Validity of Hololens Augmented Reality Head Mounted Display for Measuring Gait Parameters in Healthy Adults and Children with Cerebral Palsy
Abstract
1. Introduction
2. Related Work
3. Materials and Methods
3.1. Participants
3.2. Gait Analysis Systems
3.2.1. MOCAP System
3.2.2. Hololens AR HMD
3.3. The HoloStep Computational Method
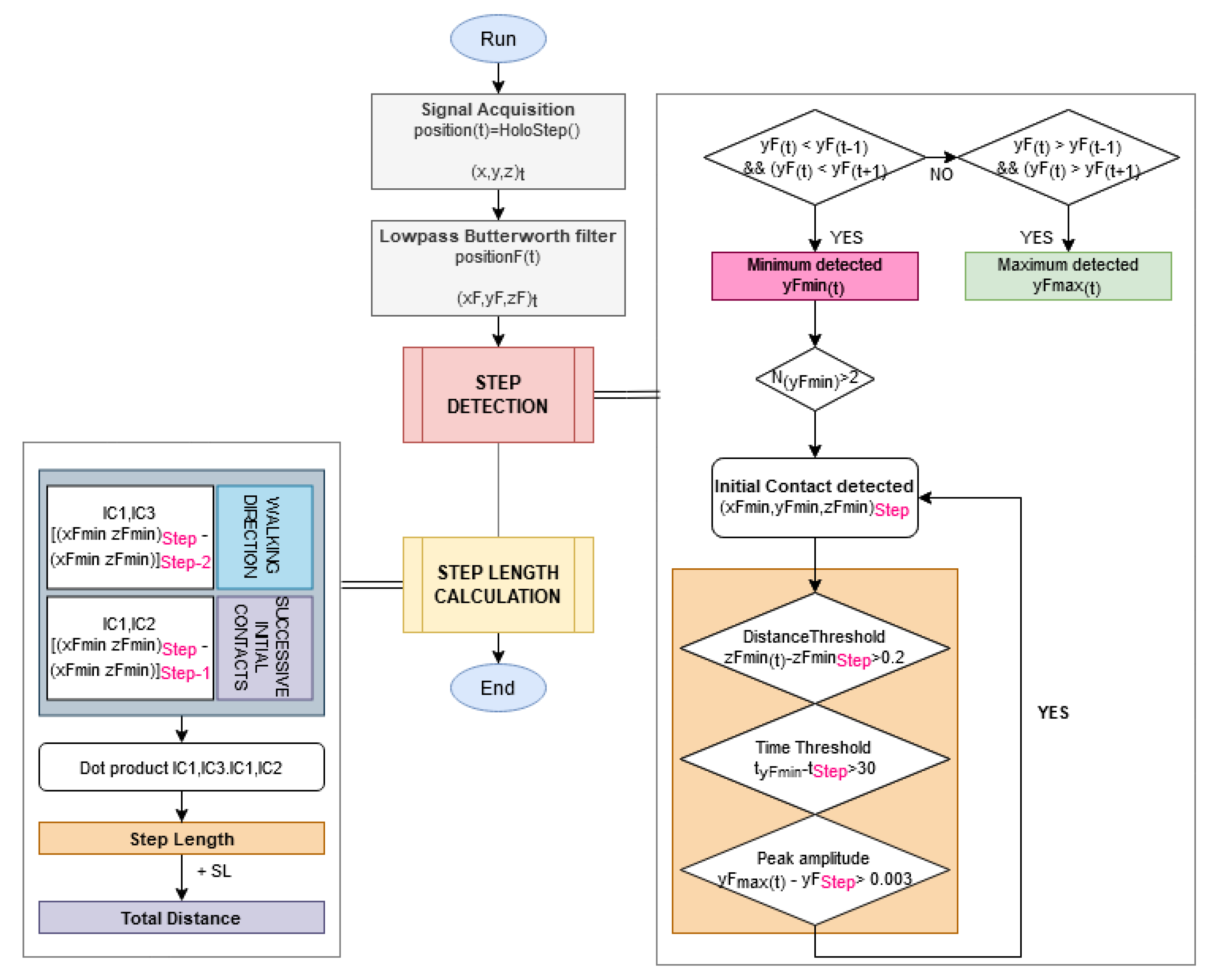
3.3.1. Step Detection
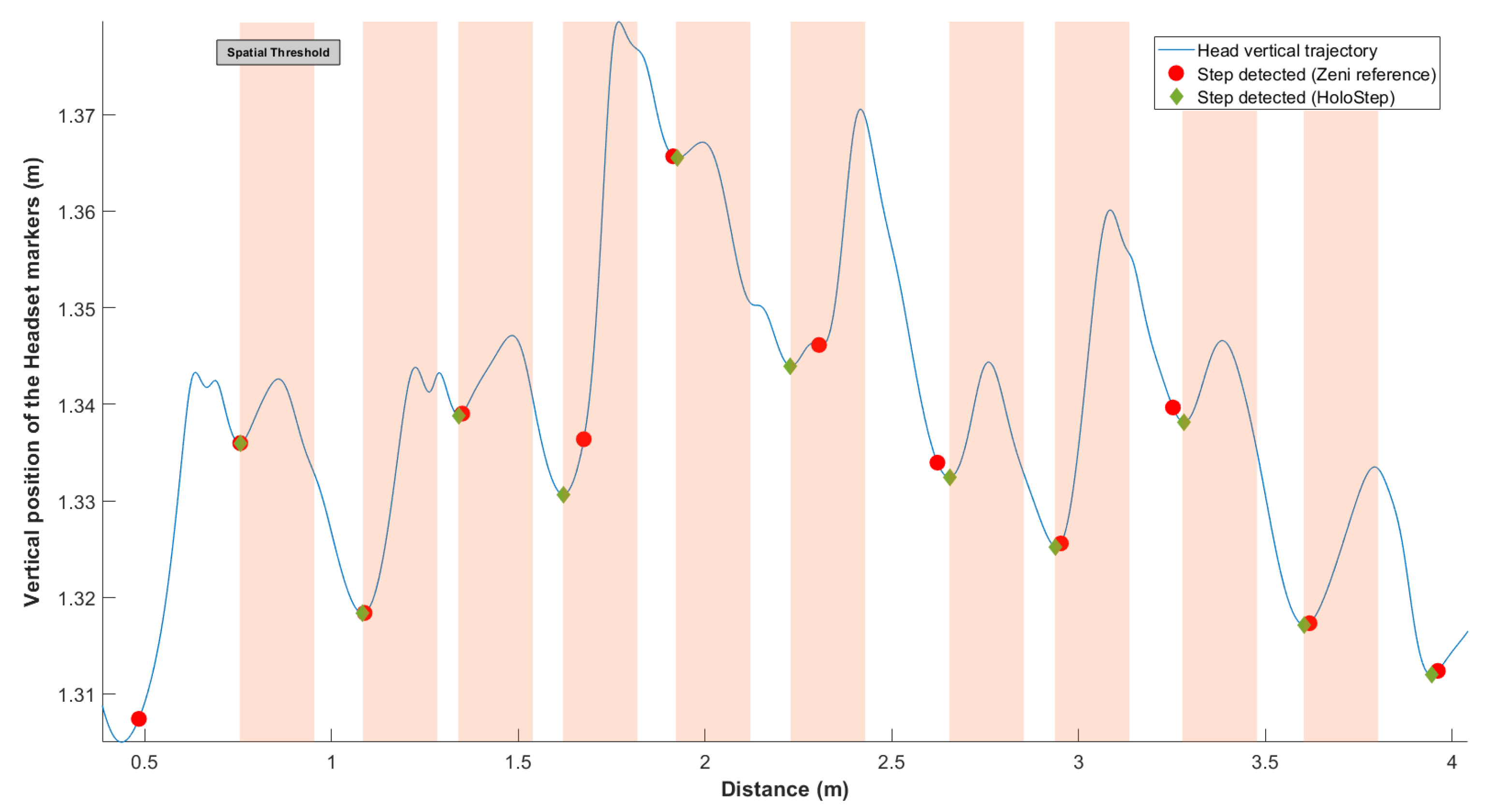
- First, the locking distance was defined: new IC was considered only if the distance between two IC was greater than this threshold (Figure 2). In order to make Holostep the most suitable for