Applicability of Physiological Monitoring Systems within Occupational Groups: A Systematic Review
Abstract
:1. Introduction
2. Methods
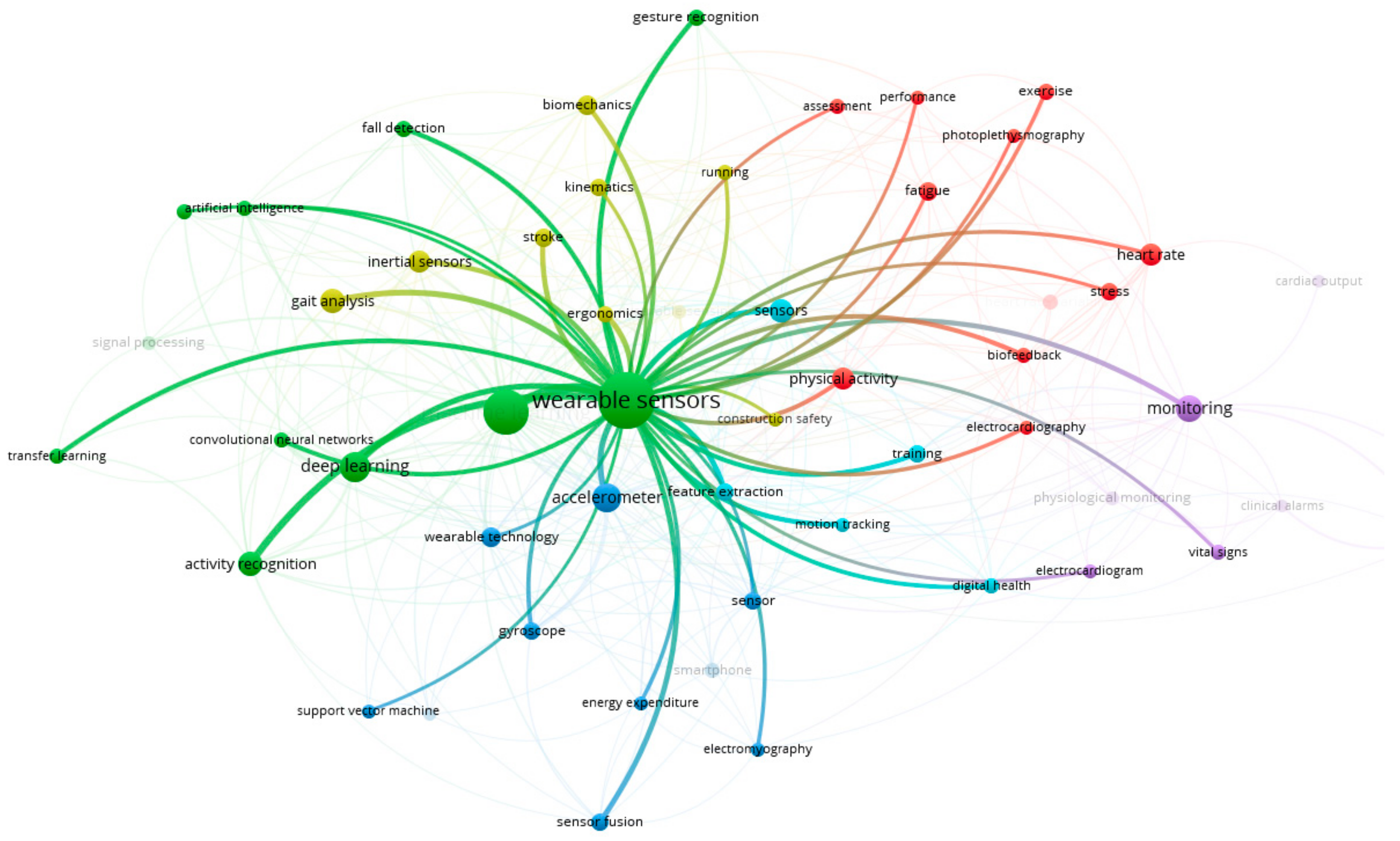
3. Results
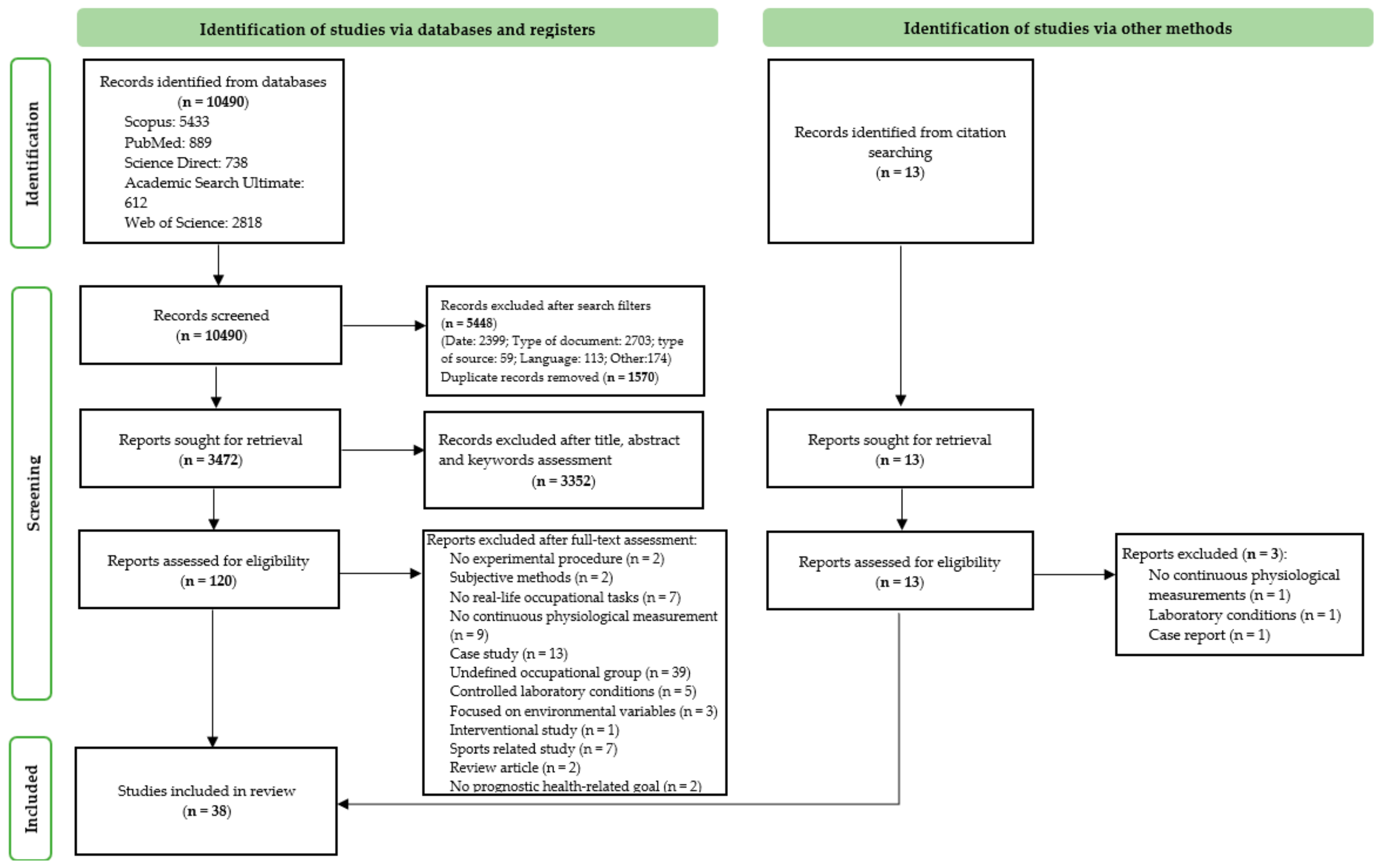
3.1. Studies Selection
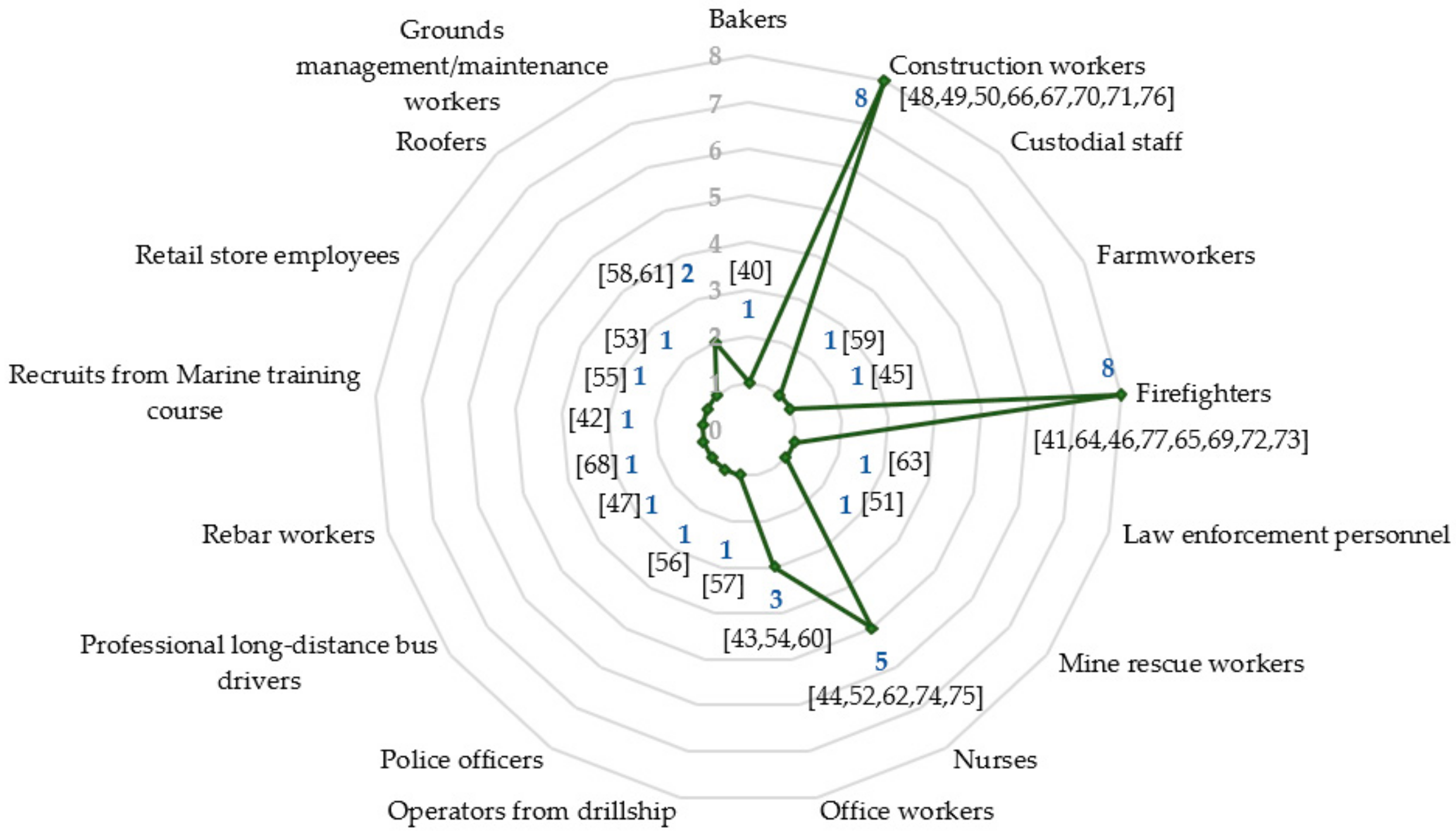
3.2. Characteristics of the Included Studies
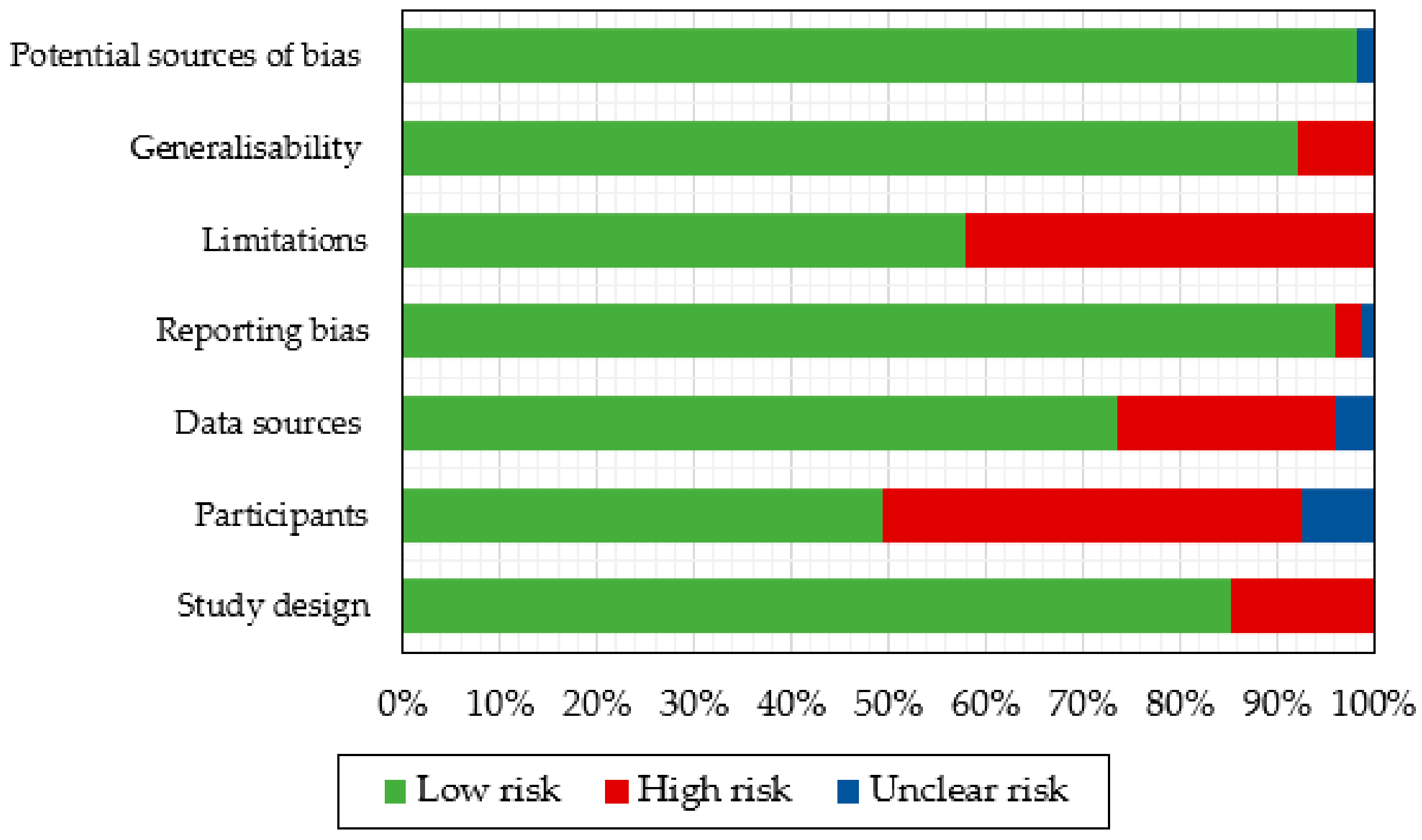
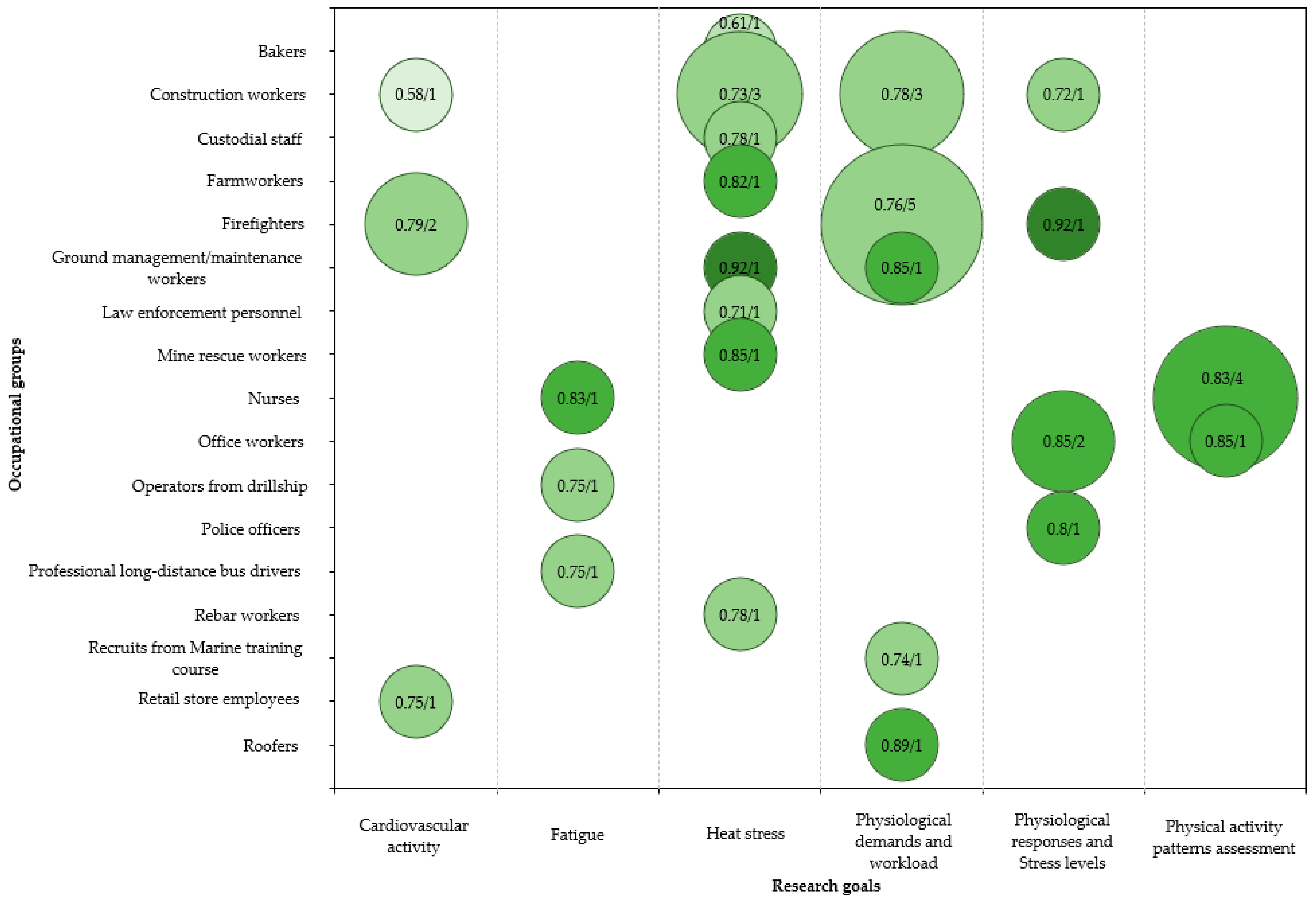
3.3. Risk of Bias Assessment and Quality of Results
4. Discussion
4.1. Monitored Physiological Variables
4.1.1. Cardiac and Thermal Responses
4.1.2. Other Monitored Variables
4.2. Physiological Monitoring Systems and Processing Methods
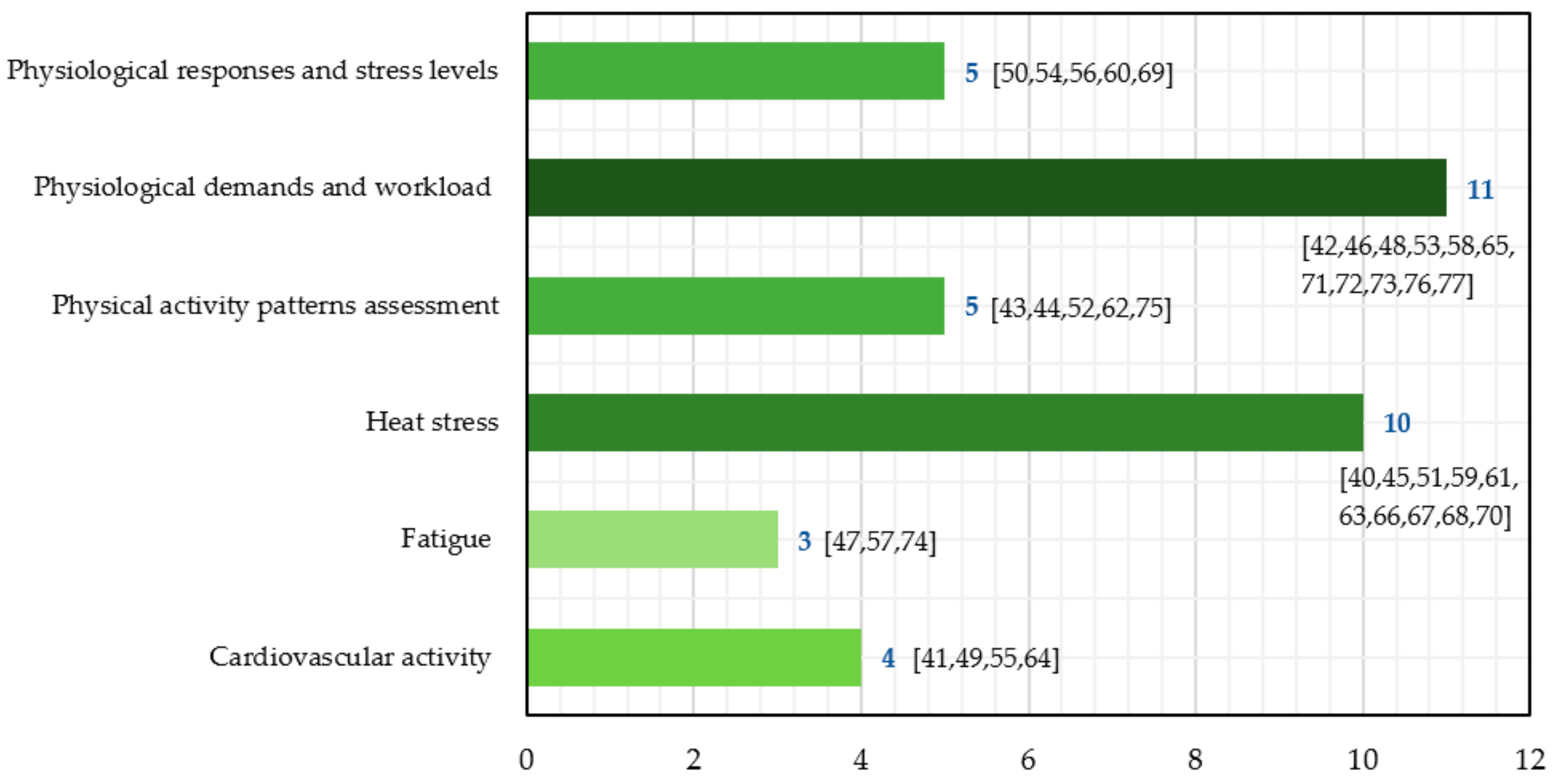
4.3. Safety and Health Applications
4.3.1. Thermal Stress
4.3.2. Physiological Workload
4.3.3. Stress Detection
4.3.4. Physical Activity Patterns
4.3.5. Cardiac Activity
4.3.6. Fatigue
4.4. Current Trends and Future Research Perspectives
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Signals Acquired | Physiological Monitoring Systems | System Specifications/Key Features | Reported Measurement Characteristics | Number of Studies | References |
|---|---|---|---|---|---|
| Cardiac only | Polar heart rate monitors (Polar Electro, Kemple, Finland): Team Pro, H7, S625X, RCX3, Vantage XL, S710 |
| Not reported | 8 | [40,49,65,67,68,70,71,72] |
| H12+ digital Holter recorder V3.12 (Mortara Instrument, Milwaukee, Brookfield, WI, USA) |
| Not reported | 3 | [41,64,72] | |
| Garmin Smartwatch (Garmin International, Olathe, KS): Forerunner 110 monitor and Vivoactive HR |
| Not reported | 3 | [46,58,61] | |
| Apple Watch Series 1 |
| Not reported | 1 | [55] | |
| Heart rate sensor myBeat WHS-2 (Union Tool Co., Ltd., Shanghai, China) |
| 5-min interval | 1 | [48] | |
| Respiratory only | Open-circuit spirometry system (K4b2, Cosmed Srl, Rome, Italy) |
| Not reported | 4 | [66,67,68,73] |
| AeroSport KB1-C ambulatory metabolic analysis, open-circuit spirometry-based system (AeroSport, Inc., Ann Arbor, MI, USA) |
| 20-s measurement interval | 1 | [71] | |
| Multivariable signals | Integrated monitor Equivital Life Monitor EQ-01 and EQ-02 (Hidalgo, Cambridge, UK) |
