Combined Use of EMG and EEG Techniques for Neuromotor Assessment in Rehabilitative Applications: A Systematic Review
Abstract
:1. Introduction
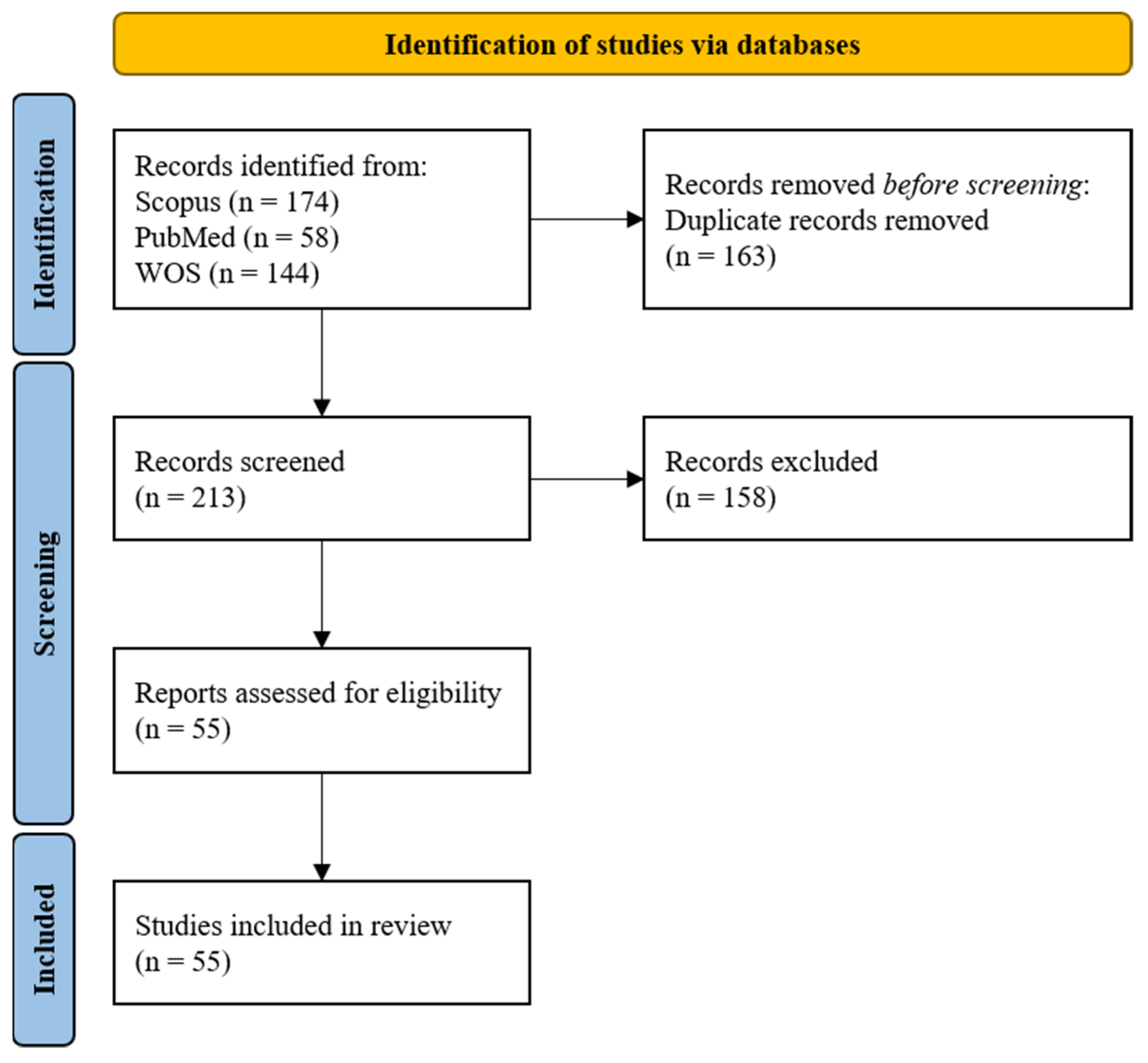
2. Materials and Methods
2.1. Criteria for Papers Classification
2.2. Bibliographic Research Criteria
2.3. Eligibility Criteria
- (A)
- To include the specified query in the abstract and/or title and/or in the keywords
- (B)
- To involve the simultaneous use of EMG and EEG
- (C)
- EMG and EEG had to be used for neuromotor assessment
- (D)
- To target rehabilitation scenarios
- (E)
- To be indexed in at least one of the screened databases
- (F)
- To be a full article (at least 4 pages)
- (G)
- To be available in English
3. Results
3.1. Selected Papers
3.2. Type of Study
3.3. Subjects and Anatomical Targets
3.3.1. Cohorts of Subjects
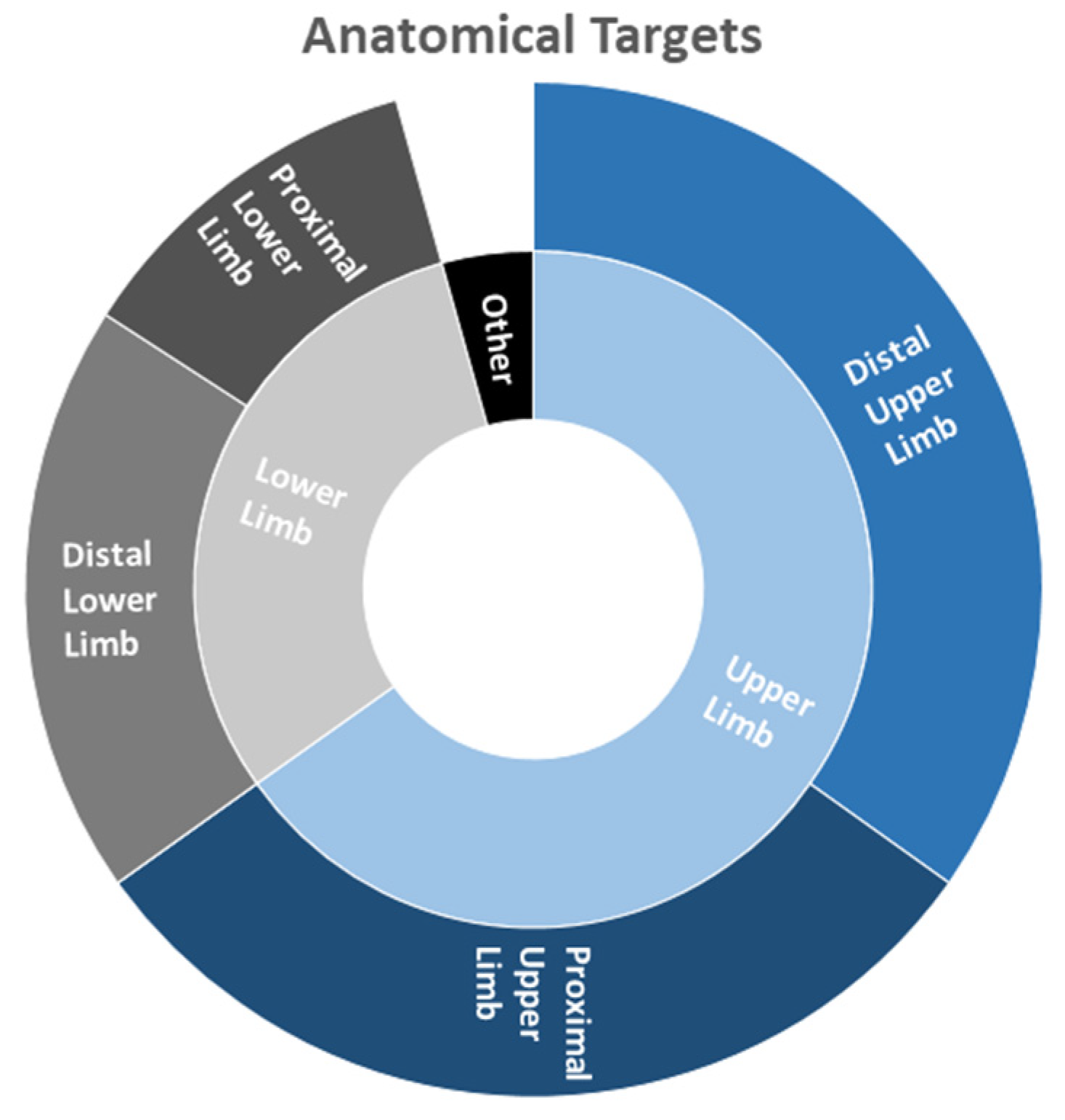
3.3.2. Anatomical Targets
3.4. Experimental Setups and Protocols
3.5. Setups for Signal Acquisition
3.6. Data Analysis
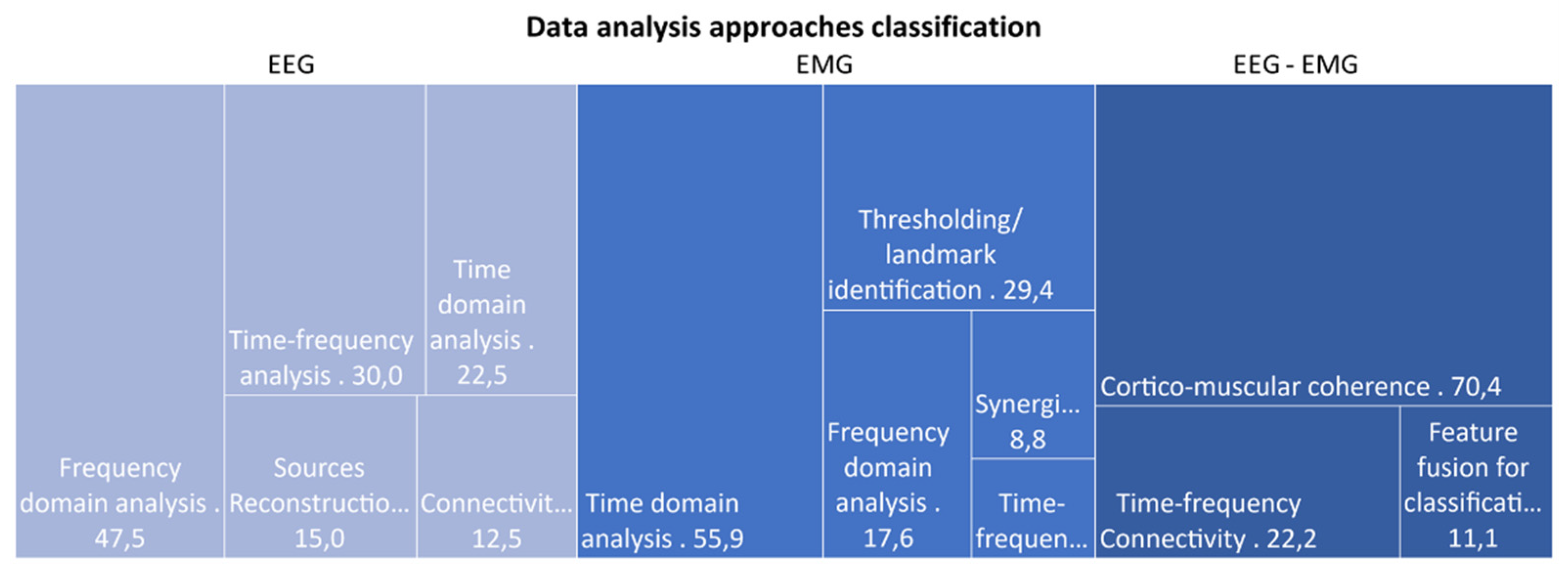
3.6.1. Analysis Techniques
3.6.2. Benefits of Combined EEG-EMG Applications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deuschl, G.; Beghi, E.; Fazekas, F.; Varga, T.; Christoforidi, K.A.; Sipido, E.; Bassetti, C.L.; Vos, T.; Feigin, V.L. The burden of neurological diseases in Europe: An analysis for the Global Burden of Disease Study 2017. Lancet Public Health 2020, 5, e551–e567. [Google Scholar] [CrossRef]
- Jones, T.A. Motor compensation and its effects on neural reorganization after stroke. Nat. Rev. Neurosci. 2017, 18, 267–280. [Google Scholar] [CrossRef]
- Maggioni, S.; Melendez-Calderon, A.; Van Asseldonk, E.; Klamroth-Marganska, V.; Lünenburger, L.; Riener, R.; Van Der Kooij, H. Robot-aided assessment of lower extremity functions: A review. J. Neuroeng. Rehabil. 2016, 13, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Debener, S.; Minow, F.; Emkes, R.; Gandras, K.; de Vos, M. How about taking a low-cost, small, and wireless EEG for a walk? Psychophysiology 2012, 49, 1617–1621. [Google Scholar] [CrossRef]
- Drost, G.; Stegeman, D.F.; van Engelen, B.G.M.; Zwarts, M.J. Clinical applications of high-density surface EMG: A systematic review. J. Electromyogr. Kinesiol. 2006, 16, 586–602. [Google Scholar] [CrossRef]
- Seeber, M.; Cantonas, L.M.; Hoevels, M.; Sesia, T.; Visser-Vandewalle, V.; Michel, C.M. Subcortical electrophysiological activity is detectable with high-density EEG source imaging. Nat. Commun. 2019, 10, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Pfurtscheller, G.; Aranibar, A. Evaluation of event-related desynchronization (ERD) preceding and following voluntary self-paced movement. Electroencephalogr. Clin. Neurophysiol. 1979, 46, 138–146. [Google Scholar] [CrossRef]
- Park, W.; Kwon, G.H.; Kim, Y.H.; Lee, J.H.; Kim, L. EEG response varies with lesion location in patients with chronic stroke. J. Neuroeng. Rehabil. 2016, 13, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Q.; Meng, L.; Pang, J.; Zhu, X.; Ming, D. Characterization of EEG data revealing relationships with cognitive and motor symptoms in Parkinson’s disease: A systematic review. Front. Aging Neurosci. 2020, 12, 373. [Google Scholar] [CrossRef]
- Pfurtscheller, G.; Lopes Da Silva, F.H. Event-related EEG/MEG synchronization and desynchronization: Basic principles. Clin. Neurophysiol. 1999, 110, 1842–1857. [Google Scholar] [CrossRef]
- Sakkalis, V. Review of advanced techniques for the estimation of brain connectivity measured with EEG/MEG. Comput. Biol. Med. 2011, 41, 1110–1117. [Google Scholar] [CrossRef] [PubMed]
- Xu, B.; Peng, S.; Song, A.; Yang, R.; Pan, L. Robot-aided upper-limb rehabilitation based on motor imagery EEG. Int. J. Adv. Robot. Syst. 2011, 8, 88–97. [Google Scholar] [CrossRef]
- Yu, G.; Wang, J.; Chen, W.; Zhang, J. EEG-based brain-controlled lower extremity exoskeleton rehabilitation robot. In Proceedings of the International Conference on Cybernetics and Intelligent Systems (CIS) and IEEE Conference on Robotics, Automation and Mechatronics (RAM), Ningbo, China, 19–21 November 2017; pp. 763–767. [Google Scholar]
- Kanna, S.; Heng, J. Quantitative EEG parameters for monitoring and biofeedback during rehabilitation after stroke. In Proceedings of the International Conference on Advanced Intelligent Mechatronic, Singapore, 14–17 July 2009; pp. 1689–1694. [Google Scholar]
- Bartur, G.; Joubran, K.; Peleg-Shani, S.; Vatine, J.J.; Shahaf, G. An EEG Tool for Monitoring Patient Engagement during Stroke Rehabilitation: A Feasibility Study. Biomed. Res. Int. 2017, 2017, 9071568. [Google Scholar] [CrossRef] [Green Version]
