What Is behind Changes in Resting Heart Rate and Heart Rate Variability? A Large-Scale Analysis of Longitudinal Measurements Acquired in Free-Living
Abstract
:1. Introduction
2. Materials and Methods
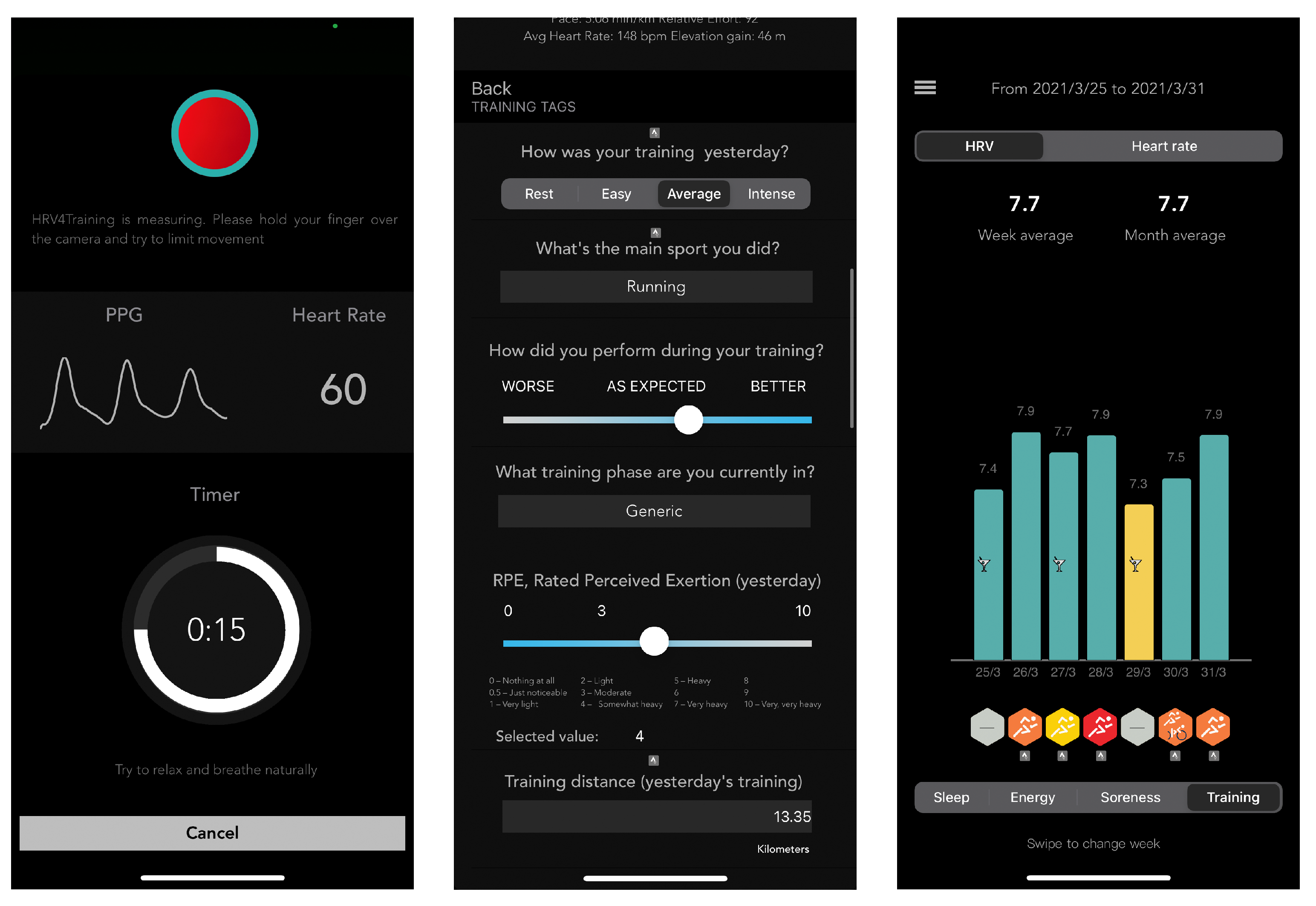
2.1. Data Acquisition
2.1.1. Heart Rate and HRV
2.1.2. Users
2.1.3. Individual Characteristics
2.1.4. Acute Stressors
2.2. Data Analysis
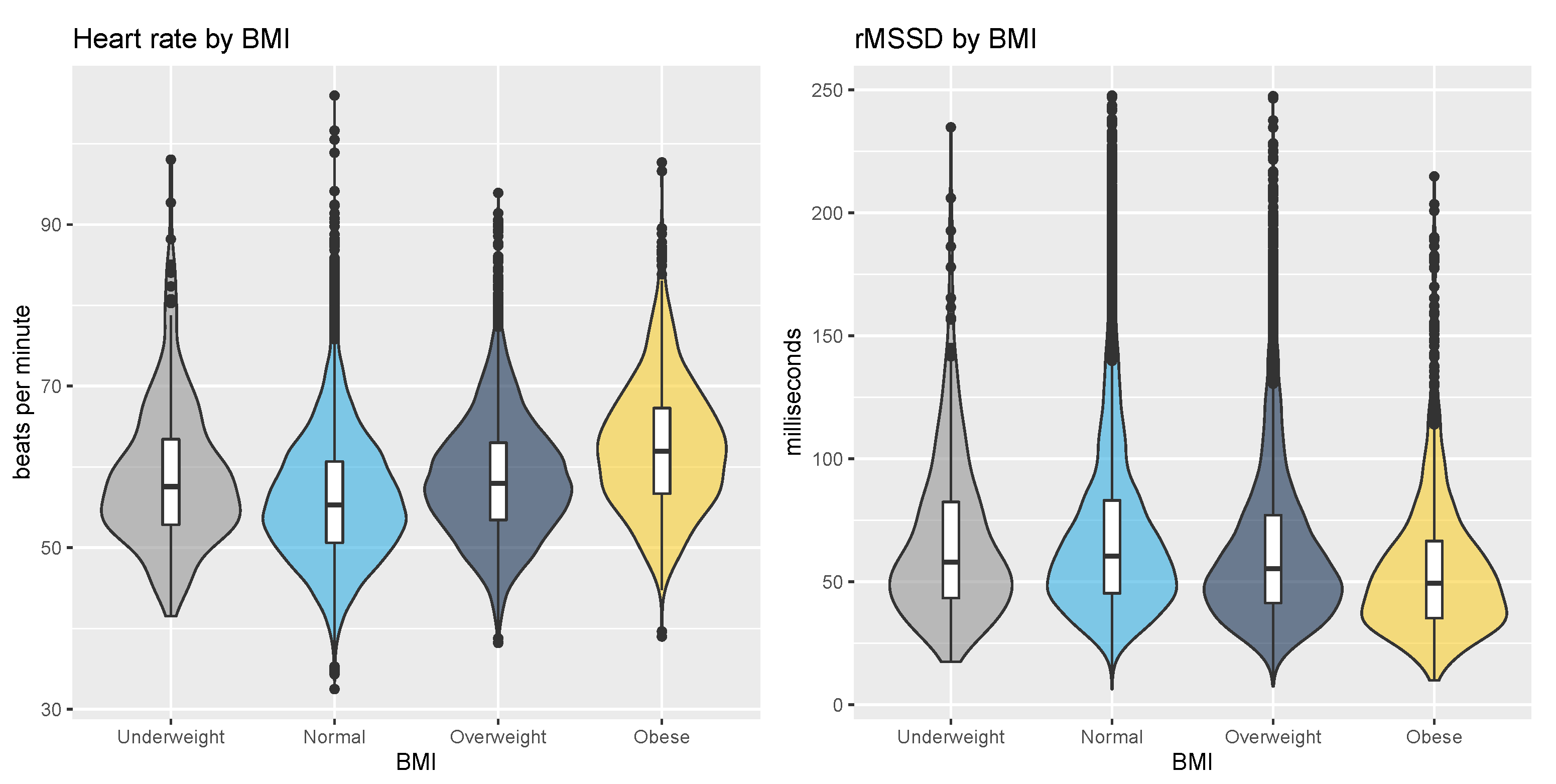
2.2.1. Population Level Analysis
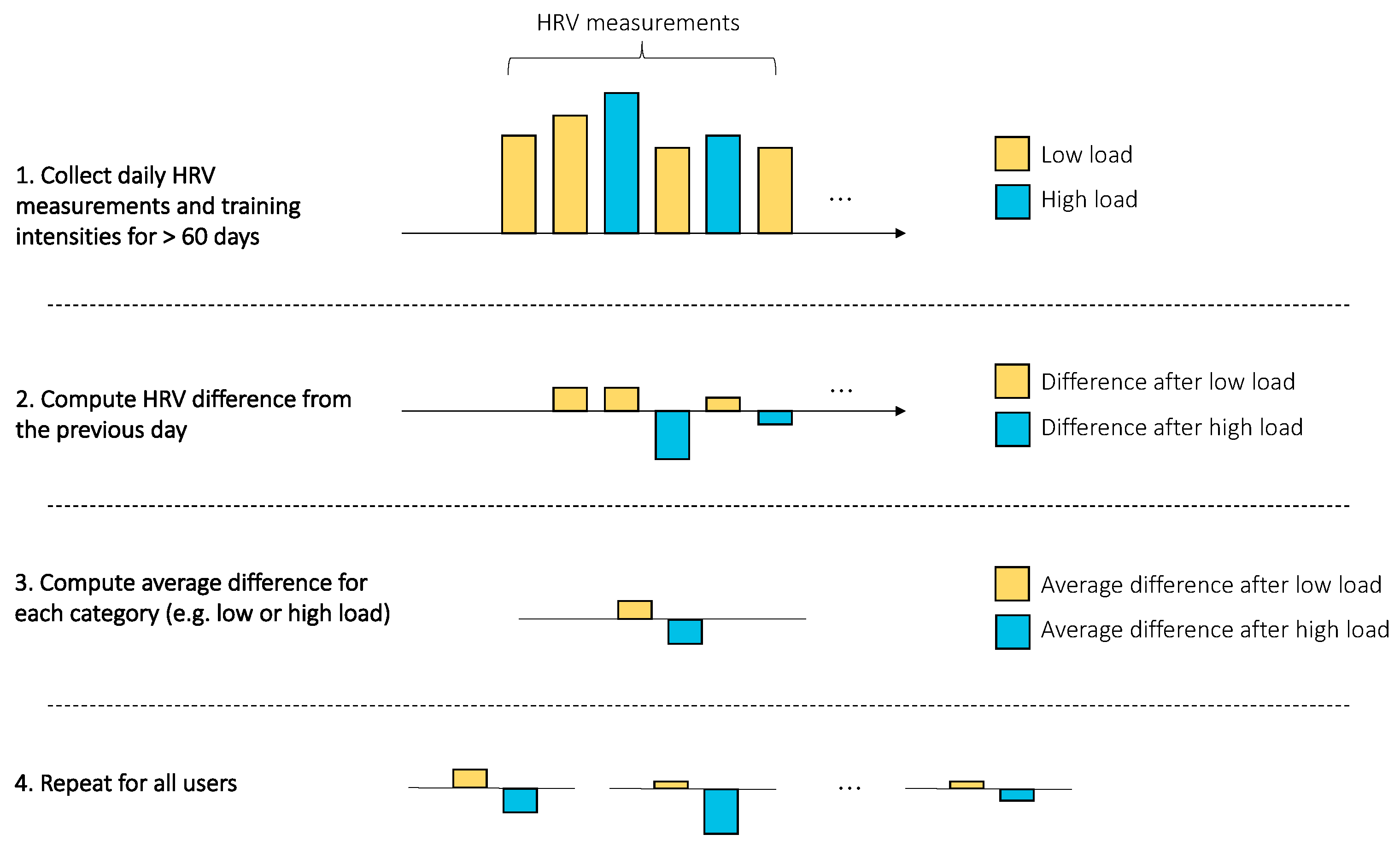
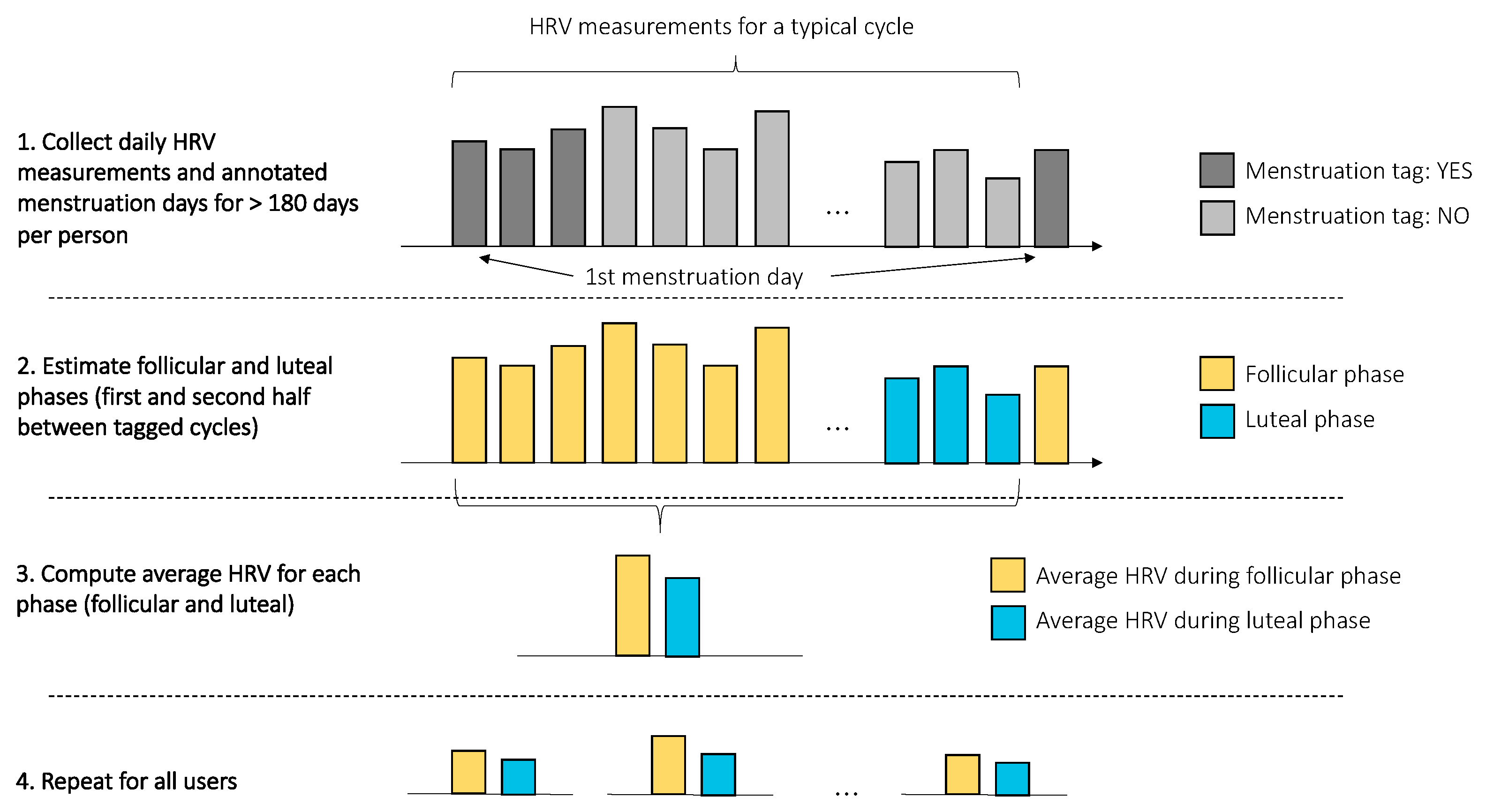
2.2.2. Analysis of Acute Stressors
2.2.3. Statistics
3. Results
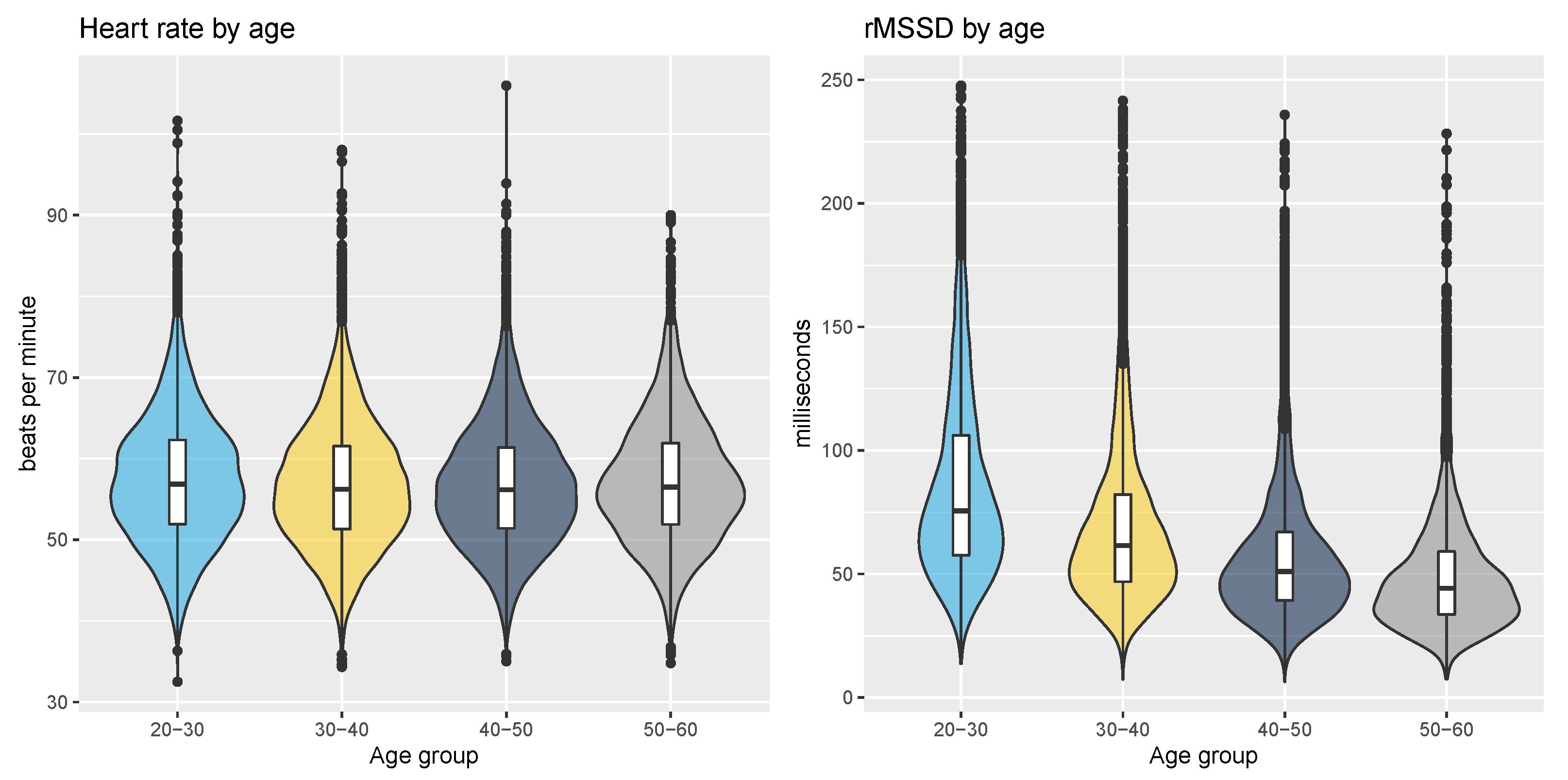
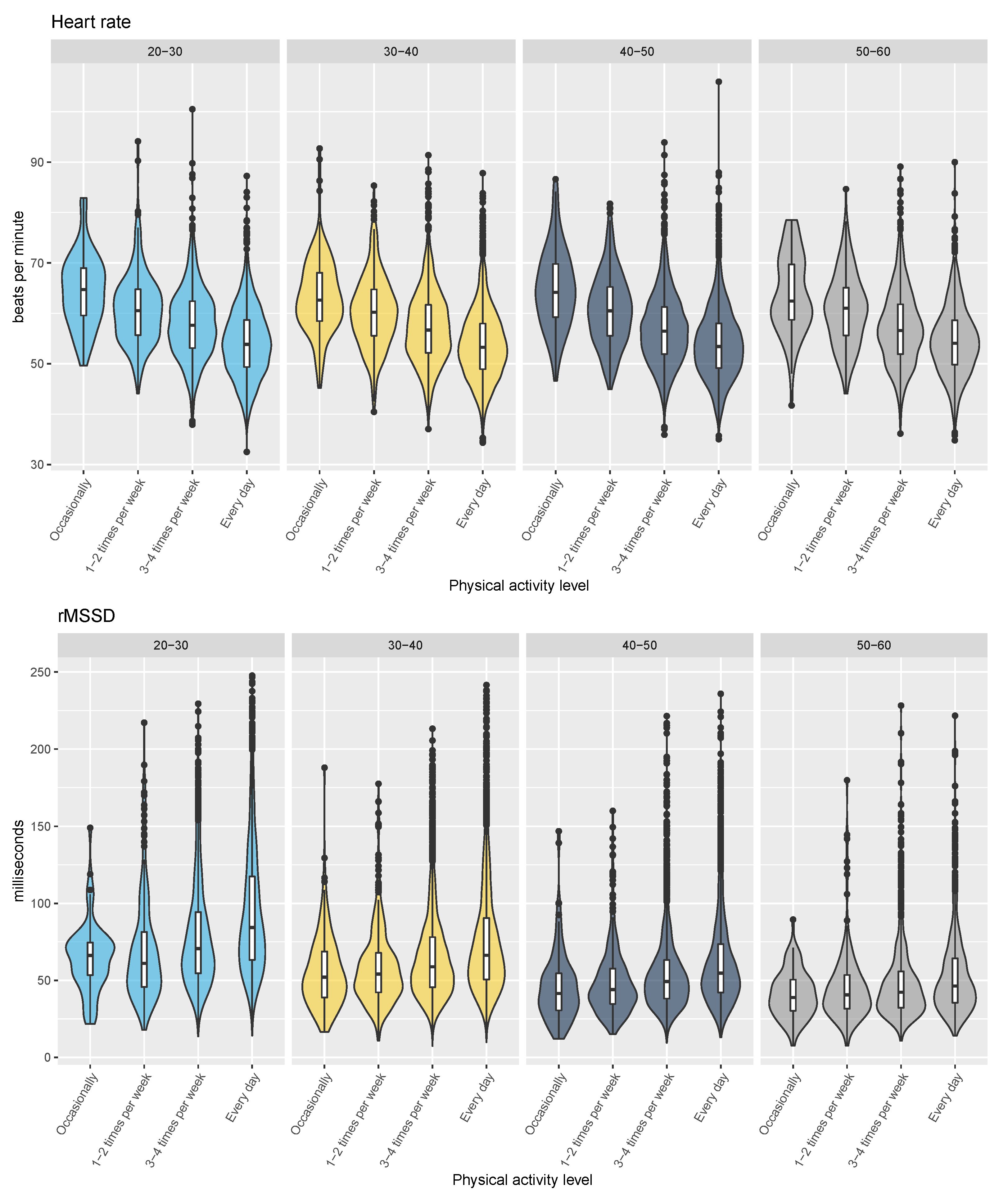
3.1. Population Level Analysis
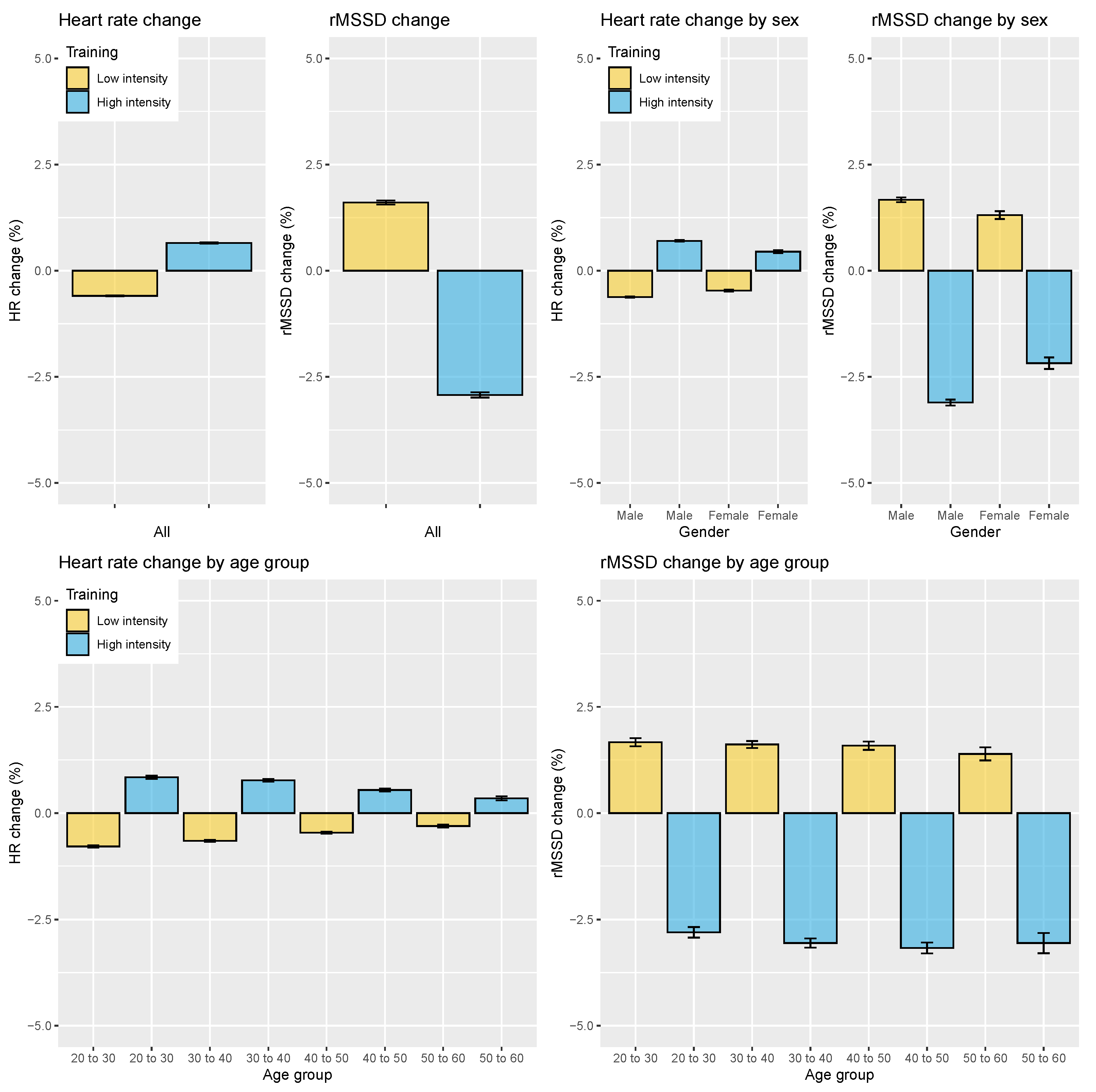
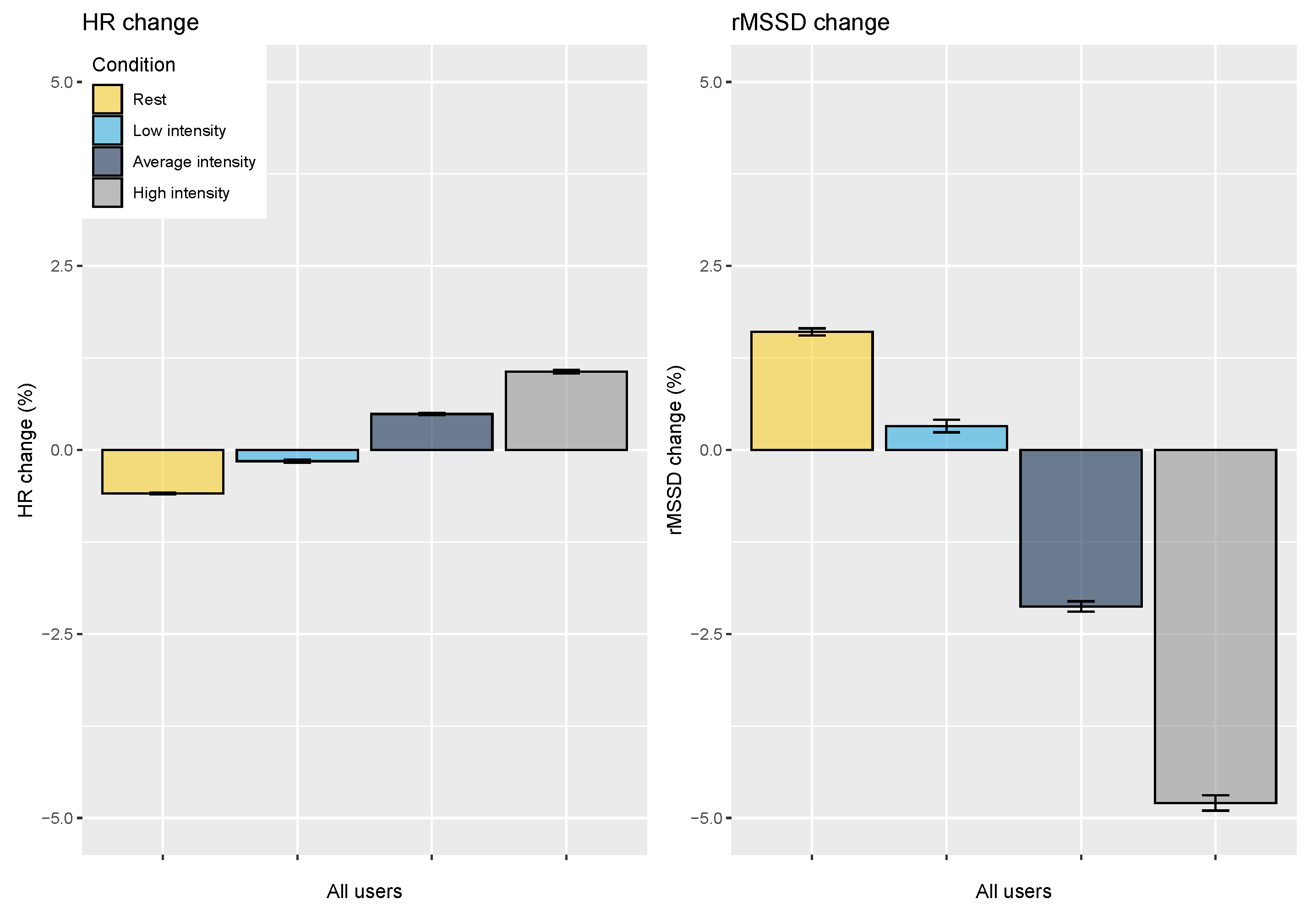
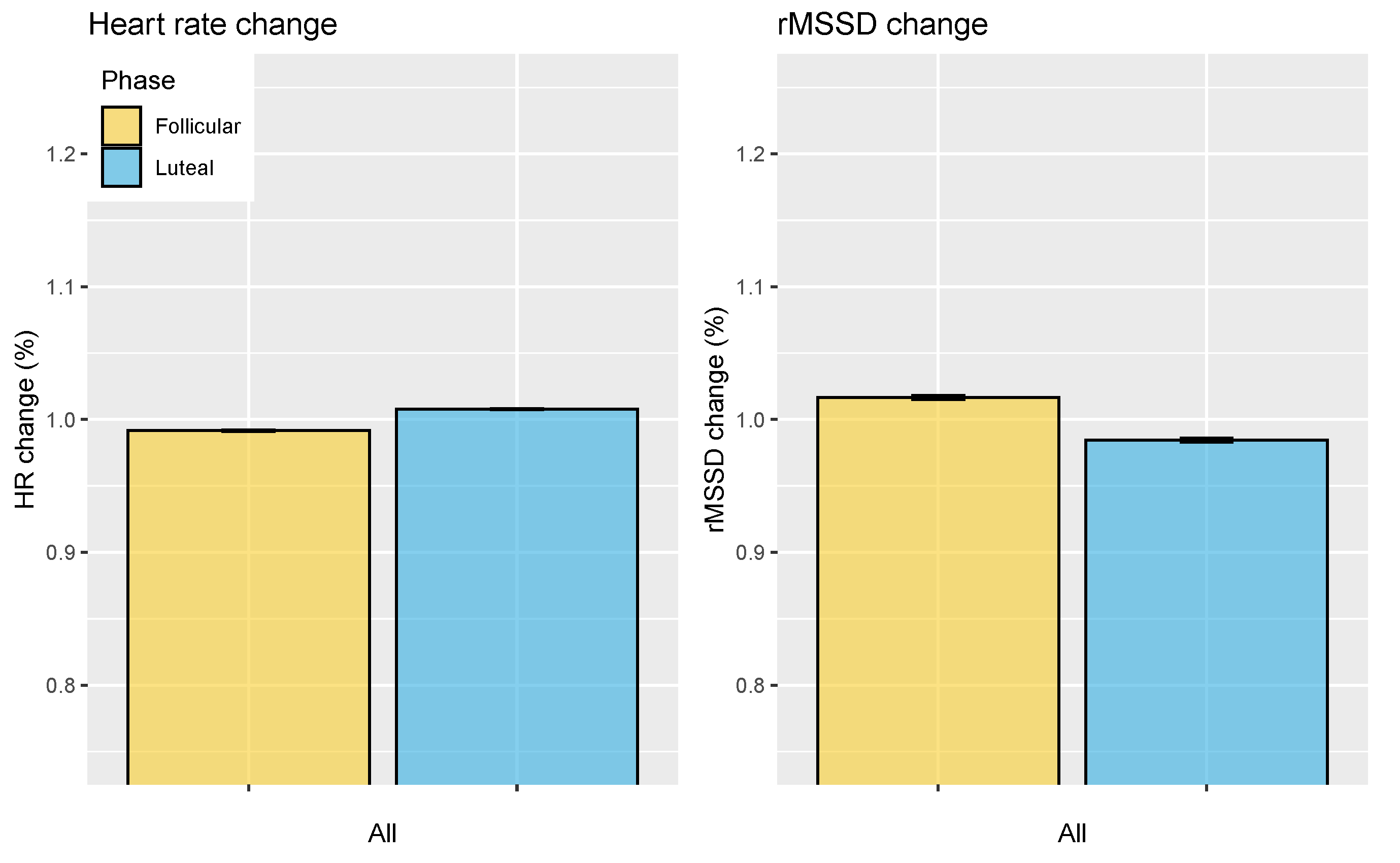
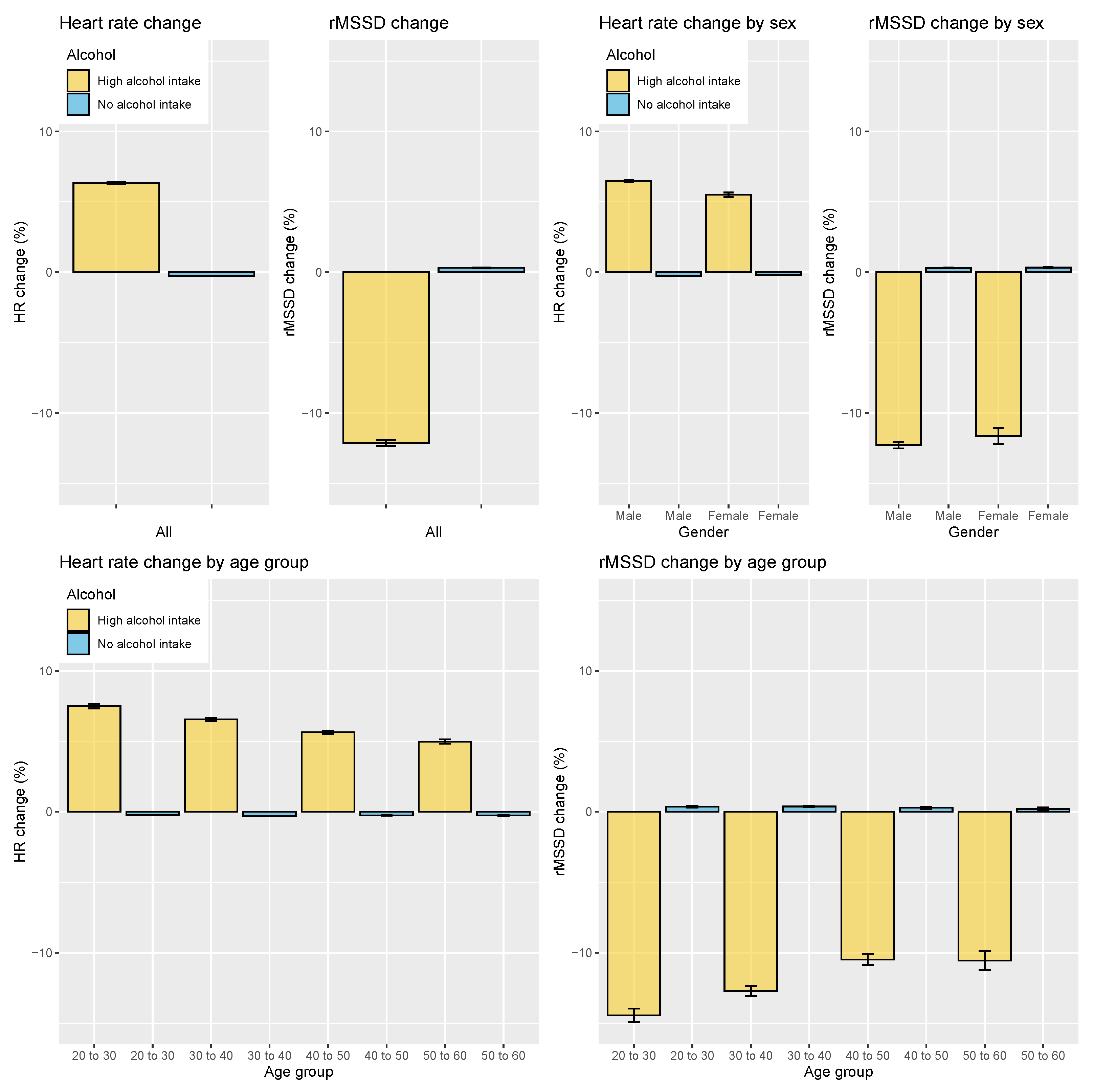
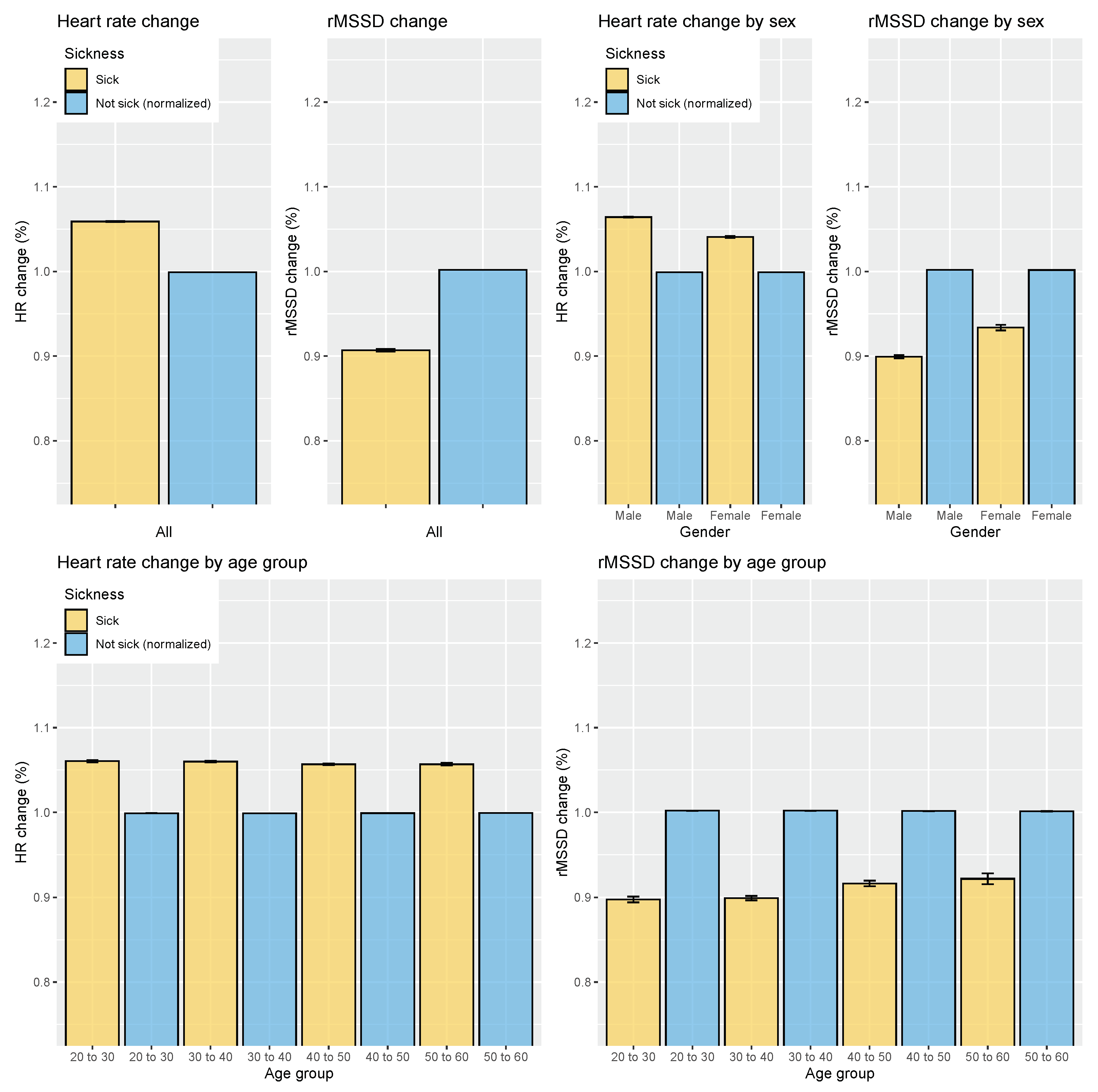
3.2. Analysis of Acute Stressors
