1. Introduction
The aging population has motivated interest in prolonging people’s ability to live independently. Many factors, such as an individual’s mental and physical condition as well as how comfortable or safe he/she feels living alone, affect an individual’s ability to live independently [
1]. Consequently, assessing an individual’s capability to live at home is a continuous process. Often, caregivers evaluate an elderly person’s independence via a questionnaire. However, this is a time-consuming process and the results do not always give an objective picture of the person’s status as answers can be interpreted subjectively by the caregiver, or the subject’s feedback can be inaccurate [
2]. Furthermore, it relies on a person’s ability and willingness to give an accurate overview of his health status and report important events such as illnesses, fall incidents, and changing sleep patterns. Unfortunately, elderly individuals often forget to mention these facts during interviews [
2].
Automated continuously monitoring involves collecting and analyzing data with minimal human involvement. This is an attractive option to support the elderly population’s health needs, which can be used to address several different tasks. One use is to automatically continuously and objectively collect data that may help assess an individual’s health status. Possibly, these data can even be analyzed to detect longer-term changes in a person’s behavior. A second use is to help an individual perform daily tasks, such as reminding him/her to take his/her medication [
3]. A third use is to raise an alarm if an event is detected that represents an immediate threat to a person’s health or well being such as falling [
4]. These examples illustrate how an automated approach can support both the elderly themselves by, for example, helping them remain self reliance (performing ADL, taking medicines, etc.) and their caregivers by, for example, promoting safety (estimating an individual’s risk of falling, detecting fall incidents, etc.). Ultimately, automated monitoring offers the potential to prolong an individual’s ability to live independently at home.
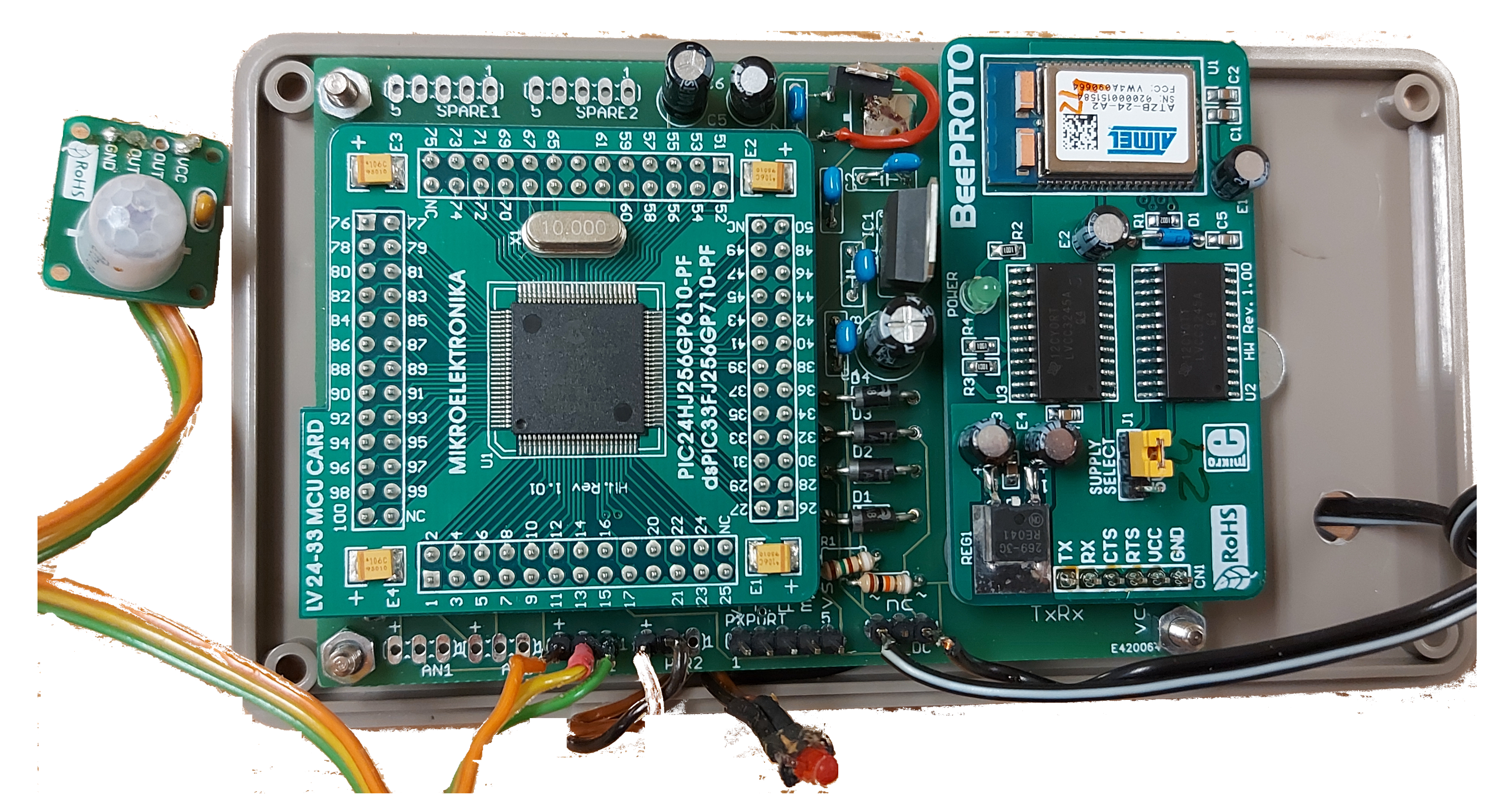
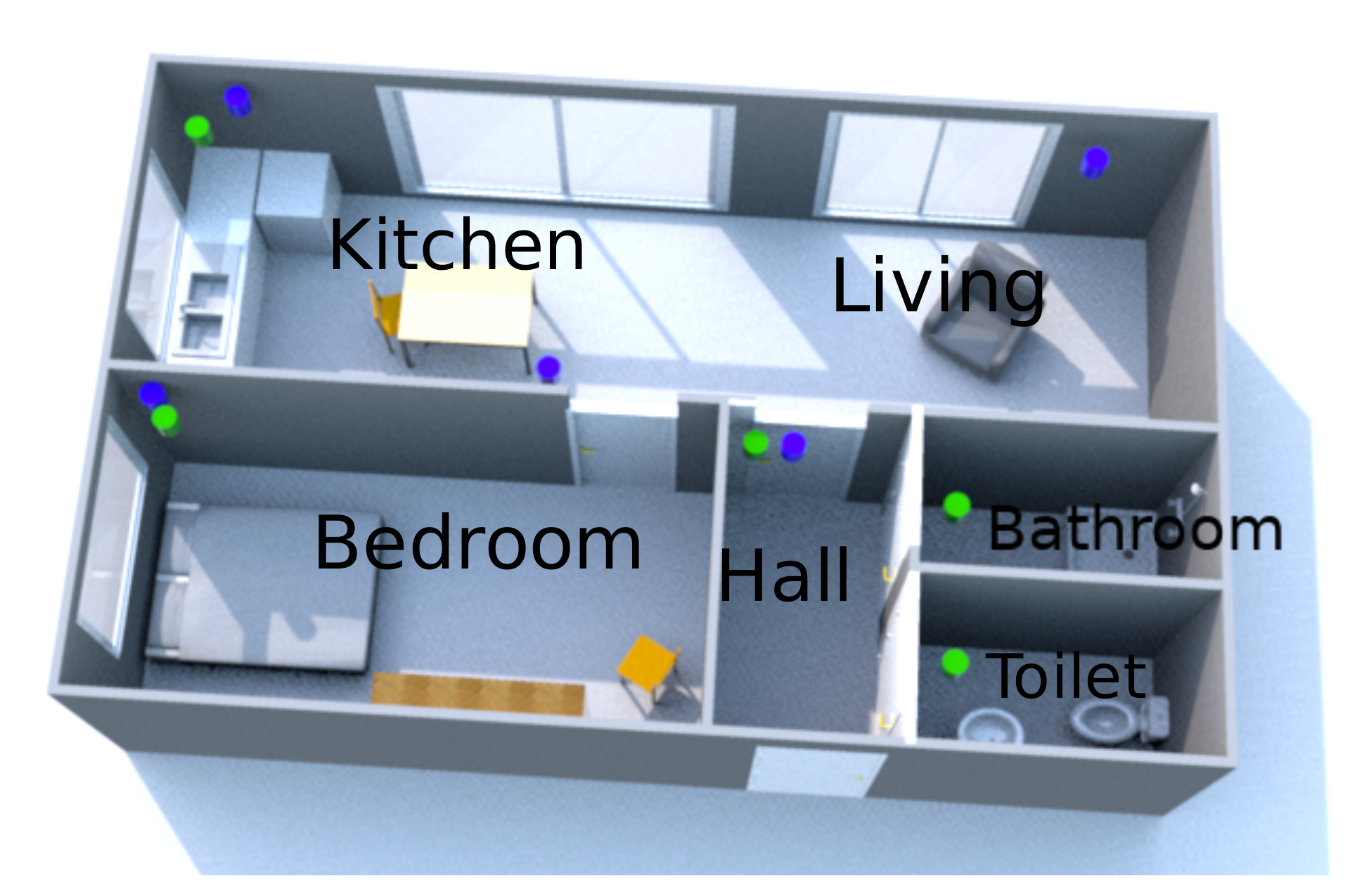
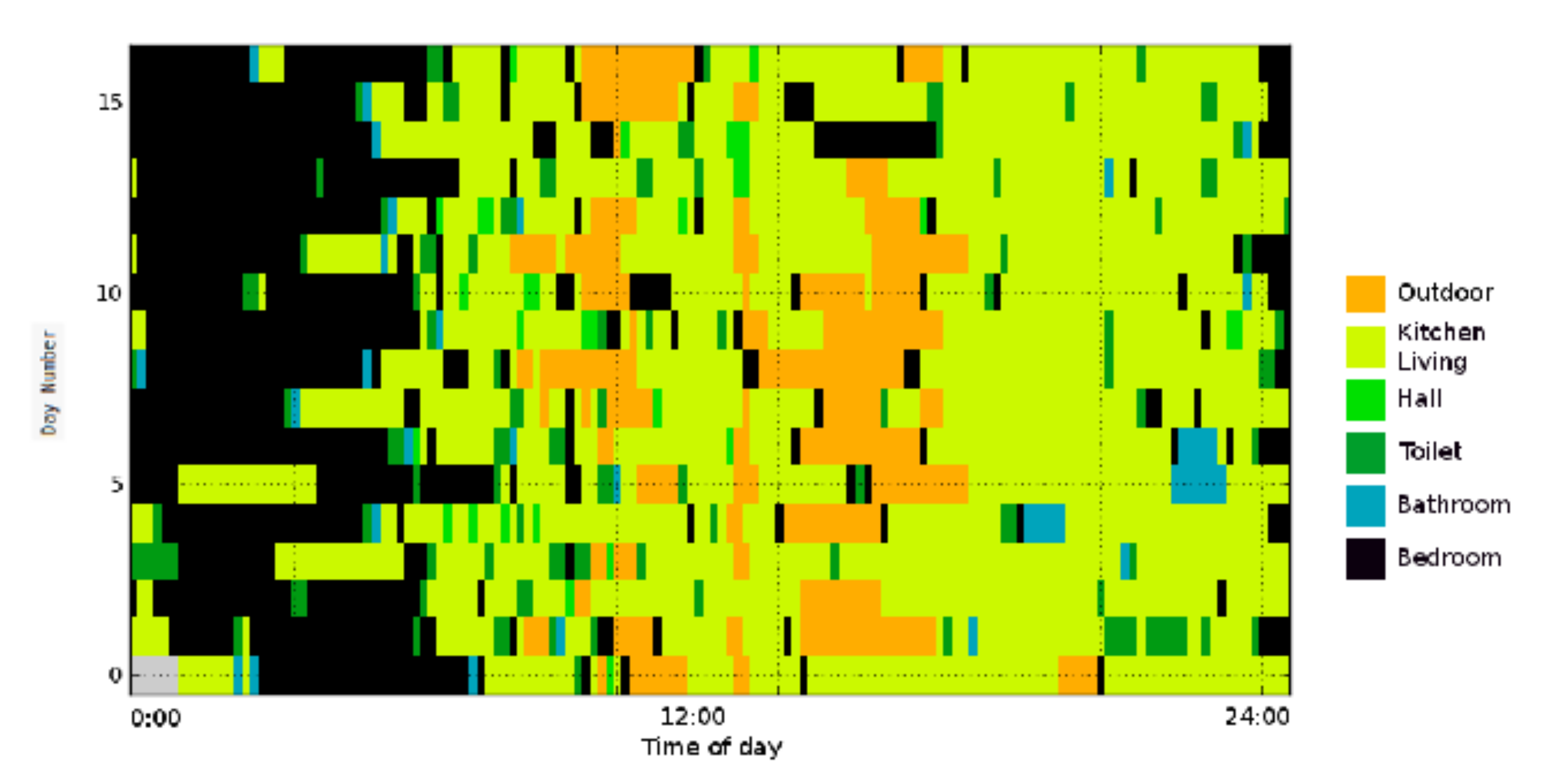
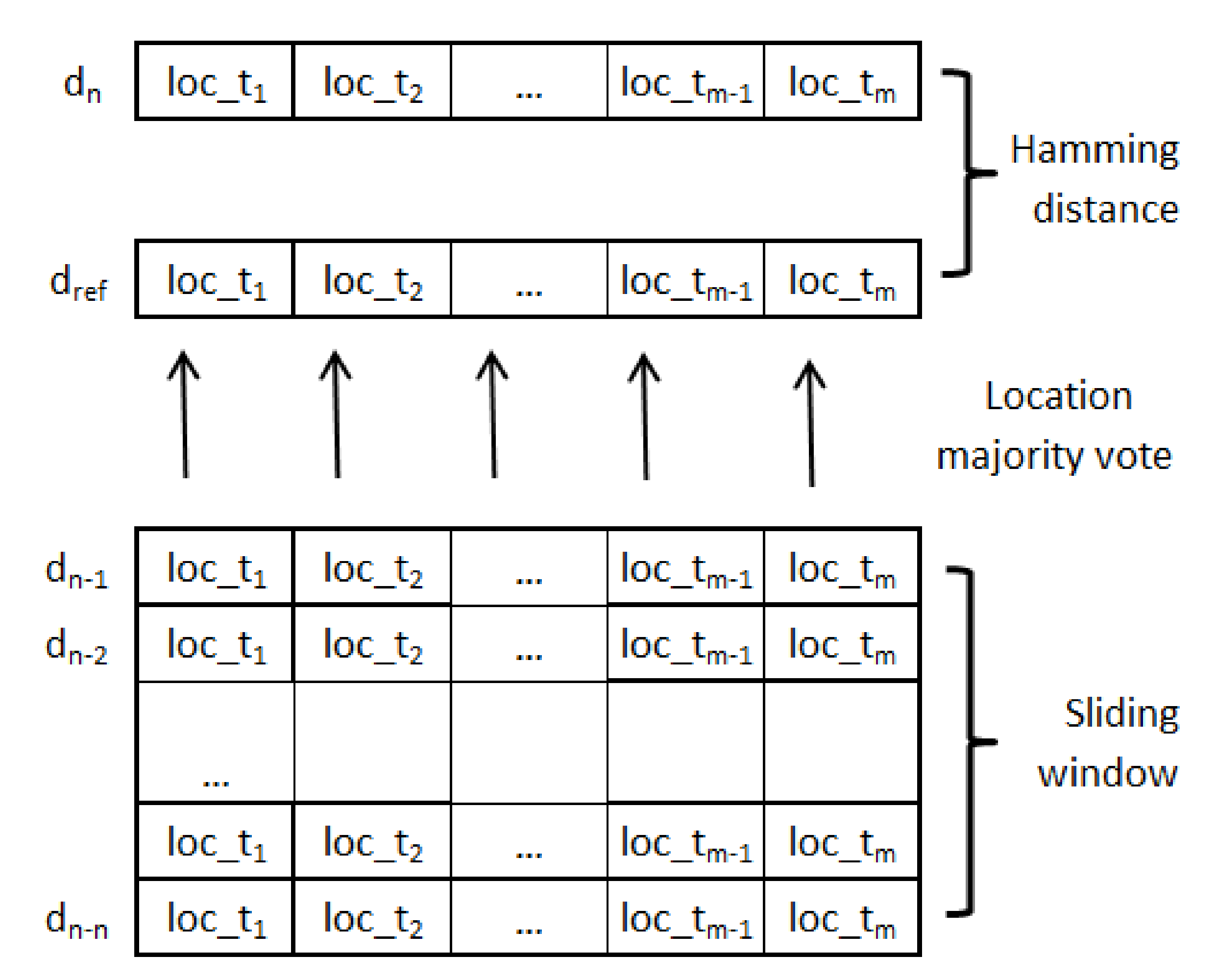
This paper describes a system that analyzes remote sensing data collected by non-intrusive, passive infrared motion detection sensors (PIR) to identify days that show locational behavior which deviates significantly from recent history. These deviations, indicating a change of habitual patterns, may be caused by the occurrence of an health-related event that needs attention. Our approach, Motion-Based Deviating Day Detector (MoBaDDD), analyzes a subject’s observed locational patterns by computing the distance between the current day’s presence pattern to a summary of the person’s recently observed presence patterns. A highly dissimilar day could indicate a condition such as being ill, having a fall incident, or a changing sleep pattern. After detecting a deviation, a statistical analysis of the underlying motion data helps the caregiver assess the subject’s status by providing clues about the cause of the deviating day through an information dashboard. An advantage of MoBaDDD is that it automatically establishes a baseline after a short period of data collection and thus does not require any person-specific background knowledge.
Our system distinguishes itself from other research in the combination of specific approaches. It is a completely self-learning, data-driven unsupervised system, unlike many other systems [