- Rogers, J.M.; Jensen, J.; Valderrama, J.T.; Johnstone, S.J.; Wilson, P.H. Single-channel EEG measurement of engagement in virtual rehabilitation: A validation study. Virtual Real. 2021, 25, 357–366. [Google Scholar] [CrossRef]
- Campanini, I.; Disselhorst-Klug, C.; Rymer, W.Z.; Merletti, R. Surface EMG in Clinical Assessment and Neurorehabilitation: Barriers Limiting Its Use. Front. Neurol. 2020, 11, 934. [Google Scholar] [CrossRef]
- Lucas, K.R.; Rich, P.A.; Polus, B.I. Muscle activation patterns in the scapular positioning muscles during loaded scapular plane elevation: The effects of Latent Myofascial Trigger Points. Clin. Biomech. 2010, 25, 765–770. [Google Scholar] [CrossRef]
- Ivanenko, Y.P.; Poppele, R.E.; Lacquaniti, F. Five basic muscle activation patterns account for muscle activity during human locomotion. J. Physiol. 2004, 556, 267–282. [Google Scholar] [CrossRef]
- Kim, D.Y.; Park, C.I.; Chon, J.S.; Ohn, S.H.; Park, T.H.; Bang, I.K. Biomechanical assessment with electromyography of post-stroke ankle plantar flexor spasticity. Yonsei Med. J. 2005, 46, 546–554. [Google Scholar] [CrossRef]
- McDonald, A.C.; Mulla, D.M.; Keir, P.J. Using EMG Amplitude and Frequency to Calculate a Multimuscle Fatigue Score and Evaluate Global Shoulder Fatigue. Hum. Factors 2019, 61, 526–536. [Google Scholar] [CrossRef]
- Lee, W.A. Neuromotor synergies as a basis for coordinated intentional action. J. Mot. Behav. 1984, 16, 135–170. [Google Scholar] [CrossRef]
- Cheung, V.C.K.; D’Avella, A.; Bizzi, E. Adjustments of motor pattern for load compensation via modulated activations of muscle synergies during natural behaviors. J. Neurophysiol. 2009, 101, 1235–1257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowden, M.G.; Clark, D.J.; Kautz, S.A. Evaluation of abnormal synergy patterns poststroke: Relationship of the fugl-meyer assessment to hemiparetic locomotion. Neurorehabil. Neural Repair 2010, 24, 328–337. [Google Scholar] [CrossRef]
- Cheung, V.C.K.; Turolla, A.; Agostini, M.; Silvoni, S.; Bennis, C.; Kasi, P.; Paganoni, S.; Bonato, P.; Bizzi, E. Muscle synergy patterns as physiological markers of motor cortical damage. Proc. Natl. Acad. Sci. USA 2012, 109, 14652–14656. [Google Scholar] [CrossRef] [Green Version]
- Kiguchi, K.; Hayashi, Y. An EMG-based control for an upper-limb power-assist exoskeleton robot. IEEE Trans. Syst. Man Cybern. Part. B Cybern. 2012, 42, 1064–1071. [Google Scholar] [CrossRef]
- Castellini, C.; Van Der Smagt, P. Surface EMG in advanced hand prosthetics. Biol. Cybern. 2009, 100, 35–47. [Google Scholar] [CrossRef] [Green Version]
- Iandolo, R.; Marini, F.; Semprini, M.; Laffranchi, M.; Mugnosso, M.; Cherif, A.; De Michieli, L.; Chiappalone, M.; Zenzeri, J. Perspectives and challenges in robotic neurorehabilitation. Appl. Sci. 2019, 9, 3183. [Google Scholar] [CrossRef] [Green Version]
- Trujillo, P.; Mastropietro, A.; Scano, A.; Chiavenna, A.; Mrakic-Sposta, S.; Caimmi, M.; Molteni, F.; Rizzo, G. Quantitative EEG for predicting upper limb motor recovery in chronic stroke robot-Assisted rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 27, 1058–1067. [Google Scholar] [CrossRef]
- Curt, A.; Dietz, V. Electrophysiological recordings in patients with spinal cord injury: Significance for predicting outcome. Spinal Cord 1999, 37, 157–165. [Google Scholar] [CrossRef]
- Stinear, C.M.; Byblow, W.D.; Ackerley, S.J.; Barber, P.A.; Smith, M.C. Predicting Recovery Potential for Individual Stroke Patients Increases Rehabilitation Efficiency. Stroke 2017, 48, 1011–1019. [Google Scholar] [CrossRef] [PubMed]
- Belfatto, A.; Scano, A.; Chiavenna, A.; Mastropietro, A.; Mrakic-Sposta, S.; Pittaccio, S.; Tosatti, L.M.; Molteni, F.; Rizzo, G. A multiparameter approach to evaluate post-stroke patients: An application on robotic rehabilitation. Appl. Sci. 2018, 8, 2248. [Google Scholar] [CrossRef] [Green Version]
- Pierella, C.; Pirondini, E.; Kinany, N.; Coscia, M.; Giang, C.; Miehlbradt, J.; Magnin, C.; Nicolo, P.; Dalise, S.; Sgherri, G.; et al. A multimodal approach to capture post-stroke temporal dynamics of recovery. J. Neural Eng. 2020, 17, 045002. [Google Scholar] [CrossRef] [PubMed]
- Bulea, T.C.; Lerner, Z.F.; Gravunder, A.J.; Damiano, D.L. Exergaming with a pediatric exoskeleton: Facilitating rehabilitation and research in children with cerebral palsy. In Proceedings of the International Conference on Rehabilitation Robotics, London, UK, 17–20 July 2017; pp. 1087–1093. [Google Scholar]
