Automated Real-Time Evaluation of Condylar Movement in Relation to Three-Dimensional Craniofacial and Temporomandibular Morphometry in Patients with Facial Asymmetry
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. 3D Morphometric Analysis
2.2.1. Craniofacial Morphology
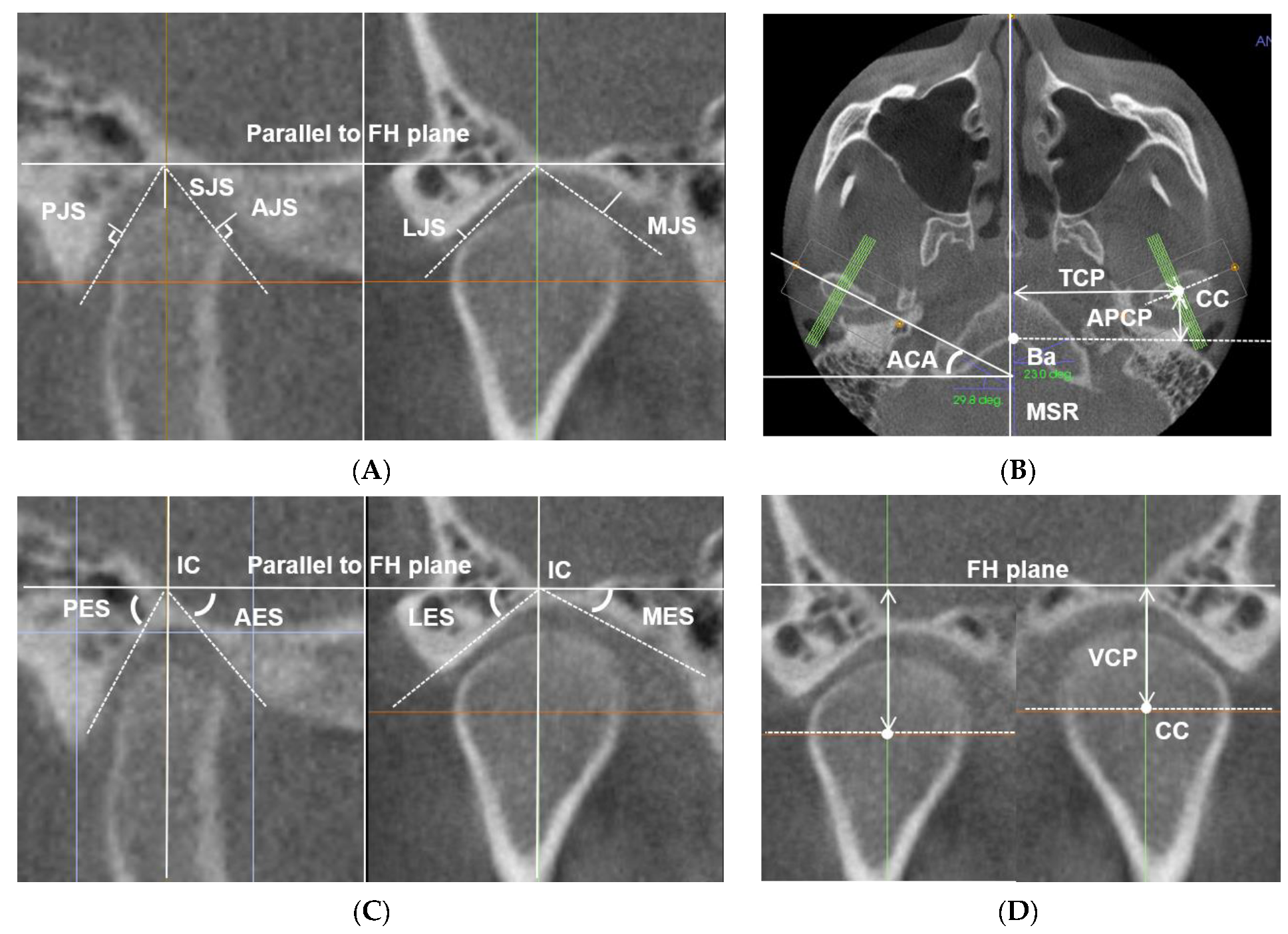
2.2.2. Temporomandibular Joint (TMJ) Morphology
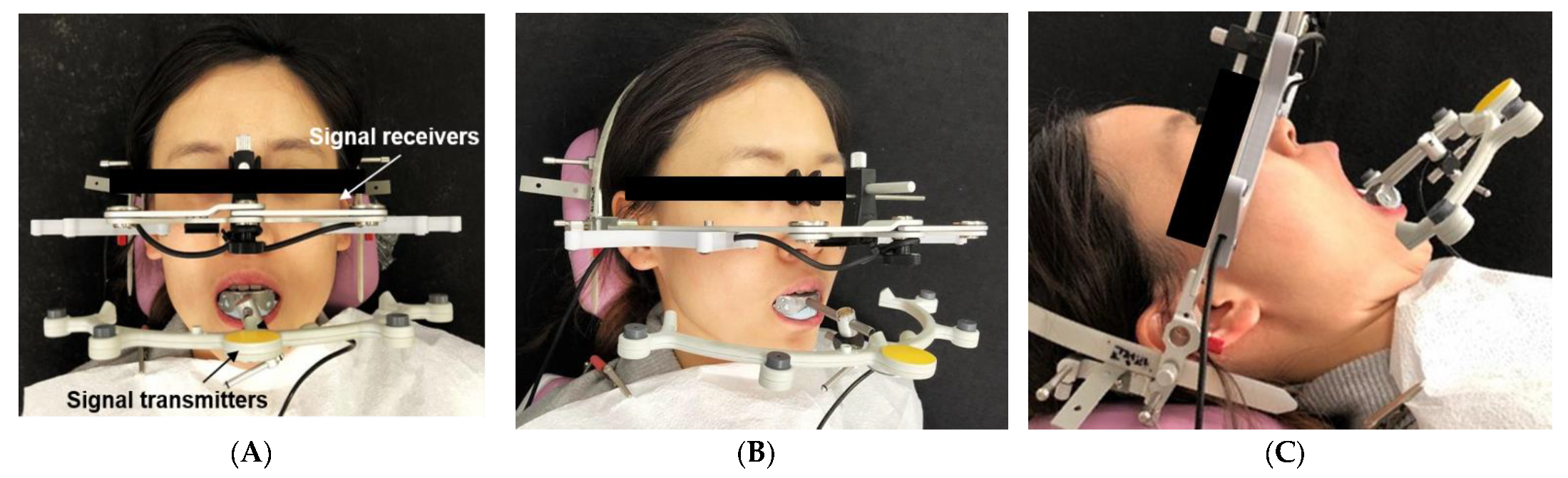
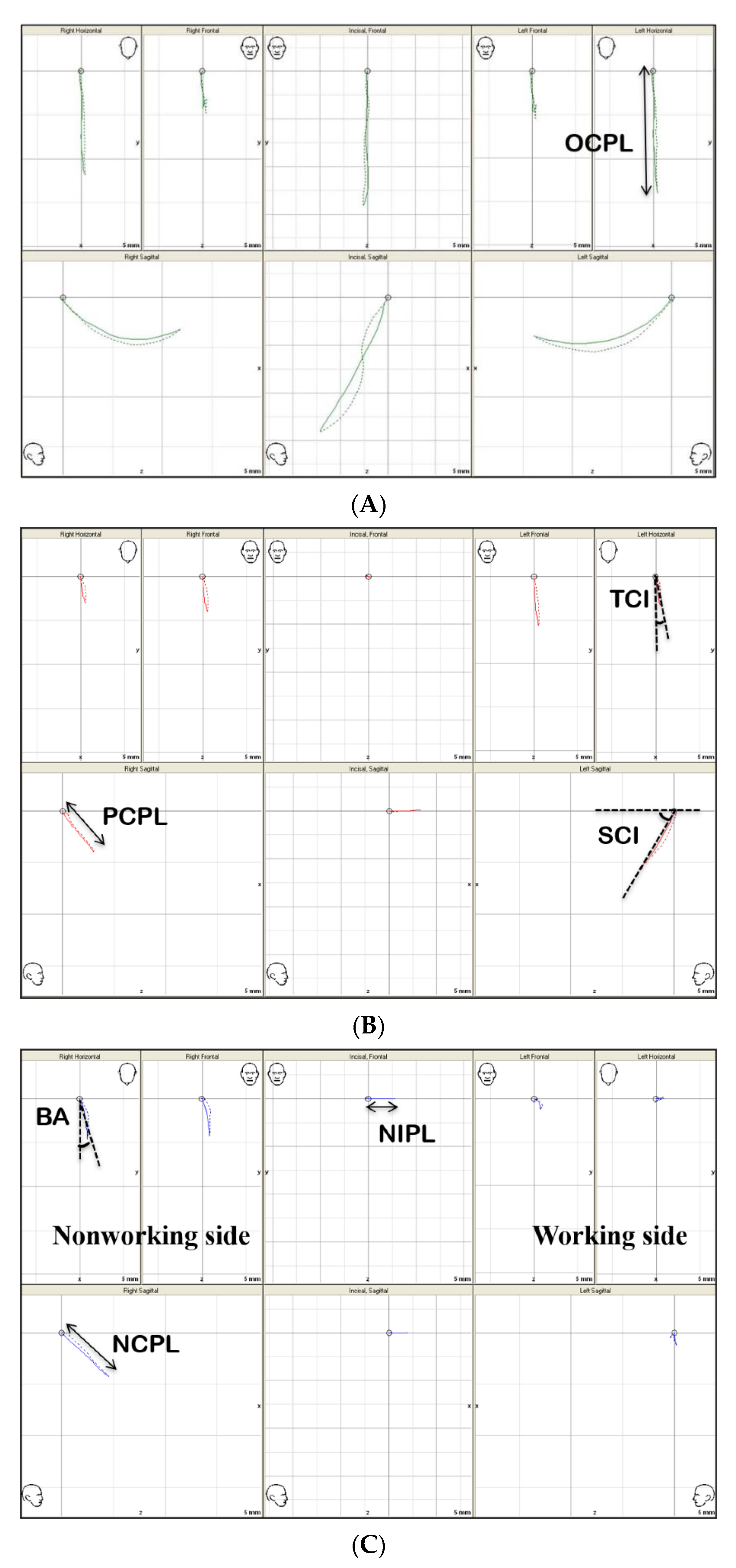
2.3. 3D Mandibular Movement Analysis
2.4. Statistical Analysis
3. Results
3.1. Comparison of Overall Measurements between the Deviated and Nondeviated Sides
3.2. Correlation between Craniofacial Morphology, TMJ Morphometry, and TMJ Function
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mimura, H.; Deguchi, T. Relationship between sagittal condylar path and the degree of mandibular asymmetry in unilateral cross-bite patients. J. Craniomandib. Prac. 1994, 12, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Biljana, T.; Paul, M.; Brian, N.; Narasimha, P. Craniofacial asymmetry and temporomandibular joint internal derangement in female adolescents: A posteroanterior cephalometric study. Angle Orthod. 2000, 70, 81–88. [Google Scholar]
- Fukui, T.; Satoh, Y.; Yamada, K.; Morita, S.; Hanada, K. Relationship between mandibular lateral deviation and bilateral condylar paths on mandibular protrusive movement. J. Jpn. Orthod. Soc. 1992, 51, 203. [Google Scholar]
- Ishizaki, K.; Suzuki, K.; Mito, T.; Tanaka, E.M.; Sato, S. Morphologic, functional, and occlusal characterization of mandibular lateral displacement malocclusion. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 454.e1–454.e9. [Google Scholar] [CrossRef]
- Buranastidporn, B.; Hisano, M.; Soma, K. Temporomandibular joint internal derangement in mandibular asymmetry. What is the relationship? Eur. J. Orthod. 2006, 28, 83–88. [Google Scholar] [CrossRef]
- Hashimoto, T.; Kuroda, S.; Lihua, E.; Tanimoto, Y.; Miyawaki, S.; Takano-Yamamoto, T. Correlation between craniofacial and condylar path asymmetry. J. Oral Maxillofac. Surg. 2008, 66, 2020–2027. [Google Scholar] [CrossRef] [PubMed]
- Pelletier, L.B.; Campbell, S.D. Comparison of condylar control settings using three methods: A bench study. J. Prosthet. Dent. 1991, 66, 193–200. [Google Scholar] [CrossRef]