5,
6,
7,
8]. It uses only motion data from a simple motion sensor, in contrast with multimodal sensor systems [
7,
8,
9,
10,
11,
12,
13]. Besides detection of a deviating day, it also provides the caregiver with a possible cause of the deviation unlike other research [
6,
8,
9,
11,
12,
14]. It also uses a general, agnostic approach which detects anomalies on a very generic level. Information as to the probable cause of the anomaly is also provided to the caregiver.
The proposed algorithm is evaluated on both simulated and real-world data. The simulated data are used to test the algorithm and to tune the initial system’s parameters. Real data were collected from the homes of three single older individuals for between three and 18 months. Solely for the purpose of validating this research, video cameras were also installed to obtain ground-truth labels and to verify detected events. From the collected data, our algorithm was able to detect deviating events such as when the subject was ill, fell, or slept in the living area as opposed to the bedroom. A clinical researcher visited each subject every two weeks for interviews and status evaluation. These observations, together with the video images, provided correlations between events detected by the algorithm and the findings from the researcher.
2. Related Work
Active assisted living for supporting older people is a very active area of research. Systems using sensors can monitor behavior and physiological data to monitor and detect specific health or social related issues. Examples in this domain of research are Austin et al. [
15] who use sensors to detect loneliness or Marschollek et al. [
16] and Mellone et al. [
17] who focus on fall risk specific assessment. Other examples are detection of respiratory problems [
18] and detection of urinary tract infections [
19]. Next to this research domain towards specific targets, there has also a wide variety of work been done in detecting general anomalies in behavior of older persons. Our research also focuses on detection of these more general anomalies. These changes in behavior can be an early indicator of functional, health or cognitive decline of an elderly. These anomalies can be disturbances in performing activities, changing activity levels, changing mobility or a significant change from an elderly person’s regular behavior. This overview only considers research that detects anomalies using sensors integrated into a resident’s environment as this is the most closely related area to this work. Additionally, wearables deployed for this purpose are often considered to be intrusive and there is always the risk that people forget to wear them.
Within the research of detecting anomalies, different approaches exist; supervised versus unsupervised systems, multimodal and single modal systems, general agnostic anomaly detection and ADL specific based detection. Finally, it is also important to consider which information in which format is given to the caregiver.
In [
6], learning is supervised by annotating activities through diary notations by the elderly. Supervised learning is also used in [
7], where the subjects are asked to perform predefined tasks, and in [
5], where only one appliance is used to detect anomalies. Our work is unsupervised and data-driven; only a short learning period is used to set user-specific detection thresholds.
As for multimodal and single modal systems, researches such as those in [
7,
9,
10,
11,
20,
