Size- and Time-Dependent Particle Removal Efficiency of Face Masks and Improvised Respiratory Protection Equipment Used during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
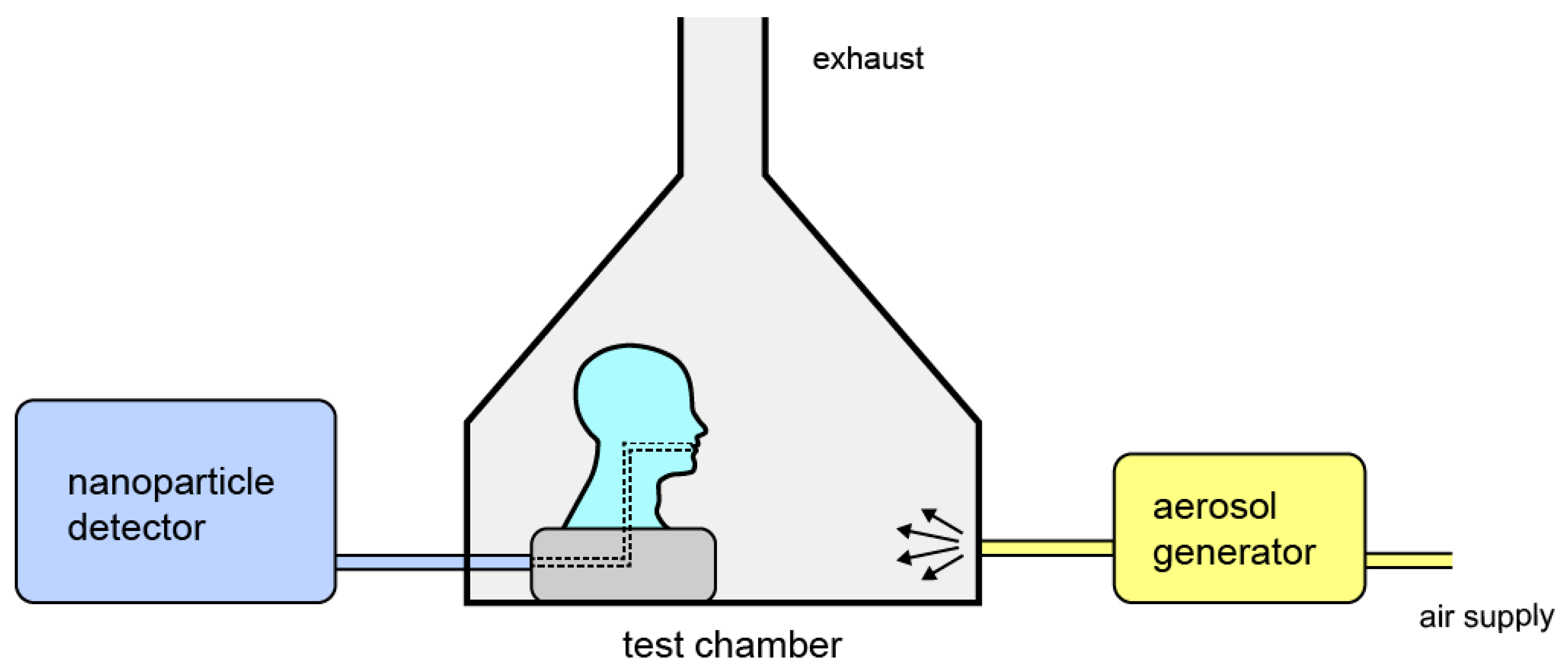
2.1. Particle Removal Efficiency Testing
2.2. Selection of Masks
2.3. Scanning Electron Microscopy
3. Results and Discussion
3.1. Size-Dependent PRE Measurements
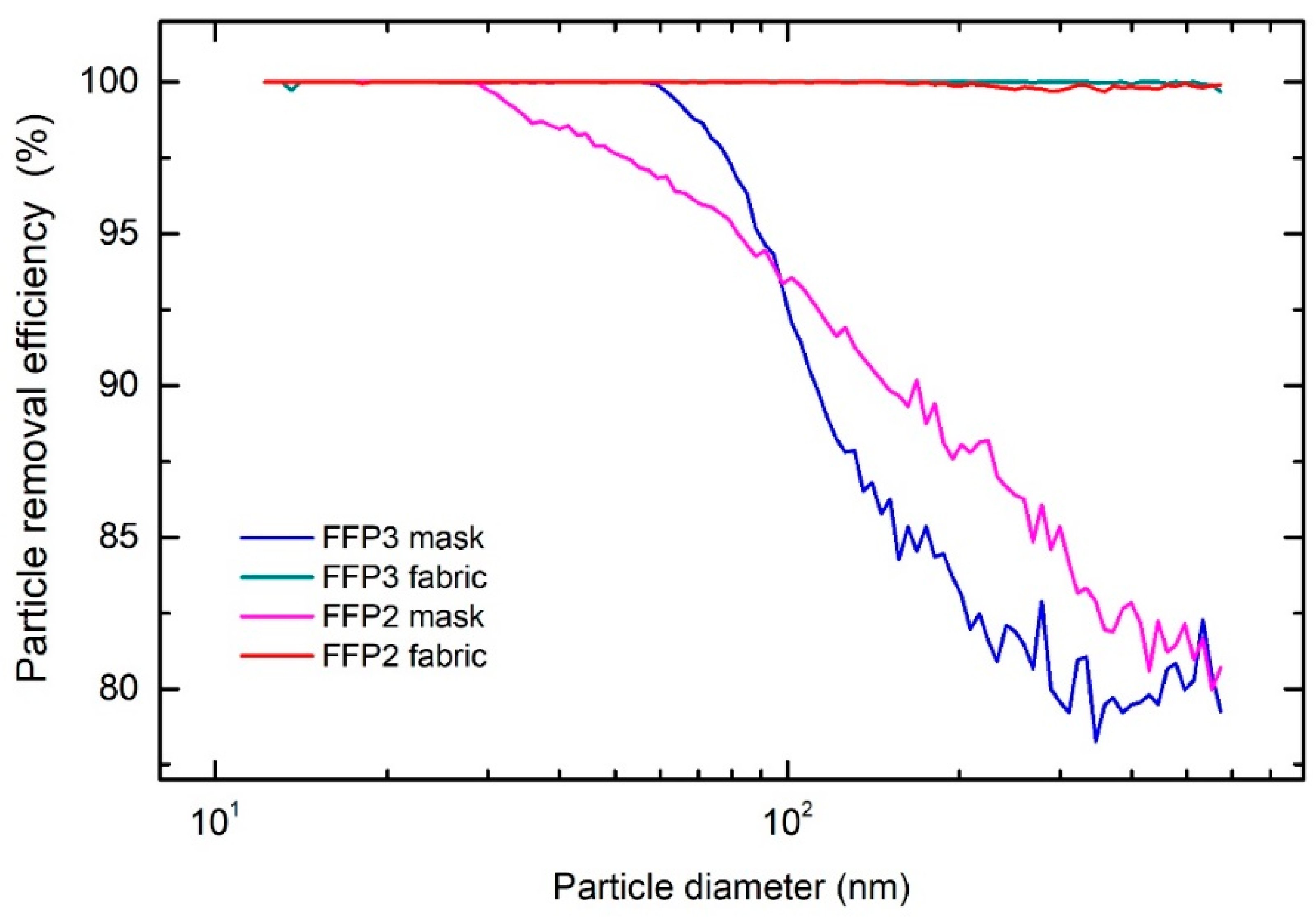
3.1.1. FFP2 and FFP3 Masks
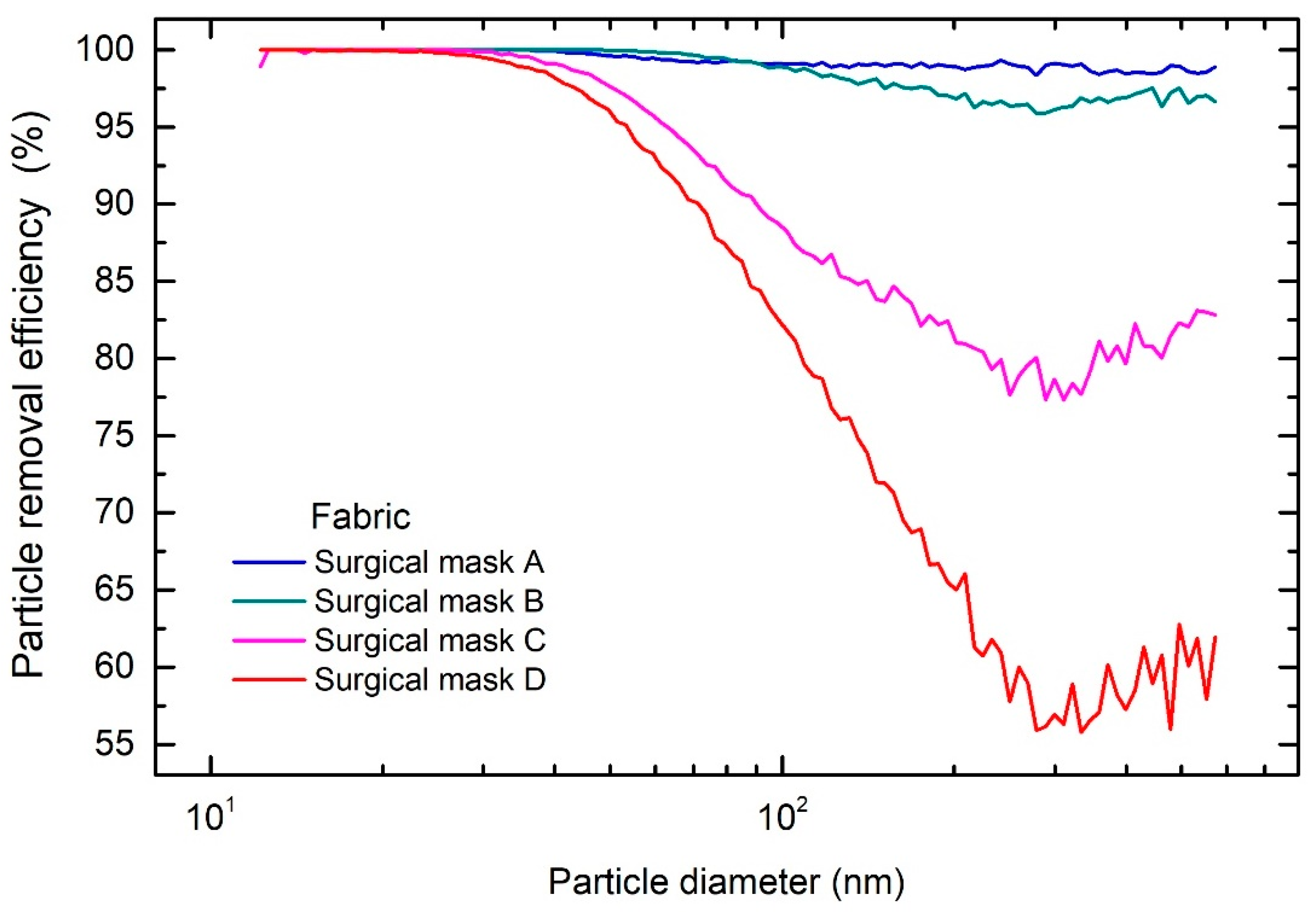
3.1.2. Surgical Masks
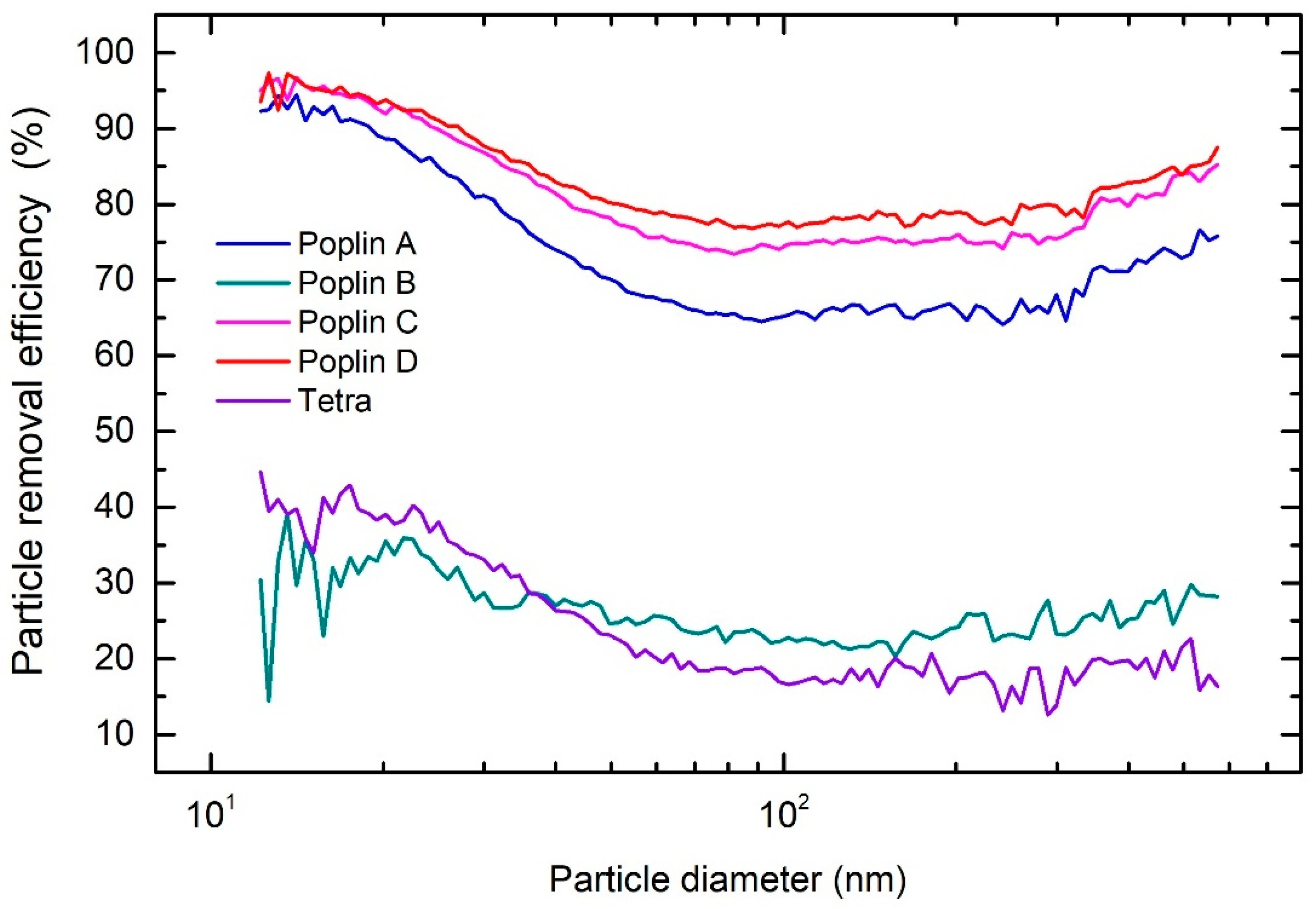
3.1.3. Cloth Masks and Fabrics
3.1.4. Improvised Respiratory Masks
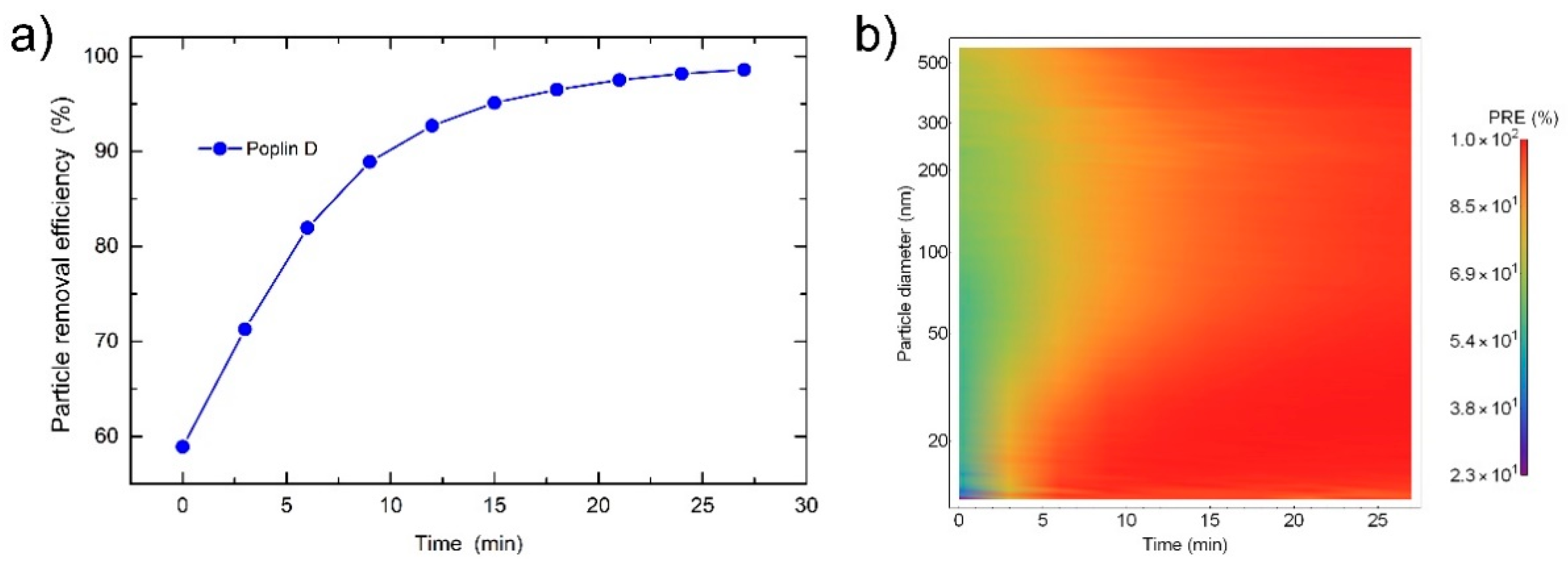
3.2. Time-Dependent Measurements