- Eriksson, P.O.; Häggman-Henrikson, B.; Nordh, E.; Zafar, H. Co-ordinated mandibular and head-neck movements during rhythmic jaw activities in man. J. Dent. Res. 2000, 79, 1378–1384. [Google Scholar] [CrossRef]
- Fukui, T.; Tsuruta, M.; Murata, K.; Wakimoto, Y.; Tokiwa, H.; Kuwahara, Y. Correlation between facial morphology, mouth opening ability, and condylar movement during opening-closing jaw movements in female adults with normal occlusion. Eur. J. Orthod. 2002, 24, 327–336. [Google Scholar] [CrossRef]
- Gerstner, G.E.; Marchi, F.; Haerian, H. Relationship between anteroposterior maxillomandibular morphology and masticatory jaw movement patterns. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 258–266. [Google Scholar] [CrossRef]
- Farella, M.; Iodice, G.; Michelotti, A.; Leonardi, R. The relationship between vertical craniofacial morphology and the sagittal path of mandibular movements. J. Oral Rehabil. 2005, 32, 857–862. [Google Scholar] [CrossRef]
- Baqaien, M.A.; Al-Salti, F.M.; Muessig, D. Changes in condylar path inclination during maximum protrusion between the ages of 6 and 12 years. J. Oral Rehabil. 2007, 34, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Baqaien, M.A.; Barra, J.; Muessig, D. Computerized axiographic evaluation of the changes in sagittal condylar path inclination with dental and physical development. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Choi, B.T.; Hwang, D.Y.; Lee, G.H.; Moon, D.N.; Lee, K.M. Computerized ultrasonic axiographic evaluation of condylar movement in patients with internal derangement of the temporomandibular joint. Angle Orthod. 2019, 89, 924–929. [Google Scholar] [CrossRef] [PubMed]
- Prasad, K.D.; Shetty, M.; Chandy, B.K. Evaluation of condylar inclination of dentulous subjects determined by axiograph and to compare with manual programming of articulators using protrusive interocclusal record. Contemp. Clin. Dent. 2015, 6, 371. [Google Scholar] [PubMed]
- Pirttineimi, P.; Kantomaa, T.; Lahtela, P. Relationship between craniofacial and condyle path asymmetry in unilateral crossbite patients. Eur. J. Orthod. 1991, 12, 408–413. [Google Scholar] [CrossRef]
