Rehabilitation and Return to Sport Assessment after Anterior Cruciate Ligament Injury: Quantifying Joint Kinematics during Complex High-Speed Tasks through Wearable Sensors
Abstract
1. Introduction
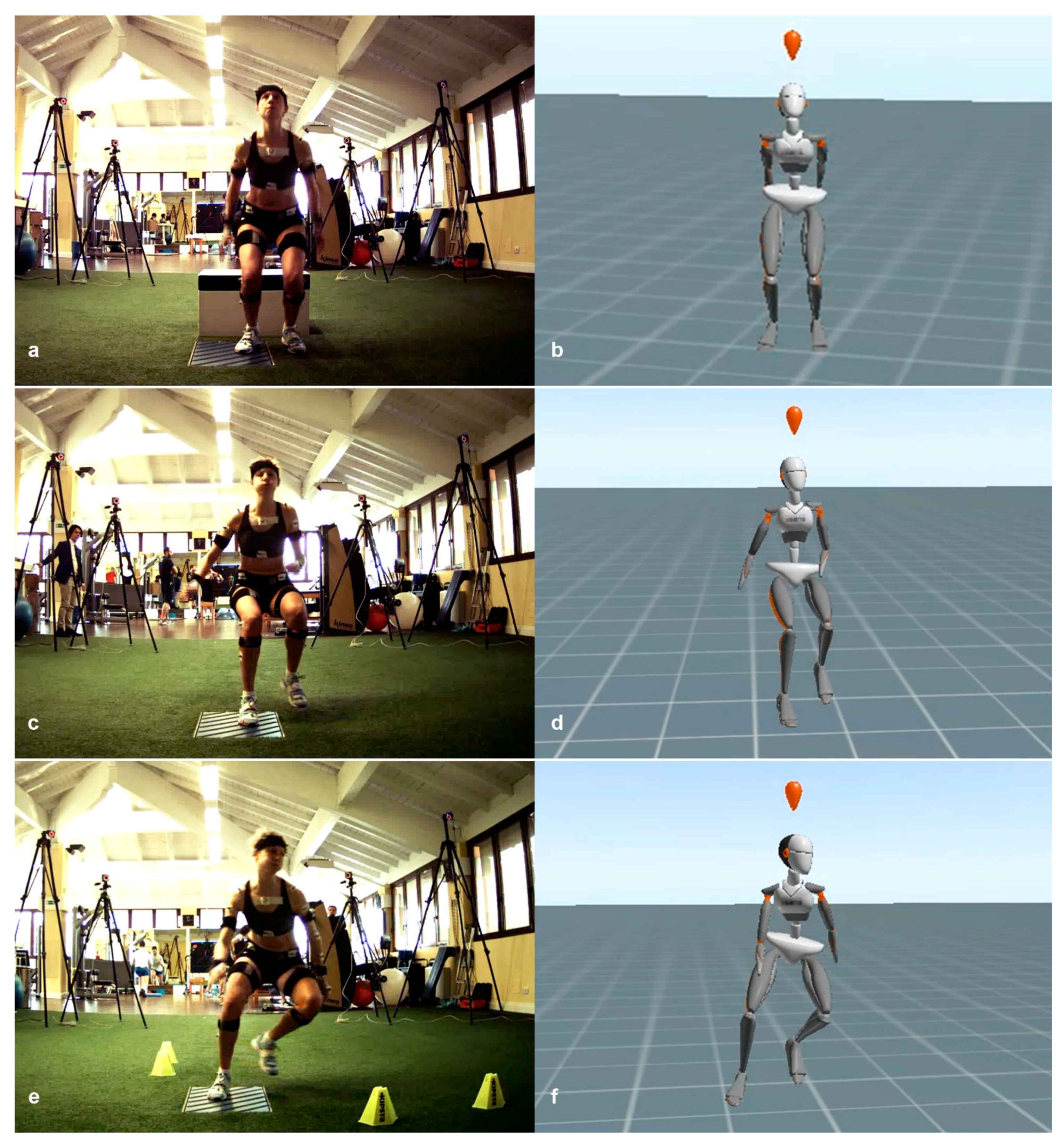
2. Materials and Methods
2.1. Experimental Protocol
2.2. Features Selection and Data Processing
2.3. Statistical Analysis
3. Results
3.1. Drop Jump
3.2. Frontal Sprint
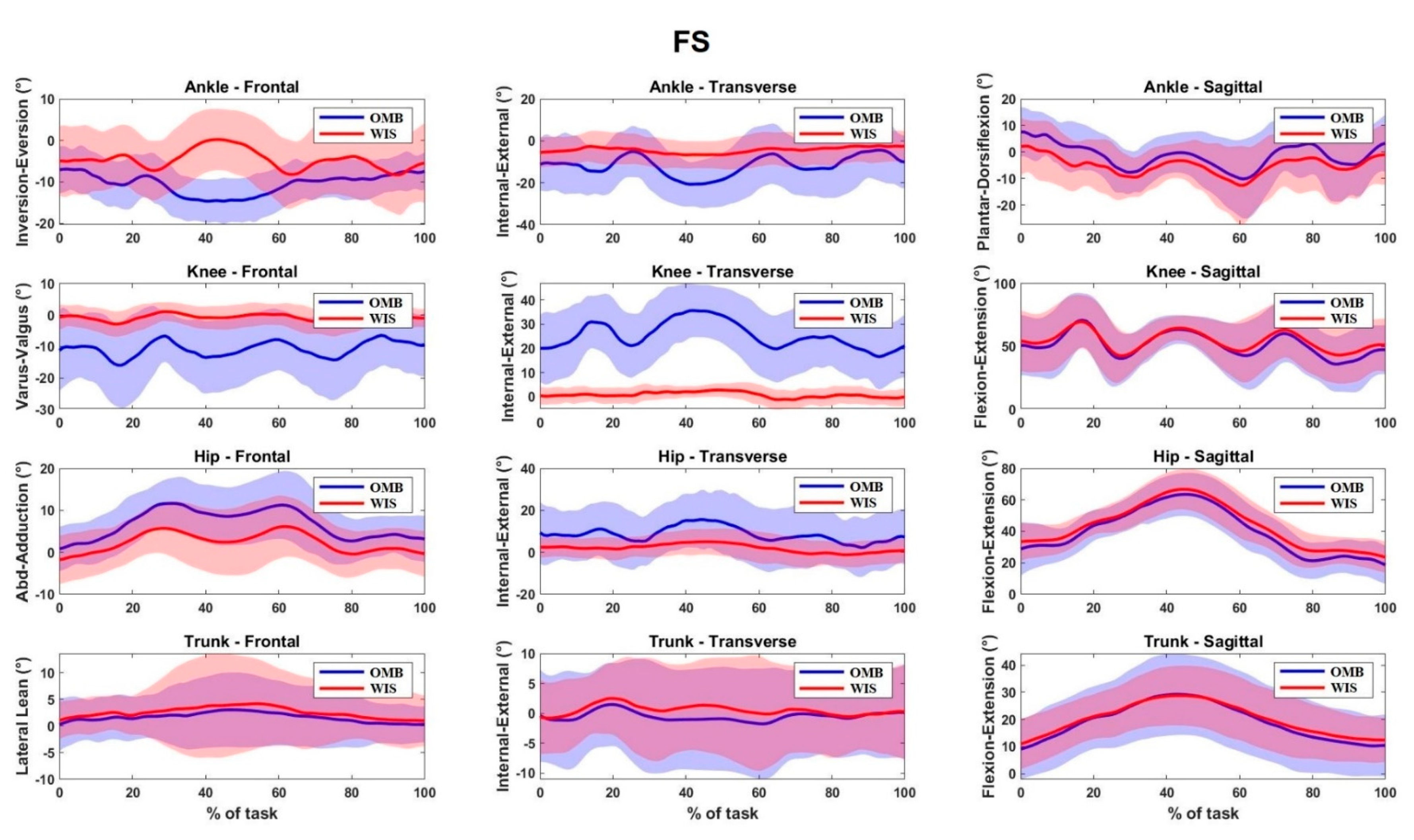
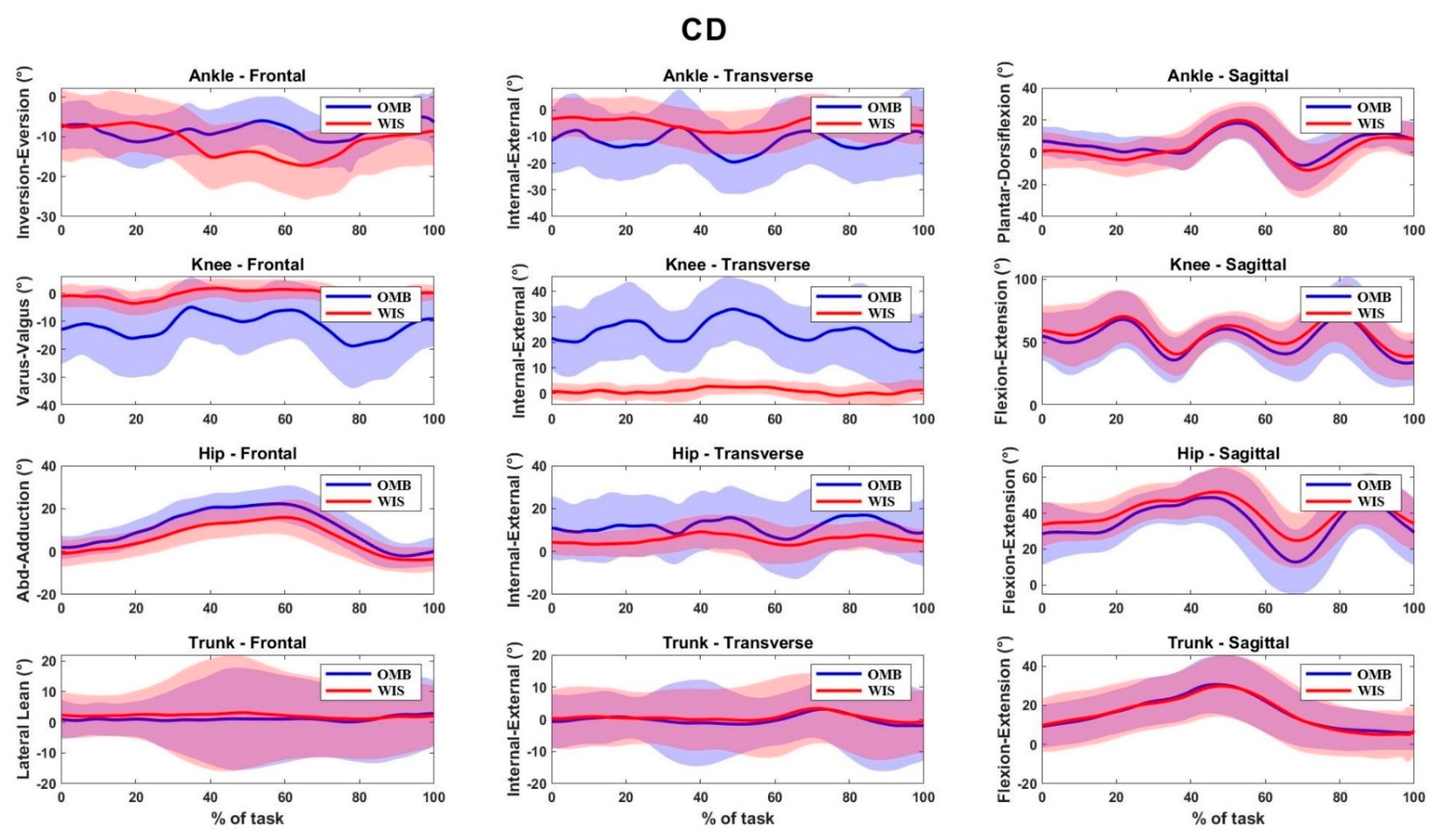
3.3. 90° Change of Direction
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A

Appendix B

References
- Della Villa, F.; Buckthorpe, M.; Grassi, A.; Nabiuzzi, A.; Tosarelli, F.; Zaffagnini, S.; Della Villa, S. Systematic Video Analysis of ACL Injuries in Professional Male Football (Soccer): Injury Mechanisms, Situational Patterns and Biomechanics Study on 134 Consecutive Cases. Br. J. Sports Med. 2020, 54, 1423–1432. [Google Scholar] [CrossRef]
- Hewett, T.E.; Myer, G.D.; Ford, K.R.; Heidt, R.S.; Colosimo, A.J.; McLean, S.G.; van den Bogert, A.J.; Paterno, M.V.; Succop, P. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. Am. J. Sports Med. 2005, 33, 492–501. [Google Scholar] [CrossRef]
- Alentorn-Geli, E.; Myer, G.D.; Silvers, H.J.; Samitier, G.; Romero, D.; Lázaro-Haro, C.; Cugat, R. Prevention of Non-Contact Anterior Cruciate Ligament Injuries in Soccer Players. Part 1: Mechanisms of Injury and Underlying Risk Factors. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 705–729. [Google Scholar] [CrossRef]
- Leppänen, M.; Pasanen, K.; Krosshaug, T.; Kannus, P.; Vasankari, T.; Kujala, U.M.; Bahr, R.; Perttunen, J.; Parkkari, J. Sagittal Plane Hip, Knee, and Ankle Biomechanics and the Risk of Anterior Cruciate Ligament Injury: A Prospective Study. Orthop. J. Sports Med. 2017, 5, 2325967117745487. [Google Scholar] [CrossRef]
- Leppänen, M.; Pasanen, K.; Kujala, U.M.; Vasankari, T.; Kannus, P.; Äyrämö, S.; Krosshaug, T.; Bahr, R.; Avela, J.; Perttunen, J.; et al. Stiff Landings Are Associated with Increased ACL Injury Risk in Young Female Basketball and Floorball Players. Am. J. Sports Med. 2017, 45, 386–393. [Google Scholar] [CrossRef]
- Webster, K.E.; Feller, J.A. Exploring the High Reinjury Rate in Younger Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2016, 44, 2827–2832. [Google Scholar] [CrossRef]