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ranney, M.L.; Griffeth, V.; Jha, A.K. Critical supply shortages—the need for ventilators and personal protective equipment during the Covid-19 pandemic. N. Engl. J. Med. 2020, 382, e41. [Google Scholar] [CrossRef] [PubMed]
- O’Dowd, K.; Nair, K.M.; Forouzandeh, P.; Mathew, S.; Grant, J.; Moran, R.; Bartlett, J.; Bird, J.; Pillai, S.C. Face masks and respirators in the fight against the COVID-19 pandemic: A review of current materials, advances and future perspectives. Materials 2020, 13, 3363. [Google Scholar] [CrossRef] [PubMed]
- Anfinrud, P.; Stadnytskyi, V.; Bax, C.E.; Bax, A. Visualizing speech-generated oral fluid droplets with laser light scattering. N. Engl. J. Med. 2020, 382, 2061–2063. [Google Scholar] [CrossRef] [PubMed]
- La Rosa, G.; Bonadonna, L.; Lucentini, L.; Kenmoe, S.; Suffredini, E. Coronavirus in water environments: Occurrence, persistence and concentration methods-A scoping review. Water Res. 2020, 179, 115899. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Pearce, T.A.; Hudnall, J.B.; Davis, K.A.; Davis, S.M.; Fisher, M.A.; Khakoo, R.; Palmer, J.E.; Clark, K.E.; Celik, I. Quantity and size distribution of cough-generated aerosol particles produced by influenza patients during and after illness. J. Occup. Environ. Hyg. 2012, 9, 443–449. [Google Scholar] [CrossRef]
- Stadnytskyi, V.; Bax, C.E.; Bax, A.; Anfinrud, P. The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission. Proc. Natl. Acad. Sci. USA 2020, 117, 11875–11877. [Google Scholar] [CrossRef] [PubMed]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J.; El-harakeh, A.; Bognanni, A.; Lotfi, T.; Loeb, M. Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: A systematic review and meta-analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Reza, M.S.; Hasan, A.B.M.K.; Afroze, S.; Bakar, M.S.A.; Taweekun, J.; Azad, A.K. Analysis on preparation, application, and recycling of activated carbon to aid in COVID-19 protection. Int. J. Integr. Eng. 2020, 12, 233–244. [Google Scholar] [CrossRef]
- EN 14683:2019+AC:2019: Medical Face Masks—Requirements and Test Methods. Available online: https://www.en-standard.eu/une-en-14683-2019-ac-2019-medical-face-masks-requirements-and-test-methods/ (accessed on 12 February 2021).
- EN 149:2001+A1:2009: Respiratory Protective Devices. Filtering Half Masks to Protect against Particles. Requirements, Testing, Marking. Available online: https://www.en-standard.eu/bs-en-149-2001-a1-2009-respiratory-protective-devices.-filtering-half-masks-to-protect-against-particles.-requirements-testing-marking/ (accessed on 12 February 2021).
- EN 143:2001/A1:2006: Respiratory Protective Devices—Particle Filters—Requirements, Testing, Marking. Available online: https://www.en-standard.eu/une-en-143-2001/a1-2006-respiratory-protective-devices-particle-filters-requirements-testing-marking/ (accessed on 12 February 2021).
- EN 13274-7: Respiratory Protective Devices—Methods of Test—Part 7: Determination of Particle Filter Penetration. Available online: https://www.en-standard.eu/din-en-13274-7-respiratory-protective-devices-methods-of-test-part-7-determination-of-particle-filter-penetration/ (accessed on 13 February 2021).