- Inui, M.; Fushima, K.; Sato, S. Facial asymmetry in temporomandibular joint disorders. J. Oral Rehabil. 1999, 26, 402–406. [Google Scholar] [CrossRef]
- Fujisaki, T. Condylar movement in patient with skeletal mandibular prognathism during maximum opening and closing movement before and after surgery. Kokubyo Gakkai Zasschi 1996, 63, 408–421. [Google Scholar] [CrossRef][Green Version]
- Corbett, N.E.; DeVincenzo, J.P.; Huffer, R.A.; Shryock, E.F. The relation of the condylar path to the articular eminence in mandibular protrusion. Angle Orthod. 1971, 41, 286–292. [Google Scholar]
- Pirttiniemi, P.; Raustia, A.; Kantomaa, T.; Pyhtinen, J. Relationships of bicondylar position to occlusal asymmetry. Eur. J. Orthod. 1991, 13, 441–445. [Google Scholar] [CrossRef]
- Ueki, K.; Nakagawa, K.; Takatsuka, S.; Shimada, M.; Marukawa, K.; Takazakura, D.; Yamamoto, E. Temporomandibular joint morphology and disc position in skeletal Class III patients. J. Craniomaxillofac. Surg. 2000, 28, 362–368. [Google Scholar] [CrossRef]
- Ingervall, B. Variation of the range of movement of the mandible in relation to facial morphology in young adults. Eur. J. Oral Sci. 1971, 79, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, M.; Miyamoto, J.J.; Takada, J.I.; Moriyama, K. Association between 3-dimensional mandibular morphology and condylar movement in subjects with mandibular asymmetry. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 324–334. [Google Scholar] [CrossRef] [PubMed]
- Sümbüllü, M.A.; Çağlayan, F.; Akgül, H.M.; Yilmaz, A.B. Radiological examination of the articular eminence morphology using cone beam CT. Dentomaxillofac. Radiol. 2012, 41, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Hatice, G.; Hakan, T.; Nureddin, B. Correlation between eminence steepness and condyle disc movements in temporomandibular joints with internal derangements on magnetic resonance imaging. Eur. J. Orthod. 2001, 23, 579–584. [Google Scholar]