- Wiggins, A.J.; Grandhi, R.K.; Schneider, D.K.; Stanfield, D.; Webster, K.E.; Myer, G.D. Risk of Secondary Injury in Younger Athletes After Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Am. J. Sports Med. 2016, 44, 1861–1876. [Google Scholar] [CrossRef]
- Poulsen, E.; Goncalves, G.H.; Bricca, A.; Roos, E.M.; Thorlund, J.B.; Juhl, C.B. Knee Osteoarthritis Risk Is Increased 4-6 Fold after Knee Injury—A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2019, 53, 1454–1463. [Google Scholar] [CrossRef] [PubMed]
- Benjaminse, A.; Holden, S.; Myer, G.D. ACL Rupture Is a Single Leg Injury but a Double Leg Problem: Too Much Focus on “symmetry” Alone and That’s Not Enough! Br. J. Sports Med. 2018, 52, 1029–1030. [Google Scholar] [CrossRef]
- Bencke, J.; Aagaard, P.; Zebis, M.K. Muscle Activation During ACL Injury Risk Movements in Young Female Athletes: A Narrative Review. Front. Physiol. 2018, 9, 445. [Google Scholar] [CrossRef] [PubMed]
- Alentorn-Geli, E.; Myer, G.D.; Silvers, H.J.; Samitier, G.; Romero, D.; Lázaro-Haro, C.; Cugat, R. Prevention of Non-Contact Anterior Cruciate Ligament Injuries in Soccer Players. Part 2: A Review of Prevention Programs Aimed to Modify Risk Factors and to Reduce Injury Rates. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 859–879. [Google Scholar] [CrossRef]
- Hewett, T.E.; Ford, K.R.; Xu, Y.Y.; Khoury, J.; Myer, G.D. Effectiveness of Neuromuscular Training Based on the Neuromuscular Risk Profile. Am. J. Sports Med. 2017, 45, 2142–2147. [Google Scholar] [CrossRef] [PubMed]
- Mandelbaum, B.R.; Silvers, H.J.; Watanabe, D.S.; Knarr, J.F.; Thomas, S.D.; Griffin, L.Y.; Kirkendall, D.T.; Garrett, W. Effectiveness of a Neuromuscular and Proprioceptive Training Program in Preventing Anterior Cruciate Ligament Injuries in Female Athletes: 2-Year Follow-Up. Am. J. Sports Med. 2005, 33, 1003–1010. [Google Scholar] [CrossRef]
- Hewett, T.E.; Bates, N.A. Preventive Biomechanics: A Paradigm Shift with a Translational Approach to Injury Prevention. Am. J. Sports Med. 2017, 45, 2654–2664. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Della Villa, F. Optimising the “Mid-Stage” Training and Testing Process After ACL Reconstruction. Sports Med. 2020, 50, 657–678. [Google Scholar] [CrossRef]