21] use more than one sensor modality to detect activities and anomalies. For example, Cook et al. [
9] use sensors to detect water flow, motion, temperature, burner, phone use, and others to characterize the quality of activities and detect anomalies. They constructed a labeled dataset and assessed the performance of five predefined activities. The anomalies are defined by the inconsistency of performing activities, such as difficulties in finding a telephone number, leaving the burner on, or forgetting to take medication. Activity performances are considered anomalous if the time they take to complete differs from the normal distribution by +/−2
. The quality of performance of activities is considered an indicator for functional wellbeing. Skubic et al. [
8] use a bed sensor, a temperature sensor, and motion sensors. Lundstrum et al. [
11] use door, motion, as well as bed and chair occupancy sensors to model, detect, and explore short time changes in human behavior. They use a technique derived from Random Forests to detect deviating patterns in time (e.g., eating breakfast at night), in space (e.g., falling in the bathroom), and in transition (e.g., waking up at night and leaving the home. Paudel et al. [
7] rely on the CASAS dataset from Washington State University to discover patterns and anomalies in the activities of residents. This dataset contains sensors for motion, temperature, item use, burner use, hot and cold water, and open or closed doors. Using a graph-based method, they detect anomalies as sign of health decline in the elderly. Nadeem et al. [
21] use the built in sensors of a smartphone to classify human activity which requires the smartphone to be attached to the waist of the test person. Jain et al. [
10] use the classification of activities resulting from multiple sensors deployed in a TigerPlace, such as motion sensors, bed sensors, and Microsoft Kinect sensors. While the results of these researches are promising to detect anomalies, they require a complex installation and maintenance procedure or very specific setup and calibration. Our system uses only simple, robust PIR sensors, in a meshing network which assures simple installation.
On the abstraction level of anomaly detection, there is a difference between a general, agnostic approach such as ours and an approach in which first ADL are classified. For instance, several studies focus on classifying activities before detecting anomalies, such as in [
5,
7,
9,
14]. Cook et al. [
9] use five predefined activities which represent basic and complex activities from activities of daily living (ADL) to perform a quality assessment. Aramendi et al. [
14] assess the functional health of elderly by first detecting activities from the instrumental activities of daily living-compensating (iADL-C) scale. Paudel et al. [
7] use activity detection strongly based on iADL to detect temporal, spatial and behavioral anomalies. Furthermore, Alcala et al. [
5] use one predefined activity, kettle use, to define behavior and deviation of this behavior. They learn a household individual schedule for kettle usage. Kettle usage outside the prediction model is considered an anomaly and an alert is raised. However, activities are confined to only one activity. Although activities defined in instruments such as ADL and iADL clearly indicate the functioning ability of a person, we believe that these miss some important behavioral changes such as wandering behavior or changing sleep wake patterns. Therefore, existing approaches may not detect anomalies related to these phenomena.