- Oguri, Y.; Yamada, K.; Fukui, T.; Hanada, K.; Kohno, S. Mandibular movement and frontal craniofacial morphology in orthognathic surgery patients with mandibular deviation and protrusion. J. Oral Rehabil. 2003, 30, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Huh, K.H.; Lee, S.S.; Heo, M.S.; Choi, S.C.; Hwang, S.J.; Yi, W.J. The relationship between the changes in three-dimensional facial morphology and mandibular movement after orthognathic surgery. J. Cranio Maxllofac. Surg. 2013, 41, 686–693. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.S.; Choi, S.C.; Lee, S.S.; Heo, M.S.; Huh, K.H.; Hwang, S.J.; Yi, W.J. Correlation between 3-dimensional facial morphology and mandibular movement during maximum mouth opening and closing. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 110, 648–656. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.A.; Lee, J.W.; Park, J.H.; Kim, B.H.; Ahn, H.W.; Kim, S.J. Targeted presurgical decompensation in patients with yaw-dependent facial asymmetry. Korean J. Orthod. 2017, 47, 195–206. [Google Scholar] [CrossRef]
- Ueki, K.; Nakagawa, K.; Takatsuka, S.; Yamamoto, E. Plate fixation after mandibular osteotomy. Int. J. Oral Maxillofac. Surg. 2001, 30, 490–496. [Google Scholar] [CrossRef]
- Kobayashi, T.; Honma, K.; Izumi, K.; Hayashi, T.; Shingaki, S.; Nakajima, T. Temporomandibular joint symptoms and disc displacement in patients with mandibular prognathism. Br. J. Oral Maxillofac. Surg. 1999, 37, 455–458. [Google Scholar] [CrossRef]
- Ueki, K.; Hashiba, Y.; Marukawa, K.; Nakagawa, K.; Alam, S.; Okabe, K.; Yamamoto, E. The effects of changing position and angle of the proximal segment after intraoral vertical ramus osteotomy. Int. J. Oral Maxillofac. Surg. 2009, 38, 1041–1047. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Hanada, K.; Hayashi, T.; Ito, J. Condylar bony change, disc displacement, and signs and symptoms of TMJ disorders in orthognathic surgery patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2001, 91, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Saccucci, M.; D’Attilio, M.; Rodolfino, D.; Festa, F.; Polimeni, A.; Tecco, S. Condylar volume and condylar area in class I, class II and class III young adult subjects. Head Face Med. 2012, 8, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, B.; Jäger, A.; Kubein-Meesenburg, D. Comparison of “normal” TMJ in Class I, II, and III individuals. Eur. J. Orthod. 1991, 13, 27–34. [Google Scholar] [CrossRef]