- King, E.; Richter, C.; Daniels, K.A.J.; Franklyn-Miller, A.; Falvey, E.; Myer, G.D.; Jackson, M.; Moran, R.; Strike, S. Biomechanical but Not Strength or Performance Measures Differentiate Male Athletes Who Experience ACL Reinjury on Return to Level 1 Sports. Am. J. Sports Med. 2021, 49, 918–927. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, K.; Miller, E.; Kingsbury, T.; Russell Esposito, E.; Wolf, E.; Wilken, J.; Wyatt, M. Reliability of 3D Gait Data across Multiple Laboratories. Gait Posture 2016, 49, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Poitras, I.; Dupuis, F.; Bielmann, M.; Campeau-Lecours, A.; Mercier, C.; Bouyer, L.; Roy, J.-S. Validity and Reliability of Wearable Sensors for Joint Angle Estimation: A Systematic Review. Sensors 2019, 19, 1555. [Google Scholar] [CrossRef]
- Van der Kruk, E.; Reijne, M.M. Accuracy of Human Motion Capture Systems for Sport Applications; State-of-the-Art Review. Eur. J. Sport Sci. 2018, 18, 806–819. [Google Scholar] [CrossRef]
- Camomilla, V.; Bergamini, E.; Fantozzi, S.; Vannozzi, G. Trends Supporting the In-Field Use of Wearable Inertial Sensors for Sport Performance Evaluation: A Systematic Review. Sensors 2018, 18, 873. [Google Scholar] [CrossRef]
- Godwin, A.; Agnew, M.; Stevenson, J. Accuracy of Inertial Motion Sensors in Static, Quasistatic, and Complex Dynamic Motion. J. Biomech. Eng. 2009, 131, 114501. [Google Scholar] [CrossRef]
- Al-Amri, M.; Nicholas, K.; Button, K.; Sparkes, V.; Sheeran, L.; Davies, J. Inertial Measurement Units for Clinical Movement Analysis: Reliability and Concurrent Validity. Sensors 2018, 18, 719. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.A.; Herrington, L.C.; Graham-Smith, P. Technique Determinants of Knee Abduction Moments during Pivoting in Female Soccer Players. Clin. Biomech. 2016, 31, 107–112. [Google Scholar] [CrossRef]
- Dempsey, A.R.; Lloyd, D.G.; Elliott, B.C.; Steele, J.R.; Munro, B.J. Changing Sidestep Cutting Technique Reduces Knee Valgus Loading. Am. J. Sports Med. 2009, 37, 2194–2200. [Google Scholar] [CrossRef]
- Ferrari, A.; Cutti, A.G.; Cappello, A. A New Formulation of the Coefficient of Multiple Correlation to Assess the Similarity of Waveforms Measured Synchronously by Different Motion Analysis Protocols. Gait Posture 2010, 31, 540–542. [Google Scholar] [CrossRef]
