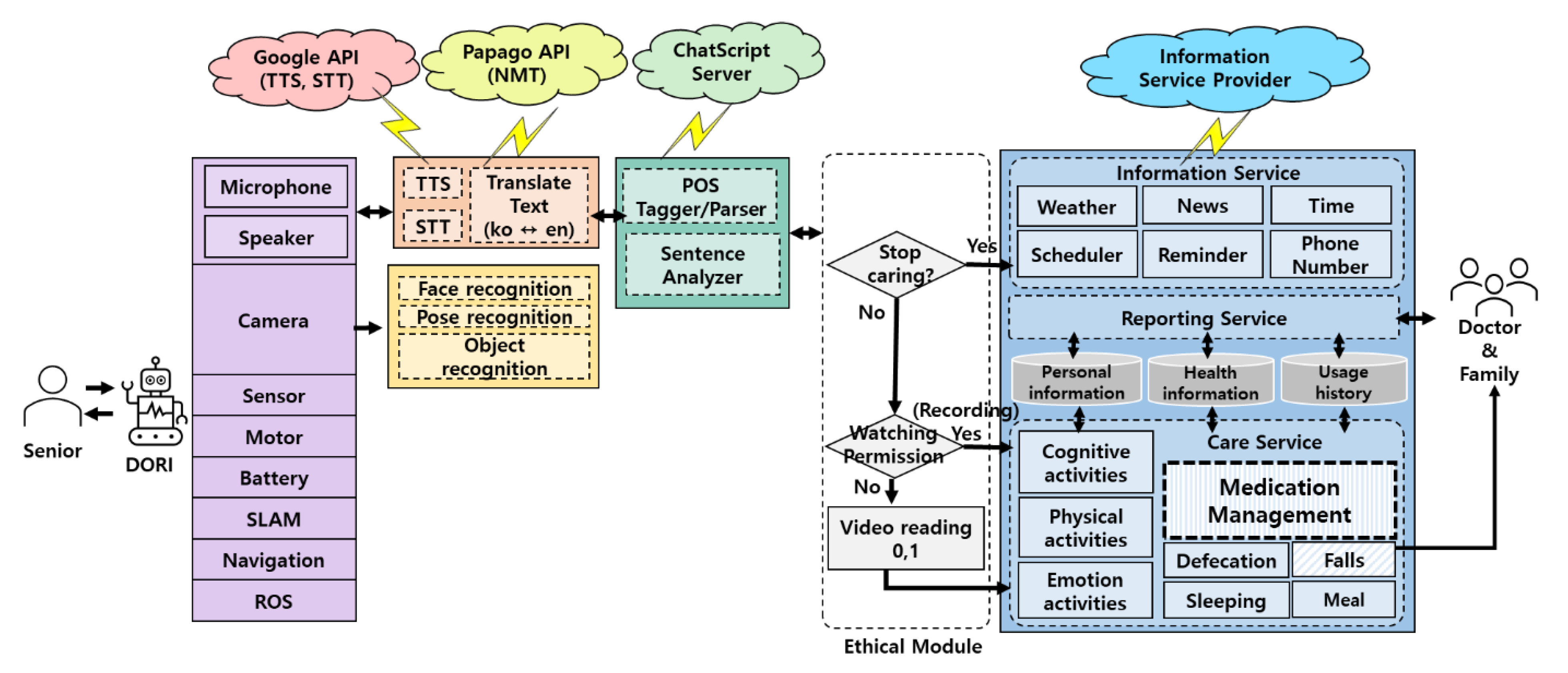
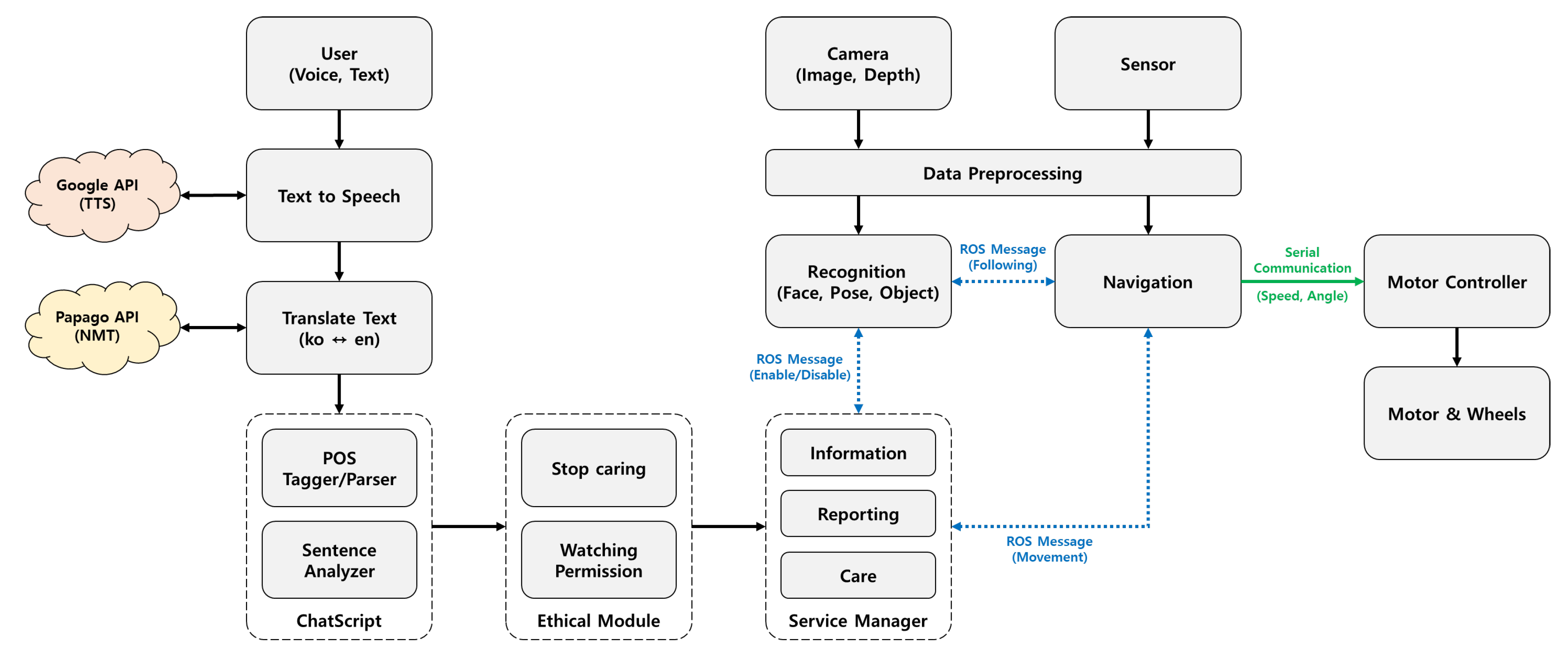
4.2. Software Architecture
- System input/output unit: modules that handle robot drive and input data from the robot’s microphone, camera, and various sensors;
- Voice and image recognition unit: module that processes STT (Speech-to-Text) and TTS (Text-to-Speech) using Google Assistant APIs [24] through microphones and speakers, and translates English to Korean through Papago NMT (Neural Machine Translation) [25]; face recognition uses the camera and OpenFace [26], pose recognition uses MediaPipe Pose [27], and object recognition uses SSD-MobileNet [28];
- Chatbot processing unit: module using ChatScript for part-of-speech tagging, parsing, and parse analysis according to service scenarios;
- Service setting unit: elderly-controlled control module that allows the halting of care services containing personal information and that allows only video recognition processing when monitoring;