| Not reported | 7 | [42,51,57,63,69,73,77] |
| Chest-strap Zephyr status monitor |
| Not reported | 4 | [45,53,56,59] | |
| Biofeedback 2000 x-pert system |
| EEG, EMG and respiration modules used, 13 data sections with 15 min interval | 1 | [47] | |
| Wristband-type biosensor E4 manufactured by Empatica, Cambridge, Massachusetts |
| PPG: sampling rate of 64 Hz and an output resolution of 09 nW/digit. EDA: 4-Hz sampling frequency, 900-pS resolution, and range of 0.01–10 μS. Infrared thermopile: sampling rate of 4 Hz and accuracy of 0.02 °C within normal skin temperature | 2 | [50,76] | |
| Chest-worn sensor EcgMove 3 (Movisens) |
| Not reported | 2 | [54,60] | |
| Smart clothing COCOMI (TOYOBO Co., Ltd., Osaka city, Japan) (heart rate, respiration, perspiration, body surface temperature and joint angle) |
| Not reported | 1 | [48] | |
| Samsung Galaxy S4 (Android 4.2.2 Jelly Bean Operation System, octa-core chipset, 1.6-GHz Quad + 1.2 GHz Quad CPU) |
| 1 | [59] | ||
| Basis Fitness Wristband: B1 and Basis Peak™ (BASIS, an Intel Company, San Francisco, CA, USA) |
| 1-min interval | 2 | [49,59] | |
| Activity sensor only | Promove 3D activity sensor (Inertia Technology, Enschede, The Netherlands) |
| Samples of accelerations in three dimensions at 40 Hz and average sum of the Integral of the Modulus of Accelerations (IMA) per minute | 1 | [43] |
| LSM9DS0 sensors by STMicroelectronics, a wearable microcontroller, the Adafruit Flora, via I2C |
| Not reported | 1 | [44] | |
| Wrist actigraph (Ambulatory Monitoring, Inc., Ardsley, NY, USA) |
| 1-min epochs | 1 | [52] | |
| ActiGraph GT9X and wGT3X-BT (ActiGraph, LLC, Pensacola, FL, USA) |
| 100 Hz | 3 | [53,62,73] | |
| Accelerometer-based wrist-worn activity tracker Fitbit Flex and Fitbit Charge 2 (Fitbit Inc., San Francisco, CA, USA) |
| Not reported | 3 | [70,74,75] | |
| GeneActiv accelerometer wristband |
| Not reported | 1 | [59] | |
| Philips Actiwatch Spectrum Pro |
| Not reported | 1 | [74] | |
| Core temperature only | Ingestible thermometric pill (Jonah VitalSense, Respironics, Bend, OR, USA) |
| Not reported | 3 | [51,65,73] |