children with CP, we reviewed a separate data set from the gait analysis of 188 children with CP in a specialised laboratory. The mean distance between two IC was 44.31 cm, with SD = 11.87. We have set the locking distance at 20 cm (rounded down of ).
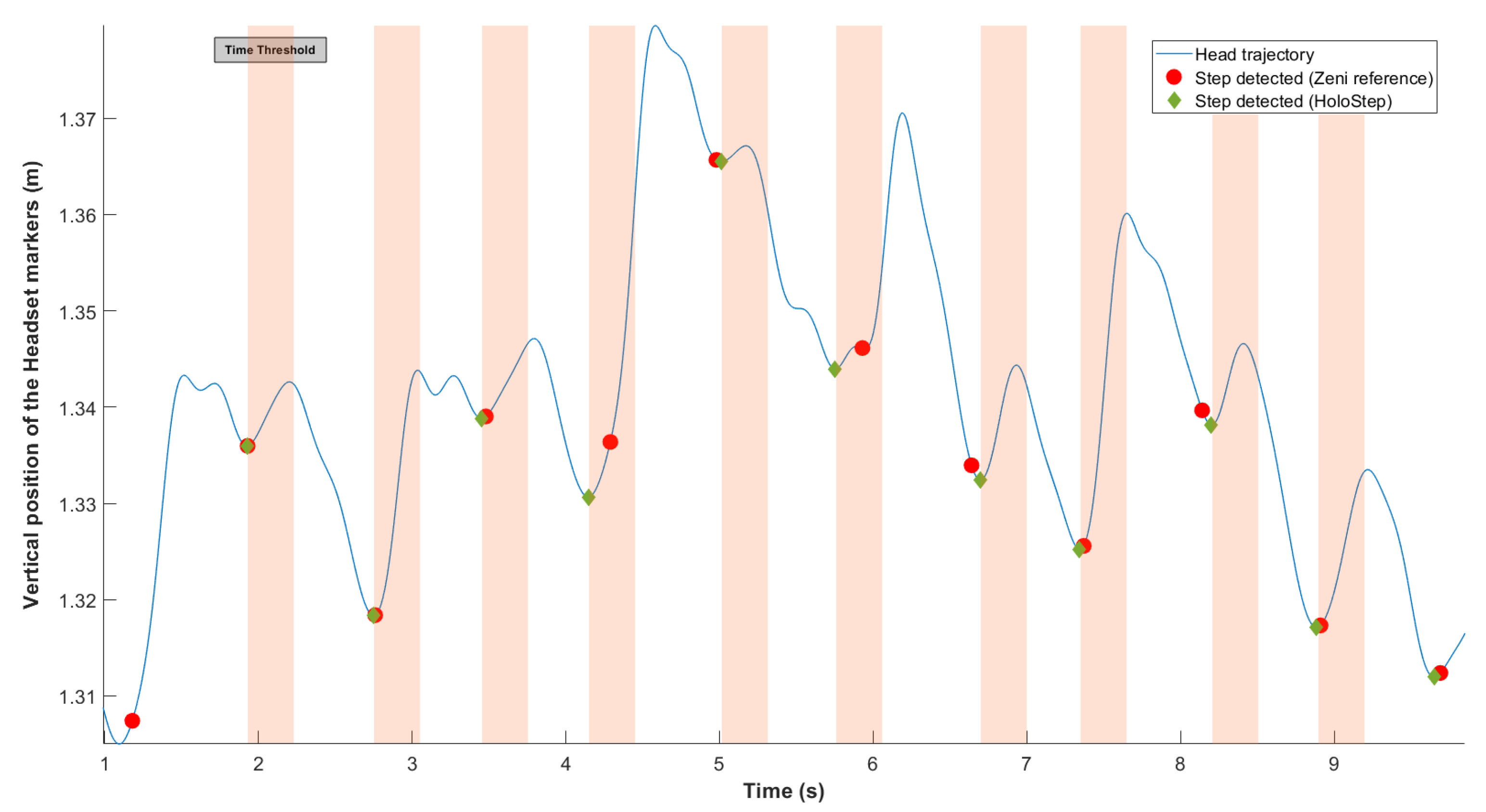
- Second, the locking time was defined: new IC was considered only if the time between two IC detected was greater than this threshold (Figure 3). As before, after analysis of the specific data set for children with CP, mean time between two IC was 56.01 ms, with SD = 12.54. The locking time was set to 30 ms (rounded down of ).