4. Discussion
4.1. Population Level Analysis
4.2. Acute Stressors Analysis
4.2.1. Strength of the Stressor
4.2.2. Interpretability
4.2.3. Implications for HRV-Guided Training
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pomeranz, B.; Macaulay, R.; Caudill, M.A.; Kutz, I.; Adam, D.; Gordon, D.; Kilborn, K.M.; Barger, A.C.; Shannon, D.C.; Cohen, R.J. Assessment of autonomic function in humans by heart rate spectral analysis. Am. J. Physiol.-Heart Circ. Physiol. 1985, 248, H151–H153. [Google Scholar] [CrossRef]
- Hedman, A.; Hartikainen, J.; Tahvanainen, K.; Hakumäki, M. The high frequency component of heart rate variability reflects cardiac parasympathetic modulation rather than parasympathetic ‘tone’. Acta Physiol. Scand. 1995, 155, 267–273. [Google Scholar] [CrossRef]
- Russo, M.A.; Santarelli, D.M.; O’Rourke, D. The physiological effects of slow breathing in the healthy human. Breathe 2017, 13, 298–309. [Google Scholar] [CrossRef]
- Gordan, R.; Gwathmey, J.K.; Xie, L.H. Autonomic and endocrine control of cardiovascular function. World J. Cardiol. 2015, 7, 204. [Google Scholar] [CrossRef] [PubMed]
- Katona, P.G.; McLean, M.; Dighton, D.H.; Guz, A. Sympathetic and parasympathetic cardiac control in athletes and nonathletes at rest. J. Appl. Physiol. 1982, 52, 1652–1657. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.; Camm, A.J. Components of heart rate variability–what they really mean and what we really measure. Am. J. Cardiol. 1993, 72, 821–822. [Google Scholar] [CrossRef]
- Mendelowitz, D. Advances in parasympathetic control of heart rate and cardiac function. Physiology 1999, 14, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Berntson, G.G.; Cacioppo, J.T.; Quigley, K.S. Respiratory sinus arrhythmia: Autonomic origins, physiological mechanisms, and psychophysiological implications. Psychophysiology 1993, 30, 183–196. [Google Scholar] [CrossRef]