Appendix B
| Study Reference | Risk of Bias Assessment Criteria | Score: | ||||||
|---|---|---|---|---|---|---|---|---|
| Study Design | Participants | Data Sources | Reporting Bias | Limitations | Generalisability | Potential Sources of Bias | ||
| [40] | 0.86 | 0.60 | 1.00 | 0.83 | 0.00 | 0.00 | 1.00 | 0.61 |
| [41] | 0.86 | 0.80 | 1.00 | 0.83 | 0.00 | 1.00 | 1.00 | 0.78 |
| [42] | 0.86 | 0.80 | 0.50 | 1.00 | 0.00 | 1.00 | 1.00 | 0.74 |
| [43] | 0.86 | 0.60 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.85 |
| [44] | 0.86 | 0.40 | 0.50 | 0.83 | 0.00 | 1.00 | 1.00 | 0.66 |
| [45] | 0.86 | 0.40 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.82 |
| [46] | 0.86 | 0.40 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.82 |
| [47] | 0.86 | 0.40 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.75 |
| [48] | 0.86 | 0.40 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.82 |
| [49] | 0.86 | 0.40 | 0.50 | 1.00 | 0.00 | 1.00 | 0.33 | 0.58 |
| [50] | 0.86 | 0.20 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.72 |
| [51] | 0.86 | 0.60 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.85 |
| [52] | 0.86 | 0.60 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.85 |
| [53] | 0.86 | 0.40 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.89 |
| [54] | 0.86 | 0.60 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.85 |
| [55] | 0.86 | 0.40 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.75 |
| [56] | 0.86 | 0.40 | 0.50 | 0.83 | 1.00 | 1.00 | 1.00 | 0.80 |
| [57] | 0.86 | 0.40 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.75 |
| [58] | 0.86 | 0.60 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.85 |
| [59] | 0.86 | 0.60 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.78 |
| [60] | 0.86 | 0.60 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.85 |
| [61] | 0.86 | 0.60 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.92 |
| [62] | 0.86 | 0.60 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.92 |
| [77] | 0.86 | 0.40 | 0.50 | 1.00 | 1.00 | 1.00 | 1.00 | 0.82 |
| [63] | 0.86 | 0.60 | 0.50 | 1.00 | 0.00 | 1.00 | 1.00 | 0.71 |