- Third, the peak amplitude threshold was defined: the minimum difference required between previous maximal and current minimal . As before, after analysis of the specific data set for children with CP, mean peak amplitude detection was small at 0.3 cm. This is the value we have retained for the peak amplitude threshold.
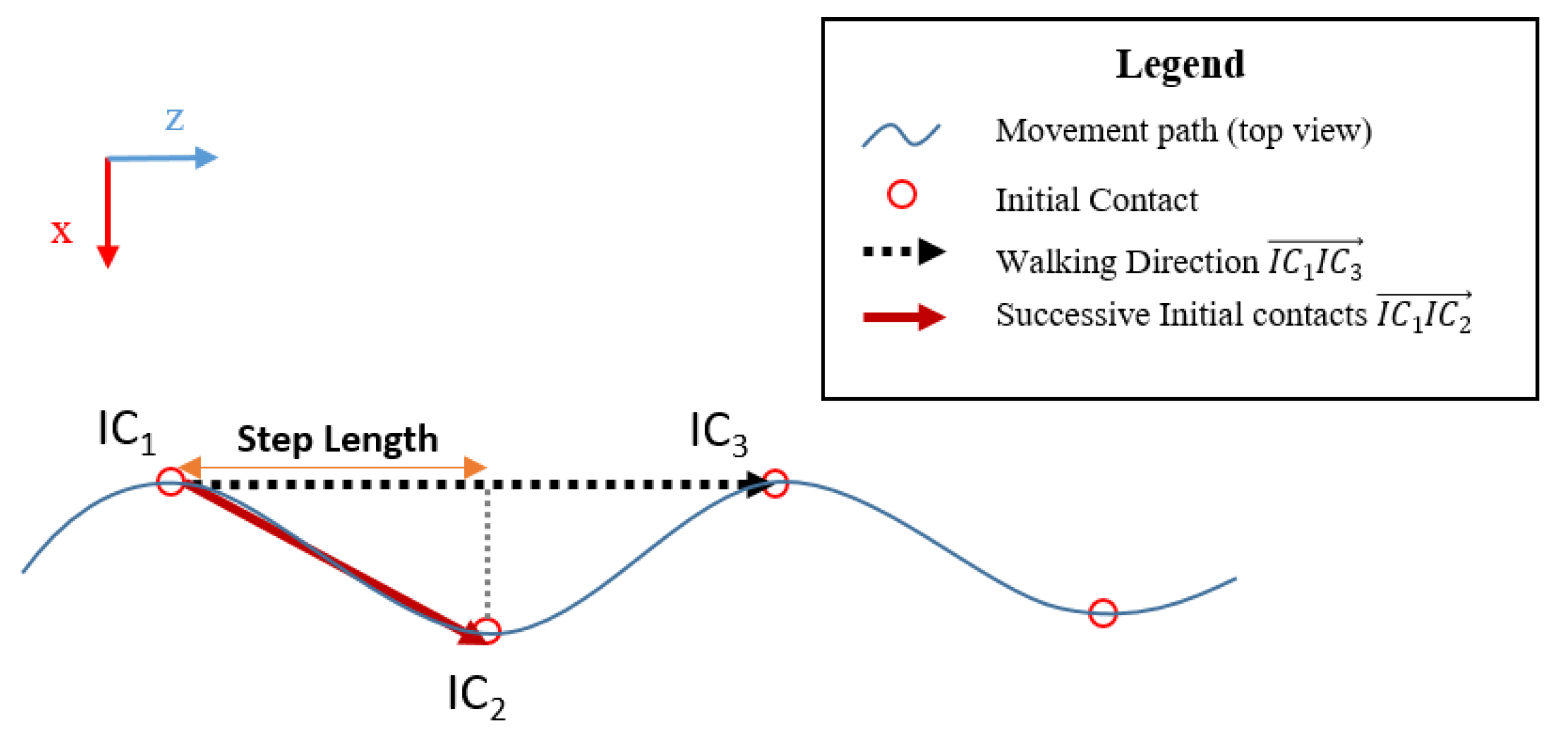
3.3.2. Step Length and Walking Distance
3.4. Experimental Procedure
3.5. Data Processing
- Reference: Zeni algorithm using a set of pelvic and feet markers calculating spatiotemporal gait parameters with high accuracy [22];
- Challenger: HoloStep algorithm using head pose.