- Forouzandeh, P.; O’Dowd, K.; Pillai, S.C. Face masks and respirators in the fight against the COVID-19 pandemic: An overview of the standards and testing methods. Saf. Sci. 2020, 133, 104995. [Google Scholar] [CrossRef]
- CDC. How to Select, Wear, and Clean Your Mask. Available online: https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html (accessed on 13 February 2021).
- Asadi, S.; Cappa, C.D.; Barreda, S.; Wexler, A.S.; Bouvier, N.M.; Ristenpart, W.D. Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Sci. Rep. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Lustig, S.; Biswakarma, J.J.H.; Rana, D.; Tilford, S.H.; Hu, W.; Su, M.; Rosenblatt, M.S. Effectiveness of Common Fabrics to Block Aqueous Aerosols of Virus-like Nanoparticles. ACS Nano 2020, 14, 7651–7658. [Google Scholar] [CrossRef] [PubMed]
- Mueller, A.V.; Eden, M.J.; Oakes, J.M.; Bellini, C.; Fernandez, L.A. Quantitative method for comparative assessment of particle removal efficiency of fabric masks as alternatives to standard surgical masks for ppe. Matter 2020, 3, 950–962. [Google Scholar] [CrossRef]
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet 2020, 395, 507–513. [Google Scholar] [CrossRef]
- Zhao, M.; Liao, L.; Xiao, W.; Yu, X.; Wang, H.; Wang, Q.; Lin, Y.L.; Kilinc-Balci, F.S.; Price, A.; Chu, L. Household materials selection for homemade cloth face coverings and their filtration efficiency enhancement with triboelectric charging. Nano Lett. 2020, 20, 5544–5552. [Google Scholar] [CrossRef]
- Kim, H.P.; Jo, M.S.; Kim, C.H.; Choi, J.S.; Yu, I.J. Re-use of health masks after autoclaving. NanoImpact 2020, 19, 100231. [Google Scholar] [CrossRef]
- Oberg, T.; Brosseau, L.M. Surgical mask filter and fit performance. Am. J. Infect. Control 2008, 36, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Pirker, L.; Krajnc, A.P.; Malec, J.; Radulović, V.; Gradišek, A.; Jelen, A.; Remškar, M.; Mekjavić, I.B.; Kovač, J.; Mozetič, M.; et al. Sterilization of polypropylene membranes of facepiece respirators by ionizing radiation. J. Memb. Sci. 2021, 619, 118756. [Google Scholar] [CrossRef]
- BS ISO 12103-1:1997 Road Vehicles. Test Dust for Filter Evaluation. Arizona Test Dust (British Standard). Available online: https://webstore.ansi.org/Standards/BSI/BSISO121031997 (accessed on 13 February 2021).
- Molter, L.; Schutz, S. Accurate particle counting of vacuum cleaner emissions. Filtr. Sep. 2003, 40, 28–31. [Google Scholar]
- IEC 62885-2:2016 Surface Cleaning Appliances—Part 2: Dry Vacuum Cleaners for Household or Similar Use—Methods for Measuring the Performance. Available online: https://webstore.iec.ch/publication/25719 (accessed on 13 February 2021).
- PD ISO/TS 16976-2:2015: Respiratory Protective Devices. Human Factors Anthropometrics. Available online: https://www.en-standard.eu/pd-iso/ts-16976-2-2015-respiratory-protective-devices.-human-factors-anthropometrics/ (accessed on 13 February 2021).