Another approach for detecting anomalies is to map behavior to a model or to compare current observations to recent history. The authors of [
12,
14] use the first rule. Mshali et al. [
12] build a forecasting behavioral model to compare to a Markovian modeled dataset to detect deviations. They use activities from the Functional Autonomy Measurement System (SMAF) which is used to assess dependency. Activities used are from ADL (e.g., washing, toileting), mobility (e.g., walking), communication (e.g., speaking), and iADL (e.g., sleeping). For these activities the duration and frequency is monitored. If observed duration or frequency for performing an activity is outside the forecasted limits, it is considered an anomaly. Furthermore, Aramendi et al. [
14] built several classification models to explore the possibility of detecting functional health decline.
To detect anomalies, some researches use experimentally defined thresholds. For example, Jain et al. [
10] use a threshold to define a deviation if an activity is higher than an experimental defined threshold above the mean from the last two observed weeks. Novak et al. [
22] use Self-Organized Maps over motion activities to detect anomalies, but this approach requires manually tuning a timing parameter to avoid false alarms. By contrast, our approach uses a threshold that is automatically set and which can adapt to an individual’s lifestyle behavior, given a small unsupervised learning period.
Finally, it is important to look at the information given to the caregiver resulting from anomalies detection. In many studies, this is long or intermediate term information such as gradual functional decline [
5,
9], health decline [
6,
12,
14], or cognitive decline [
7], among others. In [
8], deviating days are reported to the caregiver, who has to invest sensor data to determine the root of the anomaly. Our work focuses on providing immediate information to the care giver about current observations that deviate from what is expected.
The above-mentioned researches provide an overview about how anomalies can be detected to give an indication of a person’s functional or health condition. In our research, we developed a system that informs the caregiver if in the last 24 h period a deviation has occurred using a clear semantic feedback to the caregiver. It only uses one simple sensor modality, motion sensors, which largely simplifies installation and maintenance. The system is unsupervised and can be used to monitor a person’s health status and aid older people who live alone. Several principles informed the design of our approach, and help contrast it with prior work. When developing our system, we wanted to extract health related information, assess this information, and alert the caregiver if possible health related events have occurred. To lower the acceptation threshold of technology by elderly [
19], we focused on a non-intrusive and contactless monitoring framework that uses readily available and low-cost sensors. This contrasts with work that uses expensive sensors [
7,
9] or intrusive ones [
10,