3.6. Statistical Analysis
4. Results
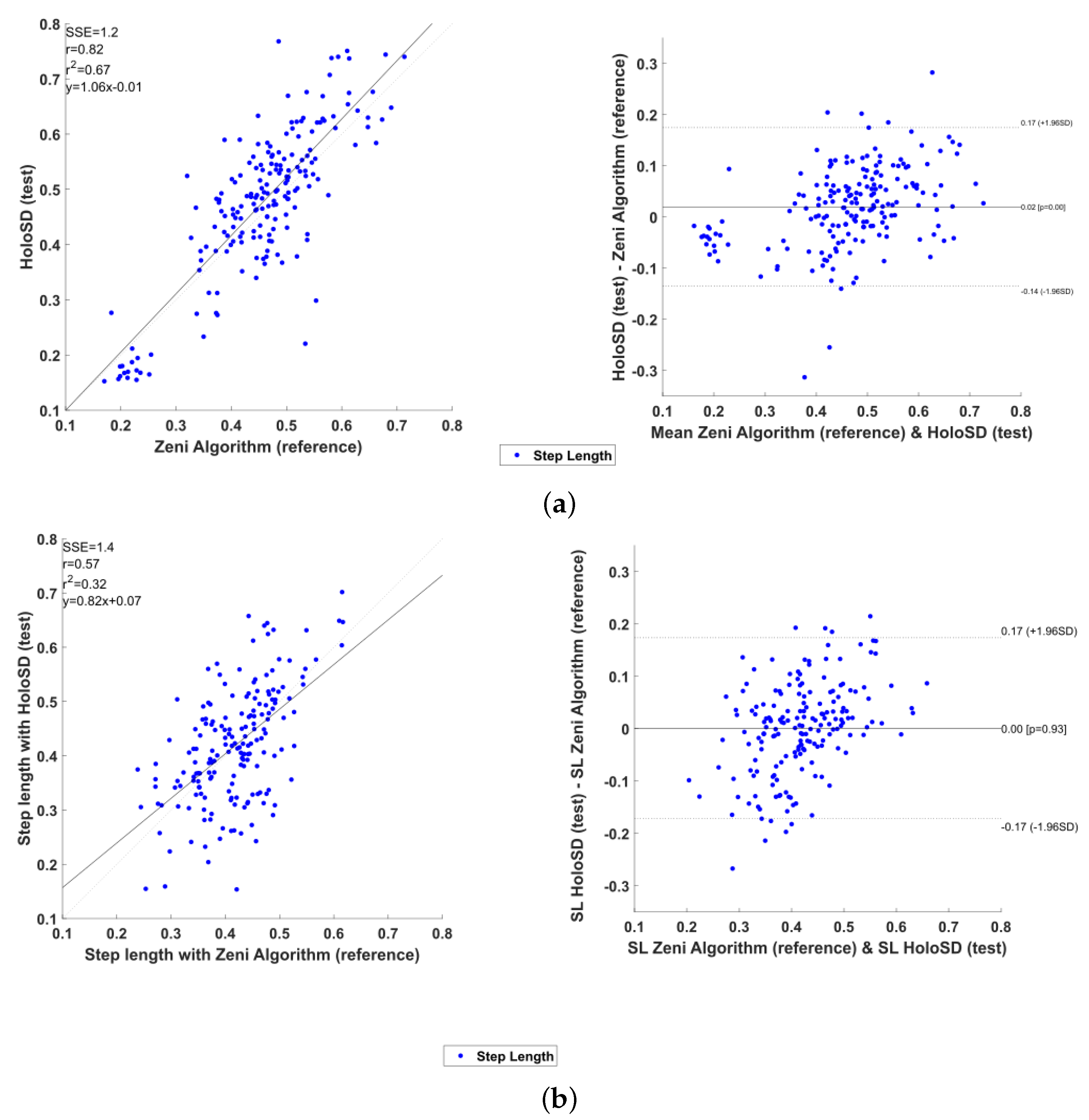
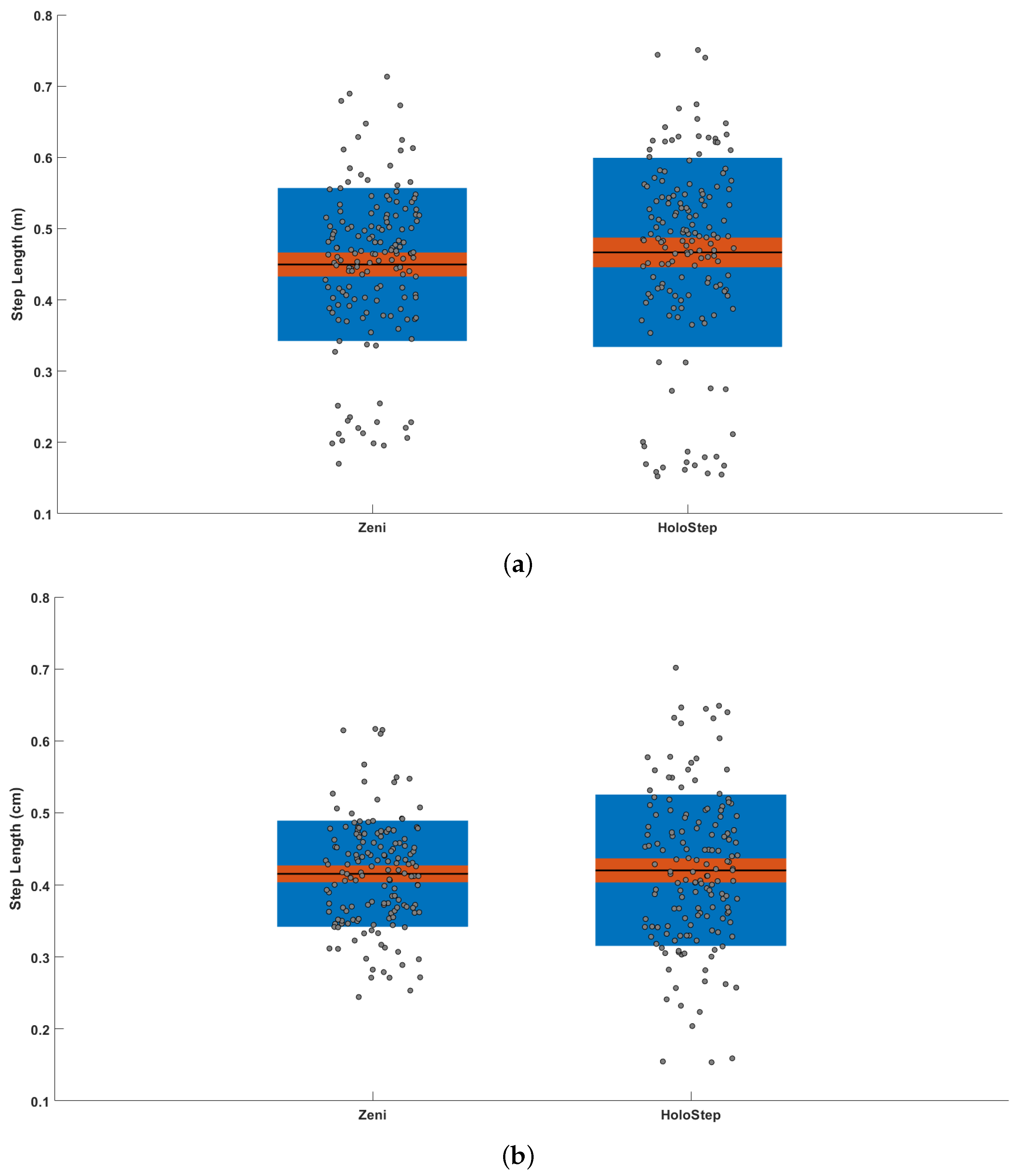
4.1. Healthy Participants
4.2. Children with CP
5. Discussion
5.1. Comparison with Other Methods
5.2. Gait Detection for Children with CP
5.3. HoloStep Limitations
6. Conclusions and Future Work
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AR | Augmented Reality |
| CP | Cerebral Palsy |
| FC | Foot Contact |
| GMFCS | Gross Motor Function Classification System |
| HMD | Head Mounted Display |
| HP | Healthy Participants |
| IC | Initial Contact |
| ICC | Intra-Class Coefficient |
| SD | Standard Deviation |
| SL | Step Length |
| TD | Typically Developing |
| TO | Toe Off |
| VR | Virtual Reality |
References
- Graham, H.K.; Rosenbaum, P.; Paneth, N.; Dan, B.; Lin, J.P.; Damiano, D.L.; Becher, J.G.; Gaebler-Spira, D.; Colver, A.; Reddihough, D.S.; et al. Cerebral palsy. Nat. Rev. Dis. Prim. 2016, 2, 15082. [Google Scholar] [CrossRef]
- Sellier, E.; Platt, M.; Andersen, G.; Krägeloh-Mann, I.; De La Cruz, J.; Cans, C. Decreasing prevalence in cerebral palsy: A multi-site European population-based study, 1980 to 2003. Dev. Med. Child Neurol. 2016, 58, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 109, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.C.; Damiano, D.L.; Abel, M.F. The evolution of gait in childhood and adolescent cerebral palsy. J. Pediatr. Orthop. 1997, 17, 392–396. [Google Scholar] [CrossRef] [PubMed]
- Armand, S.; Decoulon, G.; Bonnefoy-Mazure, A. Gait analysis in children with cerebral palsy. EFORT Open Rev. 2016, 1, 448–460. [Google Scholar] [CrossRef]
- Kim, C.J.; Son, S.M. Comparison of Spatiotemporal Gait Parameters between Children with Normal Development and Children with Diplegic Cerebral Palsy. J. Phys. Ther. Sci. 2014, 26, 1317–1319. [Google Scholar] [CrossRef]
- Gage, J.R.; Schwartz, M.H.; Koop, S.E.; Novacheck, T.F. The Identification and Treatment of Gait Problems in Cerebral Palsy; Mac Keith Press: London, UK, 2009. [Google Scholar]
- Opheim, A.; McGinley, J.L.; Olsson, E.; Stanghelle, J.K.; Jahnsen, R. Walking deterioration and gait analysis in adults with spastic bilateral cerebral palsy. Gait Posture 2013, 37, 165–171. [Google Scholar] [CrossRef]
- Booth, A.T.C.; Buizer, A.I.; Meyns, P.; Oude Lansink, I.L.B.; Steenbrink, F.; van der Krogt, M.M. The efficacy of functional gait training in children and young adults with cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2018, 60, 866–883. [Google Scholar] [CrossRef]
- Grecco, L.A.; Zanon, N.; Sampaio, L.M.; Oliveira, C.S. A comparison of treadmill training and overground walking in ambulant children with cerebral palsy: Randomized controlled clinical trial. Clin. Rehabil. 2013, 27, 686–696. [Google Scholar] [CrossRef]
- Meyns, P.; Pans, L.; Plasmans, K.; Heyrman, L.; Desloovere, K.; Molenaers, G. The Effect of Additional Virtual Reality Training on Balance in Children with Cerebral Palsy after Lower Limb Surgery: A Feasibility Study. Games Health J. 2017, 6, 39–48. [Google Scholar] [CrossRef]