- Stauss, H.M. Heart rate variability. Am. J. Physiol.-Regul. Integr. Comp. Physiol. 2003, 285, R927–R931. [Google Scholar] [CrossRef] [Green Version]
- Altini, M.; Amft, O. HRV4Training: Large-scale longitudinal training load analysis in unconstrained free-living settings using a smartphone application. In Proceedings of the 2016 38th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Orlando, FL, USA, 16–20 August 2016; pp. 2610–2613. [Google Scholar]
- Jeukendrup, A.; Hesselink, M.; Snyder, A.; Kuipers, H.; Keizer, H. Physiological changes in male competitive cyclists after two weeks of intensified training. Int. J. Sport. Med. 1992, 13, 534–541. [Google Scholar] [CrossRef]
- Plews, D.J.; Laursen, P.B.; Stanley, J.; Kilding, A.E.; Buchheit, M. Training adaptation and heart rate variability in elite endurance athletes: Opening the door to effective monitoring. Sport. Med. 2013, 43, 773–781. [Google Scholar] [CrossRef] [PubMed]
- Stanley, J.; Peake, J.M.; Buchheit, M. Cardiac parasympathetic reactivation following exercise: Implications for training prescription. Sport. Med. 2013, 43, 1259–1277. [Google Scholar] [CrossRef] [PubMed]
- Dressendorfer, R.H.; Wade, C.E.; Scaff, J.H., Jr. Increased morning heart rate in runners: A valid sign of overtraining? Phys. Sportsmed. 1985, 13, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Pichot, V.; Roche, F.; Gaspoz, J.M.; Enjolras, F.; Antoniadis, A.; Minini, P.; Costes, F.; Busso, T.; Lacour, J.R.; Barthelemy, J.C. Relation between heart rate variability and training load in middle-distance runners. Med. Sci. Sport. Exerc. 2000, 32, 1729–1736. [Google Scholar] [CrossRef] [Green Version]
- Weise, F.; Krell, D.; Brinkhoff, N. Acute alcohol ingestion reduces heart rate variability. Drug Alcohol Depend. 1986, 17, 89–91. [Google Scholar] [CrossRef]
