Wearable E-Textile and CNT Sensor Wireless Measurement System for Real-Time Penile Erection Monitoring
Abstract
:1. Introduction
2. Materials and Methods
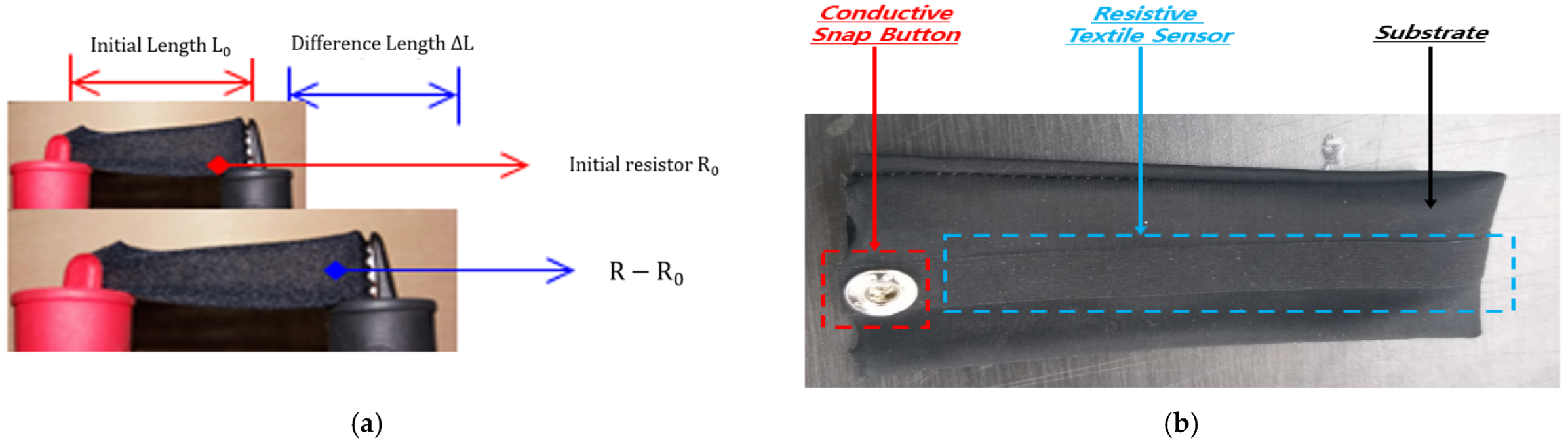
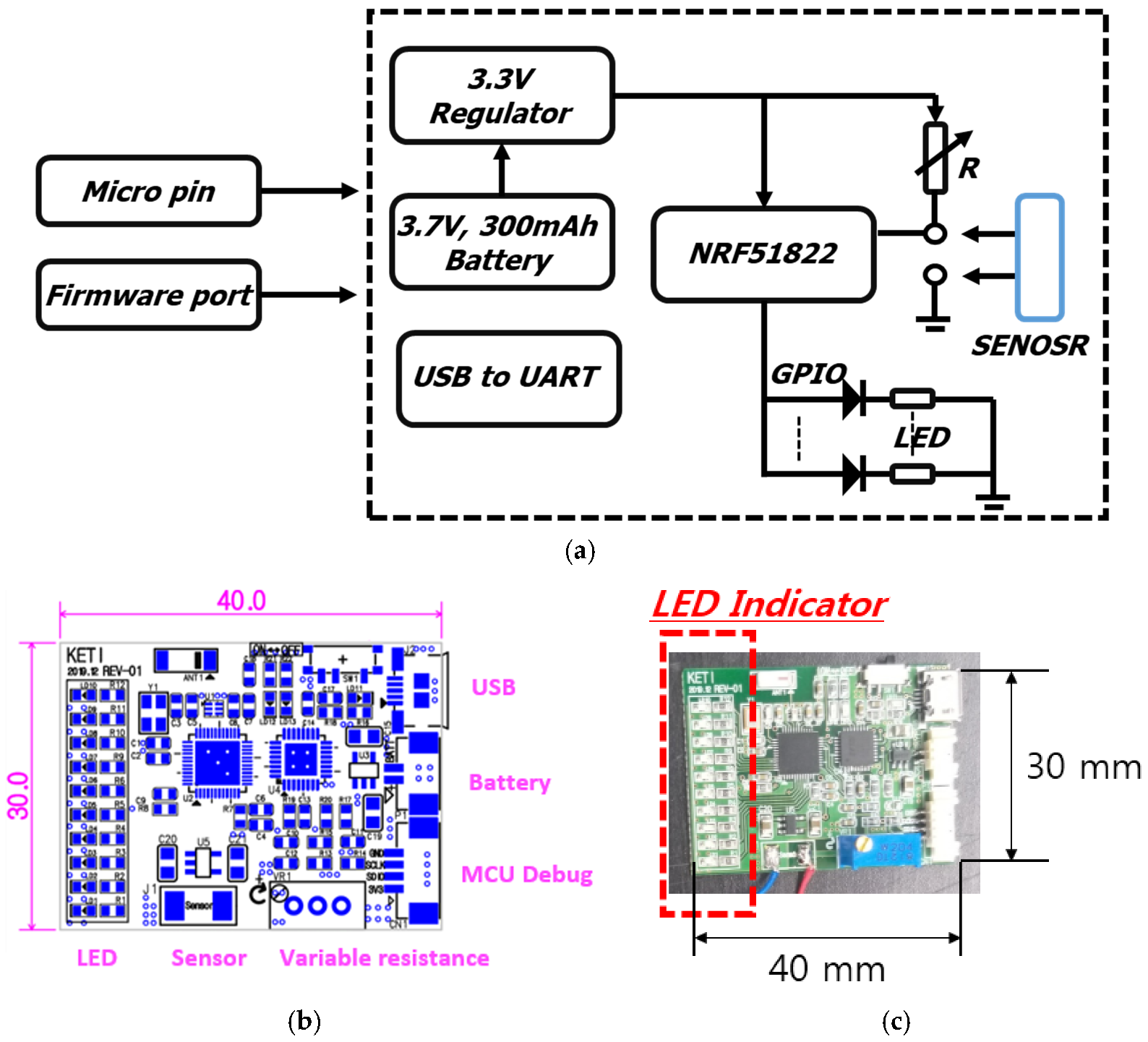
2.1. Wearable E-Textile Sensor
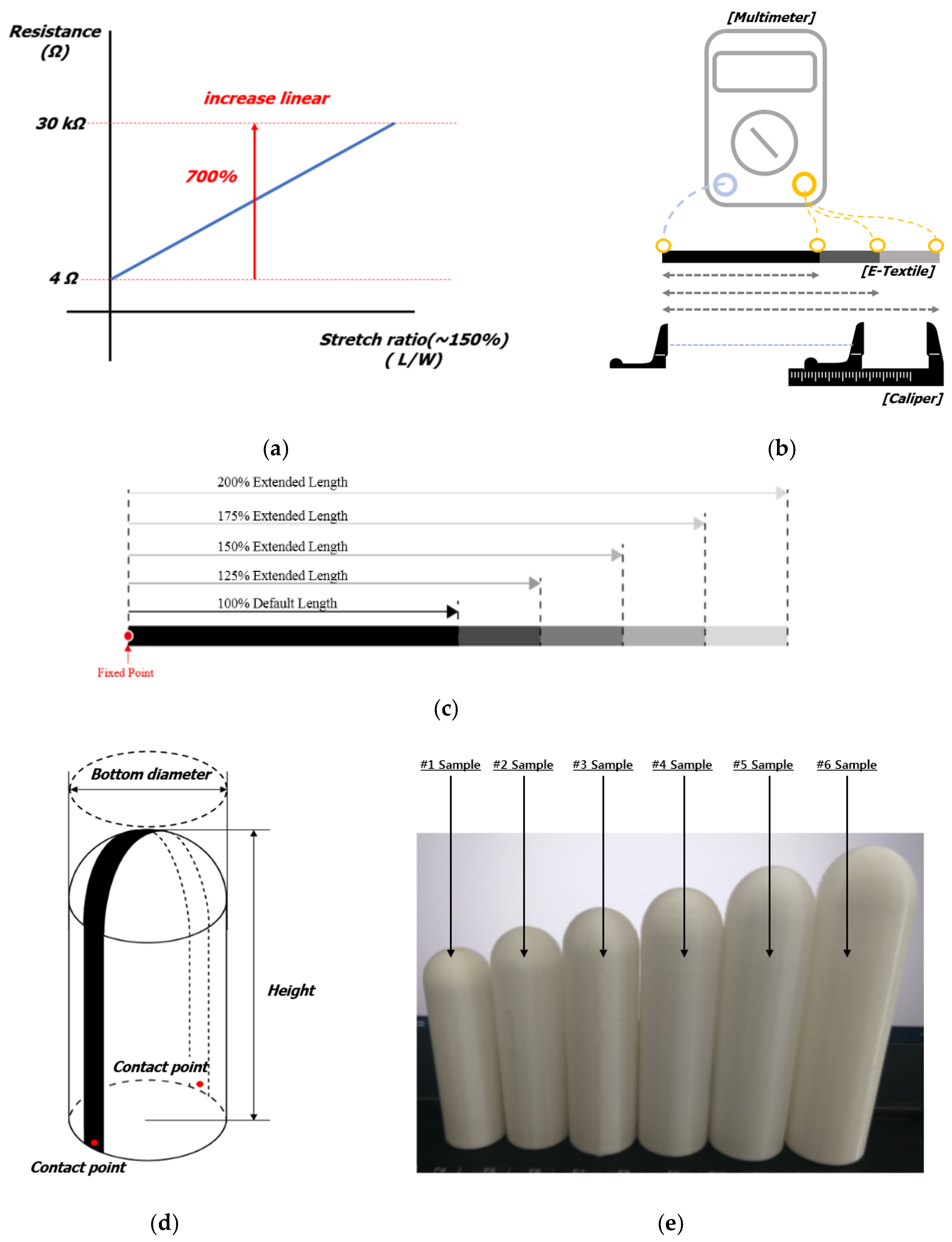
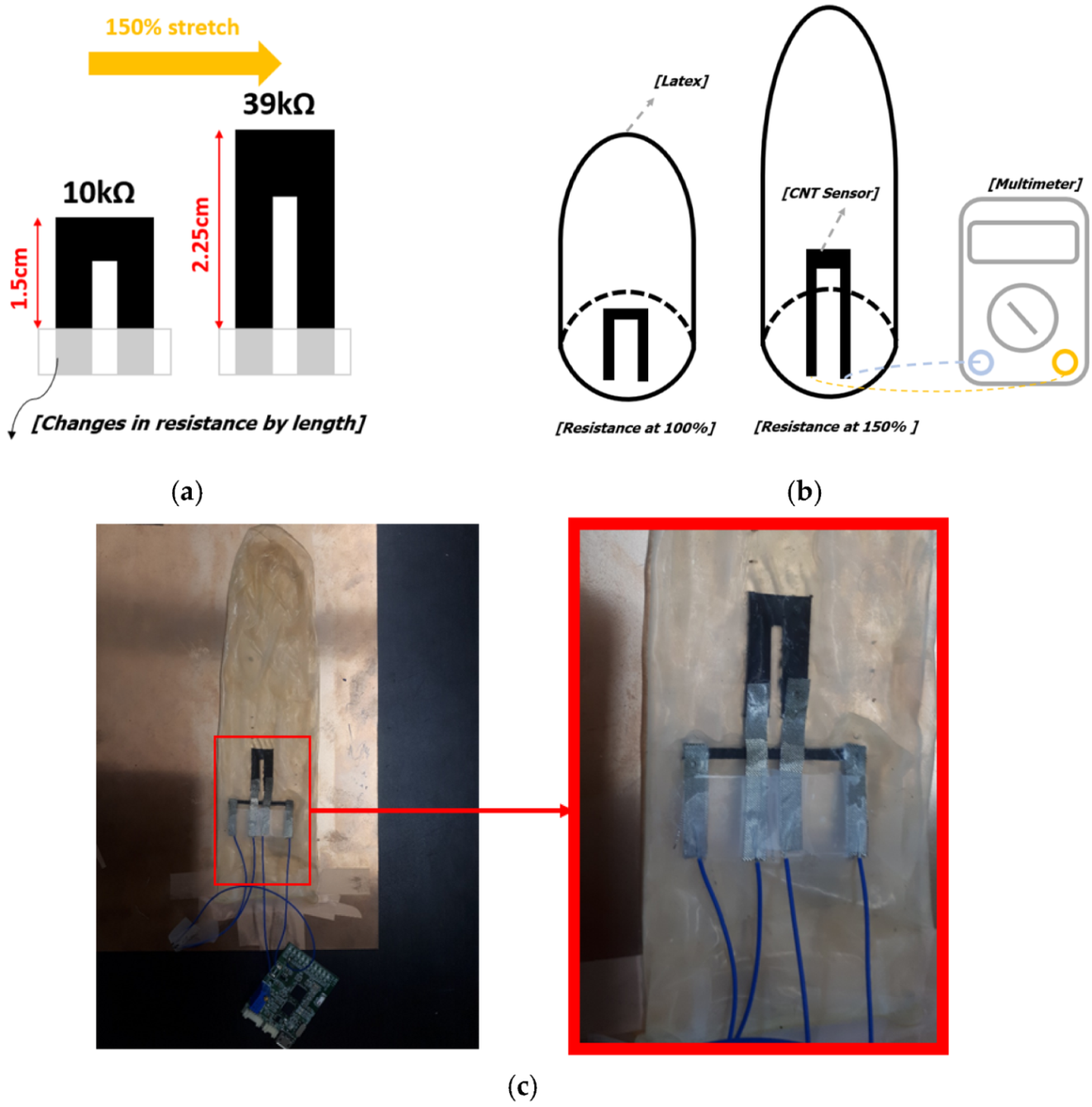
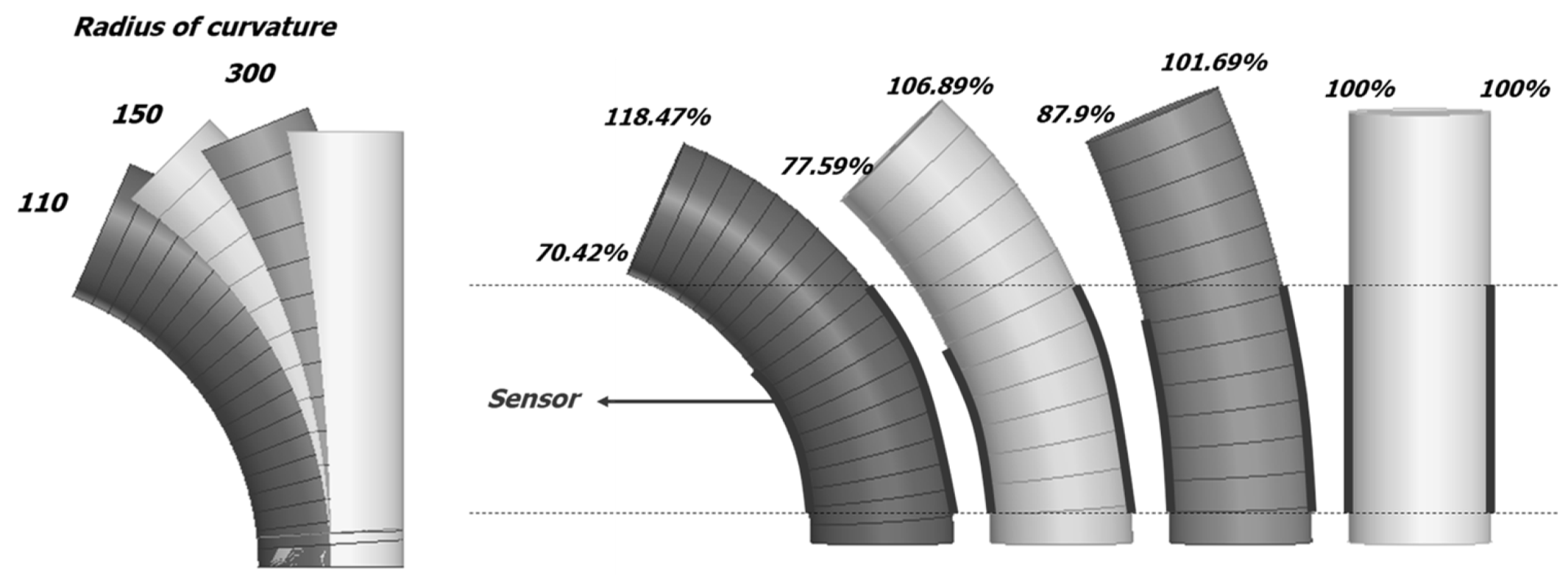
2.2. Wearable CNT Sensor
3. Results
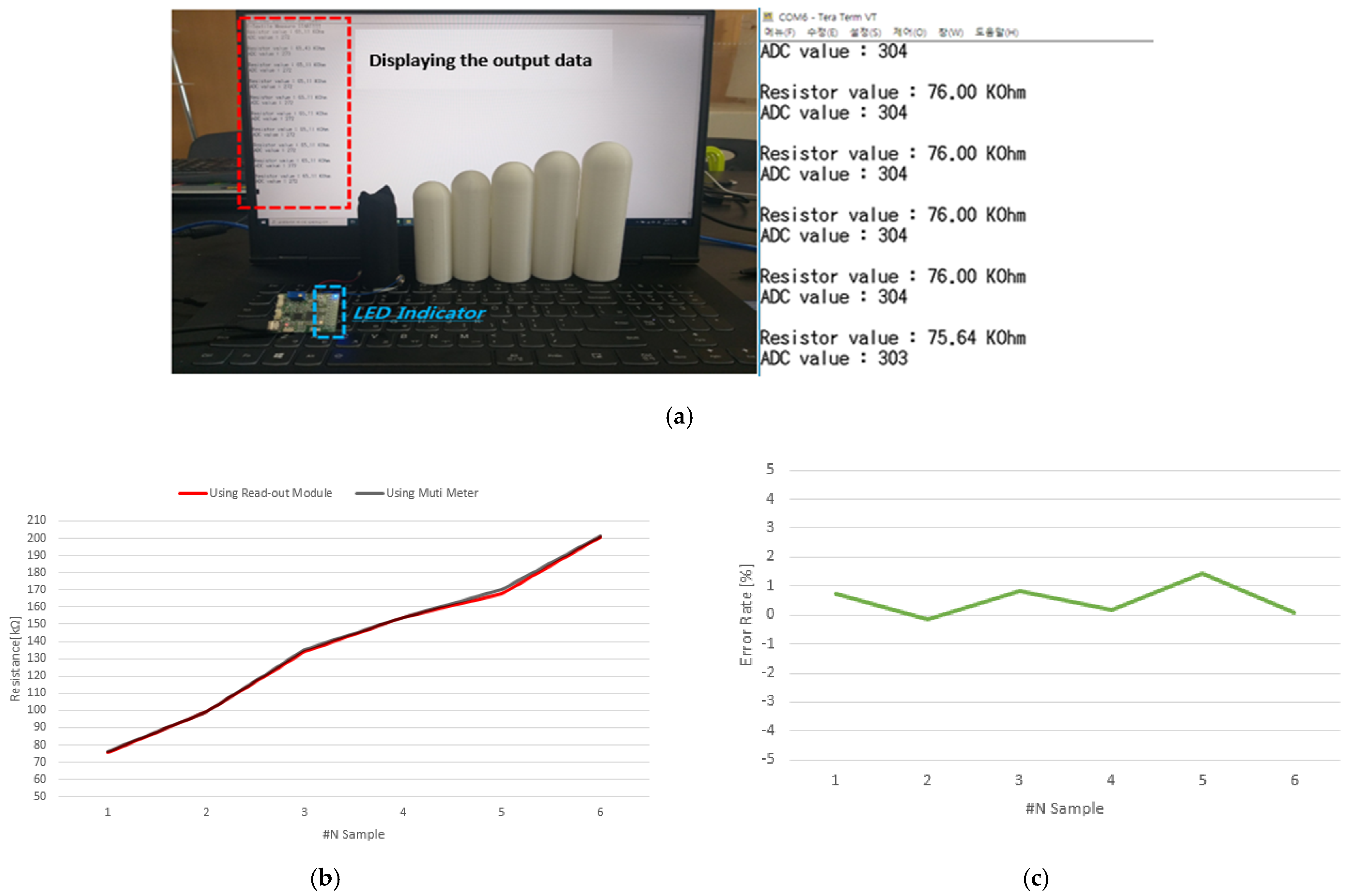
3.1. Wearable E-Textile Sensor
3.2. Wearable CNT Sensor
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chang, T.-H.; Tian, Y.; Li, C.; Gu, X.; Li, K.; Yang, H.; Sanghani, P.; Lim, C.M.; Ren, H.; Chen, P.-Y. Stretchable graphene pressure sensors with Shar-Pei-like hierarchical wrinkles for collision-aware surgical robotics. ACS Appl. Mater. Interfaces 2019, 11, 10226–10236. [Google Scholar] [CrossRef]
- Mukhopadhyay, S.C. Wearable sensors for human activity monitoring: A review. IEEE Sens. J. 2014, 15, 1321–1330. [Google Scholar] [CrossRef]
- Pang, C.; Lee, C.; Suh, K.Y. Recent advances in flexible sensors for wearable and implantable devices. J. Appl. Polym. Sci. 2013, 130, 1429–1441. [Google Scholar] [CrossRef]