- Weiss, P.L.T.; Tirosh, E.; Fehlings, D. Role of virtual reality for cerebral palsy management. J. Child Neurol. 2014, 29, 1119–1124. [Google Scholar] [CrossRef]
- An, C.M.; Park, Y.H. The effects of semi-immersive virtual reality therapy on standing balance and upright mobility function in individuals with chronic incomplete spinal cord injury: A preliminary study. J. Spinal Cord Med. 2018, 41, 223–229. [Google Scholar] [CrossRef]
- Biffi, E.; Beretta, E.; Cesareo, A.; Maghini, C.; Turconi, A.C.; Reni, G.; Strazzer, S. An Immersive Virtual Reality Platform to Enhance Walking Ability of Children with Acquired Brain Injuries. Methods Inf. Med. 2017, 56, 119–126. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability and Health (ICF); World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Chen, Y.; Fanchiang, H.D.; Howard, A. Effectiveness of Virtual Reality in Children With Cerebral Palsy: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Phys. Ther. 2018, 98, 63–77. [Google Scholar] [CrossRef] [PubMed]
- Cho, C.; Hwang, W.; Hwang, S.; Chung, Y. Treadmill Training with Virtual Reality Improves Gait, Balance, and Muscle Strength in Children with Cerebral Palsy. Tohoku J. Exp. Med. 2016, 238, 213–218. [Google Scholar] [CrossRef]
- Mukhopadhyay, S.C. Wearable sensors for human activity monitoring: A review. IEEE Sens. J. 2015, 15, 1321–1330. [Google Scholar] [CrossRef]
- Placidi, G.; Cinque, L.; Polsinelli, M.; Spezialetti, M. Measurements by a LEAP-based virtual glove for the hand rehabilitation. Sensors 2018, 18, 834. [Google Scholar] [CrossRef]
- Laffont, I.; Bakhti, K.; Coroian, F.; van Dokkum, L.; Mottet, D.; Schweighofer, N.; Froger, J. Innovative technologies applied to sensorimotor rehabilitation after stroke. Ann. Phys. Rehabil. Med. 2014, 57, 543–551. [Google Scholar] [CrossRef]
- Cavalcanti, V.C.; Santana, M.I.D.; Gama, A.E.F.D.; Correia, W.F.M. Usability assessments for augmented reality motor rehabilitation solutions: A systematic review. Int. J. Comput. Games Technol. 2018, 2018. [Google Scholar] [CrossRef]
- Zeni, J.; Richards, J.; Higginson, J. Two simple methods for determining gait events during treadmill and overground walking using kinematic data. Gait Posture 2008, 27, 710–714. [Google Scholar] [CrossRef]
- Desailly, E.; Daniel, Y.; Sardain, P.; Lacouture, P. Foot contact event detection using kinematic data in cerebral palsy children and normal adults gait. Gait Posture 2009, 29, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves, R.V.; Fonseca, S.T.; Araújo, P.A.; Araújo, V.L.; Barboza, T.M.; Martins, G.A.; Mancini, M.C. Identification of gait events in children with spastic cerebral palsy: Comparison between the force plate and algorithms. Braz. J. Phys. Ther. 2020, 24, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Zijlstra, W.; Hof, A.L. Assessment of spatio-temporal gait parameters from trunk accelerations during human walking. Gait Posture 2003, 18, 1–10. [Google Scholar] [CrossRef]
- Trojaniello, D.; Cereatti, A.; Pelosin, E.; Avanzino, L.; Mirelman, A.; Hausdorff, J.M.; Della Croce, U. Estimation of step-by-step spatio-temporal parameters of normal and impaired gait using shank-mounted magneto-inertial sensors: Application to elderly, hemiparetic, parkinsonian and choreic gait. J. Neuroeng. Rehabil. 2014, 11, 152. [Google Scholar] [CrossRef]