- Service content: information services (e.g., weather, news, time, schedule, reminders, phone numbers), care services (e.g., cognitive, emotional, physical, medication management, meal checks, fall detection), and reporting services (interactions with older users and health care information); care services can be stopped in the service setting unit; reporting service is monitored by caregivers;
4.3. Care Services Based on HCAI and Human Values
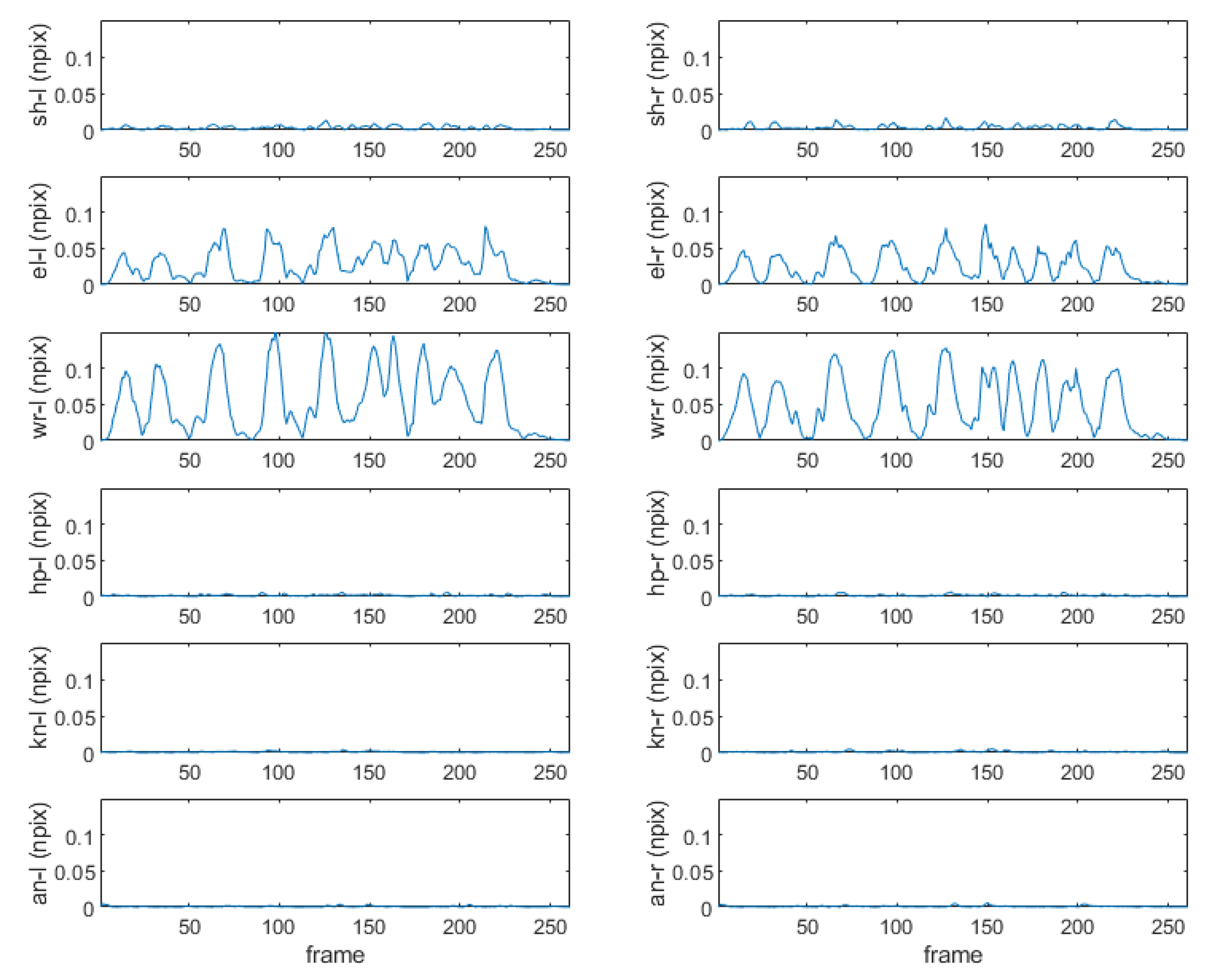
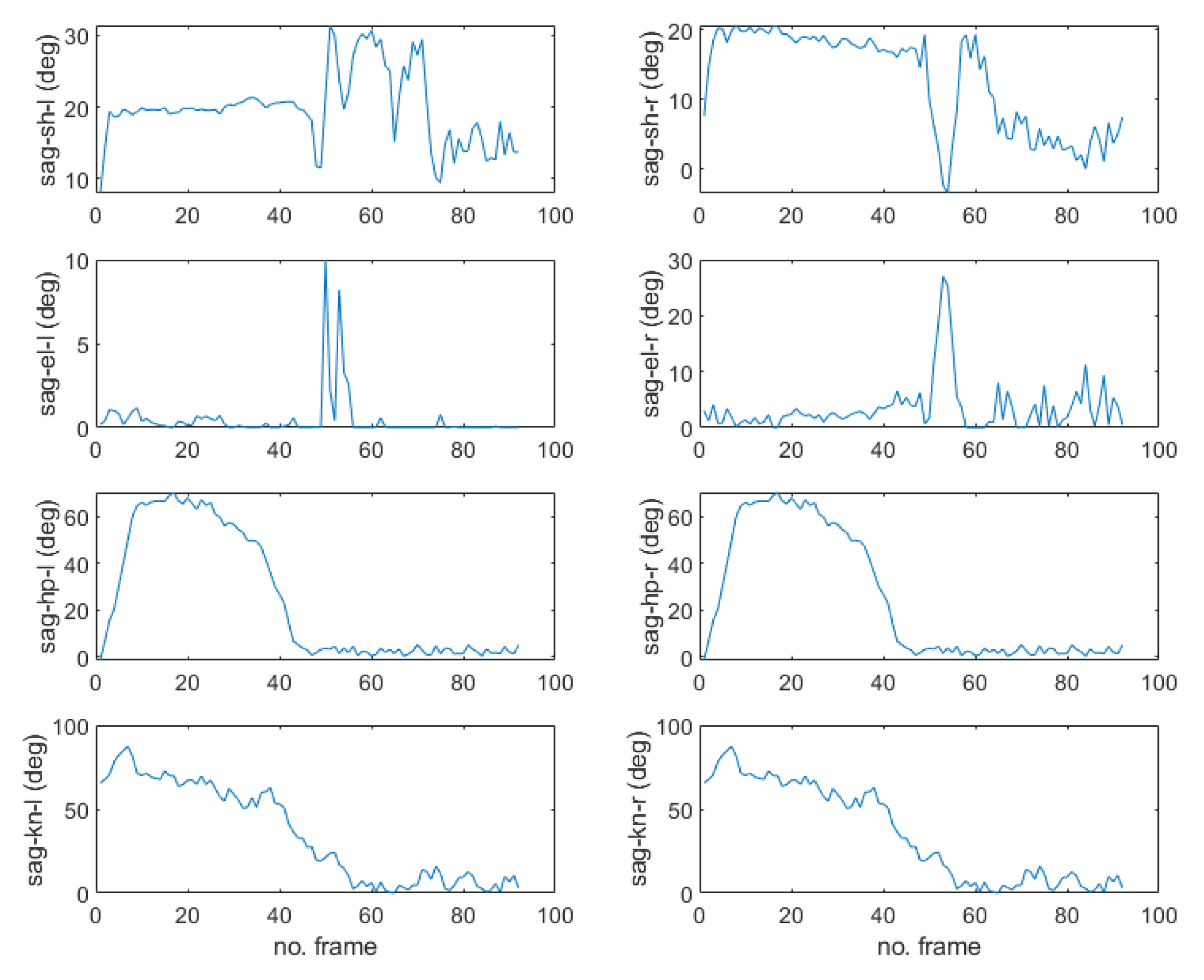
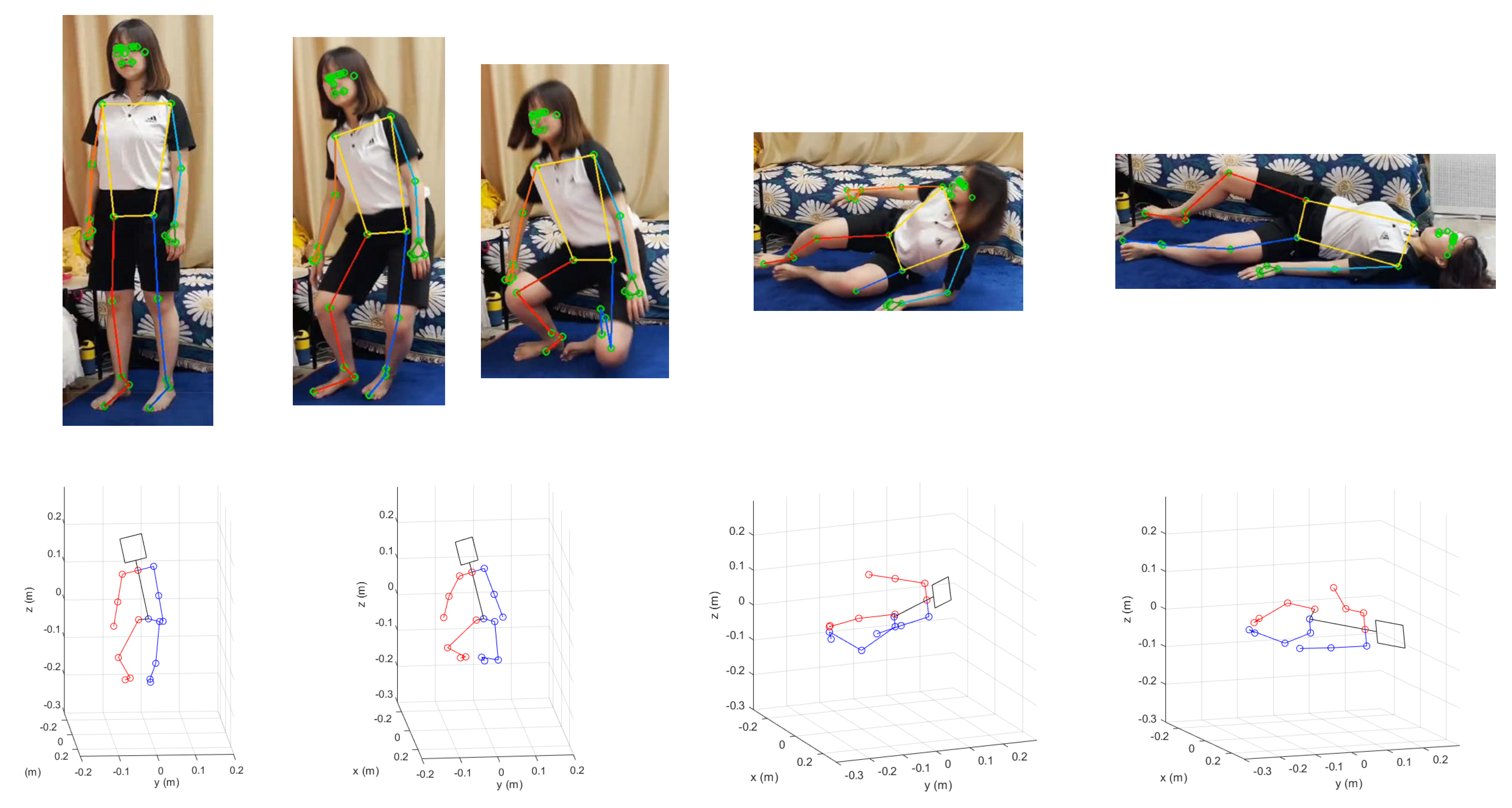
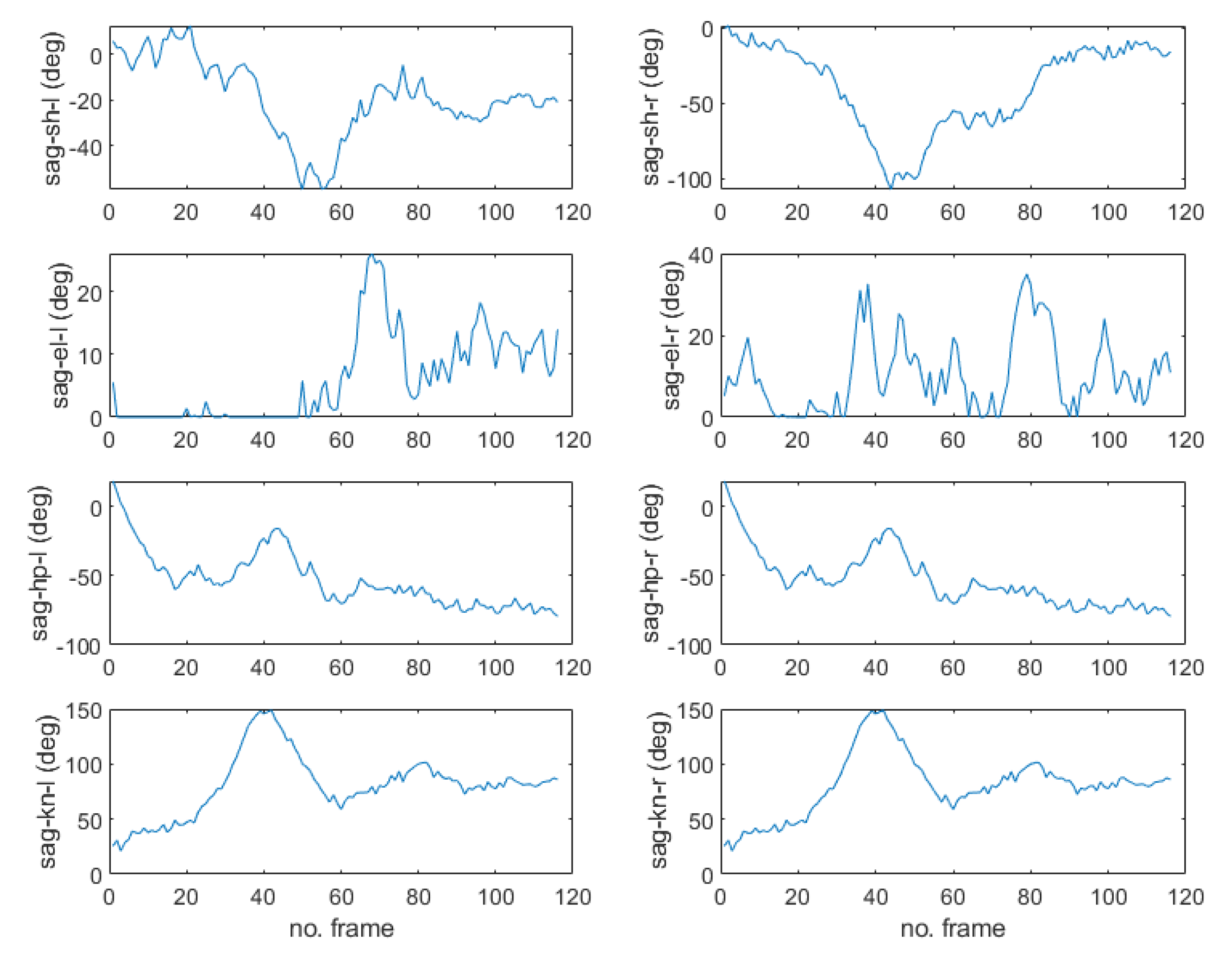
- Step 1. Acquire images from camera with the image grabber module of Dori.
- Step 2. Extract 2D pixel coordinates of the 17 landmarks for the captured human body images of each frame by executing MPP.
- Step 3. Analyze the joint movement according to the change in normalized pixel coordinates by checking whether any of the current joint positions has moved above the normalized pixel distance threshold compared to the average position of the previous 4 frames.