- Craik, A.; Kilicarslan, A.; Contreras-Vidal, J.L. A translational roadmap for a brain-machine-interface (BMI) system for rehabilitation. In Proceedings of the International Conference on Systems, Man and Cybernetics (SMC), Bari, Italy, 6–9 October 2019; pp. 3613–3618. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, 332–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mima, T.; Toma, K.; Koshy, B.; Hallett, M. Coherence between cortical and muscular activities after subcortical stroke. Stroke 2001, 32, 2597–2601. [Google Scholar] [CrossRef] [PubMed]
- Cremoux, S.; Tallet, J.; Dal Maso, F.; Berton, E.; Amarantini, D. Impaired corticomuscular coherence during isometric elbow flexion contractions in humans with cervical spinal cord injury. Eur. J. Neurosci. 2017, 46, 1991–2000. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Qian, Q.; Wong, K.; Zhu, H.; Huang, Y.; Hu, X.; Zheng, Y. Altered Corticomuscular Coherence (CMCoh) Pattern in the Upper Limb During Finger Movements After Stroke. Front. Neurol. 2020, 11, 410. [Google Scholar] [CrossRef] [PubMed]
- She, Q.; Zheng, H.; Tan, T.; Zhang, B.; Fan, Y.; Luo, Z. Time-Frequency-Domain Copula-Based Granger Causality and Application to Corticomuscular Coupling in Stroke. Int. J. Humanoid Robot. 2019, 16, 1–18. [Google Scholar] [CrossRef]
- Sui, J.; Liu, Y.; Ji, L. Effect of unilateral non-rhythmical stimulation on bilateral cerebral cortex and muscle activation in People. J. Biomim. Biomater. Tissue Eng. 2014, 19, 25–33. [Google Scholar] [CrossRef]
- Bao, S.C.; Leung, W.C.; Vincent, V.C.; Zhou, P.; Tong, K.Y. Pathway-specific modulatory effects of neuromuscular electrical stimulation during pedaling in chronic stroke survivors. J. Neuroeng. Rehabil. 2019, 16, 1–15. [Google Scholar] [CrossRef]
- Lai, M.I.; Pan, L.L.; Tsai, M.W.; Shih, Y.F.; Wei, S.H.; Chou, L.W. Investigating the effects of peripheral electrical stimulation on corticomuscular functional connectivity stroke survivors. Top. Stroke Rehabil. 2016, 23, 154–162. [Google Scholar] [CrossRef]
- Xu, R.; Wang, Y.; Wang, K.; Zhang, S.; He, C.; Ming, D. Increased corticomuscular coherence and brain activation immediately after short-term neuromuscular electrical stimulation. Front. Neurol. 2018, 9, 1–10. [Google Scholar] [CrossRef]
- Zhai, T.; Fu, A.; Xu, R.; Qiu, S.; Qi, H.; Zhou, P.; Zhang, L.; Wan, B.; Ming, D. Cortico-muscular coherence analysis under voluntary, stimulated and imaginary neuromuscular activities. Biomed. Tech. 2013, 58, 3–4. [Google Scholar] [CrossRef] [PubMed]
- Zhai, T.; Qi, C.; Xu, R.; Fu, A.; Zhang, L.; Zhao, X.; Zhou, P.; Qi, H.; Wan, B.; Cheng, X.; et al. EEG-EMG Analysis on Corticomuscular Coherence of Middle Finger Flexion Tasks. In Advances in Cognitive Neurodynamics (IV); Springer: Dordrecht, The Netherlands, 2015; pp. 337–344. ISBN 9789401795487. [Google Scholar]
- Li, J.; Dimitrakopoulos, G.N.; Thangavel, P.; Chen, G.; Sun, Y.; Guo, Z.; Yu, H.; Thakor, N.; Bezerianos, A. What Are Spectral and Spatial Distributions of EEG-EMG Correlations in Overground Walking? An Exploratory Study. IEEE Access 2019, 7, 143935–143946. [Google Scholar] [CrossRef]
- Li, J.; Thakor, N.; Bezerianos, A. Brain Functional Connectivity in Unconstrained Walking with and without an Exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Youssofzadeh, V.; Zanotto, D.; Wong-Lin, K.F.; Agrawal, S.K.; Prasad, G. Directed functional connectivity in Fronto-Centroparietal circuit correlates with motor adaptation in gait training. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 1265–1275. [Google Scholar] [CrossRef] [PubMed]
- Bartur, G.; Pratt, H.; Frenkel-Toledo, S.; Soroker, N. Neurophysiological effects of mirror visual feedback in stroke patients with unilateral hemispheric damage. Brain Res. 2018, 1700, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Jensen, P.; Jensen, N.J.; Terkildsen, C.U.; Choi, J.T.; Nielsen, J.B.; Geertsen, S.S. Increased central common drive to ankle plantar flexor and dorsiflexor muscles during visually guided gait. Physiol. Rep. 2018, 6, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Park, J.H.; Moon, H.S.; Kim, H.; Chung, S.T. Detection of movement intention for operating methods of serious games. Appl. Sci. 2021, 11, 883. [Google Scholar] [CrossRef]
- Úbeda, A.; Azorín, J.M.; Farina, D.; Sartori, M. Estimation of neuromuscular primitives from EEG slow cortical potentials in incomplete spinal cord injury individuals for a new class of brain-machine interfaces. Front. Comput. Neurosci. 2018, 12, 3. [Google Scholar] [CrossRef] [Green Version]
- Palmer, J.A.; Wheaton, L.A.; Gray, W.A.; Saltão da Silva, M.A.; Wolf, S.L.; Borich, M.R. Role of Interhemispheric Cortical Interactions in Poststroke Motor Function. Neurorehabil. Neural Repair 2019, 33, 762–774. [Google Scholar] [CrossRef]