- Lipomi, D.J.; Vosgueritchian, M.; Tee, B.C.; Hellstrom, S.L.; Lee, J.A.; Fox, C.H.; Bao, Z. Skin-like pressure and strain sensors based on transparent elastic films of carbon nanotubes. Nat. Nanotechnol. 2011, 6, 788–792. [Google Scholar] [CrossRef] [PubMed]
- Fujino, Y. Integrated Healthcare Service and it’s Application for Life-log. IEICE Tech. Rep. 2011, 111, 31–36. [Google Scholar]
- Rawassizadeh, R.; Tomitsch, M.; Wac, K.; Tjoa, A.M. UbiqLog: A generic mobile phone-based life-log framework. Pers. Ubiquitous Comput. 2013, 17, 621–637. [Google Scholar] [CrossRef]
- Tanoue, K.; Kushima, M.; Araki, K.; Suzuki, M.; Yamazaki, T.; Sonehara, N. Analysis of the Electronic Medical Record Life Log of Medical Welfare Big Data. IEICE Tech. Rep. 2013, 112, 159–164. [Google Scholar]
- Reddy, D.L.; Naik, M.R.; Srikar, D. Health Monitoring System Based on IoT. In Proceedings of the 2021 5th International Conference on Trends in Electronics and Informatics (ICOEI), Tirunelveli, India, 3–5 June 2021; pp. 468–472. [Google Scholar]
- Sabukunze, I.D.; Setyohadi, D.B.; Sulistyoningsih, M. Designing An Iot Based Smart Monitoring and Emergency Alert System for Covid19 Patients. In Proceedings of the 2021 6th International Conference for Convergence in Technology (I2CT), Pune, India, 2–4 April 2021; pp. 1–5. [Google Scholar]