- Step 4. If any joint of the frail older adult has changed during the red light-green light game or the whole body is moved as a result of Step 3, the information is sent to the Dori’s Care Service module shown in Figure 3.
- Step 5. If the current image frame is the last one or the termination condition is met, stop the motion detection process. Otherwise, go to Step 1.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- McGinn, C.; Bourke, E.; Murtagh, A.; Donovan, C.; Cullinan, M.F. Meeting Stevie: Perceptions of a socially assistive robot by residents and staff in a long-term care facility. In Proceedings of the 14th ACM/IEEE International Conference on Human-Robot Interaction (HRI), Daegu, Korea, 11–14 March 2019; pp. 602–603. [Google Scholar]
- Grube, M.M.; Möhler, R.; Fuchs, J.; Gaertner, B.; Scheidt-Nave, C. Indicator-based public health monitoring in old age in OECD member countries: A scoping review. BMC Public Health 2019, 19, 1068. [Google Scholar] [CrossRef] [PubMed]
- Oh, E.; SeolHwa, M.; Gwi-Ryung, S.H. Longitudinal changes in frailty prevalence and related factors in older adults living in long-term care facilities. Adv. Nurs. 2020, 76, 1679–1690. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, A.; Nåden, D.; Karterud, D. Robots in elder care: Some ethical questions. Nurs. Eth. 2016, 23, 369–371. [Google Scholar] [CrossRef] [PubMed]
- Park, C.; Kang, S.; Kim, J.; Oh, J. A study on service robot system for elder care. In Proceedings of the 9th International Conference on Ubiquitous Robots and Ambient Intelligence (URAI), Daejeon, Korea, 26–28 November 2012; pp. 546–547. [Google Scholar]
- Coco, K.; Kangasniemi, M.; Rantanen, T. Care personnel’s attitudes and fears toward care robots in elderly care: A comparison of data from the care personnel in Finland and Japan. J. Nurs. Scholarsh. 2018, 50, 634–644. [Google Scholar] [CrossRef] [PubMed]
- Unbehaun, D.; Aal, K.; Carros, F.; Wieching, R.; Wulf, V. Creative and cognitive activities in social assistive robots and older adults: Results from an exploratory field study with Pepper. In Proceedings of the 17th European Conference on Computer-Supported Cooperative Work: Demos and Posters, Salzburg, Austria, 8–12 June 2019; Volume 3. [Google Scholar]