- Vladimirov, A.A.; Andriyashek, Y.I. Neurophysiological markers of stress within a recovery period after acute complications of cardiovascular diseases. Neurophysiology 2014, 46, 225–232. [Google Scholar] [CrossRef]
- Yilmaz, O.; Birbaumer, N.; Ramos-Murguialday, A. Movement related slow cortical potentials in severely paralyzed chronic stroke patients. Front. Hum. Neurosci. 2015, 8. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.V.; Henry, S.M.; Nagle, K.J. Low back pain associates with altered activity of the cerebral cortex prior to arm movements that require postural adjustment. Clin. Neurophysiol. 2010, 121, 431–440. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, A.; Yao, J.; Dewald, J.P.A. A novel experimental setup combining EEG and robotics to investigate brain activity driving controlled reaching movements in chronic stroke survivors. In Proceedings of the 10th International Conference on Rehabilitation Robotics, Noordwijk, The Netherlands, 13–15 June 2007; pp. 876–882. [Google Scholar]
- Major, Z.Z.; Vaida, C.; Major, K.A.; Tucan, P.; Simori, G.; Banica, A.; Brusturean, E.; Burz, A.; Craciunas, R.; Ulinici, I.; et al. The impact of robotic rehabilitation on the motor system in neurological diseases. A multimodal neurophysiological approach. Int. J. Environ. Res. Public Health 2020, 17, 6557. [Google Scholar] [CrossRef] [PubMed]
- Park, T.; Lee, M.; Jeong, T.; Shin, Y.I.; Park, S.M. Quantitative analysis of eeg power spectrum and emg median power frequency changes after continuous passive motion mirror therapy system. Sensors 2020, 20, 2354. [Google Scholar] [CrossRef] [Green Version]
- Chwodhury, A.; Raza, H.; Dutta, A.; Nishad, S.S.; Saxena, A.; Prasad, G. A study on cortico-muscular coupling in finger motions for exoskeleton assisted neuro-rehabilitation. In Proceedings of the Annual International Conference of the Engineering in Medicine and Biology Society, Milano, Italy, 25–29 August 2015; pp. 4610–4614. [Google Scholar]
- Gandolla, M.; Ferrante, S.; Coelli, S.; Tacchino, G.; Giglioli, I.A.C.; Cottini, M.C.; Seneci, C.; Scannapieco, A.; Veniero, M.; Pedrocchi, A. Technical validation of an integrated robotic hand rehabilitation device: Finger independent movement, EMG control, and EEG-based biofeedback. In Proceedings of the 2nd International Forum on Research and Technologies for Society and Industry Leveraging a better tomorrow (RTSI), Bologna, Italy, 7–9 September 2016; pp. 5–9. [Google Scholar]
- Donati, A.R.C.; Shokur, S.; Morya, E.; Campos, D.S.F.; Moioli, R.C.; Gitti, C.M.; Augusto, P.B.; Tripodi, S.; Pires, C.G.; Pereira, G.A.; et al. Long-Term Training with a Brain-Machine Interface-Based Gait Protocol Induces Partial Neurological Recovery in Paraplegic Patients. Sci. Rep. 2016, 6, 1–16. [Google Scholar] [CrossRef] [Green Version]
- Hashimoto, Y.; Ota, T.; Mukaino, M.; Liu, M.; Ushiba, J. Functional recovery from chronic writer’s cramp by brain-computer interface rehabilitation: A case report. BMC Neurosci. 2014, 15, 1–7. [Google Scholar] [CrossRef] [Green Version]
- Leerskov, K.; Rehman, M.; Niazi, I.; Cremoux, S.; Jochumsen, M. Investigating the feasibility of combining EEG and EMG for controlling a hybrid human computer interface in patients with spinal cord injury. In Proceedings of the 20th International Conference on Bioinformatics and Bioengineering, Cincinnati, OH, USA, 26–28 October 2020; pp. 403–410. [Google Scholar]
- Kim, B.; Kim, L.; Kim, Y.H.; Yoo, S.K. Cross-association analysis of EEG and EMG signals according to movement intention state. Cogn. Syst. Res. 2017, 44, 1–9. [Google Scholar] [CrossRef]
- Lou, X.; Xiao, S.; Qi, Y.; Hu, X.; Wang, Y.; Zheng, X. Corticomuscular coherence analysis on hand movement distinction for active rehabilitation. Comput. Math. Methods Med. 2013, 2013, 908591. [Google Scholar] [CrossRef] [Green Version]
- Yang, H.; Guan, C.; Chua, K.S.G.; Chok, S.S.; Wang, C.C.; Soon, P.K.; Tang, C.K.Y.; Ang, K.K. Detection of motor imagery of swallow EEG signals based on the dual-tree complex wavelet transform and adaptive model selection. J. Neural Eng. 2014, 11, 035016. [Google Scholar] [CrossRef]
- Krauth, R.; Schwertner, J.; Vogt, S.; Lindquist, S.; Sailer, M.; Sickert, A.; Lamprecht, J.; Perdikis, S.; Corbet, T.; Del Millán, J.R.; et al. Cortico-muscular coherence is reduced acutely post-stroke and increases bilaterally during motor recovery: A pilot study. Front. Neurol. 2019, 10, 126. [Google Scholar] [CrossRef] [Green Version]
- Yao, J.; Dewald, J.P.A. Cortico-muscular communication during the generation of static shoulder abduction torque in upper limb following stroke. In Proceedings of the Annual International Conference of the Engineering in Medicine and Biology, New York, NY, USA, 30 August–3 September 2006; pp. 181–184. [Google Scholar]