| Representative Variables | Deviation Side (n = 30) | Non-Deviation Side (n = 30) | p-Value | Effect Size | Power (%) | No. of 80% Power (Each Group) |
|---|---|---|---|---|---|---|
| Anterior eminence steepness (AES) [°] | 46.54 ± 10.97 | 39.87 ± 8.66 | <0.000 *** | 0.6763 | 93.17 | 20 |
| Protrusive condylar path length (PCPL) [mm] | 6.97 ± 2.09 | 6.12 ± 1.83 | 0.001 ** | 1.0164 | 99.94 | 10 |
| Non-working condylar path length (NCPL) [mm] | 7.40 ± 1.98 | 6.02 ± 1.78 | <0.000 *** | 0.9225 | 99.69 | 12 |
| Compartment | Variables | Deviated Side | Non-Deviated Side | p-Value | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Craniofacial morphology (cm) | Maxillary height (MxH) [mm] | 49.67 | 3.56 | 50.45 | 3.30 | 0.264 | |
| Ramal height (RH) [mm] | 45.91 | 5.39 | 48.40 | 4.24 | 0.028 * | ||
| Frontal ramal inclination (FRI) [°] | 82.34 | 3.70 | 77.00 | 3.31 | 0.000 *** | ||
| Lateral ramal inclination (LRI) [°] | 86.41 | 6.84 | 83.93 | 5.59 | 0.014 * | ||
| Mandibular body length (BL) [mm] | 74.62 | 5.05 | 75.58 | 5.72 | 0.129 | ||
| TMJ morphometry (tm) | Condyle position relative to cranial base | Anteroposterior condylar posture (APCP) [mm] | 13.21 | 3.33 | 13.80 | 3.16 | 0.234 |
| Transverse condylar posture (TCP) [mm] | 52.03 | 2.51 | 52.77 | 2.40 | 0.137 | ||
| Vertical condylar posture (VCP) [mm] | 8.72 | 3.07 | 8.29 | 3.05 | 0.275 | ||
| Condyle position relative to eminence | Anterior joint space (AJS) [mm] | 2.13 | 0.71 | 1.74 | 0.53 | 0.362 | |
| Superior joint space (SJS) [mm] | 2.05 | 0.71 | 2.26 | 0.93 | 0.516 | ||
| Posterior joint space (PJS) [mm] | 1.59 | 0.46 | 2.01 | 0.68 | 0.882 | ||
| Medial joint space (MJS) [mm] | 2.65 | 0.69 | 1.60 | 0.51 | 0.002 ** | ||
| Lateral joint space (LJS) [mm] | 1.48 | 0.59 | 1.77 | 0.49 | 0.377 | ||
| Axial condylar angle (ACA) [°] | 21.18 | 6.37 | 17.23 | 6.00 | 0.019 * | ||
| Eminence steepness | Anterior eminence steepness (AES) [°] | 46.49 | 9.21 | 39.10 | 7.39 | 0.000 *** | |
| Posterior eminence steepness (PES) [°] | 58.30 | 9.03 | 58.84 | 6.60 | 0.988 | ||
| Medial eminence steepness (MES) [°] | 48.72 | 12.17 | 49.10 | 9.29 | 0.802 | ||