- Azadzoi, K.M.; Goldstein, I. Erectile dysfunction due to atherosclerotic vascular disease: The development of an animal model. J. Urol. 1992, 147, 1675–1681. [Google Scholar] [CrossRef]
- Fletcher, E.C.; Martin, R.J. Sexual dysfunction and erectile impotence in chronic obstructive pulmonary disease. Chest 1982, 81, 413–421. [Google Scholar] [CrossRef]
- Jackson, G.; Boon, N.; Eardley, I.; Kirby, M.; Dean, J.; Hackett, G.; Montorsi, P.; Montorsi, F.; Vlachopoulos, C.; Kloner, R. Erectile dysfunction and coronary artery disease prediction: Evidence-based guidance and consensus. Int. J. Clin. Pract. 2010, 64, 848–857. [Google Scholar] [CrossRef] [PubMed]
- Kloner, R.A.; Mullin, S.H.; Shook, T.; Matthews, R.; Mayeda, G.; Burstein, S.; Peled, H.; Pollick, C.; Choudhary, R.; Rosen, R. Erectile dysfunction in the cardiac patient: How common and should we treat? J. Urol. 2003, 170, S46–S50. [Google Scholar] [CrossRef] [PubMed]
- Kloner, R.; Padma-Nathan, H. Erectile dysfunction in patients with coronary artery disease. Int. J. Impot. Res. 2005, 17, 209–215. [Google Scholar] [CrossRef] [Green Version]
- Kloner, R. Erectile dysfunction and hypertension. Int. J. Impot. Res. 2007, 19, 296–302. [Google Scholar] [CrossRef]