- Yao, J.; Ellis, M.D.; Dewald, J. Mechanisms and rehabilitation of discoordination following stroke using a cortical imaging method. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology, Shanghai, China, 1–4 September 2005; Volume 7, pp. 4138–4141. [Google Scholar]
- Dutta, A.; Boulenouar, R.S.; Guiraud, D.; Nitsche, M.A. Delineating the effects of anodal transcranial direct current stimulation on myoelectric control based on slow cortical potentials. In Proceedings of the 36th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 27–31 August 2014; pp. 3094–3097. [Google Scholar]
- Li, C.; Jia, T.; Ji, L. Investigation of the Effects of Game Difficulty on the Engagement Level of Patient with Brain Injury During Rehabilitation Exercise; International Society for Optics and Photonics: Bellingham, DC, USA, 2019; p. 35. [Google Scholar]
- Qidwai, U.; Ajimsha, M.S.; Shakir, M. The role of EEG and EMG combined virtual reality gaming system in facial palsy rehabilitation—A case report. J. Bodyw. Mov. Ther. 2019, 23, 425–431. [Google Scholar] [CrossRef]
- Bao, S.C.; Wong, W.W.; Leung, T.W.H.; Tong, K.Y. Cortico-muscular coherence modulated by high-definition transcranial direct current stimulation in people with chronic stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Benninger, D.H.; Iseki, K.; Kranick, S.; Luckenbaugh, D.A.; Houdayer, E.; Hallett, M. Controlled study of 50-Hz repetitive transcranial magnetic stimulation for the treatment of parkinson disease. Neurorehabil. Neural Repair 2012, 26, 1096–1105. [Google Scholar] [CrossRef]
- Olsen, S.; Signal, N.; Niazi, I.K.; Rashid, U.; Alder, G.; Mawston, G.; Nedergaard, R.B.; Jochumsen, M.; Taylor, D. Peripheral electrical stimulation paired with movement-related cortical potentials improves isometric muscle strength and voluntary activation following stroke. Front. Hum. Neurosci. 2020, 14, 156. [Google Scholar] [CrossRef]
- Pan, L.L.H.; Yang, W.W.; Kao, C.L.; Tsai, M.W.; Wei, S.H.; Fregni, F.; Chen, V.C.F.; Chou, L.W. Effects of 8-week sensory electrical stimulation combined with motor training on EEG-EMG coherence and motor function in individuals with stroke. Sci. Rep. 2018, 8, 9217. [Google Scholar] [CrossRef]
- Shendkar, C.V.; Lenka, P.K.; Biswas, A.; Kumar, R.; Mahadevappa, M. Therapeutic effects of functional electrical stimulation on gait, motor recovery, and motor cortex in stroke survivors. Hong Kong Physiother. J. 2015, 33, 10–20. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Russo, M.; Bramanti, P.; Carioti, L.; Balletta, T.; Buda, A.; Manuli, A.; Filoni, S.; Bramanti, A. Shaping neuroplasticity by using powered exoskeletons in patients with stroke: A randomized clinical trial. J. Neuroeng. Rehabil. 2018, 15, 35. [Google Scholar] [CrossRef]
- Chen, I.H.; Yang, Y.R.; Lu, C.F.; Wang, R.Y. Novel gait training alters functional brain connectivity during walking in chronic stroke patients: A randomized controlled pilot trial 11 Medical and Health Sciences 1109 Neurosciences 11 Medical and Health Sciences 1103 Clinical Sciences. J. Neuroeng. Rehabil. 2019, 16, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nikmaram, N.; Scholz, D.S.; Großbach, M.; Schmidt, S.B.; Spogis, J.; Belardinelli, P.; Müller-Dahlhaus, F.; Remy, J.; Ziemann, U.; Rollnik, J.D.; et al. Musical Sonification of Arm Movements in Stroke Rehabilitation Yields Limited Benefits. Front. Neurosci. 2019, 13, 1378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rayegani, S.; Raeissadat, S.; Sedighipour, L.; Rezazadeh, I.; Bahrami, M.; Eliaspour, D.; Khosrawi, S. Effect of neurofeedback and electromyographic-biofeedback therapy on improving hand function in stroke patients. Top. Stroke Rehabil. 2014, 21, 137–151. [Google Scholar] [CrossRef] [PubMed]
- Cisotto, G.; Guglielmi, A.V.; Badia, L.; Zanella, A. Joint Compression of EEG and EMG Signals for Wireless Biometrics. In Proceedings of the Global Communications Conference, GLOBECOM, Abu Dhabi, United Arab Emirates, 9–13 December 2018. [Google Scholar]
- Sridhar, S.; Manian, V. Eeg and deep learning based brain cognitive function classification. Computers 2020, 9, 104. [Google Scholar] [CrossRef]
- Suprijanto; Noor, A.S.; Risangtuni, A.G.; Susanti, H. Automatic segmentation scheme for effective synchronization of EMG-EEG quantification. Int. J. Biol. Biomed. Eng. 2020, 14, 136–143. [Google Scholar] [CrossRef]
- Tryon, J.; Friedman, E.; Trejos, A.L. Performance evaluation of EEG/EMG fusion methods for motion classification. In Proceedings of the International Conference on Rehabilitation Robotics, Toronto, ON, Canada, 24–28 June 2019; pp. 971–976. [Google Scholar]