| Lateral eminence steepness (LES) [°] | 37.77 | 7.97 | 39.62 | 6.73 | 0.066 | ||
| TMJ function (tf) | Opening condylar path length (OCPL) [mm] | 15.27 | 2.75 | 14.21 | 3.60 | 0.338 | |
| Protrusive condylar path length (PCPL) [mm] | 9.18 | 1.73 | 6.88 | 1.64 | 0.001 ** | ||
| Sagittal condylar inclination (SCI) [°] | 44.39 | 5.21 | 39.57 | 7.48 | 0.002 ** | ||
| Transverse condylar inclination (TCI) [°] | 4.20 | 2.86 | −2.44 | 2.23 | 0.031 * | ||
| Bennet angle (BA) [°] | 14.39 | 3.99 | 9.11 | 2.35 | 0.041 * | ||
| Non-working condylar path length (NCPL) [mm] | 8.15 | 1.46 | 6.12 | 1.70 | 0.000 *** | ||
| Non-working incisal path length (NIPL) [mm] | 6.59 | 1.18 | 5.81 | 1.03 | 0.001 ** | ||
| Deviated Side | Non-Deviated Side | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TMJ Function (tf) | OCPL [mm] | PCPL [mm] | SCI [°] | NIPL [mm] | NCPL [mm] | OCPL [mm] | PCPL [mm] | SCI [°] | NIPL [mm] | NCPL [mm] | ||
| Cranio facial morphology [cm] | MxH [mm] | R | 0.137 | −0.168 | 0.190 | −0.067 | 0.252 | 0.101 | −0.025 | 0.203 | 0.204 | 0.080 |
| P | 0.488 | 0.392 | 0.334 | 0.734 | 0.196 | 0.609 | 0.898 | 0.301 | 0.297 | 0.685 | ||
| RH [mm] | R | 0.116 | −0.157 | −0.155 | −0.168 | −0.092 | 0.094 | 0.130 | −0.049 | −0.234 | 0.222 | |
| P | 0.558 | 0.424 | 0.431 | 0.393 | 0.642 | 0.636 | 0.509 | 0.803 | 0.231 | 0.257 | ||
| FRI [°] | R | 0.257 | 0.787 | 0.245 | 0.242 | 0.209 | −0.282 | −0.284 | 0.153 | 0.095 | −0.051 | |
| P | 0.186 | 0.009 ** | 0.209 | 0.214 | 0.286 | 0.146 | 0.144 | 0.438 | 0.632 | 0.795 | ||
| LRI [°] | R | 0.134 | 0.025 | 0.302 | 0.139 | 0.075 | 0.221 | 0.231 | 0.332 | 0.041 | 0.025 | |
| P | 0.498 | 0.900 | 0.119 | 0.480 | 0.705 | 0.259 | 0.238 | 0.084 | 0.834 | 0.900 | ||
| BL [mm] | R | −0.091 | −0.170 | 0.035 | −0.352 | −0.096 | −0.270 | −0.001 | 0.025 | 0.012 | 0.067 | |
| P | 0.646 | 0.387 | 0.860 | 0.067 | 0.627 | 0.164 | 0.998 | 0.899 | 0.953 | 0.736 | ||
| TMJ morphometry [tm] | AJS [mm] | R | −0.017 | 0.612 | 0.046 | 0.270 | 0.316 | 0.168 | 0.176 | 0.237 | −0.236 | −0.189 |
| P | 0.930 | 0.029 * | 0.817 | 0.165 | 0.102 | 0.393 | 0.370 | 0.225 | 0.227 | 0.335 | ||
| SJS [mm] | R | −0.019 | 0.189 | 0.157 | 0.212 | 0.117 | 0.348 | 0.203 | −0.109 | 0.127 | 0.045 | |