11]. We aimed for a simple and reliable prediction framework that is able to automatically adapt to each person’s individual living habits without needing to extensively configure and tune the system. We analyze an individual’s behavior by considering their observed presence patterns within their living environment and detecting when they deviate from their typical pattern. Finally, we provide the caregiver with information that describes how the current observations deviate from baseline behavior. For instance, this may entail stating that the person spent significantly more time in the bedroom on a specific day than in the recent past.
4. Results for the Small-n Case Study
To test the MoBaDDD algorithm, a small-n case study (n = 3) has been performed on the real-life data collected from the three previously described locations. Using these data, the following three questions are evaluated:
How do the different choices of in the -measure reflect usability in a real-life setting?
What is the algorithm detection capability for the chosen parameter set n, ?
How do the statistical model’s suggestions about the underlying cause of the deviating day compare to observations from the corresponding video data?
4.1. Case Study Method
Based on the analysis in
Section 3.4.2, we use the parameters according to
Table 3. The analysis begins after
day as the first
n days are used to calculate statistical data to define the mean and standard deviation of the Hamming distance, and the second
n days are used to construct the reference day. Every detected deviating day is verified by manually inspecting the video data and checking the clinical researcher’s observational reports from the visits to the subjects. Note that video cannot reveal missed events (FNs) by itself, and therefore we rely on interviews with the subjects to identify possible FNs.
4.2. Case Study Results
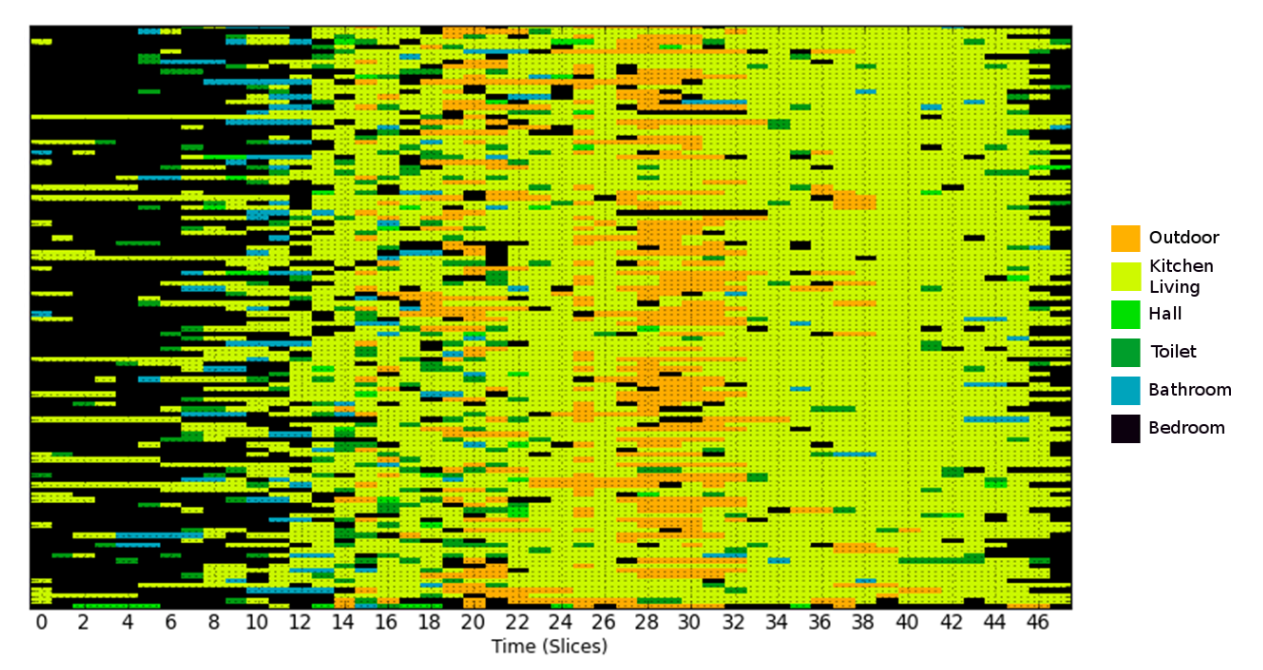
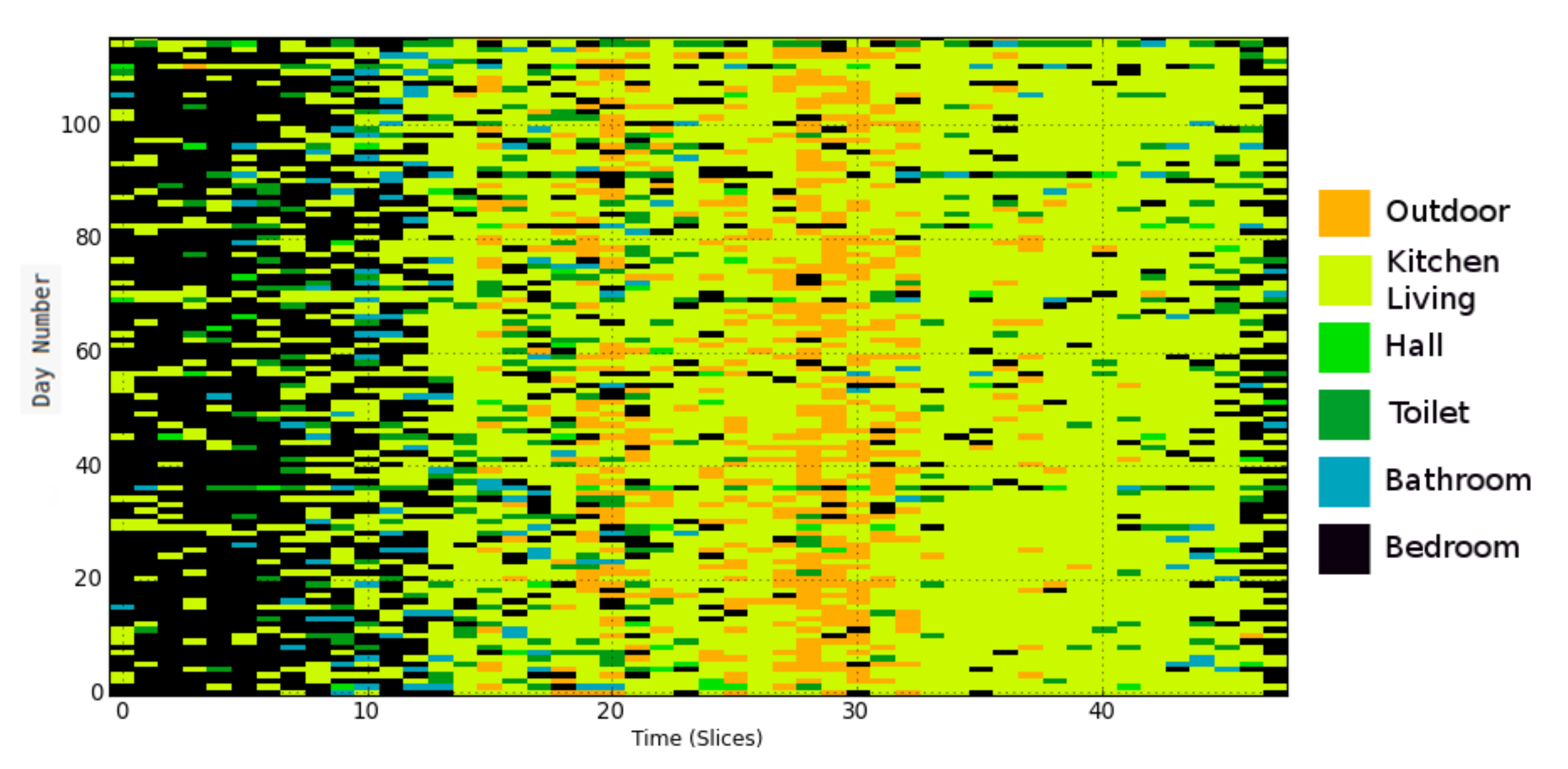
Table 4 shows an overview of the detected days that deviate from recently observed behavior for all three locations.
Next, we discuss the results for each location in detail.
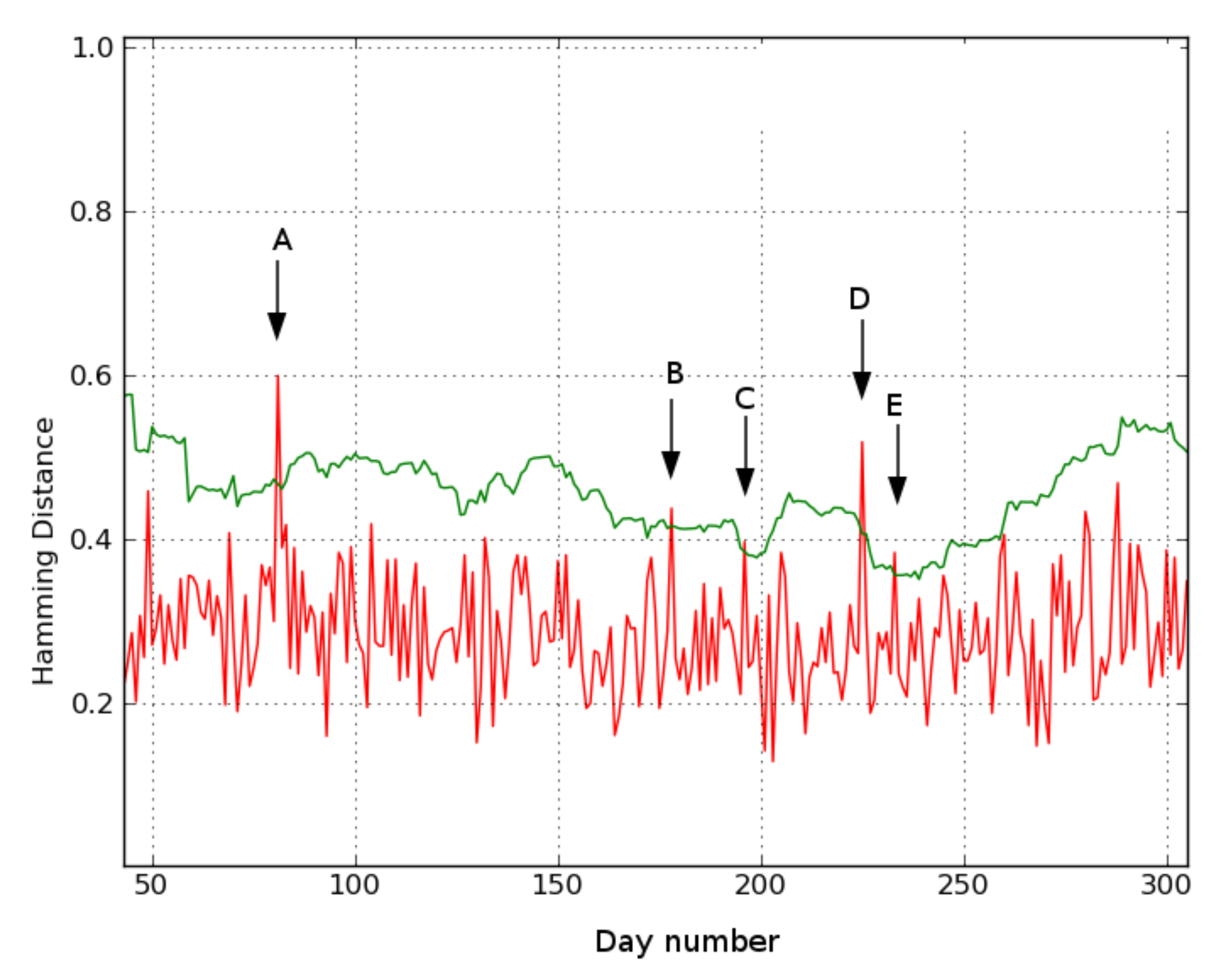
Location 1.
Figure 8 shows the results for location 1. Days 81 (A), 178 (B), 196 (C), 225 (D), and 233 (E) exceed the threshold and are flagged by the system as deviations.
Days A and B show a deviating behavior. On day A, the video and underlying presence data reveal that the subject does not go to his bedroom that night. Instead, from 11:50 p.m. on the previous day, he sits at the table in his living room, falls asleep, and remains there until 5:30 in the morning. He then gets up and resumes his daily activities without having slept in his bed. Similarly, on day B, the person again does not go to his bedroom at night and instead falls asleep sitting at his living room table. On Day D, the underlying data reveal that a sensor error leads to the deviation. Although this is not of clinical relevance, it is an important detection from the perspective of monitoring the system’s status. In a later version of the system, this type of error is automatically reported via the heartbeat mechanism. On days C and E, no obvious deviating behavior appears in either the videos or the heat maps. These days can be considered false positives.