- Ferrari, A.; Benedetti, M.G.; Pavan, E.; Frigo, C.; Bettinelli, D.; Rabuffetti, M.; Crenna, P.; Leardini, A. Quantitative Comparison of Five Current Protocols in Gait Analysis. Gait Posture 2008, 28, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Kadaba, M.P.; Ramakrishnan, H.K.; Wootten, M.E.; Gainey, J.; Gorton, G.; Cochran, G.V. Repeatability of Kinematic, Kinetic, and Electromyographic Data in Normal Adult Gait. J. Orthop. Res. 1989, 7, 849–860. [Google Scholar] [CrossRef]
- Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Plamondon, A. Validation of Inertial Measurement Units with an Optoelectronic System for Whole-Body Motion Analysis. Med. Biol. Eng. Comput. 2017, 55, 609–619. [Google Scholar] [CrossRef]
- Zhang, J.-T.; Novak, A.C.; Brouwer, B.; Li, Q. Concurrent Validation of Xsens MVN Measurement of Lower Limb Joint Angular Kinematics. Physiol. Meas. 2013, 34, N63–N69. [Google Scholar] [CrossRef]
- Richter, C.; Daniels, K.A.J.; King, E.; Franklyn-Miller, A. Agreement between Inertia and Optical Based Motion Capture during the VU-Return-to-Play- Field-Test. Sensors 2020, 20, 831. [Google Scholar] [CrossRef]
- Cannon, J.; Cambridge, E.D.J.; McGill, S.M. Anterior Cruciate Ligament Injury Mechanisms and the Kinetic Chain Linkage: The Effect of Proximal Joint Stiffness on Distal Knee Control during Bilateral Landings. J. Orthop. Sports Phys. Ther. 2019, 49, 601–610. [Google Scholar] [CrossRef]
- Sabet, S.; Letafatkar, A.; Eftekhari, F.; Khosrokiani, Z.; Gokeler, A. Trunk and Hip Control Neuromuscular Training to Target Inter Limb Asymmetry Deficits Associated with Anterior Cruciate Ligament Injury. Phys. Ther. Sport 2019, 38, 71–79. [Google Scholar] [CrossRef]
- King, E.; Richter, C.; Daniels, K.A.J.; Franklyn-Miller, A.; Falvey, E.; Myer, G.D.; Jackson, M.; Moran, R.; Strike, S. Can Biomechanical Testing After Anterior Cruciate Ligament Reconstruction Identify Athletes at Risk for Subsequent ACL Injury to the Contralateral Uninjured Limb? Am. J. Sports Med. 2021, 49, 609–619. [Google Scholar] [CrossRef]