- Tryon, J.; Trejos, A.L. Classification of task weight during dynamic motion using EEG-EMG fusion. IEEE Sens. J. 2021, 21, 5012–5021. [Google Scholar] [CrossRef]
- Roy, R.; Sikdar, D.; Mahadevappa, M.; Kumar, C.S. EEG based motor imagery study of time domain features for classification of power and precision hand grasps. In Proceedings of the International IEEE/EMBS Conference on Neural Engineering, Shanghai, China, 25–28 May 2017; pp. 440–443. [Google Scholar]
- Bizzi, E.; Cheung, V.C. The neural origin of muscle synergies. Front. Comput. Neurosci. 2013, 7, 51. [Google Scholar] [CrossRef] [Green Version]
- Lee, D.D.; Seung, H.S. Learning the parts of objects by non-negative matrix factorization. Nature 1999, 401, 788–791. [Google Scholar] [CrossRef]
- Horwitz, B. The elusive concept of brain connectivity. Neuroimage 2003, 19, 466–470. [Google Scholar] [CrossRef]
- Delorme, A.; Palmer, J.; Onton, J.; Oostenveld, R.; Makeig, S. Independent EEG Sources Are Dipolar. PLoS ONE 2012, 7, e30135. [Google Scholar] [CrossRef]
- Pascual-Marqui, R.D.; Michel, C.M.; Lehmann, D. Low resolution electromagnetic tomography: A new method for localizing electrical activity in the brain. Int. J. Psychophysiol. 1994, 18, 49–65. [Google Scholar] [CrossRef]
- Matsuya, R.; Ushiyama, J.; Ushiba, J. Inhibitory interneuron circuits at cortical and spinal levels are associated with individual differences in corticomuscular coherence during isometric voluntary contraction. Sci. Rep. 2017, 7, 44417. [Google Scholar] [CrossRef] [Green Version]
- Baccalá, L.A.; Sameshima, K. Partial directed coherence: A new concept in neural structure determination. Biol. Cybern. 2001, 84, 463–474. [Google Scholar] [CrossRef]
- Baccala, L.A.; Sameshima, K.; Takahashi, D.Y. Generalized partial directed coherence. In Proceedings of the 15th International Conference on Digital Signal Processing, Cardiff, UK, 1–4 July 2007; pp. 163–166. [Google Scholar] [CrossRef]
- Liu, J.; Sheng, Y.; Liu, H. Corticomuscular coherence and its applications: A review. Front. Hum. Neurosci. 2019, 13, 100. [Google Scholar] [CrossRef] [Green Version]
- Gao, Q.; Dou, L.; Belkacem, A.N.; Chen, C. Noninvasive Electroencephalogram Based Control of a Robotic Arm for Writing Task Using Hybrid BCI System. Biomed. Res. Int. 2017, 2017, 8316485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Leeb, R.; Sagha, H.; Chavarriaga, R.; Millán, J.D.R. Multimodal fusion of muscle and brain signals for a Hybrid-BCI. In Proceedings of the Annual International Conference of the Engineering in Medicine and Biology Society, Buenos Aires, Argentina, 31 August–4 September 2010; Volume 2010, pp. 4343–4346. [Google Scholar]
- Basteris, A.; Nijenhuis, S.M.; Stienen, A.H.; Buurke, J.H.; Prange, G.B.; Amirabdollahian, F. Training modalities in robot-mediated upper limb rehabilitation in stroke: A framework for classification based on a systematic review. J. Neuroeng. Rehabil. 2014, 11, 111. [Google Scholar] [CrossRef] [Green Version]
- Camona, C.; Wilkins, K.B.; Drogos, J.; Sullivan, J.E.; Dewald, J.P.A.; Yao, J. Improving Hand Function of Severely Impaired Chronic Hemiparetic Stroke Individuals Using Task-Specific Training With the ReIn-Hand System: A Case Series. Front. Neurol. 2018, 9, 923. [Google Scholar] [CrossRef] [Green Version]
- Nascimento, L.R.; Michaelsen, S.M.; Ada, L.; Polese, J.C.; Teixeira-Salmela, L.F. Cyclical electrical stimulation increases strength and improves activity after stroke: A systematic review. J. Physiother. 2014, 60, 22–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knutson, J.S.; Fu, M.J.; Sheffler, L.R.; Chae, J. Neuromuscular electrical stimulation for motor restoration in hemiplegia. Phys. Med. Rehabil. Clin. N. Am. 2015, 26, 729–745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitzgibbon, S.P.; Pope, K.J.; MacKenzie, L.; Clark, C.R.; Willoughby, J.O. Cognitive tasks augment gamma EEG power. Clin. Neurophysiol. 2004, 115, 1802–1809. [Google Scholar] [CrossRef]





| Type of Study | Aim |
|---|---|
| Observational study | Study of the cortico-muscular coupling (1) during motor tasks [37,38,39,40,41] and (2) with electrical stimulation [42,43,44,45,46] |
| Investigation of the effects of exoskeleton on functional connectivity [47,48,49] | |
| Investigation of the effects of visual feedback [50,51] | |
| Detection of movement intention [52,53] Study of the interhemispheric interaction with TMS [54] | |
| Study of a neurophysiological marker of stress [55] | |
| Study of slow cortical potentials in stroke [56] | |
| Study of correlation between lower back pain and altered postural stabilization [57] | |