Location 2.
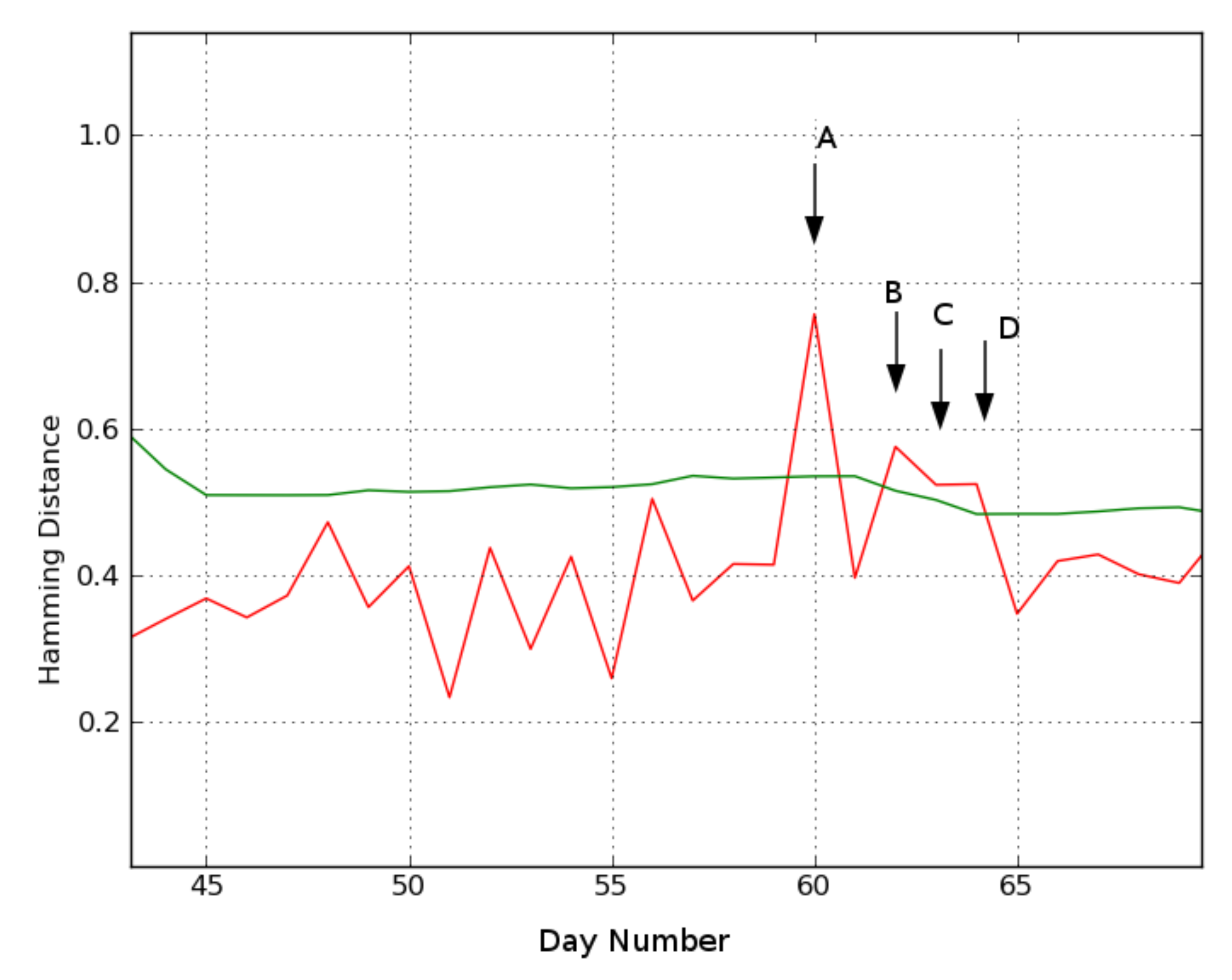
Figure 9 shows the results for location 2, where days 60 (A), 62 (B), 63 (C), and 64 (D) are identified as deviating.
The video data for day A reveal that the subject is in the bathroom from 7:45 p.m. the previous day until 2:30 a.m. Then she gets ready for bed, but instead of going to bed, lies in a chair in the living room. As no cameras are installed in the bathroom, it is impossible to deduce what activities were performed. However, the length of the bathroom stay is exceptional and therefore possibly relevant to a caregiver.
Day B is flagged as another deviating behavior by the MoBaDDD algorithm. Video assessment reveals that the subject naps in the bedroom in the afternoon. After napping, she wanders around, takes some medicine, looses her balance and eventually falls in the bathroom. Then, she crawls towards her bedroom where she remains on the ground for several hours. She pulls some sheets from the bed to cover her and she stays in that position until she is found during the night by a nurse.
Day C differs from recent behavior because the person spends most of her time in the bedroom. A caregiver can use this information and the information of the previous day’s fall incident to further assess her health condition.
Finally, on day D the subject spends significantly more time than usual in the bathroom during the day and she spends time in the living room during the night.
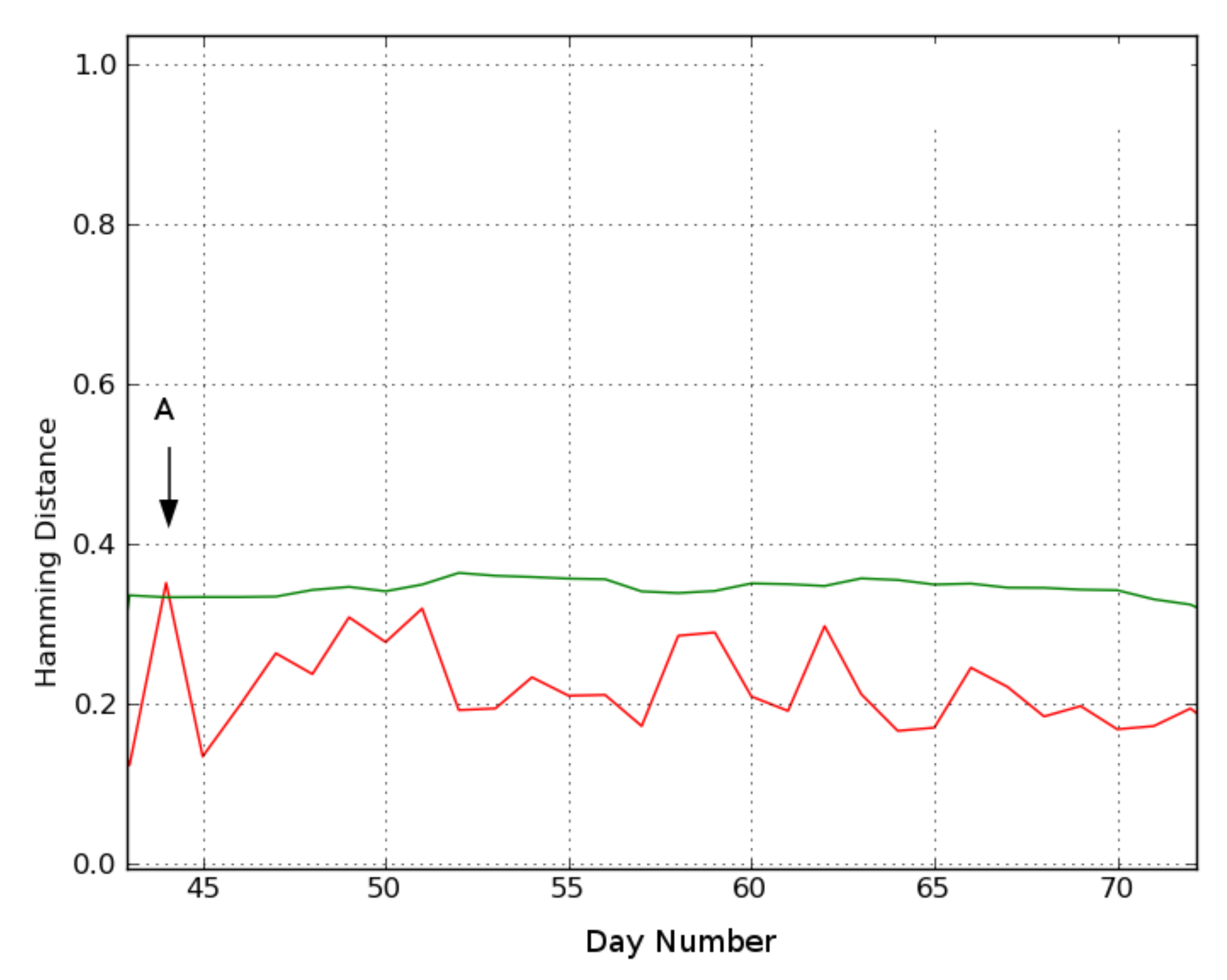
Location 3. Finally,
Figure 10 shows the results for location 3, where only day 44 (A) is considered deviating. Day A’s video reveals that the subject leaves her residence in the afternoon for a substantially longer period than in her recent history, which is not strictly an indication of any abnormal behavior.