- Radin, J.M.; Quer, G.; Ramos, E.; Baca-Motes, K.; Gadaleta, M.; Topol, E.J.; Steinhubl, S.R. Assessment of Prolonged Physiological and Behavioral Changes Associated With COVID-19 Infection. JAMA Netw. Open 2021, 4, e2115959. [Google Scholar] [CrossRef]
- Hasty, F.; García, G.; Dávila, H.; Wittels, S.H.; Hendricks, S.; Chong, S. Heart rate variability as a possible predictive marker for acute inflammatory response in COVID-19 patients. Mil. Med. 2021, 186, e34–e38. [Google Scholar] [CrossRef]
- Emmonds, S.; Heyward, O.; Jones, B. The challenge of applying and undertaking research in female sport. Sport. Med.-Open 2019, 5, 51. [Google Scholar] [CrossRef] [Green Version]
- Kokts-Porietis, R.L.; Minichiello, N.R.; Doyle-Baker, P.K. The effect of the menstrual cycle on daily measures of heart rate variability in athletic women. J. Psychophysiol. 2019, 34, 60–68. [Google Scholar] [CrossRef]
- Zhang, J. Effect of age and sex on heart rate variability in healthy subjects. J. Manip. Physiol. Ther. 2007, 30, 374–379. [Google Scholar] [CrossRef]
- Buchheit, M.; Gindre, C. Cardiac parasympathetic regulation: Respective associations with cardiorespiratory fitness and training load. Am. J. Physiol.-Heart Circ. Physiol. 2006, 291, H451–H458. [Google Scholar] [CrossRef]
- Vella, C.; Robergs, R. A review of the stroke volume response to upright exercise in healthy subjects. Br. J. Sport. Med. 2005, 39, 190–195. [Google Scholar] [CrossRef]
- Koenig, J.; Thayer, J.F. Sex differences in healthy human heart rate variability: A meta-analysis. Neurosci. Biobehav. Rev. 2016, 64, 288–310. [Google Scholar] [CrossRef]
- Plews, D.J.; Scott, B.; Altini, M.; Wood, M.; Kilding, A.E.; Laursen, P.B. Comparison of heart-rate-variability recording with smartphone photoplethysmography, Polar H7 chest strap, and electrocardiography. Int. J. Sport. Physiol. Perform. 2017, 12, 1324–1328. [Google Scholar] [CrossRef]
- HRV4Training. Available online: https://www.hrv4training.com/ (accessed on 30 October 2021).