- Lue, T.F. Erectile dysfunction. N. Engl. J. Med. 2000, 342, 1802–1813. [Google Scholar] [CrossRef] [PubMed]
- Mulhall, J.; Ahmed, A.; Parker, M.; Mohideen, N. Erectile dysfunction: The hemodynamics of erectile dysfunction following external beam radiation for prostate cancer. J. Sex. Med. 2005, 2, 432–437. [Google Scholar] [CrossRef]
- Qin, F.; Gao, L.; Qian, S.; Fu, F.; Yang, Y.; Yuan, J. Advantages and limitations of sleep-related erection and rigidity monitoring: A review. Int. J. Impot. Res. 2018, 30, 192–201. [Google Scholar] [CrossRef] [PubMed]
- Jannini, E.A.; Granata, A.M.; Hatzimouratidis, K.; Goldstein, I. Controversies in sexual medicine: Use and abuse of rigiscan in the diagnosis of erectile dysfunction. J. Sex. Med. 2009, 6, 1820–1829. [Google Scholar] [CrossRef]
- Klotz, T.; Sachse, R.; Heidrich, A.; Jockenhövel, F.; Rohde, G.; Wensing, G.; Horstmann, R.; Engelmann, R. Vardenafil increases penile rigidity and tumescence in erectile dysfunction patients: A RigiScan and pharmacokinetic study. World J. Urol. 2001, 19, 32–39. [Google Scholar] [CrossRef]
- Munoz, M.; Bancroft, J.; Marshall, I. The performance of the Rigiscan in the measurement of penile tumescence and rigidity. Int. J. Impot. Res. 1993, 5, 69–76. [Google Scholar] [PubMed]