- Trojaniello, D.; Cereatti, A.; Della Croce, U. Accuracy, sensitivity and robustness of five different methods for the estimation of gait temporal parameters using a single inertial sensor mounted on the lower trunk. Gait Posture 2014, 40, 487–492. [Google Scholar] [CrossRef]
- McCamley, J.; Donati, M.; Grimpampi, E.; Mazzà, C. An enhanced estimate of initial contact and final contact instants of time using lower trunk inertial sensor data. Gait Posture 2012, 36, 316–318. [Google Scholar] [CrossRef]
- Storm, F.A.; Buckley, C.J.; Mazzà, C. Gait event detection in laboratory and real life settings: Accuracy of ankle and waist sensor based methods. Gait Posture 2016, 50, 42–46. [Google Scholar] [CrossRef]
- Figueiredo, J.; Felix, P.; Costa, L.; Moreno, J.C.; Santos, C.P. Gait event detection in controlled and real-life situations: Repeated measures from healthy subjects. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1945–1956. [Google Scholar] [CrossRef] [PubMed]
- Ju, Y. Footstep Detection with HoloLens. Am. J. Eng. Res. 2018, 7, 223–233. [Google Scholar]
- Geerse, D.J.; Coolen, B.; Roerdink, M. Quantifying spatiotemporal gait parameters with HoloLens in healthy adults and people with Parkinson’s disease: Test-retest reliability, concurrent validity, and face validity. Sensors 2020, 20, 3216. [Google Scholar] [CrossRef]
- Sala, D.A.; Grissom, H.E.; Delsole, E.M.; Chu, M.L.; Godfried, D.H.; Bhattacharyya, S.; Karamitopoulos, M.S.; Chu, A. Measuring ambulation with wrist-based and hip-based activity trackers for children with cerebral palsy. Dev. Med. Child Neurol. 2019, 61, 1309–1313. [Google Scholar] [CrossRef]
- Kuo, Y.L.; Culhane, K.M.; Thomason, P.; Tirosh, O.; Baker, R. Measuring distance walked and step count in children with cerebral palsy: An evaluation of two portable activity monitors. Gait Posture 2009, 29, 304–310. [Google Scholar] [CrossRef]
- O’ Donoghue, D.; Kennedy, N. Validity of an activity monitor in young people with cerebral palsy gross motor function classification system level I. Physiol. Meas. 2014, 35, 2307–2318. [Google Scholar] [CrossRef] [PubMed]
- Paraschiv-Ionescu, A.; Newman, C.J.; Carcreff, L.; Gerber, C.N.; Armand, S.; Aminian, K. Locomotion and cadence detection using a single trunk-fixed accelerometer: Validity for children with cerebral palsy in daily life-like conditions. J. Neuroeng. Rehabil. 2019, 16, 24. [Google Scholar] [CrossRef] [PubMed]
- Glowinski, S.; Łosiński, K.; Kowiański, P.; Waśkow, M.; Bryndal, A.; Grochulska, A. Inertial Sensors as a Tool for Diagnosing Discopathy Lumbosacral Pathologic Gait: A Preliminary Research. Diagnostics 2020, 10, 342. [Google Scholar] [CrossRef]
- Guinet, A.; Bouyer, G.; Otmane, S.; Desailly, E. Reliability of the head tracking measured by Microsoft Hololens during different walking conditions. Comput. Methods Biomech. Biomed. Eng. 2019, 22, S169–S171. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef] [PubMed]