- Stone, J.D.; Ulman, H.K.; Tran, K.; Thompson, A.G.; Halter, M.D.; Ramadan, J.H.; Stephenson, M.; Finomore, V.S., Jr.; Galster, S.M.; Rezai, A.R.; et al. Assessing the Accuracy of Popular Commercial Technologies That Measure Resting Heart Rate and Heart Rate Variability. Front. Sport. Act. Living 2021, 3, 37. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M. Monitoring training status with HR measures: Do all roads lead to Rome? Front. Physiol. 2014, 5, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saboul, D.; Pialoux, V.; Hautier, C. The breathing effect of the LF/HF ratio in the heart rate variability measurements of athletes. Eur. J. Sport Sci. 2014, 14, S282–S288. [Google Scholar] [CrossRef] [PubMed]
- Flatt, A.A.; Esco, M.R. Heart rate variability stabilization in athletes: Towards more convenient data acquisition. Clin. Physiol. Funct. Imaging 2016, 36, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Esco, M.R.; Flatt, A.A. Ultra-short-term heart rate variability indexes at rest and post-exercise in athletes: Evaluating the agreement with accepted recommendations. J. Sport. Sci. Med. 2014, 13, 535. [Google Scholar]
- Muñoz, I.; Seiler, S.; Bautista, J.; España, J.; Larumbe, E.; Esteve-Lanao, J. Does polarized training improve performance in recreational runners? Int. J. Sport. Physiol. Perform. 2014, 9, 265–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lantz, B. The large sample size fallacy. Scand. J. Caring Sci. 2013, 27, 487–492. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences New York; Academic: New York, NY, USA, 1988; p. 54. [Google Scholar]
- Umetani, K.; Singer, D.H.; McCraty, R.; Atkinson, M. Twenty-four hour time domain heart rate variability and heart rate: Relations to age and gender over nine decades. J. Am. Coll. Cardiol. 1998, 31, 593–601. [Google Scholar] [CrossRef]
- Convertino, V.A. Blood volume: Its adaptation to endurance training. Med. Sci. Sport. Exerc. 1991, 23, 1338–1348. [Google Scholar] [CrossRef]
- Buchheit, M.; Laursen, P.B.; Al Haddad, H.; Ahmaidi, S. Exercise-induced plasma volume expansion and post-exercise parasympathetic reactivation. Eur. J. Appl. Physiol. 2009, 105, 471–481. [Google Scholar] [CrossRef]
- Armstrong, M.; Kerndt, C.C.; Moore, R.A. Physiology, Baroreceptors; [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Jones, P.P.; Christou, D.D.; Jordan, J.; Seals, D.R. Baroreflex buffering is reduced with age in healthy men. Circulation 2003, 107, 1770–1774. [Google Scholar] [CrossRef] [Green Version]
- da Cruz, C.J.G.; Porto, L.G.G.; Molina, G.E. Agreement between the Heart Rate Variability Threshold and Ventilatory Threshold in Young Women: Impact of Cardiac Parasympathetic Status and Cardiorespiratory Fitness. Meas. Phys. Educ. Exerc. Sci. 2021, 0, 1–12. [Google Scholar] [CrossRef]
- Golosheykin, S.; Grant, J.D.; Novak, O.V.; Heath, A.C.; Anokhin, A.P. Genetic influences on heart rate variability. Int. J. Psychophysiol. 2017, 115, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Singh, J.P.; Larson, M.G.; O’Donnell, C.J.; Tsuji, H.; Evans, J.C.; Levy, D. Heritability of heart rate variability: The Framingham Heart Study. Circulation 1999, 99, 2251–2254. [Google Scholar] [CrossRef] [PubMed]
- Uusitalo, A.L.; Vanninen, E.; Levalahti, E.; Battié, M.C.; Videman, T.; Kaprio, J. Role of genetic and environmental influences on heart rate variability in middle-aged men. Am. J. Physiol.-Heart Circ. Physiol. 2007, 293, H1013–H1022. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kiviniemi, A.M.; Hautala, A.J.; Kinnunen, H.; Tulppo, M.P. Endurance training guided individually by daily heart rate variability measurements. Eur. J. Appl. Physiol. 2007, 101, 743–751. [Google Scholar] [CrossRef]
- Vesterinen, V.; Nummela, A.; Heikura, I.; Laine, T.; Hynynen, E.; Botella, J.; Häkkinen, K. Individual endurance training prescription with heart rate variability. Med. Sci. Sport. Exerc. 2016, 48, 1347–1354. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Javaloyes, A.; Sarabia, J.M.; Lamberts, R.P.; Moya-Ramon, M. Training prescription guided by heart-rate variability in cycling. Int. J. Sport. Physiol. Perform. 2019, 14, 23–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Düking, P.; Zinner, C.; Trabelsi, K.; Reed, J.L.; Holmberg, H.C.; Kunz, P.; Sperlich, B. Monitoring and adapting endurance training on the basis of heart rate variability monitored by wearable technologies: A systematic review with meta-analysis. J. Sci. Med. Sport 2021, 24, 1180–1192. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Altini, M.; Plews, D. What Is behind Changes in Resting Heart Rate and Heart Rate Variability? A Large-Scale Analysis of Longitudinal Measurements Acquired in Free-Living. Sensors 2021, 21, 7932. https://doi.org/10.3390/s21237932
Altini M, Plews D. What Is behind Changes in Resting Heart Rate and Heart Rate Variability? A Large-Scale Analysis of Longitudinal Measurements Acquired in Free-Living. Sensors. 2021; 21(23):7932. https://doi.org/10.3390/s21237932
Chicago/Turabian StyleAltini, Marco, and Daniel Plews. 2021. "What Is behind Changes in Resting Heart Rate and Heart Rate Variability? A Large-Scale Analysis of Longitudinal Measurements Acquired in Free-Living" Sensors 21, no. 23: 7932. https://doi.org/10.3390/s21237932
APA StyleAltini, M., & Plews, D. (2021). What Is behind Changes in Resting Heart Rate and Heart Rate Variability? A Large-Scale Analysis of Longitudinal Measurements Acquired in Free-Living. Sensors, 21(23), 7932. https://doi.org/10.3390/s21237932