| [64] | 0.86 | 0.40 | 0.50 | 0.83 | 1.00 | 1.00 | 1.00 | 0.80 |
| [65] | 0.86 | 0.20 | 1.00 | 1.00 | 1.00 | 0.00 | 1.00 | 0.72 |
| [66] | 0.86 | 0.20 | 0.50 | 0.67 | 1.00 | 1.00 | 1.00 | 0.75 |
| [67] | 0.86 | 0.60 | 0.50 | 0.83 | 0.00 | 0.00 | 1.00 | 0.54 |
| [68] | 0.86 | 0.60 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.78 |
| [69] | 0.86 | 0.60 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.92 |
| [70] | 0.86 | 0.60 | 1.00 | 0.83 | 1.00 | 1.00 | 1.00 | 0.90 |
| [71] | 0.71 | 0.40 | 1.00 | 1.00 | 0.00 | 1.00 | 1.00 | 0.73 |
| [72] | 0.86 | 0.60 | 0.50 | 1.00 | 0.00 | 1.00 | 1.00 | 0.71 |
| [73] | 0.86 | 0.60 | 0.50 | 1.00 | 0.00 | 1.00 | 1.00 | 0.71 |
| [74] | 0.86 | 0.40 | 1.00 | 1.00 | 1.00 | 1.00 | 0.57 | 0.83 |
| [75] | 0.86 | 0.60 | 1.00 | 1.00 | 1.00 | 1.00 | 0.71 | 0.88 |
| [76] | 0.86 | 0.20 | 1.00 | 1.00 | 1.00 | 1.00 | 0.43 | 0.78 |
References
- Butlewski, M.; Dahlke, G.; Drzewiecka, M.; Pacholski, L. Fatigue of miners as a key factor in the work safety system. Procedia Manuf. 2015, 3, 4732–4739. [Google Scholar] [CrossRef] [Green Version]
- Chen, M.-L.; Chen, C.-J.; Yeh, W.-Y.; Huang, J.-W.; Mao, I.-F. Heat stress evaluation and worker fatigue in a steel plant. AIHA J. 2003, 64, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Tomes, C.; Schram, B.; Orr, R. Field Monitoring the Effects of Overnight Shift Work on Specialist Tactical Police Training with Heart Rate Variability Analysis. Sustainability 2021, 13, 7895. [Google Scholar] [CrossRef]
- Buller, M.J.; Welles, A.P.; Friedl, K.E. Wearable physiological monitoring for human thermal-work strain optimization. J. Appl. Physiol. 2017, 124, 432–441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faff, J.; Tutak, T. Physiological responses to working with fire fighting equipment in the heat in relation to subjective fatigue. Ergonomics 1989, 32, 629–638. [Google Scholar] [CrossRef]
- De Maio, M.; Onate, J.; Swain, D.; Morrison, S.; Ringleb, S.; Naiak, D. Physical Performance Decrements in Military Personnel Wearing Personal Protective Equipment (PPE). 2009. Available online: https://apps.dtic.mil/sti/pdfs/ADA567881.pdf (accessed on 13 August 2021).