- Veale, D.; Miles, S.; Bramley, S.; Muir, G.; Hodsoll, J. Am I normal? A systematic review and construction of nomograms for flaccid and erect penis length and circumference in up to 15 521 men. BJU Int. 2015, 115, 978–986. [Google Scholar] [CrossRef] [Green Version]
- Wessells, H.; Lue, T.F.; McAninch, J.W. Penile length in the flaccid and erect states: Guidelines for penile augmentation. J. Urol. 1996, 156, 995–997. [Google Scholar] [CrossRef]
- Chen, X.; Li, R.; Yang, H.; Dai, J. A comprehensive, prospective study of penile dimensions in Chinese men of multiple ethnicities. Int. J. Impot. Res. 2014, 26, 172–176. [Google Scholar] [CrossRef]
- Appelboom, G.; Camacho, E.; Abraham, M.E.; Bruce, S.S.; Dumont, E.L.; Zacharia, B.E.; D’Amico, R.; Slomian, J.; Reginster, J.Y.; Bruyère, O. Smart wearable body sensors for patient self-assessment and monitoring. Arch. Public Health 2014, 72, 28. [Google Scholar] [CrossRef] [Green Version]
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599. [Google Scholar] [CrossRef]
- Sawyer, J. Wearable Internet of Medical Things sensor devices, artificial intelligence-driven smart healthcare services, and personalized clinical care in COVID-19 telemedicine. Am. J. Med. Res. 2020, 7, 71–77. [Google Scholar]