- Microsoft. The Microsoft HoloLens (1st Gen) Hardware. Available online: https://docs.microsoft.com/en-us/hololens/hololens1-hardware (accessed on 21 October 2020).
- Capela, N.A.; Lemaire, E.D.; Baddour, N. Novel algorithm for a smartphone-based 6-minute walk test application: Algorithm, application development, and evaluation. J. Neuroeng. Rehabil. 2015, 12, 19. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kim, S.M.; Lho, H.; Cho, W.D. Real-Time Step-Count Detection and Activity Monitoring Using A Triaxial Accelerometer. Intell. Autom. Soft Comput. 2012, 18, 247–261. [Google Scholar] [CrossRef]
- Yang, M.; Zheng, H.; Wang, H.; McClean, S.; Newell, D. iGAIT: An interactive accelerometer based gait analysis system. Comput. Methods Programs Biomed. 2012, 108, 715–723. [Google Scholar] [CrossRef]
- Besl, P.; McKay, N. A method for Registration of 3-D Shapes. IEEE Trans. Pattern Anal. 1992, 14, 239–256. [Google Scholar] [CrossRef]
- Chen, Y.; Medioni, G. Object modelling by registration of multiple range images. Image Vis. Comput. 1992, 10, 145–155. [Google Scholar] [CrossRef]
- McGraw, K.O.; Wong, S.P. Forming inferences about some intraclass correlation coefficients. Psychol. Methods 1996, 1, 30–46. [Google Scholar] [CrossRef]
- Sun, R.; Aldunate, R.G.; Sosnoff, J.J. The validity of a mixed reality-based automated functional mobility assessment. Sensors 2019, 19, 2183. [Google Scholar] [CrossRef] [PubMed]
- Hsue, B.J.; Miller, F.; Su, F.C. The dynamic balance of the children with cerebral palsy and typical developing during gait. Gait Posture 2009, 29, 471–476. [Google Scholar] [CrossRef]
- Yamazoe, H.; Mitsugami, I.; Okada, T.; Yagi, Y. Analysis of head and chest movements that correspond to gaze directions during walking. Exp. Brain Res. 2019, 237, 3047–3058. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Acceleration patterns of the head and pelvis when walking on level and irregular surfaces. Gait Posture 2003, 18, 35–46. [Google Scholar] [CrossRef]
- Psarakis, M.; Greene, D.A.; Cole, M.H.; Lord, S.R.; Hoang, P.; Brodie, M. Wearable technology reveals gait compensations, unstable walking patterns and fatigue in people with multiple sclerosis. Physiol. Meas. 2018, 39, 075004. [Google Scholar] [CrossRef] [PubMed]
- Heyrman, L.; Feys, H.; Molenaers, G.; Jaspers, E.; Van de Walle, P.; Monari, D.; Aertbeliën, E.; Desloovere, K. Reliability of head and trunk kinematics during gait in children with spastic diplegia. Gait Posture 2013, 37, 424–429. [Google Scholar] [CrossRef] [PubMed]
- Peñeñory, V.M.; Collazos, C.A.; Bacca, A.F.; Manresa-Yee, C.; Cano, S.P.; Fadoun, H.M. APRehab: A methodology for serious games design oriented to psychomotor rehabilitation in children with hearing impairments. Univers. Access Inf. Soc. 2020. [Google Scholar] [CrossRef]
- Amengual Alcover, E.; Jaume-i Capó, A.; Moyà-Alcover, B.; Martinuzzi, A. PROGame: A process framework for serious game development for motor rehabilitation therapy. PLoS ONE 2018, 13, e0197383. [Google Scholar] [CrossRef] [PubMed]