| Pilot study | Test new rehabilitation paradigm [34,58,59,60,61,62] |
| Investigation of the efficacy of BMI [63] and EEG feedback [64] | |
| Study of movement classification combining EEG and EMG [65] | |
| Investigation of movement intention [66,67] and motor imagery detection [68] | |
| Study of the cortico-muscular coupling [69,70,71] | |
| Study of the neuroplasticity with electrical stimulation [72] | |
| Investigation of engagement in game rehabilitation [73] | |
| Study of the effects of the use of VR in facial rehabilitation [74] | |
| Randomized controlled trial | Study the effects of transcranial [75,76] and peripheral electrical stimulation [77,78,79] |
| Investigation of the efficacy of lower limb exoskeleton rehabilitation [80] | |
| Assessment of a novel gait training paradigm [81] | |
| Investigation of the efficacy of neurologic therapy based on music [82] | |
| Investigation of the effects of biofeedback [83] | |
| Methodological study | Presentation of a multivariate approach for motor assessment [32,33] Presentation of a method for compressing EEG-EMG signal [84] |
| Presentation of algorithms for motion detection [85,86] and motion classification [87,88] |
| Categories | Details and References | |
|---|---|---|
| Type of subjects | Healthy (Age range) | Target: 20–30 [61], n.a. [84], 24–36 [72], 60–62 [62], 18–35 [51], 57.8 ± 4.7 [66], 24 ± 2.32 [47,48], 23–27 [67], 26.86 ± 3.39 [52], 25.0 ± 1.7 [60], 22–28 [41], 22 [86], 22.8 ± 3.3 [87], 24.9 ± 5.4 [88], 21.2 ± 1.1 [44], 26.5 ± 6.5 [49], 23–27 [45,46] |
| Control group: 20–39 [42], 53–62 [58], 27 ± 4 [38], 50.08 ± 15.8 [39], 35.4 ± 5.25 [57], 24 ± 1.5 [43], 27 ± 4 [65], 53 ± 14 [54], 58 ± 16 [33], 24–27 [40], 20 ≥ 60 [85], 33.5 ± 7.9 [53], 55.1 ± 2.1 [55], 35.9 ± 7.7 [68], n.a. [69,70], 42 ± 13 [71] | ||
| Pathologic (Age range) | Chronic stroke: 53–72 [37], 37–72 [42], 35–63 [75], 61 ± 11 [32], 55–77 [80], 52–63 [58], 52.5 ± 9.7 [81], 56.5 ± 9.5 [39], 43–79 [43], 69.9 ± 10.5 [77], 46–81 [54], 56.5 ± 9.5 [78], 68 ± 18 [33], 52.7 ± 8.4 [74], 45–51 [40], 49.9 ± 10.9 [79], 56 [68], n.a. [70], 46–60 [71], 51.4 ± 11.1 [56]; Subacute stroke: 32–79 [50]; Subacute and chronic stroke: 52–64 [69], 42–92 [82] | |
| Parkinson disease: 40–80 [76]; Cerebral palsy: 5–19 [34]; Spinal cord injury: 32.5 ± 6.2 [38], 26–38 [63], 32 ± 6 [65], 43.5 ± 12.4 [53]; Writer’s cramp: 67 [64]; Low back pain: 39.2 ± 6.33 [57]; Mixed injuries and diseases: 33–54 [73], 60–80 [59]; Facial palsy: 23 [74]; MCI: n.a. [85]; Cardiovascular diseases: 56.3 ± 1.0 [55] | ||
| Nr of subjects | ≤10 | 6 [37], 5 [32], 6 [34], 3 + 4 [58], 6 [61], 1 [84], 8 [63], 10 [72], 2 [62], 1 [64], 7 [66], 5 [47], 8 [67], 7 [52], 10 [33], 1 [74], 5 + 5 [40], 10 [41], 1 [86], 4 + 4 [53], 4 + 4 [71], 6 [49], 10 [45,46] |
| 10 < n ≤ 20 | 11 [75], 14 [50], 9 + 9 [81], 10 + 8 [38], 10 + 10 [57], 16 [51], 7 + 4 [69], 10 + 8 [65], 15 [77], 12 [78], 6 + 6 [33], 18 [87], 13 [44], 10 + 1 [68], 7 + 7 [70], 20 [56] | |
| >20 | 16 + 12 [42], 26 [76], 20 + 20 [80], 14 + 10 [39], 15 + 15 [43], 30 [47,48], 23 [59], 12 + 30 [82], 19 + 14 [54], 30 [83], 14 + 14 [79], 28 + 7 [85], 32 [88], 14 + 14 [55] | |
| Rehabilitation target | Distal Upper Limb | Hand and wrist: [50,59,61,69,84]; Wrist: [37,40,44,75,82]; Hand: [39,43,45,46,51,54,56,62,64,67,73,76,78,83] |
| Proximal Upper Limb | Shoulder and elbow: [32,33,58,60,70,71,82,84]; Elbow: [37,38,39,40,62,65,76,87,88]; Arm: [52,85,86]; Shoulder: [55] | |
| Distal Lower Limb | Ankle: [42,47,48,49,51,63,80]; Leg: [41,72,77,79,81]; Foot: [81] | |
| Proximal Lower Limb | Knee: [34,42,47,48,49,80]; Hip and knee: [63] | |
| Other | Torso: [57]; Face: [74]; Neck: [68] | |
| Setup | Details and References |
|---|---|
| Miscellaneous techniques for free movements and rehabilitation | Mirror visual feedback [50] |
| Wrist movements [69,84]; wrist movements + visual feedback [73] | |
| Elbow movements [38]; elbow movements + visual feedback [65] | |
| Arm movements [37,57,70,71,87,88]; arm movements + auditory feedback [82]; arm movements + balance handle [52] | |
| Hand movements [40,67,83,86]; hand movements + motor imagery + auditory/smelling stimulus [85]; hand movements + audiovisual feedback [56]; hand movements + biofeedback [64] | |
| Leg movements [53] | |
| Motor imagery swallow and tongue protrusion [68] | |
| Respiratory movements [55] | |
| Oculus rift [74] | |
| Robotic assistance | Exoskeleton lower limb + virtual reality [34]; exoskeleton lower limb + virtual reality + BMI [63]; exoskeleton lower limb + walking [47,48,80]; exoskeleton lower limb + treadmill [49] |
| Robotic end effector upper limb [32,33,58,59] | |