- Melman, A.; Fogarty, J.; Hafron, J. Can self-administered questionnaires supplant objective testing of erectile function? A comparison between the International Index of Erectile Function and objective studies. Int. J. Impot. Res. 2006, 18, 126–129. [Google Scholar] [CrossRef] [Green Version]
- Rosen, R.C.; Allen, K.R.; Ni, X.; Araujo, A.B. Minimal clinically important differences in the erectile function domain of the International Index of Erectile Function scale. Eur. Urol. 2011, 60, 1010–1016. [Google Scholar] [CrossRef] [PubMed]
- Blander, D.S.; Sáánchez-Ortiz, R.F.; Broderick, G.A. Sex inventories: Can questionnaires replace erectile dysfunction testing? Urology 1999, 54, 719–723. [Google Scholar] [CrossRef]
- Celermajer, D.S.; Sorensen, K.E.; Spiegelhalter, D.J.; Georgakopoulos, D.; Robinson, J.; Deanfield, J.E. Aging is associated with endothelial dysfunction in healthy men years before the age-related decline in women. J. Am. Coll. Cardiol. 1994, 24, 471–476. [Google Scholar] [CrossRef] [Green Version]
- Bacal, V.; Rumohr, J.; Sturm, R.; Lipshultz, L.I.; Schumacher, M.; Grober, E.D. Correlation of degree of penile curvature between patient estimates and objective measures among men with Peyronie’s disease. J. Sex. Med. 2009, 6, 862–865. [Google Scholar] [CrossRef] [PubMed]