4.3. Results from Comparison of Visual Conclusions with Statistically Generated Clues
The deviating days found at all three locations were analyzed by applying the statistical method from
Section 3.3.3 to the underlying presence data.
Table 5 compares the findings from visually inspecting the video data to the statistical method’s output. Recall that the statistical moments model merely provides clues, not all of which are conclusive. However, they mostly agree with the findings from analysis of the video data. For example, on day A in location 1 the subject did not go to his bedroom that night. Here, the system suggested less time was spent in the bedroom and more time was spent in the living room than was expected. These hints support the conclusion from the video data. On day B at location 1, the system suggested that more time was spent in the toilet while this was not observed otherwise. This could give a caregiver another anchor when interviewing the subject.
5. Discussion
In this paper, a system is proposed to assist in assessing longitudinally and continuously the health condition of older people living alone. It does this by providing behavior related information otherwise unknown to the caregiver. An ideal system for this task should have several characteristics:
Be low-cost so it is widely applicable;
Be easy to install in a home (i.e., does not require significant renovation);
Be non-intrusive and not rely on the subject to wear or use special equipment;
Generate a limited number of false positives;
Respect the privacy of the subject.
This paper details our work in developing such a system. It relies on using simple motion detector data.
Having a continuous monitoring presence patterns provides a means to detect days that stand out compared to recently observed history. The information obtained can provide valuable input to a caregiver who no longer has to rely on possibly subjective and incomplete information given by an elderly individual. The system will detect incidental behavioral changes on a day-to-day basis. As every person has a very specific behavioral pattern, the system automatically adapts to the circadian rhythm of the person. Consequently, the system does not require a tedious and detailed configuration for each installation. Detecting deviating events is typically done at the end of each day, but the algorithm allows for analyzing the current day earlier on, e.g., in the morning or at noon. Slowly evolving or gradual changes are not detected by our system and they would require other algorithmic design choices.
The proposed algorithm has been tested in a case study where three people were monitored. In all three locations, days were detected with possible relevant clinical information such as fall incidents, possible illness, and a disturbed sleep–wake pattern. Some of these were not reported by the subjects, which highlights the value of continuous monitoring. In location 1, two days were detected where the subject did not sleep in his bedroom, which may indicate a disturbed sleep–wake balance. This was not reported by the subject, but can be a valuable piece of information for a caregiver, who can investigate the cause of this behavior. A similar behavior is detected in location 2 on day A. Knowing that the subject does not sleep in the bedroom enables the caregiver to take preventive actions to help the subject.
The fall incident at location 2 on day B is clearly clinically relevant. Furthermore, the sensor data, e.g., in the heatmap, show that several hours elapsed between the fall and when the subject was found. This information would be missing if the subject does not report it. Two days following the fall incident, the subject spent most of the day in the bedroom (day C) or in the bathroom (day D). If given this information, the caregiver can check if it is related to the fall incident on day A by, for instance, specific interviewing.
Furthermore, to aid the caregiver in his assessment, a statistical evaluation method for the underlying data is proposed to help find the cause of the deviating day. The caregiver (e.g., nurse, general practitioner, or family) can decide if the provided information has clinical relevance by using the system’s clues when talking with the monitored person. As illustrated on day B for location 1, the system suggested that the person spent more time in the toilet than in previous days. However, it is not yet robust enough to conclusively indicate the root cause of the change in behavior. The caregiver can use the system’s suggestions to augment his own expertise to reach a conclusion. In the future, a more elaborate system can be developed based on these findings.
An important advantage of MoBaDD is its self-learned and adaptive threshold (Equation (
2)). The threshold is set only based on a short learning period (i.e., no other person-specific information is needed), with results indicating around two or three weeks of data is sufficient. In this research, appropriate thresholds were selected using synthetic data that was generated from a model based on the characteristics of real-world data. Our automatically learned and updated thresholds would be highly beneficial for a large-scale installation of such a monitoring system.