- Hinds, W.C. Aerosol Technology: Properties, Behavior, and Measurement of Airborne Particles; John Wiley & Sons: Hoboken, NJ, USA, 1999. [Google Scholar]
- Rengasamy, S.; Eimer, B.C.; Szalajda, J. A quantitative assessment of the total inward leakage of NaCl aerosol representing submicron-size bioaerosol through N95 filtering facepiece respirators and surgical masks. J. Occup. Environ. Hyg. 2014, 11, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Han, D.-H.; Lee, J. Evaluation of particulate filtering respirators using inward leakage (IL) or total inward leakage (TIL) testing—Korean experience. Ann. Occup. Hyg. 2005, 49, 569–574. [Google Scholar]
- Lei, Z.; Yang, J.; Zhuang, Z.; Roberge, R. Simulation and evaluation of respirator faceseal leaks using computational fluid dynamics and infrared imaging. Ann. Occup. Hyg. 2013, 57, 493–506. [Google Scholar] [PubMed]
- Javidpour, L.; Bozic, A.; Naji, A.; Podgornik, R. Electrostatic interaction between SARS-CoV-2 virus and charged electret fibre. arXiv 2020, arXiv:2012.07160. [Google Scholar]
- Crutchfield, C.D.; Fairbank, E.O.; Greenstein, S.L. Effect of test exercises and mask donning on measured respirator fit. Appl. Occup. Environ. Hyg. 1999, 14, 827–837. [Google Scholar] [CrossRef] [PubMed]
- Grinshpun, S.A.; Haruta, H.; Eninger, R.M.; Reponen, T.; McKay, R.T.; Lee, S.-A. Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: Two pathways for particle penetration. J. Occup. Environ. Hyg. 2009, 6, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Kim, J.K.; Lee, S.; Lee, J.; Kim, J.; Tsai, P.; Yoon, C. Comparison of filtration efficiency and pressure drop in anti-yellow sand masks, quarantine masks, medical masks, general masks, and handkerchiefs. Aerosol Air Qual. Res. 2013, 14, 991–1002. [Google Scholar] [CrossRef]
- Cheng, S.; Muhaiminul, A.S.M.; Yue, Z.; Wang, Y.; Xiao, Y.; Militky, J.; Prasad, M.; Zhu, G. Effect of temperature on the structure and filtration performance of polypropylene melt-blown nonwovens. Autex Res. J. 2020, 20, 366–371. [Google Scholar] [CrossRef]
- Frederick, E.R. Some effects of electrostatic charges in fabric filtration. J. Air Pollut. Control Assoc. 1974, 24, 1164–1168. [Google Scholar] [CrossRef]
- Kravtsov, A.G.; Zotov, S.V.; Brunig, H. Peculiarities of the electret state of melt-spun and melt-blown fibrous polypropylene materials. Mech. Compos. Mater. 2000, 36, 491–496. [Google Scholar] [CrossRef]
- Lee, S.-A.; Hwang, D.-C.; Li, H.-Y.; Tsai, C.-F.; Chen, C.-W.; Chen, J.-K. Particle size-selective assessment of protection of European standard FFP respirators and surgical masks against particles-tested with human subjects. J. Healthc. Eng. 2016, 2016, 8572493. [Google Scholar] [CrossRef]