| P | 0.924 | 0.336 | 0.424 | 0.278 | 0.553 | 0.070 | 0.299 | 0.581 | 0.520 | 0.819 | ||
| PJS [mm] | R | −0.219 | −0.004 | 0.032 | 0.165 | −0.002 | 0.360 | 0.183 | −0.138 | 0.233 | 0.000 | |
| P | 0.263 | 0.984 | 0.872 | 0.402 | 0.992 | 0.060 | 0.351 | 0.485 | 0.233 | 0.998 | ||
| MJS [mm] | R | −0.008 | 0.675 | −0.020 | 0.347 | 0.210 | −0.845 | 0.321 | −0.239 | 0.167 | 0.105 | |
| P | 0.966 | 0.011* | 0.918 | 0.070 | 0.284 | 0.000 *** | 0.096 | 0.221 | 0.396 | 0.595 | ||
| LJS [mm] | R | 0.174 | 0.336 | 0.242 | 0.327 | 0.150 | 0.451 | 0.255 | 0.169 | 0.335 | 0.166 | |
| P | 0.376 | 0.081 | 0.215 | 0.089 | 0.446 | 0.105 | 0.190 | 0.390 | 0.081 | 0.397 | ||
| ACA [°] | R | 0.183 | 0.713 | 0.046 | 0.337 | 0.194 | 0.267 | 0.334 | 0.239 | −0.102 | −0.174 | |
| P | 0.352 | 0.029 * | 0.816 | 0.079 | 0.323 | 0.170 | 0.082 | 0.221 | 0.604 | 0.377 | ||
| AES [°] | R | 0.264 | 0.797 | 0.348 | 0.595 | 0.335 | 0.191 | 0.164 | 0.736 | 0.151 | 0.204 | |
| P | 0.175 | 0.007 ** | 0.069 | 0.105 | 0.081 | 0.329 | 0.403 | 0.020* | 0.442 | 0.299 | ||
| PES [°] | R | −0.144 | −0.044 | 0.284 | −0.147 | 0.082 | −0.240 | −0.100 | 0.233 | 0.173 | 0.283 | |
| P | 0.466 | 0.825 | 0.143 | 0.456 | 0.678 | 0.218 | 0.614 | 0.232 | 0.379 | 0.145 | ||
| MES [°] | R | 0.332 | −0.127 | 0.076 | −0.215 | 0.134 | −0.106 | −0.126 | −0.172 | 0.087 | −0.006 | |
| P | 0.084 | 0.518 | 0.702 | 0.271 | 0.498 | 0.591 | 0.521 | 0.380 | 0.659 | 0.978 | ||
| LES [°] | R | −0.056 | −0.057 | 0.003 | 0.005 | −0.045 | 0.129 | −0.028 | 0.071 | 0.180 | 0.103 | |
| P | 0.776 | 0.772 | 0.988 | 0.978 | 0.821 | 0.512 | 0.889 | 0.720 | 0.360 | 0.601 | ||
| Variables | Components | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| NCPL_tf | 0.773 | −0.061 | −0.056 | −0.059 |
| PCPL_tf | 0.765 | 0.213 | −0.036 | −0.371 |
| AES_tm | 0.690 | 0.502 | −0.032 | 0.080 |
| NIPL_tf | 0.644 | 0.288 | −0.224 | −0.263 |
| FRI_cm | 0.634 | 0.044 | 0.194 | −0.016 |
| SCI_tf | 0.530 | −0.108 | −0.216 | 0.365 |
| OCPL_tf | 0.449 | −0.112 | −0.063 | 0.198 |
| MES_tm | 0.187 | −0.751 | 0.146 | 0.059 |
| MJS_tm | 0.407 | 0.676 | 0.438 | −0.124 |
| SJS_tm | 0.183 | 0.659 | 0.133 | 0.328 |
| ACA_tm | 0.283 | 0.651 | 0.038 | −0.250 |