- Carros, F.; Meurer, J.; Löffler, D.; Unbehaun, D.; Matthies, S.; Koch, I.; Wieching, R.; Randall, D.; Hassenzahl, M.; Wulf, V. Exploring human-robot interaction with the elderly: Results from a ten-week case study in a care home. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems, Honolulu, HI, USA, 25–30 April 2020; pp. 1–12. [Google Scholar]
- Tuuli, T.; Jaana, P. The use of affective care robots calls forth value-based consideration. In Proceedings of the 29th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN), Naples, Italy, 31 August–4 September 2020; pp. 950–955. [Google Scholar]
- Sharkey, A.; Sharkey, N. Granny and the robots: Ethical issues in robot care for the elderly. Eth. Inf. Technol. 2010, 14, 27–40. [Google Scholar] [CrossRef]
- Berridge, C. Active subjects of passive monitoring: Responses to a passive monitoring system in low-income independent living. Ageing Soc. 2017, 37, 537–560. [Google Scholar] [CrossRef] [PubMed]
- Berridge, C. Monitoring the monitors: Medicaid integration of passive remote monitoring technology. Gerontol. Soc. Work 2019, 62, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Pullman, D. The ethics of autonomy and dignity in long-term care. Can. J. Aging 1999, 18, 26–46. [Google Scholar] [CrossRef] [PubMed]
- Gill, J.K. Ethical AI in Healthcare and Its Principles. Akira.AI. Available online: https://www.akira.ai/blog/ethical-ai-in-healthcare (accessed on 20 July 2022).
- Gallagher, A. Dignity and respect for dignity—two key health professional values: Implications for nursing practice. Nurs. Eth. 2004, 11, 587–599. [Google Scholar] [CrossRef] [PubMed]
- Shneiderman, B. Human-centered artificial intelligence: Reliable, safe, and trustworthy. Int. J. Hum. Comput. Interact. 2020, 36, 495–504. [Google Scholar] [CrossRef]
- Shneiderman, B. Human-Centered AI; Oxford University Press: Oxford, UK, 2022. [Google Scholar]
- ROBOTIS. SLAM. Available online: https://emanual.robotis.com/docs/en/platform/turtlebot3/slam (accessed on 10 June 2021).
- ROBOTIS. Dependent ROS Packages. Available online: https://emanual.robotis.com/docs/en/platform/turtlebot3/quick-start/#install-dependent-ros-packages-1 (accessed on 15 July 2021).
- Robot Operating System. Available online: https://www.ros.org (accessed on 12 May 2021).
- Soar Markup Language. SOAR. Available online: https://soar.eecs.umich.edu/articles/articles/soar-markup-language-sml (accessed on 23 July 2019).
- ChatScript. Available online: https://github.com/bwilcox-1234/ChatScript (accessed on 23 July 2021).
- SQLite. Available online: https://www.sqlite.org (accessed on 1 November 2021).
- Google Cloud. Available online: https://cloud.google.com (accessed on 10 September 2021).
- Papago Text Translation. Available online: https://guide-fin.ncloud-docs.com/docs/naveropenapiv3-translation-nmt (accessed on 10 January 2022).
- OpenFace. Available online: https://cmusatyalab.github.io/openface (accessed on 1 September 2021).
- MediaPipe Pose. Available online: https://google.github.io/mediapipe/solutions/pose.html (accessed on 21 October 2021).
- SSD-MobileNet. Available online: https://github.com/chuanqi305/MobileNet-SSD (accessed on 13 March 2021).