- Lieberman, H.R.; Bathalon, G.P.; Falco, C.M.; Kramer, F.M.; Morgan III, C.A.; Niro, P. Severe decrements in cognition function and mood induced by sleep loss, heat, dehydration, and undernutrition during simulated combat. Biol. Psychiatry 2005, 57, 422–429. [Google Scholar] [CrossRef]
- Yang, J.; Li, M. Construction characteristics and quality control measures under high altitude and cold conditions. In IOP Conference Series: Earth and Environmental Science; IOP Publishing: Bristol, UK, 2021; Volume 676. [Google Scholar] [CrossRef]
- Raimundo, A.M.; Oliveira, A.V.M.; Gaspar, A.R.; Quintela, D.A. Thermal conditions in freezing chambers and prediction of the thermophysiological responses of workers. Int. J. Biometeorol. 2015, 59, 1623–1632. [Google Scholar] [CrossRef] [PubMed]
- Yanovich, R.; Ketko, I.; Charkoudian, N. Sex differences in human thermoregulation: Relevance for 2020 and beyond. Physiology 2020, 35, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Byrne, J.; Ludington-Hoe, S.M.; Voss, J.G. Occupational Heat Stress, Thermal Comfort, and Cognitive Performance in the OR: An Integrative Review. AORN J. 2020, 111, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Tomes, C.; Schram, B.; Orr, R. Relationships between Heart Rate Variability, Occupational Performance, and Fitness for Tactical Personnel: A Systematic Review. Front. Public Health 2020, 8, 583336. [Google Scholar] [CrossRef] [PubMed]
- Toomingas, A.; Mathiassen, S.E.; Tornqvist, E.W. Occupational Physiology; CRC Press: Boca Raton, FL, USA, 2011. [Google Scholar] [CrossRef]
- Stacey, M.J.; Hill, N.; Woods, D. Physiological monitoring for healthy military personnel. BMJ Mil. Health 2018, 164. [Google Scholar] [CrossRef] [PubMed]
- Raskovic, D.; Martin, T.; Jovanov, E. Medical monitoring applications for wearable computing. Comput. J. 2004, 47, 495–504. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, C.; Rebelo, D.; Silva, F.; Analide, C. Sleep Performance and Physical Activity Estimation from Multisensor Time Series Sleep Environment Data. In Proceedings of the International Symposium on Ambient Intelligence, L’Aquila, Italy, 17–19 June 2020; pp. 166–176. [Google Scholar] [CrossRef]
- Friedl, K.E. Military applications of soldier physiological monitoring. J. Sci. Med. Sport 2018, 21, 1147–1153. [Google Scholar] [CrossRef] [Green Version]
- Hernando, D.; Garatachea, N.; Almeida, R.; Casajús, J.A.; Bailón, R. Validation of Heart Rate Monitor Polar RS800 for Heart Rate Variability Analysis During Exercise. J. Strength Cond. Res. 2018, 32. [Google Scholar] [CrossRef]
- Mündel, T.; Carter, J.M.; Wilkinson, D.M.; Jones, D.A. A comparison of rectal, oesophageal and gastro-intestinal tract temperatures during moderate-intensity cycling in temperate and hot conditions. Clin. Physiol. Funct. Imaging 2016, 36, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Compagnat, M.; Mandigout, S.; Chaparro, D.; Daviet, J.C.; Salle, J.Y. Validity of the Actigraph GT3x and influence of the sensor positioning for the assessment of active energy expenditure during four activities of daily living in stroke subjects. Clin. Rehabil. 2018, 32, 1696–1704. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, S.H.; Wang, G.H.; Ye, F.; Li, P.Z. Validity and reliability of multiparameter physiological measurements recorded by the Equivital LifeMonitor during activities of various intensities. J. Occup. Environ. Hyg. 2013, 10, 78–85. [Google Scholar] [CrossRef]
- Ye, S.; Feng, S.; Huang, L.; Bian, S. Recent Progress in Wearable Biosensors: From Healthcare Monitoring to Sports Analytics. Biosensors 2020, 10, 205. [Google Scholar] [CrossRef] [PubMed]
- Rana, M.; Mittal, V. Wearable Sensors for Real-Time Kinematics Analysis in Sports: A Review. IEEE Sens. J. 2020, 21, 1187–1207. [Google Scholar] [CrossRef]
- Kristoffersson, A.; Lindén, M. Wearable Sensors for Monitoring and Preventing Noncommunicable Diseases: A Systematic Review. Information 2020, 11, 521. [Google Scholar] [CrossRef]
- Ahn, C.R.; Lee, S.; Sun, C.; Jebelli, H.; Yang, K.; Choi, B. Wearable sensing technology applications in construction safety and health. J. Constr. Eng. Manag. 2019, 145, 03119007. [Google Scholar] [CrossRef]
- Anwer, S.; Li, H.; Antwi-Afari Maxwell, F.; Umer, W.; Wong Arnold Yu, L. Evaluation of Physiological Metrics as Real-Time Measurement of Physical Fatigue in Construction Workers: State-of-the-Art Review. J. Constr. Eng. Manag. 2021, 147, 03121001. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bustos, L.D.; Guedes, J.; Costa, J.T. Evidencing the Applicability of Physiological Monitoring For Health Management within Occupational Settings: Protocol for a Systematic Review. Int. J. Occup. Environ. Saf. 2019, 3, 68–76. [Google Scholar] [CrossRef] [Green Version]
- Wohlin, C. Guidelines for snowballing in systematic literature studies and a replication in software engineering. In Proceedings of the 18th International Conference on Evaluation and Assessment in Software Engineering, London, UK, 13–14 May 2014; pp. 1–10. [Google Scholar] [CrossRef]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- du Prel, J.-B.; Röhrig, B.; Blettner, M. Critical appraisal of scientific articles: Part 1 of a series on evaluation of scientific publications. Dtsch. Arztebl. Int. 2009, 106, 100. [Google Scholar] [CrossRef] [PubMed]
- Jadad, A.R.; Moore, R.A.; Carroll, D.; Jenkinson, C.; Reynolds, D.J.M.; Gavaghan, D.J.; McQuay, H.J. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin. Trials 1996, 17, 1–12. [Google Scholar] [CrossRef]
- Spencer, L.; Ritchie, J.; Lewis, J.; Dillon, L. Quality in Qualitative Evaluation: A Framework for Assessing Research Evidence. 2003. Available online: https://www.advance-he.ac.uk/knowledge-hub/quality-qualitative-evaluation-framework-assessing-research-evidence (accessed on 10 August 2021).
- Verhagen, A.P.; de Vet, H.C.; de Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The Prisma Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Afshari, D.; Moradi, S.; Ahmadi Angali, K.; Shirali, G.A. Estimation of Heat Stress and Maximum Acceptable Work Time Based on Physiological and Environmental Response in Hot-Dry Climate: A Case Study in Traditional Bakers. Int. J. Occup. Environ. Med. 2019, 10, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Al-Zaiti, S.; Rittenberger, J.C.; Reis, S.E.; Hostler, D. Electrocardiographic Responses during Fire Suppression and Recovery among Experienced Firefighters. J. Occup. Environ. Med. 2015, 57, 938–942. [Google Scholar] [CrossRef]
- Binsch, O.; Banko, K.M.; Veenstra, B.J.; Valk, P.J.L. Examining the relationship between mental, physical, and organizational factors associated with attrition during maritime forces training. J. Strength Cond. Res. 2015, 29, S187–S191. [Google Scholar] [CrossRef] [PubMed]
- Boerema, S.T.; Essink, G.B.; Toenis, T.M.; van Velsen, L.; Hermens, H.J. Sedentary Behaviour Profiling of OfficeWorkers: A Sensitivity Analysis of Sedentary Cut-Points. Sensors 2016, 16, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bootsman, R.; Markopoulos, P.; Qi, Q.; Wang, Q.; Timmermans, A.A. Wearable technology for posture monitoring at the workplace. Int. J. Hum. Comput. Stud. 2019, 132, 99–111. [Google Scholar] [CrossRef]
- Culp, K.; Tonelli, S. Heat-Related Illness in Midwestern Hispanic Farmworkers: A Descriptive Analysis of Hydration Status and Reported Symptoms. Workplace Health Saf. 2019, 67, 168–178. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.; Gallagher, S. Physiological demand on firefighters crawling during a search exercise. Int. J. Ind. Ergon. 2014, 44, 821–826. [Google Scholar] [CrossRef]
- Fu, R.; Wang, H.; Zhao, W. Dynamic driver fatigue detection using hidden Markov model in real driving condition. Expert Syst. Appl. 2016, 63, 397–411. [Google Scholar] [CrossRef]
- Hashiguchi, N.; Kodama, K.; Lim, Y.; Che, C.; Kuroishi, S.; Miyazaki, Y.; Kobayashi, T.; Kitahara, S.; Tateyama, K. Practical Judgment of Workload Based on Physical Activity, Work Conditions, and Worker’s Age in Construction Site. Sensors 2020, 20, 3786. [Google Scholar] [CrossRef] [PubMed]
- Hwang, S.; Seo, J.; Jebelli, H.; Lee, S. Feasibility analysis of heart rate monitoring of construction workers using a photoplethysmography (PPG) sensor embedded in a wristband-type activity tracker. Autom. Constr. 2016, 71, 372–381. [Google Scholar] [CrossRef]
- Jebelli, H.; Choi, B.; Lee, S. Application of Wearable Biosensors to Construction Sites. I: Assessing Workers’ Stress. J. Constr. Eng. Manag. 2019, 145, 04019079. [Google Scholar] [CrossRef]