- Gil-Gómez, J.A.; Manzano-Hernández, P.; Albiol-Pérez, S.; Aula-Valero, C.; Gil-Gómez, H.; Lozano-Quilis, J.A. USEQ: A Short Questionnaire for Satisfaction Evaluation of Virtual Rehabilitation Systems. Sensors 2017, 17, 1589. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Healthy Participant (n = 13) | Children Group 1 (n = 32) | Children Group 2 (n = 30) |
|---|---|---|---|
| Age (mean) | 35.9 | 12.6 | 12.3 |
| Sex (F/M) | 5/8 | 16/16 | 13/17 |
| GMFCS | NA | I | II–III |
| Walking aids | No | No | Crutches (18) |
| Posterior walker (12) |
| Sensitivity | Specificity | Accuracy | Precision | |
|---|---|---|---|---|
| Healthy participant (n = 13) | 0.969 | 1.000 | 0.999 | 1.000 |
| Children Group 1 (n = 32) | 0.969 | 0.999 | 0.999 | 0.964 |
| Children Group 2 (n = 30) | 0.989 | 1.000 | 1.000 | 0.984 |
| All CP children (n = 62) | 0.979 | 1.000 | 0.999 | 0.974 |
| MOCAP Zeni | Hololens HMD HoloStep | ||||||
|---|---|---|---|---|---|---|---|
| Mean +/− SD | Mean +/− SD | Bias (95% LoA) | t-statistics | ICC(A,1) | r corr | ||
| Walking Speed (m/s) | CP-Group 1 | 1.044 +/− 0.254 | 1.026 +/− 0.258 | 0.018 (−0.012 0.048) | t(30) = −0.28, p = 0.78 | 0.996 | 0.998 |
| CP-Group 2 | 0.667 +/− 0.180 | 0.648 +/− 0.174 | 0.018 (−0.017 0.053) | t(28) = −0.40, p = 0.69 | 0.990 | 0.995 | |
| HP | 1.277 +/− 0.199 | 1.242 +/− 0.197 | 0.035 (−0.026 0.096) | t(11) = −0.45, p = 0.66 | 0.973 | 0.988 | |
| Step Length (m) | CP-Group 1 | 0.488 +/− 0.090 | 0.514 +/− 0.105 | 0.017 (−0.106 0.140) | t(30) = 1.07, p = 0.29 | 0.922 | 0.885 |
| CP-Group 2 | 0.430 +/− 0.064 | 0.434 +/− 0.079 | 0.005 (−0.152 0.162) | t(28) = 0.18, p = 0.86 | 0.863 | 0.649 | |
| HP | 0.623 +/− 0.079 | 0.679 +/− 0.087 | 0.054 (−0.048 0.156) | t(11) = 1.74, p = 0.095 | 0.778 | 0.802 | |
| Cadence (steps/s) | CP-Group 1 | 1.980 +/− 0.272 | 1.838 +/− 0.267 | 0.142 (−0.249 0.534) | t(30) = −2.11, p = 0.29 | 0.642 | 0.726 |
| CP-Group 2 | 1.178 +/− 0.308 | 1.425 +/− 0.294 | −0.247 (−0.589 0.095) | t(28) = 3.18, p = 0.86 | 0.625 | 0.833 | |
| HP | 1.908 +/− 0.196 | 1.808 +/− 0.231 | 0.0099 (−0.288 0.486) | t(11) = −1.18, p = 0.095 | 0.534 | 0.582 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guinet, A.-L.; Bouyer, G.; Otmane, S.; Desailly, E. Validity of Hololens Augmented Reality Head Mounted Display for Measuring Gait Parameters in Healthy Adults and Children with Cerebral Palsy. Sensors 2021, 21, 2697. https://doi.org/10.3390/s21082697
Guinet A-L, Bouyer G, Otmane S, Desailly E. Validity of Hololens Augmented Reality Head Mounted Display for Measuring Gait Parameters in Healthy Adults and Children with Cerebral Palsy. Sensors. 2021; 21(8):2697. https://doi.org/10.3390/s21082697
Chicago/Turabian StyleGuinet, Anne-Laure, Guillaume Bouyer, Samir Otmane, and Eric Desailly. 2021. "Validity of Hololens Augmented Reality Head Mounted Display for Measuring Gait Parameters in Healthy Adults and Children with Cerebral Palsy" Sensors 21, no. 8: 2697. https://doi.org/10.3390/s21082697
APA StyleGuinet, A.-L., Bouyer, G., Otmane, S., & Desailly, E. (2021). Validity of Hololens Augmented Reality Head Mounted Display for Measuring Gait Parameters in Healthy Adults and Children with Cerebral Palsy. Sensors, 21(8), 2697. https://doi.org/10.3390/s21082697