- Chen, C.H.; Ramanan, D. 3D human pose estimation = 2D pose estimation + Matching. In Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 21–26 July 2017; pp. 7035–7043. [Google Scholar]
- Kim, J.-W.; Kim, T.; Park, Y.; Kim, S.W. On-load motor parameter identification using univariate dynamic encoding algorithm for searches. IEEE Trans. Energy Convers. 2008, 23, 804–813. [Google Scholar]
- Choi, J.Y.; Ha, E.J.; Kim, J.-W.; Choi, J.-H. Development of a Human Pose Recognition System based on MediaPipe Pose, an Optimization Method, and a Humanoid Robot Model. In Proceedings of the International Symposium on Advanced Intelligent Systems, Cheongju, Korea, 15–18 December 2021; pp. 1–5. [Google Scholar]


| Care Robot Service | Average Satisfaction Score (STDDEV) | T Value | p Value | |
|---|---|---|---|---|
| Caregivers | Medical Staff | |||
| Cognitive activity | 6.05 (1.77) | 5.64 (2.23) | 0.96 | 0.344 |
| Emotional activity | 6.36 (1.78) | 5.6 (3.04) | 1.63 | 0.109 |
| Physical activity | 5.82 (2.69) | 5.32 (2.62) | 1.02 | 0.311 |
| Medication instruction | 6.05 (2.59) | 6.04 (1.64) | 0.01 | 0.990 |
| Caregiver management | 5.86 (2.94) | 5.4 (2.32) | 0.96 | 0.342 |
| Value | Ethical Judgment on Dilemma 1 | Average (STDDEV) | T Value | p Value | |
|---|---|---|---|---|---|
| Caregivers | Medical Staff | ||||
| Dignity | Which of the two do you think the observation behavior of care robots is closest to? (1 = Impairment of dignity, 7 = Action for treatment) | 6.05 (2.95) | 4.88 (3.55) | 2.16 | 0.036 ** |
| Since the care robot is not a person, do you think that filming by the care robot does not undermine the dignity of frail older adults? (1 = Impairment of dignity, 7 = Does not impair dignity with safety information) | 5.23 (5.36) | 3.96 (3.96) | 1.97 | 0.054 | |
| Controllability | Do you think frail older adults or their guardians should be authorized to change ethical settings related to personal information, such as whether or not to film in sensitive situations? (1 = Do not allow changes by older adults or guardians, 7 = Allow changes by older adults or guardians) | 4.86 (6.12) | 5.08 (3.51) | −0.33 | 0.741 |
| If the older adult asks the care robot to stop filming, do you think the care robot should comply immediately? (1 = Should continue, 7 = Should stop immediately) | 3.82 (5.33) | 5.28 (2.76) | −2.46 | 0.018 ** | |
| Personal information | Do you think that the service of a care robot tracking and detecting falls is more important than the dignity or privacy of frail older adults? (1 = Privacy is more important, 7 = Fall detection is more important) | 6.41 (1.70) | 5.48 (2.81) | 2.06 | 0.046 ** |
| Do you think that providing information about a frail older adult’s bowel movements and health status to family members is an infringement of their privacy? (1 = Serious privacy infringement, 7 = Noninfringement of privacy and more important to understand health status) | 5.82 (2.97) | 4.72 (3.48) | 2.04 | 0.047 ** | |
| Ethical Judgment on Dilemma 2 | Average (STDDEV) | T Value | p Value | |
|---|---|---|---|---|
| Care- Givers | Medical Staff | |||
| Which of the two do you think best describes the continuous medication instruction by the care robot? (1 = Improper behavior ignoring Mr. K’s opinion, 7 = Very necessary action for health) | 5.27 (3.56) | 5.24 (2.74) | 0.06 | 0.951 |
| Do you think the care robot should require the frail older adult to take their medicine until they complete the prescribed dose? (1 = Strongly disagree, 7 = Strongly agree) | 4.77 (4.99) | 4.32 (3.74) | 0.73 | 0.470 |
| Do you think the care robot should stop giving instructions if the frail older adult does not respond or refuses to take the medicine even though they have been instructed about three times? (1 = Strongly disagree, 7 = Strongly agree) | 4.82 (6.24) | 4.8 (4.0) | 0.03 | 0.979 |
| Do you think the care robot should stop prompting the frail older adult immediately if they refuse to take their medication? (1 = Strongly disagree, 7 = Strongly agree) | 3.09 (5.17) | 3.2 (3.68) | −0.17 | 0.862 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.-W.; Choi, Y.-L.; Jeong, S.-H.; Han, J. A Care Robot with Ethical Sensing System for Older Adults at Home. Sensors 2022, 22, 7515. https://doi.org/10.3390/s22197515
Kim J-W, Choi Y-L, Jeong S-H, Han J. A Care Robot with Ethical Sensing System for Older Adults at Home. Sensors. 2022; 22(19):7515. https://doi.org/10.3390/s22197515
Chicago/Turabian StyleKim, Jong-Wook, Young-Lim Choi, Sang-Hyun Jeong, and Jeonghye Han. 2022. "A Care Robot with Ethical Sensing System for Older Adults at Home" Sensors 22, no. 19: 7515. https://doi.org/10.3390/s22197515
APA StyleKim, J.-W., Choi, Y.-L., Jeong, S.-H., & Han, J. (2022). A Care Robot with Ethical Sensing System for Older Adults at Home. Sensors, 22(19), 7515. https://doi.org/10.3390/s22197515