- Konrad, J.; Gagnon, D.; Serresse, O.; Oddson, B.; Leduc, C.; Dorman, S.C. Effect of a Simulated Mine Rescue on Physiological Variables and Heat Strain of Mine Rescue Workers. J. Occup. Environ. Med. 2019, 61, 251–261. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.A.; Gay, C.L.; Alsten, C.R. Home-Based Behavioral Sleep Training for Shift Workers: A Pilot Study. Behav. Sleep Med. 2014, 12, 455–468. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Lin, K.Y.; Seto, E.; Migliaccio, G.C. Wearable sensors for monitoring on-duty and off-duty worker physiological status and activities in construction. Autom. Constr. 2017, 83, 341–353. [Google Scholar] [CrossRef]
- Lindberg, C.M.; Srinivasan, K.; Gilligan, B.; Razjouyan, J.; Lee, H.; Najafi, B.; Canada, K.J.; Mehl, M.R.; Currim, F.; Ram, S.; et al. Effects of office workstation type on physical activity and stress. Occup. Environ. Med. 2018, 75, 689–695. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucas, B.; Grayson, S.; Hamidu, H.; Han, A.; No, S.; Varghese, A.; Campisi, J. Sex differences in heart rate responses to occupational stress. Stress 2020, 23, 13–18. [Google Scholar] [CrossRef]
- Marois, A.; Cloutier, M.S.; Saunier, N.; Godillon, S.; Lafond, D.; Vachon, F. Safety, stress and work zone complexity: A field study on police officers performing on-foot traffic control. Transp. Res. Interdiscip. Perspect. 2019, 1, 100018. [Google Scholar] [CrossRef]
- Mehta, R.K.; Peres, S.C.; Kannan, P.; Rhee, J.; Shortz, A.E.; Mannan, M.S. Comparison of objective and subjective operator fatigue assessment methods in offshore shiftwork. J. Loss Prev. Process Ind. 2017, 48, 376–381. [Google Scholar] [CrossRef]
- Nelson, K.B.; Runkle, J.D.; Sugg, M.M. Reporting back environmental health data among outdoor occupational workers in the cold season in north carolina, usa. Southeast. Geogr. 2020, 60, 159–182. [Google Scholar] [CrossRef]
- Pancardo, P.; Acosta, F.D.; Hernandez-Nolasco, J.A.; Wister, M.A.; Lopez-de-Ipina, D. Real-Time Personalized Monitoring to Estimate Occupational Heat Stress in Ambient Assisted Working. Sensors 2015, 15, 16956–16980. [Google Scholar] [CrossRef] [PubMed]
- Razjouyan, J.; Lee, H.; Gilligan, B.; Lindberg, C.; Nguyen, H.; Canada, K.; Burton, A.; Sharafkhaneh, A.; Srinivasan, K.; Currim, F.; et al. Wellbuilt for wellbeing: Controlling relative humidity in the workplace matters for our health. Indoor Air 2020, 30, 167–179. [Google Scholar] [CrossRef] [PubMed]
- Runkle, J.D.; Cui, C.; Fuhrmann, C.; Stevens, S.; Del Pinal, J.; Sugg, M.M. Evaluation of wearable sensors for physiologic monitoring of individually experienced temperatures in outdoor workers in southeastern U.S. Environ. Int. 2019, 129, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Schall, M.C.; Fethke, N.B.; Chen, H. Working postures and physical activity among registered nurses. Appl. Ergon. 2016, 54, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Yokota, M.; Karis, A.J.; Tharion, W.J. Thermal-work strain in law enforcement personnel during chemical, biological, radiological, and nuclear (CBRN) training. Int. J. Occup. Environ. Health 2014, 20, 126–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carey, M.G.; Thevenin, B.J.M. High-resolution 12-lead electrocardiograms of on-duty professional firefighters: A pilot feasibility study. J. Cardiovasc. Nurs. 2009, 24, 261–267. [Google Scholar] [CrossRef] [Green Version]
- Horn, G.P.; Blevins, S.; Fernhall, B.; Smith, D.L. Core temperature and heart rate response to repeated bouts of firefighting activities. Ergonomics 2013, 56, 1465–1473. [Google Scholar] [CrossRef] [PubMed]
- Yi, W.; Chan, A.P.C.; Wang, X.; Wang, J. Development of an early-warning system for site work in hot and humid environments: A case study. Autom. Constr. 2016, 62, 101–113. [Google Scholar] [CrossRef]
- Wong, D.P.-L.; Chung, J.W.-Y.; Chan, A.P.-C.; Wong, F.K.-W.; Yi, W. Comparing the physiological and perceptual responses of construction workers (bar benders and bar fixers) in a hot environment. Appl. Ergon. 2014, 45, 1705–1711. [Google Scholar] [CrossRef] [Green Version]
- Chan, A.P.C.; Yi, W.; Wong, D.P.; Yam, M.C.H.; Chan, D.W.M. Determining an optimal recovery time for construction rebar workers after working to exhaustion in a hot and humid environment. Build. Environ. 2012, 58, 163–171. [Google Scholar] [CrossRef] [Green Version]
- Meina, M.; Ratajczak, E.; Sadowska, M.; Rykaczewski, K.; Dreszer, J.; Bałaj, B.; Biedugnis, S.; Węgrzyński, W.; Krasuski, A. Heart Rate Variability and Accelerometry as Classification Tools for Monitoring Perceived Stress Levels—A Pilot Study on Firefighters. Sensors 2020, 20, 2834. [Google Scholar] [CrossRef]
- Al-Bouwarthan, M.; Quinn, M.M.; Kriebel, D.; Wegman, D.H. A Field Evaluation of Construction Workers’ Activity, Hydration Status, and Heat Strain in the Extreme Summer Heat of Saudi Arabia. Ann. Work Expo. Health 2020, 64, 522–535. [Google Scholar] [CrossRef] [PubMed]
- Abdelhamid, T.S.; Everett, J.G. Physiological demands during construction work. J. Constr. Eng. Manag. 2002, 128, 427–437. [Google Scholar] [CrossRef]
- Angerer, P.; Kadlez-Gebhardt, S.; Delius, M.; Raluca, P.; Nowak, D. Comparison of Cardiocirculatory and Thermal Strain of Male Firefighters during Fire Suppression to Exercise Stress Test and Aerobic Exercise Testing. Am. J. Cardiol. 2008, 102, 1551–1556. [Google Scholar] [CrossRef] [PubMed]
- Horn, G.P.; Kesler, R.M.; Motl, R.W.; Hsiao-Wecksler, E.T.; Klaren, R.E.; Ensari, I.; Petrucci, M.N.; Fernhall, B.; Rosengren, K.S. Physiological responses to simulated firefighter exercise protocols in varying environments. Ergonomics 2015, 58, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Brzozowski, S.L.; Cho, H.; Arsenault Knudsen, É.N.; Steege, L.M. Predicting nurse fatigue from measures of work demands. Appl. Ergon. 2021, 92, 103337. [Google Scholar] [CrossRef] [PubMed]
- Feng, T.; Booth, B.M.; Baldwin-Rodríguez, B.; Osorno, F.; Narayanan, S. A multimodal analysis of physical activity, sleep, and work shift in nurses with wearable sensor data. Sci. Rep. 2021, 11, 8693. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.G.; Choi, B.; Jebelli, H.; Lee, S. Assessment of construction workers’ perceived risk using physiological data from wearable sensors: A machine learning approach. J. Build. Eng. 2021, 42, 102824. [Google Scholar] [CrossRef]
- Sol, J.A.; Ruby, B.C.; Gaskill, S.E.; Dumke, C.L.; Domitrovich, J.W. Metabolic Demand of Hiking in Wildland Firefighting. Wilderness Environ. Med. 2018, 29, 304–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tadic, M.; Cuspidi, C.; Grassi, G. Heart rate as a predictor of cardiovascular risk. Eur. J. Clin. Investig. 2018, 48, e12892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Borg, G.; Hassmén, P.; Lagerström, M. Perceived exertion related to heart rate and blood lactate during arm and leg exercise. Eur. J. Appl. Physiol. Occup. Physiol. 1987, 56, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Hankins, T.C.; Wilson, G.F. A comparison of heart rate, eye activity, EEG and subjective measures of pilot mental workload during flight. Aviat. Space Environ. Med. 1998, 69, 360–367. [Google Scholar] [PubMed]
- Carney, R.M.; Steinmeyer, B.; Freedland, K.E.; Stein, P.K.; Hayano, J.; Blumenthal, J.A.; Jaffe, A.S. Nocturnal patterns of heart rate and the risk of mortality after acute myocardial infarction. Am. Heart J. 2014, 168, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Kang, D.; Kim, Y.; Kim, J.; Hwang, Y.; Cho, B.; Hong, T.; Sung, B.; Lee, Y. Effects of high occupational physical activity, aging, and exercise on heart rate variability among male workers. Ann. Occup. Environ. Med. 2015, 27, 22. [Google Scholar] [CrossRef] [Green Version]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research—Recommendations for Experiment Planning, Data Analysis, and Data Reporting. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ernst, G. Heart-Rate Variability—More than Heart Beats? Front. Public Health 2017, 5. [Google Scholar] [CrossRef]
- Lee, W.; Lin, K.-Y.; Johnson, P.W.; Seto, E.Y.W. Selection of wearable sensor measurements for monitoring and managing entry-level construction worker fatigue: A logistic regression approach. Eng. Constr. Archit. Manag. 2021. ahead-of-print. [Google Scholar] [CrossRef]
- Aryal, A.; Ghahramani, A.; Becerik-Gerber, B. Monitoring fatigue in construction workers using physiological measurements. Autom. Constr. 2017, 82, 154–165. [Google Scholar] [CrossRef]
- Umer, W.; Li, H.; Yantao, Y.; Antwi-Afari, M.F.; Anwer, S.; Luo, X. Physical exertion modeling for construction tasks using combined cardiorespiratory and thermoregulatory measures. Autom. Constr. 2020, 112, 103079. [Google Scholar] [CrossRef]
- ISO. ISO 9886: 2004 Ergonomics—Evaluation of Thermal Strain by Physiological Measurements. 2004. Available online: https://www.iso.org/standard/34110.html (accessed on 25 August 2021).