- van der Straaten, R.; Bruijnes, A.K.B.D.; Vanwanseele, B.; Jonkers, I.; De Baets, L.; Timmermans, A. Reliability and Agreement of 3D Trunk and Lower Extremity Movement Analysis by Means of Inertial Sensor Technology for Unipodal and Bipodal Tasks. Sensors 2019, 19, 141. [Google Scholar] [CrossRef]
- Pollard, C.D.; Sigward, S.M.; Powers, C.M. Limited Hip and Knee Flexion during Landing Is Associated with Increased Frontal Plane Knee Motion and Moments. Clin. Biomech. 2010, 25, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Kotsifaki, A.; Korakakis, V.; Whiteley, R.; Van Rossom, S.; Jonkers, I. Measuring Only Hop Distance during Single Leg Hop Testing Is Insufficient to Detect Deficits in Knee Function after ACL Reconstruction: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2020, 54, 139–153. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, A.-D.; Taylor, J.B.; Wimbish, T.G.; Keith, J.L.; Ford, K.R. Preferred Hip Strategy During Landing Reduces Knee Abduction Moment in Collegiate Female Soccer Players. J. Sport Rehabil. 2018, 27, 213–217. [Google Scholar] [CrossRef]
- Teufl, W.; Miezal, M.; Taetz, B.; Fröhlich, M.; Bleser, G. Validity of Inertial Sensor Based 3D Joint Kinematics of Static and Dynamic Sport and Physiotherapy Specific Movements. PLoS ONE 2019, 14, e0213064. [Google Scholar] [CrossRef]
- Bates, N.A.; Myer, G.D.; Hale, R.F.; Schilaty, N.D.; Hewett, T.E. Prospective Frontal Plane Angles Used to Predict ACL Strain and Identify Those at High Risk for Sports-Related ACL Injury. Orthop. J. Sports Med. 2020, 8, 2325967120957646. [Google Scholar] [CrossRef]
- Räisänen, A.M.; Pasanen, K.; Krosshaug, T.; Vasankari, T.; Kannus, P.; Heinonen, A.; Kujala, U.M.; Avela, J.; Perttunen, J.; Parkkari, J. Association between Frontal Plane Knee Control and Lower Extremity Injuries: A Prospective Study on Young Team Sport Athletes. BMJ Open Sport Exerc. Med. 2018, 4, e000311. [Google Scholar] [CrossRef]
- Jamison, S.T.; Pan, X.; Chaudhari, A.M.W. Knee Moments during Run-to-Cut Maneuvers Are Associated with Lateral Trunk Positioning. J. Biomech. 2012, 45, 1881–1885. [Google Scholar] [CrossRef]
- Markström, J.L.; Tengman, E.; Häger, C.K. ACL-Reconstructed and ACL-Deficient Individuals Show Differentiated Trunk, Hip, and Knee Kinematics during Vertical Hops More than 20 Years Post-Injury. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 358–367. [Google Scholar] [CrossRef]