| LRI_cm | 0.119 | 0.272 | −0.804 | 0.313 |
| BL_cm | −0.074 | −0.028 | 0.759 | 0.157 |
| RH_cm | −0.040 | 0.151 | 0.706 | 0.391 |
| MxH_cm | 0.154 | −0.011 | 0.308 | 0.722 |
| AJS_tm | 0.320 | 0.207 | 0.049 | −0.708 |
| Variables | Components | |||
|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |
| ACA_tm | 0.769 | −0.206 | −0.047 | 0.079 |
| OCPL_tf | 0.729 | 0.063 | −0.492 | 0.311 |
| SCI_tf | 0.680 | 0.360 | 0.461 | −0.036 |
| AES_tm | 0.670 | 0.349 | 0.204 | −0.085 |
| NCPL_tf | −0.037 | 0.865 | 0.005 | 0.066 |
| NIPL_tf | 0.017 | 0.804 | −0.017 | −0.014 |
| PCPL_tf | 0.381 | 0.638 | −0.353 | 0.158 |
| FRI_cm | 0.038 | −0.014 | 0.741 | −0.045 |
| MJS_tm | 0.027 | 0.242 | 0.706 | −0.173 |
| LRI_cm | 0.013 | 0.108 | −0.671 | −0.330 |
| AJS_tm | 0.270 | −0.326 | 0.066 | 0.702 |
| SJS_tm | 0.190 | 0.152 | −0.278 | 0.700 |
| RH_cm | −0.083 | 0.119 | 0.011 | 0.587 |
| BL_cm | −0.158 | 0.236 | 0.216 | −0.551 |
| MES_tm | −0.198 | −0.096 | 0.295 | 0.536 |
| MxH_cm | −0.137 | 0.290 | 0.120 | 0.360 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, W.-J.; Park, K.-H.; Kang, Y.-G.; Kim, S.-J. Automated Real-Time Evaluation of Condylar Movement in Relation to Three-Dimensional Craniofacial and Temporomandibular Morphometry in Patients with Facial Asymmetry. Sensors 2021, 21, 2591. https://doi.org/10.3390/s21082591
Lee W-J, Park K-H, Kang Y-G, Kim S-J. Automated Real-Time Evaluation of Condylar Movement in Relation to Three-Dimensional Craniofacial and Temporomandibular Morphometry in Patients with Facial Asymmetry. Sensors. 2021; 21(8):2591. https://doi.org/10.3390/s21082591
Chicago/Turabian StyleLee, Won-June, Ki-Ho Park, Yoon-Goo Kang, and Su-Jung Kim. 2021. "Automated Real-Time Evaluation of Condylar Movement in Relation to Three-Dimensional Craniofacial and Temporomandibular Morphometry in Patients with Facial Asymmetry" Sensors 21, no. 8: 2591. https://doi.org/10.3390/s21082591
APA StyleLee, W.-J., Park, K.-H., Kang, Y.-G., & Kim, S.-J. (2021). Automated Real-Time Evaluation of Condylar Movement in Relation to Three-Dimensional Craniofacial and Temporomandibular Morphometry in Patients with Facial Asymmetry. Sensors, 21(8), 2591. https://doi.org/10.3390/s21082591