- Cuddy, J.S.; Buller, M.; Hailes, W.S.; Ruby, B.C. Skin Temperature and Heart Rate Can Be Used to Estimate Physiological Strain During Exercise in the Heat in a Cohort of Fit and Unfit Males. Mil. Med. 2013, 178, e841–e847. [Google Scholar] [CrossRef] [Green Version]
- Hunt, A.P.; Billing, D.C.; Patterson, M.J.; Caldwell, J.N. Heat strain during military training activities: The dilemma of balancing force protection and operational capability. Temperature 2016, 3, 307–317. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheshire, W.P. Thermoregulatory disorders and illness related to heat and cold stress. Auton. Neurosci. 2016, 196, 91–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mokhlespour Esfahani, M.I.; Nussbaum, M.A.; Kong, Z. Using a smart textile system for classifying occupational manual material handling tasks: Evidence from lab-based simulations. Ergonomics 2019, 62, 823–833. [Google Scholar] [CrossRef]
- Nicolò, A.; Massaroni, C.; Schena, E.; Sacchetti, M. The Importance of Respiratory Rate Monitoring: From Healthcare to Sport and Exercise. Sensors 2020, 20, 6396. [Google Scholar] [CrossRef] [PubMed]
- Nicolò, A.; Massaroni, C.; Passfield, L. Respiratory frequency during exercise: The neglected physiological measure. Front. Physiol. 2017, 8, 922. [Google Scholar] [CrossRef] [PubMed]
- Massaroni, C.; Tocco, J.D.; Bravi, M.; Carnevale, A.; Presti, D.L.; Sabbadini, R.; Miccinilli, S.; Sterzi, S.; Formica, D.; Schena, E. Respiratory Monitoring During Physical Activities With a Multi-Sensor Smart Garment and Related Algorithms. IEEE Sens. J. 2020, 20, 2173–2180. [Google Scholar] [CrossRef]
- Hernando, A.; Lázaro, J.; Gil, E.; Arza, A.; Garzón, J.M.; López-Antón, R.; Cámara, C.d.l.; Laguna, P.; Aguiló, J.; Bailón, R. Inclusion of Respiratory Frequency Information in Heart Rate Variability Analysis for Stress Assessment. IEEE J. Biomed. Health Inform. 2016, 20, 1016–1025. [Google Scholar] [CrossRef] [PubMed]
- Khoshmanesh, F.; Thurgood, P.; Pirogova, E.; Nahavandi, S.; Baratchi, S. Wearable sensors: At the frontier of personalised health monitoring, smart prosthetics and assistive technologies. Biosens. Bioelectron. 2021, 176. [Google Scholar] [CrossRef] [PubMed]
- Austad, H.; Wiggen, Ø.; Færevik, H.; Seeberg, T.M. Towards a wearable sensor system for continuous occupational cold stress assessment. Ind. Health 2018, 56, 228–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shumate, T.; Link, M.; Furness, J.; Smith, K.K.; Simas, V.; Climstein, M. Validity of the polar vantage m watch when measuring heart rate at different exercise intensities. PeerJ 2021, 9. [Google Scholar] [CrossRef]
- Karaca, A.; Demirci, N.; Yılmaz, V.; Hazır Aytar, S.; Can, S.; Ünver, E. Validation of the ActiGraph wGT3X-BT Accelerometer for Step Counts at Five Different Body Locations in Laboratory Settings. Meas. Phys. Educ. Exerc. Sci. 2021. [Google Scholar] [CrossRef]
- Benedetti, D.; Olcese, U.; Frumento, P.; Bazzani, A.; Bruno, S.; d’Ascanio, P.; Maestri, M.; Bonanni, E.; Faraguna, U. Heart rate detection by Fitbit ChargeHR™: A validation study versus portable polysomnography. J. Sleep Res. 2021. [Google Scholar] [CrossRef] [PubMed]
- Zlatar, T.; Torres Costa, J.; Vaz, M.; Santos Baptista, J. Influence of severe cold thermal environment on core and skin temperatures: A systematic review. Work 2019, 62, 337–352. [Google Scholar] [CrossRef] [PubMed]
- Jussila, K.; Rissanen, S.; Aminoff, A.; Wahlström, J.; Vaktskjold, A.; Talykova, L.; Remes, J.; Mänttäri, S.; Rintamäki, H. Thermal comfort sustained by cold protective clothing in arctic open-pit mining—A thermal manikin and questionnaire study. Ind. Health 2017, 55, 537–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ray, M.; King, M.; Carnahan, H. A review of cold exposure and manual performance: Implications for safety, training and performance. Saf. Sci. 2019, 115, 1–11. [Google Scholar] [CrossRef]
- Abed, S.N.; Kadhim, R.A.; Abbas, D.M. Assessment of the work conditions of small slaughterhouses in the Thi-Qar Governorate in Iraq. J. Public Health Res. 2021, 10, 1–4. [Google Scholar] [CrossRef]
- Auttanate, N.; Chotiphan, C.; Maruo, S.J.; Näyhä, S.; Jussila, K.; Rissanen, S.; Sripaiboonkij, P.; Ikäheimo, T.M.; Jaakkola, J.J.K.; Phanprasit, W. Cold-related symptoms and performance degradation among Thai poultry industry workers with reference to vulnerable groups: A cross-sectional study. BMC Public Health 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, S.; Paiva, J.S.; Dias, D.; Pimentel, G.; Kaiseler, M.; Cunha, J.P.S. Wearable Biomonitoring Platform for the Assessment of Stress and its Impact on Cognitive Performance of Firefighters: An Experimental Study. Clin. Pract. Epidemiol. Ment. Health 2018, 14, 250–262. [Google Scholar] [CrossRef] [PubMed]
- Vavrinsky, E.; Stopjakova, V.; Kopani, M.; Kosnacova, H. The Concept of Advanced Multi-Sensor Monitoring of Human Stress. Sensors 2021, 21, 3499. [Google Scholar] [CrossRef] [PubMed]
- Thielmann, B.; Pohl, R.; Böckelmann, I. Heart rate variability as a strain indicator for psychological stress for emergency physicians during work and alert intervention: A systematic review. J. Occup. Med. Toxicol. 2021, 16. [Google Scholar] [CrossRef] [PubMed]
- Frazier, S.E.; Parker, S.H. Measurement of physiological responses to acute stress in multiple occupations: A systematic review and implications for front line healthcare providers. Transl. Behav. Med. 2019, 9, 158–166. [Google Scholar] [CrossRef] [Green Version]
- Robinson, A.M. Let’s Talk about Stress: History of Stress Research. Rev. Gen. Psychol. 2018, 22, 334–342. [Google Scholar] [CrossRef]
- Clark, C.C.T.; Nobre, G.C.; Fernandes, J.F.T.; Moran, J.; Drury, B.; Mannini, A.; Gronek, P.; Podstawski, R. Physical activity characterization: Does one site fit all? Physiol. Meas. 2018, 39, 09TR02. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.; Fernandez, A.M.; Lu, A.S. Application and Validation of Activity Monitors’ Epoch Lengths and Placement Sites for Physical Activity Assessment in Exergaming. J. Clin. Med. 2018, 7, 268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Achten, J.; Jeukendrup, A.E. Heart rate monitoring. Sports Med. 2003, 33, 517–538. [Google Scholar] [CrossRef] [PubMed]
- Seravalle, G.; Quarti Trevano, F.; Grassi, G. Heart rate as a predictor of cardiovascular risk. Minerva Med. 2021, 112, 130–143. [Google Scholar] [CrossRef]
- Smith, D.L.; Haller, J.M.; Benedict, R.; Moore-Merrell, L. Firefighter Incident Rehabilitation: Interpreting Heart Rate Responses. Prehosp. Emerg. Care 2016, 20, 28–36. [Google Scholar] [CrossRef]
- Knoop, V.; Cloots, B.; Costenoble, A.; Debain, A.; Vella Azzopardi, R.; Vermeiren, S.; Jansen, B.; Scafoglieri, A.; Bautmans, I.; Bautmans, I.; et al. Fatigue and the prediction of negative health outcomes: A systematic review with meta-analysis. Ageing Res. Rev. 2021, 67, 101261. [Google Scholar] [CrossRef] [PubMed]
- Bustos, D.; Guedes, J.C.; Vaz, M.P.; Pombo, E.; Fernandes, R.J.; Costa, J.T.; Baptista, J.S. Non-Invasive Physiological Monitoring for Physical Exertion and Fatigue Assessment in Military Personnel: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8815. [Google Scholar] [CrossRef] [PubMed]
- Thompson, B.J. Does work-induced fatigue accumulate across three compressed 12 hour shifts in hospital nurses and aides? PLoS ONE 2019, 14, e0211715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- ACSM. ACSM’s Health-Related Physical Fitness Assessment Manual. 2013. Available online: https://www.acsm.org/read-research/books/acsms-health-related-physical-fitness-assessment-manual (accessed on 20 August 2021).
- ISO. ISO 8996: 2004 Ergonomics of the Thermal Environment—Determination of Metabolic Rate. 2004. Available online: https://www.iso.org/standard/34251.html (accessed on 5 August 2021).