- Della Villa, F.; Ricci, M.; Perdisa, F.; Filardo, G.; Gamberini, J.; Caminati, D.; Della Villa, S. Anterior Cruciate Ligament Reconstruction and Rehabilitation: Predictors of Functional Outcome. Joints 2015, 3, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Hewett, T.E.; Torg, J.S.; Boden, B.P. Video Analysis of Trunk and Knee Motion during Non-Contact Anterior Cruciate Ligament Injury in Female Athletes: Lateral Trunk and Knee Abduction Motion Are Combined Components of the Injury Mechanism. Br. J. Sports Med. 2009, 43, 417–422. [Google Scholar] [CrossRef]
- Piazza, S.J.; Cavanagh, P.R. Measurement of the Screw-Home Motion of the Knee Is Sensitive to Errors in Axis Alignment. J. Biomech. 2000, 33, 1029–1034. [Google Scholar] [CrossRef]
- Røislien, J.; Skare, O.; Opheim, A.; Rennie, L. Evaluating the Properties of the Coefficient of Multiple Correlation (CMC) for Kinematic Gait Data. J. Biomech. 2012, 45, 2014–2018. [Google Scholar] [CrossRef]
- Mavor, M.P.; Ross, G.B.; Clouthier, A.L.; Karakolis, T.; Graham, R.B. Validation of an IMU Suit for Military-Based Tasks. Sensors 2020, 20, 4280. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Della Villa, F.; Della Villa, S.; Roi, G.S. On-Field Rehabilitation Part 1: 4 Pillars of High-Quality On-Field Rehabilitation Are Restoring Movement Quality, Physical Conditioning, Restoring Sport-Specific Skills, and Progressively Developing Chronic Training Load. J. Orthop. Sports Phys. Ther. 2019, 49, 565–569. [Google Scholar] [CrossRef]
- Buckthorpe, M.; Della Villa, F.; Della Villa, S.; Roi, G.S. On-Field Rehabilitation Part 2: A 5-Stage Program for the Soccer Player Focused on Linear Movements, Multidirectional Movements, Soccer-Specific Skills, Soccer-Specific Movements, and Modified Practice. J. Orthop. Sports Phys. Ther. 2019, 49, 570–575. [Google Scholar] [CrossRef] [PubMed]
- Verheul, J.; Nedergaard, N.J.; Vanrenterghem, J.; Robinson, M.A. Measuring Biomechanical Loads in Team Sports—From Lab to Field; SportRxiv; Taylor & Francis: Oxfordshire, UK, 2019. [Google Scholar]
- Pratt, K.A.; Sigward, S.M. Detection of Knee Power Deficits Following Anterior Cruciate Ligament Reconstruction Using Wearable Sensors. J. Orthop. Sports Phys. Ther. 2018, 48, 895–902. [Google Scholar] [CrossRef]