- Levine, L.; Greenfield, J. Establishing a standardized evaluation of the man with Peyronie’s disease. Int. J. Impot. Res. 2003, 15, S103–S112. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levy, J.A.; Marchand, M.; Iorio, L.; Zribi, G.; Zahalsky, M.P. Effects of stem cell treatment in human patients with Peyronie disease. J. Osteopath. Med. 2015, 115, e8–e13. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Sample #1 | Sample #2 | Sample #3 | Sample #4 | Sample #5 | Sample #6 | |
|---|---|---|---|---|---|---|
| Diameter(mm) | 28 | 30 | 32 | 34 | 36 | 38 |
| Height(mm) | 90 | 99 | 108 | 117 | 126 | 135 |
| Sample #1 | Sample #2 | Sample #3 | Sample #4 | Sample #5 | Sample #6 | |
|---|---|---|---|---|---|---|
| Output resistance (kΩ) | 75 | 99 | 134 | 153 | 169 | 200 |
| Measured resistance (kΩ) | 76 | 99 | 135 | 154 | 170 | 201 |
| Error (%) | 0.73 | −0.17 | 0.82 | 0.19 | 1.44 | 0.08 |
| 300 (Left/Right) | 150 (Left/Right) | 110 (Left/Right) | |
|---|---|---|---|
| 100% | 17.5 kΩ/45.6 kΩ | 17.58 kΩ/45.6 kΩ | 17.5 kΩ/45.6 kΩ |
| 110% | 19.3 kΩ/186.5 kΩ | 17.07 kΩ/231.1 kΩ | 15.4 kΩ/280.6 kΩ |