- Holmér, I.; Gavhed, D. Classification of metabolic and respiratory demands in fire fighting activity with extreme workloads. Appl. Ergon. 2007, 38, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Falcone, T.; Cordella, F.; Molinaro, V.; Zollo, L.; Del Ferraro, S. Real-time human core temperature estimation methods and their application in the occupational field: A systematic review. Measurement 2021, 183, 109776. [Google Scholar] [CrossRef]

| Database | Adapted Query and Database Filters |
|---|---|
| Scopus | ((TITLE-ABS-KEY(“physiolog* monitor*”) OR TITLE-ABS-KEY(“noninvasive monitor*”) OR TITLE-ABS-KEY(“medical monitor*”) OR TITLE-ABS-KEY (“wearable sens*”)) AND (TITLE(assessment) OR TITLE-ABS-KEY(occupational) OR TITLE(model) OR TITLE-ABS-KEY(fatigue) OR TITLE(algorithm) OR TITLE-ABS-KEY(worker) OR TITLE-ABS-KEY(training) OR TITLE-ABS-KEY(“physical exertion”))) 2014–2022/Article, Article in Press/Journals/English |
| PubMed | ((“physiological monitoring”[All Fields]) OR (“noninvasive monitoring”[All Fields]) OR (“wearable sensor”[All Fields]) OR (“medical monitoring”[All Fields])) AND ((assessment[Title]) OR (occupational[All Fields]) OR (model[Title]) OR (“fatigue”[All Fields]) OR (algorithm[Title]) OR (worker[All Fields]) OR (“training”[All Fields]) OR (“training”[All Fields]) OR (“physical exertion”[All Fields])) 2014–2021/Journal Article/English/Humans |
| Science Direct | (“physiological monitoring” OR “noninvasive monitoring” OR “wearable sensors”) AND (TITLE(assessment) OR occupational OR TITLE(model) OR fatigue OR TITLE(algorithm) OR worker) 2014–2022/Research articles/Subscribed journals |
| Web of Science | (TS = (“physiolog* monitor*”) OR TS = (“noninvasive monitor*”) OR TS = (“wearable sens*”) OR TS = (“medical monitor*”)) AND (TI = (assessment) OR TS = (occupational) OR TI = (model) OR TS = (fatigue) OR TI = (algorithm) OR TS = (worker) OR TS = (training) OR TS = (“physical exertion”)) 2014–2022/Article/English |
| Academic Search Complete | (AB “physiolog* monitor*” OR AB “noninvasive monitor*” OR AB “wearable sens*” OR AB “medical monitor*”) AND (TI assessment OR AB occupational OR TI model OR AB fatigue OR TI algorithm OR AB worker OR AB training OR AB “physical exertion”) 2014–2021/Academic journals/English |
| Research Objective | Occupational Groups | Physiological Variables | Secondary Variables | References | |||
|---|---|---|---|---|---|---|---|
| Continuously Measured (Main Variables) | Uncontinuously Measured | Biochemical | Subjective and Cognitive | Environmental | |||
| Cardiovascular activity | Construction workers | HR | N/A | N/A | N/A | N/A | [49] |
| Firefighters | HR, HRV, ECG | N/A | N/A | N/A | N/A | [41,64] | |
| Retail store employees | HR, HRV | N/A | N/A | N/A | N/A | [55] | |
| Fatigue | Operators from drillship | HR, accelerometer counts | N/A | N/A | Fatigue subjective scales | N/A | [57] |
| Professional long-distance bus drivers | EEG, EMG, respiration signals | N/A | N/A | Self-reported fatigue states | N/A | [47] | |
| Nurses | From accelerometry counts: sleep duration, number of awakenings and sleep latency at night; number and distribution of steps taken during the work shift | N/A | N/A | Fatigue levels using the Brief Fatigue Inventory | N/A | [74] | |
| Heat stress | Bakers | HR | Tympanic body temperature | N/A | N/A | Natural wet temperature Tnw and globe temperature Tg | [40] |
| Construction workers | HR, energy expenditure, oxygen consumption, physical work activity, fluid intake | Resting blood pressure | Pre- and post-shift urine specific gravity (USG) | RPE | Dry-bulb temperature, wet bulb temperature, globe temperature, Indoor and outdoor heat exposures (WBGT) | [66,67,70] | |
| Custodial staff | HR, physical activity patterns from accelerometer counts | N/A | N/A | N/A | Ambient temperature and humidity | [59] | |
| Farmworkers | BR, HR, skin temperature, core body temperature (estimated from skin temperature), kilocalories burned per hour | Baseline blood pressure | Serum glucose and serum osmolarity | Heat-related illness symptoms | WBGT | [45] | |
| Grounds management workers | HR, activity patterns | N/A | N/A | N/A | Individually experienced temperature | [61] | |
| Law enforcement personnel | HR, core temperature (estimated), physiological strain index | N/A | N/A | Self-reported thermal discomfort | N/A | [63] | |
| Mine rescue workers | HR, BR, energy expenditure, oxygen consumption, core temperature and skin temperature | N/A | N/A | N/A | Mining environmental conditions | [51] | |
| Rebar workers | HR, energy expenditure, BR, METs, minute ventilation, oxygen consumption, and respiratory exchange ratio | Ear temperature | N/A | RPE | N/A | [68] | |
| Physiological demands and workload | Construction workers | ECG (smart clothing), HR, electrodermal activity, photoplethysmogram (PPG), skin temperature, 3-axis acceleration, oxygen consumption | N/A | N/A | N/A | Air temperature, relative humidity, WBGT | [48,71,76] |
| Firefighters | HR, air consumption, core temperature, activity-based accelerometry counts, maximum oxygen uptake, ECG, speed and elevation gain | N/A | Complete blood count and differential cell count; electrolyte, muscle and liver enzymes; blood glucose, creatinine, partial thromboplastin and urine osmolarity | Body part discomfort, self-perceived conditions, RPE, perception of respiratory distress, thermal Sensation Scale, overall wellbeing (feeling scale) | N/A | [46,65,72,73,77] | |
| Grounds maintenance crew workers | HR | N/A | N/A | N/A | Ambient temperature, ultraviolet exposure | [58] | |
| Recruits from Marine training course | HR, activity-based accelerometry counts, and skin temperature measurements | N/A | N/A | Vigilance and memory evaluations | N/A | [42] | |
| Roofers | HR, HRV, activity through accelerometry data, energy expenditure, metabolic equivalents (METs), sleep quality | N/A | N/A | Self-reported productivity loss | N/A | [53] | |
| Physiological responses and Stress levels | Construction workers | cardiac reactivity (HR, IBI, HRV, HRR), electrodermal level and response (from skin temperature) | N/A | Cortisol levels in saliva | N/A | N/A | [50] |
| Firefighters | HR, activity based on tri-axial acceleration counts, skin temperature, BR | N/A | N/A | Self-assessed stress | N/A | [69] | |
| Office workers | Cardiac reactivity, physical activity, sleep quality | N/A | N/A | Perceived stress | Relative humidity | [54,60] | |
| Police officers | HR, HRV, BR | N/A | N/A | Self-reported stress | N/A | [56] | |
| Physical activity patterns assessment | Nurses | Activity, posture and sleep patterns from acceleration counts, circadian rhythm parameters and sleep quantity; angular displacement waveforms of upper arm elevation and trunk flexion/extension; HR | N/A | N/A | Emotional and physical wellbeing; behavioural variables (sleep quality, affect, anxiety, life satisfaction, personality) | N/A | [44,52,62,75] |
| Office workers | Activity based on accelerometer counts | N/A | N/A | N/A | N/A | [43] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bustos, D.; Guedes, J.C.; Baptista, J.S.; Vaz, M.P.; Costa, J.T.; Fernandes, R.J. Applicability of Physiological Monitoring Systems within Occupational Groups: A Systematic Review. Sensors 2021, 21, 7249. https://doi.org/10.3390/s21217249
Bustos D, Guedes JC, Baptista JS, Vaz MP, Costa JT, Fernandes RJ. Applicability of Physiological Monitoring Systems within Occupational Groups: A Systematic Review. Sensors. 2021; 21(21):7249. https://doi.org/10.3390/s21217249
Chicago/Turabian StyleBustos, Denisse, Joana C. Guedes, João Santos Baptista, Mário P. Vaz, José Torres Costa, and Ricardo J. Fernandes. 2021. "Applicability of Physiological Monitoring Systems within Occupational Groups: A Systematic Review" Sensors 21, no. 21: 7249. https://doi.org/10.3390/s21217249
APA StyleBustos, D., Guedes, J. C., Baptista, J. S., Vaz, M. P., Costa, J. T., & Fernandes, R. J. (2021). Applicability of Physiological Monitoring Systems within Occupational Groups: A Systematic Review. Sensors, 21(21), 7249. https://doi.org/10.3390/s21217249