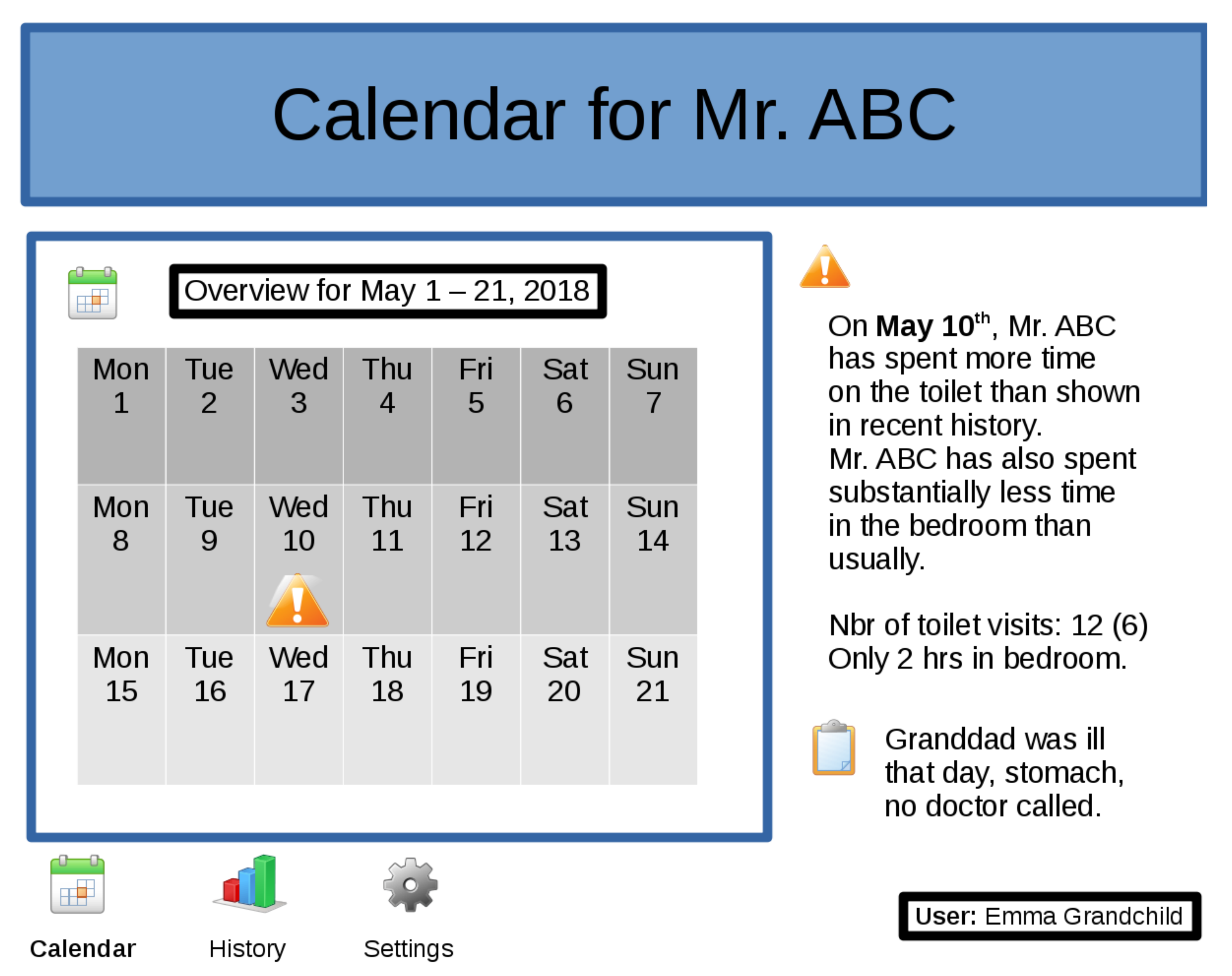
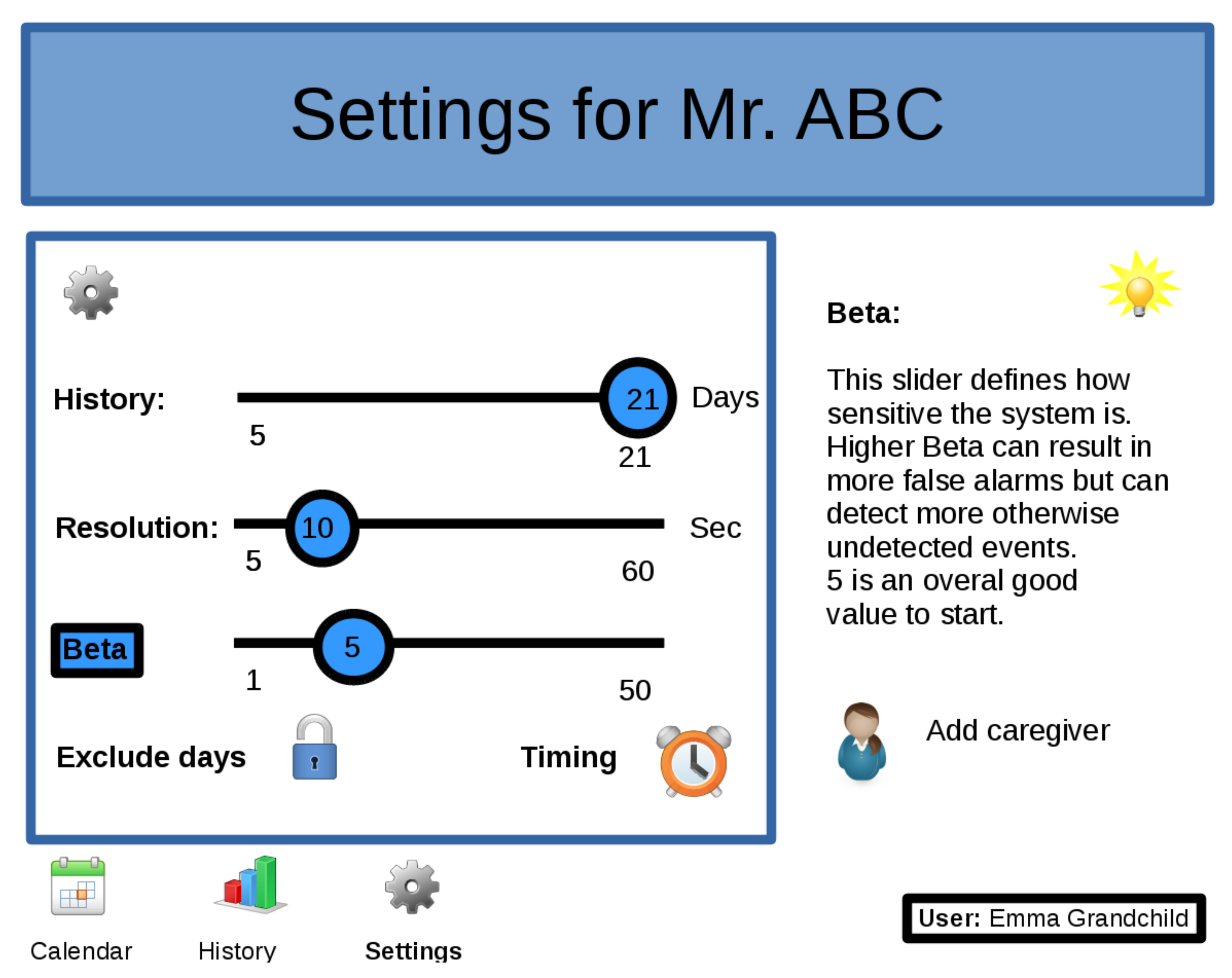
Still, it is possible to fine-tune the system individually with respect to reported events, which provides an opportunity to balance false positives against the risk of missing important events. For example, a deployed version could include a dashboard, as in
Figure 5, to give feedback, such as recent or historical overviews, in a user-friendly way to the caregiver. It would also be possible to allow a caregiver to tune the system’s parameters via a setup page as shown in
Figure 11. A self annotation mechanism, active during the learning phase of the system, could help to easily distinguish between real events and false positives. The user can also define when the system should do the analysis (e.g., at the end of the day or at midday) and which days should be excluded for analysis (e.g., weekend days, day when a trip is planned, etc.).
However, the system has some limitations. It is not guaranteed to detect all days that contain health or otherwise important events. Monitoring is limited to a person who is living alone without any free-running pets. Visits are difficult to automatically detect from the available data. Future research will address these issues. Furthermore, the specificity of the statistical method to assist the caregiver in his conclusions could be increased. On the other hand, the system can naturally capture seasonal changes. It also has the potential to account for weekly activities by constructing a day-specific reference day (e.g., compare Wednesdays to a reference day built only from recent Wednesdays). As this study only involved three participants, more clinical evidence can be collected on a more elaborate study. Furthermore, we intentionally limited ourselves to one sensor type. Other sensor types (e.g., door sensors, bed presence sensors, etc.) could give a more detailed picture of the behavior and could be explored in future work.
Table 6 shows an overview of the technical characteristics, advantages, and disadvantages of the developed system.
Finally, concerning the privacy of the subject, as Meingast et al. discuss in [
32], sensor networks and monitoring systems such as these can improve healthcare, both on a quality as a cost of care level. However, privacy and security concerns should be dealt with. In the implementation of systems like these, utter care should be given to issues like ownership of data, can the user control who gets to see which information, are the communication layers securely implemented, and what sort of data should be stored and where.
Resumptive Comparative Analysis
As discussed in
Section 1 and
Section 2, a lot of research has been done on active assisted living for supporting older people. In this section, we present a short synthesis of systems mentioned in those sections, in comparison with our system. We consider here three grounds of contrast, as we consider them to be essential for a monitor system given the characteristics as described in
Section 5: technical implementation, the abstraction level of anomaly detection, and the information provided related to the deviating event.