| Robotic mirror therapy upper limb [60] | |
| Hand mobilizer exoskeleton [39,61,62]; hand mobilizer exoskeleton + motor imagery [66] | |
| Ankle mobilizer [41] | |
| Peripheral electrical stimulation | FES + hand movements [43,78]; FES + walking [79]; FES + hand movements + motor imagery [45,46] |
| ePAS + ankle movements [77] | |
| NMES + wrist movements [44] | |
| Transcranial electrical stimulation | HD-tDCs + wrist contractions [75]; anode tDCs + ankle dorsiflexion [72] |
| rTMS [76]; TMS + wrist contractions [54] | |
| Assisted rehabilitation | Pedaling system + NMES [42] |
| Treadmill [81]; Treadmill + visual feedback [51] |
| EEG ACQUISITION | ||
|---|---|---|
| Setup | Details and References | |
| Number of electrodes | N > 100 | 163 [70,71]; 160 [58]; 128 [42,59]; |
| 100 < N < 30 | 64 [32,33,34,38,44,50,65,66,75]; 62 [47,48]; 56 [37]; 40 [68,77]; 35 [67]; 32 [40,52,53,54,81,84]; | |
| 30 < N < 10 | 21 [39,80]; 20 [69,82]; 16 [43,49,56,63,78]; 15 [85]; 14 [62,73]; 10 [57,61,64]; | |
| N < 10 | 8 [83]; 5 [72]; 3 [60,86,87,88]; 2 [45,46]; 1 [41,51,55,79]; | |
| Electrodes positioning | Motor area only [41,61,67] | |
| Sensorimotor area [39,43,60,64,78] | ||
| Whole cortex [32,34,37,38,42,47,48,50,54,58,62,63,66,70,71,75,77] | ||
| EMG ACQUISITION | ||
| Setup | Details and references | |
| Number of electrodes | 16 [53]; 15 [33,58]; 13 [71]; 10 [37,62]; 8 [32,56,70,73,76,80]; 6 [40,49]; 5 [57,63,84]; | |
| 4 [38,39,42,47,48,51,59,65,68,69,75,81]; 3 [52,60,61,64,67]; | ||
| 2 [34,44,54,87,88]; 1 [41,43,55,66,72,77,78,79,82,83,85,86]; | ||
| Electrodes positioning | Single-joint | Wrist [43,44,50,54,59,61,62,64,66,67,73,75,78,81,83,85,86] |
| Arm [38,55,60,65,82,87,88] | ||
| Leg [34,72] | ||
| Ankle [41,51,77,79] | ||
| Face [74] | ||
| Multi-joint | Lower limb [42,47,48,49,53,63,80] | |
| Upper limb [32,33,37,39,40,52,56,58,70,71,76,84] | ||
| Trunk-upper limb [57] | ||
| Multi-limb | Upper limb [37,70,71,76] | |
| EEG Analysis Techniques | |
|---|---|
| Time domain analysis | ERP: [56,57,65,76,77] |
| Cortical waves amplitude/slope: [53,74,87,88] | |
| Frequency domain analysis | Average PSD: [34,41,42,47,49,52,59,65,72,75,79,83,86,87,88] |
| Quantitative index calculation: [55,60,62,73] | |
| Time-frequency analysis | ERD/ERS: [32,33,38,44,50,57,64,68,81] |
| ERSP: [42,47,63] | |
| Connectivity | Functional: [81,85] |
| Effective: [48,54,80] | |
| Sources reconstruction | ICA: [34,42,63] |
| LORETA: [58,71,80] | |
| EMG Analysis Techniques | |
| Time domain analysis | Amplitude/RMS: [34,55,58,59,60,63,73,74,77,79,80,83,86] |
| Additional time features: [39,64,65,71,87,88] | |
| Frequency domain analysis | Average PSD: [41,47,49] |
| Median frequency: [44,60,79] | |
| Time-frequency analysis | Channels coherence: [51] |
| Time-frequency decomposition: [47] | |
| Thresholding/landmark identification | EMG-EEG temporal synchronization: [54,57,62,72,81] |
| Identification of events: [48,56,71,85,86] | |
| Synergies | Non-negative matrix factorization algorithm: [32,33,53] |
| EEG-EMG Combination | |
| Cortico-muscular coherence | EEG-EMG coherence: [37,39,41,43,44,45,49,61,64,66,67,69,70,75,78,82,84] |
| EEG-EMG PDC/gPDC: [42,46] | |
| Time-frequency connectivity | Wavelet cross-spectrum: [38,51] |
| Cross-mutual information: [66,81] | |
| Pearson’s correlation: [47] | |
| Copula Granger’s causality: [40] | |
| Feature fusion for classification | Linear discriminant analysis: [65] |
| Support vector machine: [87,88] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brambilla, C.; Pirovano, I.; Mira, R.M.; Rizzo, G.; Scano, A.; Mastropietro, A. Combined Use of EMG and EEG Techniques for Neuromotor Assessment in Rehabilitative Applications: A Systematic Review. Sensors 2021, 21, 7014. https://doi.org/10.3390/s21217014
Brambilla C, Pirovano I, Mira RM, Rizzo G, Scano A, Mastropietro A. Combined Use of EMG and EEG Techniques for Neuromotor Assessment in Rehabilitative Applications: A Systematic Review. Sensors. 2021; 21(21):7014. https://doi.org/10.3390/s21217014
Chicago/Turabian StyleBrambilla, Cristina, Ileana Pirovano, Robert Mihai Mira, Giovanna Rizzo, Alessandro Scano, and Alfonso Mastropietro. 2021. "Combined Use of EMG and EEG Techniques for Neuromotor Assessment in Rehabilitative Applications: A Systematic Review" Sensors 21, no. 21: 7014. https://doi.org/10.3390/s21217014
APA StyleBrambilla, C., Pirovano, I., Mira, R. M., Rizzo, G., Scano, A., & Mastropietro, A. (2021). Combined Use of EMG and EEG Techniques for Neuromotor Assessment in Rehabilitative Applications: A Systematic Review. Sensors, 21(21), 7014. https://doi.org/10.3390/s21217014