- Preatoni, E.; Nodari, S.; Lopomo, N.F. Supervised Machine Learning Applied to Wearable Sensor Data Can Accurately Classify Functional Fitness Exercises Within a Continuous Workout. Front. Bioeng. Biotechnol. 2020, 8, 664. [Google Scholar] [CrossRef] [PubMed]

| Number of athletes | 34 |
| Age (years) | 22.8 ± 4.1 [18,19,20,21,22,23,24,25,26,27,28,29,30,31] |
| Gender (m/f) | 18/16 |
| Body Mass Index | 22.6 ± 2.6 [18,19,20,21,22,23,24,25,26,27] |
| Dominant limb (r/l) 1 | 30/4 |
| Tegner | 8.6 ± 1.0 [5,6,7,8,9] |
| r | CMC | |||||
|---|---|---|---|---|---|---|
| DJ | FS | CD | DJ | FS | CD | |
| Ankle | ||||||
| Transverse | 0.58 [0.49, 0.67] | 0.53 [0.43, 0.62] | 0.45 [0.35, 0.55] | 0.63 [0.57, 0.69] | 0.63 [0.56, 0.69] | 0.62 [0.55, 0.69] |
| Knee | ||||||
| Frontal | 0.69 [0.59, 0.79] | 0.55 [0.43, 0.67] | 0.60 [0.50, 0.70] | 0.67 [0.58, 0.76] | 0.65 [0.57, 0.73] | 0.63 [0.55, 0.72] |
| Sagittal | 0.99 [0.98, 0.99] | 0.95 [0.94, 0.97] | 0.95 [0.93, 0.96] | 0.99 [0.99, 0.99] | 0.98 [0.97, 0.98] | 0.97 [0.96, 0.98] |
| Hip | ||||||
| Frontal | 0.81 [0.76, 0.86] | 0.85 [0.81, 0.89] | 0.96 [0.95, 0.97] | 0.88 [0.85, 0.91] | 0.91 [0.88, 0.93] | 0.96 [0.96, 0.97] |
| Transverse | 0.64 [0.55, 0.73] | 0.47 [0.34, 0.59] | 0.63 [0.56, 0.71] | 0.74 [0.68, 0.81] | 0.59 [0.48, 0.70] | 0.72 [0.67, 0.77] |
| Sagittal | 0.99 [0.98, 0.99] | 0.97 [0.97, 0.98] | 0.96 [0.94, 0.97] | 0.99 [0.99, 0.99] | 0.98 [0.98, 0.99] | 0.97 [0.96, 0.97] |
| Trunk | ||||||
| Frontal | 0.77 [0.72, 0.82] | 0.67 [0.55, 0.79] | 0.87 [0.84, 0.90] | 0.85 [0.82, 0.89] | 0.81 [0.75, 0.88] | 0.91 [0.89, 0.94] |
| Transverse | 0.74 [0.67, 0.81] | 0.84 [0.79, 0.89] | 0.81 [0.76, 0.86] | 0.83 [0.78, 0.88] | 0.90 [0.87, 0.93] | 0.89 [0.87, 0.92] |
| ΔOFF (°) | NRMSE (%) | |||||
|---|---|---|---|---|---|---|
| DJ | FS | CD | DJ | FS | CD | |
| Ankle | ||||||
| Transverse | 3.31 [0.38, 6.24] | −8.51 [−11.39, −5.64] | −7.91 [−11.16, −4.66] | 0.26 [0.23, 0.28] | 0.31 [0.27, 0.35] | 0.37 [0.32, 0.42] |
| Knee | ||||||
| Frontal | −4.14 [−5.90, −2.37] | −9.93 [−13.63, −6.22] | −10.93 [−14.67, −7.19] | 0.27 [0.22, 0.32] | 0.43 [0.35, 0.51] | 0.40 [0.33, 0.47] |
| Sagittal | −4.67 [−6.63, −2.71] | −2.45 [−5.24, 0.35] | −3.86 [−6.28, −1.43] | 0.08 [0.06, 0.09] | 0.12 [0.09, 0.14] | 0.12 [0.10, 0.14] |