- Scarano, A.; Inchingolo, F.; Lorusso, F. Facial skin temperature and discomfort when wearing protective face masks: Thermal infrared imaging evaluation and hands moving the mask. Int. J. Environ. Res. Public Health 2020, 17, 4624. [Google Scholar] [CrossRef]
- CDC Improve How Your Mask Protects You. Available online: https://www.cdc.gov/coronavirus/2019-ncov/your-health/effective-masks.html (accessed on 13 February 2021).






| Particle Removal Efficiency (%) | |||||
|---|---|---|---|---|---|
| Layer 1 (Inner layer) | Layer 2 | Layer 3 | Layer 4 (Outer layer) | All Layers | |
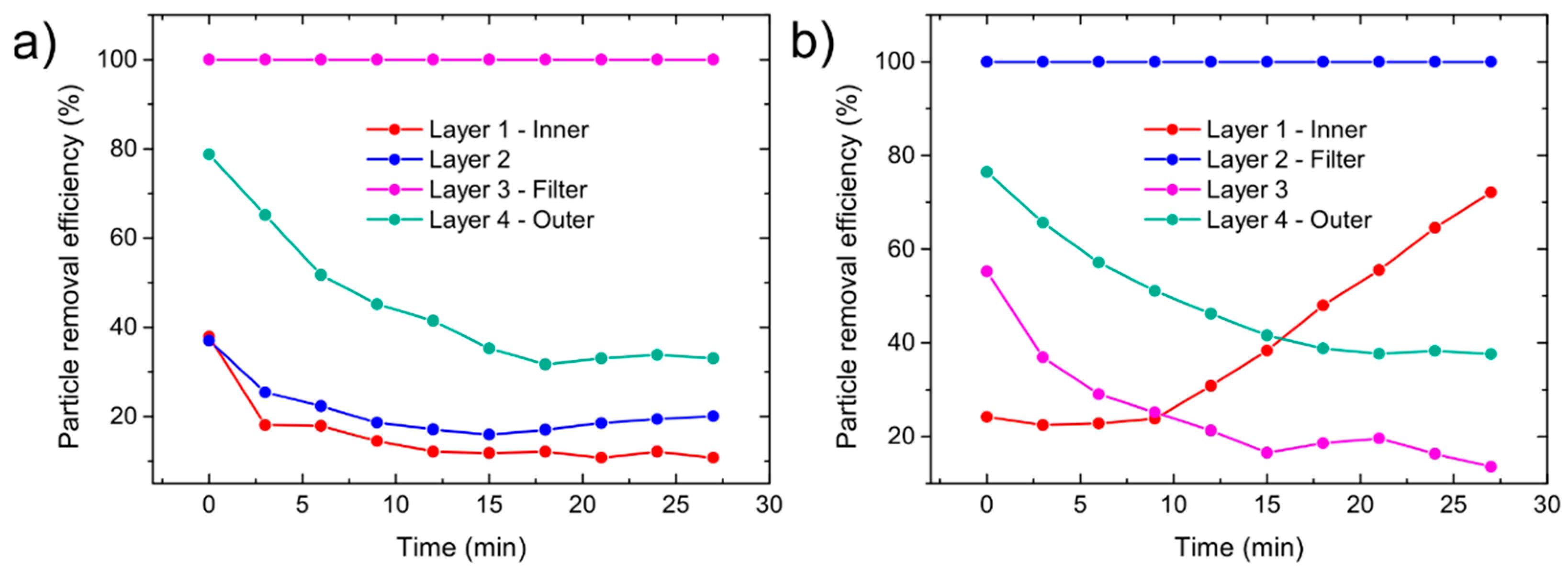
| FFP2 | 17.9 | 22.3 | 100.0 | 51.7 | 100.0 |
| FFP3 | 22.8 | 100.0 | 29.0 | 57.1 | 100.0 |
| PRE | |||
|---|---|---|---|
| Type | Mask/Fabric | Mask | Fabric |
| FFP | FFP2 | 96.0% | 98.6% |
| FFP3 | 97.0% | 99.9% | |
| Surgical mask | A | 79.9% | 99.5% |
| B | 81.6% | 99.4% | |
| C | 65.8% | 94.6% | |
| D | 76.7% | 91.5% | |
| Cotton mask | Poplin A, 120 gsm | / | 72.5% |
| Poplin B, 110 gsm | / | 26.0% | |
| Poplin C, 130 gsm | / | 79.7% | |
| Poplin D, 130 gsm | / | 82.0% | |
| Tetra, 185 gsm | / | 24.7% | |
| Gas mask | 99.9% | / | |
| Snorkeling mask | 96.8% | / | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pogačnik Krajnc, A.; Pirker, L.; Gradišar Centa, U.; Gradišek, A.; Mekjavic, I.B.; Godnič, M.; Čebašek, M.; Bregant, T.; Remškar, M. Size- and Time-Dependent Particle Removal Efficiency of Face Masks and Improvised Respiratory Protection Equipment Used during the COVID-19 Pandemic. Sensors 2021, 21, 1567. https://doi.org/10.3390/s21051567
Pogačnik Krajnc A, Pirker L, Gradišar Centa U, Gradišek A, Mekjavic IB, Godnič M, Čebašek M, Bregant T, Remškar M. Size- and Time-Dependent Particle Removal Efficiency of Face Masks and Improvised Respiratory Protection Equipment Used during the COVID-19 Pandemic. Sensors. 2021; 21(5):1567. https://doi.org/10.3390/s21051567
Chicago/Turabian StylePogačnik Krajnc, Anja, Luka Pirker, Urška Gradišar Centa, Anton Gradišek, Igor B. Mekjavic, Matej Godnič, Metod Čebašek, Tina Bregant, and Maja Remškar. 2021. "Size- and Time-Dependent Particle Removal Efficiency of Face Masks and Improvised Respiratory Protection Equipment Used during the COVID-19 Pandemic" Sensors 21, no. 5: 1567. https://doi.org/10.3390/s21051567
APA StylePogačnik Krajnc, A., Pirker, L., Gradišar Centa, U., Gradišek, A., Mekjavic, I. B., Godnič, M., Čebašek, M., Bregant, T., & Remškar, M. (2021). Size- and Time-Dependent Particle Removal Efficiency of Face Masks and Improvised Respiratory Protection Equipment Used during the COVID-19 Pandemic. Sensors, 21(5), 1567. https://doi.org/10.3390/s21051567