| 120% | 103.3 kΩ/256.0 kΩ | 18.62 kΩ/274.8 kΩ | 16.9 kΩ/312.9 kΩ |
| 130% | 205.3 kΩ/284.3 kΩ | 20 kΩ/297.9 kΩ | 18.31 kΩ/380 kΩ |
| 140% | 259.8 kΩ/314.2 kΩ | 151.1 kΩ/325.5 kΩ | 19.72 kΩ/455.1 kΩ |
| 150% | 255.6 kΩ/375.2 kΩ | 221.8 kΩ/422 kΩ | 105.5 kΩ/526.2 kΩ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heo, Y.; Kim, J.; Cha, C.; Shin, K.; Roh, J.; Jo, J. Wearable E-Textile and CNT Sensor Wireless Measurement System for Real-Time Penile Erection Monitoring. Sensors 2022, 22, 231. https://doi.org/10.3390/s22010231
Heo Y, Kim J, Cha C, Shin K, Roh J, Jo J. Wearable E-Textile and CNT Sensor Wireless Measurement System for Real-Time Penile Erection Monitoring. Sensors. 2022; 22(1):231. https://doi.org/10.3390/s22010231
Chicago/Turabian StyleHeo, Yongki, Jinhyung Kim, Cheolung Cha, Kyusik Shin, Jihyoung Roh, and Jungki Jo. 2022. "Wearable E-Textile and CNT Sensor Wireless Measurement System for Real-Time Penile Erection Monitoring" Sensors 22, no. 1: 231. https://doi.org/10.3390/s22010231
APA StyleHeo, Y., Kim, J., Cha, C., Shin, K., Roh, J., & Jo, J. (2022). Wearable E-Textile and CNT Sensor Wireless Measurement System for Real-Time Penile Erection Monitoring. Sensors, 22(1), 231. https://doi.org/10.3390/s22010231