| Hip | ||||||
| Frontal | 3.91 [2.55, 5.27] | 4.82 [3.19, 6.45] | 5.18 [3.38, 6.99] | 0.36 [0.28, 0.44] | 0.29 [0.23, 0.35] | 0.21 [0.17, 0.25] |
| Transverse | −1.05 [−4.69, 2.6] | 6.57 [1.83, 11.31] | 5.49 [1.21, 9.76] | 0.26 [0.22, 0.29] | 0.38 [0.31, 0.45] | 0.30 [0.25, 0.35] |
| Sagittal | −6.91 [−9.13, −4.68] | −2.94 [−5.62, −0.27] | −4.99 [−7.54, −2.44] | 0.10 [0.09, 0.12] | 0.13 [0.10, 0.16] | 0.14 [0.12, 0.17] |
| Trunk | ||||||
| Frontal | −0.33 [−1.30, 0.64] | −0.69 [−2.0, 0.61] | −1.05 [−2.40, 0.31] | 0.30 [0.25, 0.35] | 0.31 [0.25, 0.37] | 0.20 [0.17, 0.23] |
| Transverse | 0.38 [−1.06, 1.83] | −0.85 [−2.66, 0.97] | −1.14 [−3.26, 0.98] | 0.37 [0.30, 0.45] | 0.21 [0.17, 0.25] | 0.26 [0.21, 0.30] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Paolo, S.; Lopomo, N.F.; Della Villa, F.; Paolini, G.; Figari, G.; Bragonzoni, L.; Grassi, A.; Zaffagnini, S. Rehabilitation and Return to Sport Assessment after Anterior Cruciate Ligament Injury: Quantifying Joint Kinematics during Complex High-Speed Tasks through Wearable Sensors. Sensors 2021, 21, 2331. https://doi.org/10.3390/s21072331
Di Paolo S, Lopomo NF, Della Villa F, Paolini G, Figari G, Bragonzoni L, Grassi A, Zaffagnini S. Rehabilitation and Return to Sport Assessment after Anterior Cruciate Ligament Injury: Quantifying Joint Kinematics during Complex High-Speed Tasks through Wearable Sensors. Sensors. 2021; 21(7):2331. https://doi.org/10.3390/s21072331
Chicago/Turabian StyleDi Paolo, Stefano, Nicola Francesco Lopomo, Francesco Della Villa, Gabriele Paolini, Giulio Figari, Laura Bragonzoni, Alberto Grassi, and Stefano Zaffagnini. 2021. "Rehabilitation and Return to Sport Assessment after Anterior Cruciate Ligament Injury: Quantifying Joint Kinematics during Complex High-Speed Tasks through Wearable Sensors" Sensors 21, no. 7: 2331. https://doi.org/10.3390/s21072331
APA StyleDi Paolo, S., Lopomo, N. F., Della Villa, F., Paolini, G., Figari, G., Bragonzoni, L., Grassi, A., & Zaffagnini, S. (2021). Rehabilitation and Return to Sport Assessment after Anterior Cruciate Ligament Injury: Quantifying Joint Kinematics during Complex High-Speed Tasks through Wearable Sensors. Sensors, 21(7), 2331. https://doi.org/10.3390/s21072331







